ABSTRACT
Objective
To evaluate the clinical utility of 18F-FDG PET/CT in patients with high-risk DTC.
Subjects and methods
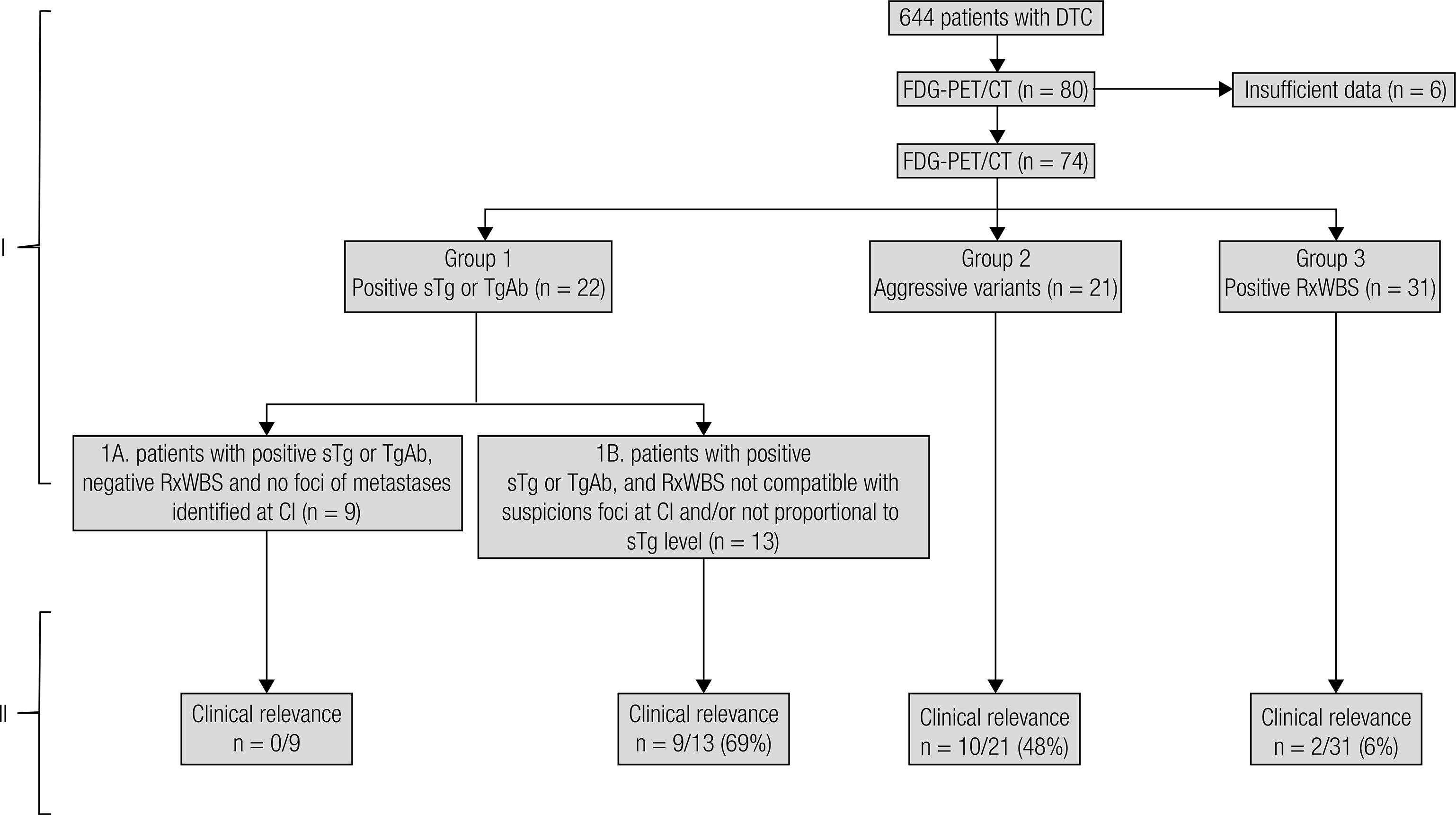
Single-center retrospective study with 74 patients with high-risk differentiated thyroid cancer (DTC), classified in 4 groups. Group 1: patients with positive sTg or TgAb, subdivided in Group 1A: negative RxWBS and no foci of metastases identified at conventional image (n = 9); Group 1B: RxWBS not compatible with suspicious foci at conventional image or not proportional to sTg level (n = 13); Group 2: patients with histological findings of aggressive DTC variants (n = 21) and Group 3: patients with positive RxWBS (n = 31).
Results
18F-FDG PET/CT identified undifferentiated lesions and helped restage the disease in groups 1B and 2. The scan helped guide clinical judgment in 9/13 (69%) patients of group 1B, 10/21 (48%) patients of group 2 and 2/31 (6%) patients of group 3. There was no clinical benefit associated with group 1A. 18F-FDG PET/CT was associated with progressive disease.
Conclusion
18F-FDG PET/CT is a useful tool in the follow-up of patients with high-risk DTC, mainly in the group of RxWBS not compatible with suspicious foci at conventional image or not proportional to sTg level and in those with aggressive DTC variants. Additionally, this study showed that 18F-FDG PET/CT was associated with progression and helped display undifferentiated lesions guiding clinical assessments regarding surgeries or expectant treatments.
Differentiated thyroid carcinoma; 18F-FDG PET/CT; radioiodine (RAI); whole-body scan (WBS); thyroglobulin (Tg)
INTRODUCTION
The routine follow-up of patients with differentiated thyroid cancer (DTC) after surgery and radioiodine (RAI) remnant ablation comprises the measurement of serum thyroglobulin (sTg), cervical ultrasound (US), whole-body scan with 131I (WBS) or conventional imaging techniques, such as computed tomography (CT) or magnetic resonance imaging (MRI).
