ABSTRACT
Purpose:
Vesicorectal fistula is one of the most devastating postoperative complications after radical prostatectomy. Definitive treatment is difficult due to morbidity and recurrence. Despite many options, there is not an unanimous accepted approach. This article aimed to report a new minimally invasive approach as an option to reconstructive surgery.
Materials and Methods:
We report on Transanal Minimally Invasive Surgery (TAMIS) with miniLap devices for instrumentation in a 65 year old patient presenting with vesicorectal fistula after radical prostatectomy. We used Alexis® device for transanal access and 3, 5 and 11 mm triangulated ports for the procedure. The surgical steps were as follows: cystoscopy and implant of guide wire through fistula; patient at jack-knife position; transanal access; Identification of the fistula; dissection; vesical wall closure; injection of fibrin glue in defect; rectal wall closure.
Results:
The operative time was 240 minutes, with 120 minutes for reconstruction. No perioperative complications or conversion were observed. Hospital stay was two days and catheters were removed at four weeks. No recurrence was observed.
Conclusions:
This approach has low morbidity and is feasible. The main difficulties consisted in maintaining luminal dilation, instrumental manipulation and suturing.
Key words:
Fistula; Postoperative Complications; Natural Orifice Endoscopic Surgery
INTRODUCTION
Vesicorectal fistula consists of an abnormal communication between the bladder urothelium and rectal mucosa, which represents a devastating condition. Diverticulitis, Crohn's disease and cancer are the most common etiologies (11. Morse FP 3rd, Dretler SP. Diagnosis and treatment of colovesical fistula. J Urol. 1974;111:22-4.–55. Walker KG, Anderson JH, Iskander N, McKee RF, Finlay IG. Colonic resection for colovesical fistula: 5-year follow-up. Colorectal Dis. 2002;4:270-4.). Vesicorectal fistula is an extremely rare complication following radical prostatectomy.
Patients may present with irritative urinary symptoms, urinary tract infection, pneumaturia, fecaluria and tenesmus (11. Morse FP 3rd, Dretler SP. Diagnosis and treatment of colovesical fistula. J Urol. 1974;111:22-4., 66. Pontari MA, McMillen MA, Garvey RH, Ballantyne GH. Diagnosis and treatment of enterovesical fistulae. Am Surg. 1992;58:258-63., 77. Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg. 2004;188:617-21.). Cystoscopy and tomography are the most accurate tests to confirm the diagnosis (11. Morse FP 3rd, Dretler SP. Diagnosis and treatment of colovesical fistula. J Urol. 1974;111:22-4., 77. Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg. 2004;188:617-21.). Non- surgical watchful waiting is an option in selected cases (88. Amin M, Nallinger R, Polk HC Jr. Conservative treatment of selected patients with colovesical fistula due to diverticulitis. Surg Gynecol Obstet. 1984;159:442-4.). Drug therapy such as antibiotics, intravenous total parenteral nutrition and bowel rest may be used in patients with few symptoms and non-toxemic and non-malignant etiology (99. Evans JP, Steinhart AH, Cohen Z, McLeod RS. Home total parenteral nutrition: an alternative to early surgery for complicated inflammatory bowel disease. J Gastrointest Surg. 2003;7:562-6.). Proximal colostomy and urinary catheterization are options in poorly responsive or very symptomatic patients. Definitive treatment aiming to separate the organs and close the defect with preservation of function is recommended in the absence of infection or obstruction. Partial resection and interposition of omentum between suture lines may be required. It can be done in stages. (11. Morse FP 3rd, Dretler SP. Diagnosis and treatment of colovesical fistula. J Urol. 1974;111:22-4., 77. Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg. 2004;188:617-21., 1010. Shackley DC, Brew CJ, Bryden AA, Anderson ID, Carlson GL, Scott NA, et al. The staged management of complex entero-urinary fistulae. BJU Int. 2000;86:624-9.).
