Abstracts
CONTEXT AND OBJECTIVE: Transcranial Doppler (TCD) detects stroke risk among children with sickle cell anemia (SCA). Our aim was to evaluate TCD findings in patients with different sickle cell disease (SCD) genotypes and correlate the time-averaged maximum mean (TAMM) velocity with hematological characteristics. DESIGN AND SETTING: Cross-sectional analytical study in the Pediatric Hematology sector, Universidade Federal de São Paulo. METHODS: 85 SCD patients of both sexes, aged 2-18 years, were evaluated, divided into: group I (62 patients with SCA/Sß0 thalassemia); and group II (23 patients with SC hemoglobinopathy/Sß+ thalassemia). TCD was performed and reviewed by a single investigator using Doppler ultrasonography with a 2 MHz transducer, in accordance with the Stroke Prevention Trial in Sickle Cell Anemia (STOP) protocol. The hematological parameters evaluated were: hematocrit, hemoglobin, reticulocytes, leukocytes, platelets and fetal hemoglobin. Univariate analysis was performed and Pearson's coefficient was calculated for hematological parameters and TAMM velocities (P < 0.05). RESULTS: TAMM velocities were 137 ± 28 and 103 ± 19 cm/s in groups I and II, respectively, and correlated negatively with hematocrit and hemoglobin in group I. There was one abnormal result (1.6%) and five conditional results (8.1%) in group I. All results were normal in group II. Middle cerebral arteries were the only vessels affected. CONCLUSION: There was a low prevalence of abnormal Doppler results in patients with sickle-cell disease. Time-average maximum mean velocity was significantly different between the genotypes and correlated with hematological characteristics.
Ultrasonography, Doppler, transcranial; Anemia, sickle cell; Hemoglobin SC disease; Stroke; Child; Adolescent
CONTEXTO E OBJETIVO: Doppler transcraniano (DTC) detecta risco de acidente vascular cerebral (AVC) em crianças com anemia falciforme (AF). O objetivo foi avaliar os resultados ao DTC nos diferentes genótipos da doença falciforme (DF) e correlacionar a velocidade média-máxima (VMMáx) às características hematológicas. TIPO DE ESTUDO E LOCAL: Estudo transversal analítico realizado no setor de Hematopediatria da Universidade Federal de São Paulo. MÉTODOS: 85 pacientes com DF, 2-18 anos, ambos os sexos, foram avaliados e divididos em: grupo I (62 com AF ou Sß0 talassemia); e grupo II (23 com hemoglobinopatia SC ou Sß+ talassemia). DTC foi realizado e revisado por um único investigador usando um aparelho de ultrassonografia Doppler com transdutor de 2MHz, conforme critérios do protocolo STOP (Stroke Prevention Trial in Sickle Cell Anemia). As variáveis hematológicas avaliadas foram: hematócrito, hemoglobina, reticulócitos, leucócitos, plaquetas, hemoglobina fetal. Análise univariada e coeficiente de Pearson calculados para parâmetros hematológicos e VMMáx, P < 0,05. RESULTADOS: As média das VMMáx foram de 137 ± 28 cm/s e 103 ± 19 cm/s nos grupos I e II, respectivamente. Houve correlação negativa da VMMáx com hematócrito e hemoglobina no grupo I. Houve um (1,6%) resultado anormal e 5 (8,1%) condicionais no grupo I; no grupo II, todos estavam normais. Artérias cerebrais médias foram as únicas acometidas. CONCLUSÃO: Houve baixa prevalência de resultados anormais ao DTC em pacientes com DF. A VMMáx foi significativamente diferente entre os genótipos da DF e apresentou correlação com variáveis hematológicas.
