Abstracts
Guyon's canal syndrome, an ulnar nerve entrapment at the wrist, is a well-recognized entity. The most common causes that involve the ulnar nerve at the wrist are compression from a ganglion, occupational traumatic neuritis, a musculotendinous arch and disease of the ulnar artery. We describe two cases of Guyon's canal syndrome and discuss the anatomy, aetiology, clinical features, anatomical classification, diagnostic criteria and treatment. It is emphasized that the knowledge of both the surgical technique and anatomy is very important for a satisfactory surgical result.
Guyon's canal syndrome; ulnar nerve; anatomy; electromyography
A síndrome do canal de Guyon, um encarceramento do nervo ulnar a nível do punho, é bem conhecida. Ela é causada por neurite ocupacional traumática, doenças e traumas do arco músculo-tendíneo e doença de artéria ulnar. Descrevemos dois casos de síndrome do canal de Guyon e discutimos os aspectos anatômicos e etiológicos, suas características clínicas, classificação anatômica e critérios de diagnóstico, bem como fazemos uma análise crítica do tratamento imposto. Enfatizamos também que, para obter um resultado cirúrgico satisfatório, é importante conhecer bem tanto as técnicas cirúrgicas como sua anatomia.
síndrome do canal de Guyon; nervo ulnar; anatomia; eletromiografia
SURGICAL MANAGEMENT OF GUYON'S CANAL SYNDROME
AN ULNAR NERVE ENTRAPMENT AT THE WRIST
Report of two cases
Paulo Henrique Aguiar1 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil. , Edson Bor-Seng-Shu1 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil. , Fernando Gomes-Pinto1 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil. , Ricardo Jose de Almeida- Leme1 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil. , Alexandre Bruno R. Freitas2 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil. , Roberto S. Martins1 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil. , Edison S. Nakagawa1 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil. , Antonio J. Tedesco-Marchese1 1 M.D., Peripheral Nerve Group of Division of Neurosurgery of São Paulo University Medical School, São Paulo, Brazil; 2M.D., Neurosurgical Clinic of Pinheiros, São Paulo, Brazil.
ABSTRACT - Guyon's canal syndrome, an ulnar nerve entrapment at the wrist, is a well-recognized entity. The most common causes that involve the ulnar nerve at the wrist are compression from a ganglion, occupational traumatic neuritis, a musculotendinous arch and disease of the ulnar artery. We describe two cases of Guyon's canal syndrome and discuss the anatomy, aetiology, clinical features, anatomical classification, diagnostic criteria and treatment. It is emphasized that the knowledge of both the surgical technique and anatomy is very important for a satisfactory surgical result.
KEY WORDS: Guyon's canal syndrome, ulnar nerve, anatomy, electromyography.
Síndrome de compressão do nervo ulnar a nível do punho (síndrome do canal de Guyon): relato de dois casos
RESUMO A síndrome do canal de Guyon, um encarceramento do nervo ulnar a nível do punho, é bem conhecida. Ela é causada por neurite ocupacional traumática, doenças e traumas do arco músculo-tendíneo e doença de artéria ulnar. Descrevemos dois casos de síndrome do canal de Guyon e discutimos os aspectos anatômicos e etiológicos, suas características clínicas, classificação anatômica e critérios de diagnóstico, bem como fazemos uma análise crítica do tratamento imposto. Enfatizamos também que, para obter um resultado cirúrgico satisfatório, é importante conhecer bem tanto as técnicas cirúrgicas como sua anatomia.
PALAVRAS-CHAVE: síndrome do canal de Guyon, nervo ulnar, anatomia, eletromiografia.
Guyon's canal syndrome, an ulnar nerve entrapment at the wrist, is a well-recognized entity. The ulnar carpal tunnel (Guyon's canal) was first described by Felix Guyon in 18611. Gessler (1896) described a peculiar form of muscle atrophy in the hands of gold polishers but did not recognize the lesion as an ulnar neuropathy2. Later, authors reported various occupations or hobbies as predisposing to ulnar neuropathy3,4. A detailed review of the syndrome was presented by Shea and McClain based on 136 reported cases in 19695.
The most common causes that involve the ulnar nerve at the wrist are compression from a ganglion, occupational traumatic neuritis, presence of musculotendinous arch and disease of the ulnar artery5-10. Some authors have described the presence of accessory or anomalous muscles traversing Guyon's canal and variations in the anatomy of the ulnar nerve, some of which can rarely lead to entrapment neuropathy11-15.
