Abstracts
OBJECTIVE: To estimate which is the best period to realize uterine artery Doppler for the prediction of pregnancy complications. MATERIALS AND METHODS: A prospective study was conducted with 45 women without a history of chronic diseases and in their first pregnancy. The uterine artery Doppler was performed between the pregnancy weeks 18-20, 24-26, 28-30 and 34-36, with determination of the resistance index, the pulsatility index, the A/B ratio and presence or absence of notch on the flow velocity waveform, as well as the result of the pregnancy. RESULTS: The Doppler index showed decrease in the course of the pregnancy, more pronounced in the normal pregnancies in comparison with the complicated pregnancies. This was most noticed in the examinations performed between the weeks 24-26. The best sensitivity/specificity relation for detecting pregnancy complications was achieved in the examination performed in this same period. CONCLUSION: The best period to perform uterine artery Doppler for prediction of pregnancy complications is between weeks 24-26 of gestation.
Doppler; Uterine artery; Preeclampsia; Intrauterine growth restriction
OBJETIVO: Avaliar, prospectivamente, qual o melhor período para a realização do Doppler das artérias uterinas na predição de complicações da gestação. MATERIAIS E MÉTODOS: Foi conduzido estudo prospectivo em 45 pacientes primigestas, sem história de doenças crônicas. O Doppler das artérias uterinas foi realizado entre 18-20, 24-26, 28-30 e 34-36 semanas, com determinação do índice de resistência, índice de pulsatilidade, relação A/B e a presença ou ausência de incisura na onda de velocidade de fluxo, assim como o resultado da gestação. RESULTADOS: Os índices Doppler apresentaram decréscimo com o decorrer da gestação, mais pronunciado nas gestações normais quando estas foram comparadas com aquelas que tiveram complicações, de maneira mais acentuada no exame realizado entre 24-26 semanas. A melhor relação entre sensibilidade e especificidade para a detecção de complicações durante a gestação foi obtida no exame realizado entre 24-26 semanas. CONCLUSÃO: O melhor período para a realização do Doppler das artérias uterinas na predição de complicações da gestação é o intervalo entre 24-26 semanas.
Doppler; Artérias uterinas; Pré-eclâmpsia; Restrição do crescimento intra-uterino
ORIGINAL ARTICLE
Which is the best period to perform uterine artery Doppler in the prediction of pregnancy complications?* * Study developed at the Gynecology and Obstetrics Department of the Ribeirão Preto Faculty of Medicine, Universidade de São Paulo, Ribeirão Preto, SP.
Fabrício da Silva CostaI; Sérgio Pereira da CunhaII; Aderson Tadeu BerezowskiIII
IDoctor Professor of Imagenology in the Course of Medicine, Universidade Estadual do Ceará
IITitular Professor at Gynecology and Obstetrics Department of the Ribeirão Preto Faculty of Medicine, Universidade de São Paulo
IIIDoctor Professor at Gynecology and Obstetrics Department of the Ribeirão Preto Faculty of Medicine, Universidade de São Paulo
Mailing address Mailing address: Prof. Dr. Fabrício da Silva Costa Mestrado Profissional em Saúde da Criança e do Adolescente Centro de Ciências da Saúde, Universidade Estadual do Ceará Avenida Paranjana, 1700, Campus do Itaperi Fortaleza, CE, Brasil 60740-000 E-mail: fabriciouece@hotmail.com
ABSTRACT
OBJECTIVE: To estimate which is the best period to realize uterine artery Doppler for the prediction of pregnancy complications.
MATERIALS AND METHODS: A prospective study was conducted with 45 women without a history of chronic diseases and in their first pregnancy. The uterine artery Doppler was performed between the pregnancy weeks 1820, 2426, 2830 and 3436, with determination of the resistance index, the pulsatility index, the A/B ratio and presence or absence of notch on the flow velocity waveform, as well as the result of the pregnancy.
