ABSTRACT
OBJECTIVE:
To analyze the clinical-functional parameters and quality of life of patients undergoing minimally invasive surgical treatment for extra-articular fractures of the proximal phalanx, using an intramedullary screw (Acutrak(r)).
METHODS:
Between January 2011 and September 2014, a prospective study was conducted on 41 patients (48 fingers) with unstable extra-articular fractures of the proximal phalanx, who underwent minimally invasive surgical treatment using an intramedullary screw (Acutrak(r)). These patients were evaluated 12 months after the surgery by means of the DASH quality-of-life questionnaire, VAS pain scale, measurement of range of motion (ROM, in degrees) and radiographic assessment.
RESULTS:
All the patients achieved adequate reduction and consolidation of their fractures. There were statistically significant improvements in quality of life on the DASH scale, pain on the VAS scale and range of motion.
CONCLUSION:
The minimally invasive technique for treating unstable extra-articular fractures of the proximal phalanx using an intramedullary screw (Acutrak(r)) is effective and safe, and it presents satisfactory clinical-functional results.
Keywords:
Fracture fixation; Internal facture fixation; Fractures of the proximal phalanx
RESUMO
OBJETIVO:
Analisar os parâmetros clínico-funcionais e a qualidade de vida de pacientes submetidos ao tratamento cirúrgico minimamente invasivo das fraturas extra-articulares da falange proximal com uso do parafuso intramedular (Acutrak(r)).
MÉTODOS:
Um estudo prospectivo foi feito de janeiro de 2011 a setembro de 2014 e incluiu 41 pacientes e 48 dedos acometidos com fratura da falange proximal extra- articular e instável submetidos ao tratamento cirúrgico minimamente invasivo com parafuso intramedular (Acutrak(r)). Esses pacientes foram avaliados 12 meses após a cirurgia por meio do questionário DASH de qualidade de vida, escala de dor VAS, arco de movimento (adm em graus) e avaliação radiográfica.
RESULTADOS:
Todos os pacientes obtiveram redução adequada e consolidação das fraturas. Houve melhoria estatisticamente significativa da qualidade de vida (DASH), escala de dor (VAS) e arco de movimento.
CONCLUSÃO:
A técnica minimamente invasiva no tratamento das fraturas instáveis e extra-articulares da falange proximal com o parafuso intramedular Acutrak(r) é eficaz e segura e apresenta resultados clínico-funcionais satisfatórios.
Palavras-chave:
Fixação de fratura; Fixação interna de fraturas; Fraturas da falange proximal
Introduction
Fractures of the phalanges are frequent injuries and account for 6% of all fractures.11. Packer GJ, Shaheen MA. Patterns of hand fractures and dislocations in a district general hospital. J Hand Surg Br. 1993;18(4):511-4.and22. Emmett JE, Breck LW. A review and analysis of 11,000 fractures seen in a private practice of orthopaedic surgery, 1937-1956. J Bone Joint Surg Am. 1958;40(5): 1169-75. Fractures of the proximal phalanx occur more often than those of the middle or distal phalanges.33. de Jonge JJ, Kingma J, van der Lei B, Klasen HJ. Fractures of the metacarpals. A retrospective analysis of incidence and aetiology and a review of the English-language literature. Injury. 1994;25(6):365-9.and44. Kamath JB, Harshvardhan Naik DM, Bansal A. Current concepts in managing fractures of metacarpal and phalanges. Indian J Plast Surg. 2011;44(2):203-11.
Indications for surgical treatment of these fractures need to take into consideration the type of fracture line, the displacement between the fragments and the difficulty in maintaining open reduction of the fracture.33. de Jonge JJ, Kingma J, van der Lei B, Klasen HJ. Fractures of the metacarpals. A retrospective analysis of incidence and aetiology and a review of the English-language literature. Injury. 1994;25(6):365-9. This treatment has the main aim of restoring the anatomy and function of the finger affected.44. Kamath JB, Harshvardhan Naik DM, Bansal A. Current concepts in managing fractures of metacarpal and phalanges. Indian J Plast Surg. 2011;44(2):203-11.and55. Barton N. Internal fixation of hand fractures. J Hand Surg Br. 1989;14(2):139-42.
The techniques that have been described vary from provision of relative stability to the principle of absolute stability. A combination of methods is sometimes necessary,66. Margic´ K. External fixation of closed metacarpal and phalangeal fractures of digits. A prospective study of one hundred consecutive patients. J Hand Surg Br. 2006;31(1):30-40. and this depends on the nature of the fracture line, the availability of implants and the surgeon's preference.
