Abstract
We present a case of ocular syphilis after a renal transplantation involving progressive vision loss without clinically identifiable ocular disease. Electroretinography showed signs of ischemia, especially in the internal retina. A serological test was positive for syphilis. Lumbar puncture revealed lymphocytic meningitis and a positive serologic test for syphilis in the cerebrospinal fluid. The patient was treated with penicillin, and had a quick vision improvement. In the case of transplant recipients, clinicians should always consider the diagnosis of ocular syphilis in cases with unexplained visual acuity decrement, as this condition may cause serious complications if not treated.
Kidney transplant; Syphilis; Ocular syphilis
INTRODUCTION
The incidence of syphilis has increased in many countries over the last decade11. Pucch C, Gennai S, Pavese P, Pelloux I, Maurin M, Romanet JP, et al. Ocular manifestations of syphilis: recent cases over a 2.5 year period. Arch Clin Exp Ophthalmol. 2010;248:1623-9.
2. Doris JP, Saha K, Jones NP, Sukhthankar A. Ocular syphilis: the new epidemic. Eye(Lond). 2006;20:703-5.
3. Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433-41.-44. Centers for Disease Control and Prevention. Sexually transmitted diseases surveillance 2012. Atlanta: CDC; 2012.. In Australia, the reported number of syphilis cases has increased more than tenfold55. Read PJ, Donovan B. Clinical aspects of adult syphilis. Int Med J. 2012;42:614-20.. The same trend has been reported in developing countries66. Hook EW 3rd, Peeling RW. Syphilis control- a continuing challenge. N Engl J Med. 2004; 251:122-4.,77. Fernandes FR, Zanini PB, Rezende GR, Castro LS, Bandeira LM, Puga MA, et al.Syphilis infection, sexual practices and bisexual behaviour among men who have sex with men and transgender women: a cross sectional study. Sex transm Infect. 2015;91:42-9.. However, there are very few reported cases of syphilis in kidney transplantation88. Marty CL, Snow JL. Secondary syphilis in an immunocompromised kidney transplant recipient. Cutis. 2011;88:284-9.,99. Camarero-Temiño V, Mercado-Valdivia V, Izquierdo-Ortiz MJ, Santos-Barajas JJ, Hijazi-Prieto B, Sáez-Calero I, et al. Neurosyhilis in a renal transplant patient. Nefrologia. 2013; 33:277-9.. Although ocular syphilis is relatively rare; manifestations of syphilis belonging to secondary as well as tertiary/late stages have been described22. Doris JP, Saha K, Jones NP, Sukhthankar A. Ocular syphilis: the new epidemic. Eye(Lond). 2006;20:703-5.. There have been recent reports of an ocular syphilis outbreak in Sydney1010. Hughes EH, Guzowski M, Simunovic MP, Hunyor AP, McCluskey P. Syphilitic retinitis and uveitis in HIV-positive adults. Clin Experiment Ophthalmol. 2010;38:851-6., in HIV-positive cases11. Pucch C, Gennai S, Pavese P, Pelloux I, Maurin M, Romanet JP, et al. Ocular manifestations of syphilis: recent cases over a 2.5 year period. Arch Clin Exp Ophthalmol. 2010;248:1623-9.,22. Doris JP, Saha K, Jones NP, Sukhthankar A. Ocular syphilis: the new epidemic. Eye(Lond). 2006;20:703-5.,1010. Hughes EH, Guzowski M, Simunovic MP, Hunyor AP, McCluskey P. Syphilitic retinitis and uveitis in HIV-positive adults. Clin Experiment Ophthalmol. 2010;38:851-6.
11. Mathew RG, Goh BT, Westcott MC. British ocular syphilis study (BOSS): a 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014;55:5394-400.
12. Fonollosa A, Martinez-Indart L, Artaraz J, Martinez-Berriotxa A, Agirrebengoa K, Garcia M, et al. Clinical manifestations and outcome sofsyphilis-associated uveitis in northern Spain. Ocul Immunol Inflamm. 2014. doi:10.3109/09273948.2014.943349.
https://doi.org/10.3109/09273948.2014.94...
13. Nguyen A, Berngard SC, Lopez JP, Jenkins TC. A case of ocular syphilis in a 36-year-old HIV-positive male. Case Rep Infect Dis. 2014;2014/352047.