The objective of this study is to bring a better knowledge of the surgical techniques and the anatomy in view of the importance of both in obtaining satisfactory surgical results. The anatomy, aetiology, clinical features, diagnostic criteria and treatment of the Guyon's canal syndrome were reviewed.
CASES
Case 1. This 36-year-old woman presented with a three year history of intermittent dull aching and burning pain in the right palm and 6 months with progressive weakness of the right hand. She tended to drop objects and she noticed a slow onset weakness while working at home as a housewife.
On examination, there was a weakness of abductor digiti quinti and a marked weakness of the opponent digiti quinti, interossei, and adductor pollicis. There was sensory impairment to light touch or pinprick. Tinel's sign was positive. Rheumatological and endocrinological blood tests and exams presented normal values.
Electromyographic examination showed fibrillation and positive sharp waves at rest and weakness in ulnar muscles of the hand (lumbricals, abductor digiti quinti, abductor pollicis brevis, flexor carpi ulnaris. Conduction velocity studies of the right ulnar nerve for interosseous muscle showed delayed latencies, sparing of the abductor digiti quinti. (Type 1 Guyon syndrome electromyographic pattern).
A linear incision was made over the right palm on the ulnar surface, starting just proximal to the pisiform bone and extending to the palm for about 4.5 cm, then curving laterally to the midpalm (Fig 1). Microdissection was made through the palmar aponeurosis, and the ulnar artery was identified. Medially to ulnar artery, it was found the ulnar nerve with the deep and superficial branches (Fig 2). An extra-neural neurolysis of ulnar at the wrist was completely performed with section of the volar wrist crease. The wound was closed in layers as a rule. The symptoms improved one year after the surgery with partial recovery of motor weakness and sensibility. The electromyographic control was performed, showing increase of the conduction velocity as the same time as the last follow up.
Case 2. A 42-year-old woman presented with one-year duration history of burning pain in the right palm and 5 months after the onset of impairment of sensibility, progressive weakness of the right hand. She was unable to hold objects and a strong hypotrophy of thenar and hypothenar eminence (Fig 5), as well as interosseous and lumbrical muscle were noted. She denied any injury and all the rheumatological and endocrinological tests were done with negative results for diabetes, rheumatism, acromegaly and other clinical disturbances.
On examination, there was a slight weakness of abductor digiti quinti and marked weakness of the opponents digiti quinti, interossei, and adductor pollicis. There was sensory impairment to light touch or pinprick in ulnar region of the wrist. Tinel's sign was positive distal to the wrist.
Electromyographic examination showed fibrillation and positive sharp waves at rest and weakness in ulnar muscles of the hand (lumbricals, abductor digiti quinti, abductor pollicis brevis, flexor carpi ulnaris) similar to the first case. Conduction velocity studies of the right ulnar nerve for interosseous muscle showed an important delayed latency, without reaching the abductor digiti quinti. (Type 1 Guyon syndrome, electromyographic pattern).
Surgery with microsurgical technique was performed as in the first case, however with a minor skin incision of about 3.0 cm. An extra-neural neurolysis of ulnar nerve at the wrist was totally performed with section of the volar wrist crease. The patient was discharged from the hospital at the second postoperative day without pain but she did not return for a follow up.
DISCUSSION
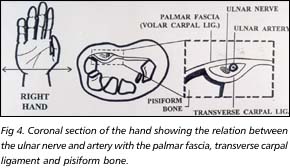
Guyon's canal syndrome refers to compression neuropathy of the ulnar nerve at the wrist. The ulnar tunnel, or Guyon's canal, is an oblique fibro-osseous tunnel that lays within the proximal part of the hypothenar eminence; it is confined by the pisiform and hook of the hamate and is covered proximally by the palmar carpal ligament and distally by the short palmar muscle (Fig 4). The canal contains the ulnar nerve, the ulnar artery with their venae comitantes and loose fibrofatty tissue. Within the canal, the ulnar nerve divides into superficial sensory and deep motor branches (Fig 3).
The superficial branch proceeds distally in line with the main trunk of the nerve and, on exit from the canal, it supplies a small branch to the palmaris brevis muscle. Its terminal branches provide sensation to the little finger and the ulnar half of the ring finger. The deep motor branch along with the ulnar artery takes an acute lateral turn about the hook of the hamate. At this point it passes under a fibrotendinous arch (pisohamate hiatus), which in part gives origin to the muscles of the hypothenar eminence. This is the most vulnerable site for compression of the deep motor branch of the ulnar nerve. The deep motor branch innervates hypothenar muscles, lumbricals 3 and 4 and all interossei1,16.
