Abstract
Objective:
To identify, using a systematic review and meta-analysis of observational studies, which risk factors are significantly associated with neonatal mortality in Brazil, and to build a comprehensive national analysis on neonatal mortality.
Sources:
This review included observational studies on neonatal mortality, performed between 2000 and 2018 in Brazilian cities. The MEDLINE, Elsevier, Cochrane, LILACS, SciELO, and OpenGrey databases were used. For the qualitative analysis, the Newcastle-Ottawa Scale was used. For the quantitative analysis, the natural logarithms of the risk measures and their confidence intervals were used, as well as the DerSimonian and Laird method as a random effects model, and the Mantel-Haenszel model for heterogeneity estimation. A confidence level of 95% was considered.
Summary of findings:
The qualitative analysis resulted in six studies of low and four studies of intermediate-low bias risk. The following exposure factors were significant: absence of partner, maternal age ≥35 years, male gender, multiple gestation, inadequate and absent prenatal care, presence of complications during pregnancy, congenital malformation in the assessed pregnancy, Apgar < 7 at the fifth minute, low and very low birth weight, gestational age ≤ 37 weeks, and caesarean delivery.
Conclusion:
The most significant risk factors presented in this study are modifiable, allowing aiming at a real reduction in neonatal deaths, which remain high in the country.
KEYWORDS
Neonatal mortality; Risk factors; Brazil; Review systematic; Meta-analysis
Resumo:
Objetivo:
Identificar, através de uma revisão sistemática e da metanálise de estudos observacionais, quais fatores de risco associam-se significativamente com a mortalidade neonatal no Brasil e construir uma análise nacional abrangente sobre a mortalidade neonatal.
Fontes:
Foram avaliados os estudos observacionais sobre mortalidade neonatal realizados entre 2000 e 2018 em cidades brasileiras. Usaram-se as bases MEDLINE, Elsevier, Cochrane, LILACS, SciELO e OpenGrey. Para a análise qualitativa, foi usada a Escala Newcastle-Ottawa. Para a análise quantitativa, foram utilizados os logaritmos naturais das medidas de risco e de seus intervalos de confiança, o método de DerSimonian e Laird como modelo de efeitos aleatórios e o modelo de Mantel-Haenszel para estimativa da heterogeneidade. Considerou-se nível de confiança de 95%.
Resumo dos achados:
A análise qualitativa resultou em seis estudos de baixo e quatro estudos de intermediário-baixo risco de viés. Foram significativos os seguintes fatores de exposição: ausência de companheiro, idade materna ≥ 35 anos, sexo masculino, gestação múltipla, pré-natal inadequado e ausente, presença de intercorrências durante a gestação, de malformação congênita na gestação em estudo, Apgar < 7 no quinto minuto, baixo e muito baixo peso ao nascer, idade gestacional ≤ 37 semanas e parto cesariano.
Conclusão:
Os fatores de risco mais significativos apresentados neste estudo são modificáveis, o que possibilita almejar uma redução real das mortes neonatais, que ainda permanecem elevadas no país.
Palavras-chave
Mortalidade neonatal; Fatores de risco; Brasil; Revisão sistemática; Metanálise
Introduction
Neonatal death is defined as the death of a newborn before completing 28 days of life. 11 Lehtonen L, Gimeno A, Parra-Llorca A, Vento M. Early neonatal death: a challenge worldwide. Semin Fetal Neonatal Med. 2017;22:153-60.,22 Blencowe H, Calvert C, Lawn JE, Cousens S, Campbell OM. Measuring maternal, foetal and neonatal mortality: challenges and solutions. Best Pract Res Clin Obstet Gynaecol. 2016;36:14-29. In Brazil, the neonatal mortality rate in 2016 consisted of eight neonatal deaths per 1000 live births - a significant reduction when compared to 1990, when it was 26 neonatal deaths per 1000 live births. 33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,44 United Nations Inter-agency Group for Child Mortality Estimation. Levels and Trends in Child Mortality Report 2017. UNICEF; 2017. In 2011, the country reached goal four of the Millennium Development Goals, a commitment of the member governments of the United Nations to reduce infant mortality.33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207. The Brazilian neonatal mortality rate, despite this reduction, is still high and unevenly distributed regionally, with the difference between the North/Northeast and South/Southeast regions being the most discrepant.55 Rodrigues NC, Monteiro DL, Almeida AS, Barros MB, Pereira Neto A, O'Dwyer G, et al. Temporal and spatial evolution of maternal and neonatal mortality rates in Brazil, 1997-2012. J Pediatr (Rio J). 2016;92:567-73.
The reduction of this rate is a goal to be pursued and a reality that can be achieved, since preventable factors, such as low birth weight, prematurity, neonatal asphyxia, and low-quality prenatal care are the main reasons for this high value. 66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.
7 Pedrosa LD, Sarinho SW, Ordonha MR. Análise da qualidade da informação sobre causa básica de óbitos neonatais registrados no Sistema de Informações sobre Mortalidade: um estudo para Maceió, Alagoas, Brasil, 2001-2002. Cad Saude Publica. 2007;23:2385-95.-88 Almeida MC, Gomes CM, Nascimento LF. Spatial analysis of neonatal mortality in the state of São Paulo, 2006-2010. Rev Paul Pediatr. 2014;32:374-80. However, the maternal causes constitute a complementary factor of equal importance, with a significant contribution to neonatal mortality in developing countries. 55 Rodrigues NC, Monteiro DL, Almeida AS, Barros MB, Pereira Neto A, O'Dwyer G, et al. Temporal and spatial evolution of maternal and neonatal mortality rates in Brazil, 1997-2012. J Pediatr (Rio J). 2016;92:567-73.,88 Almeida MC, Gomes CM, Nascimento LF. Spatial analysis of neonatal mortality in the state of São Paulo, 2006-2010. Rev Paul Pediatr. 2014;32:374-80. Nevertheless, there is no systematic evaluation of all these factors in Brazil at this time.
