ABSTRACT
BACKGROUND AND OBJECTIVE:
Sedation in dialysis dependent end-stage renal disease patients requires caution as a result of performing high doses of sedatives and its complications. Multidrug sedation regimens might be superior and advantage on lesser drug consumption and by the way adverse events which occur easily in end-stage renal disease patients. We evaluated the effects of dexmedetomidine premedication on propofol consumption, sedation levels with Observer's Assessment of Alertness and Sedation scores and the bispectral index and the hemodynamic changes, potential side effects in geriatric patients with end-stage renal disease who underwent hip fracture surgery under spinal anesthesia.
METHOD:
In this randomized, controlled, double-blind study 60 elderly patients (age ≥ 65 years) with end-stage renal disease and hip fracture scheduled for anterograde femoral intramedullary nailing were assigned to groups that received either intravenous saline infusion (Group C) or dexmedetomidine 0.5 g/kg/10 min infusion for premedication (Group D). All the patients received propofol infusion after the induction of the spinal anesthesia.
RESULTS:
Total propofol consumption, propofol dose required for targeted sedation levels according to Observer's Assessment of Alertness and Sedation scores and bispectral index levels, recovery times were significantly lower in Group D (p < 0.001). The time to reach to Observer's Assessment of Alertness and Sedation score 4 and to achieve bispectral index ≤ 80 was significantly lower in Group C compared with Group D (p < 0.001). Adverse events were similar in both groups.
CONCLUSION:
Dexmedetomidine premedication lowers intraoperative propofol consumption to maintain targeted level of sedation. Therefore low dose dexmedetomidine premedication in addition to propofol infusion might be an alternative in geriatric patients with end-stage renal disease for sedation
Keywords:
Geriatric patient; End stage renal disease; Dexmedetomidine; Propofol
RESUMO
JUSTIFICATIVA E OBJETIVO:
A sedação em paciente dependente de diálise com doença renal em estágio terminal (DRET) requer cautela como resultado da administração de altas doses de sedativos e suas complicações. Os regimes de sedação com múltiplas drogas podem ser superiores e vantajosos em relação ao consumo menor de drogas e aos eventos adversos que ocorrem facilmente em pacientes com DEET. Avaliamos os efeitos da pré-medicação com dexmedetomidina sobre o consumo de propofol, os níveis de sedação com os escores da Observer's Assessment of Alertness and Sedation (OAA/S) e do índice bispectral (BIS), as alterações hemodinâmicas e os potenciais efeitos colaterais em pacientes geriátricos com DRET submetidos à cirurgia para fratura de quadril sob raquianestesia.
MÉTODO:
Neste estudo randômico, controlado e duplo-cego, 60 pacientes idosos (idade ≥ 65 anos), com DRET e fratura de quadril, agendados para fixação intramedular de haste femoral anterógrada foram designados para grupos para receberam infusão intravenosa de solução salina (Grupo C) ou pré-medicação com infusão de 0,5 mg kg/10 min de dexmedetomidina (DEX) (Grupo D). Todos os pacientes receberam infusão de propofol após a indução da raquianestesia.
RESULTADOS:
O consumo total de propofol, a dose de propofol necessária para os níveis-alvo de sedação de acordo com os escores da OAA/S, os valores do BIS e os tempos de recuperação foram significativamente menores no Grupo D (p < 0,001). O tempo para atingir o escore 4 na OAA/S e valores BIS ≤ 80 foi significativamente inferior no Grupo C em comparação com o Grupo D (p < 0,001). Os eventos adversos foram semelhantes em ambos os grupos.
CONCLUSÃO:
A pré-medicação com dexmedetomidina reduz o consumo de propofol no intraoperatório para manter o nível-alvo de sedação. Portanto, a pré-medicação com DEX em dose baixa em combinação com infusão de propofol pode ser uma opção para sedação em pacientes geriátricos com DRET.
