Keywords
Pulmonary Embolism; Thromboembolism; Ventricular Dysfunction,Right; Hypertension, Pulmonary; Indicators of Morbidity and Mortality
Introduction
PE is a condition that is often difficult to recognize due to its varied clinical presentation, ranging from unclear symptoms to severe conditions that quickly leading the patient to shock and death.11 Álvares F, Ignácio de Pádua A, Terra Filho J. Tromboembolismo pulmonar: diagnóstico e tratamento. Medicina (Ribeirão Preto). 2003;36:214-40. It is the third most common cardiovascular disease worldwide, of high mortality and morbidity, with an estimated incidence of 100-200 per 100,000 inhabitants, according to the Guidelines of the European Society of Cardiology.22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.
There is a variety of related risk factors, including major orthopedic surgeries, traumas, prolonged immobilization, malignant neoplasia, spastic and flaccid paralysis, hormonal contraception, congestive heart failure, thrombophilia, obesity and pregnancy.33 Caramelli B, Gottschall CA, Blacher C, Casagrande EL, Lucio EA, Manente ER, et al; Sociedade Brasileira de Cardiologia. Diretriz de embolia pulmonar. Arq Bras Cardiol. 2004;83(supl 11)1-9.,44 Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I9-16. However, PE can occur even in the absence of known risk factors.22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.
About 10% of all PE patients die within three months after the diagnosis, which is established by right ventricular failure caused by massive occlusion of pulmonary circulation.22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69. Acute cor pulmonale in PE is an important determinant of the severity and early clinical outcome. Therefore, rapid recognition of serious medical conditions is of the essence.
Diagnosis should be suspected in patients with suggestive clinical symptoms in the presence of risk factors. The most common symptoms are non-specific, such as dyspnea, pleuritic pain and hemoptysis.11 Álvares F, Ignácio de Pádua A, Terra Filho J. Tromboembolismo pulmonar: diagnóstico e tratamento. Medicina (Ribeirão Preto). 2003;36:214-40.
2 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.-33 Caramelli B, Gottschall CA, Blacher C, Casagrande EL, Lucio EA, Manente ER, et al; Sociedade Brasileira de Cardiologia. Diretriz de embolia pulmonar. Arq Bras Cardiol. 2004;83(supl 11)1-9. Syncope is not a common symptom and may occur even in the absence of hemodynamic instability, where brief and self-limited hypotension may occur due to vasovagal reflection.55 Thames MD, Alpert JS, Dalen JE. Syncope in patients with pulmonary embolism. JAMA. 1977;238(23):2509-11.,66 Castelli R, Tarsia P, Tantardini C, Pantaleo G, Guariglia A, Porro F. Syncope in patients with pulmonary embolism: comparison between patients with syncope as the presenting symptom of pulmonary embolism and patients with pulmonary embolism without syncope. Vasc Med. 2003;8(4):257-61.
The Wells and Geneva probability scores include clinical criteria for the diagnosis of PE,77 Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998;129(12):997-1005. simply obtained and validated on three levels (high, intermediate and low probability) or two levels (probable or improbable PE), as shown in Table 1.22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69. The investigation continues with complementary tests to confirm or rule out the diagnosis. For patients with improbable PE, a D-dimer test is run. D-dimer is a fibrin degradation product with high negative predictive value for the diagnosis of PE. A low D-dimer value in this context can virtually rule out such diagnosis.22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.,33 Caramelli B, Gottschall CA, Blacher C, Casagrande EL, Lucio EA, Manente ER, et al; Sociedade Brasileira de Cardiologia. Diretriz de embolia pulmonar. Arq Bras Cardiol. 2004;83(supl 11)1-9. The method of choice for diagnosing patients with probable PE and D-dimer greater than 1. 600 is the computed tomography angiography of the chest, which shows thrombi in the pulmonary tree.88 Silva CI, Muller NL. Imaging of acute pulmonary thromboembolism. J Bras Pneumol. 2004;30(5) 474-9.
