Abstracts
Background
The hepatitis C virus is one of the main causes of liver disease worldwide and may develop nutritional deficiencies.
Objective
The objective of this study was to assess and compare different nutritional status methods of adult patients with chronic hepatitis C virus, and to describe inadequacies in dietary intake.
Methods
A cross-sectional study was conducted with adult outpatients with hepatitis C virus at a Brazilian hospital. Nutritional assessment included the 24-hour dietary recall, anthropometry (body weight, height, body mass index, triceps skinfold, mid-upper arm circumference, mid-arm muscle circumference, mid-upper arm muscle area, adductor policis muscle), Subjective Global Assessment, Royal Free Hospital Global Assessment and handgrip strength.
Results
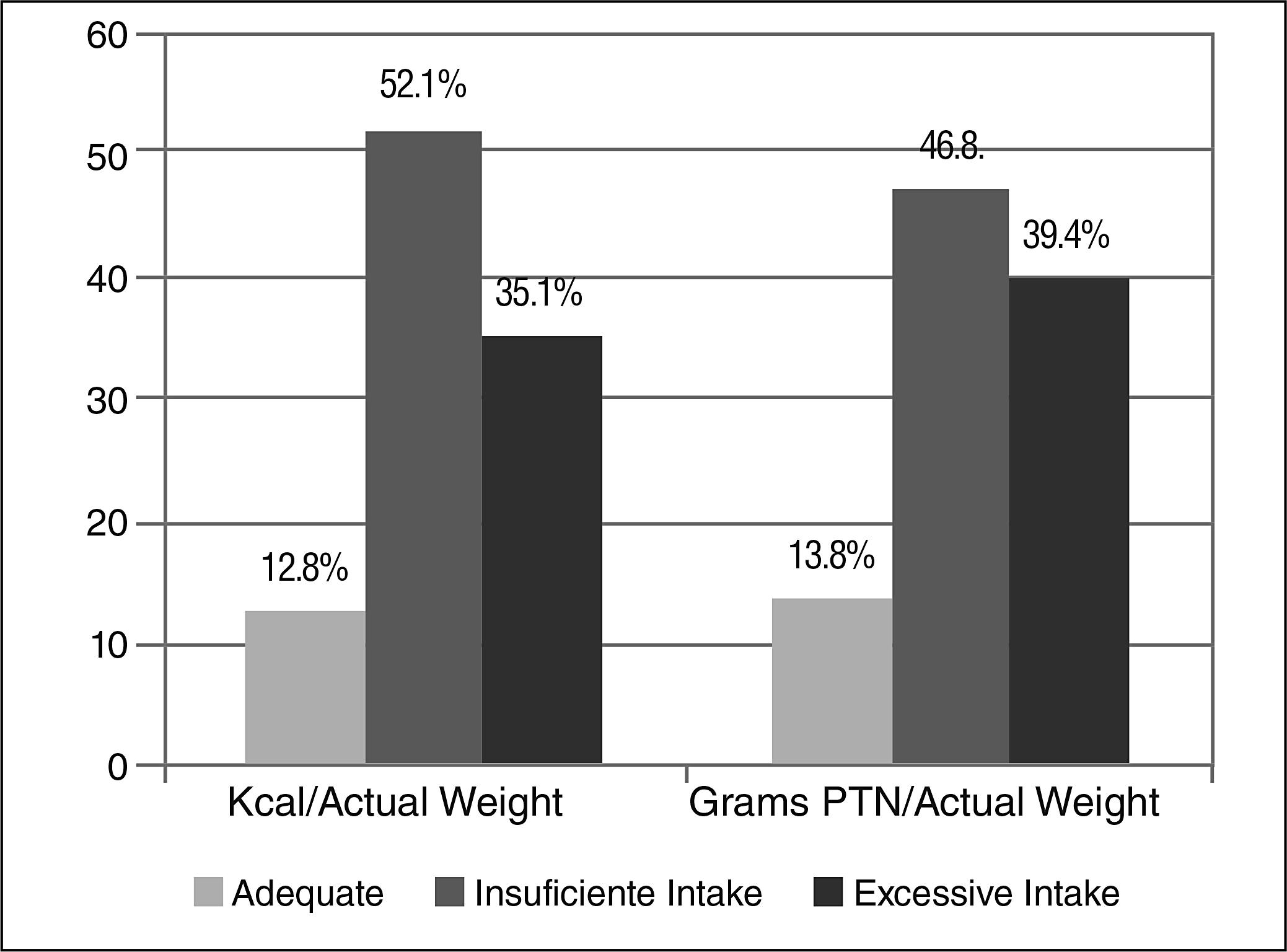
A total of 94 outpatients (ages 30 to 76 years), was included, 46 were men. The prevalence of malnutrition as measured by the different methods was 6.4% (body mass index); 60.6% (handgrip strength), and 53.2% (Royal Free Hospital Global Assessment). There was correlation between mid-upper arm circumference and mid-arm muscle circumference (r=0.821), mid-upper arm circumference and triceps skinfold (r=0.575) and mid-upper arm circumference and mid-upper arm muscle area (r=0.781). Energy and protein intakes were below recommended levels in 49 (52.1%) and 44 (46.8%) of patients, respectively. Inadequate calcium, potassium, zinc and vitamin C intakes occurred in 92.6%, 97.9%, 63.8% and 60.6% of patients. There was an association between dietary energy and protein intake with Royal Free Hospital Global Assessment (P<0.001) and a tendency for them to be associated with handgrip strength (P=0.076 and P=0.054).