Definitive treatment is challenging due to the morbidity of the classic techniques and the high recurrence rate. Currently we prefer traditional approaches like transanal, transabdominal, trans-sphincteric and transperineal (1111. Hechenbleikner EM, Buckley JC, Wick EC. Acquired rectourethral fstulas in adults: a systematic review of surgical repair techniques and outcomes. Dis Colon Rectum. 2013;56:374-83.). However, there is not an universally accepted approach. Techniques described for minimally invasive repair such as laparoscopic transperitoneal approach can reduce the morbidity of treatment and was recently described with good results (1212. Wilbert DM, Buess G, Bichler KH. Combined endoscopic closure of rectourethral fistula. J Urol. 1996;155:256-8.–1414. Sotelo R, Mirandolino M, Trujillo G, Garcia A, de Andrade R, Carmona O, et al. Laparoscopic repair of rectourethral fistulas after prostate surgery. Urology. 2007;70:515-8.).
These evidences have motivated us to evaluate new approaches as options to treat vesicorectal fistulas in selected cases. This article aims to describe and evaluate the results of a new minimally invasive approach to treat vesicorectal fistula.
MATERIALS AND METHODS
A 65 year old patient developed a vesico-rectal fistula in the first 20 days after radical prostatectomy to treat prostate cancer. The diagnosis was confirmed by cystoscopy and CT scan, which showed the fistula in the trigone. Conservative treatment was attempted with high absorption diet, suprapubic cystostomy and proximal colostomy, but the treatment failed after two months.
We performed Transanal Minimally Invasive Surgery (TAMIS) with miniLap devices for instrumentation. Initially, the patient was positioned in lithotomy and cystoscopy was made for implant of a hydrophilic guide wire through fistula to facilitate identification and dissection. We did not position ureteral catheters but it can be made to improve safety.
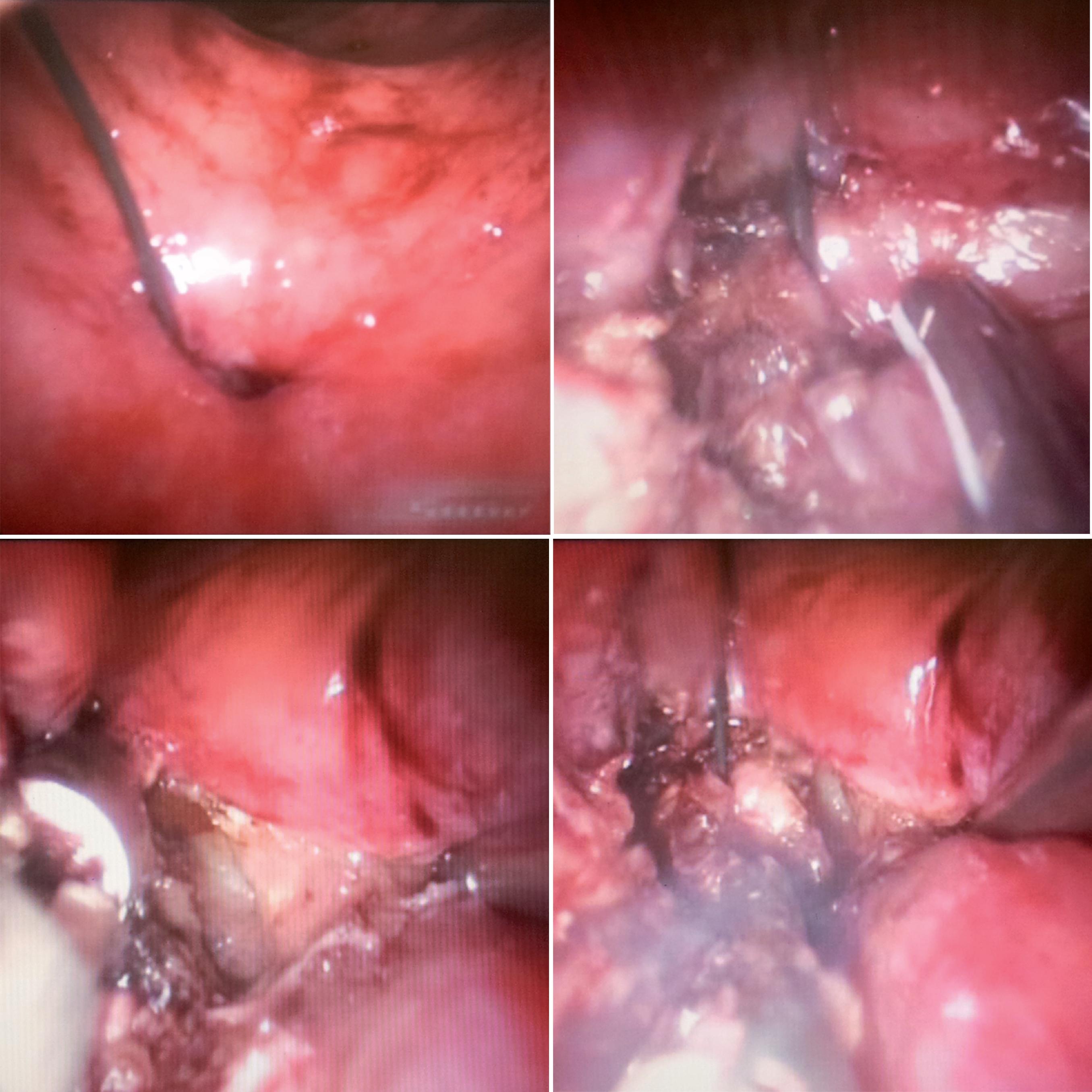
The patient was placed in the jack-knife position with the buttocks apart. We used Alexis® (Applied Medical System) device for 2.5-6 cm size incisions to configure the TAMIS platform. The device was inserted into the anal canal and rectum. A silicone glove was fixed in the outer ring of the device and the self-retaining design held the anal canal open, allowing access to the operative field (Figure-1). We positioned three triangulated ports (one 11 mm port for rigid endoscope 0 degrees, one 5 mm port for ultrasonic scalpel and one 3 mm port for minilap devices). We kept the pneumorectum around 15 mmHg.
