Abstracts
INTRODUCTION: Many studies have shown that resistance training has a positive effect on bone mineral density (BMD). However, few studies have compared the BMD of individuals undergoing resistance training and those training aquatic weight-bearing exercises. OBJECTIVE: To compare, in a cross-sectional study, the BMD of postmenopausal women undergoing resistance training and postmenopausal women training aquatic weight-bearing exercises. METHODS: The sample comprised 63 women divided into the following three groups: resistance training (STRENGTH: n = 15; 51.4 ± 2.7 years); aquatic weight-bearing exercises (WA-TER: n = 22; 54.5 ± 3.3 years); and non-trained controls (CONTROL: n = 26; 52.0 ± 3.3 years). All volunteers were on hormone replacement therapy for at least one year. The STRENGTH and WATER groups were training for at least one year prior to study beginning (mean years of training - STRENGTH: 4.5 ± 2.0; WATER: 4.2 ± 2.2). RESULTS: The STRENGTH group had higher BMD of total body, femoral neck, lumbar spine L2-L4 as compared with the CONTROL group (all P < 0.05). The WATER group had higher BMD of total body, total hip, lumbar spine L2-L4 as compared with the CONTROL group (all P < 0.05). However, no difference was observed between the STRENGTH and WATER groups regarding the sites assessed. CONCLUSIONS: Those findings suggest that not only the resistance training, but also aquatic weight-bearing exercises might be a non-pharmacological strategy to prevent BMD loss in postmenopausal women.
Strength training; Aquatic weight-bearing exercises; Bone density; Postmenopause
INTRODUÇÃO: Há um grande número de estudos mostrando que o treinamento de força tem um efeito positivo sobre a densidade mineral óssea (DMO). Porém, existem poucos estudos comparando a DMO entre praticantes de hidroginástica e treinamento de força. OBJETIVO: Comparar, em uma análise transversal, a DMO de mulheres praticantes de treinamento de força com mulheres praticantes de hidroginástica, na pós-menopausa. MÉTODOS: A amostra foi composta de 63 mulheres, divididas em três grupos: treinamento de força (FORÇA: n = 15; 51,4 ± 2,7 anos), hidroginástica (HIDRO: n = 22; 54,5 ± 3,3 anos) e controles não treinadas (CONTROLE: n = 26; 52,0 ± 3,3 anos). Todas as voluntárias estavam em terapia de reposição hormonal há no mínimo um ano. Os grupos FORÇA e HIDRO treinavam há pelo menos um ano antes do início do estudo (média de anos de treinamento - FORÇA: 4,5 ± 2,0; HIDRO: 4,2 ± 2,2). RESULTADOS: O grupo FORÇA apresentou maior DMO de corpo total, colo femoral e coluna lombar L2-L4 quando comparado ao grupo-controle (todos P < 0,05). O grupo HIDRO apresentou maior DMO no corpo total, quadril total e coluna lombar L2-L4 quando comparado ao grupo-controle (todos P < 0,05). Entretanto, não foram observadas diferenças entre os grupos FORÇA e HIDRO em nenhum dos sítios avaliados. CONCLUSÕES: Estes achados sugerem que não apenas o treinamento de força, mas também a hidroginástica podem ser estratégias não farmacológicas para prevenção da perda de DMO em mulheres na pós-menopausa.
Treinamento de força; Hidroginástica; Densidade óssea; Pós-menopausa
ORIGINAL ARTICLE
IPostgraduate Program in Medical Sciences, Medical School, Universidade de Brasília (UnB), Brasília, DF, Brazil
IIDepartment of Physical Education, Centro Universitário Euro-Americano (UNIEURO), Brasília, DF, Brazil
IIIResearch group of strength training and Health (GEPEEFS), Brasília, DF, Brazil
IVPostgraduate Program in Physical Education, School of Physical Education, Universidade Católica de Brasília (UCB), Brasília, DF, Brazil
VSchool of Physical Education, Universidade de Brasília (UnB), Brasília, DF, Brazil
VIDepartment of Medicine, Universidade Católica de Brasília (UCB), Brasília, DF, Brazil
VIIPostgraduate Program in Sciences for Health, Health Sciences Teaching and Research Foundation, Secretary of State of Health (FEPECS/SESDF), Ministry of Health, Brasilia, DF, Brazil
ABSTRACT
INTRODUCTION: Many studies have shown that resistance training has a positive effect on bone mineral density (BMD). However, few studies have compared the BMD of individuals undergoing resistance training and those training aquatic weight-bearing exercises.
