Abstracts
The present review was aimed at providing help for correct interpretation of gallbladder wall thickening and differential diagnosis at ultrasonography. Gallbladder wall thickening is a frequent sonographic finding and has been subject of great interest for being considered as a hallmark feature of acute cholecystitis, despite the fact that such a finding is observed in a number of other medical conditions. An appropriate characterization and interpretation of this finding is of great importance, considering that the correct diagnosis has a direct impact on the treatment that in some cases includes surgery. In the present article, the authors describe a set of sonographic signs that, in association with clinical and laboratory findings can reduce the number of diagnostic hypotheses allowing a more accurate establishment of the cause for gallbladder wall thickening through a rational data evaluation.
Gallbladder; Ultrasonography; Inflammation; Neoplasm
O objetivo desta revisão é fornecer auxílio na interpretação correta do espessamento das paredes da vesícula biliar e seus possíveis diagnósticos diferenciais. O espessamento da vesícula biliar é um achado frequente em exame de ultrassonografia e um tema de grande interesse, por ter sido considerado durante muito tempo como sinal específico de colecistite aguda, apesar de se reconhecer que ocorre em uma série de outras situações clínicas. A adequada caracterização e interpretação desse achado é de grande importância, pois o diagnóstico correto tem impacto direto no tratamento, que em alguns casos inclui intervenção cirúrgica. Neste artigo procuramos apresentar um conjunto de sinais ultrassonográficos que, associados ao quadro clínico e laboratorial do paciente, permitem restringir as alternativas diagnósticas e estabelecer, com maior precisão, a causa do espessamento parietal da vesícula biliar, através de uma avaliação racional dos dados obtidos.
Vesícula biliar; Ultrassonografia; Inflamação; Neoplasia
REVIEW ARTICLE
Gallbladder wall thickening at ultrasonography: how to interpret it?*
Aldo Benjamim Rodrigues BarbosaI; Luis Ronan Marquez Ferreira de SouzaII; Rogério Silva PereiraIII; Giuseppe D'IppolitoIV
IMD, Radiologist at Santa Casa de Misericórdia de Ituverava, Special Student, Course of Post-graduation in Pathology, Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil
IIPhD, Associate Professor, Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil
IIIMD, Radiologist, Department of Imaging Diagnosis, Santa Casa de Misericórdia de Ituverava, Ituverava, SP, Brazil
IVFellow PhD degree, Associate Professor, Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil
Mailing Address
ABSTRACT
The present review was aimed at providing help for correct interpretation of gallbladder wall thickening and differential diagnosis at ultrasonography. Gallbladder wall thickening is a frequent sonographic finding and has been subject of great interest for being considered as a hallmark feature of acute cholecystitis, despite the fact that such a finding is observed in a number of other medical conditions. An appropriate characterization and interpretation of this finding is of great importance, considering that the correct diagnosis has a direct impact on the treatment that in some cases includes surgery. In the present article, the authors describe a set of sonographic signs that, in association with clinical and laboratory findings can reduce the number of diagnostic hypotheses allowing a more accurate establishment of the cause for gallbladder wall thickening through a rational data evaluation.
Key words: Gallbladder; Ultrasonography; Inflammation; Neoplasm.
INTRODUCTION
Gallbladder wall thickening is a controversial topic among sonographers for being frequently found and for having been considered, for a long time, a sign highly suggestive acute cholecystitis. Such a concept has been undergoing changes as a result of a greater experience of the professionals involved in imaging diagnosis and the considerable technological development of ultrasonography (US) apparatuses(1).
Among the different diseases that cause gallbladder walls thickening besides acute cholecystitis, pancreatitis, diverticulitis, heart failure, pyelonephritis and hepatitis can be mentioned. The appropriate characterization and interpretation of such finding is of utmost importance, considering that the correct diagnosis has a direct impact on the treatment and that in some cases some of these diseases require surgical approach(2).
Ultrasonography is the initial imaging method for diagnostic approach and evaluation of the biliary system, as it is widely available, safe, innocuous and non-expensive. This method allows the detailed real-time study of the gallbladder, besides the evaluation of other findings that contribute to the final diagnosis, thus avoiding unnecessary cholecystectomies and their complications(3-5). Additionally, pre-operative US (24 to 48 hours prior to surgery) may be utilized as a safe and effective method to avoid intraoperative endoscopic retrograde cholangiopancreatography (IERC)(6). In the present article, gallbladder wall thickening is contextualized to guide its accurate interpretation in the light of clinical data and to allow the choice of the appropriate therapeutic approach.