Conclusion
Malnutrition is frequently in hepatitis C virus patients. They have high prevalence of inadequate energy, protein and micronutrients intake, even in the absence of cirrhosis.
Nutrition Assessment; Chronic hepatitis C; Anthropometry; Protein-energy malnutrition
Contexto
O vírus da hepatite C é uma das principais causas de hepatopatia no mundo todo. Hepatopatas podem apresentar deficiências nutricionais e desnutrição, influenciando no seu prognóstico.
Objetivo
O objetivo do estudo foi avaliar o estado nutricional de pacientes adultos portadores crônicos do vírus da hepatite C, comparar os métodos de avaliação nutricional e descrever a prevalência de inadequação de ingestão alimentar.
Métodos
Foi realizado um estudo transversal em adultos portadores do vírus da hepatite C não cirróticos e não transplantados em acompanhamento ambulatorial no Hospital de Clínicas de Porto Alegre. A avaliação nutricional incluiu antropometria (peso, altura, índice de massa corporal, prega cutânea tricipital, circunferência do braço, circunferência muscular do braço, área muscular do braço e músculo adutor do polegar), Avaliação Subjetiva Global, Avaliação Subjetiva do Royal Free Hospital, dinamometria e Inquérito Recordatório de 24 horas.
Resultados
De 94 pacientes (idade: 30 a 76 anos), 46 eram homens. A prevalência de desnutrição foi de 6,4% (índice de massa corporal), 60,6% (dinamometria) e 53,2% (Avaliação Subjetiva do Royal Free Hospital). Houve correlação entre circunferência do braço e circunferência muscular do braço (r=0,821), circunferência do braço e prega cutânea tricipital (r=0,575), circunferência do braço e área muscular do braço (r=0,781). Ingestão energética abaixo do recomendado ocorreu em 49 (52,1%) indivíduos e baixa ingestão proteica em 44 (46,8%). Consumo inadequado de cálcio, potássio, zinco, vitamina C ocorreu em 92,6%, 97,9%, 63,8% e 60,6% da amostra, respectivamente e consumo excessivo de sódio ocorreu em 53,2%. Houve associação significativa entre o consumo de energia e proteína com o Avaliação Subjetiva do Royal Free Hospital (P<0,001) e uma tendência de associação com a dinamometria (P=0,076 e P=0,054).
Conclusão
Desnutrição é frequente em portadores crônicos de hepatite C. Pacientes com vírus da hepatite C têm alta prevalência de ingestão energética e proteica inadequada.
Avaliação nutricional; Hepatite C crônica; Antropometria; Desnutrição proteico-calórica
INTRODUCTION
The hepatitis C virus (HCV) is one of the main causes of chronic liver disease(3030. Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis. 2005;5:558–67.) and it is estimated that 3% of the world population is currently infected(33. Associação Médica Brasileira e Conselho Federal de Medicina. Hepatite C crônica: tratamento. Projeto Diretrizes, 2009., 3232. World Health Organization, Geneva. Weekly Epidemiological Record. 1997;46:341-8.). In Brazil, the estimated prevalence in the general population is between 1 to 2% (3131. Sociedade Brasileira de Hepatologia. Epidemiologia da infecção pelo vírus da hepatite C no Brasil. Available from: http://www.fmt.am.gov.br/trabalhos/anais/virologia/infec_brasil.htm
http://www.fmt.am.gov.br/trabalhos/anais...
