Abstract
Objective:
A first-degree relative affected by obsessive-compulsive disorder (OCD) and obsessive-compulsive symptoms (OCS) in childhood is an important risk factor for developing the disorder in adulthood. The relationship between a family history of OCD and the presence of OCS and its correlates in childhood is not well established.
Methods:
A total of 66 children whose parents or siblings have been diagnosed with OCD were assessed for the presence of OCS and clinical correlates.
Results:
Three children (4.5%) were reported to have received an OCD diagnosis and another 26 (39.4%) were identified as having OCS. Children with OCS had higher rates of coercive behavior and came from families with lower socioeconomic status. Contamination/cleaning dimension symptoms in the proband were associated with OCS in the assessed children.
Conclusion:
OCS are frequent among family members of individuals with OCD and are associated with socioeconomic status, coercive behaviors and proband contamination/cleaning symptoms. Future longitudinal studies should test the risk of developing OCD in association with these characteristics.
Obsessive-compulsive symptoms; children; familial OCD; coercive behaviors
Introduction
Obsessive-compulsive disorder (OCD) affects 2 to 4% of children and adolescents11. Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, et al. Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry. 1988;27:764-71. and 2 to 3% of adults.22. Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53-63. Twin and family studies indicate that OCD aggregates in families, and both genetic and environmental factors are relevant to the etiology of the disorder.33. Pauls DL Alsobrook JP 2nd, Goodman W, Rasmussen S, Leckman JF. A family study of obsessive-compulsive disorder. Am J Psychiatry. 1995;152:76-84.,44. Iervolino AC, Rijsdijk FV, Cherkas L, Fullana MA, Mataix-Cols D. A multivariate twin study of obsessive-compulsive symptom dimensions. Arch Gen Psychiatry. 2011;68:637-44. Studies indicate that the heritability of obsessive-compulsive symptoms (OCS) is higher in children (45-65%) than in adults (27-47%),55. Van Grootheest DS, Cath DC, Beekman AT, Boomsma DI. Twin studies on obsessive-compulsive disorder: a review. Twin Res Hum Genet. 2005;8:450-8. and approximately 50% of adults diagnosed with the disorder have their first OCS before age 11.66. De Mathis MA, Diniz JB, Hounie AG, Shavitt RG, Fossaluza V, Ferrão Y, et al. Trajectory in obsessive-compulsive disorder comorbidities. Eur Neuropsychopharmacol. 2013;23:594-601.
The prevalence of OCS in childhood is estimated at 5-8%66. De Mathis MA, Diniz JB, Hounie AG, Shavitt RG, Fossaluza V, Ferrão Y, et al. Trajectory in obsessive-compulsive disorder comorbidities. Eur Neuropsychopharmacol. 2013;23:594-601. and can occur as part of normal development.77. Evans DW, Gray FL, Leckman JF. The rituals, fears and phobias of young children: insights from development, psychopathology and neurobiology. Child Psychiatry Hum Dev. 1999;29:261-76. The large majority of children with OCS will not go on to develop OCD later in life.88. Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, et al. Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry. 2009;166:329-36. However, children with OCS have a six-fold increased risk of developing full-blown OCD in adulthood compared to those without OCS.88. Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, et al. Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry. 2009;166:329-36. Family history of OCD further increases the risk of the disorder in children with OCS.99. Hanna GL, Himle JA, Curtis GC, Gillespie BW. A family study of obsessive-compulsive disorder with pediatric probands. Am J Med Genet B Neuropsychiatr Genet. 2005;134B:13-9.,1010. Black DW, Gaffney GR, Schlosser S, Gabel J. Children of parents with obsessive-compulsive disorder -- a 2-year follow-up study. Acta Psychiatr Scand. 2003;107:305-13.
