Abstracts
PURPOSE: To investigate the body weight, pulmonary function and quality of life of twenty patients with morbid obesity six months after the Fobi-Capella operation. METHODS: Patients were evaluated before and six months after surgery. The patients were mainly female (75%), the average age was 40.5 ± 10.27 years; average weight 110.11 kg ± 21.77 and average body mass index (BMI) 39.93 ± 7.13 kg/m² in the postoperative evaluation. Pulmonary function was assessed by spirometry using a Pulmonet/Godart NV Bilt Vetr Hotland spirometer and quality of life was assessed by applying the Moorehead-Ardelt questionnaire. The pre- and postoperative spirometry values were compared by the paired Student t test and the correlation between weight loss and pulmonary function was determined by linear regression, with the level of significance set at p < 0.05. RESULTS: The spirometry variables Respiratory Frequency (RF), Expiratory Reserve Volume (ERV) and Functional Residual Capacity (FRC) differed significantly between the pre- and postoperative periods, whereas Residual Volume (RV), Vital Capacity (VC), Total Lung Capacity (TLC), FEF25-75 (Forced Expiratory Flow between 25 and 75% FVC) and FEV1/FVC% (Forced Expiratory Volume in the 1st second/ Forced Vital Capacity ratio) did not differ between periods. Only one patient reported worsening of quality of life. There was a positive correlation between weight loss and ERV (p=0.0117, r=0.5514), but no correlations were observed for the other variables. CONCLUSIONS: There was a significant weight loss and an improvement of pulmonary function as seen by respiratory frequency, reduction and increased expiratory reserve volume and functional residual capacity. The quality of life of the patients also improved after the Fobi-Capella operation.
Obesity, Morbid; Respiratory Function Tests; Quality of Life; Bariatric Surgery
OBJETIVO: Investigar a evolução do peso corpóreo, da função pulmonar e da qualidade de vida de 20 pacientes obesos mórbidos seis meses após operação de Fobi-Capella. MÉTODOS: Os pacientes foram avaliados antes e seis meses após a cirurgia e o sexo feminino predominou em 75%, com média de idade de 40,5 anos ± 10, 27, média de peso de 110,11 kg ± 21,77 e IMC de 39,93 kg/m² ± 7,13. Para a avaliação da função pulmonar foi realizada espirometria por meio do espirômetro Pulmonet Godart NV Bilt Vetr Holland, e para a qualidade de vida foi aplicado o questionário de Moorehead-Ardelt. As comparações entre os valores espirométricos do pré e do pós-operatório foram realizadas pelo teste t de Student para amostras pareadas, e para a correlação entre a perda de peso e função pulmonar utilizou-se análise de regressão linear simples, adotando-se p < 0,05 para todos os resultados. RESULTADOS: As variáveis espirométricas Freqüência Respiratória (FR), Volume de Reserva Expiratório (VRE) e Capacidade Residual Funcional (CRF) apresentaram, aos seis meses após a operação, diferença estatisticamente significativa com os valores pré-operatórios, porém, não houve diferença significativa de Volume Residual (VR), Capacidade Vital (CV), Capacidade Pulmonar Total (CPT), Fluxo Expiratório Médio entre 25 e 75% da curva de CVF (FEF25-75%) e Razão entre Volume Expiratório Forçado no 1º segundo e Capacidade Vital Forçada (VEF1/CVF %). Apenas uma paciente relatou piora da qualidade de vida após a operação. Houve correlação positiva entre a perda da porcentagem do excesso de peso e VRE (p=0,0117, r=0,5514); as demais variáveis não apresentaram correlação significativa. CONCLUSÕES: Houve perda significante de peso, melhora da função pulmonar evidenciada pela redução da freqüência respiratória, aumento do volume de reserva expiratório e da capacidade residual funcional. A qualidade de vida dos pacientes melhorou nos seis meses após a operação de Fobi-Capella.
Obesidade Mórbida; Testes de Função Respiratória; Qualidade de Vida; Cirurgia Bariátrica
5 ORIGINAL ARTICLE
ALIMENTARY TRACT
Pulmonary function and quality of life in patients with morbid obesity six months after bariatric surgery1 1 Research performed at Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, University of Sao Paulo (USP), Brazil.
