Abstracts
BACKGROUND AND OBJECTIVES: The CEROF-HC is a public hospital specialized in ophthalmology. Anesthetic blocks for ophthalmic surgeries are common and effective. But the technique is not devoid of risks, and there is the possibility of meningeal perforation and injection of the local anesthetic (LA) in the central nervous system (CNS). The objective of this study was to report a case of brainstem anesthesia as a complication of the ophthalmologic regional anesthesia, stress the importance of preventing this accident, and discuss the treatment. CASE REPORT: A female patient, 60 years old, ASA II, with a diagnosis of grade II cataract, was scheduled for a facectomy and implantation of intraocular lens in the right eye. The patient had a past medical history of hypertension and vitrectomy. Physical exam, laboratory and cardiologic exams were normal. An extraconal retrobulbar block was performed with local anesthetic (lidocaine and bupivacaine) and hyaluronidase (total volume of 5 mL). Immediately after, the patient developed apnea and loss of consciousness. She was treated with tracheal intubation and mechanical ventilation, remaining stable. The surgery was performed as planned. Thirty minutes after the intubation, the patient began to move, recovering completely, without deficits. CONCLUSIONS: Although safe, ophthalmic block is not devoid of risks. The main risk factor is improper anesthetic technique. In the ophthalmic block, the local anesthetic (LA) can reach the CNS by inadvertently puncturing the ophthalmic artery or the meninges that surround the optic nerve, with dispersion to the subarachnoid space. Although rare, it can lead to a severe complication with respiratory arrest that can be fatal if it is not diagnosed promptly. Here we present the possibilities of such a complication, and discuss the nomenclature of anesthetic blocks used in ophthalmology. The importance of the knowledge of this and other complications by the surgical team is paramount, as well as the preparation and adequate monitoring to diagnose and treat immediately this complication to minimize the risks to the patient.
ANESTHETIC TECHNIQUES, Regional; COMPLICATIONS; SURGERY, Ophthalmic
JUSTIFICATIVA E OBJETIVOS: O CEROF-HC é uma instituição pública especializada em oftalmologia. A realização de bloqueios anestésicos para intervenções cirúrgicas oftálmicas é prática comum e eficiente. Como técnica não é isenta de riscos, há possibilidade de perfuração de meninges e a injeção de anestésico local (AL) na região do sistema nervoso central (SNC). O objetivo deste relato foi mostrar um caso de anestesia do tronco encefálico como complicação do bloqueio oftálmico e chamar a atenção para a profilaxia do acidente e o tratamento das complicações. RELATO DO CASO: Paciente do sexo feminino, 60 anos, ASA II, com diagnóstico de catarata grau II, indicada para facectomia com implante de lente intra-ocular no olho direito. Histórico clínico de hipertensão arterial e antecedente de vitrectomia. Exames físicos, laboratoriais e cardiológicos normais. Foi realizado bloqueio retrobulbar extraconal, com anestésico local (lidocaína e bupivacaína) e hialuronidase (volume total de 5 mL). Imediatamente após, a paciente apresentou apnéia e perda da consciência. Foi tratada com intubação traqueal (IOT) e ventilação mecânica, mantendo-se estável. Foi realizada a operação. Começou a se movimentar 30 minutos após IOT, recuperando-se totalmente, sem apresentar qualquer seqüela. CONCLUSÕES: O bloqueio oftálmico, apesar de seguro, não é isento de riscos. O principal fator de risco é a inadequada realização da técnica anestésica. O anestésico local (AL), no bloqueio oftálmico, pode atingir o SNC por punção inadvertida da artéria oftálmica ou por punção das meninges que envolvem o nervo óptico, com a dispersão para o espaço subaracnóideo. Embora rara, pode levar a complicação grave, com parada respiratória, que, se não diagnosticada e tratada prontamente, pode ser fatal. São apresentadas as possibilidades de ocorrência dessa complicação, assim como a discussão da nomenclatura dos bloqueios anestésicos realizados em oftalmologia. Ressalta-se a importância do conhecimento desta e de outras complicações pela equipe cirúrgica, com necessidade de preparo e de monitorização adequada para que se diagnostique a possível complicação e se instale prontamente o tratamento, objetivando riscos mínimos para o paciente.
