Abstracts
The objective was to describe time trends in cervical cancer mortality rates in Brazil as a whole and in the country's major geographic regions and States from 1980 to 2009. This was an ecological time series study using data recorded in the Mortality Information System (SIM) and census data collected by the Brazilian Institute of Geography and Statistics (IBGE). Analysis of mortality trends was performed using Poisson regression. Cervical cancer mortality rates in Brazil tended to stabilize. In the geographic regions, a downward trend was observed in the South (-4.1%), Southeast (-3.3%), and Central-West (-1%) and an upward trend in the Northeast (3.5%) and North (2.7%). The largest decreases were observed in the States of São Paulo (5.1%), Rio Grande do Sul, Espírito Santo, and Paraná (-4.0%). The largest increases in mortality trends occurred in Paraíba (12.4%), Maranhão (9.8%), and Tocantins (8.9%). Cervical cancer mortality rates stabilized in the country as a whole, but there was a downward trend in three geographic regions and 10 States, while two geographic regions and another 10 States showed increasing rates.
Uterine Cervical Neoplasms; Mortality; Mortality Rate
O objetivo deste estudo foi fornecer um quadro quanto à tendência da mortalidade por câncer do colo de útero no Brasil, em suas regiões e estados, entre 1980 e 2009. Estudo ecológico de série temporal, com uso de informações sobre óbitos (Sistema de Informações sobre Mortalidade - SIM) e base demográfica (Instituto Brasileiro de Geografia e Estatística - IBGE). Foram realizadas análises das tendências da mortalidade por meio da regressão de Poisson. Houve estabilização nas taxas de mortalidade no Brasil. Nas regiões, houve queda no Sul (-4,1%), Sudeste (-3,3%) e Centro-Oeste (-1%); aumento no Nordeste (3,5%) e Norte (2,7%). As maiores reduções foram observadas em São Paulo (-5,1%), Rio Grande do Sul, Espírito Santo e Paraná (-4,0%). Os maiores aumentos foram observados na Paraíba (12,4%), Maranhão (9,8%) e Tocantins (8,9%). No Brasil, houve estabilização na mortalidade por câncer do colo do útero. No entanto, houve redução em 3 regiões e em 10 estados, enquanto, em 2 regiões e em outros 10 estados, a mortalidade segue aumentando. Uma das razões para essa disparidade pode ser o menor acesso ao tratamento para as pacientes de áreas menos desenvolvidas.
Neoplasias do Colo do Útero; Mortalidade; Coeficiente de Mortalidade
El objetivo fue analizar la mortalidad por cáncer de cuello de útero en Brasil, en sus macrorregiones y estados en el período de 1980 a 2009. Se trata de un estudio ecológico de serie temporal, con uso de información sobre óbitos del Sistema de Información sobre Mortalidad (SIM), y base demográfica del Instituto Brasileño de Geografía y Estadística (IBGE). Se realizaron análisis de las tendencias de la mortalidad, mediante la regresión de Poisson. En Brasil se observó la estabilización en las tasas de mortalidad. En las macrorregiones, hubo caída en el Sur (-4,1%), Sudeste (-3,3%) y Centro-Oeste (-1%); aumento en el Nordeste (3,5%) y Norte (2,7%). En los estados, las principales caídas fueron observadas en São Paulo (-5,1%), Rio Grande do Sul, Espírito Santo y Paraná (-4%). Los mayores aumentos se observaron en Paraíba (12,4%), Maranhão (9,8%) y Tocantins (8,9%). Conclusión: Brasil presenta estabilización en las tasas de mortalidad. No obstante, hubo una reducción en 3 macrorregiones y en 10 estados, mientras que en 2 macrorregiones y en 10 estados la mortalidad sigue aumentando. Una de las razones para esa disparidad puede ser el menor acceso al tratamiento para las pacientes de áreas menos desarrolladas.