Função pulmonar e qualidade de vida em pacientes obesos mórbidos seis meses após cirurgia bariátrica
Márcia Arruda Fajardo XavierI; Reginaldo CenevivaII; João Terra FilhoIII; Ajith Kumar SankarankuttyIV
IPhysiotherapist, MSc, University Hospital, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, USP, Sao Paulo, Brazil
IIFull Professor, Division of Digestive Surgery, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, USP, Sao Paulo, Brazil
IIIFull Professor, Department of Internal Medicine, Head of the Laboratory of Pulmonary Function, Faculty of Medicine of Ribeirao Preto, USP, Sao Paulo, Brazil
IVAssistant Professor, Division of Digestive Surgery, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, USP, Sao Paulo, Brazil
Correspondence Correspondence: Márcia Arruda Fajardo Xavier/Prof. Dr. Reginaldo Ceneviva Departamento de Cirurgia e Anatomia (9º andar) Faculdade de Medicina, Universidade de São Paulo Av. dos Bandeirantes, 3900 14048-900 Ribeirão Preto SP Brasil Phones: (55 16)3966-7618 / 3602-2508 / 9729-0973 marcia.usp@gmail.com / marciaxavier@usp.br
ABSTRACT
PURPOSE: To investigate the body weight, pulmonary function and quality of life of twenty patients with morbid obesity six months after the Fobi-Capella operation.
METHODS: Patients were evaluated before and six months after surgery. The patients were mainly female (75%), the average age was 40.5 ± 10.27 years; average weight 110.11 kg ± 21.77 and average body mass index (BMI) 39.93 ± 7.13 kg/m2 in the postoperative evaluation. Pulmonary function was assessed by spirometry using a Pulmonet/Godart NV Bilt Vetr Hotland spirometer and quality of life was assessed by applying the Moorehead-Ardelt questionnaire. The pre- and postoperative spirometry values were compared by the paired Student t test and the correlation between weight loss and pulmonary function was determined by linear regression, with the level of significance set at p < 0.05.
RESULTS: The spirometry variables Respiratory Frequency (RF), Expiratory Reserve Volume (ERV) and Functional Residual Capacity (FRC) differed significantly between the pre- and postoperative periods, whereas Residual Volume (RV), Vital Capacity (VC), Total Lung Capacity (TLC), FEF25-75 (Forced Expiratory Flow between 25 and 75% FVC) and FEV1/FVC% (Forced Expiratory Volume in the 1st second/ Forced Vital Capacity ratio) did not differ between periods. Only one patient reported worsening of quality of life. There was a positive correlation between weight loss and ERV (p=0.0117, r=0.5514), but no correlations were observed for the other variables.
CONCLUSIONS: There was a significant weight loss and an improvement of pulmonary function as seen by respiratory frequency, reduction and increased expiratory reserve volume and functional residual capacity. The quality of life of the patients also improved after the Fobi-Capella operation.
Key words: Obesity, Morbid. Respiratory Function Tests. Quality of Life. Bariatric Surgery.
RESUMO
OBJETIVO: Investigar a evolução do peso corpóreo, da função pulmonar e da qualidade de vida de 20 pacientes obesos mórbidos seis meses após operação de Fobi-Capella.
MÉTODOS: Os pacientes foram avaliados antes e seis meses após a cirurgia e o sexo feminino predominou em 75%, com média de idade de 40,5 anos ± 10, 27, média de peso de 110,11 kg ± 21,77 e IMC de 39,93 kg/m2 ± 7,13. Para a avaliação da função pulmonar foi realizada espirometria por meio do espirômetro Pulmonet Godart NV Bilt Vetr Holland, e para a qualidade de vida foi aplicado o questionário de Moorehead-Ardelt. As comparações entre os valores espirométricos do pré e do pós-operatório foram realizadas pelo teste t de Student para amostras pareadas, e para a correlação entre a perda de peso e função pulmonar utilizou-se análise de regressão linear simples, adotando-se p < 0,05 para todos os resultados.
RESULTADOS: As variáveis espirométricas Freqüência Respiratória (FR), Volume de Reserva Expiratório (VRE) e Capacidade Residual Funcional (CRF) apresentaram, aos seis meses após a operação, diferença estatisticamente significativa com os valores pré-operatórios, porém, não houve diferença significativa de Volume Residual (VR), Capacidade Vital (CV), Capacidade Pulmonar Total (CPT), Fluxo Expiratório Médio entre 25 e 75% da curva de CVF (FEF25-75%) e Razão entre Volume Expiratório Forçado no 1º segundo e Capacidade Vital Forçada (VEF1/CVF %). Apenas uma paciente relatou piora da qualidade de vida após a operação. Houve correlação positiva entre a perda da porcentagem do excesso de peso e VRE (p=0,0117, r=0,5514); as demais variáveis não apresentaram correlação significativa.
