Abstracts
Dermatomyositis is an inflammatory myopathy with skin manifestations. In the adult over the age of 50 years, it can be associated with malignant neoplasias, being, thus, a signal of malignancy. OBJECTIVE: To show the association of dermatomyositis of atypical presentation with two synchronous tumors, usually not related to that. CASE REPORT: We report the case of a 72-year-old male, who developed dermatomyositis, initially with only classic skin findings, which progressed to vesiculobullous lesions, and, months later, to myopathy. After extensive investigation, prostate adenocarcinoma was diagnosed. After treatment of the cancer and administration of glucocorticoid, the disease went into remission. During gradual glucocorticoid withdrawal, dermatomyositis recurred, and the new investigation revealed the presence of squamous cell carcinoma of the tongue. After treating this neoplasia, complete remission occurred, even after total corticoid withdrawal. CONCLUSION: This is a rare case involving less usual dermatomyositis presentation forms, relating to the cutaneous-muscle findings and the association with prostate and tongue tumors (tumors never reported together). This case demonstrates the importance of a careful investigation, searching for neoplasias, when approaching such patients.
dermatomyositis; paraneoplastic syndromes; prostate neoplasias; tongue neoplasias
A dermatomiosite é uma miopatia inflamatória que cursa com manifestações cutâneas. No adulto acima de 50 anos, pode estar associada a neoplasias malignas, comportando-se como um grande sinalizador de malignidade. OBJETIVO: Demonstrar essa associação com aspectos peculiares: dermatomiosite de apresentação atípica paralela a dois tumores sincrônicos, em geral, não relacionados àquela. RELATO DO CASO: Descrevemos o caso de um paciente do gênero masculino de 72 anos, que desenvolveu dermatomiosite, inicialmente apenas com quadro cutâneo clássico, evoluindo com lesões vesiculobolhosas, e, meses após, com miopatia. Após extensa investigação, foi localizado um adenocarcinoma de próstata. Houve remissão da doença após tratamento do câncer e administração de glicocorticoide. Durante a retirada gradual do glicocorticoide, ocorreu reativação da dermatomiosite, sendo reiniciadas investigações, que revelaram a presença de carcinoma escamoso de língua. Tratada esta neoplasia, houve remissão completa, mesmo após a retirada total do corticoide. CONCLUSÃO: Trata-se de um caso raro por envolver as formas menos usuais de apresentação da dermatomiosite, tanto com relação ao quadro cutaneomuscular, quanto à sua associação a tumores de próstata e língua (tumores nunca antes relatados juntos). Este caso demonstra a importância da investigação minuciosa em busca de neoplasias na abordagem desses pacientes.
dermatomiosite; síndromes paraneoplásicas; neoplasias da próstata; neoplasias da língua
CASE REPORT
IMedical student of the UFF
IIResident physician of Internal Medicine of the Hospital Antônio Pedro of the UFF
IIIRheumatologist of the Hospital Antônio Pedro of the UFF
IVProfessor of Dermatology of the Hospital Antônio Pedro of the UFF
VProfessor of the Internal Medicine Residency of the Hospital Antônio Pedro of the UFF
Correspondence to
ABSTRACT
Dermatomyositis is an inflammatory myopathy with skin manifestations. In the adult over the age of 50 years, it can be associated with malignant neoplasias, being, thus, a signal of malignancy.
OBJECTIVE: To show the association of dermatomyositis of atypical presentation with two synchronous tumors, usually not related to that.
CASE REPORT: We report the case of a 72-year-old male, who developed dermatomyositis, initially with only classic skin findings, which progressed to vesiculobullous lesions, and, months later, to myopathy. After extensive investigation, prostate adenocarcinoma was diagnosed. After treatment of the cancer and administration of glucocorticoid, the disease went into remission. During gradual glucocorticoid withdrawal, dermatomyositis recurred, and the new investigation revealed the presence of squamous cell carcinoma of the tongue. After treating this neoplasia, complete remission occurred, even after total corticoid withdrawal.