Ultrassonografia Doppler transcraniana; Anemia falciforme; Doença da hemoglobina SC; Acidente cerebral vascular; Criança; Adolescente
ORIGINAL ARTICLE
Results from transcranial Doppler examination on children and adolescents with sickle cell disease and correlation between the time-averaged maximum mean velocity and hematological characteristics: a cross-sectional analytical study
Resultados do estudo do Doppler transcraniano em crianças e adolescentes portadores de doença falciforme e correlação entre a velocidade média máxima e características hematológicas: um estudo transversal analítico
Mary HokazonoI; Gisele Sampaio SilvaII; Edina Mariko Koga SilvaIII; Josefina Aparecida Pellegrini BragaIV
IMD, MSc. Pediatrician, Department of Pediatrics, Universidade Federal de São Paulo (Unifesp), São Paulo, Brazil
IIMD, PhD. Neurologist, Department of Neurology, Universidade Federal de São Paulo (Unifesp), São Paulo, Brazil
IIIMD, PhD. Adjunct Professor of Evidence-Based Medicine and Emergency Medicine, Universidade Federal de São Paulo (Unifesp), São Paulo, Brazil
IVMD, PhD. Adjunct Professor, Discipline of Pediatric Specialties, Division of Pediatric Hematology, Department of Pediatrics, Universidade Federal de São Paulo (Unifesp), São Paulo, Brazil
Address for correspondence Address for correspondence: Mary Hokazono Rua Diogo de Faria, 307 São Paulo (SP) - Brasil CEP 04037-000 Tel. (+55 11) 5539-1093 E-mail: mhoka@ig.com.br
ABSTRACT
CONTEXT AND OBJECTIVE: Transcranial Doppler (TCD) detects stroke risk among children with sickle cell anemia (SCA). Our aim was to evaluate TCD findings in patients with different sickle cell disease (SCD) genotypes and correlate the time-averaged maximum mean (TAMM) velocity with hematological characteristics.
DESIGN AND SETTING: Cross-sectional analytical study in the Pediatric Hematology sector, Universidade Federal de São Paulo.
METHODS: 85 SCD patients of both sexes, aged 2-18 years, were evaluated, divided into: group I (62 patients with SCA/Sß0 thalassemia); and group II (23 patients with SC hemoglobinopathy/Sß+ thalassemia). TCD was performed and reviewed by a single investigator using Doppler ultrasonography with a 2 MHz transducer, in accordance with the Stroke Prevention Trial in Sickle Cell Anemia (STOP) protocol. The hematological parameters evaluated were: hematocrit, hemoglobin, reticulocytes, leukocytes, platelets and fetal hemoglobin. Univariate analysis was performed and Pearson's coefficient was calculated for hematological parameters and TAMM velocities (P < 0.05).
RESULTS: TAMM velocities were 137 ± 28 and 103 ± 19 cm/s in groups I and II, respectively, and correlated negatively with hematocrit and hemoglobin in group I. There was one abnormal result (1.6%) and five conditional results (8.1%) in group I. All results were normal in group II. Middle cerebral arteries were the only vessels affected.
CONCLUSION: There was a low prevalence of abnormal Doppler results in patients with sickle-cell disease. Time-average maximum mean velocity was significantly different between the genotypes and correlated with hematological characteristics.
Key words: Ultrasonography, Doppler, transcranial. Anemia, sickle cell. Hemoglobin SC disease. Stroke. Child. Adolescent.
RESUMO
CONTEXTO E OBJETIVO: Doppler transcraniano (DTC) detecta risco de acidente vascular cerebral (AVC) em crianças com anemia falciforme (AF). O objetivo foi avaliar os resultados ao DTC nos diferentes genótipos da doença falciforme (DF) e correlacionar a velocidade média-máxima (VMMáx) às características hematológicas.
TIPO DE ESTUDO E LOCAL: Estudo transversal analítico realizado no setor de Hematopediatria da Universidade Federal de São Paulo.