The ulnar nerve may be compressed anywhere along the course of the Guyon's canal causing sensorimotor, only motor, or only sensory abnormalities.
Shea and McClain (1969) divided lesions of the ulnar nerve in Guyon's canal into three types, depending on the anatomical site at the wrist at which the ulnar nerve is compromised5 (Fig 6).
In type I, the ulnar nerve is involved just proximal to or within Guyon's canal and there are both motor and sensory abnormalities; weakness in all intrinsic hand muscles innervated by ulnar nerve and sensory deficit in the hypothenar eminence and ulnar half of the ring finger, both on the palmar surface only but not at the dorsum that is innervated by the dorsal cutaneous nerve.
In type II, the location of compression is along the deep branch and there is only weakness in muscles innervated by the deep branch; depending on the location, it may spare hypothenar muscles.
In type III, the location of compression is distal in the end of the Guyon's canal and only sensory abnormalities on palmar ulnar distribution; there is no motor deficit. It is the most rare of the three syndromes.
Types I and II are always associated with atrophy of the first dorsal interosseous muscle5,17.
Hirooka et al.17 reported a case with a different clinical presentation caused by an atypical fibrous band, which passed from the pisiform bone to the palmar carpal ligament; a nerve constriction, proximal to the musculotendinous arch, was observed on the superficial sensory branch and a part of the deep branch, which carried the branch supplying abductor digiti minimi. Claw-finger deformity of the little finger, abductor digiti minimi atrophy without atrophy of the first dorsal interosseous muscle and hypoaesthesia on the ulnar side of the little finger were observed. In this case the syndrome could not be classified into one of three classical types (I, II, III)17.
Shea and McClain listed 19 different lesions causing compression of the ulnar nerve at the wrist and hand; the most frequent cause was ganglion (28.7%), occupational neuritis (23.5%), laceration (10.3%), ulnar artery disease (8.1%), fracture of carpal bones (5.9%). Most of lesions (52%) were type II, 30% were type I and 18% were type III5,18.
The causes of involvement of the ulnar nerve in the vicinity of Guyon's canal are: congenital (anomalous muscles, accessory ossicles), trauma (closed or penetrating), inflammation (rheumatoid arthritis), mass lesions (intrinsic or extrinsic), vascular (thrombosis of the ulnar artery) and degenerative (osteoarthritis)16. Trauma can be penetrating (stab wounds) or acute closed (with or without fracture-dislocation) or chronic closed-multiple repetitive trauma from occupation or hobby, lifestyle or anecdotal events as bicycle riding, motorcycle riding, amateur gardener, manually cracking large sacks of nuts. Mass lesions can be neoplastic extrinsic (lipoma), non-neoplastic extrinsic (ganglion, benign giant cell tumour, neoplastic intrinsic (neurofibroma) or non-neoplastic intrinsic (intraneural cysts)4,15,16,19. Compression of the ulnar nerve in Guyon's canal by a benign giant cell tumour is rare16.
O'Hara and Stone (1988) described an unique case of ulnar neuropathy of the wrist due to an aberrant flexor carpi ulnaris insertion with approximately one-fifth of the tendon inserted 5 mm radially to the major insertion 20.Later, Al-Qattan and Duerkson (1992) described a similar recurrent branch and Papierski (1996) described a similar case which the reunion with the main trunk of the ulnar nerve occurred distal to the pisiform. Although it is a rare variant, the possibility of this recurrent branch should be considered when exploring Guyon's canal15.
According to Streib et al., axonal degeneration may be an early abnormality in distal ulnar neuropathy; as nerve damaged from compression increases, segmental demyelisation occurs21.
The diagnosis of distal ulnar neuropathy is based on clinical criteria but electromyography and determination of the nerve conduction should be done to localize the lesion and to determine the extent of nerve damage21. An accurate history must be taken including details about occupation, hobby and life style2. Generalized disorders have to be considered such as rheumatoid arthritis, scleroderma, and diabetes mellitus. The possibility of an abnormality of the cervical spine, shoulder, and elbow must be excluded5.
