ABSTRACT
BACKGROUND AND OBJECTIVES:
This study assessed long-term efficacy of an interdisciplinary group intervention of patients with fibromyalgia as compared with standard medical care.
METHODS:
A partially randomized controlled study with two groups and repeated measures. Variables were measured at baseline; immediately after the program; 4 months and 1 year later. Fibromyalgia patients were recruited by newspaper ads or physician references from two Quebec regions. Sixty women suffering from fibromyalgia were randomized to the experimental group (ISF) or the control group CG. The program, called Interactional School of Fibromyalgia (ISF), consists of nine sessions with eight participants and two clinicians. Five variables were measured: Fibromyalgia Impact Questionnaire (FIQ), Physical and Mental components summary of Short Form Health Survey 36 (SF-36), Clinical pain, and pressure pain threshold at tender points.
RESULTS:
Efficacy analyses from completers, as well as intent-to-treat analyses, showed a treatment effect on measures even one year after the end of the program. The experimental group experienced lower FIQ scores (p<0.01), less clinical pain (p<0.05), higher pressure-pain thresholds (p<0.01), and higher physical component summary scores on the SF-36 (p<0.05).
CONCLUSION:
This interdisciplinary group intervention of patients with fibromyalgia demonstrated better long-term outcomes compared with standard medical care.
Keywords:
Coping; Exercise therapy; Fibromyalgia; Pain management
RESUMO
JUSTIFICATIVA E OBJETIVOS:
Este estudo avaliou a eficácia em longo prazo de uma intervenção interdisciplinar em grupo de pacientes com fibromialgia, comparando-a ao atendimento médico padrão.
MÉTODOS:
O estudo foi realizado randomicamente com dois grupos e coleta de dados de repetição. As variáveis foram medidas antes do início do programa; imediatamente após o programa; 4 meses e 1 ano depois. Os pacientes com fibromialgia foram recrutados por anúncios em jornais ou referências médicas, de duas regiões de Quebec. Sessenta mulheres que sofriam de fibromialgia foram randomizadas para o grupo experimental (EIF) ou o grupo controle (GC). O programa, denominado Escola Interrelacional de Fibromialgia (EIF), consiste em nove sessões com oito participantes e dois clínicos. Cinco variáveis de resultados foram medidas: Questionário de Impacto da Fibromialgia (QIF), resumo de componentes físicos e mentais do Short Form Health Survey 36 (SF-36), dor clínica e limiar de dor por pressão em pontos sensíveis.
RESULTADOS:
As análises de eficácia dos que completaram o programa, bem como as análises de intenção de tratar, mostraram um efeito de tratamento nas medições mesmo um ano após o término do programa. O grupo experimental apresentou pontuações mais baixas do QIF (p<0,01), menos dor clínica (p<0,05), os mais altos limiares de dor por pressão (p<0,01) e as mais altas pontuações do resumo de componente físico no SF-36 (p<0,05).
CONCLUSÃO:
Esta intervenção interdisciplinar em grupo de pacientes com fibromialgia demonstrou melhores resultados em longo prazo em comparação com os cuidados médicos padrão.
Descritores:
Adaptação psicológica; Fibromialgia; Manejo da dor; Terapia por exercício
INTRODUCTION
Fibromyalgia (FM) is a chronic pain syndrome characterized by widespread pain and muscle tenderness. The long-lasting widespread pain of FM is often accompanied by fatigue, stiffness, non-restorative sleep, and mood disturbance11 Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, et al. Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319-29.,22 Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160-72.. Population-based estimates indicate that the prevalence of FM is around 2% and is six times higher for women than men33 McNally JD, Matheson DA, Bakowsky VS. The epidemiology of self-reported fibromyalgia in Canada. Chronic Dis Can. 2006;27(1):9-16.. The FM etiology is unclear, and several conceptual models have been proposed to explain the reported hyperalgesia and allodynia, including disorders of the central nervous system such as neurochemical imbalances44 Russell IJ, Orr MD, Littman B, Vipraio GA, Alboukrek D, Michalek JE, et al. Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome. Arthritis Rheum. 1994;37(11):1593-601., disturbed sleep patterns55 Moldofsky HK. Disordered sleep in fibromyalgia and related myofascial facial pain conditions. Dent Clin North Am. 2001;45(4):701-13., autonomic nervous system dysfunction66 Chalaye P, Lafrenaye S, Goffaux P, Marchand S. The role of cardiovascular activity in fibromyalgia and conditioned pain modulation. Pain. 2014;155(6):1064-9., and deficient endogenous pain-modulating systems77 Julien N, Goffaux P, Arsenault P, Marchand S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain. 2005;114(1-2):295-302..
The complex clinical manifestations and the unfavorable prognosis for patients suffering from FM88 Wigers SH. Fibromyalgia outcome: the predictive values of symptom duration, physical activity, disability pension, and critical life events--a 4.5 year prospective study. J Psychosom Res. 1996;41(3):235-43.,99 Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Flub E, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76(2):318-28. have encouraged health care professionals to use multidisciplinary programs. The promising results achieved by study1010 Bennett RM, Burckhardt CS, Clark SR, O'Reilly CA, Wiens AN, Campbell SM. Group treatment of fibromyalgia: a 6-month outpatient program. J Rheumatol. 1996;23(3):521-8. using a multidisciplinary approach have inspired subsequent studies1111 Lemstra M, Olszynski WP. The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clin J Pain. 2005;21(2):166-74.
12 Bourgault P, Lacasse A, Marchand S, Courtemanche-Harel R, Charest J, Gaumond I, et al. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. PLoS One. 2015;10(5):e0126324.-1313 Jacobs H, Bockaert M, Bonte J, D'Haese M, Degrande J, Descamps L, et al. The impact of a group-based multidisciplinary rehabilitation program on the quality of life in patients with fibromyalgia: results from the QUALIFIBRO Study. J Clin Rheumatol. 2019;19. [Epub ahead of print].. Although some studies have demonstrated good short-term results with multidisciplinary approaches, evidence of long-term benefits remains sparse1313 Jacobs H, Bockaert M, Bonte J, D'Haese M, Degrande J, Descamps L, et al. The impact of a group-based multidisciplinary rehabilitation program on the quality of life in patients with fibromyalgia: results from the QUALIFIBRO Study. J Clin Rheumatol. 2019;19. [Epub ahead of print].. The few multidisciplinary studies conducted using long-term follow-ups (more than 6 months) have reported relatively modest clinical and statistical effects, and weak rates of adherence.