MÉTODOS: 85 pacientes com DF, 2-18 anos, ambos os sexos, foram avaliados e divididos em: grupo I (62 com AF ou Sß0 talassemia); e grupo II (23 com hemoglobinopatia SC ou Sß+ talassemia). DTC foi realizado e revisado por um único investigador usando um aparelho de ultrassonografia Doppler com transdutor de 2MHz, conforme critérios do protocolo STOP (Stroke Prevention Trial in Sickle Cell Anemia). As variáveis hematológicas avaliadas foram: hematócrito, hemoglobina, reticulócitos, leucócitos, plaquetas, hemoglobina fetal. Análise univariada e coeficiente de Pearson calculados para parâmetros hematológicos e VMMáx, P < 0,05.
RESULTADOS: As média das VMMáx foram de 137 ± 28 cm/s e 103 ± 19 cm/s nos grupos I e II, respectivamente. Houve correlação negativa da VMMáx com hematócrito e hemoglobina no grupo I. Houve um (1,6%) resultado anormal e 5 (8,1%) condicionais no grupo I; no grupo II, todos estavam normais. Artérias cerebrais médias foram as únicas acometidas.
CONCLUSÃO: Houve baixa prevalência de resultados anormais ao DTC em pacientes com DF. A VMMáx foi significativamente diferente entre os genótipos da DF e apresentou correlação com variáveis hematológicas.
Palavras-chaves: Ultrassonografia Doppler transcraniana. Anemia falciforme. Doença da hemoglobina SC. Acidente cerebral vascular. Criança. Adolescente.
INTRODUCTION
Sickle cell disease is a hemoglobinopathy characterized by the presence of more than 50% hemoglobin S on hemoglobin electrophoresis. The homozygote SS form is known as sickle cell anemia. Hemoglobin S can occur in association with other anomalous types of hemoglobin, and among these are hemoglobin C and thalassemia beta, thus forming different genotypes of sickle cell disease: hemoglobin SC disease and S-beta thalassemia.1
It has been estimated that more than seven million people have hemoglobin S in Brazil, and that more than 25,000 to 30,000 people have the homozygote form, with more than 3,500 new cases born every year.1,2
In the S-beta globin gene, a normal codon (GAG) is replaced by another (GTG), thus resulting in exchanging the sixth amino acid of the beta globin. This exchange of glutamic acid for valine causes polymerization of hemoglobin S, when exposed to media with low oxygen tension, which leads to sickling of red blood cells. This vaso-occlusive process is responsible for most of the clinical manifestations of sickle cell disease.3,4
Stroke is one of the most feared clinical complications from this disease because of its high morbidity-mortality.5 In children and adolescents, the most common form is ischemic stroke, and around 5-10% of patients with sickle cell anemia present stroke by the age of 20 years.3,5,6 The physiopathology of ischemic stroke differs from the mechanisms of the other complications of the disease. In autopsy studies, arteriography and other diagnostic methods, it has been observed that ischemic stroke in cases of sickle cell anemia is caused by hypertrophy of the intimal layer of the intracranial arteries, with proliferation of fibroblasts and smooth muscle of blood vessels.3,7,8 Transcranial Doppler enables early detection of arterial abnormalities in individuals with sickle cell anemia, which is extremely important for instituting primary prevention.9-14
The normal blood flow velocities obtained through transcranial Doppler are influenced by several factors, of which the main three determinants are the difference in pressure gradient along the vessel, the vessel length and cross-sectional area (caliber) and the blood viscosity. The hematocrit level and leukocyte and platelet counts influence blood viscosity and thus may have a bearing on blood flow velocity.15-20
Adams et al. conducted several studies using transcranial Doppler among individuals with sickle cell anemia to demonstrate the usefulness of this examination for evaluating stroke risk. They defined normal blood flow velocity as values of up to 170 cm/s, intermediate values as 170 to 200 cm/s and values greater than 200 cm/s as critical, with a high risk of developing stroke.8,18,19,21 Among these patients, if they had abnormal results from two Doppler examinations, they received a transfusion for primary stroke prevention.9 Blood transfusion was used because it is highly effective in reducing the risk of recurrence stroke in sickle cell anemia.7
The clinical picture of sickle cell disease is very variable, and hematocrit levels, leukocyte counts and hemoglobin S and fetal hemoglobin percentages correlate with the clinical severity of these patients' conditions.22 In this light, and given that these parameters have been little studied in relation to other genotypes of sickle cell disease, our aim in this study was to evaluate the results from transcranial Doppler among patients with sickle cell disease who were being followed at the Pediatric Hematology Outpatient Clinic of Universidade Federal de São Paulo (Unifesp), correlating the time-averaged maximum mean velocity obtained through transcranial Doppler with the different genotypes of sickle cell disease and the hematological characteristics.