).
Liver disease, affects nutrient digestion, absorption, storage and metabolism, which may lead to vitamin and mineral deficiencies and protein-energy malnutrition(66. Canadian guidelines for Health Care Providers. Hepatitis C: Nutrition Care. Dietitians of Canada, 2003.).
Malnutrition is frequently in this population, but it is undiagnosed(2626. Ritter L, Gazzola J. Nutritional evaluation of the cirrhotic patient: an objective, subjective or multicompartmental approach? Arq Gastroenterol. 2006;43(1):66-70.). It is directly related with patient prognosis, and leads to increased morbidity, mortality and hospital expenditures in patients with cirrhosis(22. Álvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21(2):113-7., 1010. Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Desnutrição e inadequação alimentar de pacientes aguardando transplante hepático. Rev Assoc Med Brás. 2009;55(4):389-93., 2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.). There is no gold standard to the diagnosis of malnutrition in liver disease patients(22. Álvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21(2):113-7., 1212. Gottschall CBA, Nunes FF, Aydos MED, Bragança AC, Felix DR, Rabito EI, Álvares-da-Silva MR. Contribution of dynamometry and the royal free hospital global assessment to the nutritional assessment of patients with chronic liver diseases. Rev Chil Nutr. 2012;39(4):152-8., 1313. Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4.).
As there are few studies on the nutritional status of non-cirrhotic HCV patients(1212. Gottschall CBA, Nunes FF, Aydos MED, Bragança AC, Felix DR, Rabito EI, Álvares-da-Silva MR. Contribution of dynamometry and the royal free hospital global assessment to the nutritional assessment of patients with chronic liver diseases. Rev Chil Nutr. 2012;39(4):152-8., 2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.), the objectives of this study were to assess the nutritional status of this population, comparing different nutritional assessment methods, and to evaluate their dietary intake.
METHODS
A cross-sectional study was performed with non-cirrhotic chronic HCV patients (18 years or older), of both gender, attending the outpatient clinic at the Gastroenterology Division (Liver Unit) of the Hospital de Clínicas de Porto Alegre (HCPA), Brazil. Patients with biopsy-proven or clinical evident cirrhosis, hepatocellular carcinoma, chronic renal failure, HIV and/or hepatitis B virus co-infection and those unable to be tested with the dynamometer were excluded.
Data collection occurred between April and September of 2012. All included patients signed an informed consent form. The study was approved by the HCPA’s Ethics in Research Board.
Information on HCV genotype, liver biopsy, and antiviral therapy was obtained. Current body weight, height, body mass index (BMI), triceps skinfold (TSF) and mid-upper arm circumference (MUAC) were taken. Mid-arm muscle circumference (MAMC) and mid-upper arm muscle area (MUAMA) were then calculated(1414. Heyward VH, Stolarczyk LM. Avaliação da composição corporal aplicada. Barueri: Manole, 2000.). The anthropometric parameters were classified based on Frisancho(1111. Frisancho AR. Anthropometric standards for the assessment of growth and nutrition status. The University of Michigan Press: Ann Arbor, 1990.), according to the sex and age. Patients were asked about their usual body weight and based on the reported values, their 6-month weight loss was calculated. Finally, the adductor policis muscle (APM)(2121. Lameu EB, Gerude MF, Corrêa RC, Lima KA. Adductor policis muscle: a new anthropometric parameter. Rev Hosp Clín Fac Med. 2004;59(2):57-62.) was measured and classified according to Lameu (2004). Handgrip strength (HGS) in the non-dominant hand(2828. Schlüssel MM, Dos Anjos LA, Vasconcellos MTL, Kac G. Reference values of handgrip dynamometry of health adults: a population-based study. Clinical Nutrition 2008;27:601-7.) was classified according to Schlüssel (2008). Subjective Global Assessment (SGA), proposed by Detsky et al.(88. Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, Jeejeebhoy KN. What is Subject Global Assessment of Nutritional Status? JPEN. 1987;11:8-13.), which is based on patients’ clinical history and physical examination, and Global Assessment proposed by the Royal Free Hospital (RFH-GA)(2222. Morgan MY, Madden AM, Soulsby CT, Morris RW. Derivation and validation of a new global method for assessing nutritional status in patients with cirrhosis. Hepatology. 2006;44(4):823-5.) were also assessed. The 24-hour recall(99. Duarte ACG. Avaliação nutricional: aspectos clínicos e laboratoriais. São Paulo: Atheneu, 2007.) (24 hR) was used to assess dietary intake. Energy and protein intake were compared to ESPEN’s(2525. Plauth M, Merli M, Kondrup J, Weimann A, Ferenci P, Müller MJ. Espen guidelines for nutrition in liver diseases and transplantation. Clinical Nutrition. 1997;16:43-55.) recommendations for patients with liver disease, which are 25 to 30 kcal/kg and 1.0 to 1.2 g/kg of current body weight, respectively. Micronutrient intake was compared to the DRIs(1515. Institute of Medicine (IOM). Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, D.C.: National Academy Press, 1997a, 454p.