Poor long-term success could be related to the following factors: (a) ignoring the patients’ needs when defining treatment objectives1212 Bourgault P, Lacasse A, Marchand S, Courtemanche-Harel R, Charest J, Gaumond I, et al. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. PLoS One. 2015;10(5):e0126324.,1414 Briones-Vozmediano E, Vives-Cases C, Goicolea I. "I'm not the woman I was": Women's perceptions of the effects of fibromyalgia on private life. Health Care Women Int. 2016;37(8):836-54., (b) weak therapeutic alliance1212 Bourgault P, Lacasse A, Marchand S, Courtemanche-Harel R, Charest J, Gaumond I, et al. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. PLoS One. 2015;10(5):e0126324.,1515 Ollevier A, Vanneuville I, Carron P, Baetens T, Goderis T, Gabriel L, et al. A 12-week multicomponent therapy in fibromyalgia improves health but not in concomitant moderate depression, an exploratory pilot study. Disabil Rehabil. 2019;29:1-8 [Epub ahead of print].,1616 Ericsson A, Mannerkorpi K. How to manage fatigue in fibromyalgia: nonpharmacological options Pain Manag. 2016;6(4):331-8., (c) poor compliance with physical activity programs1717 Malfliet A, Van Oosterwijck J, Meeus M, Cagnie B, Danneels L, Dolphens M, et al. Kinesiophobia and maladaptive coping strategies prevent improvements in pain catastrophizing following pain neuroscience education in fibromyalgia/chronic fatigue syndrome: an explorative study. Physiother Theory Pract. 2017;33(8):653-60.,1818 Dobkin PL, Sita A, Sewitch MJ. Predictors of adherence to treatment in women with fibromyalgia. Clin J Pain. 2006;22(3):286-94., and (d) ignoring the psychological impact of FM1111 Lemstra M, Olszynski WP. The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clin J Pain. 2005;21(2):166-74.. To incorporate these four important factors, we developed a program called the Interactional School of Fibromyalgia (ISF) adapted from the Interactional School of Low Back Pain1919 Charest J, Lavignolle B, Chenard J-R, Provencher M, Marchand S. École interactionnelle du dos. Rhumatologie 1994;48(8):221-37., based on the principles of brief strategic therapy from the Palo Alto group 2020 Fisch R, Schlanger K. Brief therapy with intimidating cases. San Fransico: Jossey-Bass; 1999.. Strategic therapy focuses on the interactions between individuals (other patients, clinicians and significant others) and fosters an environment where patients can become active (empowered) agents in the management of their symptoms. As a result, patients progressively come to consider themselves as “able to cope” with their symptoms. In our program, this also applies to physical complaints, since patients actively take part in the management of their symptoms by accomplishing various prescribed tasks. In addition, patients acquire a better understanding of their disease and learn how to manage it successfully.
The goal of the present study was to verify if our program (the ISF) would provide short-term and long-term benefits (up to one year) for patients suffering from FM. To evaluate the efficacy of our program, we compared our ISF patients with patients treated by standard medical practices.
METHODS
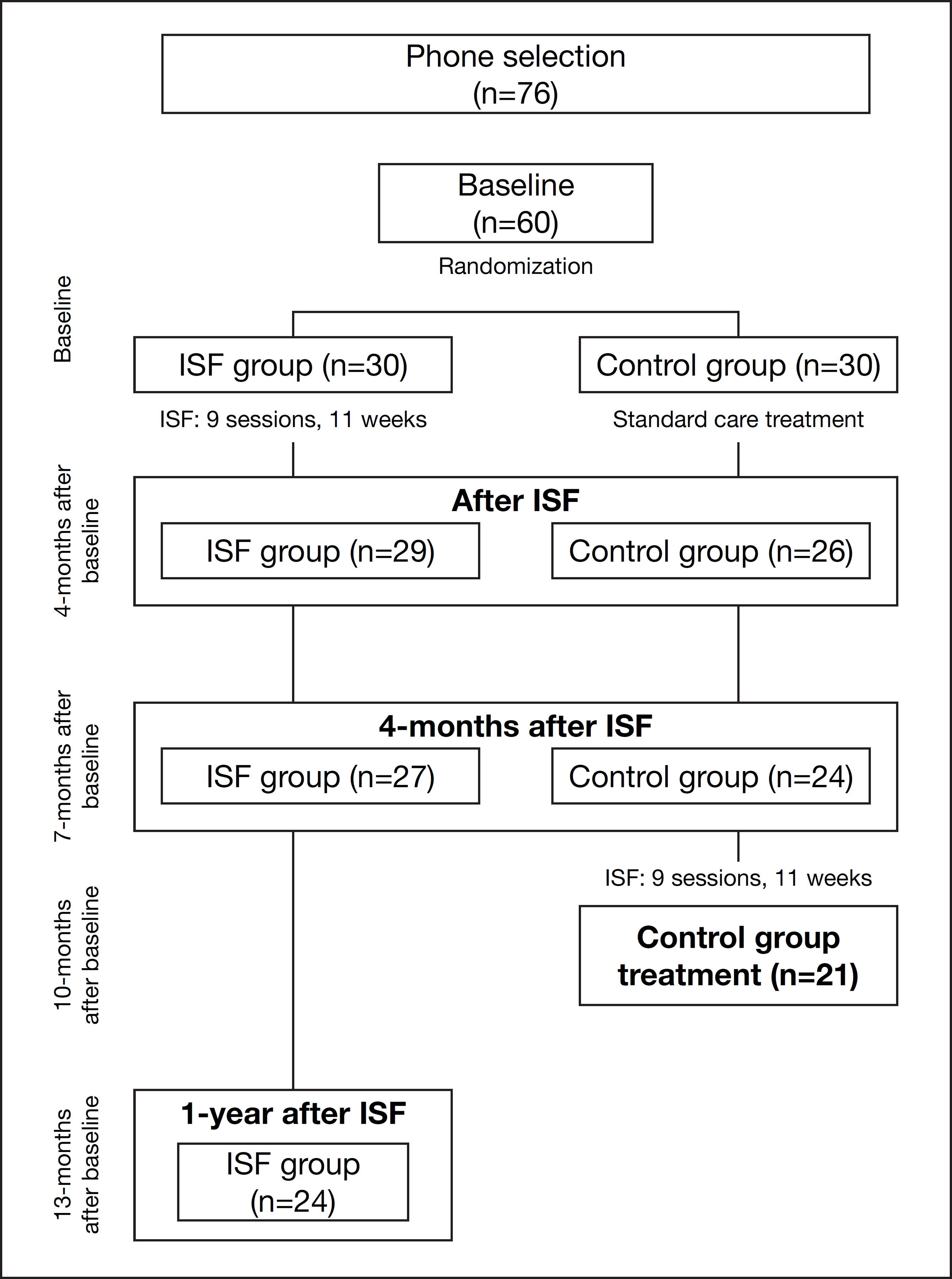
A partially randomized controlled study with two groups. The first group was a waiting list control group (CG) that consisted of patients following standard care treatments. The second group (ISF group) consisted of patients following the ISF. To evaluate outcomes, we applied a repeated-measures protocol. All participants underwent three evaluations: baseline; after the completion of the treatment (11 weeks) and 4-month follow-up (after the end of ISF program). Patients belonging to the ISF group also had a follow-up 1 year after the end of the ISF program (Figure 1). Research assistants, not involved in the intervention, made evaluation sessions.