OBJECTIVE: To compare, in a cross-sectional study, the BMD of postmenopausal women undergoing resistance training and postmenopausal women training aquatic weight-bearing exercises.
METHODS: The sample comprised 63 women divided into the following three groups: resistance training (STRENGTH: n = 15; 51.4 ± 2.7 years); aquatic weight-bearing exercises (WA-TER: n = 22; 54.5 ± 3.3 years); and non-trained controls (CONTROL: n = 26; 52.0 ± 3.3 years). All volunteers were on hormone replacement therapy for at least one year. The STRENGTH and WATER groups were training for at least one year prior to study beginning (mean years of training - STRENGTH: 4.5 ± 2.0; WATER: 4.2 ± 2.2).
RESULTS: The STRENGTH group had higher BMD of total body, femoral neck, lumbar spine L2-L4 as compared with the CONTROL group (all P < 0.05). The WATER group had higher BMD of total body, total hip, lumbar spine L2-L4 as compared with the CONTROL group (all P < 0.05). However, no difference was observed between the STRENGTH and WATER groups regarding the sites assessed.
CONCLUSIONS: Those findings suggest that not only the resistance training, but also aquatic weight-bearing exercises might be a non-pharmacological strategy to prevent BMD loss in postmenopausal women.
Keywords: Strength training, Aquatic weight-bearing exercises, Bone density, Postmenopause
Introduction
There is growing evidence that exercise contributes to the prevention and treatment of osteoporosis due to the osteogenic effect of mechanical stimulus on bone tissue.1-3 It has been suggested that activities that require heavy loading with few repetitions, resulting in high strain rates, may be optimal for increasing bone mineral density (BMD).4 Cross-sectional studies have shown that resistance-trained individuals showed more BMD than inactive5,6. Some experts recommendations,7 prospective8 or meta-analysis9 studies have shown increases or maintenance of BMD on those individuals.
On the other hand, water weight bearing exercises has been associated with improve in neuromuscular and functional fitness10 and cardiometabolic health,11 and also is highly recommended for old people with disability, because of security.10,12 Although, in the last 20 years, only a few studies have investigated BMD and water weight bearing exercises.13-16 Nevertheless, the literature is not clear whether there is an association between water weight bearing exercises and BMD. Most studies have yielded conflicting results ranging from worsening14 to improve bone health.15 Additionally, to date, no studies have compared, in a cross-sectional analysis, BMD in postmenopausal women resistance-trained versus postmenopausal women who are practicing aquatic weight bearing exercise, which is a novel approach.
The purpose of this study was to compare BMD in postmenopausal women resistance-trained with postmenopausal women aquatic-trained with weight bearing exercises, and both with untrained controls. It was hypothesized that postmenopausal women aquatic-trained with weight bearing exercises would have similar BMD as postmenopausal women resistance-trained, and they would have higher BMD than untrained controls.
Materials and methods
Subjects
The research project was approved by the Research Ethics Committee of the Universidade Católica de Brasília (UCB) according to the institutional policies and the Declaration of Helsinki.17 All the participants were from Brasília and were recruited by means of electronic mail and leaflets and posters distributed in the city of Brasília. During the study, a single blinded rheumatologist analyzed the medical records and conducted the structured interviews with 95 women. The volunteers were composed by three groups: resistance-trained (STRENGTH), aquatic-trained with weight bearing exercises (WATER) and untrained controls (CONTROL).
Inclusion criteria
All participants should be: a) at the minimum of one year in menopause; b) in exclusive estrogen hormone replacement therapy (HRT); c) into the STRENGTH and WATER groups required that the subject had been training at least one year before the study; d) into the CONTROL group the participants should not be engaged in regular physical activities programs for at least six months prior to the study. We used a questionnaire consisting of three questions to identify type of exercise, its regularity, frequency, intensity, and duration: 1) What type of exercise do you practice regularly during one week?; 2) How often do you do this exercise during one week?; and 3) Which is the average duration in minutes of a single session of physical exercises?
Exclusion criteria
All the participants with the following characteristics were excluded: a) using drugs or treatment that affects bone metabolism, except for calcium supplementation and HRT; b) smoking; c) with the body mass index (BMI) < 18 kg/m2 and > 30 kg/m2 (obesity); d) have any disease that affects the bone metabolism or strength (hypothyroidism/fibromyalgia/rheumatoid arthritis).