CIRURGIA, Oftálmica; COMPLICAÇÕES; TÉCNICAS ANESTÉSICAS, Regional
JUSTIFICATIVA Y OBJETIVOS: El CEROF-HC es una institución pública especializada en oftalmología. La realización de bloqueos anestésicos para intervenciones quirúrgicas oftálmicas es una práctica común y eficiente. Como técnica no está exenta de riesgos, existe la posibilidad de perforación de meninges y la inyección de anestésico local (AL) en la región del sistema nervioso central (SNC). El objetivo de este relato fue mostrar un caso de anestesia del tronco encefálico como complicación del bloqueo oftálmico y destacar la profilaxis del accidente y el tratamiento de las complicaciones. RELATO DE CASO: Paciente del sexo femenino, 60 años, ASA II, con diagnóstico de catarata grado II, indicada para facectomía con implante de lente intraocular en el ojo derecho. Hoja clínica de hipertensión arterial y antecedente de vitrectomía. Exámenes físicos, laboratoriales y cardiológicos normales. Fue realizado bloqueo retrobulbar extraconal con anestésico local (lidocaína y bupivacaína) e hialuronidasis (volumen total de 5 mL). Inmediatamente después, la paciente presentó apnea y pérdida de la conciencia. Fue tratada con intubación traqueal (IOT) y ventilación mecánica, manteniéndose estable. Se realizó la operación. Empezó a moverse 30 minutos después del IOT, recuperándose totalmente sin presentar ninguna secuela. CONCLUSIONES: El bloqueo oftálmico, a pesar de seguro, no está exento de riesgos. El principal factor de riesgo es la inadecuada realización de la técnica anestésica. El anestésico local (AL), en el bloqueo oftálmico, puede alcanzar el SNC por punción inadvertida de la arteria oftálmica o por punción de las meninges que envuelven el nervio óptico, con la dispersión para el espacio subaracnoideo. Aunque sea rara, puede conllevar a complicación grave, con parada respiratoria, que, si no se diagnostica y se trata rápidamente, puede ser fatal. Se presentan las posibilidades de esta complicación, y la discusión de la nomenclatura de los bloqueos anestésicos realizados en oftalmología. Se destaca la importancia del conocimiento de esta y de otras complicaciones por el equipo quirúrgico, con necesidad de preparación y monitorización adecuada para que se diagnostique la posible complicación y se instale rápidamente el tratamiento, objetivando los riesgos mínimos para el paciente.
CLINICAL REPORT
Brainstem anesthesia after extraconal retrobulbar block. Can it be avoided? Case report* * Received from CET do Hospital das Clínicas da Universidade Federal de Goiás (HC-UFG) e Centro de Referência em Oftalmologia da UFG CEROF/HC. Goiânia, GO
Anestesia del tronco encefálico depués de bloqueo retrobular extracional. ?Se puede evitar? Relato de caso
Haroldo Maciel CarneiroI; Bruno OliveiraII; Marcos P. ÁvilaIII; Onofre Alves Neto, TSAIV
ICoordenador do Serviço de Anestesiologia do CEROF-HC; Membro do CET/SBA do Hospital das Clínicas da UFG; Mestrando em Ciências da Saúde pela UFG
IIME3 do CET-SBA do Hospital das Clínicas da UFG
IIIProfessor Titular de Oftalmologia da UFG; Chefe do CEROF-HC
IVProfessor Adjunto de Anestesia da UFG; Responsável pelo CET/SBA do Hospital das Clínicas da UFG
Correspondence to Correspondence to: Dr. Haroldo Maciel Carneiro Rua T-37, 3280/300 Ed. Mares do Sul Setor Bueno 74230-020 Goiânia, GO E-mail: haroldo62@hotmail.com
SUMMARY
BACKGROUND AND OBJECTIVES: The CEROF-HC is a public hospital specialized in ophthalmology. Anesthetic blocks for ophthalmic surgeries are common and effective. But the technique is not devoid of risks, and there is the possibility of meningeal perforation and injection of the local anesthetic (LA) in the central nervous system (CNS). The objective of this study was to report a case of brainstem anesthesia as a complication of the ophthalmologic regional anesthesia, stress the importance of preventing this accident, and discuss the treatment.
