Abstracts
PURPOSE: To determine biomechanical property of autogenous bone graft covered with hydroxyapatite in the defect of radial bone in rabbit. METHODS: Eighteen adult male New Zealand white rabbits were used which were divided into three groups (I, II, III) of six rabbits each. A segmental bone defect of 10 mm in length was created in the middle of the right radial shaft under general effective anesthesia in all rabbits and were stabilized using mini-plate with four screws. The defects In group I were left as such without filler, whereas in group II the defect were filled up with harvested 10 mm rib bone and in group III the defect were packed with rib bone covered with nano-hydroxyapatite. All rabbits in three groups were divided into two subgroups (one month and three months duration with three rabbits in each one). RESULTS: The mechanical property and the mean load for fracturing normal radial bone was recorded 388.2±6 N whereas it was 72.4±12.8 N for group I in 1 month duration which was recorded 182.4±14.2 N for group II and 211.6±10.4 N for group III at the end of 1 month. These values were 97.6±10.2 N for group I and 324.6±8.2 N for group II and 372.6±17.4 N for group III at the end of three months after implantation. CONCLUSION: Implantation of autologous graft covered with hydroxyapatite indicated to have positive effect in integral formation of qualitative callus at the site of fracture and early re-organization of callus to regain mechanical strength too.
Transplantation; Autologous; Bone; Durapatite; Rabbits
OBJETIVO: Determinar as propriedades biomecânicas de enxerto ósseo autógeno coberto com hidroxiapatita em defeito do osso radial em coelhos. MÉTODOS: Foram utilizados 18 coelhos adultos, machos, brancos, Nova Zelândia, distribuídos em três grupos (I, II, III) de seis coelhos cada. Um defeito segmentar de 10 mm de comprimento foi criado no meio do eixo radial direito sob anestesia geral efetiva em todos os coelhos e foram fixados usando mini-placa com quatro parafusos. Os defeitos no grupo I foram deixados sem preenchimento, enquanto no grupo II o defeito foi preenchido com 10 mm de costela recoberta com nano-hidroxiapatita. Os coelhos nos três grupos foram distribuídos em dois subgrupos (Um e três meses, com três coelhos cada um). RESULTADOS: A propriedade mecânica e a média do peso para fraturar o osso radial normal foi 388,2±6 N, enquanto para o Grupo I, com um mês foi 72,4±12,8 N, para o grupo II 182,4±14,2 N e para o Grupo III 211,6±10,4 N. Após três meses de implantação, os valores foram 97,6±10,2 N para o Grupo I, 324,6±8,2 N para o Grupo II e 372,6±17,4 N para o Grupo III. CONCLUSÃO: A implantação de enxerto autólogo recoberto com hidroxiapatita indicou ter um efeito positivo na formação integral qualitativa do calo ósseo no local da fratura e precoce reorganização do calo com recuperação da força mecânica.
Transplante Autólogo; Osso; Durapatita; Coelhos
9 - ORIGINAL ARTICLE
EXPERIMENTAL ORTHOPAEDIC SURGERY
Mechanical properties of radial bone defects treated with autogenous graft covered with hydroxyapatite in rabbit1 Correspondence: Davood Sharifi Department of Veterinary Surgery Faculty of Specialized Veterinary Sciences Science and Research Branch Islamic Azad University Tehran, Iran Tel.: 00989123194096 Fax: 00982122110193 dsharifi@ut.ac.ir
Propriedades mecânicas de defeito de osso radial tratado com enxerto autógeno coberto com nano-hydroxyapatite em coelho
Davood SharifiI; Hamid Reza KhoushkerdarII; Gholamreza AbediIII; Ahmad AsghariIII; Saeed HesarakiIV
IFull Professor, Department of Surgery, Science and Research Branch, Islamic Azad University, Tehran, Iran. Responsible for design of the study, manuscript preparation, acquisition and interpretation of data. Part of PhD thesis
IIPostgraduate Student, Department of Surgery, Science and Research Branch, Islamic Azad University, Tehran, Iran. Designed the protocol, helped with technical procedures, anesthesia
IIIAssistant Professor, Department of Surgery, Science and Research Branch, Islamic Azad University, Tehran, Iran. Analysis and interpretation of data
IVAssistant Professor, Department of Materials and Energy Research, Karaj, Iran. Responsible for manuscript preparation
Correspondence Correspondence: Davood Sharifi Department of Veterinary Surgery Faculty of Specialized Veterinary Sciences Science and Research Branch Islamic Azad University Tehran, Iran Tel.: 00989123194096 Fax: 00982122110193 dsharifi@ut.ac.ir
ABSTRACT
PURPOSE: To determine biomechanical property of autogenous bone graft covered with hydroxyapatite in the defect of radial bone in rabbit.
