ABSTRACT
Objective:
Minimally invasive techniques are used increasingly by virtue of advancements in technology. Surgery for prostate cancer, which has high morbidity, is performed with an increasing momentum based on the successful oncological and functional outcomes as well as cosmetic aspects.
Materials and methods:
Sixty two patients underwent robot-assisted perineal radical prostatectomy (R-PRP) surgery at our clinic between November 2016 and August 2017. Six pelvimetric dimensions were defined and measured by performing multiparametric magnetic resonance imaging (mpMRI) prior to operation in all patients. In light of these data, we aimed to investigate the effect of pelvimetric measurements on surgery duration and surgical margin positivity.
Results:
By using this technique in pelvic area, we observed that measurements only representing surgical site and excluding other pelvic organs had a significant effect on surgery duration, and pelvic dimensions had no significant effect on surgical margin positivity.
Conclusion:
In R-PRP technique, peroperative findings and oncological outcomes can vary depending on several variable factors, but although usually not taken into account, pelvimetric measurements can also affect these outcomes. However, there is a need for randomised controlled trials to be conducted with more patients.
Keywords:
Prostatic Neoplasms; Prostatectomy; Perineum
INTRODUCTION
As the prostate anatomy and distribution of neurovascular bundle (NVB) have been better understood, radical prostatectomy has become increasingly used as part of multimodal treatment to eradicate the disease in local-stage cancer and high-risk prostate cancer (11. Bianco FJ Jr, Scardino PT, Eastham JA. Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function (“trifecta”). Urology. 2005;66(5 Suppl):83-94.). While radical prostatectomy results in eradication of disease, open, laparoscopic or robot-assisted radical prostatectomy (RALP) can be performed by considering benefits and side effects of the technique (22. Yaxley JW, Coughlin GD, Chambers SK, Occhipinti S, Samaratunga H, Zajdlewicz L, et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet. 2016;388:1057-1066. Erratum in: Lancet. 2017;389:e5.). According to literature findings, pelvic dimensions were determined to be an important impact factor in oncological and functional outcomes of surgical methods used. Apical prostate depth is an important impact factor for laparoscopic radical prostatectomy (LRP) and retropubic radical prostatectomy (RRP) (33. Matikainen MP, von Bodman CJ, Secin FP, Yunis LH, Vora K, Guillonneau B, et al. The depth of the prostatic apex is an independent predictor of positive apical margins at radical prostatectomy. BJU Int. 2010;106:622-6.). Another important study showed that the pelvic diameter measurements were not predictive of improvement in erectile function in patients underwent RRP (44. von Bodman C, Matikainen MP, Favaretto RL, Matsushita K, Mulhall JP Eastham JA, et al. Pelvimetric dimensions do not impact upon nerve sparing or erectile function recovery in patients undergoing radical retropubic prostatectomy. J Sex Med. 2011;8:567-74.). Based on the evidence from studies of RALP method, pelvimetric dimensions were proved to be ineffective for surgery duration, amount of bleeding, and recovery of potency and continence at 6-month follow-up of patients underwent this technique (55. Hong SK, Lee ST, Kim SS, Min KE, Hwang IS, Kim M, et al. Effect of bony pelvic dimensions measured by preoperative magnetic resonance imaging on performing robot-assisted laparoscopic prostatectomy. BJU Int. 2009;104:664-8.).
Unlike conventional methods, robot-assisted perineal radical prostatectomy (R-PRP) is performed through perineal approach. In addition, it has many advantages in patients with a history of major abdominal surgery and high body mass index. As this technique is performed below the endopelvic fascia and bladder neck level, anatomy and physiology created by several prior surgeries such as kidney transplantation or intestinal bypass systems for colorectal cancer can be maintained. Tugcu et al. performed this technique in 15 patients and reported that it can be safely performed in terms of oncological and functional outcomes (66. Tuğcu V, Akça O, Şimşek A, Yiğitbaşı İ, Şahin S, Taşçı Aİ. Robot-assisted radical perineal prostatectomy: first experience of 15 cases. Turk J Urol. 2017;43:476-83.). In this study, we aimed to investigate the effect of pelvimetric diameters measured preoperatively by multiparametric magnetic resonance imaging on peroperative findings and postoperative oncological outcomes.