However, serum Tg levels may not be a reliable tool in some patients, mainly due to the presence of anti-thyroglobulin antibodies (TgAb) (11. Spencer CA. Challenges of serum thyroglobulin (Tg) measurement in the presence of Tg autoantibodies. J Clin Endocrinol Metab. 2004;89(8):3702-4.) or to undifferentiated tumors that do not secrete Tg. Similarly, WBS may fail to localize residual thyroid tissue in less differentiated tumors due to its impaired ability to concentrate RAI (22. Pineda JD, Lee T, Ain K, Reynolds JC, Robbins J. Iodine-131 therapy for thyroid cancer patients with elevated thyroglobulin and negative diagnostic scan. J Clin Endocrinol Metab. 1995;80(5):1488-92.).
In recent years, combined 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) has emerged as a valuable tool in the follow-up of thyroid cancers. By correlating the metabolic information of 18F-FDG PET with the morphologic resolution of CT and due to the enhanced glucose metabolism in thyroid cancers, particularly in less differentiated tumors, this imaging technique has been employed beyond the classical indication of DTC patients with positive sTg and negative WBS. Furthermore, current applications extend to disease extension, including the detection of undifferentiated metastases (33. Hall NC, Kloos RT. PET imaging in differentiated thyroid cancer: where does it fit and how do we use it? Arq Bras Endocrinol Metabol. 2007;51(5):793-805.), guidance of therapy assessments and prediction of prognosis (44. Marcus C, Antoniou A, Rahmim A, Ladenson P, Subramaniam RM. Fluorodeoxyglucose positron emission tomography/computerized tomography in differentiated thyroid cancer management: Importance of clinical justification and value in predicting survival. J Med Imaging Radiat Oncol. 2015;59(3): 281-8.
5. Pace L, Klain M, Salvatore B, Nicolai E, Zampella E, Assante R, et al. Prognostic role of 18F-FDG PET/CT in the postoperative evaluation of differentiated thyroid cancer patients. Clin Nucl Med. 2015;40(2):111-5.-66. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.). Some studies have shown that 18F-FDG PET and 18F-FDG PET/CT can induce changes in clinical management plans in 10-78% of patients with DTC (77. Wang W, Macapinlac H, Larson SM, Yeh SD, Akhurst T, Finn RD, et al. [18F]-2-fluoro-2-deoxy-D-glucose positron emission tomography localizes residual thyroid cancer in patients with negative diagnostic (131)I whole body scans and elevated serum thyroglobulin levels. J Clin Endocrinol Metab. 1999;84(7): 2291-302.
8. Helal BO, Merlet P, Toubert ME, Franc B, Schvartz C, Gauthier-Koelesnikov H, et al. Clinical impact of (18)F-FDG PET in thyroid carcinoma patients with elevated thyroglobulin levels and negative (131)I scanning results after therapy. J Nucl Med. 2001;42(10):1464-9.
9. Lee JW, Lee SM, Lee DH, Kim YJ. Clinical utility of 18F-FDG PET/CT concurrent with 131I therapy in intermediate-to-high-risk patients with differentiated thyroid cancer: dual-center experience with 286 patients. J Nucl Med. 2013;54(8):1230-6.
10. Rosenbaum-Krumme SJ, Görges R, Bockisch A, Binse I. 18F-FDG PET/CT changes therapy management in high-risk DTC after first radioiodine therapy. Eur J Nucl Med Mol Imaging. 2012;39(9):1373-80.
11. Pomerri F, Cervino AR, Al Bunni F, Evangelista L, Muzzio PC. Therapeutic impact of (18)F-FDG PET/CT in recurrent differentiated thyroid carcinoma. Radiol Med. 2014;119(2):97-102.-1212. Leboulleux S, Schroeder PR, Busaidy NL, Auperin A, Corone C, Jacene HA, et al. Assessment of the incremental value of recombinant thyrotropin stimulation before 2-[18F]-Fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography imaging to localize residual differentiated thyroid cancer. J Clin Endocrinol Metab. 2009;94(4):1310-6.), thereby improving clinical judgment. In the Brazilian population, there has been only one study using 18F-FDG PET/CT in thyroid cancer patients with negative WBS and positive sTg in a small patient sample (1313. Yamaga LY, Cunha ML, Wagner J, Thom AF, Daniel MM, Funari MB. [Diagnostic value of positron emission tomography/computed tomography with fluorine-18 fluordeoxyglucose in patients with differentiated thyroid gland carcinoma, high thyroglobulin serum levels and negative iodine whole body scan]. Arq Bras Endocrinol Metabol. 2007;51(4):581-6.).
The potential to induce changes in the clinical management and the lack of other studies in our country motivated this work. Therefore, the aim was to evaluate the clinical utility of the 18F-FDG PET/CT in a large cohort of patients with DTC in various groups.
SUBJECTS AND METHODS
A total of 644 patients with DTC were referred, evaluated, treated and followed by a single team of physicians at the associated Thyroid Disease Centers in the Division of Endocrinology, Department of Medicine, Escola Paulista de Medicina, Universidade Federal de São Paulo and the Instituto Israelita de Ensino e Pesquisa Albert Einstein (in São Paulo, Brazil). In this population, 80 patients were submitted to 18F-FDG PET/CT scans from February 2008 to June 2013. Six patients were lost to follow-up; the medical records of the remaining 74 patients (who performed 95 total 18F-FDG PET/CT scans) were analyzed retrospectively. This study was approved by the Institutional Ethics Committee.
According to the medical indications of 18F-FDG PET/CT, the 74 patients were classified in 4 groups (Figure 1, part I); clinical and epidemiological information is shown in Table 1:
-
Group 1. Patients with positive sTg or TgAb were subdivided in Group 1A (n = 9): negative post-therapeutic -131 whole body scan (RxWBS) and no foci of metastases identified at conventional image, and Group 1B (n = 13): RxWBS not compatible with suspicious foci at conventional image or not proportional to sTg level.
-
Group 2. Patients with histological findings of aggressive DTC variants (n = 21): oncocytic (n = 3), poorly differentiated areas (n = 2), tall-cell (n = 4), diffuse sclerosing (n = 4), insular (n = 5) and solid variant (n = 3) with incomplete biochemical or structural disease.
-
Group 3. Patients with positive RxWBS (n = 31): in this group, 18F-FDG PET/CT was performed to detect additional foci of undifferentiated metastases.