Neoplasias del Cuello Uterino; Mortalidad; Tasa de Mortalidad
ARTICLE ARTIGO
Cervical cancer mortality trends in Brazil: 1980-2009
Tendência da mortalidade por câncer do colo do útero no Brasil: 1980 a 2009
Tendencia de la mortalidad por cáncer del cuello de útero en Brasil: 1980 a 2009
Carolina Maciel Reis GonzagaI; Ruffo Freitas-JuniorI,II; Aline Almeida BarbarescoII; Edesio MartinsIII; Bruno Teixeira BernardesIV; Ana Paula Magalhães ResendeV
IPrograma de Mastologia, Universidade Federal de Goiás, Goiânia, Brasil
IIInstituto de Patologia Tropical e Saúde Pública Universidade Federal de Goiás, Goiânia, Brasil
IIIDepartamento de Medicina, Pontifícia Universidade Católica de Goiás, Goiânia, Brasil
IVDepartamento de Ginecologia e Obstetrícia, Universidade Federal de Uberlândia, Uberlândia, Brasil
VDepartamento de Ginecologia, Universidade Federal de São Paulo, São Paulo, Brasil
Correspondence Correspondence A. P. M. Resende Departamento de Ginecologia, Universidade Federal de São Paulo. Rua Napoleão de Barros 715, 7º andar, São Paulo, SP 04024-002, Brasil. anapaulamrb@faefi.ufu.br
ABSTRACT
The objective was to describe time trends in cervical cancer mortality rates in Brazil as a whole and in the country's major geographic regions and States from 1980 to 2009. This was an ecological time series study using data recorded in the Mortality Information System (SIM) and census data collected by the Brazilian Institute of Geography and Statistics (IBGE). Analysis of mortality trends was performed using Poisson regression. Cervical cancer mortality rates in Brazil tended to stabilize. In the geographic regions, a downward trend was observed in the South (-4.1%), Southeast (-3.3%), and Central-West (-1%) and an upward trend in the Northeast (3.5%) and North (2.7%). The largest decreases were observed in the States of São Paulo (5.1%), Rio Grande do Sul, Espírito Santo, and Paraná (-4.0%). The largest increases in mortality trends occurred in Paraíba (12.4%), Maranhão (9.8%), and Tocantins (8.9%). Cervical cancer mortality rates stabilized in the country as a whole, but there was a downward trend in three geographic regions and 10 States, while two geographic regions and another 10 States showed increasing rates.
Uterine Cervical Neoplasms; Mortality; Mortality Rate
RESUMO
O objetivo deste estudo foi fornecer um quadro quanto à tendência da mortalidade por câncer do colo de útero no Brasil, em suas regiões e estados, entre 1980 e 2009. Estudo ecológico de série temporal, com uso de informações sobre óbitos (Sistema de Informações sobre Mortalidade SIM) e base demográfica (Instituto Brasileiro de Geografia e Estatística IBGE). Foram realizadas análises das tendências da mortalidade por meio da regressão de Poisson. Houve estabilização nas taxas de mortalidade no Brasil. Nas regiões, houve queda no Sul (-4,1%), Sudeste (-3,3%) e Centro-Oeste (-1%); aumento no Nordeste (3,5%) e Norte (2,7%). As maiores reduções foram observadas em São Paulo (-5,1%), Rio Grande do Sul, Espírito Santo e Paraná (-4,0%). Os maiores aumentos foram observados na Paraíba (12,4%), Maranhão (9,8%) e Tocantins (8,9%). No Brasil, houve estabilização na mortalidade por câncer do colo do útero. No entanto, houve redução em 3 regiões e em 10 estados, enquanto, em 2 regiões e em outros 10 estados, a mortalidade segue aumentando. Uma das razões para essa disparidade pode ser o menor acesso ao tratamento para as pacientes de áreas menos desenvolvidas.