ANATOMY AND SONOGRAPHIC TECHNIQUE
The gallbladder is a hollow pear-shaped viscera with thin and regular walls, located in the gallbladder fossa between the IV and V segments of the liver, an area which is devoid of the visceral peritoneum(7). The gallbladder is divided into the infundibulum, body and fundus (Figure 1), and its walls comprise four layers: a mucosa formed by a simple columnar epithelium and by a basal lamina; a second layer comprising irregular muscular tissue; a third layer constituted by loose connective tissue; and a last layer formed by the serosa(8-10). Its function is to store the bile, and presents a volume of 30 to 50 ml(6).
Gallbladder US is routinely performed with a convex transducer. In order to acquire appropriate images, a systematic scanning should be carried out with longitudinal and cross sectional views of the organ, evaluating its shape, dimensions, wall thickness, regularity and texture pattern of its walls and contents, besides locoregional and Doppler velocimetric al-terations(8). In order to assist the sonographic evaluation, the apparatuses are equipped with resources that enhance the methods accuracy, such as the harmonic imaging, which allows increased lateral resolution, signal-noise and contrast-noise ratios(9).
Sonographic images provide a faithful representation of the gallbladder which can be correlated with its anatomical structure. By means of US it is possible to identify three layers: the innermost, corresponding to the mucosa, that is linear, echogenic and presents a regular surface; the second one, corresponding to the muscular layer, is thin and slightly hypoechoic; and outermost layer corresponding to the organ's serosa, that is linear, echogenic and regular(1,9).
According to several authors(1,2), the upper limit for normality of the gallbladder wall thickness is 3 mm. However, in patients under inappropriate fasting, the parietal thickness may exceed such a limit because of the organ's smooth muscle con-traction(8). So, 8-hour fasting before the examination is recommended, particularly in cases where the gallbladder is the focus of the study. The main differential diagnosis of parietal thickening is that of functional changes of the organ, in which one observes a persistently withered gallbladder, even at a re-evaluation after extended fasting(9). Another cause of "pseudothickening" is related to erroneous insonation by the transducer. In this case, the performance of maneuvers changing the decubitus is useful in the correct definition of the gallbladder wall thickness. An important differential diagnosis in these cases is the functional change of the gallbladder (10,11) (Figure 2).
Gallbladder wall thickening is classified as mild (between 4 and 7 mm), marked (> 7 mm), and in focal or diffuse. As a rule, systemic diseases such as heart, renal or hepatic failure cause diffuse and less marked thickening, contrary to tumor lesions that cause focal and more exuberant thickening, frequently greater than 10 mm(7). The presence of some associated signs allows the observer to direct the diagnosis towards a more specific etiology(9-11). Among such signs, the following can be mentioned: biliary tract dilation, presence of a static gallstone, perivesicular fluid, hilar lymph node enlargement, perivesicular fat heterogeneity and increased gallbladder transverse diameter. The disorders that cause gallbladder wall thickening may be classified as inflammatory, neoplastic and systemic, and their differentiation may be obtained by means of a combined evaluation of clinical and imaging findings.
INFLAMMATORY CAUSES
Acute calculous cholecystitis
It is the most common inflammatory complication that affects the gallbladder, and is related to choledocholithiasis in 90 95% of the cases. It is the fourth most common cause of acute abdomen requiring hospitalization( 3). In 95% of cases it is caused by persistent obstruction by stones in the infundibulum or in the cystic duct. In spite of not being pathognomonic, acute calculous cholecystitis is the main cause of gallbladder wall thickening at US. In general, the gallbladder wall is less than 7 mm thick, presenting regular contour and trilaminar appearance(3,9,11). Such echotextural appearance of the gallbladder walls may change, for example in cases of emphysematous cholecystitis, where echogenic parietal images with acoustic reverberation compatible with gas are observed(12) (Figure 3).