CONCLUSÕES: Houve perda significante de peso, melhora da função pulmonar evidenciada pela redução da freqüência respiratória, aumento do volume de reserva expiratório e da capacidade residual funcional. A qualidade de vida dos pacientes melhorou nos seis meses após a operação de Fobi-Capella.
Descritores: Obesidade Mórbida. Testes de Função Respiratória. Qualidade de Vida. Cirurgia Bariátrica.
Introduction
Obesity is a worldwide disease of increasing prevalence, currently representing a major public health problem superimposed on ancient problems such as malnutrition and infectious-contagious diseases in emerging countries such as Brazill1,2. The health consequences of obesity range from a higher risk of premature death to severe chronic diseases that reduce the quality of life1.
Obesity is a multifactorial phenomenon with genetic, endocrine, metabolic, behavioral, psychological, and social causes. It is not a moral or psychological problem or a problem due to lack of strength of will, as erroneously considered up to a short time ago due to misinformation. Today, obesity is known to be a disease whose treatment leads to the reduction of mortality and to improvement of quality of life3.
The therapeutic approach to obese patients involves measures of re-education regarding eating habits, physical activity, as well as psychotherapy and medication. The non-surgical approach is usually ineffective for patients with morbid obesity and bariatric surgery represents an important treatment option4.
Although there are various surgical techniques for the treatment of obesity, the Fobi-Capella technique is currently the one most frequently used in Brazil and in the USA since it is the most physiological and presents lower morbidity among the operations that achieve good results regarding weight loss maintained on a long-term basis. This operation consists of a vertical gastroplasty with gastric banding and a Roux-en-Y gastrojejunal shunt and is the technique adopted by the Division of Digestive Surgery, University Hospital, Faculty of Medicine of Ribeirão Preto (HCFMRP/USP).
After the weight loss obtained with the operation, the quality of life of morbidly obese patients improves significantly, with a reduction of the doses of medication for the treatment of associated diseases or frequently with complete resolution of diabetes mellitus, systemic arterial hypertension and sleep apnea, in addition to improved physical ability5.
In addition to these diseases, several other conditions are associated with morbid obesity, among them alveolar hypoventilation syndrome. Excess weight may cause impaired pulmonary function, especially in morbid obesity6-8. Thus, it is interesting to study pulmonary function by spirometry during the preoperative period in order to investigate the possibility of restrictive or obstructive pulmonary disorder. Obese patients commonly present respiratory symptoms such as dyspnea, explained in part by the fact that obese persons tend to breathe in a more rapid and shallow manner as an adaptation to the increase in total respiratory work and in the resistance caused by obesity. Several studies have shown that obese patients without co-morbidities present dyspnea even at rest and in the absence of other causes9.
As a function of the mechanical and physiological changes occurring in the pulmonary volumes as a result of obesity, the pulmonary function of morbidly obese patients is expected to improve after weight loss.
Many literature reports emphasize the fact that morbidly obese patients have reduced expiratory reserve volume (ERV) and reduced al functional residual capacity (FRC), as well as restrictive respiratory behavior in many cases10,11. In severely obese patients, ventilatory normality is reestablished after weight loss as a consequence of increased FRC, residual volume (RV), total lung capacity (TLC), and ERV. A significant improvement of pulmonary function, more notably in ERV (54%), was observed in a study conducted on 59 patients after weight loss by means of bariatric surgery using the Mason technique (54%)12.
In addition morbidly obese patients present important changes in their quality of life. The weight loss obtained by surgical treatment is infrequently achieved in the same magnitude by any modality of clinical treatment. This significant weight loss involves a series of benefits, i.e., suppression or reduction of oral hypoglycemic agents and of insulin in 95% of type 2 diabetic patients, cure of sleep apnea in 90% of all patients, improvement of stress urinary incontinence, of hirsutism, of acne associated with polycystic ovary syndrome and with insulin resistance, of reflux esophagitis symptoms, as well as reduced arterial blood pressure levels, improved lipid profile and arthropathy and, most of all, improved quality of life5.
The objective of the present study was to assess the evolution of pulmonary function by spirometry and of quality of life six months after bariatric surgery, and to determine a possible correlation between weight loss and pulmonary function.