METHODS: Eighteen adult male New Zealand white rabbits were used which were divided into three groups (I, II, III) of six rabbits each. A segmental bone defect of 10 mm in length was created in the middle of the right radial shaft under general effective anesthesia in all rabbits and were stabilized using mini-plate with four screws. The defects In group I were left as such without filler, whereas in group II the defect were filled up with harvested 10 mm rib bone and in group III the defect were packed with rib bone covered with nano-hydroxyapatite. All rabbits in three groups were divided into two subgroups (one month and three months duration with three rabbits in each one).
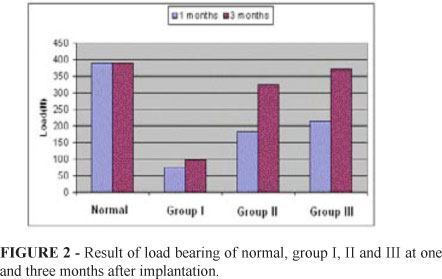
RESULTS: The mechanical property and the mean load for fracturing normal radial bone was recorded 388.2±6 N whereas it was 72.4±12.8 N for group I in 1 month duration which was recorded 182.4±14.2 N for group II and 211.6±10.4 N for group III at the end of 1 month. These values were 97.6±10.2 N for group I and 324.6±8.2 N for group II and 372.6±17.4 N for group III at the end of three months after implantation.
CONCLUSION: Implantation of autologous graft covered with hydroxyapatite indicated to have positive effect in integral formation of qualitative callus at the site of fracture and early re-organization of callus to regain mechanical strength too.
Key words: Transplantation, Autologous. Bone. Durapatite. Rabbits.
RESUMO
OBJETIVO: Determinar as propriedades biomecânicas de enxerto ósseo autógeno coberto com hidroxiapatita em defeito do osso radial em coelhos.
MÉTODOS: Foram utilizados 18 coelhos adultos, machos, brancos, Nova Zelândia, distribuídos em três grupos (I, II, III) de seis coelhos cada. Um defeito segmentar de 10 mm de comprimento foi criado no meio do eixo radial direito sob anestesia geral efetiva em todos os coelhos e foram fixados usando mini-placa com quatro parafusos. Os defeitos no grupo I foram deixados sem preenchimento, enquanto no grupo II o defeito foi preenchido com 10 mm de costela recoberta com nano-hidroxiapatita. Os coelhos nos três grupos foram distribuídos em dois subgrupos (Um e três meses, com três coelhos cada um).
RESULTADOS: A propriedade mecânica e a média do peso para fraturar o osso radial normal foi 388,2±6 N, enquanto para o Grupo I, com um mês foi 72,4±12,8 N, para o grupo II 182,4±14,2 N e para o Grupo III 211,6±10,4 N. Após três meses de implantação, os valores foram 97,6±10,2 N para o Grupo I, 324,6±8,2 N para o Grupo II e 372,6±17,4 N para o Grupo III.
CONCLUSÃO: A implantação de enxerto autólogo recoberto com hidroxiapatita indicou ter um efeito positivo na formação integral qualitativa do calo ósseo no local da fratura e precoce reorganização do calo com recuperação da força mecânica.