MATERIALS AND METHODS
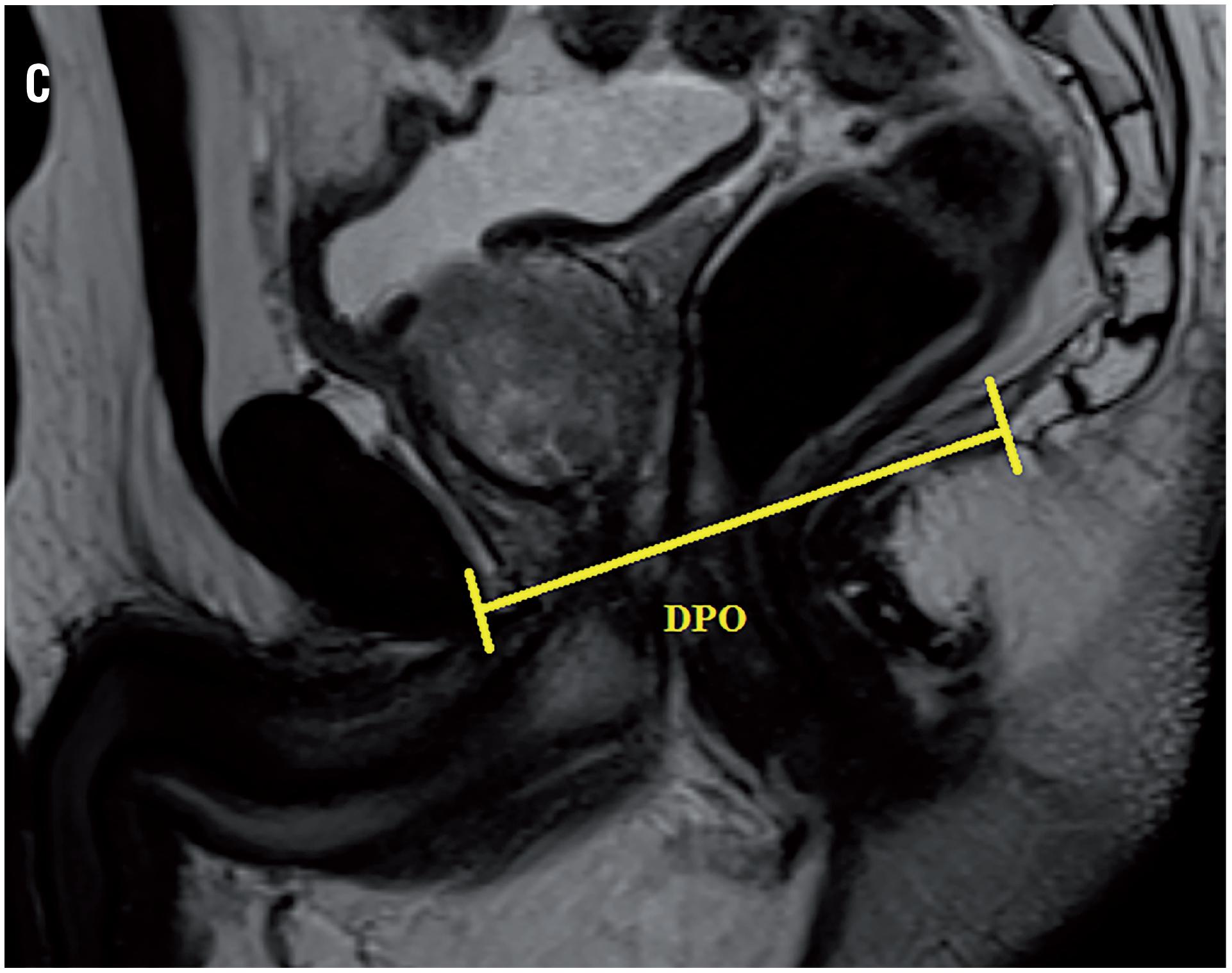
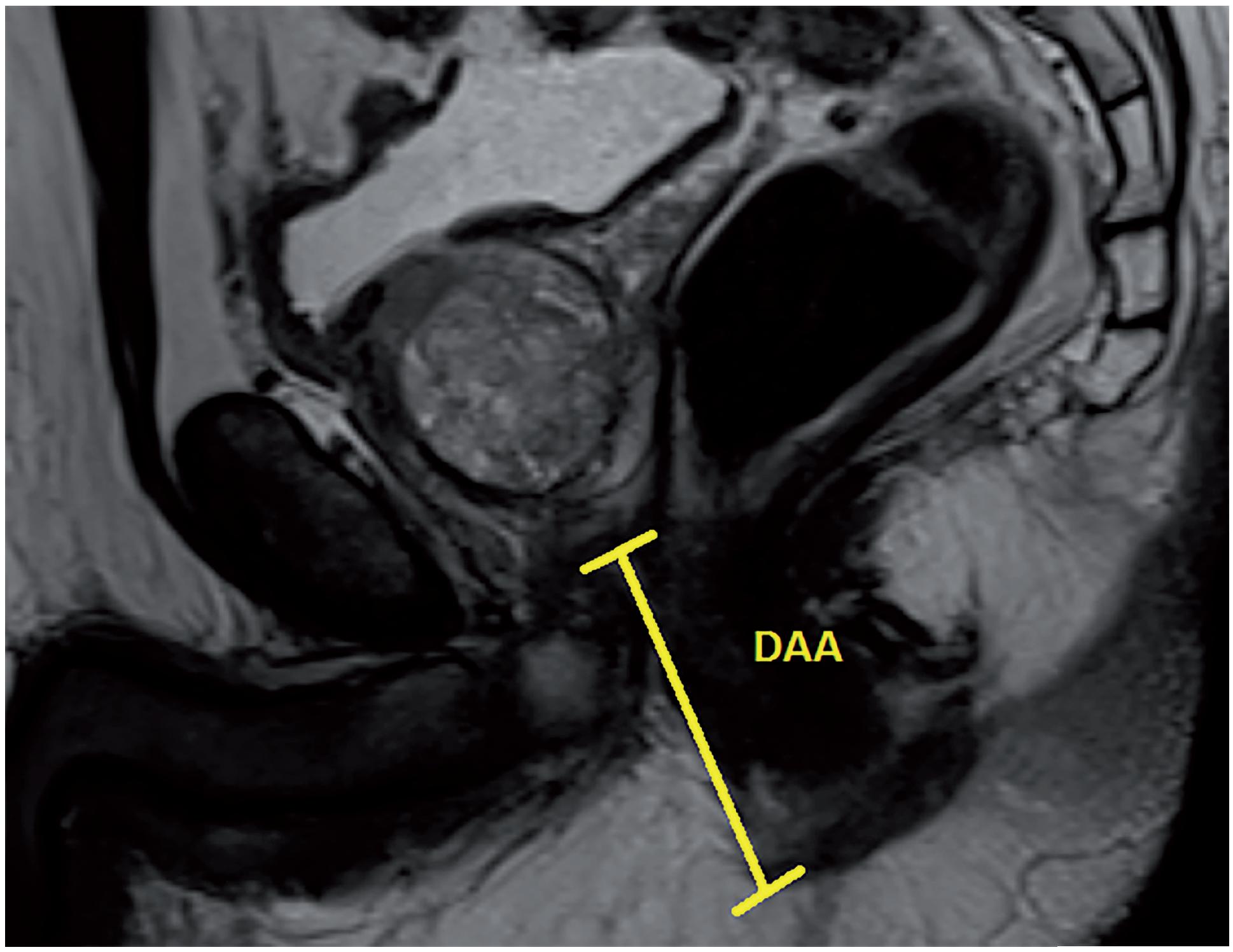
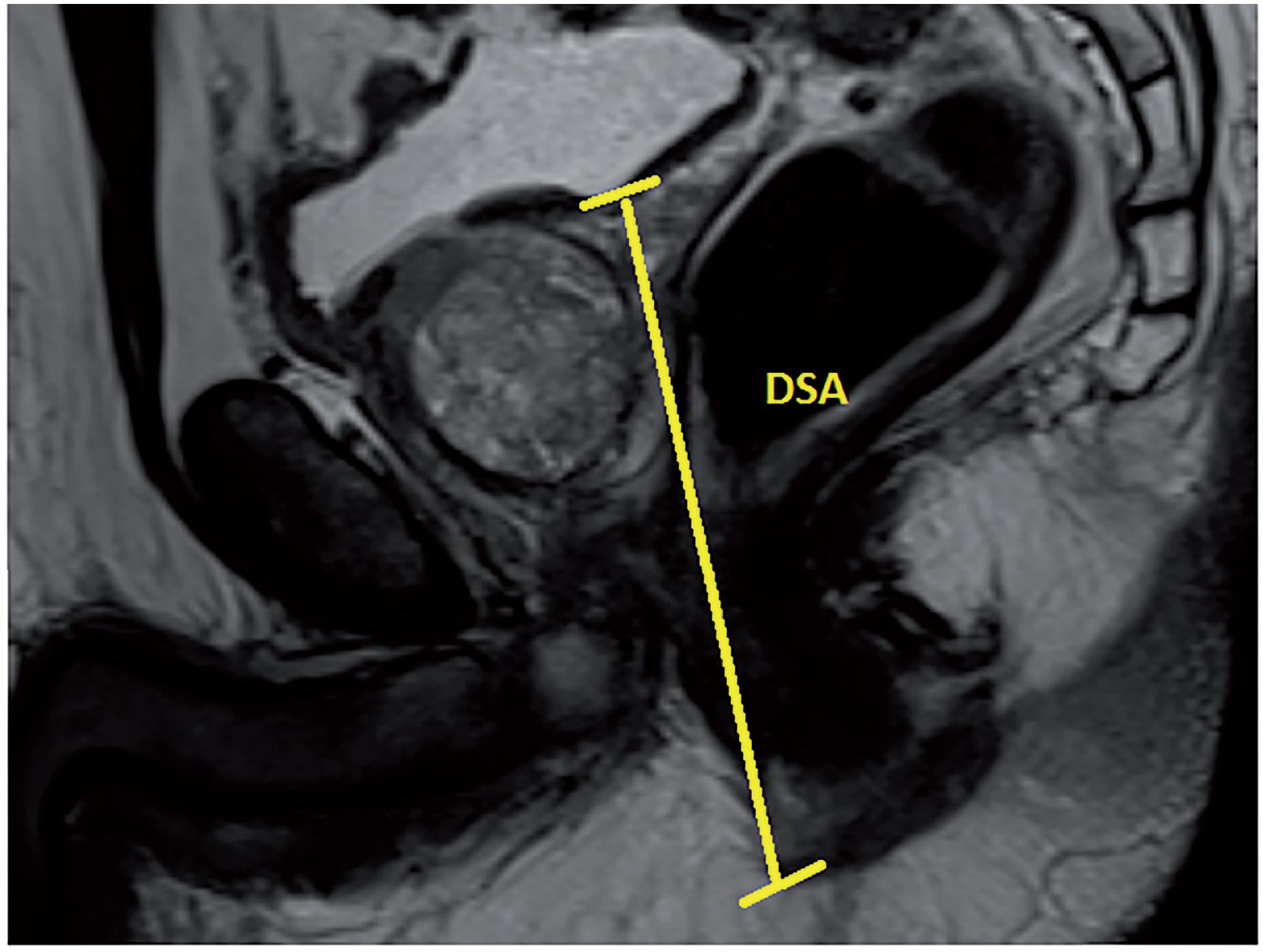
Based on our database collected prospectively, 62 patients received R-PRP treatment for prostate cancer between November 2016 and August 2017. All mpMRI images were obtained using 3 Tesla MRI machine (Magnetom Verio; Siemens, Erlanger, Germany). Sequences taken were T1--weighted axial and T2-weighted triplanar (axial, sagittal and coronal) and diffusion-weighted images (b values were calculated to be 0, 400, 800, 1400 and 1400). mpMRI did not reveal extraprostatic spread in any of the patients. We performed R-PRP method by placing a gel-port platform on the potential space, which was demarcated by rectourethral muscles and created by open perineal dissection, followed by robotic procedure. All the cases were performed by a single surgeon who has advanced experiences on robotic surgery. In our study, 6 