RESULTS: The Doppler index showed decrease in the course of the pregnancy, more pronounced in the normal pregnancies in comparison with the complicated pregnancies. This was most noticed in the examinations performed between the weeks 2426. The best sensitivity/specificity relation for detecting pregnancy complications was achieved in the examination performed in this same period.
CONCLUSION: The best period to perform uterine artery Doppler for prediction of pregnancy complications is between weeks 2426 of gestation.
Keywords: Doppler; Uterine artery; Preeclampsia; Intrauterine growth restriction.
INTRODUCTION
Until recently, the placental bed perfusion during the normal pregnancy was indirectly assessed through the study of the hydro-iso-androsterone sulphateclearance(1) or by means of radioisotopes(2). Direct measurements of the uterine arteries flow also were obtained by means of electromagnetic techniques(3). Notwithstanding the great contribution to the current knowledge on uteroplacental flow, these studies have relied on invasive methods and radioisotopes which are currently impracticable, considering their high cost and risk.
Only the incorporation of the Doppler effect to ultrasound equipment by Satomura(4) has enabled Fitzgerald & Drumm(5), for the first time, to study the maternal-fetal circulation in a non-invasive and physiological way.
The normal pregnancy is a result of a complex series of changes in the vascular anatomy of the mother, principally in the uterine perfusion that is fundamental for the pregnancy success. With the implantation of the fertilized ovum in the uterine cavity, the arterial system that irrigates the endometrium and the subjacent myometrium undergoes a series of changes which lead to the uteroplacental circulation. Such changes in the arterial system are a result of the decidua invasion by the trophoblast(6).
One believes that the trophoblastic invasion occurs in two waves: the first wave extends from the 6th to the 10th week of gestation and affects the spiral arteries from the distal end, up to the border between the basal decidua and the myometrium; the second wave starts between the 14th and 16th weeks and develops during 4-6 weeks, reaching the myometrial segment of the spiral arteries, including the most distal portions of the radial arteries(7).
These morphologic changes in the uterine vascularization can be demonstrated by the color and pulsed Doppler(8), with detection and analysis of main uterine arteries and their ramifications into arcuate and radial arteries up to their spiral artery terminal branches. The blood flow velocity increases in the uteroplacental circulation, while its impedance decreases as the gestation develops. The studies of Valentin et al.(9) showed that the impedance index decreased with the gestation evolution in both uterine arteries, but this decrease was lower in the arteries contralateral to the placenta.
Studies in which placental bed biopsies were performed on the third quarter of gestation, have reported inappropriate or abnormal trophoblastic invasion as predominant lesion in women with preeclampsia; the mechanism responsible for this failure still remains to be known(10). These histologic findings have a good correlation with the increase of resistance to the flow in the uterine arteries evaluated by Doppler(11) and a relation of this increase in resistance and the subsequent onset of preeclampsia(12,13).
Using Doppler as a screening test, several studies have demonstrated an association of abnormalities in the flow velocity waveform of uterine arteries with the subsequent onset of preeclampsia, intrauterine growth restriction (IUGR), premature placental separation (PPS) and preterm delivery (PTD).
The diastolic notch present in the uterine arteries since the beginning of the gestation disappears around the 20th week. Eventually, it may be detected up to the 24th26th week(13). The original study of Campbell et al.(12), using pulsed Doppler, has established a relation between the high resistance flow velocity waveform and preeclampsia and the potential use of uterine artery Doppler as an early predictor of subsequent development of pregnancy-specific hypertensive disease and of the IUGR.
A study by Chan et al.(14), utilizing the Color Doppler in a medium risk population demonstrated a better preeclampsia prediction at the 20th week of gestation, considering as an altered Doppler the combination of a resistance index (RI) higher than a 90th percentile with the presence of bilateral notch.