Other sonographic findings are important, as they increase the method specificity, such as: impacted calculus in the common bile duct with upstream dilatation, infundibular calculi, tense gallbladder with a transverse diameter > 4 cm (hydrops of the gallbladder), positive painful decompression at the cystic point (sonographic Murphy's sign), presence of perivesicular fluid and hyperflow from its walls at Doppler(5) (Figure 4).
The US sensitivity ranges between 80% and 100%, and specificity ranges between 60% and 100%. The positive predictive value in the identification of calculi is 88%, increasing to 92% as associated with sonographic Murphy's sign. Gallbladder wall thickening associated with the Murphy's sign has a predictive value of up to 94%(11,12).
Another rare condition that determines gallbladder wall thickening associated with inflammatory process is the Mirizzi syndrome. In such a situation, an impacted gallstone located in the gallbladder neck or in the cystic duct causes dilatation of the biliary tract, causing compression of the common hepatic duct or secondary inflammation, producing edema or fibrosis on the duct wall. At US, besides the impacted calculus, one observes a distal common bile duct with normal caliper, peribiliary inflammatory signs and gallbladder wall thickening, similar to acute cholecystitis. Magnetic resonance imaging (MRI) and MRI cholangiography are very useful in such cases, particularly to rule out the presence of a pancreatic head tumor or primary sclerosing cholangitis(11) (Figure 5).
Chronic calculous cholecystitis
It consists of an inflammatory process of the gallbladder, originated from a transitory gallbladder obstruction, causing inflammation and fibrosis(11,12). Porcelain gallbladder is a rare presentation of chronic cholecystitis, where the gallbladder walls are partially or completely calcified. In spite of the lack of consensus, many authors consider that the inflammatory process represents a risk factor for gallbladder carcinoma, and, even being it an accidental finding in asymptomatic patients submitted to routine US examinations, many advocate the prophylactic cholecystectomy(1,3,13) (Figure 4).
Acalculous cholecystitis
Acalculous cholecystitis is an uncommon and severe entity, affecting patients with diabetes and in poor general conditions. It is more common in hospitalized patients (undergoing mechanical ventilation and hyperalimentation therapy) and trauma victims, or in extensive burn patients, with a high mortality rate. Such a condition was described in 1970, in seriously wounded soldiers during the Vietnam war(14).
During the interpretation of the sonographic findings, i.e., gallbladder wall thickening, tense and distended gallbladder, and presence of perivesicular fluid, the correlation with the clinical context is of utmost importance for a correct diagnosis(3,14). The absence of sonographic Murphy's sign does not rule out the diagnosis(14,15) (Figure 6).
Acalculous cholecystitis is frequently misdiagnosed, as some sonographers equivocally attribute to chronic acalculous cholecystitis, the secondary thickening determined by systemic pathologies such as pyelonephritis(16), for example. Another common erroneous interpretation occurs in cases of acute cholecystitis caused by non-visualized small obstructive calculi in the common bile duct(3) (Figure 7).
Xanthogranulomatous cholecystitis
It is an uncommon pathology, described in the early 1980's as a pseudotumor presentation of chronic calculous cholecystitis, secondary to bile extravasation through the gallbladder walls, frequently associated with adenocarcinoma(17,18). At macroscopic examination, one observes a nodular thickening of the walls in association with the presence of calculi and possible loco-regional infiltration. Lymph nodes enlargement and coexistence with gallbladder cancer may also be found.
Its main sonographic sign is diffuse gallbladder wall thickening, besides hypo-echoic nodules, which may be found in up to 35% of the patients(3,17,18). Such cases may be undistinguishable from the infiltrative presentation of gallbladder carcinoma(18). Clinically, it manifests with a clinical picture of cholecystitis in women aged from 60 to 70 years.
Adenomyomatosis of the gallbladder
It is characterized by excessive proliferation of the surface epithelium towards the Rokitansky-Aschoff sinuses, determining wall thickening that may be focal, segmental or diffuse(5). The main sonographic presentation corresponds to segmental parietal thickening with multiple echogenic intramural foci, which cause posterior reverberation artifacts, known as comet-tail artifacts. Other signs such as gallbladder distension, presence of perivesicular fluid or positive sonographic Murphy's sign are not observed(3,18).
