Abstracts
In its various forms, antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is characterized by a systemic inflammation of the small and medium-sized arteries (especially in the upper and lower respiratory tracts, as well as in the kidneys). The forms of AAV comprise Wegener's granulomatosis (now called granulomatosis with polyangiitis), microscopic polyangiitis, renal AAV, and Churg-Strauss syndrome. In this paper, we discuss the phases of AAV treatment, including the induction phase (with cyclophosphamide or rituximab) and the maintenance phase (with azathioprine, methotrexate, or rituximab). We also discuss how to handle patients who are refractory to cyclophosphamide.
Anti-neutrophil cytoplasmic antibody-associated vasculitis; Wegener granulomatosis; Antibodies, antineutrophil cytoplasmic
As vasculites antineutrophil cytoplasmic antibody (ANCA, anticorpo anticitoplasma de neutrófilos) associadas (VAAs) são caracterizadas por uma inflamação sistêmica das artérias de pequeno e médio calibre (especialmente no trato respiratório superior e inferior, e nos rins). As VAAs compreendem a granulomatose de Wegener (agora chamada de granulomatose com poliangeíte), poliangeíte microscópica, VAA limitada ao rim e a síndrome de Churg-Strauss. Neste artigo, discutiremos as fases de tratamento dessas vasculites, como fase de indução (com ciclofosfamida ou rituximab) e fase de manutenção (com azatioprina, metotrexato ou rituximab). Além disso, discutiremos como manusear os casos refratários à ciclofosfamida.
Vasculite associada a anticorpo anticitoplasma de neutrófilos; Granulomatose de Wegener; Anticorpos anticitoplasma de neutrófilos
REVIEW ARTICLE
Treatment of antineutrophil cytoplasmic antibody-associated vasculitis: update*
Alfredo Nicodemos Cruz SantanaI; Viktoria WoronikII; Ari Stiel Radu HalpernIII; Carmen S V BarbasIV
IAttending Physician. Thoracic Unit, Hospital Regional da Asa Norte - HRAN, North Wing Regional Hospital - Escola Superior de Ciências da Saúde/Secretaria de Estado da Saúde - ESCS/SES, Graduate School of Health Sciences/State Department of Health - Brasília, Brazil
IIAttending Physician. Department of Nephrology, Faculdade de Medicina da Universidade de São Paulo - HCFMUSP, University of São Paulo School of Medicine - Hospital das Clínicas, São Paulo, Brazil
IIIAttending Physician. Department of Rheumatology, Faculdade de Medicina da Universidade de São Paulo - HCFMUSP, University of São Paulo School of Medicine - Hospital das Clínicas, São Paulo, Brazil
IVTenured Professor. Department of Pulmonology, Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo - InCor/HCFMUSP, Heart Institute/University of São Paulo School of Medicine Hospital das Clínicas - São Paulo, Brazil
Correspondence to
ABSTRACT
In its various forms, antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is characterized by a systemic inflammation of the small and medium-sized arteries (especially in the upper and lower respiratory tracts, as well as in the kidneys). The forms of AAV comprise Wegener's granulomatosis (now called granulomatosis with polyangiitis), microscopic polyangiitis, renal AAV, and Churg-Strauss syndrome. In this paper, we discuss the phases of AAV treatment, including the induction phase (with cyclophosphamide or rituximab) and the maintenance phase (with azathioprine, methotrexate, or rituximab). We also discuss how to handle patients who are refractory to cyclophosphamide.
Keywords: Anti-neutrophil cytoplasmic antibody-associated vasculitis; Wegener granulomatosis; Antibodies, antineutrophil cytoplasmic.