Based on three parameters of maternal uterine arteries (A/B ratio, presence of notch and difference of the A/B ratio among the arteries), Boller & Cabral(15) have evaluated 108 high risk pregnant women and observed that, with the uterine artery Doppler, it is possible to establish an accurate maternal prognosis. The presence of notch in the artery homolateral to the placenta was the main isolated finding to be associated with poor gestational prognosis.
A recent study with women undergoing Doppler between the 18th and the 20th weeks has demonstrated the presence of bilateral notch in 27.7% of the cases. The sensitivity of the bilateral notch to the preeclampsia was of 100%, but the positive predictive value (PPV) was just 19.0%. Combining the presence of bilateral notch and the A/B ratio > 2.6, there was a small decrease in sensitivity (87.5%), but an expressive increase in PPV to 67.7% was observed(16).
Silva(17), in a recent study using transvaginal ultrasound, has evaluated the changes in the uterine, ovarian, umbilical and embryonic arteries in the first quarter of gestation. The resistance index and the pulsatility index in the uterine artery showed significant changes with gestational age development, but these changes were not significant in the other vessels assessed. The author has concluded that the transvaginal pulsed color Doppler is a highly effective, non-invasive method, that can evaluate the vasculature in the early pregnancy; besides being innocuous to the embryo and easily reproducible.
The preeclampsia and the IUGR are associated with significant perinatal morbidity and mortality and the prevention of these entities remains as an important objective of the obstetric assistance.
Nevertheless, it is important to take into consideration that other studies have adopted different methodologies and Doppler examinations were performed at different gestational ages.
In this study we have prospectively evaluated the best period to perform the uterine artery Doppler for the prediction of pregnancy complications.
MATERIALS AND METHODS
This study casuistic included 45 women in their first gestation, without a history of chronic, gestational or gynecologic diseases, assisted at the Department of Gynecology and Obstetrics Prenatal Ambulatory at the Hospital of Clinics of the "Faculdade de Medicina de Ribeirão Preto (HCFMRP) da Universidade de São Paulo" or at the Municipal Public Health Service of Ribeirão Preto, SP, and referred for ultrasonographic gestational assessment. This study was approved by the Committee of Ethics on Research of the HCFMRP. The examinations were performed after a previous explanation to the patients and signature of a term of free and conscious consent.
The determination of the gestational age was based on the date of the last menstruation and on transvaginal ultrasound performed at the first quarter of pregancy in the patient's unit of origin or by the researcher in the case of absence of a previous examination.
The patients kept undergoing the pre-natal follow-up at their respective units of origin till the end of the gestation. In cases of intercurrent events or upon request of the physician providing pre-natal care, the women were offered extra-protocol examinations. In cases of complicated pregancy, the patients were referred for follow-up at the Pathologic Pre-Natal Care Ambulatory of the HCFMRP Department of Gynecology and Obstetrics.
The exclusion criteria of this study were: the existence of chronic, gestational or gynecologic diseases, chronic use of medications, smoking, multiple gestations, presence of fetal malformations, miscarriage, non attendance to scheduled return consultations and labor in other hospitals.
Patients always were examined by the same observer, after (spontaneous) urination, in dorsal decubitus position, the table tilted at 45°. The equipment was an ATL (Advanced Technologies Laboratories, USA), model HDI 3000, coupled with a 25 MHz (wide band) convex transducer, with color Doppler and power Doppler; the filter was adjusted at 100 Hz.
The Doppler study was performed between weeks 1820, 2426, 2830 and 3436 of pregnancy. The vessels evaluated by the Doppler method were the ascendent branches of the right and left uterine arteries. For the purpose of examination, the transducer was placed on the abdomen inferior lateral quadrant, in a medially angulated position. The color Doppler was used to identify the uterine artery homolateral to the transducer, on the intersection with the external iliac artery, and the volume sample was placed approximately at 1 cm of the crossing point (Figure 1). The Doppler indexes average measurements were performed when five similar and satisfactory flow velocity waveforms were observed. Additionally, the presence or absence of notches in the uterine arteries was evaluated.