Multiple environmental factors are implicated in the etiology of the disorder,1111. Degnan KA, Almas AN, Fox NA. Temperament and the environment in the etiology of childhood anxiety. J Child Psychol Psychiatry. 2010;51(4):497-517. including specific patterns of child-parent interaction, such as overprotective parenting1212. Wilcox HC, Grados M, Samuels J, Riddle MA, Bienvenu OJ 3rd, Pinto A, et al. The association between parental bonding and obsessive compulsive disorder in offspring at high familial risk. J Affect Disord. 2008;111:31-9. and family accommodation to the symptoms.1313. Calvocoressi L, Mazure CM, Kasl SV, Skolnick J, Fisk D, Vegso SJ, et al. Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family behavior. J Nerv Ment Dis. 1999;187:636-42. In addition, specific OCS and associated clinical characteristics may be associated with the establishment of rigid behavior patterns and the development of the disorder. Coercive behavior that can assume the topography of aggressive outbursts in children with OCD has been identified as rather common in the clinical presentation of the disorder.1414. Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, et al. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry. 2012;51:582-92. According to behavior-analytic theory, coercion is a behavioral control mechanism based on negative reinforcement.1515. Sidman M. Coercion and its fallout. Boston: Authors Cooperative; 1989. Recurrent aggressive and angry behavior triggered by minor provocations can be defined as coercive behavior.1616. Budman CL, Bruun RD, Park KS, Olson ME. Rage attacks in children and adolescents with Tourette's disorder: a pilot study. J Clin Psychiatry. 1998;59:576-80. Such behaviors are not exclusively related to obsessions or compulsions and could be part of the broad clinical presentation of children with OCD.1414. Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, et al. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry. 2012;51:582-92. Although not previously investigated, it is theoretically possible that children with OCS and a positive family history of the disorder who also present coercive behavior may have a higher risk of developing OCD, since this behavior helps perpetuate rituals through negative reinforcement.