Introduction
In its various forms, antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is characterized by a systemic inflammation of the small and medium-sized arteries. The inflammation occurs mainly in the upper and lower respiratory tracts (Figure 1), as well as in the kidneys (pauci-immune necrotizing glomerulonephritis). The forms of AAV comprise Wegener's granulomatosis (WG)-now called granulomatosis with polyangiitis-microscopic polyangiitis (MPA), renal AAV, and Churg-Strauss syndrome.(1-6) However, in the present article, we do not discuss Churg-Strauss syndrome, because it does not usually require intensive immunosuppression.(7)
In the 1980s, a relationship was found between these forms of vasculitis and the presence of ANCA in the serum. The presence of a common serum marker, as well as the good response of these pathologies to treatment with cyclophosphamide, led some authors to classify these forms of systemic vasculitis as a single group. Nevertheless, it should be emphasized that not every form of AAV shows this marker and not every ANCA-positive patient has vasculitis.(8)
Immunofluorescence is the primary technique for the study of ANCA. With this method, it is possible to observe two patterns closely related to the presence of clinically evident vasculitis: cytoplasmic ANCA (c-ANCA), present in 80% of cases of WG and in 30% of cases of MPA, and perinuclear ANCA (p-ANCA), present in 10% of cases of WG and in 60% of cases of MPA. The cytoplasmic pattern usually corresponds to the existence of antibodies against proteinase 3 that can be detected with greater sensitivity by ELISA. This association is highly specific for this type of vasculitis, especially WG. In contrast, p-ANCA immunofluorescence is nonspecific, typically showing anti-myeloperoxidase antibodies on ELISA, and can occur in many situations not related to systemic vasculitis, potentially representing the existence of antibodies against different intracellular antigens. The presence of antibodies against myeloperoxidase, which can also be detected by ELISA, is closely related to AAV, especially MPA. The ELISA test (specific for antiproteinase 3 or antimyeloperoxidase) is more sensitive than is immunofluorescence, the former being particularly useful in cases of inconclusive immunofluorescence results, in cases of atypical immunofluorescence patterns, or in cases of p-ANCA in which one wishes to determine the relationship with the presence of antimyeloperoxidase antibodies (especially in situations of clinical uncertainty). However, unlike immunofluorescence, the ELISA technique to be used has yet to be internationally standardized. Therefore, screening for the presence of these antibodies should always be performed by immunofluorescence, ELISA being reserved for special cases.(8)
In AAV, pulmonary manifestations occur especially in WG. A study conducted in Brazil and involving 98 patients (mean age, 48 ± 15 years) with WG who were recruited from a department of pulmonology, which represents a bias, revealed that 98% of the cases had pulmonary involvement, characterized by (cavitary or noncavitary) pulmonary nodules, (cavitary or noncavitary) masses, pulmonary consolidations, ground-glass areas (commonly associated with alveolar hemorrhage), and lower airway injury (subglottic stenosis, tracheal stenosis, bronchial stenosis, etc).(9) In addition, 95% of the patients had sinus involvement, and 90% of those patients were ANCA-positive. Pulmonary involvement is much less common in MPA than in WG and is usually characterized by ground-glass areas (which is consistent with alveolar hemorrhage) or interstitial involvement (which is consistent with pulmonary fibrosis; Table 1, Figure 2).(9)
The second most common form of AAV is renal AAV, which presents as necrotizing glomerulonephritis with crescent formation and a lack of immunoglobulin expression (pauci-immune). In addition, there is fibrin deposition and thrombus formation in the glomerulus, and, in the 1970s, there were sporadic reports of reversion of renal failure in AAV with the use of anticoagulation therapy.(10) A finding of acute tubular necrosis is also quite common.