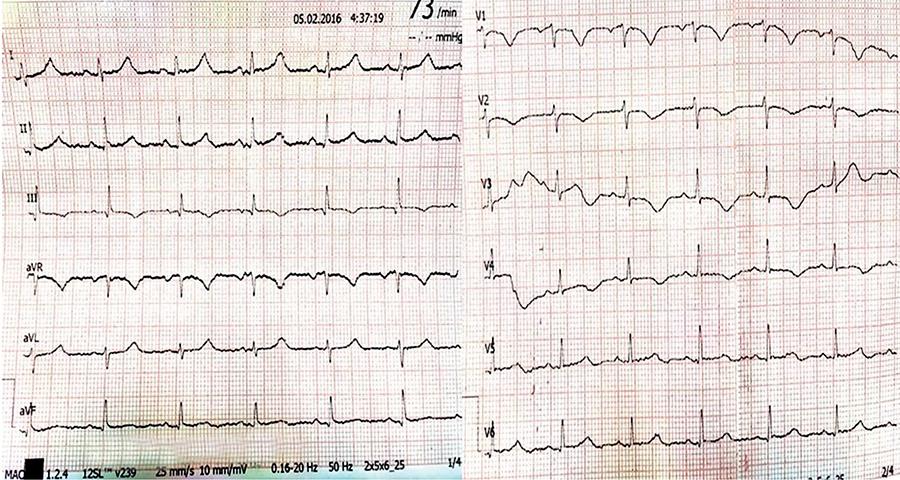
Despite the applicability of probability scores, diagnosis only considers clinical parameters, leaving out an essential tool for the evaluation of most cardiac disorders: ECG. PE may present abnormalities on electrocardiogram, such as T-wave inversion on leads V1 to V4, QR complex on V1, S1Q3T3 pattern and right bundle branch block, suggesting RV overload.11 Álvares F, Ignácio de Pádua A, Terra Filho J. Tromboembolismo pulmonar: diagnóstico e tratamento. Medicina (Ribeirão Preto). 2003;36:214-40.,22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.,99 Daniel KR, Courtney DM, Kline JA. Assessment of cardiac stress from massive pulmonary embolism with 12-lead ECG. Chest. 2001;120(2):474-81. These signs point to a more serious condition associated with pulmonary hypertension and acute cor pulmonale in cases of suspected PE, confirmed with relative ease by transthoracic echocardiogram (TTE).22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.,33 Caramelli B, Gottschall CA, Blacher C, Casagrande EL, Lucio EA, Manente ER, et al; Sociedade Brasileira de Cardiologia. Diretriz de embolia pulmonar. Arq Bras Cardiol. 2004;83(supl 11)1-9.
We describe a clinical case in which, despite the low pretest probability found by the scores of Wells and Geneva, and no high-risk of death detected by PESI and simplified PESI, ECG drew attention to the presence of pulmonary hypertension, serving as useful tool not only for the diagnosis but also for the prognosis of this disease with well-established severity.
Case report
Female, 35-year-old patient, black ethnicity, overweight, sedentary and hypertensive, under regular use of clonidine, losartan and amlodipine. She was an assistant nurse and reported palpitation preceding fatigue and dyspnea on great exertion for three months, progressively worsening in the last month, which made it impossible for her to work.
The patient was admitted to the emergency service after a syncope episode preceded by tachycardia and dyspnea on moderate exertion. That episode was the third similar episode in the last four days. The patient had a questionable history of thrombophlebitis a year ago and miscarriage 10 years ago in the fourth month of pregnancy. Patient is currently not using contraception.
On admission, she reported dyspnea and fatigue on exertion and 90% saturation in ambient air, blood pressure (BP): 140x100 mmHg; heart rate (HR): 98 bpm and respiratory rate (RR): 22 irpm. On physical examination, the patient was bruised on her left eyebrow and in the parietal and occipital region due to traumatic brain injury (TBI) in the first two syncope episodes. There were no signs of deep vein thrombosis.
Laboratory tests found 0.035 troponin (VR<0.015) CK-mass 5.3, D-dimer 6,400 and BNP 729. On admission, ECG showed S1Q3T3 pattern and right ventricular (RV) strain, and negative and symmetric T-waves in THE right precordial leads, from V1 to V4 (Figure 1). Chest X-ray was normal and computed tomography of the head revealed subgaleal hematomas in the parietal, occipital and frontal left regions.
Full anticoagulation with enoxaparin 1 mg/kg 12/12h, O22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69. by nasal catheter and medication reconciliation were initiated.
Due to clinical suspicion, TTE, lower limb venous Doppler and chest computed tomography angiography were requested. ECHO revealed increased right cavities with RV failure, pulmonary hypertension (pulmonary artery pressure (PAP): 86 mmHg), correction of interventricular septum and bulging into the left ventricle (LV) without LV systolic dysfunction. Lower limb venous Doppler showed recent-looking thrombosis in the left popliteal vein and fresh thrombus in the left common iliac vein. Finally, computed tomography angiography of the chest revealed bilateral thrombosis in the pulmonary arteries (PA) with dilated main PA (3.5 cm), confirming severe PE diagnosis (Figure 2).