It is a benign non-inflammatory condition of the gallbladder, found in 8.7% of the cholecystectomies(5). It manifests with persistent pain in the right hypochondrium, and is most commonly found in women, in association with gallstones in 90% of the cases. Upon symptoms persistence, cholecystectomy is indicated(5,15).
Cholesterol polyp
Focal and nodular gallbladder wall thickening represent approximately 50% of all polypoid lesions, and most of the times do not present a malignant potential(1). The patients do not present any symptoms and at US, a static echogenic well defined nodular image is identified. The main differential diagnoses include adenoma and adenocarcinoma(1,19).
Two-dimensional US is not capable of differentiating small neoplastic polypoid lesions from non-neoplastic ones, but some studies have demonstrated the usefulness of three-dimensional US in the differential diagnosis between polyps (Figure 8). In such cases, MRI may be very useful in that differentiation(20).
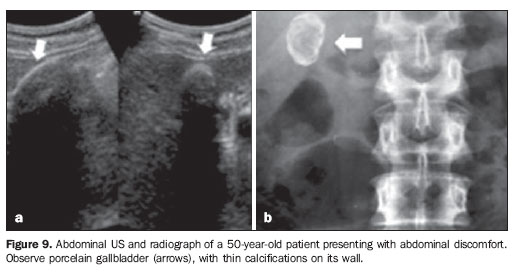
Porcelain gallbladder
It is an uncommon chronic cholecystitis variation characterized by extensive cal-cification of the gallbladder walls, which can be partially or completely affected. The term "porcelain" is utilized because of its consistency and appearance (Figure 9). Its prevalence in cholecystectomies is 0.06% to 0.8%. In 95% of cases, association with cholelithiasis is found. It is five times more common in women than in men, and is most frequent in the fifth and sixth decades of life(7,12). Early in the 20th century, one believed that there was an association with neoplasia, but most recently, studies have not confirmed the initial findings, thus demonstrating a low incidence of coexistence of neoplasia with porcelain gallbladder(20,21).
NEOPLASTIC CAUSES
Gallbladder carcinoma
It is the most common neoplasia of the biliary system, with 2.5 new cases per 100,000 inhabitants per year. It has a high mortality rate as its diagnosis is most of times achieved at advanced stages of the disease, because of the scarcity of symptoms. When present, the initial symptoms are nonspecific and include weight loss, abdominal pain, fever and jaundice(1,2,7,16) and are frequently associated with the presence of calculi (73% to 98%)(6). Only 1% of the cholecystectomies performed for cholelithiasis result in incidental finding of gallbladder carcinoma(2). The most significant risk factor is the presence of chronic inflammatory process usually triggered by the calculi. The main differential diagnoses include complicated acute cholecystitis, hepatocellular carcinoma and metastasis to the gallbladder fossa.
Adenocarcinoma is the malignant histological type of tumor that most frequently affects the gallbladder, occurring in 90% of cases. Such tumor generally presents three image patterns: a) mass occupying and obscuring the gallbladder bed; b) focal or diffuse parietal thickening; c) polypoid parietal lesion projecting towards its lumen. Its most frequent presentation is a large solid lesion in the gallbladder fossa in association with calculi and extending to the liver and adjacent organs (Figure 10).
When focal or asymmetric wall thickening > 10 mm is found, the possibility of neoplasia is high. In such cases the characterization of other factors such as loco-regional lymph nodes enlargement enhances the diagnostic hypothesis. Computed tomography (CT) presents a characteristic enhancement pattern that is typical of lesions suspicious for malignancy, with iodinated contrast uptake in the arterial phase, becoming isodense in the equilibrium phase(22,23). Magnetic resonance imaging demonstrates hyperintense and heterogeneous images on T2-weighted sequences and hypointense on T1-weighted sequences, with post-contrast enhancement. In the cases of diffuse thickening with uniform infiltration, its imaging appearance is similar to that of chronic cholecystitis(21).
The accurate differentiation between malignant and benign polypoid lesions cannot be made by means of US alone. Generally, malignant polyps are > 1 cm and seldom present calcification and necrosis. They present early and prolonged contrast uptake after administration of gadolinium, contrary to benign lesions, which present early contrast uptake with subsequent washout(21-23).