A new classification of glomerular involvement in AAV has recently been proposed. This classification can predict renal survival and is subdivided into four classes:
Class 1 - Focal glomerulonephritis: 50% or more of the glomeruli are normal (that is, without vasculitic lesions, without global sclerosis, although mild ischemic changes or minimal inflammatory infiltration can occur)
Class 2 - Crecentic glomerulonephritis: 50% or more of the glomeruli have (cellular or fibrotic) crescents
Class 3 - Mixed glomerulonephritis: fewer than 50% of the glomeruli are normal; fewer than 50% of the glomeruli have crescents; fewer than 50% of the glomeruli are completely sclerosed
Class 4 - Sclerosing glomerulonephritis: 50% or more of the glomeruli are completely sclerosed
This classification was validated in renal biopsies from 100 patients who had had at least one year of clinical follow-up and revealed that end-stage chronic renal failure was more common in classes 3 and 4 than in classes 1 and 2. It should be borne in mind that classes 2, 3, and 4 did not differ regarding baseline renal function, although class 2 showed greater function gain over the course of the cases. It should also be borne in mind that in the first year of follow-up, the last three of the four classes resulted in high mortality (25-39%).(11)
Treatment overview
History
When Wegener described AAV in 1936, this new disease was characterized by high mortality, with a one-year survival of only 10%. However, in the 1970s, cyclophosphamide began to be used, which resulted in a drastic change in survival from this disease.(12) Currently, five-year survival is 70-90%, including in a study conducted in Brazil.(9) However, the extended use of cyclophosphamide (for at least 18 months) is associated with an increased risk of hemorrhagic cystitis, bladder cancer, leukemia, and lymphoma. Therefore, treatment of vasculitis has been defined as consisting of an induction phase (the patient is freed of the inflammation), with the use of cyclophosphamide, and a maintenance phase (the patient is kept free of the inflammation), ideally with the use of a less toxic drug than cyclophosphamide.(13-20)
In addition to the problem of the maintenance phase, there is the risk of disease recurrence (reinstitution of cyclophosphamide is indicated to treat the inflammation, with consequent increased risks inherent in its use, because of repeated use of the drug) and the risk of developing disease that is refractory to cyclophosphamide (the inflammation persists despite treatment with the drug).(15)
Below, we specifically discuss the phases of AAV treatment: induction; maintenance; treatment of AAV recurrence; and treatment of AAV that is refractory to cyclophosphamide.
Induction phase
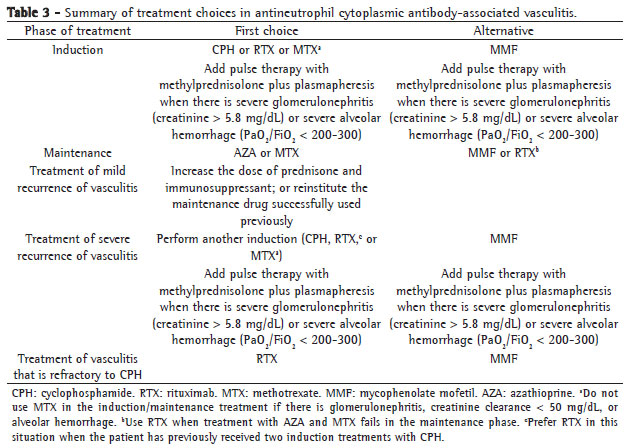
The principal remedies used in the induction phase are cyclophosphamide, methotrexate, rituximab, plasmapheresis, and pulse therapy with methylprednisolone. Mycophenolate mofetil (MMF) can also be used in the induction phase; however, it has lower efficacy than do cyclophosphamide and rituximab, and is therefore considered a second-line drug.(13)
In the induction phase, the combination of cyclophosphamide (2 mg kg-1 day-1) and prednisone (1 mg kg-1 day-1) is used. Cyclophosphamide should be used for up to 1-2 months after remission of AAV is achieved, which usually equates to approximately 3-9 months of treatment. Absence of inflammation in AAV is defined as urinalysis results (sediments and abnormal elements) without glomerular hematuria and absence of active lung injury.(21)
Regarding prednisone, the patient begins to show signs that the inflammation is subsiding usually after 1 month of treatment at a dose of 1 mg kg-1 day-1, and, thereafter, the dose can be tapered at a rate of 2.5 mg/week. Some authors recommend discontinuing prednisone at month 6 of treatment if control of vasculitis is achieved, whereas others suggest using prednisone at a dose of 5-10 mg/day continuously, because it might reduce the risk of AAV recurrence.(13,14) We opted to maintain the dose of 5-10 mg/day continuously.