The therapy chosen was chemical thrombolysis with intravenous rTPA 100 mg as the patient was young, at major negligible risk of bleeding and computed tomography scans of the chest showing only subgaleal hematomas, no intracranial bleeding or subarachnoid hemorrhage. After thrombolysis, there was significant increase of subgaleal hematomas, reports of pain, but without major bleeding. Thrombolysis was successful, regular analgesia was established for pain control, as well as ice packs on hematomas.
The day after thrombolysis, further TTE was done, showing increased right cavities with significant drop in PAP from 86 to 35 mmHg and normal RV systolic function. Fatigue and shortness of breath disappeared completely after the 2nd day of hospitalization. TTE and lower limb venous Doppler were repeated on the 5th day of hospitalization with evolutionary improvement in volumetric RV overload, maintaining normal function, and no more thrombi in the deep lower limb veins. Computed tomography of the head CT was also repeated on the 6th day of hospitalization and showed persisting yet not increased left parietal, occipital and frontal subgaleal hematomas. There was no bleeding at other sites.
The patient was discharged from the Intensive Care Unit (ICU) to the room on the 4th day of admission under coumarin, full anticoagulation and enoxaparin to stay in hospital until the target International Normalized Ratio (INR) was reached - between 2 and 3 - and was discharged on the 9th day of hospitalization.
Discussion
The case described above is about a young woman with few comorbidities, with submassive PE, as she was not in shock, but with signs, symptoms and laboratory tests compatible with the presence of acute cor pulmonale.22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.,33 Caramelli B, Gottschall CA, Blacher C, Casagrande EL, Lucio EA, Manente ER, et al; Sociedade Brasileira de Cardiologia. Diretriz de embolia pulmonar. Arq Bras Cardiol. 2004;83(supl 11)1-9. Although controversial and open to interpretation, the case is undoubtedly rich in terms of lessons learned.
The first lesson was the need to give greater value to easier and cheaper cardiology tests, which can give valuable information about the cardiac impact of PE. The patient was not in shock, but ECG showed inverted T-waves deeper than 2 mm, rS pattern in D1, qR in D3 and T-wave inverted in D3. In 2001, Kurt et al.99 Daniel KR, Courtney DM, Kline JA. Assessment of cardiac stress from massive pulmonary embolism with 12-lead ECG. Chest. 2001;120(2):474-81. published a paper studying 61 patients with PE and analyzed ECG scans 48 hours prior to pulmonary arteriography, where 25 patients died from PE, 26 had PE and did not die, and the remaining 34 did not have PE. Based on the ECG scans of patients confirmed as having PE (tachycardia, complete or incomplete right bundle branch block, inverted T-wave in the right precordial leads and S1Q3T3 pattern), a 21 point (Table 2) score was drawn up, where a score > 10 points is highly suggestive of massive PE with severe pulmonary hypertension. Our patient had an ECG and score=14, which led us to proceed with the investigation, although she presented inconsistent Wells and Geneva probability scores with intermediate PE probability (on 3 levels) or improbable PE probability (on 2 levels). The lesson learned here was that ECG should not be underestimated and it can bring decisive information both for diagnosis and for the stratification of death risk.99 Daniel KR, Courtney DM, Kline JA. Assessment of cardiac stress from massive pulmonary embolism with 12-lead ECG. Chest. 2001;120(2):474-81.
The patient had slow onset of clinical symptoms, which started three months ago, but with significant worsening in the last month and three episodes of syncope in the past four days, which could be signs of chronic PE with new acute episodes in past days which eventually led the patient to present acute cor pulmonale with very high PAP, but with no circulatory shock. Another interesting fact is the absence of tachycardia that accompanies severe cases as the one reported above, which may be due to the chronic use of centrally acting alpha 2 agonist medication (clonidine) which, therefore, had a lowering effect on adrenergic flow, which may have contributed to the absence of tachycardia in the context of acute cor pulmonale. Therefore, we assumed that the absence of tachycardia in this patient was not synonymous with benignity, so we proceeded with the treatment.
The main treatment for PE is systemic anticoagulation allowing the dissolution of the thrombus by the fibrinolytic system of the individual itself. For PE with circulatory shock and persistent hypotension, the use of thrombolytic agents is well established to speed up this process and reduce mortality, but in the absence of hemodynamic impairment, its use is controversial. About 10% of patients die three months after diagnosis, and acute cor pulmonale in PE is an important determinant of the severity and early clinical outcome of this disease.11 Álvares F, Ignácio de Pádua A, Terra Filho J. Tromboembolismo pulmonar: diagnóstico e tratamento. Medicina (Ribeirão Preto). 2003;36:214-40.