OBJECTIVE
To evaluate the results from transcranial Doppler among patients with sickle cell disease and correlate the time-averaged maximum mean velocity obtained through transcranial Doppler with the different genotypes of sickle cell disease and the hematological characteristics.
METHODS
This was a single-center cross-sectional study on all patients with sickle cell disease between the ages of 2 and 18 years who came to the Pediatric Hematology Outpatient Clinic of Unifesp in 2004 and 2005.
The inclusion criteria were that the patients needed to have no previous clinical diagnosis of stroke and no acute crises.
Patients were excluded if they did not cooperate with transcranial Doppler examination, if they did not agree to undergo the examination, if they were using hydroxyurea or if they had received red blood cell transfusions over the preceding three months.
This study was approved by the Research Ethics Committee of Unifesp (no. 149/03). An informed consent statement was obtained from all the adults responsible for the patients participating in the study.
All the transcranial Doppler examinations were performed by the same professional, who had been trained to perform transcranial Doppler (Silva GS), using the Nicolet EME-Companion TC2000 apparatus with a 2 MHz transducer and following the criteria of the STOP (Stroke Prevention Trial in Sickle Cell Anemia) study.9 From this examination, the time-averaged maximum mean velocities were determined every 2 mm along the following arteries: bilateral internal carotid arteries, bilateral anterior cerebral arteries, anterior-middle cerebral artery bifurcations, middle cerebral arteries, bilateral posterior cerebral arteries, bilateral vertebral arteries and basilar artery. The highest value from the right or left middle cerebral arteries, bilateral internal carotid arteries or anterior-middle cerebral artery bifurcations was taken as the time-averaged maximum mean velocity for each patient and was used in the data analysis. When the time-averaged maximum mean velocity result was conditional or abnormal, the examinations were repeated until two consecutive abnormal results were obtained.
The blood tests performed were total hemoglobin and hematocrit assays; leukocyte and platelet counts, performed in an electronic counter (Coulter model Ssr or Coulter model T-890); hemoglobin S assay by means of hemoglobin electrophoresis on cellulose acetate with tris-EDTA-borate buffer (pH 8.6); and fetal hemoglobin assay, quantified by means of alkaline denaturation.
The patients were divided into two groups, in accordance with the clinical and hematological differences already recognized in the literature. One group was composed of patients with the homozygote form and Sβ0 thalassemia (group I), and the other was composed of patients with SC hemoglobinopathy and Sβ+ thalassemia (group II).
The results were described through calculations of means and standard deviations for variables with normal distribution. Hematological parameters predictive of time-averaged maximum mean velocities were investigated by means of univariate analysis. Pearson's coefficient was calculated to evaluate correlations between the time-averaged maximum mean velocity and the hemoglobin S percentage, fetal hemoglobin percentage, hemoglobin level, hematocrit percentage, platelet count, leukocyte count and reticulocyte percentage. The Statistical Package for the Social Sciences (SPSS) 10.0 software (SPSS Inc., Chicago, United States) was used for the statistical analyses. P values < 0.05 were taken to be statistically significant.