pelvimetric dimensions were measured by an experienced radiologist. The first dimension consists narrowest distances between tips of the ischial spines (ISD) in T2-weighted axial images (Figure-1a). Unlike other techniques in R-PRP, surgery is performed in only minor pelvis with perineal approach. The second dimension is composed angle of the intersection of the straight lines extending from the tuber ischiadicum to the symphysis pubis (ASP) in the T2 weighted sequence coronal images (Figure-1b). We think that this angle represents the minor pelvis. The third dimension is the anteroposterior diameter of pelvic midplane between lower tip of the symphysis pubis and the coccyx representing the pelvic outlet (DPO) (Figure-1c). In other techniques, pelvic inlet and outlet are important because of the operation with abdominal approach, in R-PRP only pelvic outlet is important because technique is performed below endopelvic fascia level. The fourth dimension is the distance of the pelvic midplane from the anterior border of the anus to the apex of the prostate in sagittal images (DAA) (Figure-2a). The fifth dimension is the distance of the pelvic midplane from the anterior border of the anus to anterior border of the centre of seminal vesicles in sagittal images (DSA) (Figure-2b). The sixth dimension is the angle formed by the intersection of the axis passing through the lower and upper tips of the symphysis pubis and the axis intersecting of the seminal vesicles in cranio-caudal line on the sagittal midplane of pelvis (ASS) (Figure-2c). This angle represents the area below the level of endopelvic fascia when the rectum is excluded from the minor pelvis. In addition, prostate volume and body mass index of patients were measured and the effects of results on open perineal procedure time, console time and total operative time, and perioperative findings and postoperative oncological outcomes were examined.