Patients in this study were recruited by newspaper ads, FM associations and doctors’ references in two Quebec regions. To be eligible, subjects: (a) were between 20 and 65 years of age; (b) were taking the same pharmacological treatment for more than three months or no treatment at all; and (c) had a medical diagnosis of FM for more than six months. This diagnosis was re-tested to confirm ACR classification criteria of FM22 Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160-72.: (i) reported widespread pain for at least 3 months and (ii) pain at least 11 of the 18 tender points measured with a pressure of ≤4kg.cm2 using a digital algometer. Patients involved in litigation concerning social disability income or patients with the comorbidity of hypothyroidism, depression, chronic lower back pain or post-traumatic stress disorder were also included. However, patients were excluded for the following reasons: pregnancy or breastfeeding, and the following pathologies: pain associated with cancer, depressive patients with suicidal thoughts, and other serious psychiatric diseases including schizophrenia. From an initial group of 76 patients, 60 women met the inclusion criteria.
Patients were randomly placed into the ISF or CG group using a concealed allocation, block randomization method, stratified by the level of pain intensity on the Fibromyalgia Impact Questionnaire (FIQ) measured at the baseline evaluation. The lower-moderate-pain block equaled a score of 1 to 50 on a scale of 100 and the moderate-severe-pain block, a score of 51 or more on a scale of 100. The name of each patient was placed in a separate, opaque and sealed envelope, marked on the outside with their block: lower-moderate or moderate-severe pain intensity. The participants were randomly allocated in blocks with permutation in order to have the ISF and CG group. After the baseline evaluation, an equal number of participants from each of these blocks were randomly placed in the ISF group and the CG.
Patients belonging to ISF group were asked not to change their pharmacological treatment and not to follow a new treatment during our program. In contrast, patients in the CG followed standard medical care and could change the nature of their treatments on an as-needed basis. As a result, 37% of patients in the CG changed their pharmacological treatment, 7% began receiving steroid injections, 37% started walking, and 7% started relaxation. The ISF program was always offered to CG patients after the third evaluation, that is, 7 months after baseline. Patients were not remunerated for their participation in this research.
Twenty-nine patients out of 30 (97%) completed the ISF program. Twenty-eight of these patients completed the 4-month follow-up and 24 patients completed the one-year follow-up. In the CG, 24 out of 30 patients completed the follow-up evaluation.
The ISF is a structured group intervention (8 patients) consisting in nine weekly sessions of 2 hours each, led by two clinicians (ex: a psychologist and a physiotherapist). Each session is organized around a theme for discussion and around the supervised practice of different strategies for symptom control (breathing, relaxation, physical exercises, problem solving etc.). At the end of each session, a new task (physical, social or cognitive activities adapted to each patient) is prescribed to be accomplished prior to the next session.
The sessions are organized around nine themes, namely: Therapeutic contract, Symptoms management, Physical force, Mental force, Energy management, Nutrition, Chronicity, Treatment, and Retrospective (Table 1). An additional, follow-up session is held four months after the end of ISF where patients are encouraged to progress slowly with their new habits.
Given the importance of physical activity, a physiotherapist was always present to prescribe exercises that were tailored to the goals set by each participant. The physiological goals of the training in the ISF group were obtained through stretching, strength and aerobic exercises. Stretching and strength training were to attain personal goals such as “increase my arm strength, from 3 to 5 on a scale of 10” or “to be able to cook without dropping objects”. Aerobic training (50% maximum heart rate) was to improve symptoms related to pain, fatigue, sleep and mood 2121 Jones KD, Adams D, Winters-Stone K, Burckhardt CS. A comprehensive review of 46 exercise treatment studies in fibromyalgia (1988-2005). Health Qual Life Outcomes. 2006;4:67-73.. A systematic review article, published after our study, validates the usefulness of aerobic, strength and stretching exercises for FM patients2222 Busch AJ, Schachter CL, Overend TJ, Peloso PM, Barber KA. Exercise for fibromyalgia: a systematic review. J Rheumatol. 2008;35(6):1130-44.. Manipulation techniques, passive therapies, and individual sessions were never prescribed. During the ISF program, patients did not receive any new non-pharmacological or pharmacological treatment.
Clinical pain
Clinical pain ratings were recorded at home using a visual analog scale (VAS). Two 100-millimeters VAS were used, one for pain intensity and one for pain unpleasantness. The endpoints for these scales varied from “no pain” to “the most intense/unpleasant pain imaginable”. Patients were instructed to record their pain ratings every two hours - while awake - during three discontinuous days of a week (two weekdays and one weekend day). At-home evaluations have previously been used with chronic pain patients and provide an accurate profile of their clinical pain1919 Charest J, Lavignolle B, Chenard J-R, Provencher M, Marchand S. École interactionnelle du dos. Rhumatologie 1994;48(8):221-37.,2323 Marchand S, Charest J, Li J, Chenard JR, Lavignolle B, Laurencelle L. Is TENS purely a placebo effect? A controlled study on chronic low back pain. Pain. 1993;54(1):99-106.. Clinical pain was calculated by producing the mean pain rating for all three days for each scale. The test-retest reliabilities were high (r=0.7-0.9)2424 Price DD. Psychological mechanisms of pain and analgesia. Seattle: IASP; 1999.. The at-home evaluations of clinical pain were recorded during the week that followed the baseline evaluation. After each evaluation meeting (Figure 2), research assistants not involved in the intervention handed the questionnaire to the patient with instructions to return it to the research team in the included pre-addressed, postage paid envelope.
The FIQ is a self-administered questionnaire that measures the components of health status most affected by FM over the past week2525 Burckhardt CS, Clark SR, Bennett RM. The fibromyalgia impact questionnaire: development and validation. J Rheumatol. 1991;18(5):728-33.. The FIQ has been shown to be one of the most responsive measures of clinical improvement in FM patients. In the present study, the French version of the FIQ was administered. This version is widely used by researchers and clinicians and has acceptable test-retest reliability (ranged from 0.56 on the pain score to 0.95 for physical function)2626 Bennett R. The Fibromyalgia Impact Questionnaire (FIQ): a review of its development, current version, operating characteristics and uses. Clin Exp Rheumatol. 2005;23(5 Suppl 39):S154-62. and construct validity2727 Perrot S, Dumont D, Guillemin F, Pouchot J, Coste J. Quality of life in women with fibromyalgia syndrome: validation of the QIF, the French version of the fibromyalgia impact questionnaire. J Rheumatol. 2003;30(5):1054-9..