CASE REPORT: A female patient, 60 years old, ASA II, with a diagnosis of grade II cataract, was scheduled for a facectomy and implantation of intraocular lens in the right eye. The patient had a past medical history of hypertension and vitrectomy. Physical exam, laboratory and cardiologic exams were normal. An extraconal retrobulbar block was performed with local anesthetic (lidocaine and bupivacaine) and hyaluronidase (total volume of 5 mL). Immediately after, the patient developed apnea and loss of consciousness. She was treated with tracheal intubation and mechanical ventilation, remaining stable. The surgery was performed as planned. Thirty minutes after the intubation, the patient began to move, recovering completely, without deficits.
CONCLUSIONS: Although safe, ophthalmic block is not devoid of risks. The main risk factor is improper anesthetic technique. In the ophthalmic block, the local anesthetic (LA) can reach the CNS by inadvertently puncturing the ophthalmic artery or the meninges that surround the optic nerve, with dispersion to the subarachnoid space. Although rare, it can lead to a severe complication with respiratory arrest that can be fatal if it is not diagnosed promptly. Here we present the possibilities of such a complication, and discuss the nomenclature of anesthetic blocks used in ophthalmology. The importance of the knowledge of this and other complications by the surgical team is paramount, as well as the preparation and adequate monitoring to diagnose and treat immediately this complication to minimize the risks to the patient.
Key Words: ANESTHETIC TECHNIQUES, Regional: peribulbar, retrobulbar extraconal; COMPLICATIONS: respiratory arrest; SURGERY, Ophthalmic: cataract
RESUMEN
JUSTIFICATIVA Y OBJETIVOS: El CEROF-HC es una institución pública especializada en oftalmología. La realización de bloqueos anestésicos para intervenciones quirúrgicas oftálmicas es una práctica común y eficiente. Como técnica no está exenta de riesgos, existe la posibilidad de perforación de meninges y la inyección de anestésico local (AL) en la región del sistema nervioso central (SNC). El objetivo de este relato fue mostrar un caso de anestesia del tronco encefálico como complicación del bloqueo oftálmico y destacar la profilaxis del accidente y el tratamiento de las complicaciones.
RELATO DE CASO: Paciente del sexo femenino, 60 años, ASA II, con diagnóstico de catarata grado II, indicada para facectomía con implante de lente intraocular en el ojo derecho. Hoja clínica de hipertensión arterial y antecedente de vitrectomía. Exámenes físicos, laboratoriales y cardiológicos normales. Fue realizado bloqueo retrobulbar extraconal con anestésico local (lidocaína y bupivacaína) e hialuronidasis (volumen total de 5 mL). Inmediatamente después, la paciente presentó apnea y pérdida de la conciencia. Fue tratada con intubación traqueal (IOT) y ventilación mecánica, manteniéndose estable. Se realizó la operación. Empezó a moverse 30 minutos después del IOT, recuperándose totalmente sin presentar ninguna secuela.