In the beginning of the study, 59 of 95 18F-FDG PET/CT scans were performed after TSH stimulation (Tg/TSH): hypothyroidism, TSH > 30 mcUI/mL or after recombinant human TSH, rhTSH, Genzyme Transgenics Corp., Cambridge, Massachusetts. Over the course of follow-up, the literature demonstrated that despite studies showing that the number of positive scans and standard uptake value (SUV) increase under rhTSH stimulation, there was no conclusive evidence that those findings improve clinical management (1212. Leboulleux S, Schroeder PR, Busaidy NL, Auperin A, Corone C, Jacene HA, et al. Assessment of the incremental value of recombinant thyrotropin stimulation before 2-[18F]-Fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography imaging to localize residual differentiated thyroid cancer. J Clin Endocrinol Metab. 2009;94(4):1310-6.,1414. Wiebel JL, Esfandiari NH, Papaleontiou M, Worden FP, Haymart MR. Evaluating Positron Emission Tomography Use in Differentiated Thyroid Cancer. Thyroid. 2015;25(9):1026-32.). Consequently, the remaining 36 scans were performed using LT4 (Tg/LT4). 18F-FDG PET/CT imaging and analysis were performed in accordance with the protocol described by Yamaga and cols. (1313. Yamaga LY, Cunha ML, Wagner J, Thom AF, Daniel MM, Funari MB. [Diagnostic value of positron emission tomography/computed tomography with fluorine-18 fluordeoxyglucose in patients with differentiated thyroid gland carcinoma, high thyroglobulin serum levels and negative iodine whole body scan]. Arq Bras Endocrinol Metabol. 2007;51(4):581-6.).
For the predictive value analysis, the following criteria defined by Hooft and cols. (1515. Hooft L, Hoekstra OS, Devillé W, Lips P, Teule GJ, Boers M, et al. Diagnostic accuracy of 18F-fluorodeoxyglucose positron emission tomography in the follow-up of papillary or follicular thyroid cancer. J Clin Endocrinol Metab. 2001;86(8):3779-86.) were used: 1) histology/cytology; 2) US-FNAC for cervical lesions; 3) focal 131I-uptake; 4) pathognomonic bone scan or MRI for bone metastases; 5) CT/MRI for brain metastases; and 6) progression of radiological documented lesions suspect for malignancy. The results were considered positive in the presence of 18F-FDG uptake in suspected lesions (visualized on conventional image) or in those patients with biochemical disease. The results were considered negative if there was no 18F-FDG uptake. All patients underwent cervical US as the routine serial assessment, and suspicious cervical lesions were submitted to US-guided fine-needle aspiration cytology (US-FNAC) (1616. Biscolla RP, Ikejiri ES, Mamone MC, Nakabashi CC, Andrade VP, Kasamatsu TS, et al. [Diagnosis of metastases in patients with papillary thyroid cancer by the measurement of thyroglobulin in fine needle aspirate]. Arq Bras Endocrinol Metabol. 2007;51(3):419-25.). Conventional imaging was performed during the follow-up if necessary (high levels of sTg measurements, WBS uptake, lung, retropharyngeal or bone suspicious metastases).
Serum Tg levels were measured by a highly sensitive chemiluminescence assay (Tg Access immunoassay, Beckman Coulter, Brea, CA) with a functional sensitivity of 0.1 ng/mL. TSH levels were measured using a third-generation assay that provided a functional sensitivity of 0.05 mUI/mL (1717. Vieira JG, Kunii IS, Nishida SK, Matsumura LK, Russo EMK, Maciel RMB. Development of an immunofluorimetric assay for the measurement of human thyrotropin (TSH) in serum and in total blood collected in filter paper. In. Arq Bras Endocrinol Metabol, 1992;36:7-12.).
According to the combined and serial data of conventional imaging, the patient’s clinical status was classified as stable or progressive disease. Progressive disease was defined as an increase in tumor size during the follow-up, and stable disease was defined as stability of the lesions. Then, we analyzed the association between 18F-FDG uptake and progressive disease. We also studied the association between the PET/CT results and sTg levels using the cutoff recommended by ATA, 10 ng/mL.
For the continuous variables, the difference between positive and negative 18F-FDG PET/CT groups was assessed using the Mann-Whitney test. The ROC curve was used for the continuous variables to calculate the best cut-off point. The chi-square test was used to determine the differences in the frequency of the categorical variables. A p < 0.05 result was considered significant.
RESULTS
18F-FDG PET/CT results and clinical relevance
Group 1A: patients with positive sTg or TgAb, negative RxWBS and no foci of metastases identified at conventional image (n = 9)
Ten scans were performed in this group. Although 18F-FDG PET/CT displayed 6 cervical positive lesions in only 3 patients, none was confirmed as metastasis based on US-FNAC. The sTg levels in this group were 0.2-4.9 ng/mL (Tg/LT4) and 3.9-7.4 ng/mL (Tg/TSH).
In conclusion, 18F-FDG PET/CT did not provide additional information in this group of patients.
Group 1B: patients with positive sTg or TgAb and RxWBS not compatible with suspicious foci at conventional image or not proportional to sTg level (n = 13)
Twenty 18F-FDG PET/CT scans were performed in this group of 13 patients, and nine of 13 presented positive 18F-FDG PET/CT scans (Table 2, patients 1-9). In those patients, the results helped clarify lesions visualized in conventional images that were RAI negative; in three of them, a second 18F-FDG PET/CT demonstrated the efficacy of the surgery indicated after the first scan results (Table 2, patients 1-3); in other three patients, the second 18F-FDG PET/CT was useful to show progression of the metastases (Table 2, patients 4, 6-7). The 18F-FDG PET/CT displayed, in all, cervical, mediastinal or retropharyngeal uptake in 4 patients who had confirmed metastatic lesions based on histological results (Table 2, patients 1-4). One patient (Table 2, patient 4) and the remaining 5 (Table 2, patient 5-9) presented diffuse pulmonary 18F-FDG uptake.
In group 1B, we considered that the 18F-FDG PET/CT results helped localize metastases in 9/13 (69%).
Group 2: patients with aggressive variants at the histological findings with incomplete biochemical or structural disease (n = 21)
Twenty-seven scans were performed in this group of 21 patients. In 10 of 21 patients, 18F-FDG PET/CT provided relevant information.