Methods
The study was approved by the Research Ethics Committee of the University Hospital, Faculty of Medicine of Ribeirão Preto/USP (process no. 466/2006).
Twenty patients of both genders with grade III obesity were selected at random and studied before and six months after the Fobi-Capella operation at the University Hospital of the Faculty of Medicine of Ribeirão Preto/USP.
The inclusion and exclusion criteria are listed in Chart 1.
Pulmonary function was assessed by spirometry, quality of life by the application of the Moorehead-Ardelt13 questionnaire, and percent loss of excess weight was calculated according to the ideal weight table of the Metropolitan Life Foundation (1983).
For the spirometry procedure, the patient rested for 5 to 10 minutes before the test, which was carefully applied with emphasis on the need to avoid leaks around the mouthpiece and on the need for maximum inspiration followed by rapid and sustained expiration until the maneuver was interrupted. The exam was performed in an air-conditioned room with a temperature of 20-25°C in order to prevent a great difference between the temperature of the spirometer and body temperature. All volumes recorded were converted from ambient conditions (ambient temperature and pressure saturated - ATPS) to body conditions (body pressure and temperature saturated - BTPS with water vapor). All patients were weighed on a Filizola® scale and their height was measured using the ruler of the Filizola® scale itself. The patients were instructed to come for the test wearing light clothing that would not interfere significantly with the weight.
The spirometric measurements were made with a Pulmonet spirometer (GODART NV de Bilt Vetr. Holland) equipped with a closed, water-sealed volume dislocation system, with volume being recorded on draft paper at the rate of 1200 and 600 mm/sec. according to the maneuver performed.
The helium (He) dilution method was used for the measurement of FRC and total lung capacity in a closed circuit. Forced vital capacity was measured by recording the pulmonary volume x time curve.
The following spirometric variables were analyzed: respiratory frequency, expiratory reserve volume, functional residual capacity, vital capacity, residual volume, total lung capacity, forced expiratory volume in the 1st second/forced vital capacity ratio, and forced expiratory flow between 25 and 75% FVC. All values were calculated according to the norms of the American Thoracic Society (ATS)14 using the equations of Knudson15 and Crapo16.
Loss of excess weight was determined as the difference between the preoperative and six months postoperative values, with the ideal weight being considered according to the table of the Metropolitan Life Foundation (1983).
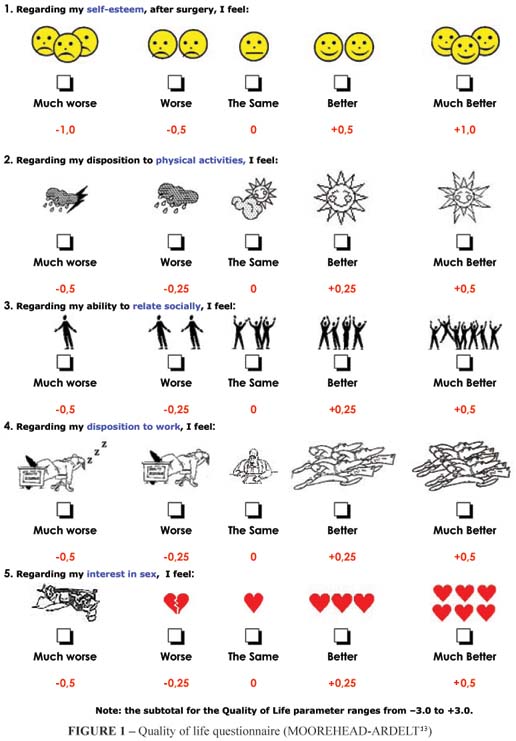
Quality of life was assessed by the BAROS method according to Oria and Moorehead13 based on the subjective criteria mentioned by the patients (self-esteem, physical activity, social relations, disposition to work, and sexual activity).
The questionnaire contains five questions represented by drawings and answered by placing an x on the alternative selected, with a value being attributed to each question (Figure 1).
Data were analyzed statistically by the parametric Student t test for paired samples, with the level of significance set at p<0.05.
Simple linear regression analysis was used to determine a possible correlation between percent loss of excess weight using the Instat software, with the level of significance set at p<0.05.
Results
Seventy-five percent of the patients were women.
Preoperative age and height data are presented in Table 1 and preoperative and postoperative weight and body mass index (BMI) data (mean + SD) are presented in Table 2.