CONCLUSION: This is a rare case involving less usual dermatomyositis presentation forms, relating to the cutaneous-muscle findings and the association with prostate and tongue tumors (tumors never reported together). This case demonstrates the importance of a careful investigation, searching for neoplasias, when approaching such patients.
Keywords: dermatomyositis, paraneoplastic syndromes, prostate neoplasias, tongue neoplasias.
INTRODUCTION
Dermatomyositis (DM) is an idiopathic inflammatory myopathy, more common in women (2:1). In adults, the incidence peak is between 40 and 50 years. It is clinicall y characterized by proximal symmetric muscle weakness and skin findings, such as Gottron's papules, heliotrope rash, shawl or "V" sign, periungual erythema and telangiectasia, and, more rarely, vesiculobullous formations. The inner organs can also be affected, resulting in the following: interstitial lung disease; dysphagia, due to involvement of the esophageal musculature; myocarditis; and malignant neoplasias concomitant to the disease (paraneoplastic DM). In some cases, the skin lesions begin in patients with no subjective complaint of muscle weakness, but with evidence of myositis on laboratory, imaging and histopathological tests, a condition called hypomyopathic DM. In the absence of any complaint or evidence of myositis, but in the presence of typical skin lesions, the disorder is called amyopathic DM. Some authors have suggested that those forms can represent up to 20% of the DM cases.1
The following elements are important to the DM diagnosis: the myopathic pattern on muscle and skin biopsy and on electroneuromyography; muscle inflammation on magnetic resonance imaging; elevation of muscle enzymes [creatine kinase (CK), lactic dehydrogenase (LDH), aldolase, aminotransferases]; and presence of ANA (80%) and myositis-specific autoantibodies, such as anti-Jo-1 and antiMi-2 antibodies. The major treatment for DM consists in the administration of glucocorticoids at immunosuppressing doses (prednisone, 1 mg/kg/day) and management of the subjacent neoplasia, when present. The therapy with glucocorticoids should be accompanied by immunosuppressant drugs (azathioprine or methotrexate). Those drugs are used as glucocorticoid savers, and, at higher doses, when the response to glucocorticoids fails in one to two months or in the presence of frequent relapses.2
CASE REPORT
The patient is a 72-year-old male nurse technician, of mixed heritage, who reported erythema, pruritus and scaly eruption on the face and cervical region, which progressed to the lower limbs, chest, abdomen, and thighs, assuming a violaceous color. He was treated with antihistamines, antibiotics, and topic glucocorticoids unsuccessfully. Four months later, he began to experience the following: mild proximal muscle weakness; weight loss of approximately 6 kg; hyporexia; significant adynamia; temporo-occipital, pulsatile, intermittent headache, refractory to tramadol and amitriptyline; and urinary incontinence. The patient had arterial hypertension, diabetes, and, in the past, hepatitis B. He was on enalapril, chlorthalidone and metformin. He was an ex-smoker (40 years ago), drank socially, and knew no allergies.
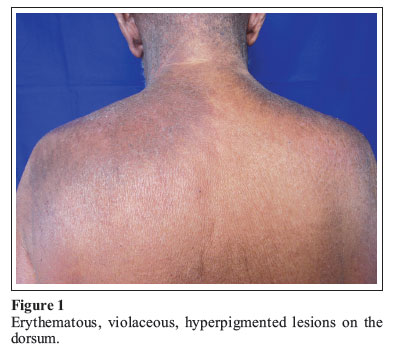
On physical examination, the patient was pale (+/4) and had erythematous, violaceous, scaly lesions affecting his face, upper limbs, chest and thighs, in addition to periungual areas of hyperpigmentation (Figure 1) and erythema. The neurological exam showed proximal and symmetric muscle weakness in upper and lower limbs (grade IV muscle strength), preserved static strength, slow deep reflexes, preserved superficial and deep sensitivity, and mild trembling and dysmetria in the right upper limb. The cranial nerves were preserved. The rest of the physical exam was within the normal range.