Neoplasias do Colo do Útero; Mortalidade; Coeficiente de Mortalidade
RESUMEN
El objetivo fue analizar la mortalidad por cáncer de cuello de útero en Brasil, en sus macrorregiones y estados en el período de 1980 a 2009. Se trata de un estudio ecológico de serie temporal, con uso de información sobre óbitos del Sistema de Información sobre Mortalidad (SIM), y base demográfica del Instituto Brasileño de Geografía y Estadística (IBGE). Se realizaron análisis de las tendencias de la mortalidad, mediante la regresión de Poisson. En Brasil se observó la estabilización en las tasas de mortalidad. En las macrorregiones, hubo caída en el Sur (4,1%), Sudeste (3,3%) y Centro-Oeste (1%); aumento en el Nordeste (3,5%) y Norte (2,7%). En los estados, las principales caídas fueron observadas en São Paulo (5,1%), Rio Grande do Sul, Espírito Santo y Paraná (4%). Los mayores aumentos se observaron en Paraíba (12,4%), Maranhão (9,8%) y Tocantins (8,9%). Conclusión: Brasil presenta estabilización en las tasas de mortalidad. No obstante, hubo una reducción en 3 macrorregiones y en 10 estados, mientras que en 2 macrorregiones y en 10 estados la mortalidad sigue aumentando. Una de las razones para esa disparidad puede ser el menor acceso al tratamiento para las pacientes de áreas menos desarrolladas.
Neoplasias del Cuello Uterino; Mortalidad; Tasa de Mortalidad
Introduction
Uterine cervical cancer is the third most common type of cancer and the fourth cause of death from cancer in women worldwide, accounting for 9% (529,800) of all new cancer cases in women in 2008 and 8% (275,100) of all the deaths 1. More than 85% of cases and deaths occurred in developing countries, and the following are thus considered high-risk regions: East and West Africa (incidence > 30/100,000), South Africa (26.8/100,000), South-Central Asia (24.6/100,000), and South and Central America (23.0/100,000) 2. The incidence rates are lower in West Asia, North America, and Australia (< 6/100,000).
Most cases of cervical cancer are associated with extrinsic, environmental, and lifestyle factors 3. The principal risk factors associated with cervical cancer include human papillomavirus virus (HPV), early sexual initiation (< 16 years), numerous sex partners (more than four), genital warts, and smoking 4. This calls attention to the potential use of measures to avert these risk factors and thus decrease the incidence of cervical cancer. However, it is not easy to change a population's lifestyle, especially in the midst of poverty and insufficient schooling 3.
The advent of Pap smear screening some 50 years ago resulted in a 50-70% drop in mortality rates from cancer cervical 5.
According to the World Health Organization (WHO), 80% to 100% coverage of the target population with Pap smear screening and an organized network for adequate diagnosis and treatment would allow a 60% to 90% reduction in invasive cervical cancer 6. High cervical cancer rates in developing countries and in poor populations are due largely to lack of screening (which would allow early-stage detection) 1.
In the United States, the expected number of new cervical cancer cases in 2011 was 12,710, with an estimated 4,290 deaths 7. In Brazil, the expected number of new cases in 2012 is 17,540, with an estimated risk of 17 cases per 100 thousand women 8. There were a total of 5,063 reported deaths in 2009 (Departamento de Informática do SUS. http://www2.datasus.gov.br/DATASUS/index.php?area=0205, accessed on 14/May/2011). However, little is known about cervical cancer mortality trends in Brazil.
Mortality data allow continuous monitoring of vital events and the development of health indicators 9. The quality of data on deaths in Brazil was classified as average in 2000 10. However, there are considerable differences in the degree of data comprehensiveness in the records 8,11. Most of States in the North and Northeast regions present high levels of underreporting of deaths and a high proportion of ill-defined causes 12,13. Beginning in 2004, the Ministry of Health implemented the Program to Reduce the Percentage of Deaths with Ill-Defined Causes in the North and Northeast, and in 2008 it launched the implementation of verbal autopsy in Brazil as a method for investigation of deaths from ill-defined causes 14.