Descritores: Transplante Autólogo. Osso. Durapatita. Coelhos.
Introduction
There is a growing need for bone regeneration due to various clinical bone diseases such as bone infections, bone tumors and bone loss by trauma. Current therapies for bone defects include auto graft, allograft, xenografts and other artificial substitutes such as metals, synthetic cements and bioceramic1,2. The ideal bone graft or osseous reconstructive material should possess the following characteristics: It should be implantable through a minimal surgical exposure, it should be moldable to conform to and fill irregular defects, it should be as rigid and strong as intact bone for immediate load-bearing capability, it should promote new bone formation and incorporation by host, and finally it should be fully synthetic. Ceramic materials (i.e. hydroxyapatite and tricalcium phosphate blocks or cylinders) have been widely studied as potential bone graft substitutes3,4. Bioactive biomaterials such as bioglass, hydroxyapatite5 and glass ceramic A-W have been known to form a bioactive bone like apatite layer spontaneously on their surfaces and bond to bone through the apatite layer in vivo6,7. Therefore, it is generally accepted that an essential prerequisite for an artificial bone biomaterial to directly bond to living bone tissue is the formation of a bone like apatite layer on its surface when implanted in vivo6,7. HA has been attractive in hard tissue repair because of its good biocompatibility and bioactivity recently, researchers have developed nano-hydroxyapatite with polyamide (n-HA/PA) biocomposites for load-bearing orthopedic applications8,9. In bone tissue engineering, scaffold serves as the matrices of tissue formation, and play pivotal role in osseointegration and tissue integration, as bone grafting is frequently used to augment bone healing with numerous approaches to reconstructing or replacing skeletal defects10. Autologous bone graft remains the most effective grafting materials because it provides the three elements required for bone regeneration; osteoconduction, osteoinduction11-13. In this study autologous rib bone covered with that of nano hydroxyapatite was intended to be suitable for defects of defined shape.
Methods
All animal procedures were carried out according to the guidelines of the Animal Ethics Committee of Islamic Azad University .Eighteen New Zealand 24 week old and weighing 3.0-3.5 kg male rabbits were used, and divided into three groups (I, II and III) of six rabbits each, according to the procedure performed. Animals in each group were subdivided into two subgroups of three rabbits for one month and three months duration. All rabbits were kept in individual cage during the whole experimental period, under strict hygienic conditions and fed with standard ration for rabbits and water ad labium.
Surgical procedure
Under intramuscular Diazepam (1mg/kg) premedication and intravenous Ketamine hydrochloride (35mg/kg) and Xylazine (5mg/kg) general anesthesia. Right radius was routinely prepared for surgery. A 4cm longitudinal skin incision was made. The space between extensor and flexor muscles groups was dissected, providing a wide view of radial bone, a segmental bone defect was created in the middle of the radius shaft, 10-mm in length, using a delicate orthopedic motor saw and defect was stabilized with a miniplate having 4 screws. In group I, the defect was left empty, whereas in group II, the bone defect was packed with autologous spongy rib bone. In group III, the bone defect was packed with piece of rib bone covered with nano-hydroxyapatite.
Post operative care
Antibiotics (penicillin G procaine 40000 IU/kg IM, bid), dexamethasone (0.6 mg/kg, IM), vitamin B.complex (0.2 mg/kg, IM) and analgesic such as Tramadol hydrochloride (5 mg/kg, IM, bid) were administered for 3 post-operative days.
Compressive pressure analysis
All mechanical testing were performed using a Zwick/Roell 2005 with a crosshead speed of 0.01 mm/s. A load-distance curve was recorded to obtain the mechanical properties (Figure 1). Load bearing was obtained with maximum load recorded of the linear portion of the load-distance curve. The mechanical properties of the normal radial bone were measured to provide reference values. Three specimens were tested for each condition, and data were represented as mean standard deviations (SD). Statistical analysis was carried out on the load bearing data using one way analysis of variance with the software program SPSS for Windows, version 9 (SPSS Inc., Chicago, IL, USA). P<0.05 was considered to be statistically significant. Tukey HSD multiple comparison testing was used to determine the significance of the deviations in the mechanical property of each sample for different times.