Short-Form Health Survey (SF-36)
This instrument is a self-administered questionnaire used to assess general health status. The SF-36 contains 36 questions designed to measure physical and mental components of health among the clinical and general population2828 Ware JE Jr. SF-36 health survey update. Spine. 2000;25(24):3130-9.. The mean scores of physical and mental components summary of SF36 were standardized to simplify interpretation of results. Norm-based scoring was very useful when interpreting differences across scales in the SF-36 profile. The French version of the SF-36 was used in the present study and presents excellent psychometric properties2929 Leplege A, Ecosse E, Verdier A, Perneger TV. The French SF-36 Health Survey: translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol 1998;51(11):1013-23.. The reliability of these two component measures has been estimated using internal consistency and test-retest method, and it had exceeded the minimum standard of 0.703030 McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247-63..
Experimental pain (Pressure-Pain Threshold at tender points)
Pressure-pain thresholds at tender points were assessed by a trained investigator, using a digital force gauge with a 1cm2 tip (Shimpo, FGE-100). Pressure was applied at a rate of 1kg/s on each one of the18 FM-specified tender points11 Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, et al. Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319-29.. Subjects were instructed to verbally report when the perception at the examination site changed from pressure to pain. The mean tender-point threshold (kg) was calculated for the 18 points.
The Human Ethics Committees of the Université du Québec en Abitibi-Témiscamingue and the Centre Hospitalier de l’Université de Sherbrooke approved the study protocol, and all participants provided written Free Informed Consent Term (FICT) before study procedures were initiated.
Statistical analysis
A priori sample size estimates indicate that 24 patients would be required in each group to detect a significant difference on clinical pain (a=5% and b=20%), with an expected effect size at 0.80. Given the shrinking sample size over time (Figure 1), we tested for group and time differences by conducting a series of ANOVAs (2x2) with paired times of measures (baseline X after ISF, 4 months after ISF) and groups (control and experimental group), and student-t-test for intra-group differences with all times of measures for ISF group (baseline X after ISF, 4 months after ISF, 1 year after ISF) and for treated CG (data from 4 months after ISF, so immediately before the CG treatment X CG data). Effect size (d) was defined as large effect size if it was over 0.8. The significant level was defined at 5%. However, because there are a set of ANOVAs, a Bonferroni type adjustment was made for inflated Type I error of pairwise comparisons3131 Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed. New York: Perason Education; 2007..
To avoid bias and maximize the randomization process we used intention-to-treat analysis (ITT), and control for the potential negative impact of attrition, we conducted an ITT where experimental group subjects, who dropped out were kept but where their missing values were replaced by the baseline data. Our ITT analyses were conducted on long-term outcomes (baseline versus 1 year follow-up data for the ISF group) and were compared to the results obtained when only completers (n=24) were analyzed (efficacy analyses) using a paired t-test. The alpha level was defined at 5%, normality of variables was confirmed by exploratory analyses. Statistical analyses were computed with SPSS for Windows, (Chicago, IL).
RESULTS
The baseline demographic, clinical and psychological characteristics of patients were similar for each group (Table 2). No significant differences were observed comparing outcomes between different ISF groups/times (PM versus night), neither between different clinicians.
The program was applied by different therapists in two different regions of Quebec: an educational setting (Université du Québec en Abitibi-Témiscamingue) and in a clinical environment (Centre Hospitalier Universitaire de Sherbrooke) with no difference between regions baseline data (all t-values>-1.090; p>0.29), neither outcomes data (all t-values>1.393; p>0.18). Five subjects at baseline and seven at 4-month follow up from CG did not return their Clinical VAS scores by mail. All subjects successfully completed all other measures. Of the four ISF groups, two occurred in the afternoon (2-4PM) and the others in the evening (6-8PM). There were no statistical differences in outcome measures between the ISF groups. Patients chose the time-group in which they wanted to participate.
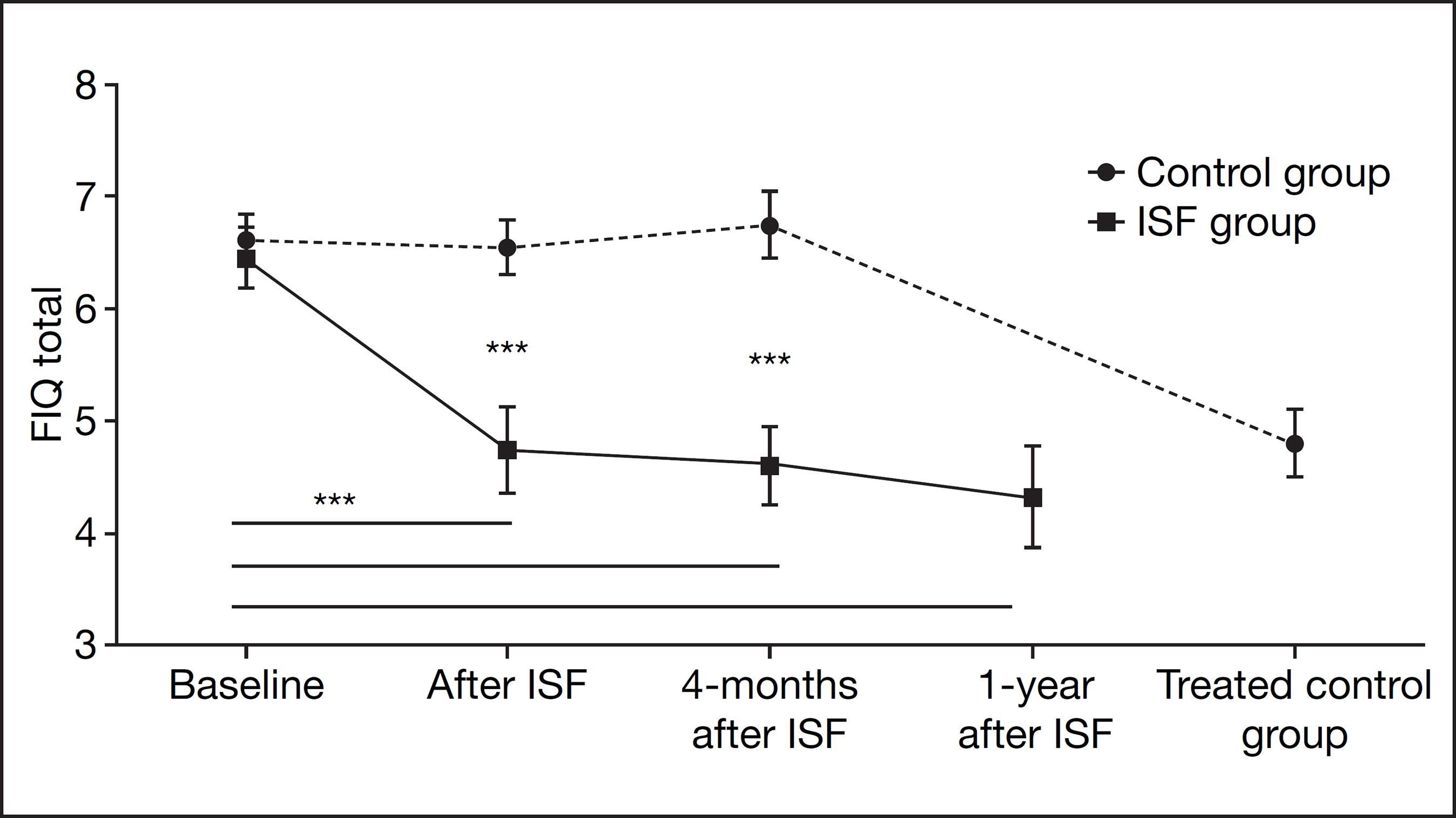
At the end of the ISF program, dependent variables (FIQ and PPT) were assessed on the CG. Some of these outcomes for the ISF group (continuous line) and the CG (broken line) are illustrated in figure 2. Three CGs were offered, one morning group, one afternoon and an evening group. Again, patients chose their own time-group
The set of MANOVAs conducted on clinical pain intensity scores showed a significant improvement of the ISF compared to CG measures assessed immediately after the program (F1,46 =7.457; p<0.05; d=0.74), and 4-months after ISF (F1,43=7.870; p<0.05; d=0.78). Multivariate analysis testing for interaction terms (time x group) was not significant (F2,80=2.816; p=0.07).