Oncocytic variant (n = 2): The scan was indicated for an undetectable sTg and positive RxWBS cervical metastasis uptake, and there was 18F-FDG uptake in the cervical subcutaneous tissue. The other patient presented with RAI negative but suspicious pulmonary lesions on conventional images, and the 18F-FDG PET/CT scan showed lung uptake. Both lesions were confirmed as metastases based on histological analysis (Table 3, patients 1-2), indicating that 18F-FDG PET/CT provided relevant information.
Poorly differentiated areas on histology (n = 1): the patient presented a positive RxWBS lumbar vertebrae metastasis with accelerated elevation of sTg, and the positive 18F-FDG uptake suggested possible tumor undifferentiation. This patient also presented with cerebral metastasis and had been treated with cerebral and vertebrae radiotherapy (Table 3, patient 4).
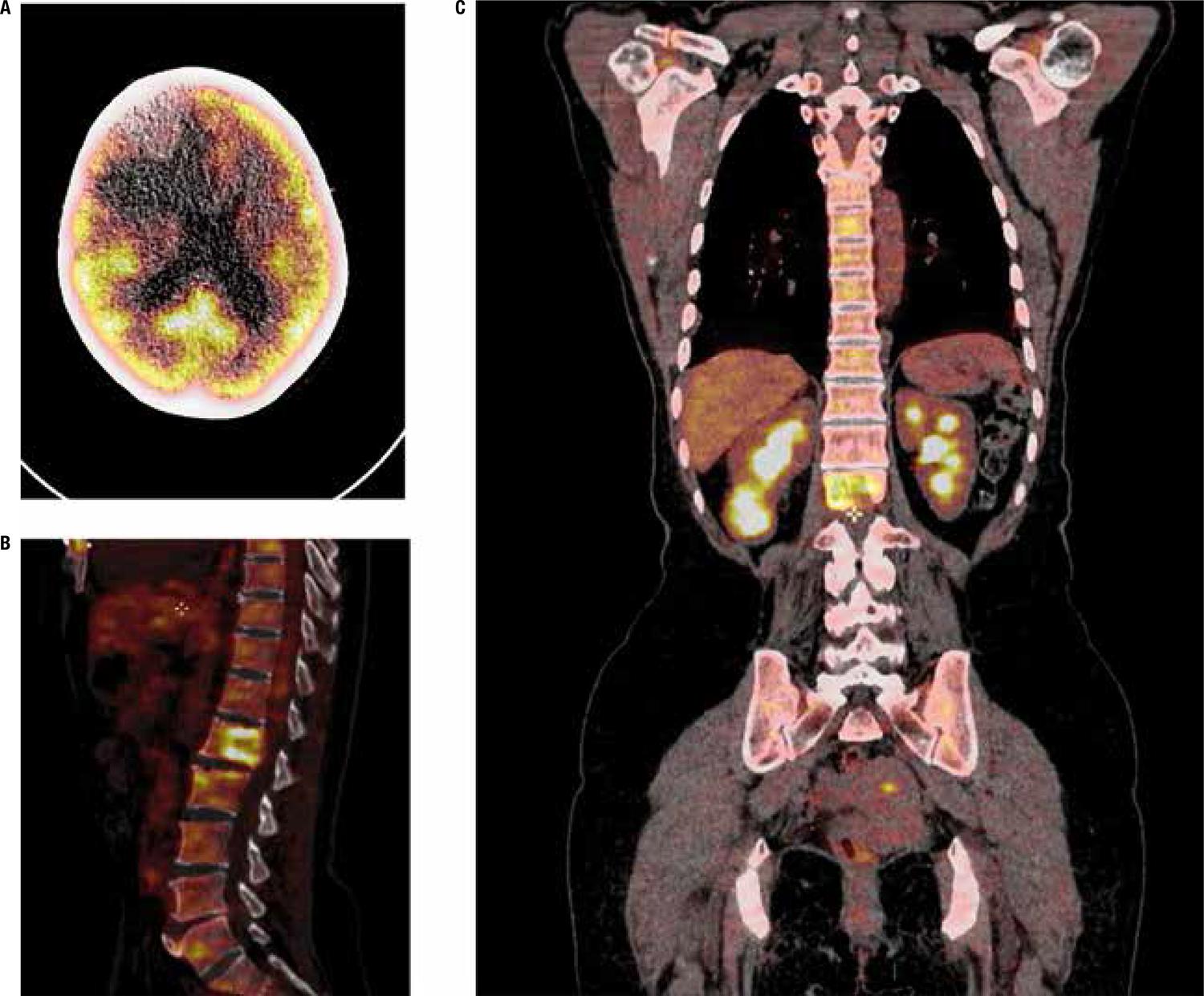
Other aggressive variants (n = 7):18F-FDG PET/CT provided relevant information in 7 patients. Two patients without previous RAI treatment underwent paired 18F-FDG PET/CT and DxWBS scans. A 18F-FDG negative scan combined with positive RAI uptake endorsed the first RAI treatment indication (Table 3, patients 6-7). The other 5 patients had 18F-FDG uptake in pulmonary nodules, suggesting undifferentiated metastases (Table 3, patients 8-12). Three patients underwent resection of the 18F-FDG positive metastases (Table 3, patients 8-10), but despite treatment, the disease progressed in all patients, and one patient presented with renal metastasis confirmed on histopathology, cerebral metastasis refractory to radiotherapy and death (Table 3, patient 8, Figure 2). In this group, the 18F-FDG PET/CT results contributed to the clinical management in 10/21 patients (48%).
18F-FDG PET/CT images show increased metabolic activity in 62-y-woman: A. Expansive lesion on frontal lobe of the brain; B. Lytic lesion on L2 vertebral body; C. Right lower renal mass. (Table 3, patient 8).
Group 3: patients with positive RxWBS (n = 31)
This group included 31 patients with positive WBS who underwent 39 scans. There was no additional 18F-FDG uptake suggestive of metastases in respect to RxWBS or conventional images. However, 2 patients with previous RxWBS positive pulmonary disease and increasing sTg/TgAb levels showed pulmonary 18F-FDG uptake, suggesting tumor undifferentiation. In this group of 31 patients, the 18F-FDG PET/CT results delineated prognosis in 2 patients (6%).