Importantly, verbal autopsy makes key contributions, including questions on family composition as well as occupation and habits like smoking and alcohol consumption. Insofar as possible, the family reports the disease history for the deceased individual. According to Article 77 of Brazil's Law 6,015 of December 31, 1973, amended by Law 6,216, of June 30, 1975, "No burial may be performed without a death certificate issued by the notary public of the place of death, having recorded the place of death, based on the physician's report, if there be one in said place, or else by two qualified persons who have witnessed or verified the death" 15. We should thus use verbal autopsies with caution; according to the WHO, this recourse is only justified when all other investigative methods have been attempted 6.
More detailed epidemiological knowledge on cervical cancer mortality in Brazil should provide a scientific basis for planning public policies and clinical trials that can be implemented in a more structured and effective way for early detection and treatment. The aim of this study was thus to analyze time trends in cervical cancer mortality in Brazil as a whole and in its major geographic regions and States from 1980 to 2009.
Methods
Study design
This was an ecological time series study using data on deaths from cervical cancer in Brazilian women from 1980 to 2009.
Study area
Brazil, located in South America, has a total territory of 8,514,876km2, with a political and administrative division comprising 26 States and the Federal district, distributed in five major geographic regions (South, Southeast, Central-West, North, and Northeast) which display different human development indices or HDI (Instituto Brasileiro de Geografia and Estatística. http://www.ibge.gov.br, accessed on Mar/2012).
The Brazilian population in 2010 was 190,755,799, with 96.0 men for every 100 women and a mean population density of 22.5 inhabitants per square kilometer (Instituto Brasileiro de Geografia and Estatística. http://www.ibge.gov.br, accessed on Mar/2012).
Data collection and analysis
Data on deaths from cervical cancer were collected from the Mortality Information System or SIM (Departamento de Informática do SUS. http://www2.datasus.gov.br/DATASUS/index.php?area=0205, accessed on 14/May/2011). Population data were obtained from the Brazilian Institute of Geography and Statistics [Instituto Brasileiro de Geografia and Estatística IBGE] (http://www.ibge.gov.br).
The study included deaths from cervical cancer in Brazilian women over 20 years of age and excluded cases with unknown or missing age.
Statistical methods
The crude cervical cancer mortality rate was calculated as the number of deaths of residents divided by the total population residing in a given geographic area in the given year (x 100,000).
Age-standardized mortality was calculated using the indirect method, with a Segi world population as the reference 16.