The resistance-trained and aquatic-trained with weight bearing exercises group
The STRENGTH group had traditional resistance training at least three nonconsecutive days per week with supervision with a physical education teacher, each session lasting approximately 60 minutes, and the program consisted in a zone of 10 to 15 repetitions each exercise (included leg press, knee extension, knee flexion, seated bench press, seated row/lat pull down, biceps curls and core exercise). The WATER group had classes through at least three nonconsecutive days per week (one hour each session) with a physical education teacher certified by the Aquatic Exercise Association (AEA). The goal was to reach a heart rate of 60%-80% of maximum during the session, being exercised the major muscle groups with movements of pushing and pulling, jumping and displacements. We could not control exactly how many training sessions the trained groups (STRENGTH/WATER) did in last year(s).
Procedures
Participants eligible for the study attended to the laboratory at the same time (8 am to 12 pm). Participants had to attend the following procedures prior to the laboratory visits: avoid practicing intense activities, caffeine use or alcohol derivatives 24 hours before the test, and have their last meal (including water) at least two hours before the test. All the tests were evaluated by a single blinded examiner.
Anthropometric measurements
For height, weight, BMI, individuals were asked to remove shoes and any weight that might interfere in the measurements. For measuring the height, the individual should be barefoot with heels and trunk against the wall, head in the Frankfurt plane. The subject's body weight in minimal clothing was measured to the nearest 100 g with a precision scale weight (Filizola ID-1500, Brazil), and height was measured to the nearest 5 mm with a wall-mounted stadiometer (Sanny Standard ES 2030, Brazil).
Bone densitometry
The BMD of the total body, lumbar spine L2-L4, femur neck, total hip and forearm - 33% radius, ultradistal radius, and total radius were measured using a dual-energy X-ray absorptiometry (DPX-L; Lunar Radiation Corporation, Madison, Wisconsin, U.S.A) and the scan were analyzed using software version 3.6. Before the tests, the devices were calibrated according to manufacturers recommendations and the same examiner performed all examinations.
Statistical analysis
Values are presented as mean and standard error. We used a model analysis of covariance (ANCOVA) by a factor, with the measure of BMD as the dependent variable and measures of age, total muscle mass, fat mass and body fat percentage as covariates. The Bonferroni correction was used to adjust the pre-specified comparisons and it was considered, in the analysis, a significance level of 5%. Coefficient of variation (CV) was used to calculate within-participant variation (CV% = [SD/mean] x 100). To identify the differences among groups of the percentage of voluntaries with osteoporosis, osteopenia and normal scores, according ISCD (2005), the Kruskal-Wallis test was applied using the Mann-Whitney test with Bonferroni correction, considering in this test a significance level of P < 0.012. Data were analyzed using SAS for Windows.
Results
Sample: Sixty-three healthy postmenopausal women were eligible for the study [32 excluded: hypothyroidism (n = 4); fibromyalgia (n = 3); BMI < 18 kg/m2 (n = 3) and > 30 kg/m2 (n = 14); smoking (n = 4); drugs or treatment that affects bone metabolism (n = 4). Fifteen in the STRENGTH group, 22 in the WATER group and 26 in the CONTROL group. Ninety percent of the STRENGTH and WATER group had been training regularly in the past year of the study in Young Men Christian Associations (YMCA).
Main characteristics of the three groups (STRENGTH; WATER; CONTROL) are presented in Table 1. There were no significant differences between groups for BMI, HRT (the dose of estrogen varied, e.g., 0.3-2.5 mg in all groups), and years of menopause. And the training time (years) of STRENGTH and WATER groups were not different (P > 0.05). However, the WATER group was older then the STRENGTH and CONTROL groups.