A systematic review with meta-analysis constitutes a real possibility to assess the impact of risk factors on neonatal mortality in the Brazilian territory, aiding clinical decision-making and the professionals' epidemiological understanding of the situation, especially by public health managers in Brazil.99 Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;:4:1. The study aims to identify, through a systematic review and meta-analysis of observational studies, which risk factors are significantly associated with neonatal mortality in Brazil, and to build a comprehensive national analysis on the subject.
Methods
A PROSPERO protocol (https://www.crd.york.ac.uk/prospero/) was published under No. CRD42018108716.
Study selection, data extraction, and risk of bias analysis were independently performed by two authors. The differences were resolved by consensus between the authors; if there was no consensus, a third author would end the impasse.
Eligibility criteria
The inclusion criteria consisted of the following items: observational studies on neonatal mortality; studies carried out between 2000 and 2018; studies carried out in Brazilian cities; studies that used adjusted risk measures, together with their confidence intervals; studies that employed one or more of the following exposure factors: maternal schooling and/or marital status of the mother and/or maternal age (years) and/or gender of the newborn and/or type of delivery and/or previous stillbirth and/or type of gestation and/or adequacy of prenatal care and/or maternal complications and/or birth weight (g) and/or gestational age (weeks) and/or congenital malformation and/or Apgar at the 5th minute of life.
Databases
The main databases used for this study were MEDLINE, accessed via PubMed (https://www.ncbi.nlm.nih.gov/pubmed/) and Bireme (http://bvsalud.org/). The secondary database was Elsevier (https://www.sciencedirect.com/). The regional databases were LILACS (http://bvsalud.org/) and SciELO (http://www.scielo.org/php/index.php). The grey literature database was OPENGREY (http://www.opengrey.eu/).
Search strategy
The search strategy was defined based on the PECOS strategy (Patients | Exposure | Comparison | Outcome | Type of study). Therefore, two base strategies were constructed, one in the English language, using MeSH terms (https://www.ncbi.nlm.nih.gov/mesh), and another in the Portuguese language, using DeCS terms (http://decs.bvs.br/), as follows:
-
(early neonatal mortality OR neonatal mortality OR perinatal mortality OR infant mortality) AND (risk factors OR socioeconomic factors OR low birth weight OR perinatal care) AND (Brazil OR Brasil) AND (case control studies OR cohort studies);
-
(mortalidade neonatal OR mortalidade perinatal OR mortalidade infantil) AND (fatores de risco OR fatores socioeconômicos OR baixo peso ao nascer) AND (caso-controle OR coorte).
Study selection
Study selection consisted of three stages: title phase, abstract phase, and full-article phase, which started after the searches in all the databases. In addition to this selection, the inclusion of the articles was complemented by the search for help from specialists in the area upon finding studies relevant to this review. Duplicates were removed with the help of Mendeley software (Mendeley, version 1.17.1,1 Elsevier - NY, USA).
Data extraction
A spreadsheet was created using Microsoft Excel software (Microsoft, Excel software, version 2016, WA, USA) containing the following elements: name of the authors of the study; city and state of the study; year of study; type of study; total number of study subjects; adjusted risk measures, and confidence intervals of the included exposure factors.
Factors of exposure and outcome
The assessed exposure factors were: "maternal schooling," "mother's marital status," "maternal age (years)," "newborn's gender," "previous stillbirth," "type of pregnancy," "prenatal care adequacy," "complications during the pregnancy," "birth weight," "congenital malformation," "Apgar at the 5th minute," "gestational age (weeks)," and "type of delivery." The outcome was neonatal mortality.
Risk of bias in individual studies
The risk of bias was based on the Newcastle-Ottawa Scale (NOS)1010 Wells GA, Shea B, O'Cornell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [cited 2018 Sep 14]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
http://www.ohri.ca/programs/clinical_epi...
to assess the quality of non-randomized studies in a meta-analysis. The NOS evaluates the bias regarding three aspects: the selection of study groups; the comparability of groups; the determination of exposure for case-control studies, or the outcome of interest for cohort studies. A maximum of four stars is given to the first aspect; to the second, two stars; and, finally, to the third, three stars.
Analysis of data
The data analysis was based on the quantitative study of the variables. Stata 12 software (StataCorp - College Station - TX, USA) was used for this investigation. The analyzed data were the adjusted risk measures in each exposure factor analyzed, in addition to their confidence intervals. The natural logarithms of the risk measures and of their confidence intervals, the DerSimonian and Laird method as a random effects model, and the Mantel-Haenszel model for estimation of heterogeneity were used. A confidence level of 95% was considered.
Heterogeneity was considered important when I2 was >50%. If necessary, the sensitivity analysis was performed by removing the studies one by one to investigate the origin of the divergence. The evaluation of publication bias was performed using a funnel plot.