CONCLUSIONES: El bloqueo oftálmico, a pesar de seguro, no está exento de riesgos. El principal factor de riesgo es la inadecuada realización de la técnica anestésica. El anestésico local (AL), en el bloqueo oftálmico, puede alcanzar el SNC por punción inadvertida de la arteria oftálmica o por punción de las meninges que envuelven el nervio óptico, con la dispersión para el espacio subaracnoideo. Aunque sea rara, puede conllevar a complicación grave, con parada respiratoria, que, si no se diagnostica y se trata rápidamente, puede ser fatal. Se presentan las posibilidades de esta complicación, y la discusión de la nomenclatura de los bloqueos anestésicos realizados en oftalmología. Se destaca la importancia del conocimiento de esta y de otras complicaciones por el equipo quirúrgico, con necesidad de preparación y monitorización adecuada para que se diagnostique la posible complicación y se instale rápidamente el tratamiento, objetivando los riesgos mínimos para el paciente.
INTRODUCTION
The Centro de Referência em Oftalmologia of Universidade Federal de Goiás (CEROF-UFG) is a public institution affiliated with the Hospital das Clínicas da UFG, which treats exclusively patients with ophthalmic disease of the Sistema Único de Saúde (SUS)** ** N. T.: SUS - public health system in Brazil. . The Center also teaches ophthalmology-related subjects for graduate and post-graduate courses. Anesthesiology residents have their ophthalmic anesthesia training here, where more than 4,000 ophthalmic surgeries are performed each year. The main anesthetic block is the extraconal retrobulbar block (ERB).
The orbit is a quadrangular pyramid-shaped cavity, with its apex facing posteriorly and the base is its anterior opening. It is filled with adipose tissue that protects the eye, which is located in its anterior portion. There are four rectus muscles of the eye: inferior, superior, lateral, and medial, which insert in the apex of the orbit through a common tendon, called tendon of Zinn. They run anteriorly and fuse with the Tenon's capsule at the level of the equatorial axis of the eyeball (Figure 1). These muscles form a muscular cone, dividing the retrobulbar compartment in intraconal (inside the cone) and extraconal (outside the cone). Most of the sensitive and motor innervation of the eye, as well as its main arteries, is inside this muscular cone. The optic nerve is in the center of this cone, being surrounded by the three meningeal membranes, characterizing an extracranial extension of the subarachnoid space.
The retrobulbar block (RB) is characterized by the injection of small volumes of a local anesthetic (LA) in the intraconal retrobulbar space (3 to 5 mL). This technique, which was widely used in ophthalmic surgeries in the past, is important due to the inherent risks of the presence of a needle close to the optic nerve and ophthalmic artery 1. Lesion of the optic nerve, perforation of the eye, retrobulbar hemorrhage, and injection of the LA in the sheath of the optic nerve have been described 2-7. Although rare, these complications can risk both the vision and life of the patient.
The peribulbar block (PB), described by Davis and Mendel 3 in 1986, was developed as a safer option of ophthalmic block, without decreasing the quality of the anesthesia. It is done by inserting the needle in the extraconal retrobulbar space. For this reason, the volume of the anesthetic administered should be greater than in the RB, so it can diffuse within the muscular cone, providing adequate anesthesia and akinesia of the eye. The peribulbar block, either in its initial technique, described as a double, inferolateral and superomedial, puncture, or one of its variations, has gained the preference of the majority of the anesthesiologists and ophthalmologists, especially by the theoretical advantage in terms of safety.
With the evolution of ophthalmic surgical techniques, the superior puncture was gradually abandoned, due to the risks of multiple punctures 1, to become virtually a complement of the inferior punctures, when they do not provide enough akinesia and/or anesthesia of the eye. With the improved knowledge of the anatomy of the orbit, the use of smaller needles, with no more than 30 mm in length, was suggested for a safer PB, decreasing the possibility of reaching intraorbital structures 4. Peribulbar anesthesia is known by several names, such as posterior peribulbar block, periconal block, and extraconal retrobulbar block. This occurs because the technique is performed blindly and one cannot be sure of the exact position of the tip of the needle. In this report, we refer to it as extraconal retrobulbar block (ERB), because we consider that the needle always goes beyond the equatorial axis of the eye, being placed behind it. Ripart et al. 5 questioned the presence of a membranous intermuscular septum separating anatomically the intra- and extraconal spaces, suggesting that the retrobulbar space has only one chamber.
