Abstracts
The purpose of this paper, which was conducted on 175 children with hemiparetic cerebral palsy (H-CP), was to verify the etiological risk period for this disease. Etiological risk factors (ERF) were detected through anamnesis: 23% in the prenatal period, 18% in the perinatal period and 59% of the patients the period was undefined (ERF in the prenatal and perinatal period was 41% and no ERF was 18% of the cases. The computerized tomographic scan (CT) and MRI were performed on all the patients, who were then classified according to their etiopathogenic data: CT1= normal (18%); CT 2= unilateral ventricular enlargement (25%); CT 3= cortical/ subcortical cavities (28%); CT4= hemispheric atrophy and other findings (14%); CT 5= malformations (15%). CT 5 was associated with physical malformations beyond the central nervous system and with prenatal ERF's , while CT 2 was associated with the perinatal ERF's, mainly in premature births. Magnetic resonance imaging was performed on 57 patients and demonstrated a good degree of concordance with the CT. Etiology remained undefined in only 37% of the cases after neuroimaging was related to ERF. A high perinatal RF frequency (59%) was observed and emphasized the need for special care during this period.
cerebral palsy; hemiparetic cerebral palsy; etiology; etiological risk factors; computerized tomography; magnetic resonance imaging; children
Foram estudadas 175 crianças com paralisia cerebral hemiparética (PC-H) para elucidar o período de risco etiológico. Através da anamnese constataram-se fatores de risco para etiologia (FRE) pré-natal em 23%, perinatal em18% e período indefinido em 59% dos pacientes (com FRE pré e perinatal 41% e sem FRE 18%). A tomografia computadorizada (TC) foi realizada em todos os sujeitos e classificada de acordo com dados etiopatogênicos em: TC1= normal (18%); TC2= alargamento ventricular unilateral (25%); TC3= cavidades córtico-subcorticais (28%); TC4= atrofia hemisférica e outros achados (14%); TC5= malformações (15%). A TC5 se associada a malformações físicas fora do sistema nervoso central e aos FRE pré-natais e a TC2 aos perinatais, principalmente, nascer prematuro. A ressonância magnética foi realizada em 57 sujeitos demonstrando boa concordância com a TC. Após associação da neuroimagem e FRE a etiologia ficou indefinida em apenas 37%. Constatou-se alta frequência de FRE perinatais (59%), alertando para melhores cuidados neste período.
paralisia cerebral; paralisia cerebral hemiparética; etiologia; fatores de risco; tomografia axial computadorizada; ressonância magnética; crianças
HEMIPARETIC CEREBRAL PALSY
Etiological risk factors and neuroimaging
Ana Maria Sedrez Gonzaga Piovesana1 1 Pediatric Neurology Division, Department of Neurology, Faculty of Medical Sciences (FCM), State University of Campinas (UNICAMP), Campinas, Brazil: MD, PhD, Assistant Professor; 2 MD, PhD, Adjunct Professor; 3 MD, PhD, Assistant Professor, Departmento of Radiology FCM-UNICAMP. , Maria Valeriana Leme de Moura-Ribeiro2 1 Pediatric Neurology Division, Department of Neurology, Faculty of Medical Sciences (FCM), State University of Campinas (UNICAMP), Campinas, Brazil: MD, PhD, Assistant Professor; 2 MD, PhD, Adjunct Professor; 3 MD, PhD, Assistant Professor, Departmento of Radiology FCM-UNICAMP. , Verônica de Araújo Zanardi3 1 Pediatric Neurology Division, Department of Neurology, Faculty of Medical Sciences (FCM), State University of Campinas (UNICAMP), Campinas, Brazil: MD, PhD, Assistant Professor; 2 MD, PhD, Adjunct Professor; 3 MD, PhD, Assistant Professor, Departmento of Radiology FCM-UNICAMP. ,Vanda Maria Gimenes Gonçalves1 1 Pediatric Neurology Division, Department of Neurology, Faculty of Medical Sciences (FCM), State University of Campinas (UNICAMP), Campinas, Brazil: MD, PhD, Assistant Professor; 2 MD, PhD, Adjunct Professor; 3 MD, PhD, Assistant Professor, Departmento of Radiology FCM-UNICAMP.