The clinical relevance of each group is summarized in Figure 1, part II.
18F-FDG PET/CT result as predictor of progressive disease
From the 95 18F-FDG PET/CT scans, we found 61 positive, 28 negative and 6 indeterminate scans. All eighteen patients who presented with progressive disease showed 18F-FDG uptake (100%) compared to twenty-nine of fifty-six patients who were stable (52%). The 18F-FDG uptake was associated with progressive disease (p = 0.0004).
18F-FDG PET/CT results and sTg measurements
The median serum Tg/LT4 was 9.4 ng/mL (0.1-898) in the positive PET/CT patients, compared to 0.8 ng/mL (0.1-44) in the PET/CT negative group (p = 0.001). In analyzing the Tg/TSH level, the median level in the positive PET/CT patients was 26 ng/mL (0.9-1,000), in contrast to 5.1 ng/mL (0.1-271) in the PET/CT negative group (p = 0.003) (Table 4A). In analyzing each group separately, there was a significant difference between the positive and negative PET/CT results in group 1 (for both Tg/LT4 and Tg/TSH) and group 2 (only for Tg/LT4). If we used the sTg level of 10 ng/mL, there were abnormal PET/CT results in 52% of all patients with Tg/LT4 levels ≤ 10 ng/mL and in 90% of patients with Tg/LT4 levels of > 10 ng/mL (p < 0.001) (Table 4B). For Tg/TSH, the outcome was 38% in Tg/TSH levels of ≤ 10 ng/mL versus 74% if Tg/TSH was > 10 ng/mL (p < 0.009). For each group, separately, there was a significant difference in only group 1 (for both Tg/LT4 and Tg/TSH) and group 2 (only for Tg/LT4).
– A. The median of thyroglobulin level from 18F-FDG PET/CT positive (FDG +) and negative (FDG -) patients. B. 18F-FDG PET/CT positive result according to the cutoff of sTg = 10 ng/mL.
DISCUSSION
High metabolic activity revealed by 18F-FDG avidity represents advanced tumor and undifferentiation. In these cases, poorly differentiated follicular cells might lose the ability to concentrate RAI, synthesize sTg, and progressively enhance glucose metabolism due to high cell activity and metabolic demand. In this way, 18F-FDG PET/CT has become a powerful tool to improve staging and tumor aggressiveness and investigate undifferentiated lesions that do not take up radioiodine, denoting important diagnostic and prognostic implications (1818. Robbins RJ, Larson SM. The value of positron emission tomography (PET) in the management of patients with thyroid cancer. Best Pract Res Clin Endocrinol Metab. 2008;22(6):1047-59.
19. Robbins RJ, Wan Q, Grewal RK, Reibke R, Gonen M, Strauss HW, et al. Real-time prognosis for metastatic thyroid carcinoma based on 2-[18F]fluoro-2-deoxy-D-glucose-positron emission tomography scanning. J Clin Endocrinol Metab. 2006;91(2):498-505.-2020. Hong CM, Ahn BC, Jeong SY, Lee SW, Lee J. Distant metastatic lesions in patients with differentiated thyroid carcinoma. Clinical implications of radioiodine and FDG uptake. Nuklearmedizin. 2013;52(4):121-9.).
The classical indication to perform 18F-FDG PET/CT in thyroid cancer patients is positive sTg measurements with negative WBS uptake (66. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.). In the literature, 18F-FDG PET/CT provides additional information not revealed by traditional images in 21-71% of patients, mostly in negative WBS (77. Wang W, Macapinlac H, Larson SM, Yeh SD, Akhurst T, Finn RD, et al. [18F]-2-fluoro-2-deoxy-D-glucose positron emission tomography localizes residual thyroid cancer in patients with negative diagnostic (131)I whole body scans and elevated serum thyroglobulin levels. J Clin Endocrinol Metab. 1999;84(7): 2291-302.,88. Helal BO, Merlet P, Toubert ME, Franc B, Schvartz C, Gauthier-Koelesnikov H, et al. Clinical impact of (18)F-FDG PET in thyroid carcinoma patients with elevated thyroglobulin levels and negative (131)I scanning results after therapy. J Nucl Med. 2001;42(10):1464-9.), and in 13-50% of patients with positive TgAb (2121. Ozkan E, Soydal C, Araz M, Aras G, Ibis E. The additive clinical value of 18F-FDG PET/CT in defining the recurrence of disease in patients with differentiated thyroid cancer who have isolated increased antithyroglobulin antibody levels. Clin Nucl Med. 2012;37(8):755-8.,2222. Seo JH, Lee SW, Ahn BC, Lee J. Recurrence detection in differentiated thyroid cancer patients with elevated serum level of antithyroglobulin antibody: special emphasis on using (18)F-FDG PET/CT. Clin Endocrinol (Oxf). 2010;72(4):558-63.).
In our study, we analyzed the classical indication of 18F-FDG PET/CT in 22 patients with positive sTg or TgAb, negative RxWBS and no foci of metastases identified at conventional image (Group 1A, n = 9) and those with positive sTg or TgAb and RxWBS not compatible with suspicious foci at conventional image or not proportional to sTg level (Group 1B, n = 13). In group 1A, 18F-FDG PET/CT did not detect additional metastases. The low sTg levels (0.2-4.9 ng/mL), even under stimulation (3.9-7.4 ng/mL), combined with microscopic metastasis might explain the lack of 18F-FDG-avid lesions, as 18F-FDG is limited in detecting minimal disease (under 1.0 cm). However, the 18F-FDG PET/CT scan helped unveil undifferentiated cervical, lung and mediastinal metastases in 9 patients (69%) in group 1B. The positive FDG uptake observed in this subgroup was associated with higher levels of sTg (Tg/LT4: 0.6-91 ng/mL and Tg/TSH: 2.4-292 ng/mL) and higher dimensions of metastasis.