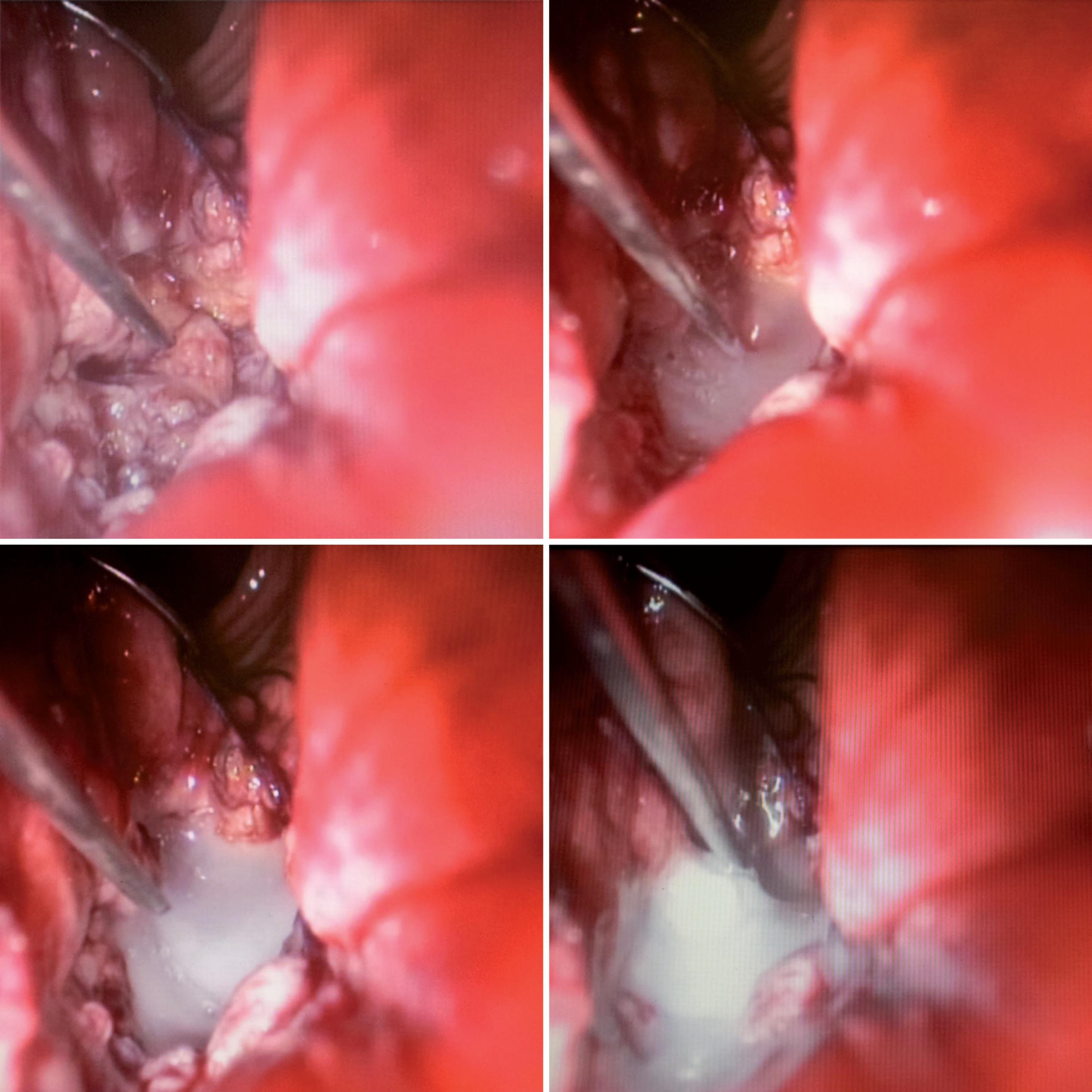
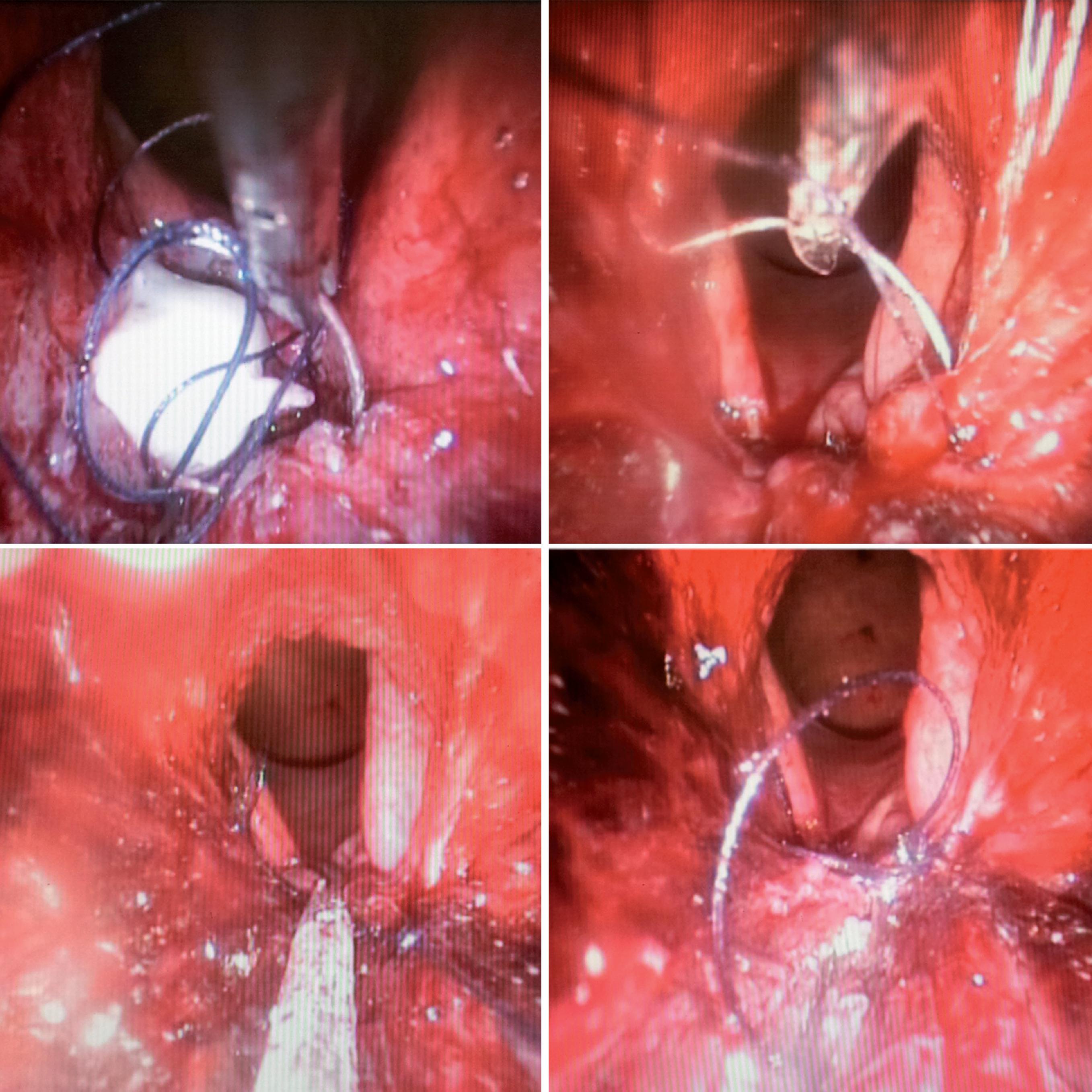
The fistula was identified 5 cm from the anal verge. The fistula tract was excised with ultrasonic scalpel. The guidewire was removed only at the end of excision (Figure-2). The bladder wall was closed with 3-0 Vicryl in a running suture. The space between the bladder wall and rectal wall was filled with fibrin glue (Figure-3). The rectal wall was closed with 3-0 Vicryl in a running suture (Figure-4). Finally we maintained a urethral catheter 18 Fr and cystostomy 20 Fr.
RESULTS
The operative time was 240 minutes for TAMIS with 120 minutes for reconstruction.
There was no conversion, perioperative or postoperative complications in the procedure, including bleeding and rectal perforation. The hospital stay was two days.
The full return to daily activities was in two weeks. Cystoscopy was performed after four weeks of surgery and it revealed no signs of fistula. After four months of follow-up no recurrence was observed. There was no stenosis of anal canal and patient is defecating and voiding normally.
DISCUSSION
There is no consensus about the better approach to treat recto-urinary fistula. Conventional open surgery remains the preferred choice, however it has some limitations (1515. Abdalla MA. Posterior sagittal pararectal approach with rectal mobilization for repair of rectourethral fistula: an alternative approach. Urology. 2009;73:1110-4.–1717. Joshi HM, Vimalachandran D, Heath RM, Rooney PS. Management of iatrogenic recto-urethral fistula by transanal rectal flap advancement. Colorectal Dis. 2011;13:918-20.). Trans-abdominal and posterior approaches have the disadvantages of large incisions to achieve good access. Transperineal and transanal approaches are less invasive but limited visualization and small working space can difficult a good repair. Laparoscopic transperitoneal surgery was introduced in 2003. With an excellent magnification the posterior bladder wall is opened including the fistula tract to achieve good visualization and dissection. The advantages are fast recovery with preliminary good results (1414. Sotelo R, Mirandolino M, Trujillo G, Garcia A, de Andrade R, Carmona O, et al. Laparoscopic repair of rectourethral fistulas after prostate surgery. Urology. 2007;70:515-8.). The refinement of this technique using robotic assistive technology was also described with good results (1818. Sotelo R, de Andrade R, Carmona O, Astigueta J, Velasquez A, Trujillo G, et al. Robotic repair of rectovesical fistula resulting from open radical prostatectomy. Urology. 2008;72:1344-6.).