ABSTRACT - The purpose of this paper, which was conducted on 175 children with hemiparetic cerebral palsy (H-CP), was to verify the etiological risk period for this disease. Etiological risk factors (ERF) were detected through anamnesis: 23% in the prenatal period, 18% in the perinatal period and 59% of the patients the period was undefined (ERF in the prenatal and perinatal period was 41% and no ERF was 18% of the cases. The computerized tomographic scan (CT) and MRI were performed on all the patients, who were then classified according to their etiopathogenic data: CT1= normal (18%); CT 2= unilateral ventricular enlargement (25%); CT 3= cortical/ subcortical cavities (28%); CT4= hemispheric atrophy and other findings (14%); CT 5= malformations (15%). CT 5 was associated with physical malformations beyond the central nervous system and with prenatal ERF's , while CT 2 was associated with the perinatal ERF's, mainly in premature births. Magnetic resonance imaging was performed on 57 patients and demonstrated a good degree of concordance with the CT. Etiology remained undefined in only 37% of the cases after neuroimaging was related to ERF. A high perinatal RF frequency (59%) was observed and emphasized the need for special care during this period.
KEY WORDS: cerebral palsy, hemiparetic cerebral palsy, etiology, etiological risk factors, computerized tomography, magnetic resonance imaging, children.
Paralisia cerebral hemiparética: fatores de risco etiológico e neuroimagem
RESUMO - Foram estudadas 175 crianças com paralisia cerebral hemiparética (PC-H) para elucidar o período de risco etiológico. Através da anamnese constataram-se fatores de risco para etiologia (FRE) pré-natal em 23%, perinatal em18% e período indefinido em 59% dos pacientes (com FRE pré e perinatal 41% e sem FRE 18%). A tomografia computadorizada (TC) foi realizada em todos os sujeitos e classificada de acordo com dados etiopatogênicos em: TC1= normal (18%); TC2= alargamento ventricular unilateral (25%); TC3= cavidades córtico-subcorticais (28%); TC4= atrofia hemisférica e outros achados (14%); TC5= malformações (15%). A TC5 se associada a malformações físicas fora do sistema nervoso central e aos FRE pré-natais e a TC2 aos perinatais, principalmente, nascer prematuro. A ressonância magnética foi realizada em 57 sujeitos demonstrando boa concordância com a TC. Após associação da neuroimagem e FRE a etiologia ficou indefinida em apenas 37%. Constatou-se alta frequência de FRE perinatais (59%), alertando para melhores cuidados neste período.
PALAVRAS-CHAVE: paralisia cerebral, paralisia cerebral hemiparética, etiologia, fatores de risco, tomografia axial computadorizada, ressonância magnética, crianças
Despite the recent improvement in maternal infantile health care, cerebral palsy (CP) and its mechanisms are still not fully understood. The incidence of this disease, in its moderate and serious forms is around 2.5:1000 live births1. CP is defined as a non progressive motor disorder which is secondary to a lesion of an immature brain and includes abnormalities in tonus, posture and movement that is frequently modified 2. Hemiparetic cerebral palsy (CP-H) is defined as CP with a unilateral motor disorder 3.
Recent studies have indicated that prenatal etiologies contribute to C P 4,5. Injury resulting from ischemic-hypoxic mechanisms constitutes a serious prenatal cause and the consequences mainly depend on the moment at which the aggression occurs, although individual genetic factors are also believed to contribute 6,7. Nowadays, the brain computerized tomography (CT) and magnetic resonance imaging (MRI) makes it is possible to detect, in many cases, the etiopathogeny as well as the developmental stage of the central nervous system (CNS) during which the aggression has occurred 1,8.
Hagberg et al. 9, studied the etiological aspects of CP and defined prenatal etiology in 22% of the cases, probable perinatal etiology in 40% and undefined etiology in 38% of the cases. The etiologies considered as prenatal were: CNS malformations (CNS-MF); periventricular leukomalacia (PVL) in full term newborn infants without perinatal risk factors; prenatal intracranian hemorrhage confirmed by ultrasound; congenital physical malformations outside the CNS; low birth weight (LBW).