Identification of significant changes in mortality trends used the Poisson regression model 17 based on Joinpoint, version 3.4.3 (National Cancer Institute; http://www.surveillance.cancer.gov/joinpoint). This study used a maximum number of 01 joinpoint. The trend in each period was described by obtaining the annual percent change (APC), with a 95% confidence interval (95%CI) and significance set at p < 0.05.
DATASUS, the Information Technology Department of the Brazilian Unified National Health System, makes available the databases from the SIM and the IBGE. These are secondary, public-domain data, so there was no need for approval by an Ethics and Research Committee.
Results
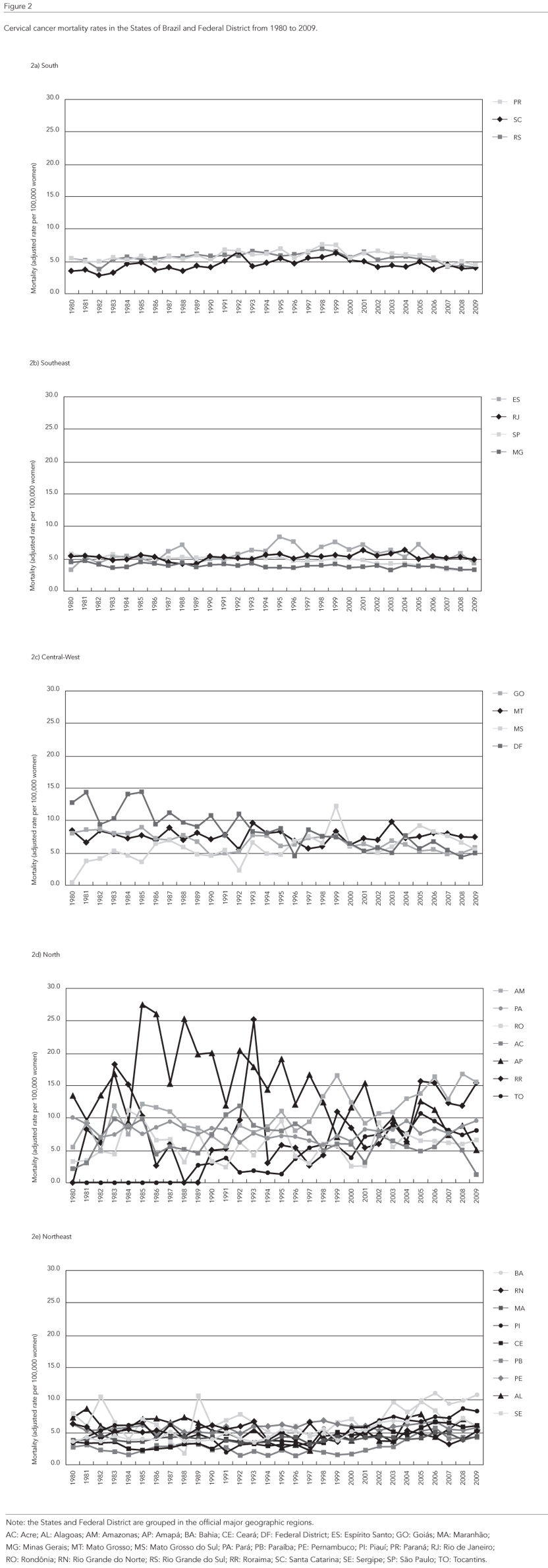
From 1980 to 2009, a total of 100,788 deaths from cervical cancer were reported in Brazilian women. The North was the region with the highest mortality coefficient (9.9/100,000 women), followed by the Central-West (8.6/100,000), South (6.7/100,000), Northeast (6.3/100,000), and Southeast (5.2/100,000) (Figure 1). In the States, the cervical cancer mortality rates showed the same profile as the respective regions, and the widest variations were seen in the States of the North (Figure 2).
The mortality trend analysis for Brazil as a whole showed a stabilization (Table 1), with APC varying from 0.2% (1980 to 2005) to 2.2%, without statistical significance until 2009. In the country's major geographic regions, there was a downward trend in the South (APC = -4.1%) beginning in 1999, Southeast (APC = -3.3%) from 2001 to 2009, and Central-West (APC = -1%) during the study period, while the Northeast (APC = 3.5%) and North (APC = 2.7%) showed an upward trend in mortality.
As for the mortality trends by State (Table 2), there was a significant downward trend in 10 States, São Paulo (APC = -5.1%), Rio Grande do Sul (APC = -4%), Espírito Santo (APC = -4%), Paraná (APC = 3.9%), Santa Catarina (APC = -3.4%), Distrito Federal (APC = -3.3%), Amapá (APC = -2.8%), Goiás (APC = -1.4%), Rio Grande do North (APC = -1%), and Minas Gerais (APC = -0.6%), and a non-significant reduction in Rio de Janeiro and Mato Grosso do Sul.
The States of Mato Grosso, Amazonas, Pará, Roraima, Tocantins, Maranhão, Piauí, Paraíba, Alagoas, and Ceará showed an increase in cervical cancer mortality, the worst of which in Paraíba (APC = 12.4%), Maranhão (APC = 9.8%), Tocantins (APC = 8.9%), and Piauí (APC = 6.6%).
Discussion
From 1980 to 2009, there was a sharp disparity in cervical cancer mortality among Brazilian women. These findings mirror the country's socioeconomic inequalities. It is widely acknowledged that access to primary care and Pap test coverage is lower among women with lower socioeconomic status 18,19. There is no precision related to access to diagnosis and treatment for these women, since mortality coefficients are heterogeneous in the various regions of Brazil.