14. Moradi A, Salek S, Daniel E, Gangaputra S, Ostheimer TA, Burkholder BM, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159:334-43.-1515. Anshu A, Cheng CL, Chee SP. Syphilitic uveitis: an Asian perspective. Br J Ophthalmol. 2008;92:594-7.. To the best of our knowledge, there are no previous reports of ocular syphilis in renal transplant recipients. There is no typical clinical presentation of ocular syphilis, and it may evolve as an optic neuritis, anterior uveitis, vitritis, nodular scleritis1616. Shaikh SI, Biswas J, Rishi P. Nodular syphilitic scleritis masquerading as an ocular tumor. J Ophthalmic Inflamm Infect. 2015;5:8., chorioretinitis, or vasculitis, and serous retinal detachment, often resulting in late diagnosis and clinical complications. Ocular manifestations of syphilis respond readily to treatment when identified early enough, preventing scaring or permanent damage, such as retinal detachment1010. Hughes EH, Guzowski M, Simunovic MP, Hunyor AP, McCluskey P. Syphilitic retinitis and uveitis in HIV-positive adults. Clin Experiment Ophthalmol. 2010;38:851-6.,1717. Gaudio PA. Update on ocular syphilis.Curr Opin Ophthalmol. 2006;17:562-6.,1818. Balaskas K, Sergentanis TN, Giuleri S, Guex-Crosier Y. Analysis of significant factors influencing visual acuity in ocular syphilis. Br J Ophthalmol. 2011;95:1568-72.. This case report describes the clinical features of a kidney transplant recipient who presented confirmed ocular and neuro-syphilis.
CASE REPORT
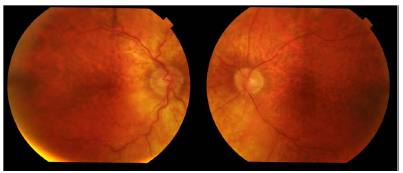
A 44-year-old Caucasian female with branchio-oto-renal (BOR) syndrome1919. Morisada N, Nozu K, IIjima K. Branchio-oto-renal syndrome: comprehensive review based on nationwide surveillance in Japan. Pediatr Int. 2014;56:309-14., who received a renal transplant from a deceased donor 20 years ago, came to the outpatient clinic complaining of bilateral progressive vision loss over the past 11 months (worse in her right eye, and at night), associated to central scotoma, without improvement when her lens prescription was updated. She did not report any other ocular symptoms such as pain or epiphora. Her visual acuity was 20/50 (right eye) and 20/80 (left eye). Slit lamp examination revealed corneal scars (sequelae from a refractive surgery) as well as diffuse and mild corneal opacities in both eyes. The fundoscopy showed a diffuse rarefaction of the retinal pigment epithelium, compatible with high myopia (Fig. 1). There were no signs of intraocular inflammation or infection on clinical examination. At this point, her visual acuity decreased to 20/400 (right eye) and 20/200 (left eye) without any clinically identifiable ocular disease. Electroretinography showed signs of ischemia, especially in the internal retina (Fig. 2A). Her current immunosuppressive treatment was tacrolimus, azathioprine and prednisone. In the individual patient history, she reported a refractive surgery to correct the high degree of myopia in both eyes 20 years ago, and also previous unprotected sex.
Right (A) and left (B), retinal fundus images showing rarefaction of the retinal pigment epithelium, but no signs of retinal vasculitis or lesions that could be indicative of syphilitic uveitis. 173 x 75 mm (150 x 150 DPI).
Electroretinogram (left eye, scotopic) before medical treatment (A), showing impairment of inner retinal layers, potentially attributed to retinal ischemia (B). Electroretinogram (left eye, scotopic) 12 months after medical treatment, showing an augmented B wave amplitude, suggesting improvement of retinal function. 187 x 114 mm (96 x 96 DPI).
A VDRL (Venereal Disease Research Laboratory) test was ordered and the titer was 1: 2,048 and a positive treponemal test (fluorescent treponemal antibody absorption - FTA/ABS) was noted. The patient was admitted to the hospital for further tests and treatment. On the physical examination, she was in good health and had a discreet maculopapular erythematous rash on both palms, which spread to thoracic areas. She had no detected lesions in the genital region, abdominal masses, lymph node enlargements or branchial cleft cysts, neurologic deficits, or cardiovascular abnormalities. At admission, her blood creatinine was 1.5 g/dL. A confirmatory VDRL titer showed 1:512 and the FTA/ABS was positive. Others tests for HIV, hepatitis B and C were negative. Computed tomography of the brain was normal. The cerebrospinal fluid (CSF) showed a lymphocytic pleocytosis with the presence of 66.3 cells/ µL (100% lymphocytes), normal glucose and protein. VDRL was positive, but the titer decreased to 1/4 of the initial values and Cryptococcus antigens were negative. After the diagnosis of neuro-syphilis associated to retinopathy (bilateral vision loss associated to abnormalities seen at the electroretinography), the patient was treated with penicillin G (24 million IU/day) for 14 days. A few days after the penicillin was initiated, the patient reported a partial improvement of her visual acuity, although fundoscopy and electroretinography showed no differences in relation to the initial values. Four months after treatment, there was a partial improvement of the electroretinographic parameters (Fig. 2B), and in her last evaluation performed 6 months after treatment, she was asymptomatic, with a visual acuity of 20/40 in her right eye and 20/30 in her left eye. The VDRL titer was 1: 256.