Despite its apparent safety, it has not been confirmed that ERB has lower risks and complications than RB 6. Perforation of the eyeball, retrobulbar hemorrhage, and injection of the LA in the sheath of the optic nerve when performing the ERB with needles longer than 30 mm have been reported 7,8.
For this reason, shorter needles where introduced. The 25-mm long needles are currently preferred for ERB by the majority of professionals. Longer needles have a higher risk of complications, while shorter needles need complementation of the blockade more often 9.
This case describes a brainstem anesthesia of the CNS by a presumed injection of the LA in the sheath of the optic nerve, during the course of a modified ERB with one inferolateral puncture 10 with a 25 ´ 7 mm needle, stressing the importance of its diagnosis and immediate treatment. This is the first report in the literature of this type of complication using needles less than 30-mm long.
CASE REPORT
A female patient, 60 years old, physical status ASA II, with hypertension treated with captopril, 25 mg/day, and no other comorbidities, with a past surgical history of vitrectomy in the right eye (RE) one year before this surgery, without anesthetic complications.
After the diagnosis of grade II cataract was made, a facectomy by phaco-emulsification and implantation of intraocular lens in the RE was indicated. The axial length of her eye, measured by echobiometry, was 22.71 mm.
The anesthetic procedure began with a peripheral venipuncture with a 20G catheter and administration of D5W. Oxygen, at a rate of 2 L.min-1, was administered by nasal catheter. Monitoring consisted of continuous cardioscopy at the DII derivation, pulse oxymetry (SpO2), and non-invasive blood pressure (BP). The initial BP was 140 ´ 80 mmHg and the heart rate (HR), 70 bmp.
After sedation with 5 mg of diazepam and 25 µg of fentanyl, the area was prepared with 70% alcohol followed by one orbital puncture, modified inferolateral, with a 25 ´ 7 mm needle, perpendicular to the skin for the first 10 mm and, after supramedial angulation, the remaining of the needle was introduced (Figure 2). An anesthetic solution containing 1 mL of lidocaine, 4 mL of 0.75% bupivacaine and 20 U.mL-1 of hyaluronidase, was injected.
Immediately after the injection of the anesthetic solution, the patient developed apnea and lost consciousness, without response to verbal stimuli. Manual ventilation with a face mask and 100% oxygen was instituted. Pulse oxymetry was maintained between 94% and 99%, BP was 200 ´ 120 mmHg, and HR of 150; at this moment, bilateral photoplegic mydriasis was present. Sublingual captopril, 25 mg, was administered.
After 5 minutes of manual ventilation, the patient was intubated under direct laryngoscopy, demonstrating complete arreflexia. Mechanical ventilation was instituted with 100% oxygen. After 20 minutes, her BP was 130 ´ 80 mmHg, HR of 90 bpm, and SpO2 99%. Since the patient improved, the proposed surgical procedure was performed. Thirty minutes after tracheal intubation, the patient was began to move her head and legs. A bolus of intravenous propofol (70 mg) was administered and isoflurane was added, through a universal vaporizer, to the oxygen, to maintain the anesthetic plane.
The surgery lasted 30 minutes, without any other intercurrence. The patient was extubated 30 minutes after the surgery and was awake, without motor deficit, and with total amnesia for what happened after the blockade.
The patient was transferred to the recovery room, where she remained for two hours, lucid and hemodynamically stable. It was explained to the patient and her companion what had happened and they received the proper orientation.