Palavras-chave:
Paciente geriátrico; Doença renal em estágio terminal; Dexmedetomidina; Propofol
Introduction
The incidence of end stage renal disease and dialysis population in the elderly continues to increase universally.11. Ismail N, Hakim RM, Oreopoulos DG, et al. Renal replacement therapies in the elderly: Part 1. Hemodialysis and chronic peri- toneal dialysis. Am J Kidney Dis. 1993;22:759-82. 22. Keith DS. Transplantation in the elderly patient. Clin Geriatr Med. 2013;29:707-19. and 33. Sasaki Y, Marioni R, Kasai M, et al. Chronic kidney disease: a risk factor for dementia onset: a population-based study The Osaki- Tajiri Project. J Am Geriatr Soc. 2011;59:1175-81. Hip fractures are also major problem and the anesthesia technique should be planned in detail due to potential alterations in volume distribution, protein binding, and drug metabolism and excretion.44. Le- Wendling L, Bihorac A, Baslanti TO, et al. Regional anesthe- sia as compared with general anesthesia for surgery in geriatric patients with hip fracture: does it decrease morbidity, mortal- ity, and health care costs? Results of a single-centered study. Pain Med. 2012;13:948-56. 55. Jørgensen TSH, Hansen AH, Sahlberg M, et al. Falls and comorbidity: the pathway to fractures. Scand J Public Health. 2014;42:287-94. and 66. Trainor D, Borthwick E, Ferguson A. Perioperative management of the hemodialysis patient. Semin Dial. 2011;24:314-26. In an ideal anesthesia regime, the most important parameters are providing hemodynamic stability with optimal fluid and electrolyte balance, using drugs with a lower metabolism, shorter half-life and non-renal clearance, targeting early recovery and return of cognitive and psychomotor functions.77. Byrick RJ. Anesthesia and end stage renal failure: is TIVA an advance? Can J Anaesth. 1999;46:621-2.
Neuraxial techniques such as single spinal injection is frequently performed for the intraoperative anesthesia management of patients with chronic renal failure.88. Hadimioglu N, Ulugol H, Akbas H, et al. Combination of epidural anesthesia and general anesthesia attenuates stress response to renal transplantation surgery. Transplant Proc. 2012;44:2949-54. Coadministration of spinal anesthesia and sedation became a standard protocol for providing patients' anxiolysis and amnesia at the intraoperative period.99. Brown DL. Spinal, epidural, and caudal anesthesia. In: Miller RD, editor. Miller's anesthesia. Elsevier Health Sciences; 2010. p. 1612-27. Propofol is the frequently used agent and combination regimens such as propofol vs alfentanil or midazolam vs fentanyl for sedation are commonly used in patients with chronic renal failure.1010. Eddleston JM, Pollard BJ, Blades JF, et al. The use of propofol for sedation of critically ill patients undergoing haemodiafiltration. Intensive Care Med. 1995;21:342-7. and 1111. Lee SM, Kim GH, Lee JJ, et al. Does propofol and alfentanil- induced sedation cause periodic apnoea in chronic renal failure patients? Int J Clin Pract. 2010;64:1-5. The sedoanalgesia drug doses should be titrated and to reduce dose consumption combination regimens should be performed in hemodialysis patients.1212. Beathard GA, Urbanes A, Litchfield T, et al. The risk of sedation/analgesia in hemodialysis patients undergoing inter- ventional procedures.. Semin Dial 2011;24:97-103.
Dexmedetomidine (DEX) is a selective a2 receptor agonist agent, might be an alternative of choice for combination regimen with propofol due to its sedative and analgesic properties with minimal effects on ventilation.1313. Ok HG, Baek SH, Baik SW, et al. Optimal dose of dexmedetomi- dine for sedation during spinal anesthesia. Korean J Anesthesiol. 2013;64:426-31. There are limited number of studies investigating the effect of DEX in patients with end stage renal disease (ESRD), however these studies are not specific to geriatric patients at the same time.1414. Rutkowska K, Knapik P, Misiolek H. The effect of dexmedeto- midine sedation on brachial plexus block in patients with end-stage renal disease. Eur J Anaesthesiol. 2009;26:851-5. and 1515. De Wolf AM, Fragen RJ, Avram MJ, et al. The pharmacokinetics of dexmedetomidine in volunteers with severe renal impair- ment. Anesth Analg. 2001;93:1205-9.