The present study aims to estimate the prevalence of OCS among children with a first degree relative (parent or sibling) with OCD. Additionally, we investigated the presence of clinical correlates, specifically coercive behavior, obsessive-compulsive dimensions, and demographic characteristics of higher risk children and their relatives.
Methods
Participants and procedures
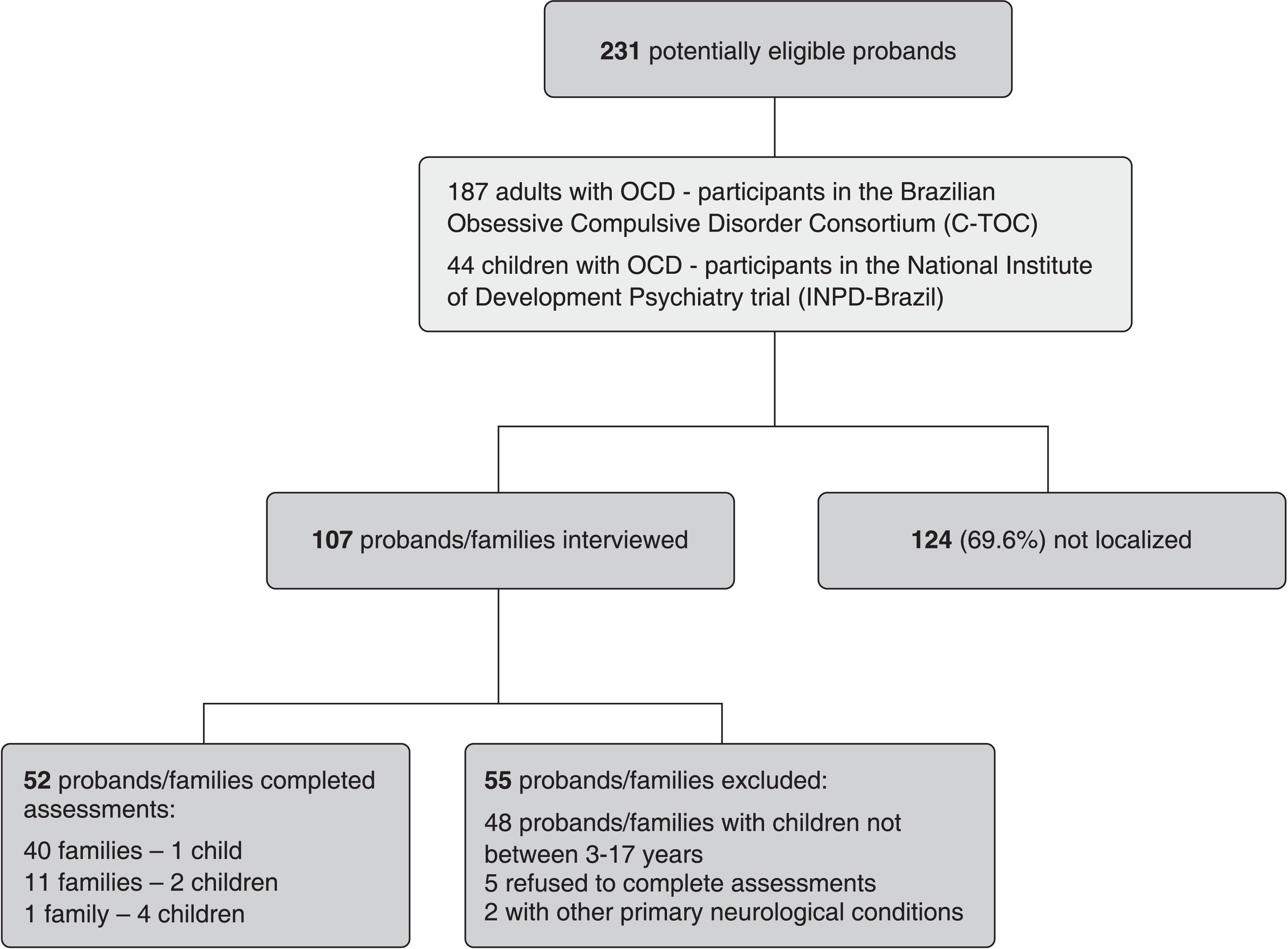
Children aged 3 to 17 years with a first-degree relative (proband) with a confirmed OCD diagnosis according to DSM-IV criteria were selected for this study. Probands were identified through two studies conducted by our research group. The first study (Study 1) is the Brazilian obsessive-compulsive consortium,1717. Miguel EC, Ferrão YA, Rosário MC, Mathis MA, Torres AR, Fontenelle LF, et al. The Brazilian research consortium on obsessive-compulsive spectrum disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Rev Bras Psiquiatr. 2008;30:185-96. a national database of adult patients with OCD selected from seven sites who have undergone directed interviews with experienced psychiatrists. We contacted all patients with offspring living in the state of São Paulo. The second study (Study 2) is a clinical trial of children with OCD conducted in the context of the National Institute of Developmental Psychiatry for Children and Adolescents.1818. Miguel EC, Mercadante MT, Grisi S, Rohde LA. [The National Science and Technology Institute in child and adolescence developmental psychiatry: a new paradigm for Brazilian psychiatry focused on our children and their future]. Rev Bras Psiquiatr. 2009;31:85-8. Children aged 7 to 17 years with a primary OCD diagnosis that had been confirmed by a child and adolescent psychiatrist were invited to participate in this clinical trial. For the present study, the siblings of children with OCD were invited to participate.
We succeeded in contacting 102 probands with OCD (Figure 1), of which 52 had children or siblings aged 3 to 17 years (40 families with one child, 11 families with two, and 1 with four children); thus, a total 66 children were assessed. The assessments were conducted via phone with the primary caregiver (78.8% mothers) by a psychologist experienced with OCD (PC). Children with a reported diagnosis of autistic spectrum disorders, schizophrenia, organic mental disorders or intellectual disability were excluded. This project was approved by the ethics committee of the Hospital das Clinicas, Universidade de São Paulo (protocol 0656/11).