The laboratory findings were as follows: anemia of chronic disease; ESR: 77 mm/h (N: up to 15 mm/h); total CK: 65 U/L (N: 38-174 U/L); GOT: 26 U/L (N:12-38 U/L); GPT: 20 U/L (N: 7-41 U/L); LDH: 320 U/L (N:2 40-480 U/L); ANA 1:1280, fine speckled cytoplasmic pattern.
The patient developed bullous lesions on the previously affected skin areas (Figure 2). The myopathic pattern was evident on electromyography. The skin biopsy revealed subepidermal vacuolar and vesicular interface dermatitis associated with the presence of melanophages in the papillary dermis, scarce lymphocytic infiltration, and mucin deposition in the papillary dermis. Those alterations suggest DM with subepidermal vesicular formations. The histopathological study of the muscle supported the diagnosis of DM, revealing perimysial perivascular mononuclear lymphocytic infiltration and mild perifascicular atrophy.
Once the clinical suspicion was confirmed, subjacent neoplasias were investigated. Chest radiography and computed tomography, high digestive endoscopy, and colonoscopy showed no signs of malignancy. Abdominal ultrasound evidenced moderate bilateral hydronephrosis and overdistended urinary bladder. This finding added to a PSA of 44 ng/mL (N: < 5 ng/mL) and urinary incontinence, which was attributed to overflow, directed our search to prostate disease. Transrectal ultrasound with prostate biopsy was performed, and acinar adenocarcinoma was identified. The patient was diagnosed as having paraneoplastic DM associated with prostate adenocarcinoma. Systemic corticotherapy with 80 mg/day of prednisone was initiated, leading to a significant improvement in muscle weakness and skin lesions. The patient was discharged from the hospital, and followed up at the Internal Medicine and Rheumatology outpatient clinics. He was also referred to Oncology for treating the prostate neoplasia with hormone and radiation therapy. Due to remission, progressive glucocorticoid withdrawal was started. Approximately six months after beginning the treatment and on a prednisone dose of 30 mg/day, the patient still complained from that pulsatile right temporo-occipital headache and began to experience reappearance of some skin lesions. During a new investigation, single lymphadenomegaly in the left submandibular region was observed and confirmed on computed tomography of the cervical region, which also revealed an expanding lesion in the base of the tongue. On videolaryngoscopy, a lesion was observed in the base of the tongue, to the right, passing over the midline. Biopsy was performed and epidermoid carcinoma of the tongue with cervical metastasis (T3N2M0) was diagnosed. The patient, then, underwent radiation therapy of the cervical region associated with chemotherapy. Seven months later, surgery for cervical lymph node removal was performed. The symptoms subsided, even after complete prednisone withdrawal.
DISCUSSION
The patient had a set of atypical manifestations, such as the findings of hypomyopathic DM, the vesiculobullous form of skin lesions, accompanied by two simultaneous tumors, which are not commonly associated with DM.
The hypo-/amyopathic form of DM can represent up to 20% of the cases of that disease, and, despite muscle weakness, normal levels of muscle enzymes can be observed,3 similarly to our case. The anti-CADM-140 antibody can be a marker of that form of DM.2
A high malignancy rate has been reported in patients with DM, about five to seven times greater than that of the gene ral population, behaving like a paraneoplastic syndrome. The link between DM and cancer might be related to the expression of autoantigens shared by the neoplastic and muscle tissues in some patients. A recently discovered antibody, the anti-155/140 or anti-p155 antibody, might be associated with the development of cancer.
Some possible risk factors for the association with neoplasias are as follows: leukocytoclastic vasculitis; presence of anti-p155/p140 or anti-p155 autoantibody;4 excessive elevation of muscle enzymes;5 male sex;6 vesiculobullous DM;7 and advanced age at the time of DM diagnosis. The last three were observed in our patient.