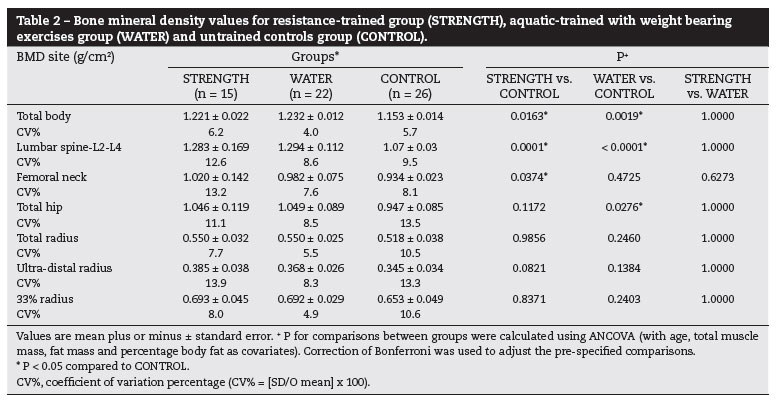
The results of dependent variable BMD in the STRENGTH group was significantly higher compared to the CONTROL in total body (5.73%), in the sites lumbar spine, L2-L4 (16.40%) and femoral neck (8.73%), all P < 0.05. However no significant difference was found in the other sites (total hip, total radius, ultra-distal radius and 33% radius). The WATER group also showed a significantly higher BMD compared to CONTROL group in total body (6.50%) and in the sites lumbar spine, L2-L4 (17.69%) and total hip (9.52%), all P < 0.05. However no significant difference was found in the other sites (femoral neck, total radius, ultra-distal radius and 33% radius) (Table 2).
The groups STRENGTH and WATER did not differ regarding the total body BMD and also in all the tested sites (lumbar spine L2-L4; femoral neck; total hip; total radius; ultra-distal radius; 33% radius) (P > 0.05) (Table 2).
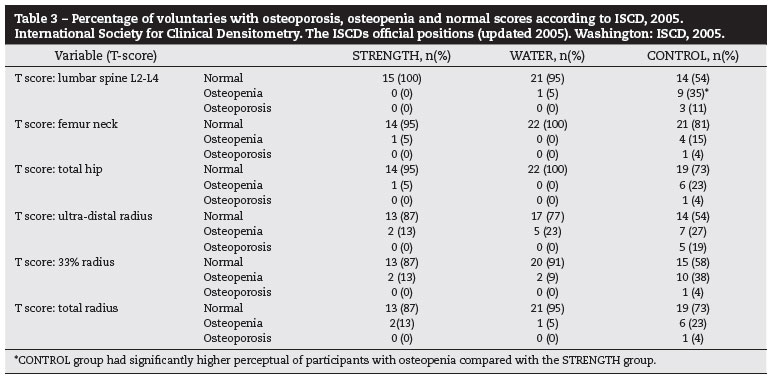
The number of participants with osteopenia in lumbar spine L2-L4 (T-score of BMD) was higher in the CONTROL group compared with the STRENGTH group (P < 0.05). For other variables, no significant difference was detected (all P > 0.05). More details of the percentage of voluntaries with osteoporosis, osteopenia and normal are presented in the Table 3.
Discussion
This study aimed to compare the DMO of postmenopausal women for at least one year, training for a period of at least one year, and in use of HRT therapy. We compare a STRENGTH group that were resistance-trained with WA-TER group that were weight-bearing-exercise-trained, and both with untrained controls. It was hypothesized that postmenopausal women aquatic-trained with weight bearing exercises would have similar BMD as postmenopausal women resistance-trained, and they would have higher BMD than untrained controls. Our hypotheses were confirmed data from no significant difference between WATER group and STRENGTH group in total body BMD and in any of the evaluated sites. Also the present study confirms the initial hypothesis that, compared to CONTROL group, WATER presented a higher BMD in lumbar spine L2-L4, total hip sites and in total body. Furthermore, the STRENGTH group presented higher BMD in lumbar spine L2-L4, femoral neck and total body compared with CONTROL group. Additionally the CONTROL group presented significant higher percentage of participants with osteopenia in lumbar spine L2-L4 T-score compared with the STRENGTH group.
The present study methodology exclusion criteria provide minimal bias and/or potential confounders aspects that could influence in the results of BMD, such as with all participants, were all postmenopausal, and physical characteristics such BMI, body composition, weight, height and clinical conditions, were all similar with HRT. Also, no participant was smoker or had concurrent disease that affects BMD. In addition the STRENGTH and the WATER group were for at least one year trained prior to the study. In addition our new approach revealed that those postmenopausal women who practiced aquatic weight-bearing exercises had similar BMD to that of women who did resistance-trained. The current study is unique in that it is not an intervention study. This is a relevant information because in a cross sectional analysis we can compare different sports and modalities. Moreover, osteogenic responses are associated with specific and intensity loading,4,8 but not with low intensity and/or short time of intervention.8 Previous studies with WATER exercise had investigated short time of intervention to bone modulation15 with low intensity14 and with osteopenic women;14 rather, we compare the total body BMD and BMD in different sites in postmenopausal women STRENGTH group with postmenopausal women WATER group, and both with a CONTROL group which was evaluated to data.
