Introduction
Bilateral middle ear congenital cholesteatoma (CC) is an extremely rare disease.11 Potsic WP, Korman SB, Samadi DS, Wetmore RF. Congenital cholesteatoma: 20 years' experience at The Children's Hospital of Philadelphia. Otolaryngol Head Neck Surg. 2002;128:810-4.
2 Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts and 53 patients. Otolaryngol Clin North Am. 2006;39:1081-94.-33 Koltai PJ, Nelson M, Castellon RJ, Garabedian EN, Triglia JM, Roman S, et al. The natural history of congenital cholesteatoma. Arch Otolaryngol Head Neck Surg. 2002;128:804-9.
Middle ear CC grows from birth behind the intact ear drum, with no symptoms. Usually, it is detected by the pediatrician at the time of a routine visit.11 Potsic WP, Korman SB, Samadi DS, Wetmore RF. Congenital cholesteatoma: 20 years' experience at The Children's Hospital of Philadelphia. Otolaryngol Head Neck Surg. 2002;128:810-4.
2 Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts and 53 patients. Otolaryngol Clin North Am. 2006;39:1081-94.-33 Koltai PJ, Nelson M, Castellon RJ, Garabedian EN, Triglia JM, Roman S, et al. The natural history of congenital cholesteatoma. Arch Otolaryngol Head Neck Surg. 2002;128:804-9. Undetected, it may grow for years until becoming quite large.
Etiology of middle ear CC is still controversial, but it seems that an embryologic origin is the most acceptable.11 Potsic WP, Korman SB, Samadi DS, Wetmore RF. Congenital cholesteatoma: 20 years' experience at The Children's Hospital of Philadelphia. Otolaryngol Head Neck Surg. 2002;128:810-4.
2 Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts and 53 patients. Otolaryngol Clin North Am. 2006;39:1081-94.-33 Koltai PJ, Nelson M, Castellon RJ, Garabedian EN, Triglia JM, Roman S, et al. The natural history of congenital cholesteatoma. Arch Otolaryngol Head Neck Surg. 2002;128:804-9. Progressive hearing loss and soft tissue density mass within the middle ear cavity usually differentiate the CC from other pathologies that include hearing loss and intact tympanic membrane.44 Kim SH, Cho YS, Chu HS, Jang JY, Chung WH, Hong SH. Open-type congenital cholesteatoma: differential diagnosis for conductive hearing loss with a normal tympanic membrane. Acta Otolaryngol. 2012;132:618-23. Treatment of CC requires early surgery and long-term follow-up.55 El-Bitar MA, Choi SS, Emamian SA, Vezina LG. Congenital middle ear cholesteatoma: need for early recognition - role of computed tomography scan. Int J Pediatr Otorhinolaryngol. 2003;67:231-5. Spread and location of CC influences the outcome of surgery.
Recently, two cases of CC spontaneous regression were described.66 Kodama K, Hara M, Hasegawa M, Matsuzawa S, Shinnabe M, Kanazawa H, et al. Two cases of spontaneous regression of congenital cholesteatomas. Int J Pediatr Otorhinolaryngol. 2012;76:142-9.
Case report
A 3-year-old boy was admitted to the hospital during his first episode of right-sided acute otitis media (AOM), accompanied by discrete facial nerve palsy (House-Brackmann Grade II) on the side of the involved ear.
Otomicroscopy showed a red, bulging tympanic membrane on the right side, without perforation. The left tympanic membrane was normal. Myringotomy was performed as a medical urgency, with no preoperative radiologic exam. During myringotomy, a large cholesteatoma was discovered in the middle ear cavity. For a complete surgical removal of the cholesteatoma and facial nerve decompression a canal wall down (CWD) technique was necessary. Facial nerve has improved after six months.
After one year, routine otoscopic follow-up showed a normal postoperative finding on the right ear, but on the left ear, a white pearl in the anterosuperior quadrant, behind the intact tympanic membrane, was detected. Again, there was no history of otitis media or evidence of any trouble with the boy's left ear.
Multidetector computed tomography (MDCT) scan of the temporal bone confirmed that there was no sign of disease recurrence on the right side. On the left side, a mass in the epitympanum suspicious of cholesteatoma was discovered (Figs. 1-4). Surgery confirmed the diagnosis, and cholesteatoma was removed through retroauricular approach, canal wall up technique (CWU).
Coronal MDCT scan of the left temporal bone showing aerated mesotympanum and the soft tissue mass around malleus head and incus body (arrow).
Axial MDCT scan of the left temporal bone at the level of the horizontal portion of the facial nerve (arrow), showing the soft tissue mass in the attic and antrum.