The distribution of the hierarchical levels of care within Brazil's territory is unequal, showing a disparity between areas that have a well-structured urban network (in the Central and Southern regions), with the presence of well-fitted levels of care situated at regular intervals, and areas with an absence of some intermediate hierarchical levels (in the North and Northeast). The North and Central-West regions have a scarce health care system, where there is sparse occupation of the territory. Despite the consolidated occupation of the Northeast, cities there traditionally concentrate the supply of equipment and services, and there are few cases of intermediate level healthcare centers 20.
According to this study's findings, the Central-West, Southeast, and South of Brazil show a drop in cervical cancer mortality, while the North and Northeast show an upward trend. The States display the same heterogeneous profile, with the worst situations in Paraíba, Maranhão, and Tocantins, which rank low in human development, while the States with a higher human development index (HDI) showed a downward trend in mortality. Cervical cancer is in fact the most frequent type of cancer in the North (24/100,000). It ranks second in the Central-West (28/100,000) and Northeast (18/100,000), third in the Southeast (15/100,000), and fourth in the South (14/100,000) 21.
Specifically in the Central-West region, the Federal District shows downward cervical cancer mortality coefficients, while the rates practically stabilized in São Paulo and Rio de Janeiro. The level of development appears to be proceeding quite well in the Federal District, seat of the national capital, Brasilia. Meanwhile the South of Brazil showed a clear downward trend in all the States beginning in the year 2000.
These findings are consistent with the literature, since high cervical cancer mortality rates are expected in less developed regions. Meanwhile, there has been an important drop in mortality from this neoplasm in recent decades in developed countries like Finland, Iceland, Belgium, Scotland, and the United Kingdom, especially since the introduction of screening programs in the 1960 and 70s. Importantly, the above-mentioned countries have had organized cervical cancer screening programs for at least three decades 22,23.
Although the current study's findings point to high cervical cancer mortality in the North (9.9) and Central-West (8.6) of Brazil, the rates are low as compared to other Latin American countries such as Venezuela (15.2), Ecuador (18.6), Bolivia (22.2), Nicaragua (26.1) and Haiti (53.3) 24.
It is important to highlight the difficulties in obtaining a completely reliable scenario for cancer mortality in these countries, including Brazil. Although a population-based cancer registry was launched in recent years, there are persistent difficulties in producing high-quality data. Many cases of cervical cancer are still reported as "cancer of the uterus, part unspecified" 25. Due to these factors, a correction method was recently suggested for these data based on underreporting, in which rates of 4.6 and 5.1 deaths per 100,000 women were reported from 1996 to 2005 in Brazil. However, the correction increased these values by 103.4% 26. Another possible explanation for the observed disparity in cervical cancer mortality rates among Brazilian women could be the variation in exposure to risk factors and diagnostic practices.
Although mortality data in Brazil have improved in the majority of the States 11,13, only the Federal District and the States of Rio de Janeiro and São Paulo were classified as having "good" quality data in 2000. The other States of the Southeast had "satisfactory" data; those of the Central-West improved from "fair" to "satisfactory". Many States of the North and Northeast had no better than "fair" data, and some remained "deficient" 13. Thus, the findings for the Northeast should be interpreted with caution. In this sense, reliability and validity issues should be considered in the estimates of the Brazilian population, in addition to the limitations in the information on death, which can create biases in the mortality rates, particularly in women living in the North and Northeast regions of the country 12,27.
The year 2012 witnessed the publication of the document Brazilian Guidelines for Cervical Cancer Screening, with recommendations that incorporate the needs of various segments of society and that are feasible and usable by health centers and professionals 21. According to the National Cancer Institute (INCA), in 2012 in Brazil the Pap smear test was the priority screening strategy recommended by the Ministry of Health for women 25 to 59 years of age. An estimated 80% reduction in mortality from cervical cancer could be achieved by screening women in the 25 to 65-year age bracket with the Pap smear test and treatment of precursor lesions with a high potential for malignancy, or in situ carcinoma. This would require organization, comprehensiveness, and quality in the screening program, as well as follow-up of patients 21.