16. Institute of Medicine (IOM). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, D.C.: National Academy Press, 2005a, 1357p.
17. Institute of Medicine (IOM). Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc. Washington, D.C.: National Academy Press, 2001a, 773p.
18. Institute of Medicine (IOM). Dietary reference intakes for vitamin C, vitamin E, selenium and carotenoids. Washington, D.C.: National Academy Press, 2000a, 506p.-1919. Institute of Medicine (IOM). Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, D.C.: National Academy Press, 2004a, 638p.).
Statistical analysis
The database for this study was created using Microsoft Office Excel 2007, and the Statistical Package for Social Science (SPSS, version 18.0.0) software was used for the data analysis. Categorical variables were described using frequency tables and continuous variables had their means and standard deviations calculated. Pearson’s chi-squared test was used for the comparative analysis between categorical variables. Pearson’s correlation and Bland-Altman’s analysis, respectively, were used to assess the correlation and agreement between the different nutritional status assessment methods. The kappa coefficient was also used to verify the agreement between the different methods.
RESULTS
Ninety-four patients were included, and their characteristics are shown in Table 1. Their average age was 52.6 years (30 to 76 years), and 23 were 60 years old or older. Eight (8.5%) patients had not undergone liver biopsy, but had no signs of clinically evident cirrhosis.
Average anthropometric figures are shown in Table 2. Two patients had significant 6-month weight loss (ranging between 5% to 10%) and four (4.2%) patients had severe weight loss of more than 10% of their usual weight. The percentage of individuals classified as having malnutrition according to each method is described in Figure 1. During the physical exam which is part of the SGA, no patients had edema or ascites.
Malnutrition according to different nutritional assessment methods.
BMI: body mass index; MUAC: mid-upper arm circumference; TSF: triceps skinfold; MAMC: mid-arm muscle circumference; MUAMA: mid-upper arm muscle área; HGS: handgrip strenght; APM: adductor policis muscle; SGA: subjective global assessment; RFH-GA: Royal Free Hospital Global Assessment.
When compared by the kappa coefficient, only the MUAC (k=0.448) agreed moderately with the MUAMA (k=0.490). According to the Bland-Altman analysis, however, there was correlation between MUAC and TSF, TSF and MAMC, and TSF and MUAMA. Pearson’s linear correlation was shown to be good between MUAC and MAMC (r=0.821), MUAC and TSF (r=0.575) and MUAC and MUAMA (r=0.781).
Most patients had lower intakes of calcium, potassium, zinc and vitamin C, and higher intakes of sodium, iron, phosphorus and cholesterol (Table 3). Median energy and protein intakes were 24.6 kcal/kg and 1.16 g/kg of current body weight, respectively. Figure 2 shows the percentage of patients with adequate versus inadequate energy and protein intakes, according to ESPEN(2525. Plauth M, Merli M, Kondrup J, Weimann A, Ferenci P, Müller MJ. Espen guidelines for nutrition in liver diseases and transplantation. Clinical Nutrition. 1997;16:43-55.).
There was a significant association between Royal Free Hospital’s Global Assessment and energy and protein intakes (P<0.001), and HGS tended to be associated with dietary intake (energy and protein) (P=0.054). Other correlations between dietary intake and antiretroviral treatment, degree of fibrosis and percent weight loss were not significant (Table 4).