Weight, BMI and percent excess weight loss
Mean preoperative body weight was 149.31 ± 21.47 kg and differed significantly (p < 0.0001) from the mean postoperative weight (110.11 ± 21.77 kg), with a 26.30% reduction in the postoperative value (Figure 2).
Mean preoperative BMI (54.46 ± 7.76 kg/m²) differed significantly (p<0.0001) from mean postoperative BMI (39.93 ± 7.13 kg/m²), with the postoperative value corresponding to a 26.68% reduction of the original BMI (Figure 3).
Mean excess weight was 87.06 ± 18.81 kg during the preoperative period and 47.86 ± 19.25 kg during the postoperative period, with a difference of 39.20 kg between the two values (Figure 4).
The mean loss of excess weight was 46.29 ± 12.10% (Figure 5).
Pulmonary function
Mean respiratory frequency (RF) was 16.4 ± 4.79 inspirations per minute (ipm) during the preoperative period and 14.0 ± 3.86 ipm during the postoperative period. Comparison by the Student t-test revealed a significant difference between means (p = 0.0250). Preoperative RF ranged from 8 to 25 ipm, and postoperative RF ranged from 8 to 21 ipm (Figure 6).
Mean ERV was 0.70 ± 0.34 l during the preoperative period and 1.04 ± 0.59 l during the postoperative period, with a significant difference between values (p=0.0110) (Figure 7).
Mean preoperative FRC was 2.60 ± 0.75 l and mean postoperative FRC was 3.07 ± 0.58 l, with a significant difference between them (p=0.0087) (Figure 8).
Spirometric values such as vital capacity, residual volume, total lung capacity, FEV1/FVC%, and FEF25-75% did not differ significantly before and after surgery.
Correlation between percent loss of weight excess and pulmonary function parameters
There was a positive correlation between percent loss of weight excess and ERV (p=0.0117, r=0.5514). The linear regression curve is illustrated in Figure 9.
There was no correlation between loss of weight excess and the remaining spirometric variables such as respiratory frequency, functional residual capacity, residual volume, total lung capacity, vital capacity or FEV1/FVC% and FEF25-75%.
Quality of life
The data regarding the subjective evaluation of the parameters of the Moorehead-Ardelt quality of life questionnaire by the patient are listed in Table 3.
Regarding self-esteem, 25% of the patients reported improvement and 70% reported that they felt much better.
Regarding physical activity, 10% stated that they felt the same, 40% stated that they felt better and 45% that they felt much better.
For social relations, 10% stated that they felt the same, 35% that they felt better, and 50% that they felt much better.
For disposition to work, 35% stated that they felt better and 60% that they felt much better.
Regarding interest in sex, 25% reported that their interest was the same, 35% reported improvement and 35% stated that they felt much better.
Only one female patient (corresponding to 5%), who reported that she felt much worse in terms of self-esteem and the other parameters, could be considered to have a worse quality of life after surgical treatment.
Discussion
The objective of the present study was to assess whether patient weight loss influenced pulmonary function and quality of life based on spirometry and on the application of the Moorehead-Ardelt questionnaire. Another objective was to correlate the changes caused by improved pulmonary function with percent loss of weight excess. Bariatric surgery consisted of vertical gastroplasty with a restriction ring and a gastrojejunal shunt (Fobi-Capella), this being the preferred surgery at the Bariatric Surgery Center of HCFMRP/USP since it is accepted as the most physiological procedure and it involves fewer undesirable side effects among patients who achieve long-term maintenance of weight reduction.
In the series under study there was a marked predominance of female gender (75%), an almost universal finding regarding the prevalence of morbid obesity17.
Mean body weight and BMI were significantly reduced from 149.31 to 110.11 kg and from 54.46 to 39.93 kg/m² and mean percent loss of excess weight was 46.29%. The reduction of the original weight and BMI six months after the Fobi-Capella surgery observed in the present study (26.25% and 26.68% on average) was similar to that reported in the literature for the same conditions (25.60% and 25.89%)3.
Spirometry was the method chosen for the evaluation of pulmonary function because it is a reliable, reproducible and practical method that does not cause discomfort and that is universally accepted.
Crapo et al.18 emphasized the use of spirometry as a safe preoperative test for morbidly obese patients as an inexpensive, easily applied and advantageous test of sufficient precision to identify the risk of postoperative respiratory complications.
Spirometry was performed six months after the Fobi-Capella operation because a significant weight loss is predicted to occur during this period, validating, in the absence of other causes, the correlation of the eventual changes in pulmonary function and in quality of life with weight reduction.