With regard to perinatal etiologies, most researchers agree that premature infants differ from full term infants (FTI) because of the high incidence of CP in premature infants and the characteristics of the lesions8-10. The premature infants present unstable cardiac and respiratory regularity which lead to cerebral hypoperfusion and consequently PVL or periventricular hemorrhagic infarct, both of which are commonly found in CP-H 11-15. Hypodense areas are common in FTI, mainly in the watershed areas, and probably represent areas of perfusional failure15-18. In cases of CP-H which occur in full term infants, the most common finding is a lesion in the area of the middle cerebral artery - mainly the left one and this factor is not described for the other types of CP 6,15,17,19. Ischemic lesion in the parasagital white matter is generally related to hypoxic ischemic encephalopathy (HIE) or prolonged hypoxy which results in subcortical leukomalacia with a reduction in the white mater and ex-vacuum ventricular enlargement resulting in hemispheric atrophy 7.
A study on the clinical condition and etiology of CP-H has been conducted, since 1984, at the Clinical Hospital, Faculty of Medical Sciences, UNICAMP, to clarify the pathophysiology of the lesions as well as the prognosis for the disease 20,21.
The objective in this study was to identify the etiological risk factors (ERF) for CP-H and the period during which the aggression occurred.
METHOD
We studied 175 patients diagnosed with CP-H, seen at the CP ambulatory from 1984 to 1999. All the patients who filled in the research protocol had undergone CT scan and were more than 24 months old at the follow up visit.
The ERF's of CP cited by Kuban & Leviton1 and Hagberg et al.9 as well as those considered relevant in Piovesana20 were used to define the obvious or probable period of the lesion. The following indicators were included:
Maternal and genetic background - Maternal history of previous abortions and /or natimortality, long and irregular menstrual cycles. The indicators added on were: family history of consanguinity, CP, retarded development or CNS-MF in close relatives.
During pregnancy - Physical malformation unrelated to the CNS (cardiac, gastrointestinal, dimorphism, single crease only in hemiparetic hand, congenital deafness); LBW; multiple gestation; abnormal fetus; chronic maternal disease; imminent abortion ; hemorrhages during pregnancy and abortive attempts.
During the perinatal period - Born prematurely; chorionitis or amnionitis; previous detachment of the placenta; serious asphyxia (Apgar <7 at the 5th minute); neonatal convulsions; intracranial hemorrhage; metabolic disturbances; hypotension; persistent respiratory distress; mechanical ventilation; necrotizing enterocolitis; polycythemia; infection.
After checking these ERF's, patients were classified in 3 groups according to the period of injury: prenatal, perinatal and unknown (with or without ERF).
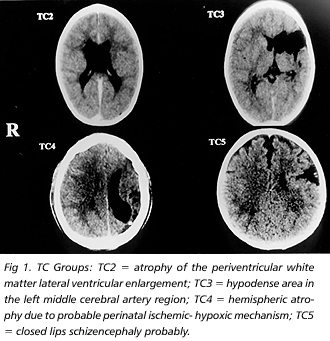
The CT was divided into 5 subgroups according to Wiklund et al.: CT 1= normal; CT 2= unilateral ventricular enlargement; CT 3= cortical /subcortical cavities; CT 4= hemispheric atrophy and other findings; CT 5= CNS-MF (Fig 1).
MRI findings of 57 children was classified according to Okumura et al; 15, and adapted by Piovesana21: MR1= normal; MR2a= PVL; MR2b= periventricular post-hemorrhagic porencephaly with or without PVL (these two subtypes are generally associated to lesions before the 35th gestational week and correspond to CT2); MR 3= cortical/subcortical hypodense lesions related to vascular accidents; MR4= hemispheric atrophies and other findings; MR5= CNS-MF (Fig 2). MRI was compared with CT using Kappa coefficient 22.
Two different approaches were used: 1)only clinical criteria -ERF; 2) clinical criteria associated to neuroimaging, or rather, the clinical data associated to the CT aspect to define the moment at which the lesion occurred.
Statistical methodology - The Chi-squared test or the Fisher test was used, whenever necessary 22,23. The Kappa coefficient 22 was used to compare the CT and MRI exams, values greater or equal to 0.75 were considered as having excellent concordance. The polytomic logistic regression analysis - generalized model of logs22, 23 was used to detect the ERF associated with the CT result.
RESULTS
Eighty nine patients had right sided CP-H, and 86 left sided CP-H, 95 were boys (54%). The CT showed the following patient distribution: CT1= 31 (18%); CT2= 44 (25%); CT3= 49% (28%); CT4= 25 (14%); CT5= 26 (15%).