In the subgroup 1B, surgery was possible in 4 of 9 patients with positive 18F-FDG PET/CT scan results. As described by Hall and Kloos (33. Hall NC, Kloos RT. PET imaging in differentiated thyroid cancer: where does it fit and how do we use it? Arq Bras Endocrinol Metabol. 2007;51(5):793-805.), the ideal of 18F-FDG, to identify resectable lesions to pursue a cure, should be attempted as undifferentiated lesions are less likely to respond to RAI, and additional surgery can lead to a higher rate of full remission during follow-up (2323. Ruhlmann M, Binse I, Bockisch A, Rosenbaum-Krumme SJ. Initial [18F]FDG PET/CT in high-risk DTC patients. A three-year follow-up. Nuklearmedizin. 2016;55(3):99-103.). The other 6 patients presented diffuse pulmonary 18F-FDG uptake, and there was no role for surgery.
The other aspect to consider is the behavior of aggressive histological variants. Those variants have unfavorable prognosis as they feature low iodine avidity and aggressive clinical behavior with more local and distance recurrences, less disease-free intervals and shorter survivals, requiring close follow-up and continued surveillance to pursue occult metastases. Publications regarding 18F-FDG PET/CT and aggressive variants describe these subtypes as more 18F-FDG-avid than RAI tumors. Concerning oncocytic cell tumors, 80% of patients have no iodine-avid tumor (2424. Palaniswamy SS, Subramanyam P. Diagnostic utility of PETCT in thyroid malignancies: an update. Ann Nucl Med. 2013;27(8):681-93.), and therefore, 18F-FDG PET/CT is a valuable tool for screening occult recurrence, evaluating prognosis, and providing additional images not presented by WBS or conventional image (2525. Pryma DA, Schöder H, Gönen M, Robbins RJ, Larson SM, Yeung HW. Diagnostic accuracy and prognostic value of 18F-FDG PET in Hürthle cell thyroid cancer patients. J Nucl Med. 2006;47(8):1260-6.,2626. Plotkin M, Hautzel H, Krause BJ, Schmidt D, Larisch R, Mottaghy FM, et al. Implication of 2-18fluor-2-deoxyglucose positron emission tomography in the follow-up of Hürthle cell thyroid cancer. Thyroid. 2002;12(2):155-61.). In regard to the other aggressive subtypes, few studies consider 18F-FDG PET/CT as a useful guide in the management of insular (2727. Diehl M, Graichen S, Menzel C, Lindhorst E, Grünwald F. F-18 FDG PET in insular thyroid cancer. Clin Nucl Med. 2003;28(9):728-31.), sclerosing diffuse (2828. Kuo CS, Tang KT, Lin JD, Yang AH, Lee CH, Lin HD. Diffuse sclerosing variant of papillary thyroid carcinoma with multiple metastases and elevated serum carcinoembryonic antigen level. Thyroid. 2012;22(11):1187-90.) and tall cell (2929. Nascimento C, Borget I, Al Ghuzlan A, Deandreis D, Hartl D, Lumbroso J, et al. Postoperative fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography: an important imaging modality in patients with aggressive histology of differentiated thyroid cancer. Thyroid. 2015;25(4):437-44.) variants. Treglia and cols. (3030. Treglia G, Annunziata S, Muoio B, Salvatori M, Ceriani L, Giovanella L. The role of fluorine-18-fluorodeoxyglucose positron emission tomography in aggressive histological subtypes of thyroid cancer: an overview. Int J Endocrinol. 2013;2013:856189.) concluded that the 18F-FDG PET scan usefulness is clear for the oncocytic cell, uncertain for poorly differentiated cancers and suggestive in the other aggressive forms. The concept of tumor undifferentiation was also observed in patients in group 2 (n = 21). In our study, the results corroborate the findings in the literature. The higher FDG uptake presented in this group can be attributed to more undifferentiated thyroid tumors with more avid uptake for 18F-FDG and high levels of sTg. Pryma and cols. (2525. Pryma DA, Schöder H, Gönen M, Robbins RJ, Larson SM, Yeung HW. Diagnostic accuracy and prognostic value of 18F-FDG PET in Hürthle cell thyroid cancer patients. J Nucl Med. 2006;47(8):1260-6.) suggested that 18F-FDG PET/CT could be indicated in oncocytic cell carcinoma in postoperative staging and as follow-up in patients with an increase in sTg or recurrent disease, whereas Nascimento and cols. (2929. Nascimento C, Borget I, Al Ghuzlan A, Deandreis D, Hartl D, Lumbroso J, et al. Postoperative fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography: an important imaging modality in patients with aggressive histology of differentiated thyroid cancer. Thyroid. 2015;25(4):437-44.) recommended routine early postoperative 18F-FDG PET/CT concomitantly with RxWBS in all patients with aggressive histological DTC.
18F-FDG and RAI may function as complementary tools in DTC (99. Lee JW, Lee SM, Lee DH, Kim YJ. Clinical utility of 18F-FDG PET/CT concurrent with 131I therapy in intermediate-to-high-risk patients with differentiated thyroid cancer: dual-center experience with 286 patients. J Nucl Med. 2013;54(8):1230-6.,3131. Riemann B, Uhrhan K, Dietlein M, Schmidt D, Kuwert T, Dorn R, et al. Diagnostic value and therapeutic impact of (18)F-FDG-PET/CT in differentiated thyroid cancer. Results of a German multicentre study. Nuklearmedizin. 2013;52(1):1-6.) to investigate additional undifferentiated metastases. However, in our cohort, we did not find additional metastases visualized by WBS. WBS-positive patients have no classical indication for 18F-FDG PET/CT and cost-efficacy must be considered in WBS positive group patients.