At the 4-months after ISF follow up, clinical pain scores reduced by approximately 8 points on the VAS (from 40.40±15.97 at baseline to 32.85±14.41 at 4-months after ISF; n=20). One-year after the ISF, clinical pain intensity was at 27.59±17.75 (n=22) for ISF. The intra-group clinical pain intensity improvement on ISF subjects was significant immediately after the program (t25, 5%= 4.547; p<0.05; d=0.59) and 1-year after ISF (t21, 5%= 4.635; p<0.05; d=0.74). No significant change has been observed on clinical pain scores for CG (changing from 53.12±20.48 at baseline to 49.36±23.06 at 4 months after ISF; n=22).
The set of MANOVAs conducted on clinical pain unpleasantness scores showed a significant improvement of the ISF compared to CG measures assessed immediately after the program (F1,46 =6.251; p<0.05; d=0.69), and 4-months after ISF (F1,43=5.994; p<0.05; d=0.69). Multivariate analysis testing for interaction terms (time x group) was not significant (F2,80=2.464; p=0.09).
At the 4-months after ISF follow up, unpleasantness clinical pain scores reduced almost 6 points on VAS (from 36.42±16.32 at baseline to 30.66±14.89 at 4-months after ISF; n=20). Clinical pain unpleasantness also decreased significantly immediately after the program (t25, 5%= 3.107; p<0.05; d=0.48) and 1-year after ISF (t21, 5%=3.421; p<0.05; d=0.60). No significant change has been observed on clinical pain scores for CG (changing from 49.48±23.82 at baseline to 46.92±25.00 at 4-months after ISF; n=22).
Fibromyalgia Impact Questionnaire (FIQ)
The set of MANOVAs conducted on FIQ scores showed a significant improvement of ISF compared to CG measures assessed immediately after the program (F1,53 =10.485; p<0.01; d=0.81) and 4-months after ISF (F1,48 =20.711; p<0.01; d=1.09). Multivariate analysis testing for interaction terms (time x group) was also significant (F2,96=15.108; p<0.01).
At the 4-months after ISF follow up, FIQ scores reduced almost 14 points (from 50.75±12.15 at baseline to 36.81±14.74 at 4-months after ISF; n=27) in contrast to no significant change on FIQ scores for CG (from 51.63±9.75 at baseline to 53.95±11.55 at 4-months after ISF; n=24). The intra-group FIQ improvement of ISF subjects was significantly improved immediately after the program (t28, 5% = 5.314; p<0.01; d=0.83), 4-month after the ISF (t26, 5%= 5.118; p<0.05; d=0.98), and 1-year after ISF (t23, 5%= 5.358; p<0.05; d=0.86). On the other hand, patients in the CG showed no change on their FIQ scores over this same period (F2,46=1.582; p=0.22; n=24). Figure 2 illustrates the FIQ values obtained by ISF and CG patients over the course of the study.
It is important to note that the data shown in figure 3 include the 1-year follow-up scores obtained by the ISF and include the post-treatment scores obtained by the “treated” CG.
Percentage of Improvement after the Interactional School of Fibromyalgia and at 1-year follow up compared to baseline
* p<0,01; *** p<0,0001. The p-values of the paired t-test results at the different evaluation times are indicated by the *** next to horizontal lines (for the ISF group: continuous line and the control group: broken line). The length of which represent the evaluation times indicated along the x-axis. The p-value is not repeated if it was the same.
FIQ = Fibromyalgia Impact Questionnaire; Physical-SF36 = Physical Components Summary of SF-36; Mental-SF36 = Mental Component Summary of SF36; PPT = Pressure Pain Threshold at tender points.
Short-Form Health Survey (SF-36)
The set of MANOVAs conducted on physical health outcome scores (physical component summary of SF-36) showed a significant improvement of ISF group compared to CG measures assessed immediately after the program (F1,51 =18.461; p<0.01; d=1.02) and 4-months after ISF (F1,49 =16.298; p<0.01; d=0.99). Multivariate analysis testing for interaction terms (time x group) was significant (F2,98=20.881; p<0.01).
At the 4-months after ISF follow up, PCS of SF-36 improved from 30.78±6.53 at baseline to 39.18±9.54 at 4-months after ISF (n=27) in contrast of no changes on scores for CG (from 31.02±5.33 at baseline to 29.90±6.33 at 4-months after ISF; n=24).
Intra-group PCS of SF-36 for ISF subjects showed significant improvement immediately after the program (t27, 5% = 7.679; p<0.05; d=1.11), 4-month after the ISF (t26, 5%= 6.539; p<0.05; d=0.88), and 1-year after ISF (t23, 5%= 4.702; p<0.05; d=0.87).
The intra-group mental component summary (MCS) of SF-36 improvement of ISF subjects was significant only at 1-year follow-up (t23, 5% = 2.227; p<0.05; d=0.46). Multivariate analysis testing for interaction terms (time x group) was not significant (F2,98=0.373; p=0.69).
At the 4-months after ISF follow up, MC summary of SF-36 had a clinical improvement from 41.08±11.91 at baseline to 44.83±13.21 at 4-months after ISF (n=27) in contrast no changes on scores for CG (from 37.98±10.83 at baseline to 38.80±9.63 at 4-months after ISF; n=24).