Results
Study selection
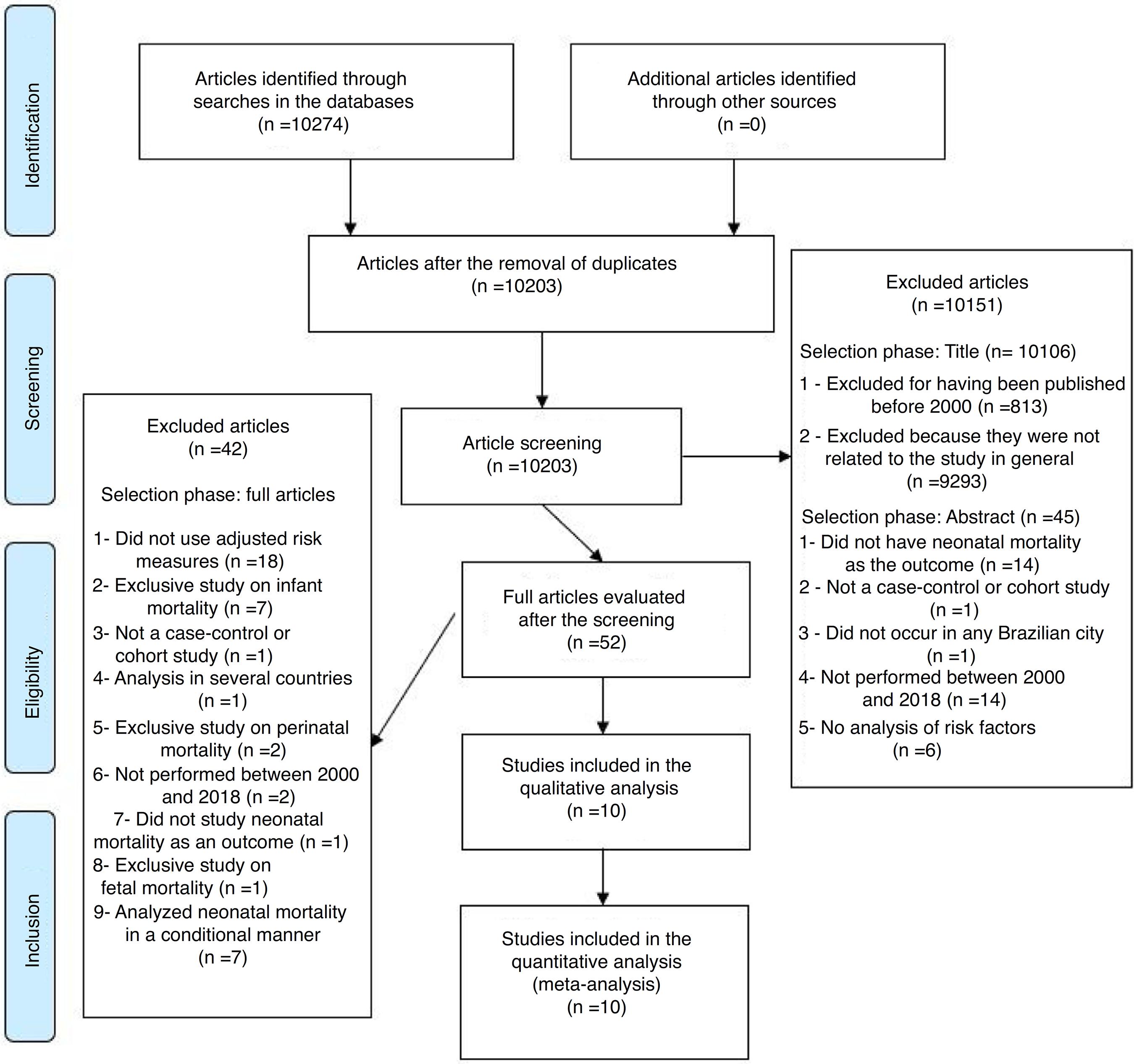
The search in the databases identified 10,274 articles. Of these, 61 were duplicates, resulting in 10,203 articles. After reading all the titles, 98 articles were chosen to be analyzed in the abstract phase. At the end of this phase, 17 articles were selected, of which ten articles were included in the study 33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.
12 Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35.
13 Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.
14 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.
15 Paulucci RS, Nascimento LF. Mortalidade neonatal em Taubaté: um estudo caso-controle. Rev Paul Pediatr. 2007;25:358-63.
16 Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.
17 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85.-1818 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8. (Fig. 1). The overall characteristics of the ten studies included in the analysis are available in Table 1 and the characteristics relevant to the quantitative analysis are shown in Table 2.
Bias risk assessment of included studies
The ten studies included in the present analysis were qualitatively assessed using the Newcastle-Ottawa Scale. Four studies33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,1313 Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.,1616 Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.,1717 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85. obtained a high classification, i.e., they show low risk of bias. However, six studies 66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.,1212 Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35.,1414 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.,1515 Paulucci RS, Nascimento LF. Mortalidade neonatal em Taubaté: um estudo caso-controle. Rev Paul Pediatr. 2007;25:358-63.,1818 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8. obtained an intermediate-high classification, thus showing an intermediate-low risk (Table 3).
Analysis of data of the included studies
Fig. 2 shows the overall association between the analyzed factors and the association with neonatal mortality, represented in the image by the final adjusted odds ratios (faOR) and their respective confidence intervals. The result of each exposure factor can be seen below, separately.
Overall view of factors associated with neonatal mortality. Abbreviations: OR, odds ratio; CI, confidence interval.
Maternal schooling
Maternal schooling could only be analyzed in two ways: complete elementary school (8-11 years of schooling) and incomplete elementary school (4-7 years of schooling). Complete elementary school did not show a significant association with neonatal mortality (faOR = 1.853; 95% CI: [0.417-8.241]; p = 0.418; I2 = 87.4%; p = 0.005). The same was observed for incomplete elementary school (faOR = 1.727, 95% CI: [0.466-6.400], p = 0.414, I2 = 84.8%, p = 0.010).
Mother's marital status
The pregnancy of mothers who did not have a partner showed a significantly higher chance of neonatal mortality (faOR = 2.236, 95% CI: [1.630-3.068], p < 0.001, I2 = 0.0%, p = 0.344).
Maternal age
The pregnancy of mothers aged 35 years or older showed a significantly higher chance of neonatal mortality (faOR = 1.568, 95% CI: [1.141-2.154], p = 0.006, I2 = 0.0%, p = 0.882).
Newborn's gender
Male newborns had a significantly higher chance of neonatal mortality (faOR = 1.591, 95% CI: [1.193-2.121], p = 0.002, I2 = 0.0%, p = 0.362).
Previous stillbirth
The pregnancy of mothers who had a previous stillbirth did not show a significant association with neonatal mortality (faOR = 2.090, 95% CI: [0.762-5.733], p = 0.152, I2 = 90.6%, p = 0.001).
Type of pregnancy
A multiple pregnancy showed a significantly higher chance of neonatal mortality (faOR = 3.361, 95% CI: [1.612-7.009], p = 0.001, I2 = 48.7%, p = 0.163).