DISCUSSION
Malnutrition is frequently in patients with liver disease, but in clinical practice little attention is given to this condition. Studies using different methods of nutritional assessment report the prevalence of malnutrition and inadequate energy and protein intakes in patients with cirrhosis who are waiting for a liver transplant(11. Álvares-da-Silva MR, Gottschall CBA, Waechter FL, Hadlich E, Sampaio JA, Francesconi CFM. The use of early enteral feeding post orthotopic liver transplantation in adults. Arq Gastroenterol. 2004;41(3):147-9., 22. Álvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21(2):113-7., 55. Bragança ACC, Álvares-da-Silva MR. Prevalence of diabetes mellitus and impaired glucose tolerance in patients with decompensated cirrhosis being evaluated for liver transplantation: the utility of oral glucose tolerance test. Arq Gastroenterol. 2010;47(1):22-7., 77. Carvalho L, Parise ER. Evaluation of nutritional status of nonhospitalized patients with liver cirrhosis. Arq Gastroenterol. 2006;43(4):269-74., 1010. Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Desnutrição e inadequação alimentar de pacientes aguardando transplante hepático. Rev Assoc Med Brás. 2009;55(4):389-93., 1313. Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4., 2424. Peng S, Plank LD, McCall,JL, Gillanders LK, McIlroy K, Gane E. Body composition, musclefunction, and energy expenditure in patients with liver cirrhosis: a comprehensive study. Am J Clin Nutr. 2007;85:1257-66., 2727. Roongpisuthipong C, Sobhonlidsuk A, Nantiruj K, Songchitsomboon S. Nutritional assessment in various stages of liver cirrhosis. Nutrition. 2001;17(9):761-5.) but few studies assess patients with chronic hepatitis C without complications, such as cirrhosis(1212. Gottschall CBA, Nunes FF, Aydos MED, Bragança AC, Felix DR, Rabito EI, Álvares-da-Silva MR. Contribution of dynamometry and the royal free hospital global assessment to the nutritional assessment of patients with chronic liver diseases. Rev Chil Nutr. 2012;39(4):152-8., 2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.).
In this study, the nutritional assessment methods that were correlation were MUAC and TSF, TSF and MAMC, and TSF and MUAMA. This finding is not clinically relevant, however, given that the amplitude of these measurements is very high, thus demonstrating ample variation between the results of each method.
The results of patients’ nutritional status based on their BMI reflect the current nutritional status of the Brazilian population. An increase in the prevalence of overweight has been observed as a consequence of unfavorable changes in the dietary and physical activity patterns of the population (an increase in the consumption of processed foods and a reduction in occupational energy expenditure)(2929. Schmidt MI, Duncan BB, Silva GA, Menezes AN, Monteiro CA, Barreto SM, Chor D, Menezes PR. Chronic non-communicable diseases in Brazil: burden and current challenges. Lancet. 2011;9;61-74.).
According to the HGS and the RFH-GA indicators, however, more than half of our study population was at risk for malnutrition - 60.6% and 53.2%, respectively. Ismail et al.(2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.)studied patients with hepatitis C of all disease stages (control group, chronic hepatitis C, well-compensated cirrhosis and decompensated cirrhosis), and found a significant risk of malnutrition in the chronic hepatitis C group (14%), similar to what we found in this study (16%). The results of Ismail et al.(2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.) were unexpected, since the nutritional status of patients with chronic infection without liver complications is expected to closely match that of the control group. Our study, however, is limited in not having a control group for further statistical comparisons.
However, the high prevalence of patients at risk for malnutrition according to the RFH-GA is justified by the also high percentage of patients with inadequate energy intake, as assessed by the 24-hour recall (52.1%). The RFH-GA takes dietary intake as well as BMI and MUAC into account, and therefore a statistically significant association was found between this method and energy and protein intakes.