Assessments
Initially, the assessment intended to identify children of interest by contacting the probands. Subsequently, OCS and age of onset were investigated. OCS were defined as the presence of any recognized OCS that involved no functional impairment or discomfort. The following questions were made to assess their presence: 1) “Has your child ever talked about intrusive thoughts, fears or images that he/she can’t get out of his/her mind and are very repetitive?”; 2) “Have you noticed repetitive questions, such as whether the door is really locked, whether he/she is actually in good health, or whether he/she is dirty?”; 3) “Does your child do the same thing over and over again, like organizing his/her belongings or washing his/her hands, or checking to see if the door is locked?”; 4) “Does your child have the urge to count things like books on a shelf or organize things in a certain order?”; 5) “Have you ever observed your child pronouncing a certain word repetitively?” If parents responded positively about a certain symptom, the clinician probed further to confirm its presence and classified it as one of the following (non-mutually exclusive) dimensions: aggression, sexual/religious, symmetry/ordering, contamination/cleaning, hoarding and miscellaneous, according to the Yale-Brown Obsessive-Compulsive Scale (YBOCS) checklist.1919. Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, et al. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006;11:495-504. Age of onset was defined as the first time the parents noticed the symptoms. The parents were asked whether their children were diagnosed with OCD by a mental health professional and whether treatment was indicated. Finally, three specific questions directly investigating the presence of coercive behaviors or rage attacks from the Childhood Temperament Questionnaire2020. Sanson A, Smart D, Prior M, Oberklaid F. The structure of temperament from age 3 to 7 years: age, sex, and sociodemographic influences. J Dev Psychol. 1994;40:233-52. were asked: 1) When upset or annoyed with a task, my child throws down what he is holding, cries, slams doors, etc.; 2) When shopping together, if I do not buy what my child wants (e.g. sweets, clothing), he/she cries and yells; 3) When my child objects to wearing certain clothing, he/she argues loudly or cries. Responses were given in a Likert scale as follows: 0 meaning never, 1 meaning almost never, 2 meaning rarely, 3 meaning sometimes, 4 meaning often, 5 meaning almost all the time. If a child scored 4 or 5 on at least two of these three questions, he/she was considered to present coercive behavior. The mean length of the phone interviews was 35 minutes.
Statistical analysis
Descriptive analyses were conducted and the children were then compared based on the presence of OCS. Continuous variables were compared with the t-test and categorical variables were compared with the χ2 and Fischer test. The level of statistical significance was set at 5%. SPSS version 15.0 was used for all analyses.
Results
Sixty-six children were assessed, of which three (4.5%) were reported to be diagnosed with OCD and were currently in treatment, while another 26 (39.4%) presented OCS. The parents of 47 (71.2%) children had been diagnosed with OCD (from Study 1), and the siblings of 16 (24.2%) had been diagnosed with OCD (Study 2). There were no differences in demographic or clinical characteristics between the children according to relationship to the proband (data available upon request). Table 1 shows the demographic and clinical characteristics of the full sample (n=66). Most of the children were male (56%), caucasian (86.4%), and from a higher (A and B) socioeconomic class (59.1%). Among children with OCS, ordering/symmetry and cleaning/contamination were the most prevalent dimensions of symptoms, followed by aggression, miscellaneous, hoarding and sexual/religious. Tics were reported in 3 (4.5%) children. Mental health care had been sought for 23 (34.8%) children.
To investigate whether the presence of OCS in children with a family history of OCD were associated with other risk markers, we compared children with vs. without OCS (Table 2). Since there were 26 children from families with more than 2 siblings evaluated and risk factors can correlate between members of the same family, we excluded the younger siblings of each family from the analysis. A total of 11 children from 11 families with 2 evaluated siblings and 3 children from one family with 4 evaluated children were excluded from the comparative analysis between OCS-positive and OCS-negative groups. Children with OCD were also excluded. A total of 49 children were considered for analysis, as presented in Table 2. Fourteen children whose parents were diagnosed with OCD presented OCS (66.7%) and there were seven children whose siblings presented OCS χ2 = 0.408; p = 0.523). Regarding the children’s characteristics, OCS-positive children had a lower socioeconomic status (64.2% of the OCS-negative children were in class A or B while only 38% of the OCS-positive children were); χ2 = 11.941, p = 0.008) and displayed more coercive behaviors (61.9% vs. 25%; χ2 = 6.766, p = 0.009). Regaring the proband characteristics, probands of OCS-positive children more frequently presented cleaning/contamination symptoms (95.2% vs. 67.9%). The two groups did not differ in the other assessed characteristics (Table 2).
Discussion
This study evaluated the presence of OCS in children with a first-degree relative diagnosed with OCD and its clinical and demographic correlates. Approximately 40% of the sample presented OCS (28 of 63 evaluated children), which was associated with lower socioeconomic status, coercive behavior, and family members with cleaning/contamination symptoms.