Furthermore, the Brazilian health system has low capacity for cervical cancer diagnosis. Proper capacity requires adequate collection of material from the uterine cervix for oncologic cytology (Papanicolaou), but especially the ability of the service to supply the test results 25,26. According to a survey of 89 hospitals and seven chemotherapy or radiotherapy services affiliated with a High Complexity Oncology Center (CACON), from 1995 to 2002, 45.5% of women presented cervical cancer in stages III or IV at the time of diagnosis 28. These data reflect problems in access to services and especially the lack of oncology centers outside the State capitals.
Finally, it is important to recall that cancer of the uterine cervix is among those with the greatest potential for cure and prevention when diagnosed early. The data presented here may be considered indicators for cervical cancer control in Brazil. They should certainly contribute to better planning of health actions, support, surveillance, and evaluation of interventions 29. Such results highlight the importance of priority-setting in primary and secondary prevention in less developed regions of the country. Thus, the current study's importance lies in having discussed the current state of cervical cancer mortality in the States of Brazil while providing information that can be useful in other countries.
Limitations
The use of mortality data from the SIM is conditioned on corrections due to the frequent undercounting of deaths in less developed areas. Importantly, the study excluded death records with the individual's age missing. Thus, the database may display sources of imprecision that are inherent to data collection, or to the methodology used to prepare population estimates. Meanwhile, use of the cervical cancer mortality rate is limited whenever there are a high proportion of deaths without medical care or due to ill-defined causes.
Contributors
A. P. M. Resende collaborated with the conceptualization of the study idea, writing of the manuscript, and final revision of the article. B. T. Bernardes participated in the conceptualization of the study idea and final revision of the article. R. Freitas-Junior contributed to the conceptualization of the study idea, statistical analysis, project management, and final revision of the article. A. A. Barbaresco collaborated with the writing of the manuscript and final revision of the article. E. Martins participated in the statistical analysis and final revision of the article. C. M. R. Gonzaga contributed to the conceptualization of the study idea, data collection, writing of the manuscript, and final revision of the article.
Submitted on 11/Jun/2012
Final version presented on 15/Sep/2012
Approved on 09/Oct/2012
- 1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011; 61:69-90.
- 2. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008: cancer incidence and mortality worldwide. Lyon: International Agency for Research on Cancer; 2010. (IARC CancerBase, 10).
- 3. Lima CA, Palmeira JAV, Cipolotti R. Fatores associados ao câncer do colo uterino em Propriá, Sergipe, Brasil. Cad Saúde Pública 2006; 22:2151-6.
- 4. Rama CH, Roteli-Martins CM, Derchain SFM, Oliveira EZ, Aldrighi JM, Mariani Neto C. Detecção sorológica de anti-HPV 16 e 18 e sua associação com os achados do Papanicolaou em adolescentes e mulheres jovens. Rev Assoc Med Bras 2006; 52:43-7.
- 5. Fahey MT, Irwing L, Macaskill P. Meta analysis of Pap test accuracy. Am J Epidemiol 1995; 141:680-9.
- 6. International Agency for Research on Cancer. World cancer report 2008. Lyon: International Agency for Research on Cancer; 2008.
- 7. National Cancer Institute. Estimated new cancer cases and deaths for 2011, all races, by sex. http://seer.cancer.gov/csr/1975_2008/results_single/sect_01_table.01.pdf (accessed on 16/Jun/2011).
- 8. Instituto Nacional de Câncer. Estimativa 2012: incidência de câncer no Brasil. Rio de Janeiro: Instituto Nacional de Câncer; 2012.
- 9. Frias PG, Pereira PMH, Andrade CLT, Lira PIC, Szwarcwald CL. Avaliação da adequação das informações de mortalidade e nascidos vivos no Estado de Pernambuco, Brasil. Cad Saúde Pública 2010; 26:671-81.
- 10. Mathers CD, Ma Fat D, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: An assessment of the global status of cause of death data. Bull World Health Organ 2005; 83:171-7.
- 11. Mello-Jorge MH, Laurenti R, Gotlieb SLD. Análise da qualidade das estatísticas vitais brasileiras: a experiência de implantação do SIM e do SINASC. Ciênc Saúde Coletiva 2007; 12:643-54.