Some prospective studies had similar results when STRENGTH group was compared with CONTROL group in the total body BMD18 and in the sites total hip sites,7 femoral neck8 and also Kelley et al.9 meta-analysis in the spine L2-L4. Most of these studies involved high intensity protocols, what explains the efficiency of the stimulus on bone progenitor cells. It is possible that, in the present study, no significant difference was found between STRENGTH group and WATER group because both methods of training were sufficient positive to stimulate the BMD. Moreover, in radius sites our results were different of meta-analysis of Kelley et al.,9 although, similar of Bassey et al.19 It seems that this site requires a more intense stimulus to improve osteogenic responses.4
This is the first study to report that the WATER group had a higher total body BMD compared with the CONTROL group. Also, presented higher BMD in spine and total hip when compared with the CONTROL group. Our results are in agreement with those by Tsukahara et al.16 and Rotstein et al,.15 who demonstrated that the water group also had similar BMD in spine and total hip compared to the controls. Furthermore, Littrell and Snow (a published conference communication abstract) reported that in a short time study (six months) of aquatic training only preserved BMD in postmenopausal women in all sites, showing that this type of training was useful to maintain bone mass while BMD in the CONTROL group decreased.20
The results of this study agree with the experimental study of Bravo et al.,14 which showed no significant difference in femoral neck BMD of osteopenic women after one year of an aquatic physical activity similar to WATER. Additionally, Rotstein et al.15 found no significant difference in femoral neck BMD after only seven months of training in healthy postmenopausal women. It is important to remember that DXA provides a static measurement of BMD and, therefore, does not reflects metabolic activity. To this effect, Ay and Yurtkur13,21 studied bone anabolic (IGF-1 and calcitonin) and catabolic (parathormone, PTH) hormone activity and analyzed BMD using an ultrasound test in postmenopausal women after an aquatic training program. The results showed increased levels of calcitonin and IGF-1, improvement of the ultrasonography values and decrease of PTH in the experimental group while the opposite happened to the CONTROL group. Thus, it can be stated that aquatic training affects bone metabolism positively.
This is the primary study to analyze forearm radius on the WATER group compared with the CONTROL-group. These results suggest that this strategy of exercise provides little stimulus to the forearm region and perhaps wrist flexion, extension and hand grip exercises are not effective to improve BMD in these sites.
Regarding the BMD in all evaluated sites, there were no significant differences between STRENGTH group and WA-TER group. Recently, Tolomio et al.12 did not present significant differences in femoral neck among postmenopausal women with osteoporosis. The experimental protocol consisted of combined land and water exercise program. With resistance training and water weight bearing exercises, were performed combined in two sessions per week, for 11 months.
Most studies associate BMD with resistance exercise due to its specific and localized effect on body mass.4,5 However, in the present study, in spite of being significantly older than the STRENGTH group (three years), the evaluated sites did not present higher values in STRENGTH group in comparison to WATER group.
The present study has limitations. Its design was not experimental since researchers do not allocated the participants in groups. Participants had chosen to exercise (STRENGTH/WATER) or not and then were observed by the investigators. The intervention was not pre-defined by the researchers. Consider to include in limitations/pitfalls section the effect of previous physical activities, especially during the bone mass acquisition period (up to reach peak bone mass). In conclusion, the findings reported herein provide novel evidence that weight-bearing water exercise produces a strain stimulus for muscle development and provides continuous limb movement against water resistance. These results have important practical implications, suggesting that not only resistance training, but also weight-bearing water exercises could be a nonpharmacological strategy for prevention of BMD loss in postmenopausal women. This information is also important for professionals involved with healthcare and physical exercise, as water exercise is very popular in health centers and tends to pose little risk, but further research is required to provide supporting evidence for this exercise modality.
Conflicts of interest
The authors declare no conflicts of interest.
REFERENCES
-
1Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510-30.