In the current decade, transluminal procedures have been developed to manage selected cases of urologic pathologies. The potential advantages include less effects of carbonic gas, no mobilization or contact with other organs and reduction of entrance ports. The main disadvantages consist in the small working space that requires more skills to reconstructive procedures. Transvesicoscopic surgery has been reported to treat bladder foreign body, lithiasis, diverticula, ureteral reimplantation and vesicovaginal fistula with excellent results (1919. Puntambekar S P, Desai R, Galagali A, Joshi GA, Joshi S, Kenawadekar R, et al. Laparoscopic transvesical approach for vesicovaginal fistula repair. J Minim Invasive Gynecol. 2013;20:334.–2121. Yoshizawa T, Yamaguchi K, Obinata D, Sato K, Mochida J, Takahashi S. Laparoscopic transvesical removal of erosive mesh after transobturator tape procedure. Int J Urol. 2011;18:861-3.).
Transanal Minimally Invasive Surgery (TAMIS) is a variant of Natural Orifice Endoscopic Surgery (NOES). Presented in 2009, this surgical platform uses access devices that traditionally are used for single site laparoscopy. The most used devices are the SILS™ Port, Alexis Wound Protector/ Retractor and the GelPOINT Path Trans anal Access Platform. The chosen device is inserted into the rectum. When pneumorectum is established, the surgical field is then increased considerably and gives to the surgeon the ability to expand their skills to include procedures from the distal rectum to the mid and proximal rectum. This platform uses standard laparoscopic or minilap instrumentation.
TAMIS was initially described for treatment of benign lesions. After that, treatment of malignant lesions was also described. We observed a growing acceptance in the use of TAMIS to approach anorectal fistulas and tumors at early grades with good results (2222. Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach SW. Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum. 2013;56:301-7.–2424. Lim SB, Seo SI, Lee JL, Kwak JY, Jang TY, Kim CW, et al. Feasibility of transanal minimally invasive surgery for mid-rectal lesions. Surg Endosc. 2012;26:3127-32.). Albert and cols. performed a retrospective analysis of 50 patients with benign and malignant rectal lesions treated with TAMIS at a tertiary referral center. All procedures were made without conversion to other approaches and 68% of patients were discharged on the day of surgery. Only 6% were found to have microscopically positive margins. No long-term complications were observed.
TAMIS platform is versatile and there are some applications beyond local excision. There are descriptions of rectourethral fistula repair, ligation of rectal Dieulafoy's lesion and extraction of foreign body. Atallah and cols. performed TA-MIS to treat a man with rectourethral fistula after cryoablation treatment for prostate cancer. A follow-up enema demonstrated resolution of the fistula (2323. Atallah S, Albert M, Debeche-Adams T, Larach S. Transanal minimally invasive surgery (TAMIS): applications beyond local excision. Tech Coloproctol. 2013;17:239-43.). Gómez et al. comment in a letter to the editor of Actas Urologicas Espanõlas (in press) one case in which TAMIS was utilized to repair an uretrorectal fistula using Gelpoint device. The procedure was successful, achieving a good exposition to 2-layer repair and hemostasis, according to the authors (2525. Gómez GA, Gutiérrez PF, López-Cubillana P, López P. Is minimally invasive transanal surgery an alternative for rectal-urinary fistula correction? Actas Urol Esp. 2014;38:276-7.).
These works motivated us to propose this new approach to treat vesicorectal fistula and evaluate its results. In our report the duration of surgery was 240 minutes, with 120 minutes for reconstruction. We believe that the limited experience with access and non-availability of a material specifically developed for these new approaches is still an obstacle to overcome and make surgery times prolonged when compared to conventional invasive procedures.
In our procedure the greatest difficulties were maintaining luminal dilation, the instrumental manipulation and intraoperative suture. Nevertheless, the length appears to be similar to trans-peritoneal laparoscopic approaches already described. No complications were observed. The procedure was completed without conversion, and intraoperative bleeding was negligible.