Pulmonary function is minimally affected in simple obesity, but may be significantly affected in morbid obesity. Thus, an adequate interpretation of spirometry requires an understanding of the effects of morbid obesity on the distribution of pulmonary volumes and on airway caliber.
Obesity as a separate factor in the absence of other respiratory diseases can affect the respiratory system19. Rubinstein et al.20 supported this statement in a study on 293 patients divided into two groups (103 obese and 190 non-obese subjects) which revealed a significant reduction of FRC, TLC, ERV and VC in the obese group and normal values in most of the non-obese subjects.
In the present study, some spirometric variables improved after surgery, with an increase in ERV and FRC and a decrease in respiratory frequency. Mean ERV was 0.70 during the preoperative period and 1.04 during the postoperative period, confirming a significant improvement of this variable after weight loss. None of the 20 patients studied here had previous pulmonary disease, but they had altered pulmonary volumes due to obesity before their weight loss. Spirometry was carried out with the patient in the sitting position both pre- and postoperatively as ERV is even more reduced when morbidly obese patients are in the lying position21.
The reduction of ERV in morbidly obese patients is due to the mechanical changes provoked by the increased abdominal adiposity and/or by the weight on the chest wall and this parameter is expected to return to predicted values with weight loss12. Biring et al.22 also used spirometry in 43 morbidly obese patients and observed that ERV was significantly reduced due to obesity, a fact attributed to reduced pulmonary compliance, to the weight of the abdomen on the chest wall and to weakening of the respiratory musculature.
The improvement in ERV observed here was positively correlated with percent loss of excess weight, further supporting the fact that obese patients, and morbidly obese ones in particular, have important changes in the respiratory volumes and that the loss of weight excess results in a clear improvement of pulmonary function.
The loss of weight excess was used here to determine a correlation with changes in pulmonary function tests because it is a better parameter than the loss of original weight frequently cited in various studies that do not take into consideration the ideal weight, an important parameter for the definition of the degree of difference in the body weight of each patient in relation to normal values.
FRC was another spirometric variable that was reduced during the preoperative period and which improved significantly after weight loss. This reduction does not represent an actual pulmonary restriction, but rather a restrictive behavior which usually tends to improve after weight loss as shown by the mean postoperative value of 3.07 1 compared to the preoperative value of value of 2.60 1. Other studies have also reported a similar improvement of FRC over a six month period after the Fobi-Capella operation6,9,10.
Although FRC improved after the weight loss, it was not correlated with percent loss of excess weight.
In the present study, respiratory frequency was significantly decreased after weight loss. In normal resting respiration, the inspiratory area is activated every five seconds, producing inspiration that lasts two seconds. Normal respiration is almost completely caused by the contraction of inspiratory muscles, with a minimal contribution of expiratory muscles23. Morbidly obese patients tend to breathe in a rapid and shallow manner for adaptation to the increased respiratory work and resistance caused by obesity. The greater the accumulation of adipose tissue on the chest wall, the greater the muscular overload required for ventilation, possibly resulting in dysfunction of the respiratory muscles.
Preoperative respiratory frequency reached a maximum value of 25 incursions, which was reduced to 21 incursions per minute after surgery, demonstrating that, after the weight loss and the consequent reduction of adipose tissue in the chest, there was a reduction in respiratory frequency resulting from the improvement of the mechanical changes due to obesity. During the evaluations, most patients reported improvement of the execution of their daily activities and stated that this condition was related to an improved respiratory pattern since they no longer experienced the respiratory difficulties frequently present during the preoperative period.
The significant reduction of respiratory frequency after surgery strongly suggests that weight loss, with an increase in ERV and FRC, resulted in a reduction of respiratory work.
With the improvement in ERV and FRC, VC was expected to improve in parallel since it is determined by the sum of ERV and inspiratory capacity. However, this parameter did not improve significantly.
The spirometric variables studied here, such as vital capacity, residual volume, total lung capacity, forced expiratory flow between 25 and 75% FVC (FEF25-75%) and forced expiratory volume in the 1st second/ forced vital capacity ratio (FEV1/FVC%) did not differ significantly between the pre- and postoperative periods.
The present results are similar to those reported by Silva24, who conducted a study on 50 patients in which he compared the spirometric values determined on the first, 14th and 30th postoperative day and observed no significant difference in FVC, FEV1, FEF25% or FEFmax. Similarly, the present study did not show a significant improvement of VC or FVC, possibly because the time of postoperative observation was insufficient for the patient to reach the necessary weight loss.