ATA recommends 18F-FDG PET/CT in high-risk DTC patients with elevated sTg, generally Tg/TSH > 10 ng/mL (66. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.). If Tg/TSH is ≤ 10 ng/mL, the sensitivity of PET/CT is low, ranging from less than 10% to 30% (66. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.). In our data, 38% of all scans performed with Tg/TSH of ≤ 10 ng/mL and 13% of group 1 were positive, similar to the literature data. In contrast, 74% of PET/CT performed with Tg/TSH of > 10 ng/mL provided positive results (as was the case for 100% of group 1). Regarding unstimulated Tg analysis, Tg/LT4 > 10 ng/mL was associated with higher lesion detection in overall patients and groups 1 and 2 when compared to Tg/LT4 ≤ 10 ng/mL. As a matter of fact, more important than the influence of rhTSH or thyroid hormone withdrawal in 18F-FDG PET/CT is the presence of high levels of Tg (Tg/TSH or Tg/LT4 > 10 ng/mL). Over the last years, it has been demonstrated that both strategies, with or without TSH stimulation, do not considerably lead to management changes (1212. Leboulleux S, Schroeder PR, Busaidy NL, Auperin A, Corone C, Jacene HA, et al. Assessment of the incremental value of recombinant thyrotropin stimulation before 2-[18F]-Fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography imaging to localize residual differentiated thyroid cancer. J Clin Endocrinol Metab. 2009;94(4):1310-6.,3232. van Tol KM, Jager PL, Piers DA, Pruim J, de Vries EG, Dullaart RP, et al. Better yield of (18)fluorodeoxyglucose-positron emission tomography in patients with metastatic differentiated thyroid carcinoma during thyrotropin stimulation. Thyroid. 2002;12(5):381-7.).
Additional factors than sTg that influence 18F-FDG PET/CT sensitivity are tumor de-differentiation and larger tumor burden (66. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.), as we have seen in our results. Additionally, the scanning is limited in detecting minimal disease (generally less than 1 cm) and well-differentiated metastases, resulting in false negative outcomes. It is well known that inflammatory lesions can take up FDG, and there may be false positive results. All these features should be considered with care to avoid misjudgments. The frequency of false positive lesions in the literature varies among studies from 0 to 39% (66. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.), and this high number justifies the PET/CT results through the combined data of clinical, laboratorial, conventional image and cytological/histological information to guide ongoing clinical assessments.
The present work has some limitations. First, this was a retrospective study, and direct comparison of the detection rate of metastases between 18F-FDG PET/CT and other diagnostic methods was not the design of this study. Additionally, we had no cytological or pathological confirmation of all lesions with 18F-FDG uptake. Based on the serial evaluation of thyroid cancer patients with laboratorial and image exams to assess tumor growth, invasive procedure to confirm the metastases is seldom necessary.
In conclusion, 18F-FDG PET/CT results changed the management in 28% (21/74) of patients, mostly in 1B group, patients with RxWBS not compatible with suspicious foci at conventional image or not proportional to sTg level (69%, 9/13) and in group 2, patients with aggressive histological variant patients (48%, 10/21), confirming the literature indications that 18F-FDG PET/CT is more useful in these two groups of patients. For group 1A patients, with positive sTg or TgAb, negative RxWBS and no foci of metastases identified at the conventional image, 18F-FDG PET/CT was not useful, probably due to low levels of sTg and low tumor burden. Additionally, this study showed that 18F-FDG uptake was associated with progressive disease and helped display undifferentiated lesions guiding clinical assessments with respect to surgeries or expectant treatments.
Acknowledgments
the authors thank the team of Thyroid Diseases Centers at Universidade Federal de São Paulo and Instituto Israelita de Ensino e Pesquisa Albert Einstein, Elza Setsuko Ikejiri, Maria da Conceição Oliveira Mamone, Felipe Augusto Brasileiro Vanderlei and Jairo Tabacow Hidal.
REFERENCES
-
1Spencer CA. Challenges of serum thyroglobulin (Tg) measurement in the presence of Tg autoantibodies. J Clin Endocrinol Metab. 2004;89(8):3702-4.
-
2Pineda JD, Lee T, Ain K, Reynolds JC, Robbins J. Iodine-131 therapy for thyroid cancer patients with elevated thyroglobulin and negative diagnostic scan. J Clin Endocrinol Metab. 1995;80(5):1488-92.
-
3Hall NC, Kloos RT. PET imaging in differentiated thyroid cancer: where does it fit and how do we use it? Arq Bras Endocrinol Metabol. 2007;51(5):793-805.
-
4Marcus C, Antoniou A, Rahmim A, Ladenson P, Subramaniam RM. Fluorodeoxyglucose positron emission tomography/computerized tomography in differentiated thyroid cancer management: Importance of clinical justification and value in predicting survival. J Med Imaging Radiat Oncol. 2015;59(3): 281-8.
-
5Pace L, Klain M, Salvatore B, Nicolai E, Zampella E, Assante R, et al. Prognostic role of 18F-FDG PET/CT in the postoperative evaluation of differentiated thyroid cancer patients. Clin Nucl Med. 2015;40(2):111-5.
-
6Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.
-
7Wang W, Macapinlac H, Larson SM, Yeh SD, Akhurst T, Finn RD, et al. [18F]-2-fluoro-2-deoxy-D-glucose positron emission tomography localizes residual thyroid cancer in patients with negative diagnostic (131)I whole body scans and elevated serum thyroglobulin levels. J Clin Endocrinol Metab. 1999;84(7): 2291-302.
-
8Helal BO, Merlet P, Toubert ME, Franc B, Schvartz C, Gauthier-Koelesnikov H, et al. Clinical impact of (18)F-FDG PET in thyroid carcinoma patients with elevated thyroglobulin levels and negative (131)I scanning results after therapy. J Nucl Med. 2001;42(10):1464-9.
-
9Lee JW, Lee SM, Lee DH, Kim YJ. Clinical utility of 18F-FDG PET/CT concurrent with 131I therapy in intermediate-to-high-risk patients with differentiated thyroid cancer: dual-center experience with 286 patients. J Nucl Med. 2013;54(8):1230-6.
-
10Rosenbaum-Krumme SJ, Görges R, Bockisch A, Binse I. 18F-FDG PET/CT changes therapy management in high-risk DTC after first radioiodine therapy. Eur J Nucl Med Mol Imaging. 2012;39(9):1373-80.
-
11Pomerri F, Cervino AR, Al Bunni F, Evangelista L, Muzzio PC. Therapeutic impact of (18)F-FDG PET/CT in recurrent differentiated thyroid carcinoma. Radiol Med. 2014;119(2):97-102.
-
12Leboulleux S, Schroeder PR, Busaidy NL, Auperin A, Corone C, Jacene HA, et al. Assessment of the incremental value of recombinant thyrotropin stimulation before 2-[18F]-Fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography imaging to localize residual differentiated thyroid cancer. J Clin Endocrinol Metab. 2009;94(4):1310-6.