Results
No operative or postoperative complications were encountered. All of the rabbits tolerated surgery well and survived until the final experimental time. No wound opening or infections were observed. At sacrifice the macroscopic evaluation revealed maintenance of correct position of sample in the defect site. There was a significant increase in compression properties of radial bone in group III in 1st and 3rd months as compared to other two groups (I, II). The biomechanical testing showed 388.2±6 N was breaking point for normal bone and in group (I) it was recorded 72.4±12.8 N, in 1 month whereas it was 182.4±14.2 N in group (II) and 211.6±10.4 N in group III in the same period. At the end of 3 months observations 97.6±10.2 N; 324.6±8.2 N and 372.6±17.4 N were recorded values of compressive pressure respectively. The results of this study show that spongy rib bone covered with nano-hydroxyapatite is good choice for the healing of segmental bone defects, as increased and attained almost normal mechanical property or tensile strength that of normal one (Table 1, Figure 2).
Discussion
The results of this experiment indicated the autologous rib graft with and without covering nano-hydroxyapatite were able to maintain strength and stiffness while improving the incorporation process. This was especially true in the group III in which cancellous bone graft of rib with nano-hydroxyapatite were used to pack the defects. One the most interesting observations from this study was the differences between control and other two groups using implants, but there was no fundamental differences between two implanted groups. There was very good osteoconduction in both the implanted groups and stiffness was proper clinical sign of very rapid resorption and replacement of implant by living bone especially in group III as the significantly increased in mechanical properties in all rabbits if this group3.An ideal bone graft substitute should have osteoconductive, osteoinductive and osteogenic properties. Autogenous bone graft is the gold standard among the graft materials because it provides all of these properties14. Autogenous bone graft has been the implant of choice for most of the orthopedic procedures. However, autogenous and allogenic bone grafts have several limitations, such as donor-site infection, pain, and disease transfer15. Because of these limitations, biosynthetic bone graft substitutes are being investigated. As a result, some investigators used mixtures of synthetic scaffolding biomaterials and osteoinductive organic agents to achieve better results and optimum tissue biomaterial contact necessary for stimulating bone in growth14. Cancellous rib bone was osteoinductive material being used as a bone graft substitute, and combination with Nano-hydroxyapatite would probably create a composite with potentiated osteoinductive properties. The results achieved in this investigation indicated that this graft covered with really stimulates a favorable reaction of lon bones and the best fracture healing was observed. The osteoconductivity of this graft promotes bone healing and helps in regaining the strength of the defect site faster. The addition of nano-hydroxyapatite creates better conditions for bone formation; the increased osteogenesis may well be attributable to the stimulatory effect of nano-hydroxyapatite on local cells involved in bone regeneration such as osteoblasts, mesenchymal progenitor cells and endothelial cells16-18.
As to cover the large gap in the body of long bones the scaffolding materials for bone tissue engineering should be osteoconductive so that osteoprogenitor cells can adhere and migrate on the scaffolds, differentiate and finally form new bone. In this investigation, we consider the cancellous rib bone covered with nano-hydroxyapatite can be a good choice for the healing of segmental bone defects, and provides a more rapid regeneration with almost normal mechanical property of bone defects.
Conclusion
The nano-hydroxyapatite is a viable option for obliteration beside autologous bone grafting for early stiffness and strength in diaphyseal defect.
Received: October 19, 2011
Review: December 14, 2011
Accepted: January 20, 2012
Conflict of interest: none
Financial source: Science and Research Branch of Tehran, Islamic Azad University
1 Research performed at Department of Veterinary Surgery, Faculty of Specialized Veterinary Sciences, Science and Research Branch, Islamic Azad University, Tehran, Iran.