HGS has been shown to be a good alternative in assessing protein depletion by being a superior indicator in detecting cirrhotic patients with malnutrition(22. Álvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21(2):113-7., 55. Bragança ACC, Álvares-da-Silva MR. Prevalence of diabetes mellitus and impaired glucose tolerance in patients with decompensated cirrhosis being evaluated for liver transplantation: the utility of oral glucose tolerance test. Arq Gastroenterol. 2010;47(1):22-7., 1313. Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4.). Álvares-da-Silva et al.(11. Álvares-da-Silva MR, Gottschall CBA, Waechter FL, Hadlich E, Sampaio JA, Francesconi CFM. The use of early enteral feeding post orthotopic liver transplantation in adults. Arq Gastroenterol. 2004;41(3):147-9.)found 100% of malnutrition in pre-liver transplant patients. Gottschall et al.(1313. Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4.)reported that 79.4% of patients with cirrhosis had malnutrition according to HGS, and had inadequate energy and protein intakes, which can affect HGS values. In other clinical conditions, such as Chron’s disease, as assessed by Bin et al.(44. Bin CM, Flores C, Álvares-da-Silva MR, Francesconi CFM. Comparison between handgrip strength, subjective global assessment, anthropometry, and biochemical markers in assessing nutritional status of patients with crohn’s disease in clinical remission. Dig Dis Sci. 2010;55:137-44.), HGS was found to be more sensitive in detecting malnutrition, thus indicating that it can identify changes affecting patients’ nutritional status at an early stage. Peng et al.(2424. Peng S, Plank LD, McCall,JL, Gillanders LK, McIlroy K, Gane E. Body composition, musclefunction, and energy expenditure in patients with liver cirrhosis: a comprehensive study. Am J Clin Nutr. 2007;85:1257-66.) reported that protein depletion, as measured by neutron activation analysis, affects HGS significantly. In the present study, HGS tended to be associated with both energy and protein intakes. This association, however, needs to be tested in a larger patient sample.
Energy and protein intakes were adequate in 52.1% and 46.8% of our sample, respectively, when compared to recommendations for liver disease(2525. Plauth M, Merli M, Kondrup J, Weimann A, Ferenci P, Müller MJ. Espen guidelines for nutrition in liver diseases and transplantation. Clinical Nutrition. 1997;16:43-55.). Roongpisuthipong et al.(2727. Roongpisuthipong C, Sobhonlidsuk A, Nantiruj K, Songchitsomboon S. Nutritional assessment in various stages of liver cirrhosis. Nutrition. 2001;17(9):761-5.)assessed patients with cirrhosis and also reported lower that recommended energy and protein intakes, as well as similar findings for malnutrition based on TSF and BMI values. Ferreira et al.(1010. Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Desnutrição e inadequação alimentar de pacientes aguardando transplante hepático. Rev Assoc Med Brás. 2009;55(4):389-93.) found that 90.7% and 75.7% of patients awaiting a liver transplant had inadequate energy and low protein intakes, respectively. Given that these patients have more advanced liver disease, the prevalence of malnutrition and inadequate dietary intake are expected to be higher.
Insufficient intakes of calcium, potassium, zinc and vitamin C were similar to those reported by Gottschall et al.(1313. Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4.), which were commonly due to unnecessary dietary restrictions and to the low palatability caused by low zinc and restricted salt intakes in these patients’ diets(1313. Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4.).
These findings related to inadequacies in dietary intake become significant given the changes in taste and appetite produced by medications for the treatment of hepatitis C(2323. Palowtsky JM. Treatment failure and resistance with direct-acting antiviral drugs against hepatitis C virus. Hepatology. 2011;53(5):1742-51.). Some of these, such as protease inhibitors, must even be administered after meals three times a day, in order to ensure its absorption and adequate serum levels(2323. Palowtsky JM. Treatment failure and resistance with direct-acting antiviral drugs against hepatitis C virus. Hepatology. 2011;53(5):1742-51.). In this study, however, there was no significant association between energy and protein intake and antiviral treatment use.
The low energy and protein intakes found in the present study may explain the prevalence of malnutrition detected by the different methods of nutritional assessment. Although this study did not investigate the cause of reductions in dietary intake, one hypothesis is that it may be due to recommendations by health professionals for patients to restrict certain foods(1010. Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Desnutrição e inadequação alimentar de pacientes aguardando transplante hepático. Rev Assoc Med Brás. 2009;55(4):389-93., 2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.) or even dietary taboos associated with liver diseases. Ismail et al.(2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.) reported that most patients restricted protein and fat in their diet, not because of their own or their family’s beliefs, but because of professional advice. This could be the reason for the 14% prevalence of moderate malnutrition in patients with chronic hepatitis C found in their study. This study, similarly to Ferreira et al.(1010. Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Desnutrição e inadequação alimentar de pacientes aguardando transplante hepático. Rev Assoc Med Brás. 2009;55(4):389-93.), reported that patients are poorly advised to restrict certain foods, especially protein sources, which are still commonly considered as foods to avoid. The authors(2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.) conclude that, just as liver disease progresses from chronic hepatitis C to uncompensated cirrhosis, patients’ nutritional status similarly evolves from “A” (well-nourished”) to “C” (severe malnutrition).