Adenocarcinomas of the cervix, lungs, ovaries, pancreas, urinary bladder, and stomach correspond to approximately 70% of the cancers associated with inflammatory myopathies. To our knowledge, only one case of paraneoplastic DM associated with tongue tumor has been reported in the literature.8 The occurrence of DM in patients with prostate cancer is very rare. One of the few cases was reported by a Spanish research group in 2008.9
The first choice treatment for DM consists in the administration of glucocorticoids (prednisone, 1 mg/kg/day) in addition to the treatment of the subjacent neoplasia, when present. The failure of steroids might be attributed to: 1) insufficient initial dose; 2) excessive reduction in the dose; 3) incorrect diagnosis; 4) associated malignancy; 5) concomitant myopathy caused by steroids; and 6) inclusion body myositis. In our patient, the relapse led us to discover a second tumor, and the presence of a certain symptom (headache) since the beginning, which improved after treating the tongue tumor, led us to consider synchronous tumors (prostate and tongue).
The cancer screening suggested by some authors in such patients should be annual up to two years after the diagnosis (except for ovary cancer that requires five years) and includes: complete anamnesis and physical exam; hemogram; ESR; biochemistry; urinalysis; fecal occult blood test; measuring CA125 (women), CA19.9, and PSA (men); mammography, transvaginal and pelvic ultrasound (women); colonoscopy; and chest, abdominal, and pelvic computed tomography.10
This routine is used in several services. However, the actual need for controlling neoplasias with that variety of complementary exams is still controversial, because, in certain countries, such as Brazil, adopting that routine seems unfeasible due to economic reasons and the non-availability of those exams in several services. Therefore, to provide an effective follow-up for a greater number of patients, we suggest that screening be conducted based on complete anamnesis and clinical exam, and complementary exams be asked according to clinical suspicion.
REFERENCES
-
1Bendewald MJ, Wetter DA, Li X, Davis MD. Incidence of dermatomyositis and clinically amyopatic dermatomyiositis: a population-based study in Olmsted County Minnesota. Arch Dermatol 2010;146(1):26-30.
-
2Miller ML. Clinical manifestations and diagnosis of adult dermatomyositis and polymyositis, Disponível em http://www.uptodate.com/online/content/search.do Acesso em 23 de fevereiro de 2010.
-
3Gerami P, Schope JM, McDonald L, Walling HW, Sontheimer RD. A systematic review of adult-onset clinically amyopathic dermatomyositis (dermatomyositis sine myositis): A missing link within the spectrum of the idiopathic inflammatory myopathies. J Am Acad Dermatol 2006;54:597-613.
-
4Kaji K, Fujimoto M, Hasegawa M, Kondo M, Saito Y, Komura K et al Identification of a novel autoantibody reactive with 155 and 140 kDa nuclear proteins in patients with dermatomyositis: an association with malignancy. Rheumatology (Oxford) 2007;46:25.
-
5Burnouf M, Mahé E, Verpillar P, Descamps V, Lebrun-Vignes B, Picard-Dahan C et al Cutaneous necrosis is predictive of cancer in adult dermatomyositis. Ann Dermatol Venerol 2003;130(3):313-6.
-
6Chen YJ, Wu CY, Shen JL. Predicting factors of malignancy in dermatomyositis and polymyositis:a case-control study. Br J Dermatol 2001;144(4):825-31.
-
7Zangrilli A, Papoutsaki M, Bianchi L, Teoli M, Chimenti S. Bullous dermatomyositis: a marker of poor prognosis and aggressive internal malignancy? Acta Derm Venereol 2008;88(4):393-4.
-
8Sugiyama T, Nakagawa T, Inui M, Tagawa T. Tongue carcinoma in young patient with dermatomyositis: a case report and review of the literature. J Oral Maxillofac Surg. 2001;59(8):925-8.
-
9Carmona O, Olivé M, Osuna T, de Pablo MJ. Paraneoplastic dermatomyositis associated with prostate cancer. Neurologia 2008;23(7):469-71.
-
10Miller M.L. Malignancy in dermatomyositis and polymyositis. Disponível em http://www.uptodate.com/online/content/search.do Acesso em 23 de fevereiro de 2010.
Paraneoplastic vesiculobullous dermatomyositis with synchronic prostate and tongue tumors: case report
Publication Dates
-
Publication in this collection
11 July 2011 -
Date of issue
Aug 2011
History
-
Received
18 May 2010 -
Accepted
30 Apr 2011