- 1. Ma PX, Zhang R, Xiao G, Franceschi R. Engineering new bone tissue in vitro on highly porous poly(alpha-hydroxyl acids) hydroxyapatite composite scaffolds. J Biomed Mater Res. 2001;54(2):284-93.
- 2. Guobao WEI, Peter XMA. Structure and properties of nano-hydroxyapatite/polymer composite scaffolds for bone tissue engineering. Biomaterials. 2004;25(19):4749-57.
- 3. Voor MJ, Arts JJC, Klein SA, Walschot LHB, Verdonschot N, Buma P. Is hydroxyapatite cement an alternative for allograft bone chips in bone grafting procedures? A mechanical and histological study in a rabbit cancellous bone defect model. J Biomed Mater Res Part B Appl Biomater. 2004;71(2):398-407.
- 4. Bucholz RW. Nano allograft osteoconductive bone graft substitutes. Clin Orthop Relat Res. 2002;395:44-52.
- 5. Yang K, Wei J, Wang CY, Yubao I. A study on in vitro and in vivo bioactivity of nano hydroxyapatite /polymer biocomposite. Chinese Sci Bull. 2007;52(2):267-71.
- 6. Ayako O, Hyun-Min K, Takuo F, Tadashi K, Toshiki M, Takashi N. Composition of Apatiteproduces in simulated body fluids. J Biomed Mater Res Part A. 2003;65(2):188-95.
- 7. Kokubo T, Kim HM, Kawasdita M. Novel bioactive materials with different mechanical properties. Biomaterials. 2003;24:2161-75.
- 8. Zambonin G, Grano M. Biomaterials in orthopaedic surgery: Effects of different hydroxyapatites and demineralized bone matrix on proliferation rate and bone matrix synthesis by human osteoblasts. Biomaterials. 1995;16:397-402.
- 9. Nascimento C, Issa JPM, Oliveira RR, Iyomasa MM, Siessere S, Regalo SCH. Biomaterials applied to the bone healing process. Int J Morphol. 2007;25(4):839-46.
- 10. Brighton CT, Robert MH. Early histology and ultra structural changes in micro vessels of periosteal callus. J Orthop Trauma. 1997;11(4):244-53.
- 11. Qian XU, Hongyan LU, Jingchao Z, Guoyu LU, Zhennan D, Anchun MO. Tissue engineering scaffold material of porous nano-hydroxyapatite/polymide 66. Int J Nanomedicine. 2010;5:331-5.
- 12. Jie W, Yubao L. Tissue engineering scaffold material of nano- apatite crystals and polyamide Composite. Eur Polym J. 2004;40:509-15.
- 13. Green DW, Walsh D, Mann S, Orffe ROC. The Potential of Biomimesis in bone tissue engineering: lessons from the design and synthesis of invertebrate skeletons. Bone. 2002;30(6):810-5.
- 14. Brighton CT, Robert MH. Early histologic and ultrastructural changes in medullary fracture callus. J Bone Joint Surg. 1991;73A(6):832-47.
- 15. Holmes RE, Buchloz RW, Mooney V. Porous hydroxyapatite as a bone-graft substitute in metaphyseal defects. A histometric study. J Bone Joint Surg Am. 1986;68:904-11.
- 16. Zambonin G, Grano M. Biomaterials in orthopaedic surgery: effects of different hydroxyapatites and demineralized bone matrix on proliferation rate and bone matrix synthesis by human osteoblasts. Biomaterials. 1995;16:397-402.
- 17. Nascimento C, Issa JPM, Oliveira RR, Iyomasa MM, Siessere S, Regalo SCH. Biomaterials applied to the bone healing process. Int J Morphol. 2007;25(4):839-46.
- 18. Harvey EJ, Henderson JE, Vengallatore ST. Nanotechnology and bone healing. J Orthop Trauma. 2010;24 Suppl 1:S25-30
Publication Dates
-
Publication in this collection
26 Mar 2012 -
Date of issue
Mar 2012
History
-
Received
19 Oct 2011 -
Accepted
20 Jan 2012 -
Reviewed
14 Dec 2011