It is worth highlighting that the 24-hour recall method, which was used in this study to assess patients’ dietary intake, has the limitation of having been applied only once. Thus, patients’ dietary intake assessment may have occurred on an atypical day, which does not reflect their usual daily intake.
The fact that patients assessed in this study who have not yet developed complications associated with the hepatitis C virus are already at risk of malnutrition and inadequate dietary intake is of particular concern, since it is well recognized that nutrient deficiencies have a direct impact on the clinical history of patients with liver disease(77. Carvalho L, Parise ER. Evaluation of nutritional status of nonhospitalized patients with liver cirrhosis. Arq Gastroenterol. 2006;43(4):269-74., 1010. Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Desnutrição e inadequação alimentar de pacientes aguardando transplante hepático. Rev Assoc Med Brás. 2009;55(4):389-93., 1313. Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4., 2020. Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42., 2727. Roongpisuthipong C, Sobhonlidsuk A, Nantiruj K, Songchitsomboon S. Nutritional assessment in various stages of liver cirrhosis. Nutrition. 2001;17(9):761-5.). This shows the importance of diagnosing and treating malnutrition caused by chronic liver disease before the onset of complications such as cirrhosis and hepatocellular carcinoma.
Malnutrition was prevalent among chronic hepatitis C patients assessed in this study, but there was no agreement among the different methods of nutritional status assessment. Insufficient energy and protein intakes were highly prevalent, demonstrating that these patients are at risk for malnutrition even before they develop the complications of liver disease such as cirrhosis.
Assessing their nutritional status and dietary intake patterns may substantiate nutrition education strategies as preventive measures in the development of malnutrition in patients with liver disease.
Authors’ contributions
Gottschall CBA has designed the study, data collection, survey execution, analyzed and interpreted the data, writing of text and reviewed it critically for the intellectual quality of the study. Pereira TG has designed the study, data collection, survey execution, analyzed and interpreted the data, writing of text. Rabito EI has interpreted the data and reviewed the text. Álvares-da-Silva MR has designed the study, interpreted the data and reviewed it critically for the intellectual quality of the study.
REFERENCES
-
1Álvares-da-Silva MR, Gottschall CBA, Waechter FL, Hadlich E, Sampaio JA, Francesconi CFM. The use of early enteral feeding post orthotopic liver transplantation in adults. Arq Gastroenterol. 2004;41(3):147-9.
-
2Álvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21(2):113-7.
-
3Associação Médica Brasileira e Conselho Federal de Medicina. Hepatite C crônica: tratamento. Projeto Diretrizes, 2009.
-
4Bin CM, Flores C, Álvares-da-Silva MR, Francesconi CFM. Comparison between handgrip strength, subjective global assessment, anthropometry, and biochemical markers in assessing nutritional status of patients with crohn’s disease in clinical remission. Dig Dis Sci. 2010;55:137-44.
-
5Bragança ACC, Álvares-da-Silva MR. Prevalence of diabetes mellitus and impaired glucose tolerance in patients with decompensated cirrhosis being evaluated for liver transplantation: the utility of oral glucose tolerance test. Arq Gastroenterol. 2010;47(1):22-7.
-
6Canadian guidelines for Health Care Providers. Hepatitis C: Nutrition Care. Dietitians of Canada, 2003.
-
7Carvalho L, Parise ER. Evaluation of nutritional status of nonhospitalized patients with liver cirrhosis. Arq Gastroenterol. 2006;43(4):269-74.
-
8Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, Jeejeebhoy KN. What is Subject Global Assessment of Nutritional Status? JPEN. 1987;11:8-13.
-
9Duarte ACG. Avaliação nutricional: aspectos clínicos e laboratoriais. São Paulo: Atheneu, 2007.
-
10Ferreira LG, Anastácio LR, Lima AS, Correia MITD. Desnutrição e inadequação alimentar de pacientes aguardando transplante hepático. Rev Assoc Med Brás. 2009;55(4):389-93.