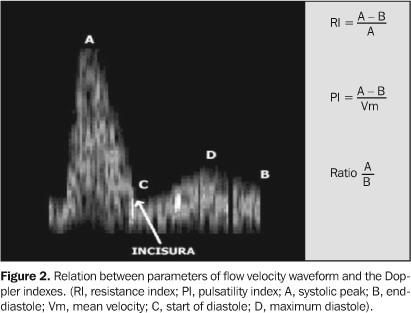
The impedance indexes used were those established in the literature: RI, PI and A/B ratio. The presence of bilateral notch in the uterine arteries was considered as an abnormality in the flow velocity waveform (Figure 2).
In the absence of complications, the patients underwent pre-natal follow-up at their respective units of origin. Those who had diagnosis of any complication, underwent follow-up at the HCFMRP, returning at pre-scheduled periods for assessment by the researcher. Labors occurred in the Obstetric Center of the HCFMRP. The neonates were received and followed-up by the team of the Pediatrics and Puericulture Department in the mentioned hospital.
The patients were divided into two groups, according to their gestational evolution and perinatal results. The group 1 consisted of women who did not presented any gestational or perinatal complications, while the group 2 consisted of women who developed gestational and perinatal complications. One has considered as gestational complications: development of preeclampsia, PPS and PTD with less than 37 weeks of pregnancy. The diagnoses of preeclampsia were performed for the patients who presented increase in the arterial pressure > 140/90 mmHg or elevation of 30 mmHg in the systolic pressure or 15 mmHg in the diastolic pressure after the 20th week of gestation, associated with edema and/or proteinuria (> 300 mg in 24 hours).
One has considered as perinatal complications: fetal centralization, presence of thick meconium in the amniotic fluid at the time of birth, and small infants for the gestational age (SGA). SGA neonates were those who, at the birth, presented a weight below the 10th percentile on the growth curve established for our population(18).
In the statistical analysis, the Mann-Whitney test was applied for non-parametric samples and the Fisher's exact test was applied for evaluation of qualitative parameters. All the tests utilized a 95% (p < 0.05) confidence interval.
RESULTS
The pregnant women recruited were longitudinally followed-up with Doppler assessment in four periods of the second half of pregnancy and were followed-up with the verification of obstetric and perinatal test results.
Table 1 shows the 12 cases of gestational and/or perinatal complications. No case of PPS was observed.
For evaluation of the Doppler parameters, RI, PI and A/B ratio were used, assessed both in the right and left uterine arteries. Additionally, the indexes average between the two vessels was calculated. The 25th, 50th, and 75th percentiles of Doppler indexes were calculated for each gestational age.
The 50th percentile of the Doppler indexes values in four gestational periods studied are graphically represented for uterine arteries (average) in the "non-complicated" patients (group 1) and patients with any complication (group 2), in Figures 3, 4 and 5.
The presence of bilateral notch in the uterine arteries between the 24th and 26th weeks was strongly associated with the onset of complications during pregnancy, differing from examinations performed in other periods. Nine patients presented diseases, representing 75% of the total of complications. All the cases of preeclampsia, one case of SAG neonate, three cases of PTD and one case of thick meconium at the time of delivery, presented alteration of the flow velocity waveform. The normality of the flow velocity waveform was not associated with the onset of gestational diseases. Of 21 patients who have not presented notch in the uterine arteries between the 24th and 26th weeks, only one case developed with complication in the perinatal period.
The effectiveness of the bilateral notch in the study performed between 24th26th weeks for definition of the gestation results is shown in Table 2.
Using the bilateral notch as a criterion of abnormality in the examination performed between 24th26th weeks, the sensitivity in the detection of preeclampsia or SAG was 100%, but the specificity was 62.5% and 60.6% respectively, resulting in a low PPV. The detection of any pregnancy complication also has presented a high sensitivity (90%), with a subtle elevation of PPV.