Metastasis to the gallbladder
Some tumors, such as carcinoid tumor, lymphoma, breast carcinoma and sarcomas metastasize to the gallbladder, thus being a possible cause of gallbladder wall thickening. Among them, the most common one is the melanoma, representing approximately 50% of cases(24). Such lesions are undistinguishable from primary neoplasia, but are much less frequently found and not associated with gallstones.
SYSTEMIC CAUSES
Inflammatory processes located in the right hypochondrium that do not originate from the gallbladder and systemic disorders may mimic acute cholecystitis, determining symmetrical and diffuse wall thickening. Such changes are caused by the extension of the inflammation or by the increase in the portal venous pressure associated with decrease in the intravascular osmotic pressure, causing parietal edema. The assessment of a patient presenting with one of such disorders should be undertaken with caution in order to avoid erroneous interpretation of a picture of acalculous cholecystitis. Clinical and laboratory tests results, signs of pneumoperitoneum, inflamed diverticula in the right/transverse colon, inflammation of the appendix with upper location, pyelonephritis signs allow the definition of the anatomical diagnosis. Even so, in several situations, the previous epidemiological history plays an extremely relevant role for the diagnostic orientation, moreover in cases of infectious diseases(4,6,23).
In the evaluation of such disorders, the key sonographic finding is the preservation of mucosal regularity and echogenicity, i.e., of the first layer. The wall thickening occurs at the expense of the hypoechoic layer corresponding to edema of the muscular layer and of the conjunctive tissue(1,4,5).
Acute pancreatitis is a common disease in our environment and its main causes are those of biliary and alcoholic origin. Approximately 64% of the patients presenting with pancreatitis evolve with gallbladder wall thickening(3,23) secondary to extension of the inflammatory process towards locoregional structures(3-5).
Based on this physiopathological principle, any inflammatory process located in the right hypochondrium, such as perforated duodenal ulcer, acute diverticulitis, appendicitis and pyelonephritis, can determine gallbladder wall thickening(3,4,9,20,25) (Figure 8).
In cases of viral hepatitis, regular and diffuse gallbladder wall thickening is observed. The gallbladder is withered, in association with the presence of ganglia adjacent to the hilum and hepatomegaly, besides malaise, fatigue, arthralgia and jaundice(2,17).
Cases of transinfection by hepatitis include diseases such as acquired immune deficiency syndrome (AIDS), dengue and malaria. In patients with AIDS, such finding may be secondary to the utilization of antiretroviral drugs, worsened nutritional status and opportunistic infections of the biliary tract(17) (Figure 11).
Hepatic dysfunctions such as cirrhosis, malnutrition and ascites, cause parietal thickening secondary to hypoalbuminemia in ascites(7). Hypoalbuminemia is the abnormality most frequently associated with ascites in children(1). Ascites may be a consequence of benign and malignant disorders. Some reports suggest that the gallbladder wall thickening is more frequently found in benign diseases, while malignant conditions do not cause gallbladder wall thickening (Figure 12).
Cardiac liver is a clinical condition found in individuals presenting with right heart failure. The physiopathological mechanism of the gallbladder wall thickening is related to increased intrahepatic pressure, determining edema in the second layer of the gallbladder wall associated with preservation of the hyperechogenic appearance of the mucosa. Other findings, such as ectasia of hepatic veins and lower vena cava, Doppler velocimetric alterations and hepatomegaly are also frequently found in this clinical condition(6).
CONCLUSION
Ultrasonography is the method of choice for the study of the gallbladder, with a high sensitivity in the detection of gallbladder wall thickening. Such a finding is not a synonymous for acute cholecystitis. The correlation with other sonographic, clinical, laboratory and epidemiological findings is of utmost importance in order to avoid unnecessary cholecystectomies.
REFERENCES
- 1. Levy AD, Murakata LA, Abbott RM, et al. From the archives of the AFIP: Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Radiographics. 2002;22:387-413.
- 2. Wibbenmeyer LA, Sharafuddin MJ, Wolverson MK, et al. Sonographic diagnosis of unsuspected gallbladder cancer: imaging findings in comparison with benign gallbladder conditions. AJR Am J Roentgenol. 1995;165:1169-74.
- 3. Spence SC, Teichgraeber D, Chandrasekhar C. Emergent right upper quadrant sonography. J Ultrasound Med. 2009;28:479-96.