Statistical analysis
Descriptive statistics were used to define continuous variables (mean, standard deviation, minimum, median, maximum). Multiple linear regression analysis was performed to examine the effect of independent variables on continuous dependent variables. Statistical significance level was considered to be 0.05. Analyses were performed using MedCalc Statistical Software version 12.7.7 (MedCalc Software bvba, Ostend, Belgium; 2013).
Surgical technique
In the first stage, surgery was initiated by performing an open perineal dissection. A potential space was created by extending the dissection into the rectourethral muscle fibres. GelPOINT® (Applied Medical, Rancho Santa Margarita, CA, USA) was placed on this space with the patient on 15-degree Trendelenburg and exaggerated lithotomy position. Three 8mm robotic trocars and one 12mm assistant trocar were placed on gel port. Trocar on 7 o'clock position was used for bipolar robotic arm and robotic trocar on 5 o'clock position was used for scissors and large needle robotic arm. Assistant trocar was placed on 6 o'clock position (Figure-3a). Robot was docked and robot-assisted perineal radical prostatectomy was performed using 3-arm Da Vinci Xi HD Surgical System (Intuitive Surgical, Inc., Sunnyvale, CA, USA). Prostate was released by dissecting lateral prostate lobes starting from apex dissection. Seminal vesicles were completely dissected. Urethra was cut following the dissection starting from dorsal plane. Urethral catheter removed from urethra was clipped with a Hem-o-Lock clip. Urethral catheter to be used for traction was cut below the clips by maintaining the insufflation of balloon. Dorsal veins were released by venous-preserving dissection. Prostatic pedicles were dissected and Hem-o-Lock® Clip (Teleflex Medical, Research Triangle Park, North Carolina, USA) was placed and cut (Figure-3b). Bladder neck was dissected and cut (Figure-3c). After completion of prostatectomy, vesicourethral anastomosis was performed by modified Van Veltoven technique using 2/4/V-Loc™ (Covidien, Mansfield, MA, ABD) sutures (Figure-3d).
RESULTS
Patient's preoperative demographics, peroperative and postoperative data and pelvimetric measurement results are summarised in Tables 1, 2, 3 and 4, respectively. Results show that the open perineal dissection time is affected by ASS and DSA dimensions during the first phase of surgery. An inverse proportion was observed with ASS (p=0.004), while a direct proportion was seen with DSA (p=0.013). Open perineal dissection time was increased 0.242-fold with a 1-degree decrease in ASS and 0.277-fold with a 1mm increase in DSA. No significant statistical relationship was observed between other measurements and open perineal dissection time. During the second phase of surgery, console time was observed to be affected inversely proportional to ASP (p=0.024) and ASS (p <0.001) dimensions. Console time was increased 1.040-fold with a 1-degree decrease in ASP and 0.845-fold with a 1-degree decrease in ASS. Total operative time was affected inversely proportional to ASP (p=0.031) and ASS (p <0.001) dimensions. It was increased 1.030-fold with a 1-degree decrease in ASP and 0.875-fold with a 1-degree decrease in ASS. Prostate volume did not cause a change in open perineal dissection time. Body mass index and prostate volume were not observed to have a statistical effect on console time and total operative time. Open perineal dissection time was found to be inversely proportional to body mass index of patient (p=0.038) and increased 0.974-fold with each increment in body mass index. Blood loss was observed to be affected inversely proportional to ASP (p=0.024) and ASS (p=0.003), and directly proportional to DSA (p=0.023). Blood loss was increased 1.456-fold with a 1-degree decrease in ASP, 1.758-fold with a 1-degree decrease in ASS and 1.160-fold with a 1-degree increase in DSA (Table-5).