-
13Yamaga LY, Cunha ML, Wagner J, Thom AF, Daniel MM, Funari MB. [Diagnostic value of positron emission tomography/computed tomography with fluorine-18 fluordeoxyglucose in patients with differentiated thyroid gland carcinoma, high thyroglobulin serum levels and negative iodine whole body scan]. Arq Bras Endocrinol Metabol. 2007;51(4):581-6.
-
14Wiebel JL, Esfandiari NH, Papaleontiou M, Worden FP, Haymart MR. Evaluating Positron Emission Tomography Use in Differentiated Thyroid Cancer. Thyroid. 2015;25(9):1026-32.
-
15Hooft L, Hoekstra OS, Devillé W, Lips P, Teule GJ, Boers M, et al. Diagnostic accuracy of 18F-fluorodeoxyglucose positron emission tomography in the follow-up of papillary or follicular thyroid cancer. J Clin Endocrinol Metab. 2001;86(8):3779-86.
-
16Biscolla RP, Ikejiri ES, Mamone MC, Nakabashi CC, Andrade VP, Kasamatsu TS, et al. [Diagnosis of metastases in patients with papillary thyroid cancer by the measurement of thyroglobulin in fine needle aspirate]. Arq Bras Endocrinol Metabol. 2007;51(3):419-25.
-
17Vieira JG, Kunii IS, Nishida SK, Matsumura LK, Russo EMK, Maciel RMB. Development of an immunofluorimetric assay for the measurement of human thyrotropin (TSH) in serum and in total blood collected in filter paper. In. Arq Bras Endocrinol Metabol, 1992;36:7-12.
-
18Robbins RJ, Larson SM. The value of positron emission tomography (PET) in the management of patients with thyroid cancer. Best Pract Res Clin Endocrinol Metab. 2008;22(6):1047-59.
-
19Robbins RJ, Wan Q, Grewal RK, Reibke R, Gonen M, Strauss HW, et al. Real-time prognosis for metastatic thyroid carcinoma based on 2-[18F]fluoro-2-deoxy-D-glucose-positron emission tomography scanning. J Clin Endocrinol Metab. 2006;91(2):498-505.
-
20Hong CM, Ahn BC, Jeong SY, Lee SW, Lee J. Distant metastatic lesions in patients with differentiated thyroid carcinoma. Clinical implications of radioiodine and FDG uptake. Nuklearmedizin. 2013;52(4):121-9.
-
21Ozkan E, Soydal C, Araz M, Aras G, Ibis E. The additive clinical value of 18F-FDG PET/CT in defining the recurrence of disease in patients with differentiated thyroid cancer who have isolated increased antithyroglobulin antibody levels. Clin Nucl Med. 2012;37(8):755-8.
-
22Seo JH, Lee SW, Ahn BC, Lee J. Recurrence detection in differentiated thyroid cancer patients with elevated serum level of antithyroglobulin antibody: special emphasis on using (18)F-FDG PET/CT. Clin Endocrinol (Oxf). 2010;72(4):558-63.
-
23Ruhlmann M, Binse I, Bockisch A, Rosenbaum-Krumme SJ. Initial [18F]FDG PET/CT in high-risk DTC patients. A three-year follow-up. Nuklearmedizin. 2016;55(3):99-103.
-
24Palaniswamy SS, Subramanyam P. Diagnostic utility of PETCT in thyroid malignancies: an update. Ann Nucl Med. 2013;27(8):681-93.
-
25Pryma DA, Schöder H, Gönen M, Robbins RJ, Larson SM, Yeung HW. Diagnostic accuracy and prognostic value of 18F-FDG PET in Hürthle cell thyroid cancer patients. J Nucl Med. 2006;47(8):1260-6.
-
26Plotkin M, Hautzel H, Krause BJ, Schmidt D, Larisch R, Mottaghy FM, et al. Implication of 2-18fluor-2-deoxyglucose positron emission tomography in the follow-up of Hürthle cell thyroid cancer. Thyroid. 2002;12(2):155-61.
-
27Diehl M, Graichen S, Menzel C, Lindhorst E, Grünwald F. F-18 FDG PET in insular thyroid cancer. Clin Nucl Med. 2003;28(9):728-31.
-
28Kuo CS, Tang KT, Lin JD, Yang AH, Lee CH, Lin HD. Diffuse sclerosing variant of papillary thyroid carcinoma with multiple metastases and elevated serum carcinoembryonic antigen level. Thyroid. 2012;22(11):1187-90.
-
29Nascimento C, Borget I, Al Ghuzlan A, Deandreis D, Hartl D, Lumbroso J, et al. Postoperative fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography: an important imaging modality in patients with aggressive histology of differentiated thyroid cancer. Thyroid. 2015;25(4):437-44.
-
30Treglia G, Annunziata S, Muoio B, Salvatori M, Ceriani L, Giovanella L. The role of fluorine-18-fluorodeoxyglucose positron emission tomography in aggressive histological subtypes of thyroid cancer: an overview. Int J Endocrinol. 2013;2013:856189.
-
31Riemann B, Uhrhan K, Dietlein M, Schmidt D, Kuwert T, Dorn R, et al. Diagnostic value and therapeutic impact of (18)F-FDG-PET/CT in differentiated thyroid cancer. Results of a German multicentre study. Nuklearmedizin. 2013;52(1):1-6.
-
32van Tol KM, Jager PL, Piers DA, Pruim J, de Vries EG, Dullaart RP, et al. Better yield of (18)fluorodeoxyglucose-positron emission tomography in patients with metastatic differentiated thyroid carcinoma during thyrotropin stimulation. Thyroid. 2002;12(5):381-7.
-
Financial disclosure: the research is supported by the São Paulo State Research Foundation (Fapesp) grant 2006/60402-1 (to R.M.B.M.) and grant 25000.168513/2008-11 from the Brazilian Ministry of Health.
Publication Dates
-
Publication in this collection
18 Sept 2017 -
Date of issue
Sept-Oct 2017
History
-
Received
12 Nov 2016 -
Accepted
18 Mar 2017