Adequacy of prenatal care
It was only possible to analyze the inadequacy and absence of prenatal care. Inadequate prenatal care showed a significantly higher chance of neonatal mortality (faOR = 2.182, 95% CI: [1.761-2.703], p < 0.001, I2 = 0.0%, p = 0.771). The same was observed with the absence of prenatal care (faOR = 6.799, 95% CI: [1.534-30.147], p = 0.012, I2 = 78.8%, p = 0.030).
Complications during pregnancy
The presence of complications during pregnancy showed a significantly higher chance of neonatal mortality (faOR = 6.961, 95% CI: [4.979-9.733], p < 0.001, I2 = 0.0%, p = 0.381).
Birth weight
It was only possible to analyze birth weight between 1500 and 2499 g (faOR = 4.044, 95% CI: [2.260-7.238], p < 0.001, I2 = 77.0%, p = 0.013), lower than 1500 g (faOR = 19.752; 95% CI: [5.556-70.223]; p < 0.001; I2 = 90.7%; p < 0.001), and lower than 2500 g (faOR = 9.876; 95% CI: [4.920-19.826]; p < 0.001; I2 = 69.4%; p = 0.003). After the sensitivity analysis, birth weight between 1500 and 2499 g (faOR = 5.424, 95% CI: [4.128-7.126], p < 0.001, I2 = 0.0%, p = 0.902), lower than 1500 g (faOR = 39.995, 95% CI: [29.026-55.109], p < 0.001, I2 = 0.0%, p = 0.633), and lower than 2500 g (faOR = 15.519, 95% CI: [9.997-24,092]; p < 0.001, I2 = 0.0%, p = 0.684) continued to show a significantly higher chance of neonatal mortality after removal of one study in the first and the second described situations,1717 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85. and after the removal of another two in the third situation. 66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,1212 Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35.
Congenital malformation
Newborns with a congenital malformation showed a significantly higher chance of neonatal mortality (faOR = 14.025, 95% CI: [10.849-18.132], p < 0.001, I2 = 0.0%, p = 0.402).
Apgar score at the 5th minute
The presence of an Apgar score less than 7 at the 5th minute showed a significantly higher chance of neonatal mortality (faOR = 12.397, 95% CI: [9.545-16.102], p < 0.001, I2 = 0.0%, p = 0.417).
Gestational age
A gestational age <37 weeks showed a significantly higher chance of neonatal mortality (faOR = 5.738, 95% CI: [2.589-12.716], p < 0.001, I2 = 86.9%, p < 0.001). After the sensitivity analysis, it continued to show a significantly higher chance of neonatal mortality after the removal of three studies1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.,1313 Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.,1818 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8. (faOR = 7.130; 95% CI: [4.329-11.742]; p < 0.001; I2 = 0.0%; p = 0.706).
Type of delivery
Caesarean delivery did not show a significant association with neonatal mortality (faOR = 1.233, 95% CI: [0.688-2.210], p = 0.483, I2 = 89.7%, p < 0.001). When exploring heterogeneity, there was a significantly greater chance of neonatal mortality after a study was removed1717 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85. (faOR = 1.551, 95% CI: 1.202-2.000, p = 0.001, I2 = 0.0%, p = 0.480).
It was not possible to perform a sensitivity analysis on the following factors: complete elementary school, incomplete elementary school, presence of previous stillbirth, and absence of prenatal care, since these analyzes consisted of only two studies. Fig. 3 shows the final overall association after the sensitivity analysis.
Final association of the factors associated with neonatal mortality after the heterogeneity analysis. Abbreviations: OR, odds ratio; CI, confidence interval.
Regarding the publication bias, it was not possible to evaluate it due to the number of studies included in each analysis. Table 4 shows a final summary-table of the results obtained in the quantitative analysis.
Discussion
The study showed that factors related to the mother (absence of partner, age ≥ 35 years, multiple pregnancy, absence or inadequacy of prenatal care, presence of complications during gestation, and Caesarean delivery) and to the newborn (male gender, congenital malformation, perinatal asphyxia, low birth weight, and prematurity) are risks associated to neonatal mortality in Brazil.
The main factor to be considered in this context is low birth weight and, more precisely, very low birth weight. In a prospective cohort study, in which neonatal mortality was analyzed in very low birth weight preterm infants in northeastern Brazil, it was observed that 76% died within the first 24 h of life.1919 Castro EC de, Leite ÁJ, Guinsburg R. Mortalidade com 24 horas de vida de recém-nascidos pré-termo de muito baixo peso da Região Nordeste do Brasil. Rev Paul Pediatr. 2016;34:106-13. This fact was also observed in another prospective cohort carried out in Brazil, based on the analysis of births in 20 public university centres, which resulted in a death rate of 30%,2020 Guinsburg R, De Almeida MF, De Castro JS, Silveira RC, Caldas JP, Fiori HH, et al. Death or survival with major morbidity in VLBW infants born at Brazilian neonatal research network centers. J Matern Neonatal Med. 2016;29:1005-9. thus showing that low birth weight is a determinant factor in the occurrence of neonatal mortality in Brazil, representing its main isolated predictor. 33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.
12 Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35.
13 Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.
14 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.
15 Paulucci RS, Nascimento LF. Mortalidade neonatal em Taubaté: um estudo caso-controle. Rev Paul Pediatr. 2007;25:358-63.
16 Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.
17 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85.
18 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8.-1919 Castro EC de, Leite ÁJ, Guinsburg R. Mortalidade com 24 horas de vida de recém-nascidos pré-termo de muito baixo peso da Região Nordeste do Brasil. Rev Paul Pediatr. 2016;34:106-13.,2121 Teixeira GA, Costa FM, Mata MS, Carvalho JB, Sousa NL, Silva RA. Risk factors for neonatal mortality in the life of first week. Rev Pesqui Cuid Fundam. 2016;8:4036.