CG showed no change on their component Summary of SF-36 scores over the 7-month period (MC summary: F2,46=0.648; p=0.53; n=24 and PCS F2,46=0.663; p=0.52; n=24).
Pressure pain threshold
The set of MANOVAs conducted on PPT showed a significant improvement of the ISF group compared to CG measures assessed immediately after the program (F1,53 =12.130; p<0.01; d=0.86) and 4-months after ISF (F1,49=26.362; p<0.01; d=1.17). Multivariate analyses testing for interaction terms (time x group) was significant (F2,98=13.100; p<0.01). Intra-group PPT improvement of ISF subjects was significant for all follow-ups (until 1 year after ISF) (F3,66=26.362; p<0.01; n=23). At the 4 months after ISF follow up, PPTs increased from 0.76±4.90 at baseline to 1.59±0.86 at 4 months after ISF (n=27). The ISF group reported an improvement of 35% after treatment (t28, 5%= 4.865; p<0.05; d=0.61), an improvement of 49% at the 4 month follow up (t26, 5%= 6.772; p<0.05; d=0.96) and an improvement of 54% at the 1 year follow up (t22, 5%= 6.246; p<0.05; d=0.97; n=23).
Long-term outcome of ISF group
One-year follow-up measures obtained for the ISF group reveal that patients maintained the statistically significant improvements described earlier. As shown in figure 3, there is a gradual improvement in outcome scores through time. This improvement can be seen in figure 3, which shows the percentage change in outcome scores calculated immediately after the treatment and at 1-year follow-up. The results obtained with ITT method were similar when efficacy analysis was applied (completers).
One-year follow-up dropout patients had significantly more pain (intensity and unpleasantness) at baseline than completers and had a lower MCS - SF36 at baseline than completers (Table 3). Applying ANOVAs to observed dropouts outcomes (n=6) we observed that PPT showed a trend to improve (F2,4= 4.865; p=0.09; mean of variable improved from 0.49±0.32 at baseline to 1.06±0.34 at 4-month follow-up). Other variables, such as FIQ, clinical pain, physical and mental components summary did not show any significant improvement (all Fs< 6.245; all Ps>0.27).
“Treated control group” outcomes
The patients from the CG followed the ISF program after their third evaluation session. The results of the CG showed an improvement equivalent to that of the ISF group. Immediately after the ISF program, CG reported a reduction on FIQ from 53.07±13.12 (data accessed on 4-months after ISF for experimental group) to 34.99±11.51 (n=17) (t16,5%=9.251; p<0.01; d=1.51). An improvement of PPT at Tender Points, increasing from 0.62±0.39kg/cm2 to 1.05±0.65 kg/cm2 (n=20) (t19,5%=-4.376; p<0.001; d=0.81), was also observed.
After a comparison between CG outcomes immediately after the program and ISF group outcomes from the 1-year follow-up, we observed that FIQ scores were not statistically different between groups (ISF group reported FIQ at 34.61±17.71 at the 1-year follow-up; n=24) (t39, 5%=0.081; p=0.94). PPT on Tender Points was significantly better at 1-year follow-up (ISF group outcomes: 1.91±1.16) than immediately outcomes after ISF (CG: 1.09±0.65) (t39, 5%=-2.885; p=0.007).
DISCUSSION
This study reveals that the ISF had not only beneficial short-term but also long-term (1-year) effects on clinical manifestations of FM. Our results show significant changes on all dependent variables including a reduction of the impact of FM, clinical and experimental pain perception and an improvement in general health status.
Prior studies have shown that an improvement in functional capacity does not always occur together with an improvement in FM clinical manifestations1212 Bourgault P, Lacasse A, Marchand S, Courtemanche-Harel R, Charest J, Gaumond I, et al. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. PLoS One. 2015;10(5):e0126324.,3232 Wang C, Schimd CH, Fielding RA, Harvey WF, Reid KF, Price LL, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ. 2018;21(360):k851.,3434 Gowans SE, Dehueck A, Voss S, Silaj A, Abbey SE. Six-month and one-year follow-up of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Rheum. 2004 15;51(6):890-8.. To address this point, ISF adapts strategies to patients’ goals. In our study, all patients reached at least one of their personal goals and 70% of ISF completers reached all their three personal goals.
The ISF was tailored to increase patient self-management of FM symptoms. Contrary to previous studies that took 15 to 25 sessions to achieve similar clinical results1010 Bennett RM, Burckhardt CS, Clark SR, O'Reilly CA, Wiens AN, Campbell SM. Group treatment of fibromyalgia: a 6-month outpatient program. J Rheumatol. 1996;23(3):521-8., the ISF program obtained greater changes and long-term effects with only nine 2-hour group sessions. The ISF also had a 97% adherence rate, which is greater than that in prior studies1111 Lemstra M, Olszynski WP. The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clin J Pain. 2005;21(2):166-74.,1818 Dobkin PL, Sita A, Sewitch MJ. Predictors of adherence to treatment in women with fibromyalgia. Clin J Pain. 2006;22(3):286-94.,3333 Mannerkorpi K, Ahlmen M, Ekdahl C. Six- and 24-month follow-up of pool exercise therapy and education for patients with fibromyalgia. Scand J Rheumatol. 2002;31(5):306-10.. ISF adherence was defined by the active participation in all activities prescribed during the program.
The long-term success of the ISF program was probably based on patients’ commitment to change and their persistence with prescribed activities. Several studies indicate that a lack of adherence to exercise programs leads to a decrease in the beneficial effects on health3333 Mannerkorpi K, Ahlmen M, Ekdahl C. Six- and 24-month follow-up of pool exercise therapy and education for patients with fibromyalgia. Scand J Rheumatol. 2002;31(5):306-10.,3434 Gowans SE, Dehueck A, Voss S, Silaj A, Abbey SE. Six-month and one-year follow-up of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Rheum. 2004 15;51(6):890-8.. Three principal elements of the ISF could explain the adherence of patients to the activities: (a) the active participation of patients in establishing their personal treatment goals, (b) the therapeutic alliance, maintained by the informal conversations between patients and facilitators and by the fact that all group sessions were facilitated by the same two therapists; and (c) the prescription of simple, personalized tasks.
In keeping with the results of prior studies showing a strong link between the active participation of patients in establishing their treatment goals and positive long-term results1212 Bourgault P, Lacasse A, Marchand S, Courtemanche-Harel R, Charest J, Gaumond I, et al. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. PLoS One. 2015;10(5):e0126324.,1313 Jacobs H, Bockaert M, Bonte J, D'Haese M, Degrande J, Descamps L, et al. The impact of a group-based multidisciplinary rehabilitation program on the quality of life in patients with fibromyalgia: results from the QUALIFIBRO Study. J Clin Rheumatol. 2019;19. [Epub ahead of print]., the active participation of the patient is solicited from the very first group session of ISF. Each patient creates her own therapeutic contract which includes both the “minimal change” (the first sign of a change) acceptable by the patient, e.g.: “a reduction of 10% of my pain by the end of the ISF” and three personal goals pertinent to the life of the patient, e.g., “able to cook for one hour in spite of the weakness in my hands”.