Despite the limitations, careful magnified dissections and subsequent repairs were the elements that allowed a better control and a minimized risk of perioperative complications and conversion.
One of the most feared troubles in the repair of vesicorectal fistulas is the loss of functionality due to rectal morbidity of most techniques traditionally used, with the emergence of problems such as anal stenosis and fecal incontinence. None of these postoperative complications were observed in our report, even with little experience with the new method. Minimally invasive surgery done by an expert professional is less aggressive, reduces the risk of complications and may reproduce the results of traditional techniques.
The length of hospital stay in our report was 2 days. This result was even slightly better than some series in the literature and reinforces the potential of minimally invasive surgery in decreasing the morbidity (1414. Sotelo R, Mirandolino M, Trujillo G, Garcia A, de Andrade R, Carmona O, et al. Laparoscopic repair of rectourethral fistulas after prostate surgery. Urology. 2007;70:515-8.,1818. Sotelo R, de Andrade R, Carmona O, Astigueta J, Velasquez A, Trujillo G, et al. Robotic repair of rectovesical fistula resulting from open radical prostatectomy. Urology. 2008;72:1344-6.,2626. Garofalo TE, Delaney CP, Jones SM, Remzi FH, Fazio VW. Rectal advancement flap repair of rectourethral fistula: a 20-year experience. Dis Colon Rectum. 2003;46:762-9.,2727. Kasraeian A, Rozet F, Cathelineau X, Barret E, Galiano M, Vallancien G. Modified York-Mason technique for repair of iatrogenic rectourinary fistula: the montsouris experience. J Urol. 2009;181:1178-83.). Although with a short follow-up, the preliminary result is encouraging and shows compliance with the findings in the literature (1414. Sotelo R, Mirandolino M, Trujillo G, Garcia A, de Andrade R, Carmona O, et al. Laparoscopic repair of rectourethral fistulas after prostate surgery. Urology. 2007;70:515-8.,2626. Garofalo TE, Delaney CP, Jones SM, Remzi FH, Fazio VW. Rectal advancement flap repair of rectourethral fistula: a 20-year experience. Dis Colon Rectum. 2003;46:762-9.).
CONCLUSIONS
Transanal Minimally Invasive Surgery (TAMIS) to treat vesicorectal fistula is feasible and seems to have lower morbidity when compared with more traditional techniques. It is effective and can be offered as an option by experienced laparoscopic surgeons to patients. The greatest difficulties were maintaining luminal dilation, instrumental manipulation and intraoperative suture.
ABBREVIATIONS
- TAMIS = Transanal Minimally Invasive Surgery.
- NOES = Natural Orifice Endoscopic Surgery.
ACKNOWLEDGEMENTS
To Language Editing Facility - Faculty of Medical Sciences, University of Campinas, UNI-CAMP
REFERENCES
-
1Morse FP 3rd, Dretler SP. Diagnosis and treatment of colovesical fistula. J Urol. 1974;111:22-4.
-
2Amendola MA, Agha FP, Dent TL, Amendola BE, Shirazi KK. Detection of occult colovesical fistula by the Bourne test. AJR Am J Roentgenol. 1984;142:715-8.
-
3Pollard SG, Macfarlane R, Greatorex R, Everett WG, Hartfall WG. Colovesical fistula. Ann R Coll Surg Engl. 1987;69:163-5.
-
4Schofield PF. Colovesical fistulas. Br J Hosp Med. 1988;39:483-7.
-
5Walker KG, Anderson JH, Iskander N, McKee RF, Finlay IG. Colonic resection for colovesical fistula: 5-year follow-up. Colorectal Dis. 2002;4:270-4.
-
6Pontari MA, McMillen MA, Garvey RH, Ballantyne GH. Diagnosis and treatment of enterovesical fistulae. Am Surg. 1992;58:258-63.
-
7Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg. 2004;188:617-21.
-
8Amin M, Nallinger R, Polk HC Jr. Conservative treatment of selected patients with colovesical fistula due to diverticulitis. Surg Gynecol Obstet. 1984;159:442-4.