The use of pulse therapy with methylprednisolone (500-1,000 mg/day for 3 days) in the induction phase is indicated in cases of AAV associated with acute renal failure or with diffuse alveolar hemorrhage (DAH), which is characterized by the triad consisting of new pulmonary infiltrates, worsening of SpO2, and decreased hemoglobin levels.(13)
In addition, plasmapheresis can be used in the AAV induction phase. Its use was evaluated in a prospective randomized study involving 137 patients with serum creatinine levels > 5.8 mg/dL. All patients received oral cyclophosphamide plus prednisone. Some of the patients also underwent plasmapheresis (seven sessions of plasmapheresis in 14 days), whereas others did not. The study results showed that plasmapheresis reduced the risk of dialysis-dependent chronic renal failure in 3 months (from 51% to 31%), with no increase in adverse events. Plasmapheresis is also used in combination with cyclophosphamide + prednisone in cases of severe DAH (PaO2/FiO2 < 200-300). Plasma replacement at the end of plasmapheresis must not be forgotten in cases of severe DAH or in cases of biopsy or recent surgical manipulation.(22)
In summary, in cases of AAV associated with severe DAH or with acute renal failure (serum creatinine levels > 5.8 mg/dL), the combination of cyclophosphamide, prednisone, pulse therapy with methylprednisolone, and plasmapheresis should be used.
Another important drug in the induction phase is rituximab, which can replace cyclophosphamide. In a prospective randomized study of 197 patients with AAV, of whom 49% had recently been diagnosed with AAV (treatment-naïve patients) and 51% had experienced AAV recurrence (patients with a history of treatment), rituximab (375 mg/m2 of body surface area, once a week, for 4 weeks) was administered in combination with pulse therapy with methylprednisolone (1 dose) and prednisone (1 mg kg-1 day-1) to a group of patients, which was compared with another group receiving the combination of cyclophosphamide (2 mg kg-1 day-1) and prednisone (1 mg kg-1 day-1).(23) The study results showed that treatment with rituximab was as successful as was treatment with cyclophosphamide in the patients with recently diagnosed AAV, and that the former was more successful than the latter in the patients with AAV recurrence. The adverse events were similar in the two groups.(23) Therefore, if these results are confirmed in future studies, rituximab becomes an excellent surrogate for cyclophosphamide in the induction phase in patients with recently diagnosed AAV, and it can be the first choice in the induction phase in patients with AAV recurrence.
Rituximab is an anti-CD20 B lymphocyte monoclonal chimeric antibody, that is, it eliminates CD20+ B lymphocytes, with the potential effect of controlling the inflammation of AAV. Treatment with rituximab can cause some adverse events, such as fever, chills, allergic reactions, and anaphylactic shock. In order to minimize them, patients should be pretreated with paracetamol (750 mg), ranitidine (50 mg), diphenhydramine (one ampoule), and methylprednisolone (100 mg). Rituximab should be diluted in 0.9% saline in order to obtain a concentration < 4 mg of rituximab/mL of 0.9% saline. Rituximab infusion should begin at a rate of 50 mg/h, and this rate should be increased by 50 mg/h every 30 min until it reaches 400 mg/h. During the one-month treatment period, prophylaxis for pneumocystis pneumonia should be performed. The contraindications to the use of rituximab are being allergic to this drug, having leukocyte counts < 1,000-3,000 mm3, having active infection, and being pregnant. The most severe adverse events associated with rituximab are mild hypotension, fever, leukopenia, thrombocytopenia, severe arrhythmia, severe congestion, and Stevens-Johnson syndrome.(23)