Maintaining a strong therapeutic alliance, shown by several studies to have a positive impact on adherence, guided all the interactions between the therapists and the patients during the ISF. In keeping with the studies showing that patients with higher personal efficacy tend to persist more in their activities1212 Bourgault P, Lacasse A, Marchand S, Courtemanche-Harel R, Charest J, Gaumond I, et al. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. PLoS One. 2015;10(5):e0126324.,1313 Jacobs H, Bockaert M, Bonte J, D'Haese M, Degrande J, Descamps L, et al. The impact of a group-based multidisciplinary rehabilitation program on the quality of life in patients with fibromyalgia: results from the QUALIFIBRO Study. J Clin Rheumatol. 2019;19. [Epub ahead of print]., therapists made regular reference to the expertise that the patient had developed in coping with her FM condition. The therapists also clearly attribute any patient improvement to the efforts of the patient.
The prescription of simple and personalized exercises improved the patient’s perception of self-management with their symptoms, which involves a change from a psychological point of view: instead of seeing herself as a “victim” of FM, the patient progressively comes to consider herself as “able to cope” with her symptoms. Patients develop strategies and acquire knowledge to successfully manage symptoms. For example, in the first session of the ISF, patients start practicing deep breathing (diaphragmatic breathing or natural breathing). The manipulation of breath movements, using techniques of slow breathing, improves autonomic functions, decreasing sympathetic activity and increasing parasympathetic activity3535 Chalaye P, Goffaux P, Lafrenaye S, Marchand S. Respiratory effects on experimental heat pain and cardiac activity. Pain Med. 2009;10(8):1334-40.. These simple breathing techniques could help patients to balance their autonomic nervous system dysfunction66 Chalaye P, Lafrenaye S, Goffaux P, Marchand S. The role of cardiovascular activity in fibromyalgia and conditioned pain modulation. Pain. 2014;155(6):1064-9.. In doing so, it could also help with sleeping problems55 Moldofsky HK. Disordered sleep in fibromyalgia and related myofascial facial pain conditions. Dent Clin North Am. 2001;45(4):701-13.. The concentration on breathing techniques during stretching and strength exercises reduces tensions and favors the relaxation feeling, e.g., breathing to relax and release neck tension while facilitating abdominal muscle contraction (diaphragm). Our patients reported that diaphragmatic breathing prevented and reduced the intensity of acute pain crises. Indeed, at the 1 year follow up, six of the 24 patients present less than 11 positive tender points and seven report no chronic pain (or persistent pain). According the FM classification criteria established by the American College of Rheumatology in 199022 Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160-72., 25% of patients from our ISF group would no longer be diagnosed as having fibromyalgia. Future research is needed to explain the mechanisms related to the PPT increase at the tender points on this FM population.
Depression could be a confounding variable of chronic pain treatments outcomes1515 Ollevier A, Vanneuville I, Carron P, Baetens T, Goderis T, Gabriel L, et al. A 12-week multicomponent therapy in fibromyalgia improves health but not in concomitant moderate depression, an exploratory pilot study. Disabil Rehabil. 2019;29:1-8 [Epub ahead of print].,1717 Malfliet A, Van Oosterwijck J, Meeus M, Cagnie B, Danneels L, Dolphens M, et al. Kinesiophobia and maladaptive coping strategies prevent improvements in pain catastrophizing following pain neuroscience education in fibromyalgia/chronic fatigue syndrome: an explorative study. Physiother Theory Pract. 2017;33(8):653-60.,3636 Niederstrasser NG, Slepian PM, Mankovsky-Arnold T, Larivière C, Vlaeyen JW, Sullivan MJL. An experimental approach to examining psychological contributions to multisite musculoskeletal pain. J Pain. 2014;15(11):1156-65.. In this study, 42% of patients reported a depression at baseline, but the percentage of ISF improvement was not different by the presence/absence of depression at baseline.
The strengths of this study are: (a) the presence of a randomized control group, evaluated during 7 months, (b) a research assistant not involved in the intervention applied the various questionnaires; (c) the program was applied by different therapists in two different regions of Quebec: an educational setting (Université du Québec en Abitibi- Témiscamingue) and a clinical (Centre Hospitalier Universitaire de Sherbrooke); and (d) the high compliance of participants, just one patient quit before the end of the program and only five did not return for the 1 year follow up.
There are some limitations to the present study. The current design does not control our ISF group with a placebo group. However, ISF was compared to the usual treatment during 7 months. Another limitation was that patients from CG were evaluated during a period of 7 months but there was no follow up at “one year”, as for the ISF group. However, as no significant difference was observed during this period, it could be speculated that these dependent variables could be equivalent after 1 year. The ISF program was not blinded to intervention status. It is possible that the ISF group responded differently in comparison to CG as a result of the Hawthorne effect. This limit was minimized but not eliminated by outcomes of the CG. The assessment of clinical pain was done on the week that followed the evaluation and responses could have been also biased by the Hawthorne effect. Another limit was that all subjects were volunteers, and it is possible that ISF patients want to achieve positive results while this Hawthorne effect was absent in the CG. This was controlled through the use of blinded measurements (patients did not have access to their original scores) and through analysis from CG outcomes. Missing data concerning the clinical pain limited our analysis. Another limit of this study was the absence of men in our sample. Females are over-represented in the FM population. It is still uncertain to generalize these results for men with FM. Finally, outcomes from the ISF program have only been tested in research setting; additional trials need to be performed to determine intervention effectiveness. This limit has been minimized but not eliminated by the evaluation of ISF program in two different regions of Quebec (Abitibi-Témiscamingue and Estrie) and two different environments (educational and clinical ones).
Future studies should measure neurobiological controls, which would provide more information concerning the hypothesis of the exercise effect on the endogenous opioids system to explain pain reduction in ISF patients.
CONCLUSION
In summary, the ISF program is a brief and structured group intervention that provides long-term beneficial outcomes in FM population. The program was sufficiently comprehensive to address the complexity of FM clinical manifestation.
-
Sponsoring sources: CAPES.
ACKNOWLEDGMENT
This research was supported by Dr. Marchand’s research grants from the Canadian Institutes of Health Research (CIHR), the FRSQ Centre de recherche linique Étienne-Le Bel du CHUS and by a postgraduate scholarship from the Coordenadoria de Aperfeiçoamento de Pessoal do Ensino Superior (CAPES, subordinate to the Brazilian Ministry of Education and Culture) given to Juliana Barcellos de Souza. The authors thanks to Michelle Provencher, MSc; Philippe Goffaux, Ph.D.; Sarah Shidler, PhD; Gertrudes Maria Oliveira Cardoso e Silva, Inf.; Pierre Arsenault, PhD, MD; Sylvie l’Heureux, MSc; Nancy Julien, PhD; and Christine Brown, MSc for their input and suggestion at various stages of this program of research. We thank Paule Julien, Edith Normand and Marie-Claude Tremblay for providing excellent technical assistance and our participants for volunteering in this study.