Among the surgical complications, the following stand out: joint stiffness, adherences and/or tearing of the extensor tendon,11. Packer GJ, Shaheen MA. Patterns of hand fractures and dislocations in a district general hospital. J Hand Surg Br. 1993;18(4):511-4. functional loss of the finger22. Emmett JE, Breck LW. A review and analysis of 11,000 fractures seen in a private practice of orthopaedic surgery, 1937-1956. J Bone Joint Surg Am. 1958;40(5): 1169-75. or, furthermore, skewed consolidation, pseudarthrosis and osteomyelitis.55. Barton N. Internal fixation of hand fractures. J Hand Surg Br. 1989;14(2):139-42.,66. Margic´ K. External fixation of closed metacarpal and phalangeal fractures of digits. A prospective study of one hundred consecutive patients. J Hand Surg Br. 2006;31(1):30-40.and77. Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: preferred methods of stabilization. J Am Acad Orthop Surg. 2008;16(10):586-95.
These complications are frequently caused by lack of knowledge of the biomechanics of this organ, by an unfounded belief that all fractures of the hand can be resolved through conservative treatment or by poor patient cooperation.88. Ouellette EA, Dennis JJ, Milne EL, Latta LL, Makowski AL. Role of soft tissues in metacarpal fracture fixation. Clin Orthop Relat Res. 2003;(412):169-75.
In seeking to minimize these complications, we provide here the first description of the principle of an intramedullary internal tutor,99. Orbay JL, Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin. 2006;22(3): 279-86.,1010. Patankar H, Meman FW. Multiple intramedullary nailing of proximal phalangeal fractures of hand. Indian J Orthop. 2008;42(3):342-6.and1111. Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724-31. comprising use of a conical compression screw (Acutrak(r)) that was inserted percutaneously. This procedure presents the advantage of not interfering with the extensor tendon, so as to avoid tendon adherence and joint stiffness.
The objective of this study was to analyze the clinical and functional results from patients with a diagnosis of unstable reducible extra-articular fracturing of the proximal phalanx with displacement, who underwent surgical treatment by means of a minimally invasive percutaneous osteosynthesis technique using an Acutrak(r) screw in order to avoid interfering with the extensor tendon of this finger.
Materials and methods
Between January 2011 and September 2014, 41 patients with 48 fingers affected were attended and evaluated at the outpatient service of the hand and microsurgery group of our institution. A prospective study was conducted, which included all the patients who presented a diagnosis of unstable reducible fractures of the proximal phalanx of the fingers and who underwent physical examination and simple posteroanterior (PA) and oblique radiography on the hand and PA and lateral (L) radiography on the finger affected.
The inclusion criteria were that the patients needed to be adults aged 18-65 years, of either sex, with a clinical and imaging diagnosis of unstable reducible fractures of the proximal phalanx of the fingers, who had signed a free and informed consent statement and a protocol of conflicts of interest, as required by our institution's research ethics committee through CAAE number 12759813.4.0000.0082.
Patients were excluded if they had any associated diseases in the hand or any osteometabolic diseases, if they had undergone any previous surgical procedure on the hand, or if they presented any chronic conditions that affected the hands bilaterally.
The functional evaluation was performed by professionals within the hospital's occupational therapy sector for the hand. The clinical and functional measurements were made as percentages of the range-of-motion (ROM) measurements in degrees on the normal finger versus the affected finger, using a single specific goniometer. The clinical analysis on pain was done by means of a visual analog scale (VAS) from zero to 10, for a subjective evaluation.
Quality of life was evaluated by means of the DASH questionnaire (Annex 1 Anexo 1. DASH questionnaire in portuguese version. ), which is an instrument validated for assessing the upper limbs.
Radiographs of the consolidation of the fracture were evaluated subjectively by the medical team.
The patients underwent osteosynthesis of the phalangeal fracture, without interfering with the extensor tendon. All of the operations were performed by means of a percutaneous minimally invasive technique, with implantation of an Acutrak(r) screw, following the intramedullary tutor principle, in order to stabilize the fracture of the proximal phalange.