Finally, methotrexate can also be used in the induction phase. Its initial dose is 0.2 mg/kg per week (the maximum dose is 15 mg/week), and it is increased by 2.5 mg/week up to the maximum dose of 25 mg/week if the patient can tolerate it (transaminase/bilirubin levels < 3 times higher than normal and leukocyte counts > 3,000-4,000 mm3). However, methotrexate can only be used in the induction phase in cases of AAV with mild activity/inflammation (without DAH and without glomerulonephritis), with creatinine clearance > 50 mg/dL. In addition, special attention should be given to its combination with sulfamethoxazole/trimethoprim (because of the risk of anemia, leukopenia, and thrombocytopenia). Folate (1 mg/day) should be administered to all patients receiving methotrexate.(13,24,25)
Maintenance phase
The maintenance phase begins 1-2 months after remission of the inflammation of AAV. The principal drug used in this phase is azathioprine (2 mg kg-1 day-1, usually for 12 months), replacing the cyclophosphamide used in the induction phase. Its use is based on a prospective randomized study of 155 patients with AAV in which the use of azathioprine after remission of vasculitis was compared with that of cyclophosphamide. In that study, recurrence of the inflammation of AAV was similar with the use of azathioprine and with that of cyclophosphamide, and the adverse events were acceptable.(21)
Another point that has recently been discussed was the duration of the maintenance phase, which until then had been established at 1 year. Since the risk of AAV recurrence can be as high as 4.3% per month, and since recurrence implies the reinstitution of cyclophosphamide (with its possible severe adverse events), some authors suggest the use of azathioprine for 2 years, for 3 years, or even indefinitely. The factors associated with AAV recurrence include PR3-ANCA positivity, upper airway injury, pulmonary involvement, and a history of AAV recurrence. A greater number of risk factors translate to a greater propensity to use azathioprine for an indefinite length of time, as follows: 2 mg kg-1 day-1 in the first year; 1.5 mg kg-1 day-1 in the second year; and 1 mg kg-1 day-1 indefinitely.(13,14)
Another drug that is also used in the maintenance phase is methotrexate (the maximum dose is 20-25 mg/week). The minimum duration of treatment with methotrexate in the maintenance phase is 24 months (in contrast to the minimum duration of 12 months for azathioprine). In addition, creatinine clearance should be > 50 mg/dL and there must be no history of glomerulonephritis. Methotrexate should be used in combination with folate (1 mg/day).(13,14,26)
In patients who do not respond well to azathioprine or to methotrexate in the maintenance phase, MMF (1,000-3,000 mg/day) or rituximab ((375 mg/m2 of body surface area, once a week, for 4 weeks, every 6 months) should be attempted.(14)
Phase of treatment of AAV recurrence
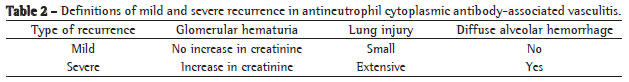
Recurrence is characterized by the onset of glomerular hematuria, pulmonary or ocular involvement, sinusitis, neuritis, skin lesion, etc. In cases of mild recurrence (Table 2) in the maintenance phase, the maintenance dose (corticosteroid + immunosuppressant: azathioprine or methotrexate) should be increased. In cases of mild recurrence after discontinuation of the maintenance phase, the maintenance phase should be reinstituted, there being no need for another induction phase.(13,14)
Conversely, in cases of severe recurrence, another induction phase is always necessary. If severe recurrence occurs in the maintenance phase, there must be another induction phase (cyclophosphamide or rituximab, the latter being preferable if the patient has already used two cycles of cyclophosphamide), and, after remission of vasculitis is achieved, there is a maintenance phase with a different drug than that used in the previous maintenance phase (if azathioprine was used before, consider methotrexate, MMF, or rituximab). In cases of severe recurrence after discontinuation of the maintenance phase, there must be another induction phase (cyclophosphamide or rituximab, the latter being preferable if there has been two previous cycles of cyclophosphamide), and, after remission of vasculitis is achieved, there is a maintenance phase with the same drug used in the previous maintenance phase (however, keep the maintenance phase for at least 24 months or even indefinitely: see "Maintenance phase").(13,14)