DISCUSSION
Recently defined, R-PRP technique is performed by a different anatomic approach and unlike conventional radical prostatectomy techniques, it causes little to no damage to physiological system created by prior intraabdominal surgeries. It may overcome many difficulties and provides additional advantages in cases where surgical treatment is usually not preferred as a treatment option due to the additional morbidity caused by conventional methods. For example, anatomic problems, intestinal injury risk and dissection of intestinal adhesions to reach the prostate area are the main challenges faced by surgeons in patients with prior history of abdominal surgery. Therefore, serious negative effects can be observed in postoperative oncological and functional outcomes. This technique is also compliant with anatomy and physiology created by prior surgeries. For example, in patients with a history of surgery such as kidney transplantation, prostate-sparing radical cystectomy and orthotopic urinary diversion and intestinal bypass for malignancy, it maintains the physiology of these surgeries postoperatively. Many surgeons try to maintain the oncological and functional outcomes despite the additional morbidities caused by prior surgeries. Thus, R-PRP provides a great convenience for surgeons in these cases and helps them cope with such issues.
Unlike other methods, this technique is performed with an instrument manoeuvre capability of 540 degrees under the high-resolution image of robotic system at a different compartment in a narrow area. However, there may be some factors that can be considered as limitations of this technique such as different pelvimetric measurements obtained in individual patients. This technique combines open and robotic surgeries and thus, requires a good knowledge on the anatomy of lower abdomen and pelvic floor. Especially during the open perineal dissection phase, rectum and surrounding soft tissue injuries may occur and lead to a process that can cause mortality. Rectum is not completely dissected during open perineal dissection phase, but mostly dissected and completely separated from prostate during robotic surgery phase. Korman et al. reported a rectal injury rate of 1-11% in a series of open perineal radical prostatectomy, Amorim et al. reported a rectal injury risk of 2.2-2.4% in laparoscopic extraperitoneal radical prostatectomy and Tewari et al. reported a rectal injury rate of 0.5-1.5% in a series of robotic radical prostatectomy (77. Korman HJ, Mulholland TL, Huang R. Preservation of fecal continence and bowel function after radical perineal and retropubic prostatectomy: a questionnaire-based outcomes study. Prostate Cancer Prostatic Dis. 2004;7:249-52.–99. Tewari A, Sooriakumaran P, Bloch DA, Seshadri-Kreaden U, Hebert AE, Wiklund P. Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol. 2012;62:1-15.). No rectal injury was observed in our series of R-PRP. Although it is believed that surgeons may experience some difficulties with the narrowing of pelvic area, good knowledge on pelvic and perineal anatomy, high-resolution images of robotic system and high level of experience in robotic surgery play important roles in success of this surgery.
According to study conducted by Violette PD, blood loss, preoperative PSA, robot malfunction and prostate volume are independent factors that prolong the operative time in RALP. In addition, mean operative time was reported to be 187 minutes (1010. Violette PD, Mikhail D, Pond GR, Pautler SE. Independent predictors of prolonged operative time during roboticassisted radical prostatectomy. J Robot Surg. 2015;9:117-23.). While completion of learning curve by the surgeon is another important factor, prior history of surgery and BMI are other factors that should be considered. Our study included 62 cases and we believe that this number of cases is sufficient for completion of learning curve. Mean operative time in our study can be considered acceptable when compared to other techniques. When all these data are ignored, pelvimetric dimensions can also be suggested as independent predictive factors for R-PRP. In result of their evaluation on prostate volume in terms of RALP, Hong et al. reported that the surgery duration, but not the pelvimetric dimensions, can be considered as an independent predictor (1111. Hong SK, Lee ST, Kim SS, Min KE, Hwang IS, Kim M, et al. Effect of bony pelvic dimensions measured by preoperative magnetic resonance imaging on performing robot-assisted laparoscopic prostatectomy. BJU Int. 2009;104:664-8.). We believe that the pelvimetric measurement can have a high degree of significance if it covers surgical site only and excludes other organs in order to be considered as a predictive factor for the effect of pelvimetric dimensions on operative time. We assessed the operation in 3 phases individually when evaluating our technique based on the pelvimetric measurements. These were open perineal dissection, console time and total operative time. Among our pelvimetric measurements, ASS was found to be statistically significant for duration of all surgical procedures and each surgical phase became shorter individually with the increase in ASS. We believe that ASS significantly affects each phase as it only represents the surgical site where operation was performed. Our technique is performed in front of the rectum below the bladder neck and endopelvic fascia level using perineal approach. Therefore, while pelvic outlet can be a predictor, pelvic inlet cannot be a predictive factor because it is located completely outside the surgical site. ASP angle was found to be significant for total operative time and console time but with a lesser statistical significance compared to ASS since ASP angle included rectum and surrounding soft tissues. While DSA and BMI affect open perineal dissection time, these parameters do not affect other procedure times. As perineal approach was adopted, DSA particularly represents the mean length of prostate depth. This can be considered as a cause of its effect on open perineal dissection time.