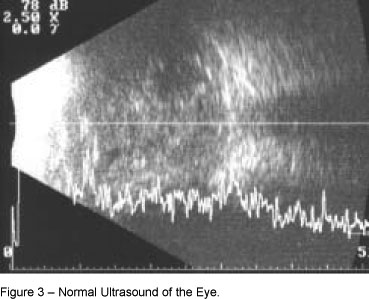
The patient was evaluated the following day and did not present any neurological deficit. A complete ophthalmic exam (biomicroscopy, tonometry, and indirect ophthalmoscopy) was normal for the first postoperative day, indicating the proper positioning of the lens in the posterior chamber. The neuro-ophthalmological exam revealed normal pupillary contraction. The ultrasound of the eye did not show any changes (Figure 3). A CT scan of the orbit, in the axial and coronal views, with and without contrast, did not show any anatomic change in the orbit, eyeball, or structures within the orbit, which could characterize the patient as being at a greater risk than the normal population to develop complications during an ophthalmic block (Figures 4 and 5). The patient was then discharged from the hospital.
DISCUSSION
Although anatomic variations might increase the risk of complications during ophthalmic blocks, the main reason is improper technique 12. The experience of the professional performing the ERB and rigid observation of measures that decrease the risk of complications are paramount for the success of this technique (Chart I).
During an ophthalmic blockade, the LA might reach the CNS by two ways: by the accidental puncture of the ophthalmic artery or by the accidental puncture of the meninges that surround the optic nerve (Figure 6), with consequent dispersion of the LA to the subarachnoid space 13. In this case, depending on the volume and concentration of the LA, one might develop bilateral mydriasis, mental confusion, and sympathetic hyperactivity, and may evolve to brainstem block (Figure 7) with respiratory arrest; or, rarely, the anesthetic might reach a variable extension of the spinal cord, adding hypotension, bradycardia, and quadriplegia to the symptoms described above.
The incidence of respiratory arrest in ophthalmic blocks is rare. It has been reported that in the retrobulbar block, when the needle is introduced more than 40 mm, in 11% of the cases it is possible to reach the optic foramen 4. Another author described 16 cases of respiratory arrest in 6,000 retrobulbar blocks 13. A case of respiratory arrest after peribulbar block using a 30-mm long needle has been reported; the authors recommended the use of needles no longer than 30 mm to reduce the risks 9.
The treatment of complications should begin immediately after their diagnosis, depending on the condition of the patient, varying from the administration of 100% oxygen and maintenance of vital signs to tracheal intubation and controlled ventilation. The evolution is usually benign, with complete remission of the symptoms in a few hours. There is no consensus whether the surgery should be cancelled in this case and regarding the ideal duration of hospitalization.
In this case, the clinical presentation was compatible with dispersion of the LA to the subarachnoid space, with brainstem anesthesia, loss of consciousness, and respiratory arrest. The absence of hypotension, bradycardia, and the presence of movements of head and legs 35 minutes after the administration of the local anesthetic, suggest that spinal cord block was not present.
The initial intention was to realize an extraconal block. However, in view of the complication, we presumed there was accidental penetration of the intraconal space. This is the only way that the meningeal layer that surrounds the optic nerve, whose trajectory is in the central area of the cone formed by the intrinsic muscles of the eye, could have been damaged (Figure 4). Using a 25-mm long needle in the extraconal retrobulbar block, it is unlikely the apex of the orbit will be reached, because the distance between the apex and the lower orbital border, the site of needle introduction, is greater than 42 mm 4.
It has been frequently questioned whether one can be 100% sure that the blockade is really intra- or extraconal with the blind techniques currently used 16, or if there really is a membrane between the muscles and the eye, dividing these spaces anatomically 5-12. The statement that it would be safer to use a 25-mm long needle for the extraconal retrobulbar block 9 should be questioned. New options should be evaluated in order to perform a safer blockade.
The anesthesiologist should be aware of the possible complications of this procedure, including the possibility of reaching the optic nerve, even using a 25-mm long needle. Due to the potential risks, we emphasize the need to monitor patients undergoing anesthesia in ophthalmic surgeries closely, as well as the presence of an experienced professional, who is not only capable of recognizing immediately the complication, but also able to act promptly to avoid that this complication will endanger the life of the patient.