DISCUSSION
The branchio-oto-renal (BOR) syndrome is a genetic condition that affects about 1 in 40,000 people, causing abnormalities of the kidney structure and function, in some cases leading to end-stage renal disease later in life1919. Morisada N, Nozu K, IIjima K. Branchio-oto-renal syndrome: comprehensive review based on nationwide surveillance in Japan. Pediatr Int. 2014;56:309-14..
Ocular syphilis has a low incidence in syphilis patients, but may be present in all stages of the disease1111. Mathew RG, Goh BT, Westcott MC. British ocular syphilis study (BOSS): a 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014;55:5394-400.. In the present case report, the disease stage was characterized as secondary syphilis based on skin lesions and high VDRL titers. Ocular syphilis, as well as syphilis itself, may affect all ocular structures, causing interstitial keratitis, retinitis, retinal vasculitis, and uveitis. The most common ocular manifestation of secondary syphilis is uveitis22. Doris JP, Saha K, Jones NP, Sukhthankar A. Ocular syphilis: the new epidemic. Eye(Lond). 2006;20:703-5.,33. Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433-41.. In this case, the only ocular manifestation observed was an abnormal ERG that was partially resolved by systemic treatment. Ocular syphilis signs could have been masked by the patient's significant corneal scaring resulting from the previous myopia surgery, and the altered fundoscopy due the high degree of myopia. The ERG suggested chronic ischemic retinitis that could not be attributed to the high myopia, and no clinically detectable inflammation was found. Ocular syphilis should always prompt an analysis of the CSF to exclude associated neuro-syphilis44. Centers for Disease Control and Prevention. Sexually transmitted diseases surveillance 2012. Atlanta: CDC; 2012.. The patient in the present report was immune compromised due to a kidney transplantation and the use of immune suppressive drugs, and lumbar puncture revealed lymphocytic pleocytosis with positive VRDL confirming the diagnosis of neuro-syphilis2020. Marra CM, Maxwell CL, Smith SL, Lukehart SA, Rompalo AM, Eaton M, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004;189:369-76..There are consistent recommendations to treat all the ocular syphilis cases as neuro-syphilis22. Doris JP, Saha K, Jones NP, Sukhthankar A. Ocular syphilis: the new epidemic. Eye(Lond). 2006;20:703-5.,33. Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433-41.,1212. Fonollosa A, Martinez-Indart L, Artaraz J, Martinez-Berriotxa A, Agirrebengoa K, Garcia M, et al. Clinical manifestations and outcome sofsyphilis-associated uveitis in northern Spain. Ocul Immunol Inflamm. 2014. doi:10.3109/09273948.2014.943349.
https://doi.org/10.3109/09273948.2014.94...
,1313. Nguyen A, Berngard SC, Lopez JP, Jenkins TC. A case of ocular syphilis in a 36-year-old HIV-positive male. Case Rep Infect Dis. 2014;2014/352047., using high doses of intravenous penicillin33. Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433-41.,55. Read PJ, Donovan B. Clinical aspects of adult syphilis. Int Med J. 2012;42:614-20.,1313. Nguyen A, Berngard SC, Lopez JP, Jenkins TC. A case of ocular syphilis in a 36-year-old HIV-positive male. Case Rep Infect Dis. 2014;2014/352047.. The outcomes are usually good with quick and significant improvement, during the first 7 days, of the visual acuity, as observed in this case.
