LEARNING BY IMAGES
Contact lens use with intraestromal hemorrhage secondary to corneal neovascularization
Thiago Gonçalves dos Santos MartinsI; Ana Luiza Fontes de Azevedo CostaII; Milton Ruiz AlvesIII; Maristella Mendes GonçalvesIV
IDepartment of Ophthalmology, Universidade Federal de São Paulo - UNIFESP, São Paulo (SP), Brazil
IIHospital Federal dos Servidores do Estado - Rio de Janeiro (RJ), Brazil
IIICorneal Service, Universidade de São Paulo - USP, São Paulo (SP), Brazi
IVClinica oftalmológica Rosai, Rio de Janeiro (RJ), Brazil
Corresponding author Corresponding author: Thiago Gonçalves dos Santos Martins Universidade Federal de São Paulo - UNIFESP - Departamento de Oftalmologia Rua Botucatu, 821 Zip code: 04023-062 - São Paulo (SP), Brazil Phone: (55 11) 96456-2182 Email: thiagogsmartins@yahoo.com.br
Click to enlarge

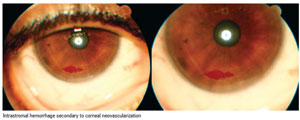
A 35 years old man who weared soft contact lenses for 5 years, was found to have superficial stromal corneal neovascularization less than 2mm from the limbus since his first visit, 3 months before. He presented during a routine examination an asymptomatic intrastromal hemorrhage due to rupture of neovessels into the cornea.
Almos all of oxygen delivered to corneal metabolism is supplied by atmosphere and is diffused by the lacrimal film, being the endothelium supplied by the aqueous humor. The lens movement and the oxygenated tears circulation behind the lens are important mechanisms that provide oxygen to the cornea. A contact lens can change the tears normal circulation, causing mechanical and hypoxic injury to the tissues and may adhere to proteins and residues that are kept in contact to the ocular surface. Long term contact lens wear, poor hygiene and incorrect adaptation are risk factors that lead to complications(1).
If the oxygen supply to the cornea is significantly reduced the normal metabolic activity is adversely affected, causing corneal edema. Prolonged and important edema may cause serious complications like loss of transparency and corneal neovascularization(2).
The appearance of blood vessels in the cornea may be due to chronic hypoxia (low water content, dense, tight contact lenses or extended wear), chronic trauma by contact lens, chronic inflammation and epithelial defect. It is often asymptomatic(3).
In response to hypoxia the tissue releases proangiogenesis growing factor and cytokines which spread to the nearest endothelial cells. The stimulated receptors in the endothelial cells start a protheases cascade production that result in extracellular matrix degradation. Endothelial cells, once activated, proliferate and move towards the growing factors. Finally, cells stop their proliferation and start to organize into tubules. Pericytes and smooth muscle cells begin to the involve neovessels aiming to keep them stabilized and turning them into mature blood vessels(4).
The superficial peripheral neovascularization <1.5mm is common in contact lens myopic users and must be followed-up(4). Blood vessels of the limbus that invade the cornea more than 1.5mm are considered abnormal. Deep and superficial stroma may be involved with risk of intrastromal hemorrhage and scar formation. When blood vessels are deep and >2mm the use of contact lenses must be discontinued, or the use of rigid gas permeable contact lenses of high Dk should be adapted
Contact lens use with intraestromal hemorrhage 525 if it is not possible to suspend the lenses use. The long term and continuous wear should be contraindicated. If vascularization <2mm it is necessary to adjust a thinner lens, with more water content or a silicone hydrogel, or even, a rigid gas permeable lens is recommended(3).
Received on: Jul 15, 2012
Accepted on: Sep 26, 2012
- 1. Kanski JJ. Oftalmologia clínica: uma abordagem sistemática. 6a ed. Rio de Janeiro: Elsevier; 2008. p. 310-2.
- 2. Zakaria N, Van Grasdorff S, Wouters K, Rozema J, Koppen C, Lion E, et al. Human tears reveal insights into corneal neovascularization. PLoS One. 2012;7(5):e36451.
- 3. Netto AL, Coral-Ghanem C, Oliveira PR. Série oftalmologia brasileira. 2a ed. Rio de Janeiro: Guanabara Koogan; 2011. Lentes de Contato. p. 386.
- 4. Holden BA, Mertz GW, McNally JJ. Corneal swelling response to contact lenses worn under extended wear conditions. Invest Ophthalmol Vis Sci. 1983;24(2):218-23.
Publication Dates
-
Publication in this collection
22 Jan 2013 -
Date of issue
Dec 2012