2 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.-33 Caramelli B, Gottschall CA, Blacher C, Casagrande EL, Lucio EA, Manente ER, et al; Sociedade Brasileira de Cardiologia. Diretriz de embolia pulmonar. Arq Bras Cardiol. 2004;83(supl 11)1-9.
According to the Guidelines of the European Society of Cardiology, the best-validated prognostic score is the PESI (Pulmonary Embolism Severity Index).22 Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69. Analyzing it in Table 3, we found that the patient had an intermediate to high risk of death, with an original PESI=105 or simplified PESI=2, echocardiographic image and laboratory markers showing RV failure.
The multicenter, double-blind, randomized, placebo-controlled PEITHO (Pulmonary Embolism Thrombolysis)1010 Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate risk pulmonary embolism. N Engl J Med. 2014;370(15):1402-11. study has recently revealed that rapid thrombolysis reduces the combination of death from any cause and hemodynamic instability in seven days in patients with RV failure and myocardial injury without circulatory shock and this is mainly due to decreased risk of hemodynamic decompensation in these patients.1010 Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate risk pulmonary embolism. N Engl J Med. 2014;370(15):1402-11. Therefore, these patients, stratified as intermediate risk, who would only receive treatment with anticoagulants, are also thrombolysis candidates with proven benefit. In this study, there was increased risk of major bleeding, more evident in the groups of patients older than 75, which leads us to consider the risk/benefit ratio of this therapy in the young population without many comorbidities.1010 Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate risk pulmonary embolism. N Engl J Med. 2014;370(15):1402-11. Our case, a young patient with intermediate risk PE, RV failure and myocardial injury, underwent thrombolysis successfully and without major bleeding, despite mild TCE prior to thrombolysis, which we believe to be not enough to contraindicate the thrombolytic drugs. Subsequent head scans and clinical outcome without significant increase in subgaleal hematomas or emergence of further intracranial hematomas corroborate our initial thoughts. However, the PEITHO study found potential bleeding risk, stressing the importance of proper selection of patients, as well as the need of an experienced medical team and the support of a tertiary institution prepared to address potential bleeding complications.1010 Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate risk pulmonary embolism. N Engl J Med. 2014;370(15):1402-11.
Thrombolysis does not change the hospital mortality rate in these cases of intermediate risk but ensures clinical improvement and decreases the chance of hemodynamic decompensation and progression to chronic cor pulmonale, which may lead to late mortality, at the expense of greater bleeding risk, though.1010 Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate risk pulmonary embolism. N Engl J Med. 2014;370(15):1402-11. Further studies comparing different doses of thrombolytics and methods for local thrombolysis with lower risk of bleeding can bring great benefits to such patients, with a smaller risk of bleeding.
-
Sources of FundingThere were no external funding sources for this study.
-
Study AssociationThis study is not associated with any thesis or dissertation work.
References
-
1Álvares F, Ignácio de Pádua A, Terra Filho J. Tromboembolismo pulmonar: diagnóstico e tratamento. Medicina (Ribeirão Preto). 2003;36:214-40.
-
2Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033-69.
-
3Caramelli B, Gottschall CA, Blacher C, Casagrande EL, Lucio EA, Manente ER, et al; Sociedade Brasileira de Cardiologia. Diretriz de embolia pulmonar. Arq Bras Cardiol. 2004;83(supl 11)1-9.
-
4Anderson FA Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I9-16.
-
5Thames MD, Alpert JS, Dalen JE. Syncope in patients with pulmonary embolism. JAMA. 1977;238(23):2509-11.
-
6Castelli R, Tarsia P, Tantardini C, Pantaleo G, Guariglia A, Porro F. Syncope in patients with pulmonary embolism: comparison between patients with syncope as the presenting symptom of pulmonary embolism and patients with pulmonary embolism without syncope. Vasc Med. 2003;8(4):257-61.
-
7Wells PS, Ginsberg JS, Anderson DR, Kearon C, Gent M, Turpie AG, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med. 1998;129(12):997-1005.
-
8Silva CI, Muller NL. Imaging of acute pulmonary thromboembolism. J Bras Pneumol. 2004;30(5) 474-9.
-
9Daniel KR, Courtney DM, Kline JA. Assessment of cardiac stress from massive pulmonary embolism with 12-lead ECG. Chest. 2001;120(2):474-81.
-
10Meyer G, Vicaut E, Danays T, Agnelli G, Becattini C, Beyer-Westendorf J, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate risk pulmonary embolism. N Engl J Med. 2014;370(15):1402-11.
Publication Dates
-
Publication in this collection
Sep-Oct 2017
History
-
Received
24 July 2016 -
Reviewed
23 Jan 2017 -
Accepted
20 Mar 2017