Operative technique for osteosynthesis using an Acutrak (r) screw
A percutaneous approach to the base of the proximal phalanx was used, comprising a 0.5 cm incision under the lateral face of the extensor tendon in its dorsal region, with a percutaneous minimal approach to the extensor hood affected. Closed reduction of the fracture of the proximal phalanx was then performed, with the aid of traction along the finder, while maintaining the proximal and distal interphalangeal joints. This reduction was done under indirect viewing, with the aid of radioscopy. A guidewire was then passed into the apex of the dorsal face of the phalange such that it crossed the fracture focus, going toward the distal and palmar region of the bone until it crossed this cortical bone, with preservation of the condyles. After this, the size of the implant was measured and the medullary canal was milled using a specific conical drill bit. The Acutrak(r) screw was then inserted into the intramedullary canal below the distal cortex, in the proximal region of the phalanx, next to the palmar cortex of this bone (Fig. 1). In this manner, compression and stabilization of the fracture focus became possible, with the aid of radioscopy, in order to maintain the screw in its ideal position. At the end of the procedure, suturing was performed in layers and postoperative radioscopy and radiography of the hand were performed for post-surgical assessment (Fig. 2 and Fig. 3).
View of the entry point of the screw at the dorsal base of the proximal phalanx, showing the preservation of the joint cartilage at the base of the proximal phalanx, in the metacarpophalangeal joint. Dissection of a cadaver.
Statistical analysis
We used Microsoft Excel electronic spreadsheets (version in Microsoft Office 2010) to organize the data and the Statistical Package for the Social Sciences (SPSS; IBM), version 22.0, to obtain the results. Values with p< 0.005 were taken to be statistically significant and a 95% confidence interval was used.
Central trend measurements were made (mean, minimum, maximum, standard deviation and percentiles) and these were then compared using Wilcoxon's signed rank test (Table 1), with the aim of checking for possible differences between continuous variables, for each variable of interest.
Results
All the patients maintained the reduction that had been achieved through the operation, along with their fracture consolidation.
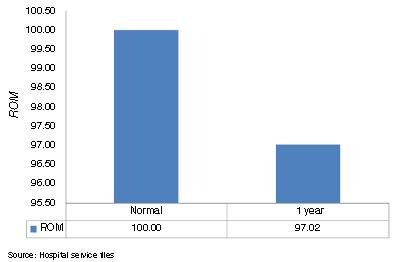
All of them presented improvement in their clinical and functional parameters and there were improvements in their results regarding the variables of range of motion (ROM) (Fig. 4), DASH (Disability of the Arm, Shoulder and Hand) score and visual analog scale (VAS) score (Table 2). All the patients achieved improved quality of life and returned to work, with significant decreases in their DASH questionnaire scores (Fig. 5). There was an improvement in pain, with decreases in their VAS scores (Fig. 6).
Comparison of the range of motion (ROM) variable between the normal and affected fingers (%). Source: Hospital service files.
Comparison of the DASH variable between the normal and affected sides. Source: Hospital service files.
Comparison of the VAS variable between the normal and affected sides. Source: Hospital service files.
In comparing the clinical and functional results with those of the unaffected side (range of motion, DASH and VAS), we observed that there was no statistically significant difference between the values analyzed, which showed that functional recovery of the fingers affected had been achieved.
The complication rate was 8.33%. Patient 4, with abrasive injuries to his fingers, presented postoperative infection, with exposure of the implant, which was removed after consolidation of the fracture. Patients 10, 15 and 32 evolved with pain in the middle phalanx, perhaps because of the great length of the screw. It was removed after the fracture had consolidated, and this improved the pain. The length of follow-up was 17 months, with a minimum of 12 and maximum of 36. The mean age was 30 years, with a minimum of 19 and maximum of 51.
Discussion
Evolution in treating fractures of the proximal phalanx is a necessity in our setting, not only because of the increasing incidence of these fractures here, but also because the results from conventional osteosynthesis methods are unconvincing.77. Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: preferred methods of stabilization. J Am Acad Orthop Surg. 2008;16(10):586-95.,88. Ouellette EA, Dennis JJ, Milne EL, Latta LL, Makowski AL. Role of soft tissues in metacarpal fracture fixation. Clin Orthop Relat Res. 2003;(412):169-75.,99. Orbay JL, Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin. 2006;22(3): 279-86.and1010. Patankar H, Meman FW. Multiple intramedullary nailing of proximal phalangeal fractures of hand. Indian J Orthop. 2008;42(3):342-6. The search for less invasive techniques has the aim of reaching procedures that act toward stabilizing the implant while enabling early mobilization of the finger with a low complication rate.1111. Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724-31.,1212. Ouellette EA, Dennis JJ, Milne EL, Latta LL, Makowski AL. The role of soft tissues in plate fixation of proximal phalanx fractures. Clin Orthop Relat Res. 2004;(418):213-8.,1313. Mantovani G, Fukushima WY, Cho AB, Aita MA, Lino W Jr, Faria FN. Alternative to the distal interphalangeal joint arthrodesis: lateral approach and plate fixation: biomechanical study. J Hand Surg Am. 2008;33(1):31-4.and1414. Wong H, Iam C, Wong K, Ip W, Fung K. Treatment of phalangeal and metacarpal fractures: a review. J Orthop. 2008;10(1):1-9.