In this study we evaluate the effects of dexmedetomidine premedication on propofol consumption, sedation levels, hemodynamic changes, potential side effects in geriatric patients with ESRD who underwent hip fracture surgery under spinal anesthesia.
Materials and methods
This study was approved by the Baskent University Institutional Review Board and Ethics Committee (Project no: KA12/166). After obtaining written informed consent from the patients, 60 elderly patients (age ≥ 65 years) with end stage renal failure on dialysis treatment (glomerular filtration rate < 15, Stage 5) and hip fracture scheduled for anterograde femoral intramedullary nailing were included in this double-blind, randomized, controlled study. Exclusion criteria were decompensated respiratory or heart failure, liver failure, obesity (body mass index > 30), mental disorders, cognitive disorders, language problems, patients with a contraindication for regional anesthesia (coagulopathy, history of anticoagulant use, spinal cord disease and patients who rejected spinal anesthesia) and history of allergy to any medications used in this study.
The randomization scheme was developed by a computer and covered in sealed envelopes. These envelopes were prepared by an independent anesthesiologist who was not associated with the study. The envelopes were opened by the anesthesia technician, who also prepared the study drugs.
Patients were randomly divided into two groups:
Group control (Group C): Saline infusion for premedication, midazolam 0.02 mg/kg; spinal block (hyperbaric bupivacaine 0.5%, 12.5 mg, n = 30).
Group DEX (Group D): 0.5 µg/kg/10 min dexmedetomidine infusion for premedication, midazolam 0.02 mg/kg; spinal block (hyperbaric bupivacaine 0.5%, 12.5 mg,n = 30).
The study drugs were brought to the operation theater by the anesthesia technician. The anesthesiologist who performed premedications, spinal anesthesia, intraoperative postoperative follow-ups and data recordings was also blinded to the study drugs and group allocation.
A peripheral intravenous line was placed using an 18-20 gauge catheter in patients. Patients arrived in the operation theater without premedication. Routine anesthesia monitoring was performed with pulse-oxymeter, 5-lead ECG, noninvasive blood pressure measurement, pulse oxymetry and BIS. BIS scores were measured using an Aspect BIS Vista Monitor (Aspect Medical Systems, Inc). Electroencefalogram (EEG) was recorded using BIS QUATRO(tm) sensor stuck to the prepared forehead skin as explained in the instructions. All the patients received 0.02 mg/kg midazolam. 0.5 µg/kg DEX in 20 mL was administered in 10 min with an infusion pump. An equivalent volume of saline solution was given to the control group by using the same method. Baseline, 1-, 5-, 10-minute OAA/S scores, BIS, peripheral oxygen saturation (SpO2), heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP) values were recorded. At this period 250 mL of 0.9% NaCl was infused. Basal SBP, DBP, HR, SpO2, BIS values were recorded before induction of the spinal block. Lumbar puncture was performed in lateral decubitis position with a Quincke(r) 27 gauge spinal needle at the L3-L4 interspaces using the midline approach. Patients were promptly rotated to supine position after block induction. Induction of the spinal block was accepted as time of 0 for all intraoperative data recordings. All parameters were recorded at 1-, 5- min and every 5 min for the first hour and following the first hour every 15 min during surgery.
Hypotension was described as ≥25% decrease in SBP from the baseline or in cases when systolic blood pressure decreases below 90 mmHg. Ephedrine 5 mg was administered intravenously and the rate of crystalloid infusion was increased.