-
2Pereira RM, Carvalho JF, Paula AP, Zerbini C, Domiciano DS, Gonçalves H, et al. Guidelines for the prevention and treatment of glucocorticoidinduced osteoporosis. Rev Bras Reumatol. 2012;52(4):580-93.
-
3Gualano B, Pinto AL, Perondi MB, Roschel H, Sallum AM, Hayashi AP, et al. Therapeutic effects of exercise training in patients with pediatric rheumatic diseases. Rev Bras Reumatol. 2011;51(5):490-6.
-
4Kerr D, Morton A, Dick I, Prince R. Exercise effects on bone mass in postmenopausal women are site-specific and loaddependent. J Bone Miner Res. 1996;11(2):218-25.
-
5Dinc H, Savci G, Demirci A, Sadikoglu MY, Tuncel E, Yavuz H. Quantitative computed tomography for measuring bone mineral density in athletes. Calcif Tissue Int. 1996;58(6):398-401.
-
6Karlsson MK, Johnell O, Obrant KJ. Bone mineral density in weight lifters. Calcif Tissue Int. 1993;52(3):212-15.
-
7Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094-105.
-
8Vincent KR, Braith RW. Resistance exercise and bone turnover in elderly men and women. Med Sci Sports Exerc. 2002;34(1):17-23.
-
9Kelley GA, Kelley KS, Tran ZV. Resistance training and bone mineral density in women: a meta-analysis of controlled trials. Am J Phys Med Rehabil. 2001;80(1):65-77.
-
10Tsourlou T, Benik A, Dipla K, Zafeiridis A, Kellis S. The effects of a twenty-four-week aquatic training program on muscular strength performance in healthy elderly women. J Strength Cond Res. 2006;20(4):811-18.
-
11Meredith-Jones K, Waters D, Legge M, Jones L. Upright waterbased exercise to improve cardiovascular and metabolic health: a qualitative review. Complement Ther Med. 2011;19(2):93-103.
-
12Tolomio S, Lalli A, Travain G, Zaccaria M. Effects of a combined weight-bearing and non-weight-bearing (warm water) exercise program on bone mass and quality in postmenopausal women with low bone-mineral density. Clin Ter. 2009;160(2):105-9.
-
13Ay A, Yurtkuran M. Evaluation of hormonal response and ultrasonic changes in the heel bone by aquatic exercise in sedentary postmenopausal women. Am J Phys Med Rehabil. 2003;82(12):942-9.
-
14Bravo G, Gauthier P, Roy PM, Payette H, Gaulin P. A weightbearing, water-based exercise program for osteopenic women: its impact on bone, functional fitness, and wellbeing. Arch Phys Med Rehabil. 1997;78(12):1375-80.
-
15Rotstein A, Harush M, Vaisman N. The effect of a water exercise program on bone density of postmenopausal women. J Sports Med Phys Fitness. 2008;48(3):352-59.
-
16Tsukahara N, Toda A, Goto J, Ezawa I. Cross-sectional and longitudinal studies on the effect of water exercise in controlling bone loss in Japanese postmenopausal women. J Nutr Sci Vitaminol (Tokyo). 1994;40(1):37-47.
-
17Gandevia B, Tovell A. Declaration of Helsinki. Med J Aust. 1964;2:320-1.
-
18Notelovitz M, Martin D, Tesar R, Khan FY, Probart C, Fields C, et al. Estrogen therapy and variable-resistance weight training increase bone mineral in surgically menopausal women. J Bone Miner Res. 1991;6(6):583-90.
-
19Bassey EJ, Ramsdale SJ. Weight-bearing exercise and ground reaction forces: a 12-month randomized controlled trial of effects on bone mineral density in healthy postmenopausal women. Bone. 1995;16(4):469-76.
-
20Littrell TR, Snow CM. Bone Density and Physical Function in Postmenopausal Women after a 12-month Water Exercise Intervention. Abstract conference of Med Sci Sports Exerc. 2004;5:289-90.
-
21Ay A, Yurtkuran M. Influence of aquatic and weightbearing exercises on quantitative ultrasound variables in postmenopausal women. Am J Phys Med Rehabil. 2005;84(1):52-61.
Resistance training versus weight-bearing aquatic exercise: a cross-sectional analysis of bone mineral density in postmenopausal women
Publication Dates
-
Publication in this collection
30 Oct 2015 -
Date of issue
Apr 2013
History
-
Received
07 Jan 2012 -
Accepted
13 Dec 2012