RESULTS
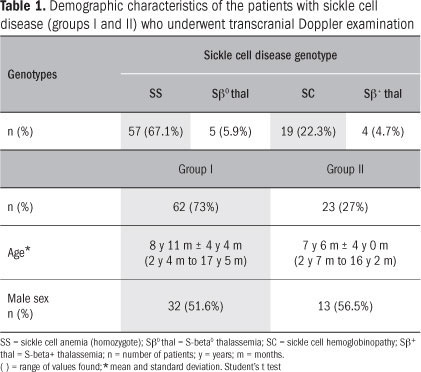
By the end of the study period, 85 patients with sickle cell disease had been evaluated. Group I was composed of 62 patients and group II was composed of 23 patients (Table 1). There were no statistically significant differences between the groups with regard to age and sex.
We observed statistically significant differences between the two groups for all the hematological parameters (Table 2).
Group I presented a negative correlation between the time-averaged maximum mean velocity and the hematocrit percentage and between the time-averaged maximum mean velocity and the hemoglobin level. Group II presented a positive correlation between the time-averaged maximum mean velocity and the reticulocyte count and a negative correlation between the time-averaged maximum mean velocity and the fetal hemoglobin percentage (Table 3).
Only one patient in group I presented an abnormal velocity (1.6%). This patient with abnormal velocity had a conditional result (190 cm/s) in the first transcranial Doppler that was performed and, in the repetitions, presented abnormal velocity in two consecutive examinations (time-averaged maximum mean velocities of 220 cm/s and 240 cm/s). Five patients (8.1%) in group I presented conditional time-averaged maximum mean velocities (Table 4).
It was observed that the arteries affected in these patients were the right or left middle cerebral artery in all the cases, both in the patient with abnormal and in the patients with conditional time-averaged maximum mean velocities.
DISCUSSION
The use of transcranial Doppler has become an important tool for stroke prevention among patients with sickle cell anemia. Stroke occurs four times more often among sickle cell anemia patients than among patients with SC hemoglobinopathy or Sβ thalassemia.5
In the STOP study, which was carried out in 1998 and is the biggest study on transcranial Doppler in relation to patients with sickle cell anemia within the pediatric age group, the proportion of abnormal results was 9.7%.9 Thus, the results differed from those of the present study, in which only one patient with a time-averaged maximum mean velocity greater than 200 cm/s was found, representing 1.6%. This finding is in agreement with the results from other studies conducted in Brazil, which also found lower frequencies of abnormal results.23-25
In Sergipe, in 2005, Melo et al. gathered data on 34 patients with sickle cell anemia, aged less than 18 years, and compared them with 80 controls. Among the results from the patients, none of them (0.0%) presented abnormal time-averaged maximum mean velocity and four (11.7%) presented conditional results.24
In São Paulo, Park et al. evaluated 77 patients with sickle cell disease, aged between 2 and 16 years. They found two patients (2.6%) with abnormal time-averaged maximum mean velocity and 11 (14.3%) with conditional results.23
In Minas Gerais, in 2008, Silva et al. evaluated 153 children with sickle cell anemia, aged 2 to 16 years. They found seven patients (4.6%) with abnormal time-averaged maximum mean velocity and 16 (10.4%) with conditional results.25
In 1999, Kinney et al.22 investigated correlations of risk factors for stroke among patients with sickle cell anemia and found a positive correlation with the Senegal haplotype. In Brazil, the most common haplotype is Bantu, which may be a factor contributing towards this difference. The presence of alpha thalassemia, adherence molecules and thrombophilic factors such as hyperhomocysteinemia or factor V Leiden have been suggested as other likely factors involved in stroke risk.22,26-30
Group II did not present any abnormal or conditional result from transcranial Doppler, probably because of the lower severity of these patients' condition. So far, there are no data in the literature indicating screening for stroke risk using transcranial Doppler among other genotypes of sickle cell disease. In 1990, Adams et al. evaluated patients with sickle cell anemia and SC hemoglobinopathy, although only 10 SC hemoglobinopathy patients were included in the sample (190 patients) and they were analyzed together. In other studies, only patients with sickle cell anemia were included.9,10,15,21
In agreement with several other studies, there was a negative correlation in group I between the time-averaged maximum mean velocities and the hematocrit percentages and hemoglobin levels.15-17,19,20,23-25 No comparison with the literature could be made with regard to the correlation that was found in group II between time-averaged maximum mean velocities and the reticulocyte percentages and fetal hemoglobin levels, since no such data is available in the literature.