The prevalence of OCD in this sample of 66 children (n=3; 4.5%) was lower than expected, since previous family studies have reported up to 11%33. Pauls DL Alsobrook JP 2nd, Goodman W, Rasmussen S, Leckman JF. A family study of obsessive-compulsive disorder. Am J Psychiatry. 1995;152:76-84. OCD in family members of affected individuals. Considering that the mean age of our sample (9.59 years, SD 4.09) was considerably lower than the mean age of childhood or adolescent onset, new cases are expected to occur in the sample, which would increase the final disorder rate.22. Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53-63.,2121. GelleR DA, Biederman J, Faraone S, Agranat A, Cradock K, Hagermoser L, et al. Developmental aspects of obsessive compulsive disorder: findings in children, adolescents, and adults. J Nerv Ment Dis. 2001;189:471-7. The high prevalence of OCS in our sample contrasts with the literature, which has reported from 8%2222. Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, et al. Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry. 2009;166:329-36.-19% of subclinical OCD.2323. Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL, et al. Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry. 1994;33:782-91. Again, the sample’s characteristics are likely to explain the substantially higher rate of OCS, suggesting that first-degree relatives of individuals with OCD have an increased risk of presenting symptoms, which may precede the development of the disorder. Longitudinal studies are necessary to confirm this hypothesis. There was a significant difference in socioeconomic status between families with OCS-positive and OC-negative children. Families with a lower socioeconomic status could have a higher risk of developing OCS.
A new and intriguing finding was that OCS is highly associated with coercive behaviors.1515. Sidman M. Coercion and its fallout. Boston: Authors Cooperative; 1989.,1616. Budman CL, Bruun RD, Park KS, Olson ME. Rage attacks in children and adolescents with Tourette's disorder: a pilot study. J Clin Psychiatry. 1998;59:576-80. Rage attacks were recently identified as a coercive behavior affecting up to 40% of children with OCD, whether related or not to obsessions or compulsions, and play an important role in perpetuating OCD.2424. Krebs G, Bolhuis K, Heyman I, Mataix-Cols D, Turner C, et al. Temper outbursts in paediatric obsessive-compulsive disorder and their association with depressed mood and treatment outcome. J Child Psychol Psychiatry. 2013;54:313-22. Indeed, rage attacks very often involve one or more family members2525. Painuly NP, Grover S, Gupta N, Mattoo SK. Prevalence of anger attacks in depressive and anxiety disorders: implications for their construct? Psychiatry Clin Neurosci. 2011;65:165-74. and have a direct impact on family accommodation of OCS.1414. Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, et al. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry. 2012;51:582-92.,2626. Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother. 2012;12:229-38.,2727. Lebowitz ER, Omer H, Leckman JF. Coercive and disruptive behaviors in pediatric obsessive-compulsive disorder. Depress Anxiety. 2011;28:899-905. Family accommodation refers to the way that family members modify their behaviors or daily routine to either avoid conflict with a relative who has OCD or even take part in the rituals.2626. Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother. 2012;12:229-38.,2828. Calvocoressi L, Lewis B, Harris M, Trufan SJ, Goodman WK, McDougle CJ, et al. Family accommodation in obsessive-compulsive disorder. Am J Psychiatry. 1995;152:441-3. Family accommodation, manifested by facilitating or participating in a given compulsion due to fear of an outburst, is a frequent response to a patient’s coercive behavior and may be one mechanism by which coercive behavior sustains obsessions and compulsions. Previous studies2929. Fava M, Rappe SM, West J, Herzog DB. Anger attacks in eating disorders. Psychiatry Res. 1995;56:205-12.
30. Grover S, Painuly N, Gupta N, Mattoo SK. Anger attacks in bipolar versus recurrent depression. Turk Psikiyatri Derg. 2011;22:239-44.-3131. Painuly NP, Grover S, Mattoo SK, Gupta N. Anger attacks in obsessive compulsive disorder. Ind Psychiatry J. 2011;20:115-9. have reported “anger attacks” by patients with anxiety, including both OCD and depression patients. Whether OCD with coercive behavior presented as rage attacks is a distinct disorder is still unclear,1414. Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, et al. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry. 2012;51:582-92. and whether the association of rage attacks and OCS further increases the risk of later development of OCD is a matter for future longitudinal studies.