The relationship between the presence and absence of ERF during the prenatal period (before and during pregnancy), during the perinatal period and the CT groups demonstrated relevant association like: CNS-MF (p=0.014), perinatal respiratory disorders (p= 0.021) and born prematurely (p= 0.000). HIE demonstrated an associative tendency (p= 0.076). These data are presented in Table 1.
A good concordance level of 0.849 between CT and MRI based on the Kappa test permitted the CT to be used as a reference in this study. The distribution in the case of MRI was the following: MR1= 4 (7%), MR2a= 17 (30%), MR2b= 7 (12%), MR3= 17 (30%), MR4= 5 (9%), MR5= 7 (12%) (Table 2).
Multivariate polytomic logistic regression analysis of ERF and CT demonstrated that the presence of physical malformations beyond the CNS had a greater probability of being found in the CT5 group and the presence of children born prematurely had a greater probability in the CT2 group.
When the polytomic logistic regression, proportional odds model, was utilized for comparison, it was observed that the greater the number of ERF during gestation, the greater possibility of defining the CT5 group in relation to the CT1 group and greater the number of perinatal ERF' s, the greater the possibility of being found in the CT2 and CT1 groups than in the CT5 group. The CT3 and CT4 groups were not associated with the ERF of a specific period.
After obtaining the ERF, each case was classified according to its risk period. There were 40 patients (23%) in the prenatal period and 31 patients in the perinatal period (18%) and there were 73 patients (41%) during both periods. ERF were not reported in 31 cases (18%). These data were associated with various CT aspects (p= 0.0011) (Table 3).
After neuroimaging assessment and a study of the ERF, the etiology of 29 cases (15.5%) was considered prenatal and 26 of these children had CNS-MF, 2 children had PVL, but were full term births without perinatal ERF and one child was diagnosed by ultrasound as having had a periventricular hemorrhagic lesion during gestation. Two of the CNS-MF cases were born prematurely and 5 cases were reported as perinatal.
The etiology was defined as perinatal in 43 cases (24.5%) based on the CT aspect and clinical data. It was not possible to establish the moment at which the lesion occurred in the other cases because the image did not support the clinical data. Therefore, the probable period was maintained for those cases that presented prenatal ERF = 24 (14%) and 14 cases (8%) as perinatal. It was observed that in 43 children ( 24.5%) the period of aggression was not determined, but they had prenatal and perinatal ERF. These data are presented in Table 4.
DISCUSSION
Recently CP has been the subject of several reports in the literature showing that many aspects of this entity still need to be studied.
When Hagberg et al.9 presented their epidemiologic data on the incidence and etiology of CP, they pointed out that the studies which they had conducted during previous decades24 were based on conventional or clinical ERF and only indicated the possible cause of CP, whereas present studies, based on neuroimaging findings, provide objective information, elucidating and classifying more clearly the etiology of CP.
We fully agree with this author because retrospective diagnosis of etiology can be conducted based on clinical and neuroimaging data. In this study, when only ERF were evaluated without any additional information obtained through neuroimaging, it was observed that it wasn't possible to define the period during which the lesion occurred in 59% of the cases. After the neuroimaging evaluation, only 37% of the cases remained undefined. The data obtained in this study is in keeping with of Hagberg et al. 9, that did not define the etiological risk in 38% of the CP cases born between 1987 and 1990.
Over the last few decades, prenatal etiology has been confirmed based on neuropathological studies 25 and more recently using MRI 6,12,15,16. Studies conducted by Wiklund et al.17showed that 17% of the CP-H cases had CNS-MF. Some reports give great importance to the presence of physical malformations outside the CNS because they indicate the occurrence of a lesion and therefore the period can be defined 1,3,4,11.
In this study, we determined prenatal etiology in 29 children, 26 of these children had CNS-MF, two of the full term births children who were with no perinatal ERF had PVL, and one child had post-hemorrhagic porencephaly diagnosed during pregnancy by ultrasound. Perinatal etiology was defined in 43 patients (24.5%). Of the 21 full term births, 14 children presented hypodense lesions with septates, common to astrocytic reactions of a mature CNS that has suffered a perinatal lesion. Seven children presented hemispheric atrophy compatible with subcortical leukomalacia .The predominant finding among the 22 children who were born prematurely was PVL, which was confirmed through MRI in 17 children and with perinatal cerebral ultrasound in the rest of the cases.