The sensorial block level and the motor block level were assessed by pinprick test and modified Bromage scale (0 = no motor block, 1 = hip flexion with extended leg blocked, 2 = knee flexion blocked, 3 = complete motor block), respectively. Time to reach the level of T10 and to Bromage 3 was also noted. Propofol infusion was started in all the patients at a dose of 50 mcg/kg/min after the level of block arised to T10 dermatome level. OAA/S scale was used for evaluating the level of sedation16 (Table 1). Intermittent 0.5 mL bolus doses of propofol were given for reaching to target OAA/S scores and BIS levels at the beginning of the sedation if necessary. Sedative agent (DEX vs propofol) infusion starting time was accepted as 0 point for the recording of the time to reach to OAA/S score 4 and the time to reach to BIS ≤ 80. Target BIS values were between 70 and 80. Infusion rate was titrated according to the targeted OAA/S scores and BIS levels. In case OAA/S score < 4 and BIS < 70, propofol infusion rate was reduced. Propofol infusion was stopped at the beginning of skin suturing.
Patients were monitored at the postoperative care unit and all monitoring parameters were registered at every 5 min for 1 h. Criteria for transferring the ward were OAA/S = 5, BIS > 90, Bromage = 0-1.
Total propofol consumption, time necessary to reach the targeted level of sedation (OAA/S score 4 and BIS ≤ 80), propofol dose required for targeted OAA/S score and BIS levels, recovery time (BIS > 90), duration of surgery, amount of bleeding, vasoactive drug need were recorded. Possible side effects and possible complications during the preoperative, intraoperative period and the postoperative follow-up such as hypotension (SBP < 90 mmHg), bradycardia (HR < 60 min), respiratory depression (SpO2 ≤ 90%), nausea, vomiting, and deep sedation were carefully monitored and recorded.
Statistical analysis
Statistical analysis was performed using the statistical package SPSS (Version 17.0, SPSS Inc., Chicago, IL, USA). The primary outcome of this study was total propofol consumption during the hip fracture surgery. A power analysis indicated that 26 patients per group were required to detect a true difference of 40 mg between groups where the anticipated standard deviation was 43.16. The standard deviation was based on a pilot group of patients undergoing hip fracture surgery. The type 1 error was set at 0.05 and type II error at 0.10. We allowed for 4 more patients in each groups to compensate for drop outs during the study period. For each continuous variable, normality was checked by Kolmogorov-Smirnov and Shapiro-Wilk tests and by histograms. Independent samplest-test and the Mann-Whitney U-test were performed for between-groups comparisons where appropriate. Pre-post measures were analyzed by Repeated Measure Analyses. Values ofp < 0.05 were considered to be statistically significant.
Results
Sixty-hemodialysis dependent chronic renal failure patient scheduled for hip fracture repair were enrolled in the study. Fig. 1presents the allocation of patients in groups. The groups were comparable with respect to demographic data, duration of surgery, time to reach to T10, to Bromage 3 and to Bromage 0 (Table 2).
Total propofol consumption, propofol dose required for targeted sedation levels and recovery time were significantly lower in Group D when compared with Group C (p < 0.001). The time to achieve to targeted sedation levels according to OAA/S score and BIS levels was significantly lower in Group C compared with Group D (p < 0.001). All the patients in Group D achieved targeted sedation levels with only DEX infusion without propofol infusion requirement ( Table 3).
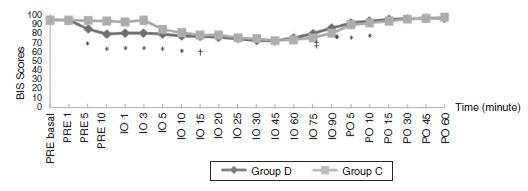
Comparison of preoperative OAA/S and BIS scores showed that the scores were significantly lower in Group D compared with Group C at preoperative 5th and 10th minutes (p < 0.001). Intraoperative OAA/S scores at 1-, 3-, 5-, 10th minutes and intraoperative BIS scores at 1-, 3-, 5-, 10-, 15th minutes were significantly lower in Group D compared with Group C (p < 0.05). The scores were similar in both groups till 75th minutes and were significantly lower at 75th, 90th minutes in group C (p < 0.05) ( Figure 2 and Figure 3). Postoperative OAA/S scores were similar between groups ( Fig. 3). Postoperative BIS scores were significantly lower at 5-, 10th minutes in Group C (p < 0.001); but was similar between groups after the 10th minutes ( Fig. 2).