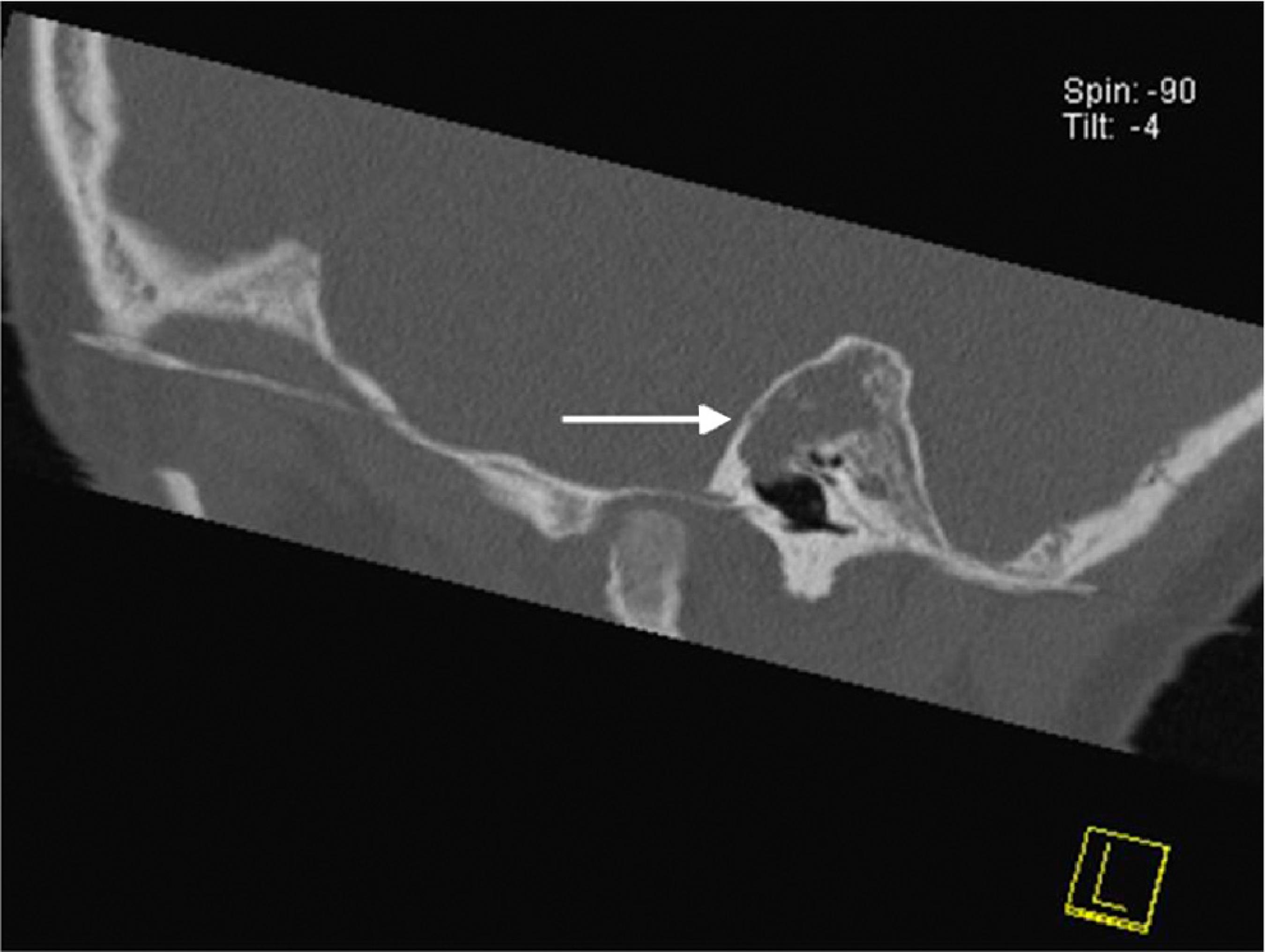
Sagittal MDCT scan of the left temporal bone at the level of malleus handle, showing the soft tissue mass in the attic (arrow).
Sagittal scan of the left temporal bone showing the soft tissue mass in the attic and aerated mesotympanum.
Discussion
Bilateral middle ear CC is a very rare disease. The most common symptom of a conventional cholesteatoma is a purulent ear discharge with a strong odor or bleeding. Most frequent signs of complication include vertigo, tinnitus, sensorineural hearing loss and facial nerve palsy.11 Potsic WP, Korman SB, Samadi DS, Wetmore RF. Congenital cholesteatoma: 20 years' experience at The Children's Hospital of Philadelphia. Otolaryngol Head Neck Surg. 2002;128:810-4.
2 Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts and 53 patients. Otolaryngol Clin North Am. 2006;39:1081-94.-33 Koltai PJ, Nelson M, Castellon RJ, Garabedian EN, Triglia JM, Roman S, et al. The natural history of congenital cholesteatoma. Arch Otolaryngol Head Neck Surg. 2002;128:804-9. Surgery is necessary.11 Potsic WP, Korman SB, Samadi DS, Wetmore RF. Congenital cholesteatoma: 20 years' experience at The Children's Hospital of Philadelphia. Otolaryngol Head Neck Surg. 2002;128:810-4.
2 Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts and 53 patients. Otolaryngol Clin North Am. 2006;39:1081-94.
3 Koltai PJ, Nelson M, Castellon RJ, Garabedian EN, Triglia JM, Roman S, et al. The natural history of congenital cholesteatoma. Arch Otolaryngol Head Neck Surg. 2002;128:804-9.