22 Borges TS, Vayego SA. Fatores de risco para mortalidade neonatal em um município na região sul. Ciênc Saúde. 2015;8:7-14.-2323 Varga P, Berecz B, Gasparics Á, Dombi Z, Varga Z, Jeager J, et al. Morbidity and mortality trends in very-very low birth weight premature infants in light of recent changes in obstetric care. Eur J Obstet Gynecol Reprod Biol. 2017;211:134-9. Low birth weight is considered one of the main risk factors for neonatal mortality in numerous locations and services, as observed in the studies carried out in Mexico,2424 Reyes JC. Neonatal mortality and associated factors in newborn infants admitted to a Neonatal Care Unit. Arch Argent Pediatr. 2018;116:42-8. Jordan,2525 Obeidat N, Khader Y, Batieha A, Abdel Razeq N, Al-Sheyab N, Khassawneh M. Neonatal mortality in Jordan: secondary analysis of Jordan Population and Family Health Survey (JPFHS) data. J Matern Neonatal Med. 2019;32:217-24. Trinidad & Tobago,2626 Cupen K, Barran A, Singh V, Dialsingh I. Risk factors associated with preterm neonatal mortality: a case study using data from Mt. Hope Women's Hospital in Trinidad and Tobago. Children (Basel). 2017;4:E108. the United States,2727 Ratnasiri AW, Parry SS, Arief VN, DeLacy IH, Halliday LA, DiLibero RJ, et al. Recent trends, risk factors, and disparities in low birth weight in California, 2005-2014: a retrospective study. Matern Heal Neonatol Perinatol. 2018;4:15. and China.2828 Hon KL, Liu S, Chow JC, Tsang KY, Lam H, So KW, et al. Mortality and morbidity of extremely low birth weight infants in Hong Kong, 2010-2017: a single-centre review. Hong Kong Med J. 2018;24:460-5.
Similarly to low birth weight, other factors are modifiable, such as perinatal asphyxia, prematurity, complications during pregnancy, prenatal care, caesarean delivery, older maternal age, and absence of a partner at home. 33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.,1414 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.,1717 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85.,1919 Castro EC de, Leite ÁJ, Guinsburg R. Mortalidade com 24 horas de vida de recém-nascidos pré-termo de muito baixo peso da Região Nordeste do Brasil. Rev Paul Pediatr. 2016;34:106-13.,2121 Teixeira GA, Costa FM, Mata MS, Carvalho JB, Sousa NL, Silva RA. Risk factors for neonatal mortality in the life of first week. Rev Pesqui Cuid Fundam. 2016;8:4036.,2222 Borges TS, Vayego SA. Fatores de risco para mortalidade neonatal em um município na região sul. Ciênc Saúde. 2015;8:7-14.,2929 Abdullah A, Hort K, Butu Y, Simpson L. Risk factors associated with neonatal deaths: a matched case-control study in Indonesia. Glob Health Action. 2016;9:30445.
30 Kaboré R, Meda IB, Koulidiati JE, Millogo T, Kouanda S. Factors associated with very early neonatal mortality in Burkina Faso: a matched case-control study. Int J Gynecol Obstet. 2016;135:S93-7.
31 Park JH, Chang YS, Ahn SY, Sung SI, Park WS. Predicting mortality in extremely low birth weight infants: comparison between gestational age, birth weight Apgar score, CRIB II score, initial and lowest serum albumin levels. PLoS ONE. 2018;13:e0192232.
32 Demitto MD, Gravena AAF, Millene C, Agnolo D, Antunes MB, Pelloso SM. Gestação de alto risco e fatores associados ao óbito neonatal. Rev Esc Enferm USP. 2017;51:e03208.-3333 Miranda MH, Fernandes FE, Campos ME. Determinantes associados à mortalidade perinatal e fatores associados. Rev Enferm UFPE Online. 2017;11:1171-8. In this context, it is worth highlighting the prenatal care, which, when properly performed, contributes to the reduction of other modifiable factors, mainly prematurity and low birth weight. 33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.,1414 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.,1616 Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.
17 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85.-1818 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8. This importance can be verified in a cross-sectional study carried out in a municipality in the Southeast region of Brazil, which showed that 26.8% of the deaths could have been prevented if an adequate prenatal care had been performed.3434 Vidal E, Silva SM, Tuon RA, Probst LF, Gondinho BV, Pereira AC, et al. Factors associated with preventable infant death: a multiple logistic regression. Rev Saude Publica. 2018;52:32. A similar example can be found in another cross-sectional study conducted in several municipalities in a state in the Brazilian Southeast region, which showed that 47% of deaths could have been prevented through the implementation of early prevention, diagnosis, and treatment actions.3535 Da Silva PL, Costa AD, Farias HM, Rocha LM, Oliveira MA, Damasceno RF. Evitabilidade da mortalidade infantil na região de saúde de Janaúba/Monte Azul, Minas Gerais, Brasil. J Heal Biol Sci. 2017;6:35. These rates indicate problems in the care given to the pregnant woman, due to the lack of professional qualification or a deficient structure. 2121 Teixeira GA, Costa FM, Mata MS, Carvalho JB, Sousa NL, Silva RA. Risk factors for neonatal mortality in the life of first week. Rev Pesqui Cuid Fundam. 2016;8:4036.,3232 Demitto MD, Gravena AAF, Millene C, Agnolo D, Antunes MB, Pelloso SM. Gestação de alto risco e fatores associados ao óbito neonatal. Rev Esc Enferm USP. 2017;51:e03208.,3333 Miranda MH, Fernandes FE, Campos ME. Determinantes associados à mortalidade perinatal e fatores associados. Rev Enferm UFPE Online. 2017;11:1171-8.,3636 Filho AC, Sales IM, Araújo AK, Almeida PD, Rocha SS. Aspectos epidemiológicos da mortalidade neonatal em capital do Nordeste do Brasil. Rev Cuid. 2017;8:1767-76.
37 Liao XP, Chipenda-Dansokho S, Lewin A, Abdelouahab N, Wei SQ. Advanced neonatal medicine in China: a national baseline database. PLoS One. 2017;12:1-15.
38 Wilmot E, Yotebieng M, Norris A, Ngabo F. Missed opportunities in neonatal deaths in Rwanda: applying the three delays model in a cross-sectional analysis of neonatal death. Matern Child Health J. 2017;21:1121-9.-3939 Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region Northern Ethiopia: prospective cohort study. BMC Pregnancy Childbirth. 2016;16:202.