BIS values of the patients. Values given are median (*p < 0.001; † p = 0.001; ‡ p = 0.002).
OAA/S scores of the patients. Values given are median (*p < 0.001; † p = 0.001). PRE, preoperative; Io, intraoperative; PO, postoperative.
The heart rate, SBP, DBP, SpO2 showed decrease at Group D but there were no significant differences among two groups. Hypotension was observed at 8 patients in Group D and 9 patients in Group C; bradycardia observed at 6 patients in Group D and 5 patients in Group C during the intraoperative period. However the difference between the groups was not statistically significant. None of the patients exhibited respiratory depression, nausea and vomiting.
Discussion
In this study we showed that in geriatric patients with chronic renal failure sedation regimen with DEX premedication reduces total propofol consumption with rapid recovery time (Group C: 16.73 ± 1.84 min; Group D: 7.30 ± 1.52 min). On the other hand, according to the pharmacokinetic properties the time required to attain the aimed level of sedation was significantly shorter with propofol in the control group (5.08 ± 0.51 min) in comparison with the DEX premedication (7.65 ± 1.49 min).
Propofol is an ultrafast agent with a peak effect within 5 min of administration and is used for sedation or anesthesia maintenance.1717. Lundström S, Twycross R, Mihalyo M, et al. Propofol. J Pain Symptom Manage. 2010;40:466-70. and 1818. Fechner J, Ihmsen H, Hatterscheid D, et al. Comparative pharmacokinetics and pharmacodynamics of the new propo- fol prodrug GPI 15715 and propofol emulsion. Anesthesiology. 2004;101:626-39. It has been reported that the pharmacokinetics of bolus or infusion doses are not affected markedly and can be used safely in ESRD patients.1919. Ickx B, Cockshott ID, Barvais L, et al. Propofol infusion for induc- tion and maintenance of anaesthesia in patients with end-stage renal disease. Br J Anaesth. 1998;81:854-60. and 2020. Kakinohana M, Tokumine J, Kawashima S, et al. Patient- controlled sedation using propofol in eight patients with endstage renal failure. J Anesth. 2004;18:39-42. DEX is a highly selective a2 adrenoceptor agonist drug with sedative, sympatholytic, and analgesic actions. It is metabolized into its inactive metabolites in liver and its elimination is unaffected by renal disease. By virtue of these properties, it may offer an alternative option for sedation in ESRD patients.1515. De Wolf AM, Fragen RJ, Avram MJ, et al. The pharmacokinetics of dexmedetomidine in volunteers with severe renal impair- ment. Anesth Analg. 2001;93:1205-9. and 2121. Gertler R, Brown HC, Mitchell DH, et al. Dexmedetomidine: a novel sedative-analgesic agent. Proc (Bayl Univ Med Cent). 2001;14:13-21. It has also been reported that it does not exert any respiratory depressant effect even in high doses, and it can be safely used for sedation in very elderly people.2222. Kunisawa T, Hanada S, Kurosawa A, et al. Dexmedetomidine was safely used for sedation during spinal anesthesia in a very elderly patient.. J Anesth 2010;24:938-41.
Dose determination studies for DEX in patients with chronic renal failure have demonstrated that the drug provided sufficient sedation with any significant side effect at a dose of 0.6 µg/kg/10 min in volunteer patients aged 18 to 65 years with creatinine clearance of <30.1515. De Wolf AM, Fragen RJ, Avram MJ, et al. The pharmacokinetics of dexmedetomidine in volunteers with severe renal impair- ment. Anesth Analg. 2001;93:1205-9. We also attained the desired sedation level without any significant hemodynamic response or side effect with similar premedication doses of DEX (0.5 µgr/kg/10 min). Also we observed that all the patients in Group D reached targeted sedation levels following preoperative DEX infusion without any propofol requirement.