DISCUSSION
Campbell et al.(12) firstly studied the uteroplacental circulation by means of the Doppler method. The authors have evaluated both normal and complicated pregnant women during the second half of gestation and observed that, in the group of patients with diseases, the abnormal Doppler, with a higher frequency, was associated with IUGR and proteinuria/preeclampsia and fetal hypoxia. After this study, several other surveys carried out in the eighties and most recently have related alterations in the uterine arteries flow velocity waveform, principally the presence of bilateral notch, with the onset of gestational complications(13,19). Based on these promising results, a great number of studies have investigated the predictive value of the uterine artery Doppler as a screening test during gestation, before the onset of the disease(20).
In literature, there are few prospective studies testing the validity of the uterine artery Doppler for prediction of gestational complications. With this purpose and also to determine the behavior of impedance indexes in the uterine arteries during the second half of gestation, besides evaluating which the best period for performance of the examination is, we have longitudinally followed-up a group of previously normal pregnant women, till the resolution of their pregnancy.
The criterion adopted in studies on uteroplacental circulation for obtaining the flow velocity waveform have been distinct. There are reports on evaluation of the arcuate and radial arteries(21), in the uterine artery and/or arcuate artery on the placental and contralateral sides(22), besides the utilization of average values of right and left uterine arteries(23). The study of the subplacental arteries or the arcuate arteries in just one of the sides of the uterus is not representative of the whole uterine flow. The alterations in the placental arcuate arteries only appear in more advanced phases of the pathologic processes, and do not allow an early diagnosis(24). In our study, we have adopted the average value of the two uterine arteries, with the volume sample placed at 1 cm from the intersection of uterine arteries with the external iliac arteries, providing a more comprehensive evaluation of the uterine perfusion(25).
The indexes more commonly utilized in Doppler studies are the RI, the PI and de A/B ratio, which have been widely accepted in obstetrics as significant parameters for the blood flow analysis(26). Although these indexes present a high correlation coefficient(27), some researchers recommend the use of the PI as a better quantifier of signs in cases of absent and diastolic velocity and in cases of reverse diastolic flow. However, these standards are not usual during the pregnancy and the RI and A/B ratio calculations are easier to be made than the PI. In our study, we have used the three indexes for analysis of flow velocity waveforms with the purpose of verifying their behavior in the second half of the gestation and the correlations with complications onset.
Data obtained from the group of pregnant women who did not developed gestational complications showed a progressive decrease of the three Doppler indexes in the four examinations performed (Figures 3, 4 e 5). This decrease in the Doppler indexes with the progress of the gestation reflects an adequate trophoblastic invasion and the consequential multiplication of the villi system, resulting in a continuous reduction of the impedance to the blood flow in the uterine arteries(28). These findings were similar to those obtained by Thaler et al.(29) and Kurjak et al.(30), who have demonstrated the decrease in the impedance to the flow from the main uterine artery up to the spiral arteries as the gestational age progresses. Thaler et al.(29) also have demonstrated, by means of Doppler, the increase of blood volume in the uterine arteries with the pregnancy development, with this increase being more pronounced as from the 20th week.
In the patients who have developed any pregnancy complication, we have also observed a decrease in the Doppler indexes during gestation, but less pronounced than in patients who have not developed disorders. Kurdi et al.(25) and Montenegro et al.(16), making a similar evaluation, have observed that the RI was higher in the patients who have developed pregnancy complications, and the method is useful for prediction of such complications.
Comparing the three Doppler indexes of normal patients with those of patients who have developed any disease, we observe statistically significant differences in the study performed between the 24th26th weeks (Figures 3, 4 e 5). This fact leads us to conclude that increased Doppler indexes at this gestational age can predict complications occurring at the end of the pregnancy.