REFERENCES
-
1Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, et al. Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319-29.
-
2Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160-72.
-
3McNally JD, Matheson DA, Bakowsky VS. The epidemiology of self-reported fibromyalgia in Canada. Chronic Dis Can. 2006;27(1):9-16.
-
4Russell IJ, Orr MD, Littman B, Vipraio GA, Alboukrek D, Michalek JE, et al. Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome. Arthritis Rheum. 1994;37(11):1593-601.
-
5Moldofsky HK. Disordered sleep in fibromyalgia and related myofascial facial pain conditions. Dent Clin North Am. 2001;45(4):701-13.
-
6Chalaye P, Lafrenaye S, Goffaux P, Marchand S. The role of cardiovascular activity in fibromyalgia and conditioned pain modulation. Pain. 2014;155(6):1064-9.
-
7Julien N, Goffaux P, Arsenault P, Marchand S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain. 2005;114(1-2):295-302.
-
8Wigers SH. Fibromyalgia outcome: the predictive values of symptom duration, physical activity, disability pension, and critical life events--a 4.5 year prospective study. J Psychosom Res. 1996;41(3):235-43.
-
9Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Flub E, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76(2):318-28.
-
10Bennett RM, Burckhardt CS, Clark SR, O'Reilly CA, Wiens AN, Campbell SM. Group treatment of fibromyalgia: a 6-month outpatient program. J Rheumatol. 1996;23(3):521-8.
-
11Lemstra M, Olszynski WP. The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clin J Pain. 2005;21(2):166-74.
-
12Bourgault P, Lacasse A, Marchand S, Courtemanche-Harel R, Charest J, Gaumond I, et al. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. PLoS One. 2015;10(5):e0126324.
-
13Jacobs H, Bockaert M, Bonte J, D'Haese M, Degrande J, Descamps L, et al. The impact of a group-based multidisciplinary rehabilitation program on the quality of life in patients with fibromyalgia: results from the QUALIFIBRO Study. J Clin Rheumatol. 2019;19. [Epub ahead of print].
-
14Briones-Vozmediano E, Vives-Cases C, Goicolea I. "I'm not the woman I was": Women's perceptions of the effects of fibromyalgia on private life. Health Care Women Int. 2016;37(8):836-54.
-
15Ollevier A, Vanneuville I, Carron P, Baetens T, Goderis T, Gabriel L, et al. A 12-week multicomponent therapy in fibromyalgia improves health but not in concomitant moderate depression, an exploratory pilot study. Disabil Rehabil. 2019;29:1-8 [Epub ahead of print].
-
16Ericsson A, Mannerkorpi K. How to manage fatigue in fibromyalgia: nonpharmacological options Pain Manag. 2016;6(4):331-8.
-
17Malfliet A, Van Oosterwijck J, Meeus M, Cagnie B, Danneels L, Dolphens M, et al. Kinesiophobia and maladaptive coping strategies prevent improvements in pain catastrophizing following pain neuroscience education in fibromyalgia/chronic fatigue syndrome: an explorative study. Physiother Theory Pract. 2017;33(8):653-60.
-
18Dobkin PL, Sita A, Sewitch MJ. Predictors of adherence to treatment in women with fibromyalgia. Clin J Pain. 2006;22(3):286-94.
-
19Charest J, Lavignolle B, Chenard J-R, Provencher M, Marchand S. École interactionnelle du dos. Rhumatologie 1994;48(8):221-37.
-
20Fisch R, Schlanger K. Brief therapy with intimidating cases. San Fransico: Jossey-Bass; 1999.
-
21Jones KD, Adams D, Winters-Stone K, Burckhardt CS. A comprehensive review of 46 exercise treatment studies in fibromyalgia (1988-2005). Health Qual Life Outcomes. 2006;4:67-73.
-
22Busch AJ, Schachter CL, Overend TJ, Peloso PM, Barber KA. Exercise for fibromyalgia: a systematic review. J Rheumatol. 2008;35(6):1130-44.
-
23Marchand S, Charest J, Li J, Chenard JR, Lavignolle B, Laurencelle L. Is TENS purely a placebo effect? A controlled study on chronic low back pain. Pain. 1993;54(1):99-106.
-
24Price DD. Psychological mechanisms of pain and analgesia. Seattle: IASP; 1999.
-
25Burckhardt CS, Clark SR, Bennett RM. The fibromyalgia impact questionnaire: development and validation. J Rheumatol. 1991;18(5):728-33.
-
26Bennett R. The Fibromyalgia Impact Questionnaire (FIQ): a review of its development, current version, operating characteristics and uses. Clin Exp Rheumatol. 2005;23(5 Suppl 39):S154-62.
-
27Perrot S, Dumont D, Guillemin F, Pouchot J, Coste J. Quality of life in women with fibromyalgia syndrome: validation of the QIF, the French version of the fibromyalgia impact questionnaire. J Rheumatol. 2003;30(5):1054-9.
-
28Ware JE Jr. SF-36 health survey update. Spine. 2000;25(24):3130-9.
-
29Leplege A, Ecosse E, Verdier A, Perneger TV. The French SF-36 Health Survey: translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol 1998;51(11):1013-23.
-
30McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247-63.
-
31Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed. New York: Perason Education; 2007.
-
32Wang C, Schimd CH, Fielding RA, Harvey WF, Reid KF, Price LL, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ. 2018;21(360):k851.
-
33Mannerkorpi K, Ahlmen M, Ekdahl C. Six- and 24-month follow-up of pool exercise therapy and education for patients with fibromyalgia. Scand J Rheumatol. 2002;31(5):306-10.
-
34Gowans SE, Dehueck A, Voss S, Silaj A, Abbey SE. Six-month and one-year follow-up of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Rheum. 2004 15;51(6):890-8.
-
35Chalaye P, Goffaux P, Lafrenaye S, Marchand S. Respiratory effects on experimental heat pain and cardiac activity. Pain Med. 2009;10(8):1334-40.
-
36Niederstrasser NG, Slepian PM, Mankovsky-Arnold T, Larivière C, Vlaeyen JW, Sullivan MJL. An experimental approach to examining psychological contributions to multisite musculoskeletal pain. J Pain. 2014;15(11):1156-65.
Publication Dates
-
Publication in this collection
15 May 2020 -
Date of issue
Jan-Mar 2020
History
-
Received
06 Nov 2019 -
Accepted
20 Mar 2020