Many studies revealed that the parameters such as BMI, prostate volume, intraabdominal pressure and patient's age at the time of robotic or laparoscopic radical prostatectomy are predictive factors for blood loss. Apart from these, it can be suggested that the pelvimetric measurements play a role in blood loss. Hong et al. reported that pelvimetric measurements do not affect the amount of blood loss in RALP operation but prostate volume is a predictive factor (1111. Hong SK, Lee ST, Kim SS, Min KE, Hwang IS, Kim M, et al. Effect of bony pelvic dimensions measured by preoperative magnetic resonance imaging on performing robot-assisted laparoscopic prostatectomy. BJU Int. 2009;104:664-8.). According to data of our study, ASS, ASP and DSA measurements have an effect on blood loss. Surgical site becomes broader with the increase in ASS and ASP and performance of radical prostatectomy becomes easier with R-PRP technique. Bleeding can be controlled more effectively with the increased manoeuvre capability at this broadened area. With the increase in DSA, operation is performed at a deeper site in perineal area, which results in increased levels of blood loss. Based on the literature, blood loss is known to be reduced in RALP technique compared to other methods. Consistent with the literature, mean blood loss during RALP surgery was measured to be 190cc in our study (1212. Ehieli EI, Howard LE, Monk TG, Ferrandino MN, Polascik TJ, Walther PJ, et al. Effect of positive end-expiratory pressure on blood loss during retropubic and robot-assisted laparoscopic radical prostatectomy. Int J Urol. 2016;23:674-8., 1313. Berge V, Berg RE, Hoff JR, Wessel N, Diep LM, Karlsen SJ, et al. A prospective study of transition from laparoscopic to robot-assisted radical prostatectomy: quality of life outcomes after 36-month follow-up. Urology. 2013;81:781-6.). For R-PRP technique, positive pressure on a narrow area, high-level robotic optical resolution and lack of need for dorsal vein complex dissection and ligation below the endopelvic fascia level are among the most important factors that reduce blood loss.
In the literature, Matikainen MP et al. reported that apical depth is an independent predictive factor for positive apical surgical margin (1414. Matikainen MP, von Bodman CJ, Secin FP, Yunis LH, Vora K, Guillonneau B, et al. The depth of the prostatic apex is an independent predictor of positive apical margins at radical prostatectomy. BJU Int. 2010;106:622-6.). Tozawa et al. reported the rate of surgical margin as 26% in their series of RALP (1515. Tozawa K, Yasui T, Umemoto Y, Mizuno K, Okada A, Kawai N, et al. Pitfalls of robot-assisted radical prostatectomy: a comparison of positive surgical margins between robotic and laparoscopic surgery. Int J Urol. 2014;21:976-9.). Positive surgical margin rates of our series are consistent with literature. We determined that the pelvimetric diameter is not an independent predictive factor for surgical margin positivity in R-PRP technique. We believe that R-PRP can be safely performed without increasing surgical margin positivity regardless of pelvimetric measurements in localised prostate cancer.
The technique we performed is a novel and developing method. Some of the dimensions evaluated were overall pelvimetric dimensions, while others were dimensions defined by us to represent the surgical site only. We showed that some pelvimetric measurements can be considered as predictive factors for surgery duration. Number of patients can be considered as the limitation of this study.
CONCLUSIONS
In R-PRP technique, peroperative findings and oncological outcomes can vary depending on several variable factors, but although usually not taken into account, pelvimetric measurements can also affect these outcomes. However, there is a need for randomised controlled trials to be conducted with large series of patients.