As with prenatal care, caesarean delivery, if correctly indicated, reduces the occurrence of prematurity, low birth weight, and perinatal asphyxia. 33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,77 Pedrosa LD, Sarinho SW, Ordonha MR. Análise da qualidade da informação sobre causa básica de óbitos neonatais registrados no Sistema de Informações sobre Mortalidade: um estudo para Maceió, Alagoas, Brasil, 2001-2002. Cad Saude Publica. 2007;23:2385-95.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.
12 Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35.
13 Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.
14 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.
15 Paulucci RS, Nascimento LF. Mortalidade neonatal em Taubaté: um estudo caso-controle. Rev Paul Pediatr. 2007;25:358-63.
16 Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.
17 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85.-1818 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8. One of the big problems is the incorrect indication and excessive number of this type of delivery. The rate of caesarean deliveries in Brazil is 56%, well above the recommended rate, which is 15%.4040 Ribeiro LB. Nascer em Belo Horizonte: Cesarianas desnecessárias e prematuridade [dissertation]. Universidade Federal de Minas Gerais, Escola de Enfermagem: Belo Horizonte; 2016. In a multicenter, observational, hospital-based study carried out in the Northeast region of Brazil, it was observed that 13.7% of neonatal deaths were related to caesarean delivery in high-risk neonatal units.4141 Silva CF, Leite AJ, Almeida NM, Leon AC, Olofin I. Factors associated with neonatal death in high-risk infants: a multicenter study in high-risk neonatal units in Northeast Brazil. Cad Saude Publica. 2014;30:355-68.
Congenital malformation, multiple pregnancy, and the newborn's male gender were found to be determinants of neonatal mortality in Brazil in the present study, but they are not modifiable factors. 33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.,66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,77 Pedrosa LD, Sarinho SW, Ordonha MR. Análise da qualidade da informação sobre causa básica de óbitos neonatais registrados no Sistema de Informações sobre Mortalidade: um estudo para Maceió, Alagoas, Brasil, 2001-2002. Cad Saude Publica. 2007;23:2385-95.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.
12 Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35.
13 Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.
14 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.
15 Paulucci RS, Nascimento LF. Mortalidade neonatal em Taubaté: um estudo caso-controle. Rev Paul Pediatr. 2007;25:358-63.
16 Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.
17 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85.-1818 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8.,3232 Demitto MD, Gravena AAF, Millene C, Agnolo D, Antunes MB, Pelloso SM. Gestação de alto risco e fatores associados ao óbito neonatal. Rev Esc Enferm USP. 2017;51:e03208. Of these, congenital malformation is the most important factor, being the second most decisive factor for neonatal mortality in Brazil. A cross-sectional observational study carried out in several municipalities of a state in the Brazilian Southeast region showed that 42.8% of infant deaths were caused by this factor.3535 Da Silva PL, Costa AD, Farias HM, Rocha LM, Oliveira MA, Damasceno RF. Evitabilidade da mortalidade infantil na região de saúde de Janaúba/Monte Azul, Minas Gerais, Brasil. J Heal Biol Sci. 2017;6:35. The same trend can be observed in a prospective cohort carried out in a Mexican city, which showed in a neonatal mortality rate of 32%.2424 Reyes JC. Neonatal mortality and associated factors in newborn infants admitted to a Neonatal Care Unit. Arch Argent Pediatr. 2018;116:42-8.
The knowledge of risk factors is essential for the prevention of neonatal mortality in Brazil, since health professionals and managers, when aware of these conditions, can find ways to prevent clinical and structural complications. 2121 Teixeira GA, Costa FM, Mata MS, Carvalho JB, Sousa NL, Silva RA. Risk factors for neonatal mortality in the life of first week. Rev Pesqui Cuid Fundam. 2016;8:4036.,3232 Demitto MD, Gravena AAF, Millene C, Agnolo D, Antunes MB, Pelloso SM. Gestação de alto risco e fatores associados ao óbito neonatal. Rev Esc Enferm USP. 2017;51:e03208.,3333 Miranda MH, Fernandes FE, Campos ME. Determinantes associados à mortalidade perinatal e fatores associados. Rev Enferm UFPE Online. 2017;11:1171-8.,3636 Filho AC, Sales IM, Araújo AK, Almeida PD, Rocha SS. Aspectos epidemiológicos da mortalidade neonatal em capital do Nordeste do Brasil. Rev Cuid. 2017;8:1767-76.
37 Liao XP, Chipenda-Dansokho S, Lewin A, Abdelouahab N, Wei SQ. Advanced neonatal medicine in China: a national baseline database. PLoS One. 2017;12:1-15.
38 Wilmot E, Yotebieng M, Norris A, Ngabo F. Missed opportunities in neonatal deaths in Rwanda: applying the three delays model in a cross-sectional analysis of neonatal death. Matern Child Health J. 2017;21:1121-9.-3939 Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region Northern Ethiopia: prospective cohort study. BMC Pregnancy Childbirth. 2016;16:202. Thus, prevention consists of training professionals and providing adequate structure for the birth, as well as offering an individualized care to the pregnancies, paying individualized attention to the pregnancies, while taking into account the specificity of each condition.3232 Demitto MD, Gravena AAF, Millene C, Agnolo D, Antunes MB, Pelloso SM. Gestação de alto risco e fatores associados ao óbito neonatal. Rev Esc Enferm USP. 2017;51:e03208.,3333 Miranda MH, Fernandes FE, Campos ME. Determinantes associados à mortalidade perinatal e fatores associados. Rev Enferm UFPE Online. 2017;11:1171-8.,3838 Wilmot E, Yotebieng M, Norris A, Ngabo F. Missed opportunities in neonatal deaths in Rwanda: applying the three delays model in a cross-sectional analysis of neonatal death. Matern Child Health J. 2017;21:1121-9.,3939 Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region Northern Ethiopia: prospective cohort study. BMC Pregnancy Childbirth. 2016;16:202. This individualization has become worldwide trend since 2015,4242 Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384:189-205. which has resulted in a 5.4% reduction in global neonatal deaths between 2015 and 2017.4343 United Nations Inter-agency Group for Child Mortality Estimation. Levels and Trends in Child Mortality Report 2018. UNICEF;2018.