The profile of the uterine arteries flow velocity waveform, when the pulsed Doppler is used, is characteristic. A wave with a high systolic peak, a prominent protodiastolic notch and low end-diastolic flow is a normal profile of the uterine artery during the first half of gestation(31). The placenta, due its implantation and development, modifies the uterine circulation from low flow with high resistance to high flow with low resistance(32). These alterations make the uterine arteries protodiastolic notch disappear around the 24th26th weeks of pregnancy. The Doppler study of the uterine arteries is considered abnormal in the persistence of diastolic notch in the flow velocity waveforms and/or Doppler indexes with high value after the 20th week, both characterizing high resistance to the flow(13).
Both the sensitivity and specificity of the uterine arteries Doppler for the prediction of pregnancy complications have already been comprehensively tested. Arduini et al.(33), studying a high risk population, have obtained a 62.5% sensitivity for the prediction of pregnancy-specific hypertensive disease and IUGR, with a specificity of 71.1%. Similar results were reported by Bewley et al.(34) and Campbell et al.(35). Using the persistence of the bilateral notch or the high RI, Bower et al.(36) have obtained a sensitivity of 45%, with 96% of specificity. Kurdi et al.(25), using the presence of bilateral notch, have obtained a sensitivity of 61.9% for the preeclampsia diagnosis, with specificity of 88.7%, PPV of 11.1% and negative predictive value (NPV) of 99.0%. However, for the diagnosis of IUGR, they have found a sensitivity of 36.8%, specificity of 89.2%, PPV of 17.9% and NPV of 95.7%. When the same authors adopted the high resistance as an abnormality criterion for Doppler, they obtained a sensitivity of 71.4%, specificity of 78.2%, PPV of 6.9% and NPV of 99.2% for the preeclampsia diagnosis, whereas, for the IUGR diagnosis, they obtained sensitivity of 47.4%, specificity of 78.7%, PPV of 12.5% and NPV of 95.9%.
Montenegro et al.(16), also adopting the presence of bilateral notch or the high RI as a Doppler abnormality criterion, have demonstrated a good sensitivity, but low PPV. The bilateral notch predicting toxemia presented a sensitivity of 100.0%, specificity of 76.3%, PPV of 19.0% and NPV of 100,0%; the high RI showed sensitivity of 83.3%, specificity of 84.7%, PPV of 23.3% and NPV of 98.9%. A very recent study by Coleman et al.(23), for the prediction of pregnancy-specific hypertensive disease, has showed sensitivity of 91.0%, specificity of 42.0% and PPV of 37.0%, and, for the prediction of SGA neonates, a sensitivity of 84.0%, specificity of 39.0% and PPV of 33.0%.
Our study has obtained results similar to those of the literature with better sensitivity and specificity observed in the examinations performed between the 24th26th weeks of gestation. When we consider the onset of any pregnancy complication, the sensitivity of 90.0%, the specificity of 62.5%, the PPV 42.9% and the NPV was 95.2%. The presence of a high RI between the 24th and 26th weeks of gestation showed sensitivity and specificity similar to the previous ones, with a very discreet improvement in the PPV.
Our data demonstrate the relevance of the uterine arteries Doppler study even in low risk population and that the best period for its realization, evaluating both the presence of bilateral notch and high impedance indexes, is between the 24th and 26th weeks of pregnancy.
REFERENCES
Received April 3, 2005.
Accepted after revision July 1, 2005.
- 1. Gant NF, Hutchinson HT, Siiteri PK, MacDonald PC. Study of the metabolic clearance rate of dehydroisoandrosterone sulfate in pregnancy. Am J Obstet Gynecol 1971;111:555563.
- 2. Clavero JA, Negueruela J, Ortiz L, De Los Heros JA, Modrego SP. Blood flow in the intervillous space and fetal blood flow. I. Normal values in human pregnancies at term. Am J Obstet Gynecol 1973;116:340346.
- 3. Assali NS, Rauramo L, Peltonen T. Measurement of uterine blood flow and uterine metabolism. VIII. Uterine and fetal blood flow and oxygen consumption in early human pregnancy. Am J Obstet Gynecol 1960;79:8688.