In our study, the children did not differ in any characteristic based on the relationship with the proband affected by OCD. Moreover, a large population-based, multigenerational, case-control family and twin study demonstrated that relatives at similar genetic distances had similar risks for OCD, despite the different degrees of shared environment.3232. Mataix-Cols D, Boman M, Monzani B, Rück C, Serlachius E, Långström N, et al. Population-based, multigenerational family clustering study of obsessive-compulsive disorder. JAMA Psychiatry. 2013;70:709-17. The risk of OCD in full siblings and parents of individuals with OCD were 6.32% (95% confidence interval [95%CI] 5.0-7.9) and 5.68% (95%CI 4.4-7.3), respectively.3232. Mataix-Cols D, Boman M, Monzani B, Rück C, Serlachius E, Långström N, et al. Population-based, multigenerational family clustering study of obsessive-compulsive disorder. JAMA Psychiatry. 2013;70:709-17. The strong association between the cleaning/contamination dimension in the affected first degree relative and OCS could indicate a possible familial subtype of OCD. However, our findings diverge from other studies that have found a familial subtype of OCD associated with early symptom onset and the presence of ordering factor.3333. Hanna GL, Fischer DJ, Chadha KR, Himle JA, Van Etten M. Familial and sporadic subtypes of early-onset obsessive-compulsive disorder. Biol Psychiatry. 2005;57:895-900. Other studies have found familial aggregation of OCS dimensions, especially symmetry and checking,3434. Leckman JF, Pauls DL, Zhang H, Rosario-Campos MC, Katsovich L, Kidd KK, et al. Obsessive-compulsive symptom dimensions in affected sibling pairs diagnosed with Gilles de la Tourette syndrome. Am J Med Genet B Neuropsychiatr Genet. 2003;116B:60-8.
35. Chacon P, Rosario-Campos MC, Pauls DL, Hounie AG, Curi M, Akkerman F, et al. Obsessive-compulsive symptoms in sibling pairs concordant for obsessive-compulsive disorder. Am J Med Genet B Neuropsychiatr Genet. 2007;144B:551-5.-3636. Hasler G, Pinto A, Greenberg BD, Samuels J, Fyer AJ, Pauls D, et al. Familiality of factor analysis-derived YBOCS dimensions in OCD-affected sibling pairs from the OCD collaborative genetics study. Biol Psychiatry. 2007;61:617-25. but also cleaning/contamination.3737. Katerberg H, Delucchi KL, Stewart SE, Lochner C, Denys DA, Stack DE, et al. Symptom dimensions in OCD: item-level factor analysis and heritability estimates. Behav Genet. 2010;40:505-17. Given the low number of individuals with symptoms in our sample, our study was not powered to investigate this issue.
Considering that family members with OCD frequently have contamination and cleaning symptoms and studies indicate that they tend to over-report their symptoms,66. De Mathis MA, Diniz JB, Hounie AG, Shavitt RG, Fossaluza V, Ferrão Y, et al. Trajectory in obsessive-compulsive disorder comorbidities. Eur Neuropsychopharmacol. 2013;23:594-601. we speculate that these families must have a particular dynamic or environment that facilitates or is more conducive to the development or maintenance of psychopathology in the offspring, possible by involving children in their cleaning/contamination obsessions and/or compulsions. Future studies should consider the presence of contamination/cleaning compulsions and coercive behaviors together to assess their relationship to the development and maintenance of OCD.
Our study should be understood in the context of its limitations. First, the assessments were limited to a telephone interview, and we were not able to rely on clinical assessments with multiple informants and strategies. Because OCS are considered silent, not directly interviewing the children probably resulted in under-estimation of their occurrence. It is already difficult for adults with OCD to seek treatment and it has been especially challenging to have parents bring in their children for clinical assessments. On the other hand, parents could over-report their children’s behavior due to having another family member with the disorder. To address this potential bias, a clinician with experience in treating children and adults with OCD conducted the interviews. Additionally, phone assessment is a time- and cost-saving strategy, and its efficiency in screening children and adolescents has already been demonstrated.3838. Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154:1593-8. Second, we were only able to interview a subsample of individuals who were potentially eligible for the study. Finally, this study relied on a small sample size, which is frequent in high-risk samples but limits the applicability of the findings.