4 Kim SH, Cho YS, Chu HS, Jang JY, Chung WH, Hong SH. Open-type congenital cholesteatoma: differential diagnosis for conductive hearing loss with a normal tympanic membrane. Acta Otolaryngol. 2012;132:618-23.-55 El-Bitar MA, Choi SS, Emamian SA, Vezina LG. Congenital middle ear cholesteatoma: need for early recognition - role of computed tomography scan. Int J Pediatr Otorhinolaryngol. 2003;67:231-5. Spread of the disease and presence of potential complications dictate the final outcome.
Our patient had no history of previous ear infection, trauma or ear surgery. The right-sided AOM masked, and at the same time revealed, a large middle ear cholesteatoma. The facial nerve palsy on the side of the involved ear was a result of the facial nerve damage caused by cholesteatoma pressure accentuated by inflammatory edema.
Urgent surgery was necessary to prevent permanent facial nerve damage. Removal of the cholesteatoma was done by CWD technique. This unpopular technique was chosen because the disease presented itself already through a complication, so any future unrecognized recurrence could lead to irreparable facial nerve damage. The disease has eroded ossicles and the bony canal of the facial nerve in its horizontal segment, above the stapes footplate. Cholesteatoma spread to the auditory tube, anterior attic, antrum, and posteriorly and medially to the lateral semicircular canal, threatening with inner ear and intracranial complications. This case confirmed the fact that the otomicroscopy is insufficient for detecting middle ear cholesteatoma, especially when there is no eardrum perforation or nearby bony defect.
Contralateral middle ear CC was detected by a postoperative MDCT, performed on the grounds of a suspicious otomicroscopy finding during the regular follow-up. The disease could be removed by CWU technique, for it was of a much smaller extent compared to the contralateral ear. Pathology was located mostly in the attic, around the incus body and malleus head, without the involvement of sinus tympani or facial recess. The ossicular chain and tympanic membrane remained intact. No recurrence of disease was noted during a 36-month follow-up.
Had the MDCT been done before or soon after the first surgery, the bilateral disease would have been discovered much earlier. On the other hand, MDCT is not and should not be performed as a routine in patients with AOM who are candidates for urgent myringotomy, but it should be a routine in patients with CC. Nevertheless, MDCT is surely an important but under-indicated diagnostic procedure that is so very useful for surgical planning. Many surgeons rely on experience and routine in middle ear operations. By indicating more radiologic examinations of the temporal bone surgeons could prepare themselves better for surgery and, at the same time, keep radiologists trained in interpreting this complex anatomy and pathology.
Conclusion
Bilateral middle ear congenital cholesteatoma is a very rare entity.
It is important to note that after the discovery of CC on one ear, bilateral disease must be ruled out. CC, just as the acquired cholesteatoma does, requires a thorough surgical removal and a long-term follow-up. Extension and location of the disease dictates the type of surgery and functional outcome. MDCT is a method of choice for diagnosing a hidden bilateral middle ear CC.
-
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.
-
☆
Please cite this article as: Ries M, Kostić M, Ajduk J, Trotić R, Bedeković V. A case of bilateral congenital middle ear cholesteatoma. Braz J Otorhinolaryngol. 2017;83:723-5.
-
☆☆
Institution: University of Zagreb, School of Medicine, Department of ENT Head and Neck Surgery, University Hospital Center "Sestre Milosrdnice", Zagreb, Croatia.
References
-
1Potsic WP, Korman SB, Samadi DS, Wetmore RF. Congenital cholesteatoma: 20 years' experience at The Children's Hospital of Philadelphia. Otolaryngol Head Neck Surg. 2002;128:810-4.
-
2Bennett M, Warren F, Jackson GC, Kaylie D. Congenital cholesteatoma: theories, facts and 53 patients. Otolaryngol Clin North Am. 2006;39:1081-94.
-
3Koltai PJ, Nelson M, Castellon RJ, Garabedian EN, Triglia JM, Roman S, et al. The natural history of congenital cholesteatoma. Arch Otolaryngol Head Neck Surg. 2002;128:804-9.
-
4Kim SH, Cho YS, Chu HS, Jang JY, Chung WH, Hong SH. Open-type congenital cholesteatoma: differential diagnosis for conductive hearing loss with a normal tympanic membrane. Acta Otolaryngol. 2012;132:618-23.
-
5El-Bitar MA, Choi SS, Emamian SA, Vezina LG. Congenital middle ear cholesteatoma: need for early recognition - role of computed tomography scan. Int J Pediatr Otorhinolaryngol. 2003;67:231-5.
-
6Kodama K, Hara M, Hasegawa M, Matsuzawa S, Shinnabe M, Kanazawa H, et al. Two cases of spontaneous regression of congenital cholesteatomas. Int J Pediatr Otorhinolaryngol. 2012;76:142-9.
Publication Dates
-
Publication in this collection
Nov-Dec 2017
History
-
Received
31 July 2015 -
Accepted
29 Sept 2015