Even though this is a rare complication, and using only 25-mm long needles, the risk can be anticipated and, although it is impossible to avoid it, everyone should be prepared to treat its consequences.
In view of what has been exposed here, and contradicting the orientations of the Royal College of Anaesthetists and the Royal College of Ophthalmologists 17, we suggest that, regardless of who will perform the blockade and, even in the absence of sedation, the presence of an anesthesiologist during this type of procedure is necessary to ensure the safety of the patient.
REFERENCES
Submitted em 20 de julho de 2006
Accepted para publicação em 18 de abril de 2007
- 01. Gillart T, Dualé C, Curt I Ophthalmic regional anasthesia. Curr Opin Anaesthesiol, 2002;15:503-509.
- 02. Hamilton RC A discourse on the complications of retrobulbar and peribulbar blocked. Am J Ophtalmol, 2000,35:363-372.
- 03. Davis DB 2nd, Mandel MR Posterior peribulbar anesthesia: an alternative to retrobulbar anesthesia. J Cataract Refract Surg, 1986,12:182-184.
- 04. Katsev DA, Drews RC, Rose BT An anatomic study of retrobulbar needle path length. Ophthalmology, 1989,96:1221-1224.
- 05. Ripart J, Lefrant JY, de la Coussaye JE et al. Peribulbar versus retrobulbar anesthesia for ophthalmic surgery: an anatomical comparison of extraconal and intraconal injections. Anesthesiology, 2001;94:56-62.
- 06. Freitas ACH, Espirandelli LC Parada respiratória após bloqueio peribulbar. Relato de caso. Rev Bras Anestesiol, 1997; 47:134-137.
- 07. Gunja N, Varshney K Brainstem anaesthesia after retrobulbar block: a rare cause of coma presenting to the emergency department. Emerg Med Australas, 2006;18:83-85.
- 08. Davis 2nd DB, Mandel MR Efficacy and complication rate of 16.244 consecutive peribulbar blocks. A prospective multicenter study. J Cataract Refract Surg, 1994;20:327-337.
- 09. nan den Berg AA An audit of peribulbar blockade using 15 mm, 25 mm and 37,5 mm needles, and sub-Tenons injection. Anaesthesia, 2004;59:775-780.
- 10. Habib NE, Balmer HG, Hocking G Efficacy and safety of sedation with propofol in peribulbar anaesthesia. Eye, 2002; 16:60-62.
- 11. Kallio H, Rosenberg PH Advances in ophthalmic regional anaesthesia. Best Pract Res Clin Anaesthesiol, 2005;19:215-227.
- 12. Ripart J, Nouvellon E, Chaumeron A Regional anesthesia for eye surgery. Reg Anesth Pain Med, 2005;30:72-82.
- 13. Nicoll JM, Acharya PA, Ahlen K et al. Central nervous system complications after 6.000 retrobulbar block. Anesth Analg, 1987; 66:1298-1302.
- 14. Unsöld R, Stanley JA, DeGroot J The CT-topography of retrobulbar anesthesia: anatomic-clinical correlation of complications and suggestion of a modified technique. Albrecht Von Graefes Arch Klin Exp Ophthalmol, 1981;217:125-136.
- 15. Pautler SE, Grizzard WS, Thompson LN et al. Blindness from retrobulbar injection into the optic nerve. Ophthalmic Surg, 1986;17:334-337.
- 16. Venkastesan VG, Smith A What´s new in ophthalmic anaesthesia? Curr Opin Anaesthesiol, 2002;15:615-620.
-
17Royal College of Anaesthetists and Royal College of Ophtalmologists – Local Anaesthesia for Intraocular Surgery An authoritatitive guideline on the preoperative management of these patients. London, 2001.
Publication Dates
-
Publication in this collection
31 July 2007 -
Date of issue
Aug 2007
History
-
Received
20 July 2006 -
Accepted
18 Apr 2007