Symptoms are similar to those of ulnar nerve involvement at the elbow, except for there will never be sensory loss in the dorsum of the hand because the dorsal cutaneous branch leaves the nerve forearm 5-8 cm proximal to the wrist.
Pain, when present, may be exacerbated by tapping over pisiform (Tinel's sign). It may also radiate up the forearm. The palmaris brevis sign may occasionally be useful in diagnosis which helps to differentiate between ulnar nerve compression at the cubital tunnel or at the wrist. When the patient abducts the little finger on volition, there is simultaneous contraction of the palmaris brevis. This contraction will be absent if the entrapment of the ulnar nerve is at the cubital tunnel but it is usually preserved when the ulnar nerve is compressed at the pisohamate hiatus22.
Acute pain and swelling occur in the wrist in patients with calcification in the flexor carpi ulnaris tendon but usually without ulnar nerve compression23.
Electrodiagnostics is usually helpful in localizing the site of the lesion. In type I, electrodiagnostic studies may reveal normal motor conduction velocity of the ulnar nerve in the across-the-elbow and elbow-to-wrist segments, prolonged distal latency to the abductor digiti minimi and first dorsal interosseous muscles, prolonged sensory latency and diminished evoked sensory responses. In type II, normal motor conduction velocity in the ulnar nerve in the across-the-elbow and elbow-to wrist segments, normal sensory latency and sensory evoked responses, normal distal motor latency to the abductor digiti quinti minimi and prolonged latency to the first dorsal interosseous; denervation potentials in the first dorsal interosseous but not in the abductor digiti quinti8,16,18,24.
X-rays of the hand and of the wrist including the carpal -canal view are necessary to demonstrate possible fractures and bone displacement5. Magnetic resonance imaging is indicated only in patients with equivocal clinical findings, a suspected mass lesion or persistent symptoms after surgery25.
The treatment requires evaluation of the etiological factor. If the syndrome results from mechanical repetitive trauma (occupation, hobby, life style), the approach is trying to avoid the pressure on the hypothenar eminence. An initial trial of conservative therapy by immobilization, discontinuance of traumatic habits and local injection of cortisone may be tried. Surgical decompression may be indicated in refractory cases5,16,18.
If mass lesions cause compression, the therapy is surgical. Mass lesions such as small ganglia may not always be palpable through the skin. Persistent signs of impairment of the deep branch of the ulnar nerve with distal latency criteria to suggest involvement of the ulnar nerve in Guyon's canal warrant surgical exploration16.
When the surgical exploration of the Guyon's canal region is performed, the ulnar nerve and artery can be freed in Guyon's canal and the nerve dissected. The skin incision should be extensive to wrist and palmar line as showed in Figure 1. If this should reveal a ganglion, it can be dissected out and removed completely with its deeper pedicle. If an obvious mass lesion is found, it is excised; otherwise, all constricting bands are divided and the pisohamate hiatus is unroofed18.
Two cases of ulnar nerve compression at the wrist due to arthrosynovial cysts arising from the hamatotriquetral joint with complete recovery was reported by Maynou et al. and confirmed the favourable prognosis of this form of compression provided surgical treatment is performed early and rigorously19,26.
We conclude that Guyon's canal syndrome is a well defined syndrome, which complains three types 1) with motor and sensory abnormalities; 2) only motor weakness and 3) pure sensory deficit. Nevertheless the syndrome is not so frequent as the carpal canal syndrome and it is crucial to know both the surgical technique and anatomy in order to obtain a satisfactory surgical result.
Acknowledgements - The authors are thankful to Flávia C. F. Tavares for the English review.
Received 21 March 2000, received in final form 19 Setpember 2000. Accepted 23 September 2000.
Dr. Paulo Henrique Aguiar Rua Maestro Torquato Amore 332/12 Bloco I 05622-050 São Paulo SP Brasil. FAX 11 282 6822. E-mail: pha-neuro@hotmail.com
- 1. Guyon F. Note sur une disposition anatomique propre ŕ la face antérieure de la région du poignet et non encour décrite par le docteur. Bull Soc Anat Paris 1861;6:184-186.
- 2. Gessler H. Eine eigenartige Form von progressiver Muskelatrophie bei Goldpolirerinnen. Med Cor-Bl d würtemb ärztl Yer Stuttg 1896;66:281-283.
- 3. Bakke JL, Wolff HG. Occupational pressure neuritis of the deep palmar branch of the ulnar nerve. Arch Neurol Psychiatry 1948;60:549-553.