It has been reported that DEX used as an additive agent decreases propofol consumption.2323. Sen S, Chakraborty J, Santra S, et al. The effect of dexmedeto- midine infusion on propofol requirement for maintenance of optimum depth of anaesthesia during elective spine surgery.. Indian J Anaesth 2013;57:358-63. Also in our study a propofol dose titration was performed after DEX premedication for sedation with the guidance of OAA/S and BIS monitoring. It was demonstrated that propofol consumption was 2.4-fold greater than the study group (197.0 mg vs 82.0 mg) and thus the recovery period was 2.29 times longer in the control group (16.73 min vs 7.30 min). According to these results, it may be suggested that the lower OAA/S and BIS scores at 75 and 90 min at the intraoperative period as well as lower BIS scores and a significantly longer recovery time at 5 and 10 min at the postoperative period observed in the control group were associated with a higher propofol consumption, and thus dexmedetomidine had an important effect on postoperative early recovery.
One other parameter that should be taken into consideration is the hemodynamic response. In addition to sympatholytic effects of spinal anesthesia, an additive interaction with cardiovascular effects of DEX and propofol may be possible. DEX is known to have some cardiovascular effects including hypotension and bradycardia owing to its sympatholytic effects. However, it has been reported that it offers a good cardiovascular stability and thus it is a good sedative agent.2424. Hall JE, Uhrich TD, Barney JA, et al. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions.. Anesth Analg 2000;90:699-705. and 2525. Bajwa S, Kulshrestha A. Dexmedetomidine: an adjuvant making large inroads into clinical practice. Ann Med Health Sci Res. 2013;3:475-83.
In a study comparing sedation application with dexmedetomidine or midazolam in ESRD patients it was reported that none of the patients experienced prolonged hypotension or bradycardia, all responded satisfactorily to the treatment, and none of them were excluded from the study even with large loading doses of 1 µg/kg/10 min of dex.1414. Rutkowska K, Knapik P, Misiolek H. The effect of dexmedeto- midine sedation on brachial plexus block in patients with end-stage renal disease. Eur J Anaesthesiol. 2009;26:851-5. We also did not demonstrate a significantly different hemodynamic response to DEX loaded at a dose of 0.5 µg/kg compared to the control group. However, both groups developed intraoperative hypotension (Group C, 30%; Group D, 26.7%) and bradycardia (Group C, 16.7%; Group D, 20%) after propofol infusion, which quickly resolved upon administration of sympathomimetics. This response may be an additive result of the venodilatative effect of propofol and the sympatholytic effect of spinal anesthesia rather than the effect of DEX.
In the present study we found that premedication with DEX at a dose of 0.5 µg/kg for 10 min attained sufficient and aimed sedation levels without propofol requirement during the preoperative period. DEX premedication also reduced intraoperative propofol consumption, significantly promoted early recovery and was not the cause of severe side effects. In conclusion, we believe that low dose DEX premedication in addition to propofol infusion might be an alternative regimen in geriatric patients with ESRD for sedation.
Acknowledgement
This study was supported by Baskent University Research Fund (Baskent University Instutional Review Board and Ethics Committee, Project number KA 12/166).
References
- 1. Ismail N, Hakim RM, Oreopoulos DG, et al. Renal replacement therapies in the elderly: Part 1. Hemodialysis and chronic peri- toneal dialysis. Am J Kidney Dis. 1993;22:759-82.
- 2. Keith DS. Transplantation in the elderly patient. Clin Geriatr Med. 2013;29:707-19.
- 3. Sasaki Y, Marioni R, Kasai M, et al. Chronic kidney disease: a risk factor for dementia onset: a population-based study The Osaki- Tajiri Project. J Am Geriatr Soc. 2011;59:1175-81.
- 4. Le- Wendling L, Bihorac A, Baslanti TO, et al. Regional anesthe- sia as compared with general anesthesia for surgery in geriatric patients with hip fracture: does it decrease morbidity, mortal- ity, and health care costs? Results of a single-centered study. Pain Med. 2012;13:948-56.
- 5. Jørgensen TSH, Hansen AH, Sahlberg M, et al. Falls and comorbidity: the pathway to fractures. Scand J Public Health. 2014;42:287-94.