This study has implications for clinicians and researchers. For clinicians, our results underscore the high prevalence of OCS in children and siblings of individuals with OCD. It also extends the previously detected association between coercive behaviors (or rage attacks), OCD and OCS. It indicates the importance and functional relevance of actively evaluating the presence of these symptoms in first-degree relatives of patients with OCD. For researchers, our results suggest the importance of assessing the predictive value of OCS and coercive behaviors on the later development of OCD. These symptoms may be additional risk markers for developing the disorder in children already at higher risk. Whether they are mediators or moderators of risk and genetically or environmentally mediated are also subjects for future longitudinal studies.
Our study demonstrated that OCS are common in first-degree relatives of individuals with OCD and are associated with lower socioeconomic status, coercive behaviors, and proband contamination/cleaning symptoms. Longitudinal studies are necessary to elucidate the long-term impact of these characteristics on the development of OCD. By further defining the profile of children at increased risk for developing OCD, significant progresses may be possible in prevention. As developmental risk factors for OCD are identified, the field may move from treatment interventions to preventive strategies, which is a desired change of paradigm.
References
-
1Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, et al. Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry. 1988;27:764-71.
-
2Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53-63.
-
3Pauls DL Alsobrook JP 2nd, Goodman W, Rasmussen S, Leckman JF. A family study of obsessive-compulsive disorder. Am J Psychiatry. 1995;152:76-84.
-
4Iervolino AC, Rijsdijk FV, Cherkas L, Fullana MA, Mataix-Cols D. A multivariate twin study of obsessive-compulsive symptom dimensions. Arch Gen Psychiatry. 2011;68:637-44.
-
5Van Grootheest DS, Cath DC, Beekman AT, Boomsma DI. Twin studies on obsessive-compulsive disorder: a review. Twin Res Hum Genet. 2005;8:450-8.
-
6De Mathis MA, Diniz JB, Hounie AG, Shavitt RG, Fossaluza V, Ferrão Y, et al. Trajectory in obsessive-compulsive disorder comorbidities. Eur Neuropsychopharmacol. 2013;23:594-601.
-
7Evans DW, Gray FL, Leckman JF. The rituals, fears and phobias of young children: insights from development, psychopathology and neurobiology. Child Psychiatry Hum Dev. 1999;29:261-76.
-
8Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, et al. Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry. 2009;166:329-36.
-
9Hanna GL, Himle JA, Curtis GC, Gillespie BW. A family study of obsessive-compulsive disorder with pediatric probands. Am J Med Genet B Neuropsychiatr Genet. 2005;134B:13-9.
-
10Black DW, Gaffney GR, Schlosser S, Gabel J. Children of parents with obsessive-compulsive disorder -- a 2-year follow-up study. Acta Psychiatr Scand. 2003;107:305-13.
-
11Degnan KA, Almas AN, Fox NA. Temperament and the environment in the etiology of childhood anxiety. J Child Psychol Psychiatry. 2010;51(4):497-517.
-
12Wilcox HC, Grados M, Samuels J, Riddle MA, Bienvenu OJ 3rd, Pinto A, et al. The association between parental bonding and obsessive compulsive disorder in offspring at high familial risk. J Affect Disord. 2008;111:31-9.
-
13Calvocoressi L, Mazure CM, Kasl SV, Skolnick J, Fisk D, Vegso SJ, et al. Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family behavior. J Nerv Ment Dis. 1999;187:636-42.
-
14Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, et al. Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry. 2012;51:582-92.
-
15Sidman M. Coercion and its fallout. Boston: Authors Cooperative; 1989.
-
16Budman CL, Bruun RD, Park KS, Olson ME. Rage attacks in children and adolescents with Tourette's disorder: a pilot study. J Clin Psychiatry. 1998;59:576-80.
-
17Miguel EC, Ferrão YA, Rosário MC, Mathis MA, Torres AR, Fontenelle LF, et al. The Brazilian research consortium on obsessive-compulsive spectrum disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Rev Bras Psiquiatr. 2008;30:185-96.
-
18Miguel EC, Mercadante MT, Grisi S, Rohde LA. [The National Science and Technology Institute in child and adolescence developmental psychiatry: a new paradigm for Brazilian psychiatry focused on our children and their future]. Rev Bras Psiquiatr. 2009;31:85-8.