For this purpose, a variety of means have been developed, such as the new 1.5 or 2 mm specific locking plates with a minimum thickness of 2 or 3 mm, in association with guiding tools and reducing tweezers that are extremely precise. The Acutrak(r) self-compressing screw, which was designed previously for treating scaphoid fractures and is now used for the proximal femur, the bones of the foot and ankle and even the proximal phalanges, under the intramedullary tutor principle, as described in this study, enables the proper stability that is needed for fractures of the proximal phalanx.
The percutaneous minimally invasive approach using a compression screw,1414. Wong H, Iam C, Wong K, Ip W, Fung K. Treatment of phalangeal and metacarpal fractures: a review. J Orthop. 2008;10(1):1-9.,1515. Kawamura K, Chung KC. Fixation choices for closed simple unstable oblique phalangeal and metacarpal fractures. Hand Clin. 2006;22(3):287-95.,1616. Yan YM, Zhang WP, Liao Y, Weng ZF, Ren WJ, Lin J, et al. Analysis and prevention of the complications after treatment of metacarpal and phalangeal fractures with internal fixation. Zhongguo Gu Shang. 2011;24(3):199-201.and1717. Itadera E, Oikawa Y, Shibayama M, Kobayashi T, Moriya H. Intramedullary fixation of proximal phalangeal fractures through a volar extra-tendon sheath approach. Hand Surg. 2011;16(2):141-7. under the internal tutor principle and without interfering with the extensor tendon, significantly diminishes the risk of adherence of the tendon to the implant. This can be explained by the fact that there is no contact between the extensor tendon and the implants. In this manner, there is less risk of joint stiffness in these fingers, since the method applied in this study is sufficiently stable to allow mobility of the metacarpophalangeal and interphalangeal joints as early as the immediate postoperative period. The deformities are minimal because of the ease of reducing the fracture and maintaining this over the course of the follow-up, when this method is applied.1616. Yan YM, Zhang WP, Liao Y, Weng ZF, Ren WJ, Lin J, et al. Analysis and prevention of the complications after treatment of metacarpal and phalangeal fractures with internal fixation. Zhongguo Gu Shang. 2011;24(3):199-201.,1717. Itadera E, Oikawa Y, Shibayama M, Kobayashi T, Moriya H. Intramedullary fixation of proximal phalangeal fractures through a volar extra-tendon sheath approach. Hand Surg. 2011;16(2):141-7.and1818. Held M, Jordaan P, Laubscher M, Singer M, Solomons M. Conservative treatment of fractures of the proximal phalanx: an option even for unstable fracture patterns. Hand Surg. 2013;18(2):229-34.
In analyzing the radiographic parameters, all the patients maintained the fracture reduction that was initially achieved. It was demonstrated that both of the implants used in this study are safe and stable and that they enable adequate bone consolidation.
In comparing the clinical and functional results horizontally with the unaffected side (range of motion, DASH and VAS), we observed that there were no statistically significant differences, which shows that functional recovery of the affected fingers was achieved.
Our clinical and functional results (ROM) were better than those obtained in the study by Itadera et al.,1717. Itadera E, Oikawa Y, Shibayama M, Kobayashi T, Moriya H. Intramedullary fixation of proximal phalangeal fractures through a volar extra-tendon sheath approach. Hand Surg. 2011;16(2):141-7. in which the patients were treated by means of a minimally invasive technique using intramedullary wires that did not produce anatomical reductions.