-
11Frisancho AR. Anthropometric standards for the assessment of growth and nutrition status. The University of Michigan Press: Ann Arbor, 1990.
-
12Gottschall CBA, Nunes FF, Aydos MED, Bragança AC, Felix DR, Rabito EI, Álvares-da-Silva MR. Contribution of dynamometry and the royal free hospital global assessment to the nutritional assessment of patients with chronic liver diseases. Rev Chil Nutr. 2012;39(4):152-8.
-
13Gottschall, CBA, Álvares-da-Silva MR, Camargo ACR, Burtett RM, Silveira TR. Nutritional assessment in patients with cirrhosis: the use of indirect calorimetry. Arq Gastroenterol. 2004;41(4):220-4.
-
14Heyward VH, Stolarczyk LM. Avaliação da composição corporal aplicada. Barueri: Manole, 2000.
-
15Institute of Medicine (IOM). Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, D.C.: National Academy Press, 1997a, 454p.
-
16Institute of Medicine (IOM). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, D.C.: National Academy Press, 2005a, 1357p.
-
17Institute of Medicine (IOM). Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc. Washington, D.C.: National Academy Press, 2001a, 773p.
-
18Institute of Medicine (IOM). Dietary reference intakes for vitamin C, vitamin E, selenium and carotenoids. Washington, D.C.: National Academy Press, 2000a, 506p.
-
19Institute of Medicine (IOM). Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, D.C.: National Academy Press, 2004a, 638p.
-
20Ismail FW, Khan RA, Kamani L, Wadalawala AA, Shah HA, Hamid SS, Jafri W. Nutritional status in patients with hepatitis C. J Coll Physicians Surg Pak. 2012;22(3):139-42.
-
21Lameu EB, Gerude MF, Corrêa RC, Lima KA. Adductor policis muscle: a new anthropometric parameter. Rev Hosp Clín Fac Med. 2004;59(2):57-62.
-
22Morgan MY, Madden AM, Soulsby CT, Morris RW. Derivation and validation of a new global method for assessing nutritional status in patients with cirrhosis. Hepatology. 2006;44(4):823-5.
-
23Palowtsky JM. Treatment failure and resistance with direct-acting antiviral drugs against hepatitis C virus. Hepatology. 2011;53(5):1742-51.
-
24Peng S, Plank LD, McCall,JL, Gillanders LK, McIlroy K, Gane E. Body composition, musclefunction, and energy expenditure in patients with liver cirrhosis: a comprehensive study. Am J Clin Nutr. 2007;85:1257-66.
-
25Plauth M, Merli M, Kondrup J, Weimann A, Ferenci P, Müller MJ. Espen guidelines for nutrition in liver diseases and transplantation. Clinical Nutrition. 1997;16:43-55.
-
26Ritter L, Gazzola J. Nutritional evaluation of the cirrhotic patient: an objective, subjective or multicompartmental approach? Arq Gastroenterol. 2006;43(1):66-70.
-
27Roongpisuthipong C, Sobhonlidsuk A, Nantiruj K, Songchitsomboon S. Nutritional assessment in various stages of liver cirrhosis. Nutrition. 2001;17(9):761-5.
-
28Schlüssel MM, Dos Anjos LA, Vasconcellos MTL, Kac G. Reference values of handgrip dynamometry of health adults: a population-based study. Clinical Nutrition 2008;27:601-7.
-
29Schmidt MI, Duncan BB, Silva GA, Menezes AN, Monteiro CA, Barreto SM, Chor D, Menezes PR. Chronic non-communicable diseases in Brazil: burden and current challenges. Lancet. 2011;9;61-74.
-
30Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis. 2005;5:558–67.
-
31Sociedade Brasileira de Hepatologia. Epidemiologia da infecção pelo vírus da hepatite C no Brasil. Available from: http://www.fmt.am.gov.br/trabalhos/anais/virologia/infec_brasil.htm
» http://www.fmt.am.gov.br/trabalhos/anais/virologia/infec_brasil.htm -
32World Health Organization, Geneva. Weekly Epidemiological Record. 1997;46:341-8.
-
Disclosure of funding: no funding received.
Publication Dates
-
Publication in this collection
Jul-Sep 2015
History
-
Received
24 Mar 2015 -
Accepted
15 May 2015