There was a statistically significant difference in the time-averaged maximum mean velocities between the groups, such that it was greater in group I. This was probably because of the lower hemoglobin levels and lower hematocrit percentages in this group (P < 0.01).
Abnormalities were only observed in the middle cerebral artery, in both cerebral hemispheres, and these were found both in the patient with abnormal time-averaged maximum mean velocities and in the patients with conditional velocities. In 1992, Adams found that around 60% of the middle cerebral arteries were affected, and that the internal carotid arteries and anterior cerebral arteries were also affected.8,21
Our results emphasize the importance of performing transcranial Doppler on cases of sickle cell anemia. National studies in Brazil involving the use of transcranial Doppler on large numbers of patients with sickle cell disease are needed, given that some findings differ from data in the literature. It is still uncertain whether there is a determining factor that would explain such differences, or whether the sample size would explain these findings.
Transcranial Doppler does not seem to be a priority examination in relation to the other genotypes of sickle cell disease. Longitudinal follow-up studies on patients with different sickle cell genotypes and their respective transcranial Doppler findings are needed to confirm this hypothesis.
CONCLUSION
There was a low prevalence of abnormal Doppler results in patients with sickle-cell disease. Time-average maximum mean velocity was significantly different between the genotypes and correlated with hematological characteristics.
Date of first submission: June 17, 2010
Last received: January 27, 2011
Accepted: February 4, 2011
Sources of funding: None
Conflict of interest: None
-
1Manual de diagnóstico e tratamento de doenças falciformes. Brasília: Anvisa; 2002. Available from: http://www.anvisa.gov.br/divulga/public/sangue/hemoglobinopatia/diagnostico.pdf Accessed in 2011 (Jan 24).
- 2. Cançado RD, Jesus JA. A doença falciforme no Brasil (editorial) [Sickle cell disease in Brazil: (editorial)]. Rev Bras Hematol Hemoter. 2007;29(3):204-6.
- 3. Huttenlocher PR, Moohr JW, Johns L, Brown FD. Cerebral blood flow in sickle cell cerebrovascular disease. Pediatrics. 1984;73(5):615-21.
- 4. Zago MA, Pinto ACS. Fisiopatologia das doenças falciformes: da mutação genética à insuficiência de múltiplos órgãos [The pathophysiology of sickle cell disease: from the genetic mutation to multiorgan dysfunction]. Rev Bras Hematol Hemoter. 2007;29(3):207-14.
- 5. Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood. 1998;91(1):288-94.
- 6. Balkaran B, Char G, Morris JS, et al. Stroke in a cohort of patients with homozygous sickle cell disease. J Pediatr. 1992;120(3):360-6.
- 7. Russell MO, Goldberg HI, Hodson A, et al. Effect of transfusion therapy on arteriographic abnormalities and on recurrence of stroke in sickle cell disease. Blood. 1984;63(1):162-9.
- 8. Adams RJ, Nichols FT, Figueroa R, McKie V, Lott T. Transcranial Doppler correlation with cerebral angiography in sickle cell disease. Stroke. 1992;23(8):1073-7.
- 9. Adams RJ, McKie VC, Hsu L, et al. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med. 1998;339(1):5-11.
- 10. Adams RJ. Stroke prevention and treatment in sickle cell disease. Arch Neurol. 2001;58(4):565-8.
- 11. Goldstein LB, Adams R, Becker K, et al. Primary prevention of ischemic stroke: A statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke. 2001;32(1):280-99.
- 12. Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37(2):577-617.
-
13Department of Health & Human Services. Clinical alert from the National Heart, Lung and Blood Institute. Bethesda: National Institutes of Health; 2004. Available from: http://www.nhlbi.nih.gov/health/prof/blood/sickle/clincial-alert-scd.pdf Accessed in 2011 (Jan 24).