Held et al.1818. Held M, Jordaan P, Laubscher M, Singer M, Solomons M. Conservative treatment of fractures of the proximal phalanx: an option even for unstable fracture patterns. Hand Surg. 2013;18(2):229-34. used conservative treatment with a specific orthosis and found that 91% maintained the fracture reduction. In our study, we believe that surgical treatment was more effective, with results close to 100%, similar to other published studies.1111. Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724-31.,1212. Ouellette EA, Dennis JJ, Milne EL, Latta LL, Makowski AL. The role of soft tissues in plate fixation of proximal phalanx fractures. Clin Orthop Relat Res. 2004;(418):213-8.,1616. Yan YM, Zhang WP, Liao Y, Weng ZF, Ren WJ, Lin J, et al. Analysis and prevention of the complications after treatment of metacarpal and phalangeal fractures with internal fixation. Zhongguo Gu Shang. 2011;24(3):199-201.and1919. Zach A. Percutaneous fixation of transverse shaft fractures of the proximal phalanx with a new compression wire. J Hand Surg Eur. 2015;40(3):318-9.
With regard to evaluating the complications, the study by Yan et al.1616. Yan YM, Zhang WP, Liao Y, Weng ZF, Ren WJ, Lin J, et al. Analysis and prevention of the complications after treatment of metacarpal and phalangeal fractures with internal fixation. Zhongguo Gu Shang. 2011;24(3):199-201. showed worse functional results and a higher complication rate among patients treated using conventional techniques. Among the complications, edema, pseudarthrosis, joint stiffness and postoperative infection of the surgical site can be highlighted. This event was observed in 8.33% of the patients in our study, and it was treated through removal of the implant, serial dressings and antibiotic therapy, with improvement of the condition beyond the sixth postoperative week. According to the review study by Gaston and Chadderdon,2020. Gaston RG, Chadderdon C. Phalangeal fractures: displaced/nondisplaced. Hand Clin. 2012;28(3):395-401. the ideal surgical approach for unstable fractures of the proximal phalanx in athletes is minimally invasive treatment in association with implants with greater resistance, so as to enable mobility and an early return to sport. This concept was applied in the present study, which showed satisfactory results such as a DASH score of 3.56 and a complication rate of 8.33%.
A comparison between intra and extramedullary tutors was made in the study by Ozer et al.,1414. Wong H, Iam C, Wong K, Ip W, Fung K. Treatment of phalangeal and metacarpal fractures: a review. J Orthop. 2008;10(1):1-9. in treating diaphyseal fractures of the femur, tibia and humerus. They showed that milled nails (intramedullary tutors) in the femur and tibia were superior and presented lower complication rates.2121. Duan X, Li T, Mohammed AQ, Xiang Z. Reamed intramedullary nailing versus unreamed intramedullary nailing for shaft fracture of femur: a systematic literature review. Arch Orthop Trauma Surg. 2011;131(10):1445-52.and2222. Heineman DJ, Bhandari M, Nork SE, Ponsen KJ, Poolman RW. Treatment of humeral shaft fractures - meta- analysis reupdated. Acta Orthop. 2010;81(4):517. However, in relation to the humerus, conservative treatment and use of percutaneous bridging plates presented lower complication rates.2323. Duan X, Al-Qwbani M, Zeng Y, Zhang W, Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev. 2012;1:CD008241.
In this study, we sought to approach the diaphysis of the phalanx by means of a minimally invasive technique, in a manner similar to approaches used in relation to other bones, as described in the literature. In an analogous manner, we used a nail (the Acutrak(r) screw)2424. Ibanez DS, Rodrigues FL, Salviani RS, Roberto FAR, Pengo Junior JR, Aita MA. Ensaio experimental para tratamento cirúrgico das fraturas transversas da falange proximal - técnica com parafuso intramedular cônico de compressão versus placa de compressão lateral. Rev Bras Ortop. 2015;50(5):509-14. as an intramedullary tutor, in order to treat extra-articular fractures of the proximal phalanx.
We observed that the learning curve was short. This technique was safe and it adequately maintained the initial reduction of the fracture that had been achieved surgically, with satisfactory results and a low complication rate (8.33%).
Conclusion
The minimally invasive technique for treating unstable extra-articular fractures of the proximal phalanx using the Acutrak(r) screw was effective and safe, and it presented a low complication rate. The implants maintained adequate reduction of the fracture.
References
-
1Packer GJ, Shaheen MA. Patterns of hand fractures and dislocations in a district general hospital. J Hand Surg Br. 1993;18(4):511-4.
-
2Emmett JE, Breck LW. A review and analysis of 11,000 fractures seen in a private practice of orthopaedic surgery, 1937-1956. J Bone Joint Surg Am. 1958;40(5): 1169-75.