- 12. Curado MP, Voti L, Sortino-Rachou AM. Cancer registration data and quality indicators in low and middle income countries: their interpretation and potential use for the improvement of cancer care. Cancer Causes Control 2009; 20:751-6.
- 13. Paes NA. Qualidade das estatísticas de óbitos por causas desconhecidas dos estados brasileiros. Rev Saúde Pública 2007; 41:436-45.
- 14. Campos D, França E, Loschi RH, Souza MFM. Uso da autópsia verbal na investigação de óbitos com causa mal definida em Minas Gerais, Brasil. Cad Saúde Pública 2010; 26:1221-33.
- 15. Fundação Nacional de Saúde. Textos de epidemiologia para vigilância ambiental em saúde. Brasília: Fundação Nacional de Saúde; 2002.
- 16. Doll R, Payne P, Waterhouse JAH, editors. Cancer incidence in five continents. v. I. Geneva: Union Internationale Contre le Cancer; 1966.
- 17. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19:335-51.
- 18. Martins LFL, Thuler LCS, Valente JG. Cobertura do exame de Papanicolaou no Brasil e seus fatores determinantes. Rev Bras Ginecol Obstet 2005; 27:485-92.
- 19. Albuquerque KM, Frias PG, Andrade CLT, Aquino EML, Menezes G, Szwarcwald CL. Cobertura do teste de Papanicolaou e fatores associados à não-realização: um olhar sobre o Programa de Prevenção do Câncer do Colo do Útero em Pernanmbuco, Brasil. Cad Saúde Pública 2009; 25 Suppl 2:S301-9.
- 20. Instituto Brasileiro de Geografia e Estatística. Regiões de influência das cidades, 2007. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2008.
- 21. Instituto Nacional de Câncer. Diretrizes brasileiras para o rastreamento do câncer do colo do útero. Rio de Janeiro: Instituto Nacional de Câncer; 2012.
- 22. Arbyn M, Raifu AO, Weiderpass E, Bray F, Antilla A. Trends of cervical cancer mortality in the member states of the European Union. Eur J Cancer 2009; 45:2640-8.
- 23. Klint A, Tryggvadóttir L, Bray F, Gislum M, Hakulinen T, Storm HH, et al. Trends in the survival of patients diagnosed with cancer in female genital organs in the Nordic countries 19642003 followed up to the end of 2006. Acta Oncol 2010; 49:632-43.
- 24. Arrossi S, Sankaranarayanan R, Parkin DM. Incidence and mortality of cervical cancer in Latin America. Salud Pública Méx 2003; 45 Suppl 3: 306-14.
- 25. Gamarra CJ, Valente JG, Silva GA. Magnitude da mortalidade por câncer do colo do útero na Região Nordeste do Brasil e fatores socioeconômicos. Rev Panam Salud Pública 2010; 28:100-6.
- 26. Gamarra CJ, Valente JG, Silva GA. Correction for reported cervical cancer mortality data in Brazil 1996-2005. Rev Saúde Pública 2010; 44:629-38.
- 27. Chatenoud L, Bertuccio P, Bosetti C, Levi F, Curado MP, Malvezzi M, et al. Trends in cancer mortality in Brazil, 1980-2004. Eur J Cancer Prev 2010; 19: 79-86.
- 28. Thuler LCS, Mendonça GA. Estadiamento inicial dos casos de câncer de mama e colo do útero em mulheres brasileiras. Rev Bras Ginecol Obstet 2005; 27:656-6.
- 29. Bittencourt SA, Camacho LAB, Leal MC. O Sistema de Informação Hospitalar e sua aplicação na saúde coletiva. Cad Saúde Pública 2006; 22:19-30.
Publication Dates
-
Publication in this collection
20 Mar 2013 -
Date of issue
Mar 2013
History
-
Received
11 June 2012 -
Accepted
09 Oct 2012 -
Reviewed
15 Sept 2012