Phase of treatment of AAV that is refractory to cyclophosphamide
This phase occurs if vasculitis remains active after 1-2 months of treatment with cyclophosphamide, that is, when there is persistent glomerular hematuria with increased creatinine levels, as well as persistent pulmonary, ocular, and cutaneous activity. It is important not to confuse refractoriness to cyclophosphamide with infection (especially in the sinuses and lungs), poor adherence to treatment (especially in those receiving oral cyclophosphamide), or drug toxicity. The risk factors for refractoriness to cyclophosphamide include being female, being over 65 years of age, and having baseline creatinine levels > 5 mg/dL.(15)
In refractory cases, the first choice is rituximab (375 mg/m2, once a week, for 4 weeks) and the second choice is MMF ((500-1,500 mg, twice a day). The benefits of rituximab in patients who are refractory to cyclophosphamide was reported in a retrospective study involving four centers in the United Kingdom and 65 patients with AAV who ranged in age from 7 to 77 years. In that study, rituximab was used (usually at a dose of 375 mg/m2, once a week, for 4 weeks), and clinical follow-up lasted 6-55 months. The rate of remission of AAV was 98%, remission occurring 1-5 months after infusion of rituximab. Recurrence of AAV occurred in 57% of the patients (usually 4-37 months after infusion). In the patients with recurrence, remission of vasculitis was again achieved by another infusion of rituximab in 84% of the cases. It should be mentioned that, at one of the centers, 15 patients with AAV that was refractory to cyclophosphamide were treated with routine infusion of rituximab every 6 months, and there was no recurrence, which offers excellent prospects for the use of rituximab in the induction and maintenance phase even in such patients (Table 3).(27)
References
- 1. Falk RJ, Gross WL, Guillevin L, Hoffman GS, Jayne DR, Jennette JC, et al. Granulomatosis with polyangiitis (Wegener's): an alternative name for Wegener's granulomatosis. Arthritis Rheum. 2011;63(4):863-4.
- 2. Santana AN. Circulating endothelial progenitor cells in ANCA-associated vasculitis: the light at the end of the tunnel? Rheumatology (Oxford). 2009;48(10):1183-4.
- 3. Santana AN, Takagaki TY, Barbas CS. Incidence of fatal venous thromboembolism in antineutrophil cytoplasmic antibody-associated vasculitis. J Bras Pneumol. 2011;37(3):409-411.
- 4. Santana AN, Ab'Saber AM, Teodoro WR, Capelozzi VL, Barbas CS. Thrombosis in small and mediumsized pulmonary arteries in Wegener's granulomatosis: a confocal laser scanning microscopy study. J Bras Pneumol. 2010;36(6):724-30.
- 5. Santana AN, Antunes T, Barbas CS. Treatment of ANCAassociated vasculitis. JAMA. 2007;298(23):2739; author reply 2740.
- 6. Santana AN, Takagaki TY, Barros JM, Antunes T, Parra ER, Capelozzi VL, et al. Re: giant leg ulcer in Wegener's granulomatosis treated with plasmapheresis and skin graft. Dermatol Surg. 2004;30(8):1182-3.
- 7. Barros JM, Antunes T, Barbas CS. Síndrome de Churg- Strauss. J Bras Pneumol. 2005;31(Suppl 1):S27-S31.
- 8. Radu AS, Levi M. Anticorpos contra o citoplasma de neutrófilos. J Bras Pneumol. 2005;31(Suppl 1):S16-S20.
- 9. Barbas CS, Santana AN, Antunes T, Parra ER, Capelozzi VL, Carvalho CR, et al. Avaliação de 98 pacientes com Granulomatose de Wegener. XXXIII Congresso Brasileiro de Pneumologia e Tisiologia; 2006. J Bras Pneumol. 2006;32(Suppl 5): S227.