- 4. Eckman PB, Perstein G, Altrocchi PH. Ulnar neuropathy in bicycle riders. Arch Neurol 1975;32:130-131.
- 5. Shea JD, McClain EJ. Ulnar-nerve compression syndromes at and bellow the wrist. J Bone Joint Surg 1969;51:10951103.
- 6. Hunt JR. Occupation neuritis of the deep palmar branch of the ulnar nerve: a well defined clinical type of professional palsy of the hand. J Nerv Ment Dis 1908;35:673-689.
- 7. Kalisman M, Laborde K, Wolff TW. Ulnar nerve compression secondary to ulnar false aneurysm at the Guyon's canal. J Hand Surg 1982;7:137-139.
- 8. Penkert G, Moringlane JR, Samii M. Beseitig kombiniertes Karpaltunnel und Loge des Guyon Syndrom. Akt Neurol 1982;9:205-207.
- 9. Uriburu IJF, Morchia FJ, Marin JC. Compression syndrome of the deep motor branch of the ulnar nerve (Pisohamate hiatus syndrome). J Bone Joint Surg 1976;58:145-147.
- 10. Vanderpool DW, Chalmers J, Lamb DW, Whiston TB. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg 1968;50:792-803.
- 11. Demman EE. An unusual branch of the ulnar nerve in the hand. Hand 1977;9:92-97.
- 12. Fenning JB. Deep ulnar nerve paralysis resulting from an anatomical abnormality: a case report. J Bone Joint Surg 1965;47:1381-1385.
- 13. Kaplan EB. Variation of the ulnar nerve at the wrist. Bull Hosp Joint Dis 1963;24:85-88.
- 14. Lassa R, Shrewbury MM. A variation in the path of the deep motor branch of the ulnar nerve at the wrist. J Bone Joint Surg 1975;57:990-991.
- 15. Papierski P. Ulnar neuropathy at the wrist associated with a recurrent branch through the flexor carpi ulnaris tendon. J Hand Surg (Br) 1996;21:347-348.
- 16. Rengachary SS, Arjunan K. Compression of the ulnar nerve in Guyon's canal by a soft tissue cell tumour. Neurosurgery 1981;8:400-405.
- 17. Hirooka T, Hashizume H, Nagoshi M, Shigeyama Y, Inoue H. Guyon's canal syndrome: a different clinical presentation caused by an atypical fibrous band. J Hand Surg (Br) 1977;22:52-53.
- 18. Cavallo M, Poppi M, Martinelli P. Distal ulnar neuropathy from carpal ganglia: a clinical and electrophysiological study. Neurosurgery 1988;22: 902-905.
- 19. Maynou C, Mestdgh H, Butruillee Y, Lecomte-Houcke M. Compression of the ulnar nerve at the wrist due to an arthro-synovial cyst: apropos of two cases. Ann Chir Main Memb Super 1997;16:146-151.
- 20. O'Hara JJ, Stone JH. Ulnar neuropathy at the wrist associated with aberrant flexor carpi ulnaris insertion. J Hand Surg 1988;13:382-384.
- 21. Streib EW, Sun SF, Cochran RM II, Leibrock LG. Distal ulnar neuropathy: clinical and electrophysiologic aspects. Surg Neurol 1985;23:281-286.
- 22. Pleet AB, Massey EW. Palmaris brevis sign in neuropathy of the deep palmar branch of the ulnar nerve. Ann Neurol 1978;3:468- 469.
- 23. Seidenstein H. Acute pain in the wrist and hand associated with calcific deposits: report of fifteen cases. J Bone and Joint Surg 1950;32:413-418.
- 24. Campion D. Electrodiagnostic testing in hand surgery. J Hand Surg (Br) 1996;21:947-956.
- 25. Oneson SR, Scales LM, Erickson SJ, Timins ME. MR imaging of the painful wrist. Radiographics 1996;16:997-1008.
- 26. Tatagiba M, Penkert G, Samii M. Kompressionssyndrom des motorischen Endastes des Nervus ulnaris: Kasuistik und Literturübersicht . Chirurg 1990;61:849-852.
Publication Dates
-
Publication in this collection
06 Apr 2001 -
Date of issue
Mar 2001
History
-
Reviewed
19 Sept 2000 -
Received
21 Mar 2000 -
Accepted
23 Sept 2000