Morbidly obese patients have an unsatisfactory quality of life that tends to improve with the substantial weight loss occurring after bariatric surgery25,26.
Many studies have been conducted worldwide in order to determine whether the weight loss achieved after bariatric surgery is really related to an improved quality of life. Many authors state that the BAROS method, in particular, the Moorehead-Ardelt questionnaire, is an effective method for the evaluation of patient quality of life after weight loss27-29. This questionnaire was used in the present study and even though most patients reported an improvement in quality of life after the surgery, there was no correlation between weight loss and quality of life.
Only one female patient in the present series reported a worsening of quality of life after the postoperative weight loss over a period of six months, but she also reported that she had severe emotional problems and that adaptation after her weight loss was difficult because her relatives did not collaborate with respect to her new life style, especially regarding eating behavior.
In contrast, the remaining patients reported a satisfactory or important improvement of quality of life according to the replies to the questionnaire applied, and few did not observe any differences up to the time when the present study was started regarding physical activity, social relations and sex (2, 2 and 5, respectively). Moneghini et al.30, in a study in which the BAROS method was used, observed that 55% of the 30 patients evaluated after biliopancreatic shunt surgery (Scopinaro procedure) presented a significant improvement in quality of life after one year of follow-up, 35% reported some improvement, and 10% reported no change in quality of life. However, no patient reported worsening of quality of life.
In the present study, the quality of life was found to improve after weight loss even though there was no correlation between these two factors. The term quality of life is ample and involves a series of questions, especially in the presence of morbid obesity and weight loss since co-morbidities (diabetes, systemic arterial hypertension, sleep apnea) improve significantly and are often completely resolved, a fact that certainly influences the quality of life of these patients. However, these questions were not investigated in the present study, a fact that may explain the lack of correlation between weight loss and quality of life observed.
Weight loss with the consequent solution of associated diseases definitely results in improvement of the subjective parameters involved in the evaluation of quality of life, at least regarding physical activity and disposition to work. The improvement of subjective parameters manifests early during the period following surgery, probably due to the expectation of positive results, including body image.
Conclusions
The study of loss of body weight excess, of pulmonary function and of quality of life of 20 morbidly obese patients six months after the Fobi-Capella operation permitted us to reach the following conclusions:
1 There was a significant loss of excess weight, an improvement of pulmonary function related to increased Expiratory Reserve Volume (ERV) and Functional Residual Capacity (FRC), a reduction of Respiratory Frequency (RF), and an improvement of quality of life.
2 There was a positive correlation between Expiratory Reserve Volume and percent weight loss, but there was no correlation between other pulmonary function variables and percent loss of excess body weight.
Received: February 09, 2010
Review: April 14, 2010
Accepted: May 18, 2010
Conflict of interest: none
Financial source: none
How to cite this article
Xavier MAF, Ceneviva R, Terra Filho J, Sankarankutty AK. Pulmonary function and quality of life in patients with morbid obesity six months after bariatric surgery. Acta Cir Bras. [serial on the Internet] 2010 Sept-Oct;25(5). Available from URL: http://www.scielo.br/acb
- 1. Prietto J, Baur LA. Management of obesity. Med J Aust. 2004;180:474-80.
- 2. Sorensen TI. The changing lifestyle in the world. Body weight and what else? Diabetes Care. 2000;23(2):B1-4.
- 3. O Brien PE, Brown AW, Dixon JB. Obesity, weight loss and bariatric surgery. Med J Aust. 2005;183(6):310-4.
- 4. Nguyen NT, Goldman CG, Rosenquist CJ, Arango A, Cole CJ, Lee SJ, Wolfe BM. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life and costs. Ann Surg. 2001;234(3):279-91.
- 5. Dixon JB, Dixon ME, O Brien PE. Quality of life after lap-band placement: influence of time, weight loss and comorbidities. Obes Res. 2001;9:713-21.
- 6. Koenig SM. Pulmonary complications of obesity. Am J Med Sci. 2001;321(4):249-79.
- 7. Ladoski W. Chest mechanics in morbidly obese non-hypoventilated patients. Respir Med. 2001;95:281-6.
- 8. Rasslan Z, Saad Jr. R, Stirbulov R, Fabbri RMA, Lima CAC. Avaliação da função pulmonar na obesidade graus I e II. J Bras Pneumol. 2004;30(6):508-14.