-
9Evans JP, Steinhart AH, Cohen Z, McLeod RS. Home total parenteral nutrition: an alternative to early surgery for complicated inflammatory bowel disease. J Gastrointest Surg. 2003;7:562-6.
-
10Shackley DC, Brew CJ, Bryden AA, Anderson ID, Carlson GL, Scott NA, et al. The staged management of complex entero-urinary fistulae. BJU Int. 2000;86:624-9.
-
11Hechenbleikner EM, Buckley JC, Wick EC. Acquired rectourethral fstulas in adults: a systematic review of surgical repair techniques and outcomes. Dis Colon Rectum. 2013;56:374-83.
-
12Wilbert DM, Buess G, Bichler KH. Combined endoscopic closure of rectourethral fistula. J Urol. 1996;155:256-8.
-
13Joo JS, Agachan F, Wexner SD. Laparoscopic surgery for lower gastrointestinal fistulas. Surg Endosc. 1997;11:116-8.
-
14Sotelo R, Mirandolino M, Trujillo G, Garcia A, de Andrade R, Carmona O, et al. Laparoscopic repair of rectourethral fistulas after prostate surgery. Urology. 2007;70:515-8.
-
15Abdalla MA. Posterior sagittal pararectal approach with rectal mobilization for repair of rectourethral fistula: an alternative approach. Urology. 2009;73:1110-4.
-
16Hadley DA, Southwick A, Middleton RG. York-Mason procedure for repair of recto-urinary fistulae: a 40-year experience. BJU Int. 2012;109:1095-8.
-
17Joshi HM, Vimalachandran D, Heath RM, Rooney PS. Management of iatrogenic recto-urethral fistula by transanal rectal flap advancement. Colorectal Dis. 2011;13:918-20.
-
18Sotelo R, de Andrade R, Carmona O, Astigueta J, Velasquez A, Trujillo G, et al. Robotic repair of rectovesical fistula resulting from open radical prostatectomy. Urology. 2008;72:1344-6.
-
19Puntambekar S P, Desai R, Galagali A, Joshi GA, Joshi S, Kenawadekar R, et al. Laparoscopic transvesical approach for vesicovaginal fistula repair. J Minim Invasive Gynecol. 2013;20:334.
-
20Kim JH, Doo SW, Yang WJ, Song YS. Laparoscopic transvesical excision and reconstruction in the management of mid-urethral tape mesh erosion and stones around the bladder neck: initial experiences. BJU Int. 2012;110:E1009-13.
-
21Yoshizawa T, Yamaguchi K, Obinata D, Sato K, Mochida J, Takahashi S. Laparoscopic transvesical removal of erosive mesh after transobturator tape procedure. Int J Urol. 2011;18:861-3.
-
22Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach SW. Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum. 2013;56:301-7.
-
23Atallah S, Albert M, Debeche-Adams T, Larach S. Transanal minimally invasive surgery (TAMIS): applications beyond local excision. Tech Coloproctol. 2013;17:239-43.
-
24Lim SB, Seo SI, Lee JL, Kwak JY, Jang TY, Kim CW, et al. Feasibility of transanal minimally invasive surgery for mid-rectal lesions. Surg Endosc. 2012;26:3127-32.
-
25Gómez GA, Gutiérrez PF, López-Cubillana P, López P. Is minimally invasive transanal surgery an alternative for rectal-urinary fistula correction? Actas Urol Esp. 2014;38:276-7.
-
26Garofalo TE, Delaney CP, Jones SM, Remzi FH, Fazio VW. Rectal advancement flap repair of rectourethral fistula: a 20-year experience. Dis Colon Rectum. 2003;46:762-9.
-
27Kasraeian A, Rozet F, Cathelineau X, Barret E, Galiano M, Vallancien G. Modified York-Mason technique for repair of iatrogenic rectourinary fistula: the montsouris experience. J Urol. 2009;181:1178-83.
Publication Dates
-
Publication in this collection
Sep-Oct 2015
History
-
Received
02 Jan 2014 -
Accepted
08 June 2014