-
ABBREVIATIONS
- R-PRP Robot-assisted radical perineal prostatectomy
- mpMRI Multiparametric magnetic resonance imaging
- NVB Neurovascular bundle
- RALP robot-assisted radical prostatectomy
- LRP Laparoscopic radical prostatectomy
- RRP Retropubic radical prostatectomy
- ISD Distance of the ischial spines
- ASP Angle of symphysis pubis
- DPO Distance of pelvic outlet
- DAA Distance between prostate apex and anus
- DSA Distance between seminal vesicles and anus
- ASS Angle of symphysis pubis-seminal vesicles
- BMI Body mass index
REFERENCES
-
1Bianco FJ Jr, Scardino PT, Eastham JA. Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function (“trifecta”). Urology. 2005;66(5 Suppl):83-94.
-
2Yaxley JW, Coughlin GD, Chambers SK, Occhipinti S, Samaratunga H, Zajdlewicz L, et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet. 2016;388:1057-1066. Erratum in: Lancet. 2017;389:e5.
-
3Matikainen MP, von Bodman CJ, Secin FP, Yunis LH, Vora K, Guillonneau B, et al. The depth of the prostatic apex is an independent predictor of positive apical margins at radical prostatectomy. BJU Int. 2010;106:622-6.
-
4von Bodman C, Matikainen MP, Favaretto RL, Matsushita K, Mulhall JP Eastham JA, et al. Pelvimetric dimensions do not impact upon nerve sparing or erectile function recovery in patients undergoing radical retropubic prostatectomy. J Sex Med. 2011;8:567-74.
-
5Hong SK, Lee ST, Kim SS, Min KE, Hwang IS, Kim M, et al. Effect of bony pelvic dimensions measured by preoperative magnetic resonance imaging on performing robot-assisted laparoscopic prostatectomy. BJU Int. 2009;104:664-8.
-
6Tuğcu V, Akça O, Şimşek A, Yiğitbaşı İ, Şahin S, Taşçı Aİ. Robot-assisted radical perineal prostatectomy: first experience of 15 cases. Turk J Urol. 2017;43:476-83.
-
7Korman HJ, Mulholland TL, Huang R. Preservation of fecal continence and bowel function after radical perineal and retropubic prostatectomy: a questionnaire-based outcomes study. Prostate Cancer Prostatic Dis. 2004;7:249-52.
-
8Amorim GL, Cruz GM, Veloso DF, Kartabil JD, Vieira JC, Alves PR. Comparative analysis of radical prostatectomy techniques using perineal or suprapubic approach in the treatment of localized prostate cancer. Einstein (Sao Paulo). 2010;8:200-4.
-
9Tewari A, Sooriakumaran P, Bloch DA, Seshadri-Kreaden U, Hebert AE, Wiklund P. Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol. 2012;62:1-15.
-
10Violette PD, Mikhail D, Pond GR, Pautler SE. Independent predictors of prolonged operative time during roboticassisted radical prostatectomy. J Robot Surg. 2015;9:117-23.
-
11Hong SK, Lee ST, Kim SS, Min KE, Hwang IS, Kim M, et al. Effect of bony pelvic dimensions measured by preoperative magnetic resonance imaging on performing robot-assisted laparoscopic prostatectomy. BJU Int. 2009;104:664-8.
-
12Ehieli EI, Howard LE, Monk TG, Ferrandino MN, Polascik TJ, Walther PJ, et al. Effect of positive end-expiratory pressure on blood loss during retropubic and robot-assisted laparoscopic radical prostatectomy. Int J Urol. 2016;23:674-8.
-
13Berge V, Berg RE, Hoff JR, Wessel N, Diep LM, Karlsen SJ, et al. A prospective study of transition from laparoscopic to robot-assisted radical prostatectomy: quality of life outcomes after 36-month follow-up. Urology. 2013;81:781-6.
-
14Matikainen MP, von Bodman CJ, Secin FP, Yunis LH, Vora K, Guillonneau B, et al. The depth of the prostatic apex is an independent predictor of positive apical margins at radical prostatectomy. BJU Int. 2010;106:622-6.
-
15Tozawa K, Yasui T, Umemoto Y, Mizuno K, Okada A, Kawai N, et al. Pitfalls of robot-assisted radical prostatectomy: a comparison of positive surgical margins between robotic and laparoscopic surgery. Int J Urol. 2014;21:976-9.
Publication Dates
-
Publication in this collection
30 Mar 2020 -
Date of issue
May-Jun 2020
History
-
Received
27 June 2019 -
Accepted
13 Oct 2019 -
Published
30 Dec 2019