- 9. Sahebjami H. Dyspnea in obese healthy men. Chest. 1998;114(5):1373-7.
- 10.Ray CS, Sue DY, Bray G, Hansen JE, Wasserman K. Effects of obesity on respiratory function. Am Rev Respir Dis. 1983;128:501-6.
- 11. Hakala K, Stenius-Arniala B, Sovijarvi A. Effects of weight loss on peak flow variability, airways obstruction and lung volumes in obese patients with asthma. Chest. 2000;118:1315-21.
- 12. Thomas PS, Cowen ERT, Hulands G, Milledge JS. Respiratory function in the morbidly obese before and after weight loss. Thorax. 1989;44:382-6.
- 13. Moorehead MK, Ardelt-Gattinger E, Lechner H, Oria HE. The validation of the Moorehead-Ardelt. Quality of Life Questionnaire II. Obes Surg. 2003;13(5):684-92.
- 14. American Thoracic Society. Standardization of Spirometry 1994 update. Am J Respir Crit Care Med. 1995;152:1107-36.
- 15. Knudson RJ, Slatin RC, Lebowitz MD, Burrows B. The maximal expiratory flow-volume curve. Normal standards, variability and effects of age. Am Rev Respir Dis. 1976;113:587-600.
- 16. Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981;123:659-64.
- 17. Kolotkin RL, Crosby RD, Willians GR, Hartley GG, Nicol S. The relationship between health-related quality of life and weight loss. Obes Res. 2001;9:564-71.
- 18. Crapo RO, Kelly TM, Elliot CG, Jones SB. Spirometry as a preoperative screening test in morbidly obese patients. Surgery. 1986;99(6):763-7.
- 19. Sahebjami H, Gartside PS. Pulmonary function in obese subjects with a normal FEV1/FVC ratio. Chest. 1996;110(6):1425-9.
- 20. Rubinstein I, Zamel N, DuBarry L, Hoffstein V. Airflow limitation in morbidly obese subjects nonsmoking men. Ann Intern Med. 1990;112:828-32.
- 21. Collins LC, Hoberty PD, Walker JF, Fletcher EC, Peiris AN. The effect of body fat distribution on pulmonary function tests. Chest. 1995;107(5):1298-302.
- 22. Biring MS, Lewis MI, Liu JT, Mohsenifar Z. Pulmonary physiologic changes of morbid obesity. Am J Med Sci. 1999;318(5):293-7.
- 23. Paisani DM, Chiavegato LD, Faresin SM. Volumes, capacidades pulmonares e força muscular respiratória no pós-operatório de gastroplastia. J Bras Pneumol. 2005;31(2):125-32.
- 24. Silva AMO, Boin IFS, Pareja JC, Magna LA. Análise da função respiratória em pacientes obesos submetidos à operação Fobi-Capella. Rev Col Bras Cir. 2007;34(5):314-20.
- 25. Suter M, Paroz A, Calmes JM, Giusti V. European experience with laparoscopic Roux en Y gastric bypass in 466 patients. Br J Surg. 2006;93(6):726-32.
- 26. Champault A, Duwat O, Polliand C, Rizk N, Champault GG. Quality of life after laparoscopic gastric banding: prospective study (152 cases) with a follow-up of 2 years. Surg Laparosc Endosc Percutan Tech. 2006;16(3):131-6.
- 27. Manplekou E, Komesidou V, Bissias CH, Papakonstantinou A, Melissas J. Psychological condition and quality of life of patients with morbid obesity before and after surgical weight loss. Obes Surg. 2005;15(8):1187-4.
- 28. Gould JC, Garren MJ, Boll V, Starling JR. Laparoscopic gastric bypass: risks versus benefits up to two years following surgery in super-super obese patients. Surgery. 2006;140(4):529-31.
- 29. Suter M, Paroz A, Calmes JM, Giusti V. European experience with laparoscopic Roux en Y gastric bypass in 466 patients. Br J Surg. 2006;93(6):726-32.
- 30. Moneghini D, Mittempergher F, Terraroli C, Di Fabio F. Bariatric analysis and reporting outcome system (BAROS) following biliopancreatic diversion. Ann Ital Chir. 2006;4(75):417-20.
Publication Dates
-
Publication in this collection
20 Sept 2010 -
Date of issue
Oct 2010
History
-
Reviewed
14 Apr 2010 -
Received
09 Feb 2010 -
Accepted
18 May 2010