- 10. Whitaker AN, Emmerson BT, Bunce IH, Nicoll P, Sands JM. Reversal of renal failure in Wegener's granulomatosis cy heparin. Am J Med Sci. 1973;265(5):399-406.
- 11. Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K, et al. Histopathologic classification of ANCAassociated glomerulonephritis. J Am Soc Nephrol. 2010;21(10):1628-36.
- 12. Novack SN, Pearson CM. Cyclophosphamide therapy in Wegener's granulomatosis. N Engl J Med. 1971;284(17):938-42.
- 13. Stone JH, Kaplan AA, Falk RJ. Initial immunosuppressive therapy in Wegener's granulomatosis and microscopic polyangiitis. In: UpToDate, Basow DS, editor. UpToDate, Waltham, MA, 2011.
- 14. Stone JH, Falk RJ. Maintenance immunosuppressive therapy in granulomatosis with polyangiitis (Wegener's) and microscopic polyangiitis. In: UpToDate, Basow DS, editor. UpToDate, Waltham, MA, 2011.
- 15. Stone JH, Falk RJ. Treatment of cyclophosphamideresistant granulomatosis with polyangiitis (Wegener's) and microscopic polyangiitis. In: UpToDate, Basow DS, editor. UpToDate, Waltham, MA, 2011.
- 16. Bosch X, Guilabert A, Espinosa G, Mirapeix E. Treatment of antineutrophil cytoplasmic antibody associated vasculitis: a systematic review. JAMA. 2007;298(6):655-69.
- 7. Niles J. Rituximab in induction therapy for antineutrophil cytoplasmic antibody (ANCA) vasculitis. Clin Exp Immunol. 2011;164 Suppl 1:27-30.
- 18. Casian A, Jayne D. Plasma exchange in the treatment of Wegener's granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome and renal limited vasculitis. Curr Opin Rheumatol. 2011;23(1):12-7.
- 19. Reinhold-Keller E, de Groot K. Use of methotrexate in ANCA-associated vasculitides. Clin Exp Rheumatol. 2010;28(5 Suppl 61):S178-82.
- 20. Chen M, Kallenberg CG. ANCA-associated vasculitides- -advances in pathogenesis and treatment. Nat Rev Rheumatol. 2010;6(11):653-64.
- 21. Jayne D, Rasmussen N, Andrassy K, Bacon P, Tervaert JW, Dadoniené J, et al. A randomized trial of maintenance therapy for vasculitis associated with antineutrophil cytoplasmic autoantibodies. N Engl J Med. 2003;349(1):36-44.
- 22. Jayne DR, Gaskin G, Rasmussen N, Abramowicz D, Ferrario F, Guillevin L, et al. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J Am Soc Nephrol. 2007;18(7):2180-8.
- 23. Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363(3):221-32.
- 24. Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, de Groot K, Gross W, et al. EULAR recommendations for the management of primary small and medium vessel vasculitis. Ann Rheum Dis. 2009;68(3):310-7.
- 25. Specks U. Methotrexate for Wegener's granulomatosis: what is the evidence? Arthritis Rheum. 2005;52(8):2237-42.
- 26. Langford CA, Talar-Williams C, Barron KS, Sneller MC. Use of a cyclophosphamide-induction methotrexate-maintenance regimen for the treatment of Wegener's granulomatosis: extended follow-up and rate of relapse. Am J Med. 2003;114(6):463-9.
- 27. Jones RB, Ferraro AJ, Chaudhry AN, Brogan P, Salama AD, Smith KG, et al. A multicenter survey of rituximab therapy for refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2009;60(7):2156-68.
Publication Dates
-
Publication in this collection
10 Jan 2012 -
Date of issue
Dec 2011
History
-
Received
17 June 2011 -
Accepted
11 July 2011