The present study consisted of six articles with low bias risk and four articles with intermediate-low bias risk, thus increasing the degree of reliability of this study. The reason for the intermediate classification is due to the non-randomization of the interviewers in three studies, in addition to the inequality between the losses of the case and control groups in another study. The former can be solved by performing randomization and ensuring blind data collection, while equality of losses between groups would solve the second impasse.
The cohort studies were able to equally represent the population, in addition to matching the control group in an equivalent manner. One of the studies33 Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207. used a structured interview, differing from the other three, 1313 Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.,1616 Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.,1717 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85. which used data from official databases. Regarding the final evaluation, all of them used linkage analysis with the official databases, in addition to establishing a sufficient follow-up period for the analysis. During follow-up, one of the studies1717 Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85. showed a loss of less than 10% of the individuals, differing from the other studies, which did not show any loss.
The case-control studies, in turn, used linkage to the official database to adapt and represent cases, as well as to select and define controls. At the final evaluation, three studies 1414 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.,1515 Paulucci RS, Nascimento LF. Mortalidade neonatal em Taubaté: um estudo caso-controle. Rev Paul Pediatr. 2007;25:358-63.,1818 Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8. used linkage analysis with data from official databases, while the other three 66 Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.,1111 Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.,1212 Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35. performed interviews without the blinding procedure. One of the studies1414 Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22. showed an unequal loss between the case and control groups, but because it was less than 10%, the final effect was not harmed. However, despite this statistical effect, the Newcastle-Ottawa Scale does not score this fact in the case-control studies. In relation to the other studies, the rates were the same in both groups.
The overall result of this study shows the importance of these risk factors for neonatal mortality in Brazil, highlighting, in this context, the power that structural, behavioural, and medical changes have in reducing these rates.
The most significant risk factors shown in this study are modifiable, making it possible to achieve a real reduction in neonatal deaths, which remain high in Brazil.
-
Study conducted at Universidade Estadual de Ciências da Saúde de Alagoas, Maceió, AL, Brazil.
-
☆
Please cite this article as: Veloso FC, Kassar LM, Oliveira MJ, Lima TH, Bueno NB, Gurgel RQ, et al. Analysis of neonatal mortality risk factors in Brazil: a systematic review and meta-analysis of observational studies. J Pediatr (Rio J). 2019;95:519-30.
-
FundingThis work was funded by the Conselho Nacional de Pesquisa e Desenvolvimento Científico e Tecnológico (No. 129015/2017-2).
References
-
1Lehtonen L, Gimeno A, Parra-Llorca A, Vento M. Early neonatal death: a challenge worldwide. Semin Fetal Neonatal Med. 2017;22:153-60.
-
2Blencowe H, Calvert C, Lawn JE, Cousens S, Campbell OM. Measuring maternal, foetal and neonatal mortality: challenges and solutions. Best Pract Res Clin Obstet Gynaecol. 2016;36:14-29.
-
3Lansky S, Lima Friche AA, Silva AA, Campos D, Azevedo Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: neonatal mortality, pregnancy and childbirth quality of care. Cad Saude Publica. 2014;30:S192-207.
-
4United Nations Inter-agency Group for Child Mortality Estimation. Levels and Trends in Child Mortality Report 2017. UNICEF; 2017.
-
5Rodrigues NC, Monteiro DL, Almeida AS, Barros MB, Pereira Neto A, O'Dwyer G, et al. Temporal and spatial evolution of maternal and neonatal mortality rates in Brazil, 1997-2012. J Pediatr (Rio J). 2016;92:567-73.
-
6Kassar SB, Melo AM, Coutinho SB, Lima MC, Lira PI. Determinants of neonatal death with emphasis on health care during pregnancy, childbirth and reproductive history. J Pediatr (Rio J). 2013;89:269-77.
-
7Pedrosa LD, Sarinho SW, Ordonha MR. Análise da qualidade da informação sobre causa básica de óbitos neonatais registrados no Sistema de Informações sobre Mortalidade: um estudo para Maceió, Alagoas, Brasil, 2001-2002. Cad Saude Publica. 2007;23:2385-95.
-
8Almeida MC, Gomes CM, Nascimento LF. Spatial analysis of neonatal mortality in the state of São Paulo, 2006-2010. Rev Paul Pediatr. 2014;32:374-80.
-
9Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;:4:1.
-
10Wells GA, Shea B, O'Cornell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [cited 2018 Sep 14]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
» http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp -
11Nascimento RM, Leite ÁJ, Almeida NM, Almeida PC, Silva CF. Determinantes da mortalidade neonatal: estudo caso-controle em Fortaleza, Ceará, Brasil. Cad Saude Publica. 2012;28:559-72.
-
12Almeida SD, Barros MB. Atenção à saúde e mortalidade neonatal: estudo caso-controle realizado em Campinas, SP. Rev Bras Epidemiol. 2004;7:22-35.
-
13Zanini RR, de Moraes AB, Giugliani ER, Riboldi J. Determinantes contextuais da mortalidade neonatal no Rio Grande do Sul por dois modelos de análise. Rev Saude Publica. 2011;45:79-89.
-
14Schoeps D, Almeida MF, Alencar GP, França I, Novaes HM, Siqueira AA, et al. Fatores de risco para mortalidade neonatal precoce. Rev Saude Publica. 2007;41:1013-22.
-
15Paulucci RS, Nascimento LF. Mortalidade neonatal em Taubaté: um estudo caso-controle. Rev Paul Pediatr. 2007;25:358-63.
-
16Garcia LP, Fernandes CM, Traebert J. Risk factors for neonatal death in the capital city with the lowest infant mortality rate in Brazil. J Pediatr (Rio J). 2019;95:194-200.