- 6. Trainor D, Borthwick E, Ferguson A. Perioperative management of the hemodialysis patient. Semin Dial. 2011;24:314-26.
- 7. Byrick RJ. Anesthesia and end stage renal failure: is TIVA an advance? Can J Anaesth. 1999;46:621-2.
- 8. Hadimioglu N, Ulugol H, Akbas H, et al. Combination of epidural anesthesia and general anesthesia attenuates stress response to renal transplantation surgery. Transplant Proc. 2012;44:2949-54.
- 9. Brown DL. Spinal, epidural, and caudal anesthesia. In: Miller RD, editor. Miller's anesthesia. Elsevier Health Sciences; 2010. p. 1612-27.
- 10. Eddleston JM, Pollard BJ, Blades JF, et al. The use of propofol for sedation of critically ill patients undergoing haemodiafiltration. Intensive Care Med. 1995;21:342-7.
- 11. Lee SM, Kim GH, Lee JJ, et al. Does propofol and alfentanil- induced sedation cause periodic apnoea in chronic renal failure patients? Int J Clin Pract. 2010;64:1-5.
- 12. Beathard GA, Urbanes A, Litchfield T, et al. The risk of sedation/analgesia in hemodialysis patients undergoing inter- ventional procedures.. Semin Dial 2011;24:97-103.
- 13. Ok HG, Baek SH, Baik SW, et al. Optimal dose of dexmedetomi- dine for sedation during spinal anesthesia. Korean J Anesthesiol. 2013;64:426-31.
- 14. Rutkowska K, Knapik P, Misiolek H. The effect of dexmedeto- midine sedation on brachial plexus block in patients with end-stage renal disease. Eur J Anaesthesiol. 2009;26:851-5.
- 15. De Wolf AM, Fragen RJ, Avram MJ, et al. The pharmacokinetics of dexmedetomidine in volunteers with severe renal impair- ment. Anesth Analg. 2001;93:1205-9.
- 16. Bagchi D, Mandal MC, Das S, et al. Bispectral index score and observer's assessment of awareness/sedation score may mani- fest divergence during onset of sedation: study with midazolam and propofol. Indian J Anaesth. 2013;57:351-7.
- 17. Lundström S, Twycross R, Mihalyo M, et al. Propofol. J Pain Symptom Manage. 2010;40:466-70.
- 18. Fechner J, Ihmsen H, Hatterscheid D, et al. Comparative pharmacokinetics and pharmacodynamics of the new propo- fol prodrug GPI 15715 and propofol emulsion. Anesthesiology. 2004;101:626-39.
- 19. Ickx B, Cockshott ID, Barvais L, et al. Propofol infusion for induc- tion and maintenance of anaesthesia in patients with end-stage renal disease. Br J Anaesth. 1998;81:854-60.
- 20. Kakinohana M, Tokumine J, Kawashima S, et al. Patient- controlled sedation using propofol in eight patients with endstage renal failure. J Anesth. 2004;18:39-42.
- 21. Gertler R, Brown HC, Mitchell DH, et al. Dexmedetomidine: a novel sedative-analgesic agent. Proc (Bayl Univ Med Cent). 2001;14:13-21.
- 22. Kunisawa T, Hanada S, Kurosawa A, et al. Dexmedetomidine was safely used for sedation during spinal anesthesia in a very elderly patient.. J Anesth 2010;24:938-41.
- 23. Sen S, Chakraborty J, Santra S, et al. The effect of dexmedeto- midine infusion on propofol requirement for maintenance of optimum depth of anaesthesia during elective spine surgery.. Indian J Anaesth 2013;57:358-63.
- 24. Hall JE, Uhrich TD, Barney JA, et al. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions.. Anesth Analg 2000;90:699-705.
- 25. Bajwa S, Kulshrestha A. Dexmedetomidine: an adjuvant making large inroads into clinical practice. Ann Med Health Sci Res. 2013;3:475-83.
Publication Dates
-
Publication in this collection
Sep-Oct 2015
History
-
Received
17 Sept 2014 -
Accepted
11 Nov 2014