Despite the low incidence of ocular syphilis, it is critical to consider this possibility as a differential diagnosis, and test the patients with ocular complaints. In addition, VDRL is an accessible and low cost test. Most patients achieve excellent visual acuities after treatment11. Pucch C, Gennai S, Pavese P, Pelloux I, Maurin M, Romanet JP, et al. Ocular manifestations of syphilis: recent cases over a 2.5 year period. Arch Clin Exp Ophthalmol. 2010;248:1623-9.,1111. Mathew RG, Goh BT, Westcott MC. British ocular syphilis study (BOSS): a 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014;55:5394-400.,1414. Moradi A, Salek S, Daniel E, Gangaputra S, Ostheimer TA, Burkholder BM, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159:334-43., however, when not treated, syphilis may result in serious complications. Although ocular syphilis has been reported in association with HIV infection, transplant teams should suspect this diagnosis in patients with an unexplained visual acuity decrease, even without clinically detected ocular inflammation.
REFERENCES
-
1Pucch C, Gennai S, Pavese P, Pelloux I, Maurin M, Romanet JP, et al. Ocular manifestations of syphilis: recent cases over a 2.5 year period. Arch Clin Exp Ophthalmol. 2010;248:1623-9.
-
2Doris JP, Saha K, Jones NP, Sukhthankar A. Ocular syphilis: the new epidemic. Eye(Lond). 2006;20:703-5.
-
3Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433-41.
-
4Centers for Disease Control and Prevention. Sexually transmitted diseases surveillance 2012. Atlanta: CDC; 2012.
-
5Read PJ, Donovan B. Clinical aspects of adult syphilis. Int Med J. 2012;42:614-20.
-
6Hook EW 3rd, Peeling RW. Syphilis control- a continuing challenge. N Engl J Med. 2004; 251:122-4.
-
7Fernandes FR, Zanini PB, Rezende GR, Castro LS, Bandeira LM, Puga MA, et al.Syphilis infection, sexual practices and bisexual behaviour among men who have sex with men and transgender women: a cross sectional study. Sex transm Infect. 2015;91:42-9.
-
8Marty CL, Snow JL. Secondary syphilis in an immunocompromised kidney transplant recipient. Cutis. 2011;88:284-9.
-
9Camarero-Temiño V, Mercado-Valdivia V, Izquierdo-Ortiz MJ, Santos-Barajas JJ, Hijazi-Prieto B, Sáez-Calero I, et al. Neurosyhilis in a renal transplant patient. Nefrologia. 2013; 33:277-9.
-
10Hughes EH, Guzowski M, Simunovic MP, Hunyor AP, McCluskey P. Syphilitic retinitis and uveitis in HIV-positive adults. Clin Experiment Ophthalmol. 2010;38:851-6.
-
11Mathew RG, Goh BT, Westcott MC. British ocular syphilis study (BOSS): a 2-year national surveillance study of intraocular inflammation secondary to ocular syphilis. Invest Ophthalmol Vis Sci. 2014;55:5394-400.
-
12Fonollosa A, Martinez-Indart L, Artaraz J, Martinez-Berriotxa A, Agirrebengoa K, Garcia M, et al. Clinical manifestations and outcome sofsyphilis-associated uveitis in northern Spain. Ocul Immunol Inflamm. 2014. doi:10.3109/09273948.2014.943349.
» https://doi.org/10.3109/09273948.2014.943349 -
13Nguyen A, Berngard SC, Lopez JP, Jenkins TC. A case of ocular syphilis in a 36-year-old HIV-positive male. Case Rep Infect Dis. 2014;2014/352047.
-
14Moradi A, Salek S, Daniel E, Gangaputra S, Ostheimer TA, Burkholder BM, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159:334-43.
-
15Anshu A, Cheng CL, Chee SP. Syphilitic uveitis: an Asian perspective. Br J Ophthalmol. 2008;92:594-7.
-
16Shaikh SI, Biswas J, Rishi P. Nodular syphilitic scleritis masquerading as an ocular tumor. J Ophthalmic Inflamm Infect. 2015;5:8.
-
17Gaudio PA. Update on ocular syphilis.Curr Opin Ophthalmol. 2006;17:562-6.
-
18Balaskas K, Sergentanis TN, Giuleri S, Guex-Crosier Y. Analysis of significant factors influencing visual acuity in ocular syphilis. Br J Ophthalmol. 2011;95:1568-72.
-
19Morisada N, Nozu K, IIjima K. Branchio-oto-renal syndrome: comprehensive review based on nationwide surveillance in Japan. Pediatr Int. 2014;56:309-14.
-
20Marra CM, Maxwell CL, Smith SL, Lukehart SA, Rompalo AM, Eaton M, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004;189:369-76.
Publication Dates
-
Publication in this collection
2016
History
-
Received
30 Aug 2015 -
Accepted
18 Nov 2015