In 1997, Okumura et al.8 studied MRI in children who had CP and related the findings to the gestational age at birth and the type of CP. They found that the relationship was significant and that about 2/3 of the patients with CP-H had unilateral lesions and infarct of the middle cerebral artery, as well as hemiatrophy resulting from leukomalacia . These findings were more common in this group than in the other groups. Children, who were born prematurely, generally presented periventricular enlargement and /or PVL. These data are similar to those in some specific studies and confirm our data which associate the CT2 group with born prematurely.
Over the last three decades, reports on neuropathological findings related to CP have singled out PVL as the main cause26. Niemann et al.12 studied 41 cases of congenital CP-H using MRI and the main finding was PVL in 56% of the cases with a predominance among pre-term births, but as the purpose of their study was to diagnose periventricular lesions they excluded cases of destructive cerebral lesion and hydrocephaly. The authors also reached the conclusion that there was a possibility that a great majority of the cases that present a normal CT presented periventricular lesion in the MRI findings, weighted images in T2, and that this kind of lesion results from an ischemic process that occurs between the 28th and 35th week of gestation.
Our findings are very similar to those of Niemann et al. Six of the 10 children who presented normal CT and underwent MRI, presented small PVL areas. MRI findings, also showed a high incidence of PVL either in isolation or in association with periventricular hemorrhagic porencephaly (42%), which contributed towards the detection of the period of aggression.
With regard to the presence of EFR and the gestational age at birth, only perinatal ERF were observed in 63% of premature births and 18 % of full term births. The verified etiology and/or the ERF during the prenatal period were present in 36% of full term births and 12% of pre-term births. These data are in concordance with those of Hagberg et al.9 regarding the predominance of perinatal etiology in pre-term births (54%) in comparison with full term births (28%). Prenatal etiology was more common in full term births (33%) than in pre-term births (8%).
Although great progress has been achieved in relation to imaging in CP-H, 8% to 24% of the exams are reported as normal15,17,21. In the present study, the CT exam was normal in 18% of the cases and the MRI in 7% of the cases, demonstrating that MRI is a more efficient tool in the neroimaging evaluation of PC-H.
CONCLUSION
The occurrence of prenatal injury is associated with the tomographic aspect of CNS-MF, while premature births and perinatal FR show a relationship with groups CT2 and CT1. Neuroimaging helps to confirm period of CNS injury in 41% of the children with CP-H, with a 22% probable risk period diagnosis . The frequency of perinatal etiology was observed to be greater among premature births and there was a greater frequency of prenatal etiology among full term births. The occurrence of destructive lesions in the subcortical and parasagittal regions in full term births demonstrates the importance of perinatal ERF suggesting the need for better care during this period. Conversely, the fact that CT3 and CT4 groups did not show relationship with any defined risk period may indicate that destructive lesions in full term births mainly occur when ERF are present during both periods, which confirms a predisposition to the occurrence of lesions.
Acknowledgements - The Commission for Research & Statistics, FCM/UNICAMP; the CP-H children and their parents, who participated in the study; colleagues and medical residents, who made data collection possible during all these years.
Received 18 July 2000, received in final form 18 September 2000. Accepted 21 September 2000.
Dr. Ana Maria Sedrez Gonzaga Piovesana - Department of Neurology FCM-UNICAMP - P.O. Box 6111 - 13083-970 Campinas SP - Brasil. Fax 19 788 7810. E-mail: piovesan@fcm.unicamp.br
- 1. Kuban KCK, Leviton A. Cerebral palsy. N Engl J Med 1994; 330: 188 -195.
- 2. Griffiths M, Clegg M. Cerebral palsy: problems and practice, London: Souvenir Press, 1988.
- 3. Uvebrant P. Hemiplegic cerebral palsy: aetiology and outcome. Acta Paediatr Scand 1988;Suppl 345:1-100.
- 4. Nelson KB, Ellenberg JH. Antecedents of cerebral palsy: multivariate analysis of risk. N Engl J Med 1986;315:81-86.
- 5. Blair E, Stanley FJ. Intrapartum asphyxia: a rare cause of cerebral palsy. J Pediatr 1988;112:515-519.
- 6. Barkovich AJ. Destructive Brain disorders of childhood. In Barkovich AJ. Pediatric neuroimaging. 2.Ed. New York: Raven Press, 1995L 107-175.