-
17Lima EdeF, Sousa AI, Griep RH, Primo CC. Fatores de risco para mortalidade neonatal no município de Serra, Espírito Santo. Rev Bras Enferm. 2012;65:578-85.
-
18Mendes KG, Olinto MT, Costa JS. Case-control study on infant mortality in Southern Brazil. Rev Saude Publica. 2006;40:240-8.
-
19Castro EC de, Leite ÁJ, Guinsburg R. Mortalidade com 24 horas de vida de recém-nascidos pré-termo de muito baixo peso da Região Nordeste do Brasil. Rev Paul Pediatr. 2016;34:106-13.
-
20Guinsburg R, De Almeida MF, De Castro JS, Silveira RC, Caldas JP, Fiori HH, et al. Death or survival with major morbidity in VLBW infants born at Brazilian neonatal research network centers. J Matern Neonatal Med. 2016;29:1005-9.
-
21Teixeira GA, Costa FM, Mata MS, Carvalho JB, Sousa NL, Silva RA. Risk factors for neonatal mortality in the life of first week. Rev Pesqui Cuid Fundam. 2016;8:4036.
-
22Borges TS, Vayego SA. Fatores de risco para mortalidade neonatal em um município na região sul. Ciênc Saúde. 2015;8:7-14.
-
23Varga P, Berecz B, Gasparics Á, Dombi Z, Varga Z, Jeager J, et al. Morbidity and mortality trends in very-very low birth weight premature infants in light of recent changes in obstetric care. Eur J Obstet Gynecol Reprod Biol. 2017;211:134-9.
-
24Reyes JC. Neonatal mortality and associated factors in newborn infants admitted to a Neonatal Care Unit. Arch Argent Pediatr. 2018;116:42-8.
-
25Obeidat N, Khader Y, Batieha A, Abdel Razeq N, Al-Sheyab N, Khassawneh M. Neonatal mortality in Jordan: secondary analysis of Jordan Population and Family Health Survey (JPFHS) data. J Matern Neonatal Med. 2019;32:217-24.
-
26Cupen K, Barran A, Singh V, Dialsingh I. Risk factors associated with preterm neonatal mortality: a case study using data from Mt. Hope Women's Hospital in Trinidad and Tobago. Children (Basel). 2017;4:E108.
-
27Ratnasiri AW, Parry SS, Arief VN, DeLacy IH, Halliday LA, DiLibero RJ, et al. Recent trends, risk factors, and disparities in low birth weight in California, 2005-2014: a retrospective study. Matern Heal Neonatol Perinatol. 2018;4:15.
-
28Hon KL, Liu S, Chow JC, Tsang KY, Lam H, So KW, et al. Mortality and morbidity of extremely low birth weight infants in Hong Kong, 2010-2017: a single-centre review. Hong Kong Med J. 2018;24:460-5.
-
29Abdullah A, Hort K, Butu Y, Simpson L. Risk factors associated with neonatal deaths: a matched case-control study in Indonesia. Glob Health Action. 2016;9:30445.
-
30Kaboré R, Meda IB, Koulidiati JE, Millogo T, Kouanda S. Factors associated with very early neonatal mortality in Burkina Faso: a matched case-control study. Int J Gynecol Obstet. 2016;135:S93-7.
-
31Park JH, Chang YS, Ahn SY, Sung SI, Park WS. Predicting mortality in extremely low birth weight infants: comparison between gestational age, birth weight Apgar score, CRIB II score, initial and lowest serum albumin levels. PLoS ONE. 2018;13:e0192232.
-
32Demitto MD, Gravena AAF, Millene C, Agnolo D, Antunes MB, Pelloso SM. Gestação de alto risco e fatores associados ao óbito neonatal. Rev Esc Enferm USP. 2017;51:e03208.
-
33Miranda MH, Fernandes FE, Campos ME. Determinantes associados à mortalidade perinatal e fatores associados. Rev Enferm UFPE Online. 2017;11:1171-8.
-
34Vidal E, Silva SM, Tuon RA, Probst LF, Gondinho BV, Pereira AC, et al. Factors associated with preventable infant death: a multiple logistic regression. Rev Saude Publica. 2018;52:32.
-
35Da Silva PL, Costa AD, Farias HM, Rocha LM, Oliveira MA, Damasceno RF. Evitabilidade da mortalidade infantil na região de saúde de Janaúba/Monte Azul, Minas Gerais, Brasil. J Heal Biol Sci. 2017;6:35.
-
36Filho AC, Sales IM, Araújo AK, Almeida PD, Rocha SS. Aspectos epidemiológicos da mortalidade neonatal em capital do Nordeste do Brasil. Rev Cuid. 2017;8:1767-76.
-
37Liao XP, Chipenda-Dansokho S, Lewin A, Abdelouahab N, Wei SQ. Advanced neonatal medicine in China: a national baseline database. PLoS One. 2017;12:1-15.
-
38Wilmot E, Yotebieng M, Norris A, Ngabo F. Missed opportunities in neonatal deaths in Rwanda: applying the three delays model in a cross-sectional analysis of neonatal death. Matern Child Health J. 2017;21:1121-9.
-
39Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region Northern Ethiopia: prospective cohort study. BMC Pregnancy Childbirth. 2016;16:202.
-
40Ribeiro LB. Nascer em Belo Horizonte: Cesarianas desnecessárias e prematuridade [dissertation]. Universidade Federal de Minas Gerais, Escola de Enfermagem: Belo Horizonte; 2016.
-
41Silva CF, Leite AJ, Almeida NM, Leon AC, Olofin I. Factors associated with neonatal death in high-risk infants: a multicenter study in high-risk neonatal units in Northeast Brazil. Cad Saude Publica. 2014;30:355-68.
-
42Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384:189-205.
-
43United Nations Inter-agency Group for Child Mortality Estimation. Levels and Trends in Child Mortality Report 2018. UNICEF;2018.
Publication Dates
-
Publication in this collection
28 Oct 2019 -
Date of issue
Sep-Oct 2019
History
-
Received
19 Oct 2018 -
Accepted
18 Dec 2018 -
Published
18 Dec 2018