- 14. Riddington C, Wang W. Blood transfusion for preventing stroke in people with sickle cell disease. Cochrane Database Syst Rev. 2002;(1):CD003146.
- 15. Adams R, McKie V, Nichols F, et al. The use of transcranial ultrasonography to predict stroke in sickle cell disease. N Engl J Med. 1992;326(9):605-10.
- 16. Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982;57(6):769-74.
- 17. Arnolds BJ, von Reutern GM. Transcranial Doppler sonography. Examination technique and normal reference values. Ultrasound Med Biol. 1986;12(2):115-23.
- 18. Adams RJ, Nichols FT, Stephens S, et al. Transcranial Doppler: the influence of age and hematocrit in normal children. J Cardiovasc Ultrasonog. 1988;7(3):201-5.
- 19. Adams RJ, Nichols FT, McKie VC, et al. Transcranial Doppler: influence of hematocrit in children with sickle cell anemia without stroke. J Cardiovasc Technol. 1989;8:97-101.
- 20. Ringelstein EB, Kahlscheuer B, Niggemeyer E, Otis SM. Transcranial Doppler sonography: anatomical landmarks and normal velocity values. Ultrasound Med Biol. 1990;16(8): 745-61.
- 21. Adams RJ, Nichols FT 3rd, Aaslid R, et al. Cerebral vessel stenosis in sickle cell disease: criteria for detection by transcranial Doppler. Am J Pediatr Hematol Oncol. 1990;12(3): 277-82.
- 22. Kinney TR, Sleeper LA, Wang WC, et al. Silent cerebral infarcts in sickle cell anemia: a risk factor analysis. The Cooperative Study of Sickle Cell Disease. Pediatrics. 1999;103(3):640-5.
- 23. Park MVF, Pádua SS, Passos RA, et al. Avaliação do Doppler transcraniano em pacientes com doença falciforme. Rev Bras Hematol Hemoter. 2006;28(2):14. [tema livre]
- 24. Melo HA, Barreto-Filho JAS, Prado RC, Cipolotti R. Doppler transcraniano em portadores de anemia falciforme: estudo dos parâmetros de fluxo sangüíneo cerebral em crianças de Aracaju, Sergipe [Transcranial doppler in sickle cell anaemia: evaluation of brain blood flow parameters in children of Aracaju, Northeast-Brazil]. Arq Neuropsiquiatr. 2008;66(2b):360-4.
- 25. Silva C, Borato M, Freitas A, et al. Rastreamento de crianças com anemia falciforme pelo Doppler transcraniano para detecção de risco de acidente vascular cerebral - experiência do hemocentro de Belo Horizonte - Hemominas. Rev Bras Hematol Hemoter. 2008;30(4):237-8. [tema livre]
- 26. Graido-Gonzales E, Doherty JC, Bergreen EW, et al. Plasma endothelin-1, cytokine, and prostaglandin E2 levels in sickle cell disease and acute vaso-occlusive sickle crisis. Blood. 1998;92(7):2551-5.
- 27. Kirkham FJ, Prengler M, Hewes DK, Ganesan V. Risk factors for arterial ischemic stroke in children. J Child Neurol. 2000;15(5):299-307.
- 28. Telen MJ. Red blood cell surface adhesion molecules: their possible roles in normal human physiology and disease. Semin Hematol. 2000;37(2):130-42.
- 29. Solovey AA, Solovey AN, Harkness J, Hebbel RP. Modulation of endothelial cell activation in sickle cell disease: a pilot study. Blood. 2001;97(7):1937-41.
- 30. McIntyre TM, Prescott SM, Weyrich AS, Zimmerman GA. Cell-cell interactions: leukocyte-endothelial interactions. Curr Opin Hematol. 2003;10(2):150-8.
Publication Dates
-
Publication in this collection
30 June 2011 -
Date of issue
May 2011
History
-
Accepted
04 Feb 2011 -
Reviewed
27 Jan 2011 -
Received
17 June 2010