-
19Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, et al. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006;11:495-504.
-
20Sanson A, Smart D, Prior M, Oberklaid F. The structure of temperament from age 3 to 7 years: age, sex, and sociodemographic influences. J Dev Psychol. 1994;40:233-52.
-
21GelleR DA, Biederman J, Faraone S, Agranat A, Cradock K, Hagermoser L, et al. Developmental aspects of obsessive compulsive disorder: findings in children, adolescents, and adults. J Nerv Ment Dis. 2001;189:471-7.
-
22Fullana MA, Mataix-Cols D, Caspi A, Harrington H, Grisham JR, Moffitt TE, et al. Obsessions and compulsions in the community: prevalence, interference, help-seeking, developmental stability, and co-occurring psychiatric conditions. Am J Psychiatry. 2009;166:329-36.
-
23Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL, et al. Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry. 1994;33:782-91.
-
24Krebs G, Bolhuis K, Heyman I, Mataix-Cols D, Turner C, et al. Temper outbursts in paediatric obsessive-compulsive disorder and their association with depressed mood and treatment outcome. J Child Psychol Psychiatry. 2013;54:313-22.
-
25Painuly NP, Grover S, Gupta N, Mattoo SK. Prevalence of anger attacks in depressive and anxiety disorders: implications for their construct? Psychiatry Clin Neurosci. 2011;65:165-74.
-
26Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother. 2012;12:229-38.
-
27Lebowitz ER, Omer H, Leckman JF. Coercive and disruptive behaviors in pediatric obsessive-compulsive disorder. Depress Anxiety. 2011;28:899-905.
-
28Calvocoressi L, Lewis B, Harris M, Trufan SJ, Goodman WK, McDougle CJ, et al. Family accommodation in obsessive-compulsive disorder. Am J Psychiatry. 1995;152:441-3.
-
29Fava M, Rappe SM, West J, Herzog DB. Anger attacks in eating disorders. Psychiatry Res. 1995;56:205-12.
-
30Grover S, Painuly N, Gupta N, Mattoo SK. Anger attacks in bipolar versus recurrent depression. Turk Psikiyatri Derg. 2011;22:239-44.
-
31Painuly NP, Grover S, Mattoo SK, Gupta N. Anger attacks in obsessive compulsive disorder. Ind Psychiatry J. 2011;20:115-9.
-
32Mataix-Cols D, Boman M, Monzani B, Rück C, Serlachius E, Långström N, et al. Population-based, multigenerational family clustering study of obsessive-compulsive disorder. JAMA Psychiatry. 2013;70:709-17.
-
33Hanna GL, Fischer DJ, Chadha KR, Himle JA, Van Etten M. Familial and sporadic subtypes of early-onset obsessive-compulsive disorder. Biol Psychiatry. 2005;57:895-900.
-
34Leckman JF, Pauls DL, Zhang H, Rosario-Campos MC, Katsovich L, Kidd KK, et al. Obsessive-compulsive symptom dimensions in affected sibling pairs diagnosed with Gilles de la Tourette syndrome. Am J Med Genet B Neuropsychiatr Genet. 2003;116B:60-8.
-
35Chacon P, Rosario-Campos MC, Pauls DL, Hounie AG, Curi M, Akkerman F, et al. Obsessive-compulsive symptoms in sibling pairs concordant for obsessive-compulsive disorder. Am J Med Genet B Neuropsychiatr Genet. 2007;144B:551-5.
-
36Hasler G, Pinto A, Greenberg BD, Samuels J, Fyer AJ, Pauls D, et al. Familiality of factor analysis-derived YBOCS dimensions in OCD-affected sibling pairs from the OCD collaborative genetics study. Biol Psychiatry. 2007;61:617-25.
-
37Katerberg H, Delucchi KL, Stewart SE, Lochner C, Denys DA, Stack DE, et al. Symptom dimensions in OCD: item-level factor analysis and heritability estimates. Behav Genet. 2010;40:505-17.
-
38Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154:1593-8.
Publication Dates
-
Publication in this collection
11 June 2018 -
Date of issue
Oct-Dec 2018
History
-
Received
03 May 2017 -
Accepted
14 Sept 2017