-
3de Jonge JJ, Kingma J, van der Lei B, Klasen HJ. Fractures of the metacarpals. A retrospective analysis of incidence and aetiology and a review of the English-language literature. Injury. 1994;25(6):365-9.
-
4Kamath JB, Harshvardhan Naik DM, Bansal A. Current concepts in managing fractures of metacarpal and phalanges. Indian J Plast Surg. 2011;44(2):203-11.
-
5Barton N. Internal fixation of hand fractures. J Hand Surg Br. 1989;14(2):139-42.
-
6Margic´ K. External fixation of closed metacarpal and phalangeal fractures of digits. A prospective study of one hundred consecutive patients. J Hand Surg Br. 2006;31(1):30-40.
-
7Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: preferred methods of stabilization. J Am Acad Orthop Surg. 2008;16(10):586-95.
-
8Ouellette EA, Dennis JJ, Milne EL, Latta LL, Makowski AL. Role of soft tissues in metacarpal fracture fixation. Clin Orthop Relat Res. 2003;(412):169-75.
-
9Orbay JL, Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin. 2006;22(3): 279-86.
-
10Patankar H, Meman FW. Multiple intramedullary nailing of proximal phalangeal fractures of hand. Indian J Orthop. 2008;42(3):342-6.
-
11Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724-31.
-
12Ouellette EA, Dennis JJ, Milne EL, Latta LL, Makowski AL. The role of soft tissues in plate fixation of proximal phalanx fractures. Clin Orthop Relat Res. 2004;(418):213-8.
-
13Mantovani G, Fukushima WY, Cho AB, Aita MA, Lino W Jr, Faria FN. Alternative to the distal interphalangeal joint arthrodesis: lateral approach and plate fixation: biomechanical study. J Hand Surg Am. 2008;33(1):31-4.
-
14Wong H, Iam C, Wong K, Ip W, Fung K. Treatment of phalangeal and metacarpal fractures: a review. J Orthop. 2008;10(1):1-9.
-
15Kawamura K, Chung KC. Fixation choices for closed simple unstable oblique phalangeal and metacarpal fractures. Hand Clin. 2006;22(3):287-95.
-
16Yan YM, Zhang WP, Liao Y, Weng ZF, Ren WJ, Lin J, et al. Analysis and prevention of the complications after treatment of metacarpal and phalangeal fractures with internal fixation. Zhongguo Gu Shang. 2011;24(3):199-201.
-
17Itadera E, Oikawa Y, Shibayama M, Kobayashi T, Moriya H. Intramedullary fixation of proximal phalangeal fractures through a volar extra-tendon sheath approach. Hand Surg. 2011;16(2):141-7.
-
18Held M, Jordaan P, Laubscher M, Singer M, Solomons M. Conservative treatment of fractures of the proximal phalanx: an option even for unstable fracture patterns. Hand Surg. 2013;18(2):229-34.
-
19Zach A. Percutaneous fixation of transverse shaft fractures of the proximal phalanx with a new compression wire. J Hand Surg Eur. 2015;40(3):318-9.
-
20Gaston RG, Chadderdon C. Phalangeal fractures: displaced/nondisplaced. Hand Clin. 2012;28(3):395-401.
-
21Duan X, Li T, Mohammed AQ, Xiang Z. Reamed intramedullary nailing versus unreamed intramedullary nailing for shaft fracture of femur: a systematic literature review. Arch Orthop Trauma Surg. 2011;131(10):1445-52.
-
22Heineman DJ, Bhandari M, Nork SE, Ponsen KJ, Poolman RW. Treatment of humeral shaft fractures - meta- analysis reupdated. Acta Orthop. 2010;81(4):517.
-
23Duan X, Al-Qwbani M, Zeng Y, Zhang W, Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev. 2012;1:CD008241.
-
24Ibanez DS, Rodrigues FL, Salviani RS, Roberto FAR, Pengo Junior JR, Aita MA. Ensaio experimental para tratamento cirúrgico das fraturas transversas da falange proximal - técnica com parafuso intramedular cônico de compressão versus placa de compressão lateral. Rev Bras Ortop. 2015;50(5):509-14.
-
☆
Work performed in the Discipline of Orthopedics and Hand Surgery, Faculdade de Medicina do ABC (FMABC), Santo André, SP, Brazil.
Anexo 1. DASH questionnaire in portuguese version.

Publication Dates
-
Publication in this collection
jan-feb 2016
History
-
Received
21 Sept 2014 -
Accepted
15 Dec 2014