- 4. Patriquin HB, DiPietro M, Barber FE, et al. Sonography of thickened gallbladder wall: causes in children. AJR Am J Roentgenol. 1983;141:57-60.
- 5. Rosenthal SJ, Cox GG, Wetzel LH, et al. Pitfalls and differential diagnosis in biliary sonography. Radiographics. 1990;10:285-311.
- 6. Watanabe Y, Nagayama M, Okumura A, et al. MR imaging of acute biliary disorders. Radiographics. 2007;27:477-95.
- 7. van Breda Vriesman AC, Engelbrecht MR, Smithuis RH, et al. Diffuse gallbladder wall thickening: differential diagnosis. AJR Am J Roentgenol. 2007;188:495-501.
- 8. AIUM practice guideline for the performance of an ultrasound examination of the abdomen and/ or retroperitoneum. J. Ultrasound Med. 2008;27: 319-26.
- 9. Hong HS, Han JK, Kim TK, et al. Ultrasonographic evaluation of the gallbladder: comparison of fundamental, tissue harmonic, and pulse inversion harmonic imaging. J Ultrasound Med. 2001; 20:35-41.
- 10. Feldman MK, Katyal S, Blackwood MS. US artifacts. Radiographics. 2009;29:1179-89.
- 11. Smith EA, Dillman JR, Elsayes KM, et al. Cross-sectional imaging of acute and chronic gallbladder inflammatory disease. AJR Am J Roentgenol. 2009;192:188-96.
- 12. Handler SJ. Ultrasound of gallbladder wall thickening and its relation to cholecystitis. AJR Am J Roentgenol. 1979;132:581-5.
- 13. Riñón C, de Mingo L, Cortés MJ, et al. Preoperatory sonography efficiency in paediatric patients with cholelithiasis undergoing laparoscopic cholecystectomy. Cir Pediatr. 2009;22:34-8.
- 14. Lindberg EF, Grinnan GL, Smith L. Acalculous cholecystitis in Viet Nam casualties. Ann Surg. 1970;171:152-7.
- 15. Boland GW, Slater G, Lu DS, et al. Prevalence and significance of gallbladder abnormalities seen on sonography in intensive care unit patients. AJR Am J Roentgenol. 2000;174:973-7.
- 16. Campos FA, Rosas GQ, Goldenberg D, et al. Freqüência dos sinais de pielonefrite aguda em pacientes submetidos a tomografia computadorizada. Radiol Bras. 2007;40:309-14.
- 17. Parra JA, Acinas O, Bueno J, et al. Xanthogranulomatous cholecystitis: clinical, sonographic, and CT findings in 26 patients. AJR Am J Roentgenol. 2000;174:979-83.
- 18. Ros PR, Goodman ZD. Xanthogranulomatous cholecystitis versus gallbladder carcinoma. Radiology. 1997;203:10-2.
- 19. Boscak AR, Al-Hawary M, Ramsburgh SR. Best cases of the AFIP: Adenomyomatosis of gallbladder. Radiographics. 2006;26:941-6.
- 20. Xu HX, Yin XY, Lu MD, et al. Comparison of three- and two-dimensional sonography in diagnosis of gallbladder diseases: preliminary experience. J Ultrasound Med. 2003;22:181-91.
- 21. Catalano OA, Sahani DV, Kalva SP, et al. MR Imaging of the gallbladder: a pictorial essay. Radiographics. 2008;28:135-55.
- 22. Zissin R, Osadchy A, Shapiro-Feinberg M, et al. CT of a thickened-wall gall bladder. Br J Radiol. 2003;76:137-43.
- 23. Yun EJ, Cho SG, Park S, et al. Gallbladder carcinoma and chronic cholecystitis: differentiation with two-phase spiral CT. Abdom Imaging. 2004;29:102-8.
- 24. Martel JP, McLean CA, Rankin RN. Melanoma of the gallbladder. Radiographics. 2009;29:291-6.
- 25. Hanbidge AE, Buckler PM, O'Malley ME, et al. From the RSNA refresher courses: imaging evaluation for acute pain in the right upper quadrant. Radiographics. 2004;24:1117-35.
Publication Dates
-
Publication in this collection
04 Jan 2012 -
Date of issue
Dec 2011
History
-
Received
23 Jan 2011 -
Accepted
03 June 2011