- 4. Satomura S. Study of the flow patterns in peripheral arteries by ultrasonics. J Acoust Soc Jap 1959; 15:151158.
- 5. Fitzgerald DE, Drumm JE. Non-invasive measurement of human fetal circulation using ultrasound: a new method. Br Med J 1977;2:14501451.
- 6. Carrera JM, Perez-Arez C, Carrera M. Bases anatómicas de la circulación maternofetal. In: Carrera JM, Mortera C, Torrentis M, editores. Doppler en obstetricia hemodinámica perinatal. Barcelona: Salvat, 1992;316.
- 7. Pijnenborg R, Dixon G, Robertson WR, Brosens F. Trophoblastic invasion of human decidua from 8-18 weeks of pregnancy. Placenta 1980;1:319.
- 8. Kurjak A, Kupesic-Urek S, Predanic M, Salihagic A. Transvaginal color Doppler assessment of uteroplacental circulation in normal and abnormal early pregnancy. Early Hum Dev 1992;29:385389.
- 9. Valentin L, Sladkevicius P, Laurini R, Soderberg H, Marsal K. Uteroplacental and luteal circulation in normal first-trimester pregnancies: Doppler ultrasonographic and morphologic study. Am J Obstet Gynecol 1996;174:768775.
- 10. Meekins JW, Pijnenborg R, Hanssens M, McFayden IR, van Asshe A. A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. Br J Obstet Gynaecol 1994;101:669674.
- 11. Olofsson P, Laurini RN, Marsal K. A high uterine artery pulsatility index reflects a defective development of placental bed spiral arteries in pregnancies complicated by hypertension and fetal growth retardation. Eur J Obstet Gynecol Reprod Biol 1993;49: 161168.
- 12. Campbell S, Diaz-Recasens J, Griffin DR, et al. New Doppler technique for assessing uteroplacental blood flow. Lancet 1983;1:675677.
- 13. Fleisher A, Schulman H, Farmakides G, et al. Uterine artery Doppler velocimetry in pregnant women with hypertension. Am J Obstet Gynecol 1986;154: 806813.
- 14. Chan FY, Pun TC, Lam C, Khoo J, Lee CP, Lam YH. Pregnancy screening by uterine artery Doppler velocimetry which criterion performs best? Obstet Gynecol 1995;85:596602.
- 15. Boller A, Cabral ACV. Dopplerfluxometria das artérias uterinas na avaliação do prognóstico materno. J Bras Ginecol 1995;105:3134.
- 16. Montenegro CAB, Chaves E, Pessoa LG, Rezende J, Oliveira AS. Valor preditivo para a toxemia do Doppler das artérias uterinas. Progresos en Diagnostico Prenatal 1998;10:1619.
- 17. Silva CL. Mapa vascular da gestação do primeiro trimestre obtido pela dopplervelocimetria a cores transvaginal. (Tese de Mestrado). Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto Universidade de São Paulo, 1998.
- 18. Matheus M, Sala MA. Crescimento intra-uterino. Evolução da altura fetal, peso do feto, da placenta e do índice placentário, na segunda metade da gestação. AMB Rev Assoc Med Bras 1977;23:8890.
- 19. Murakoshi T, Sekizuka N, Takakuwa K, Yoshizawa H, Tanaka K. Uterine and spiral artery flow velocity waveforms in pregnancy-induced hypertension and/or intrauterine growth retardation. Ultrasound Obstet Gynecol 1996;7:122128.
- 20. Zimmermann P, Eirio V, Koskinen J, Kujansuu E, Ranta T. Doppler assessment of the uterine and uteroplacental circulation in the second trimester in pregnancies at high risk for pre-eclampsia and/or intrauterine growth retardation: comparison and correlation between different Doppler parameters. Ultrasound Obstet Gynecol 1997;9:330338.