- 7. Barkovich AJ. Congenital malformations of the brain. In Barkovich AJ. Pediatric neuroimaging. 2.Ed. New York: Raven Press, 1995: 176-275.
- 8. Okumura A, Hayakawa F, Katu T, Kuno K, Watanabe K. MRI findings in patients with spastic cerebral palsy: I. Correlation with gestational age at birth. Dev Med Child Neurol 1997a;39: 363-368.
- 9. Hagberg B, Hagberg G, Olow I, Von Wendt L. The changing panorama of cerebral palsy in Sweden: VII. Prevalence and origin in the birth year period 1987-90. Acta Paediatr Scand 1996;85:954-960.
- 10. Leviton A, Paneth N. White matter damage in preterms newbornsL an epidemiological perspective. Early Hum Dev 1990;24:1-22.
- 11. Wiklund LM, Uvebrant P. Hemiplegic cerebral palsy: correlation between CT morphologic and clinical findings. Dev Med Child Neurol 1991;33:512-523.
- 12. Niemann G, Wakat JP, Krägeloh-Mann I, Grodd W, Michaelis R. Congenital hemiparesis and perventricular leukomalacia: [athogenic aspects on magnetic resonance imaging. Dev Med Child Neurol 1994;36:943-950
- 13. Rogers B, Msall M, Owens T, et al. Cystic periventricular leukomalacia and type of cerebral palsy in preterm infants. J Pediatr 1994;125:S1-S8.
- 14. Volpe JJ. Intracranial hemorrhage: intraventricular hemorrhage of the premature infant. In Volpe JJ. Neurology of the newborn. 3.Ed. Philadelphia: Saunders, 1995; 403-463.
- 15. Okumura A, Hayakawa F, Katu T, Kuno K, Watanabe K. MRI findings in patients with spastic cerebral palsy: II. Correlation with type of cerebral palsy. Dev Med Child Neurol 1997;39:369 -372.
- 16. Bouza H, Dubowitz LMZ, Rutherford M, Cowan F, Pennock JM. Late magnetic resonance imaging and clinical finding in neonates with unilateral lesions on cranial ultrasound. Dev Med Child Neurol 1994;36:951-954.
- 17. Wiklund LM, Uvebrant U, Flodmark O. Morphology of cerebral lesions in children with congenital hemiplegia: a study with computed tomography. Neuroradiology 1990;32:179-186.
- 18. Moura-Ribeiro MVL, Ciasca SM, Vale-Cavalcanti M, Etchebehere ECSC, Camargo EE. Cerebrovascular disease in newborn infants: report of three cases with clinical follow-up and brain SPECT cerebral. Arq Neuropsquiatr 1999;57:1005-1010.
- 19. Molteni B, Oleari G, Fedrizzi E, Bracchi M. Relation between CT patterns, clinical findings and etiological factors in children born at term, affected congenital hemiparesis. Neropediatrics 1987;18:75-80.
- 20. Piovesana AMSG. Paralisia cerebral hemiparética: estudo de 42 casos. Dissertaçăo de Mestrado, Faculdade de Cięncias Médicas da Universidade Estadual de Campinas. Campinas, 1993.
- 21. Piovesana AMSG. Paralisia cerebral hemiparética: aspectos evolutivos, plasticidade cerebral e especializaçăo hemisférica. Tese de Doutorado, Faculdade de Cięncias Médicas da Universidade Estadual de Campinas. Campinas, 1999.
- 22. Fleiss JL. Statistical methods for rates and proportions. 2,Ed. New York: John Wiley & Sons, 1981.
- 23. Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. Cary NC: SAS Institute, 1996.
- 24. Hagberg B, Hagberg G, Olow I. The changing panorama of cerebral palsy in Sweden: IV. Epidemiological trends 1959-78. Acta Paediatr Scand 1984;73:433-440.
- 25. Christensen E & Melchior J. Cerebral palsy: a clinical and neuropathological study. Clin Dev Med 25. London: Heinemann, 1967: 55-67.
- 26. Banker BQ, Larroche J-C. Periventricular leukomalacia of infancy: a form of neonatal anoxic encephalopathy. Arch Neurol 1962,7:386-410.
Publication Dates
-
Publication in this collection
06 Apr 2001 -
Date of issue
Mar 2001
History
-
Accepted
21 Sept 2000 -
Reviewed
18 Sept 2000 -
Received
18 July 2000