- 21. Trudinger BJ, Giles WB, Cook CM. Uteroplacental blood flow velocity time waveforms in normal and complicated pregnancy. Br J Obstet Gynaecol 1985;92:3945.
- 22. Duggan P, McCowan L. Normal ranges for Doppler flow velocity waveforms from maternal uterine and fetal umbilical arteries. Aust N Z J Obstet Gynaecol 1993;33:139141.
- 23. Coleman MA, McCowan LM, North RA. Mid-trimester uterine artery Doppler screening as a predictor of adverse pregnancy outcome in high-risk women. Ultrasound Obstet Gynecol 2000;15:712.
- 24. Amim Junior J, Lima ML, Fonseca ALA, Chaves NH, Montenegro CAB. Dopplerfluxometria das artérias uterinas no diagnóstico da toxemia e do crescimento intra-uterino retardado. J Bras Ginecol 1988;98:399402.
- 25. Kurdi W, Campbell S, Aquilina J, England P, Harrington K. The role of color Doppler imaging of the uterine arteries at 20 weeks' gestation in stratifying antenatal care. Ultrasound Obstet Gynecol 1998;12:339345.
- 26. Grab D, Hutter W, Sterzik K, Terinde R. Reference values for resistance index and pulsatility index of uteroplacental Doppler flow velocity waveforms based on 612 uneventful pregnancies. Gynecol Obstet Invest 1992;34:8287.
- 27. Thompson RS, Trudinger BJ, Cook CM. A comparison of Doppler ultrasound waveform indices in the umbilical artery. I: Indices derived from the maximum velocity waveform. Ultrasound Med Biol 1986;12:835844.
- 28. Bruner JP, Gabbe SG, Levy DW, Arger PH. Doppler ultrasonography of the umbilical cord in normal pregnancy. South Med J 1993;86:5255.
- 29. Thaler I, Manor D, Itskovitz J, et al. Changes in uterine blood flow during human pregnancy. Am J Obstet Gynecol 1990;162:121125.
- 30. Kurjak A, Crvenkovic G, Salihagic A, Zalud I, Miljan M. The assessment of normal early pregnancy by transvaginal color Doppler ultrasonography. J Clin Ultrasound 1993;21:38.
- 31. Coppens M, Loquet P, Kollen M, De Neubourg F, Buytaert P. Longitudinal evaluation of uteroplacental and umbilical blood flow changes in normal early pregnancy. Ultrasound Obstet Gynecol 1996; 7:114121.
- 32. Harrington K, Cooper D, Lees C, Hecher K, Campbell S. Doppler ultrasound of the uterine arteries: the importance of bilateral notching in the prediction of pre-eclampsia, placental abruption or delivery of a small-for-gestational-age baby. Ultrasound Obstet Gynecol 1996;7:182188.
- 33. Arduini D, Rizzo G, Romanini C, Mancuso S. Utero-placental blood flow-velocity waveforms as predictors of pregnancy-induced hypertension. Eur J Obstet Gynecol Reprod Biol 1987;26:335341.
- 34. Bewley S, Cooper D, Campbell S. Doppler investigation of uteroplacental blood flow resistance in the second trimester: a screening study for pre-eclampsia and intrauterine growth retardation. Br J Obstet Gynaecol 1991;98:871879.
- 35. Campbell S, Pearce JM, Hackett G, Cohen-Overbeek T, Hernandez C. Qualitative assessment of uteroplacental blood flow: early screening test for high risk pregnancies. Obstet Gynecol 1986;68: 649653.
- 36. Bower S, Bewley S, Campbell S. Improved prediction of preeclampsia by two-stage screening of uterine arteries using the early diastolic notch and color Doppler imaging. Obstet Gynecol 1993;82:7883.
Publication Dates
-
Publication in this collection
25 May 2006 -
Date of issue
Apr 2006
History
-
Received
04 Mar 2005 -
Accepted
01 July 2005