Abstracts
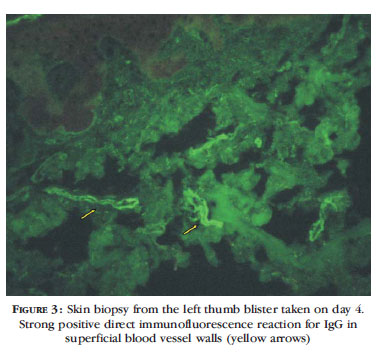
Blister formation and eccrine sweat gland necrosis is a cutaneous manifestation associated with states of impaired consciousness, most frequently reported after overdoses of central nervous system depressants, particularly phenobarbital. The case of a 45-year-old woman who developed "coma blisters" at six distinct anatomic sites after confirmed (laboratory) phenobarbital poisoning, associated with other central nervous system depressants (clonazepam, promethazine, oxcarbazepine and quetiapine), is presented. A biopsy from the left thumb blister taken on day 4 revealed focal necrosis of the epidermis and necrosis of sweat gland epithelial cells; direct immunofluorescence was strongly positive for IgG in superficial blood vessel walls but negative for IgM, IgA, C3 and C1q. The patient was discharged on day 21 with no sequelae.
Coma; Fluorescent antibody technique; Microscopy, fluorescence; Phenobarbital; Toxicology
Formação de bolhas e necrose de glândula sudoríparas écrinas é uma manifestação cutânea associada com estados de diminuição da consciência, mais frequentemente relatada após superdosagens de depressores do sistema nervoso central, particularmente fenobabital. Relatamos o caso de uma paciente de 45 anos que desenvolveu "bolhas do coma" após tentativa de suicídio por fenobarbital (confirmada laboratorialmente), associada a outros depressores do sistema nervoso central (clonazepam, prometazina, oxcarbazepina e quetiapina). Biópsia da bolha do 1o quirodáctilo esquerdo no 4o dia de internação revelou necrose focal da epiderme e necrose de células epiteliais de glândula sudorípara; a imunofluorescência direta foi fortemente positiva para IgG na parede superficial dos vasos sanguíneos, mas negativa para IgM, IgA, C3 e C1q. A paciente teve alta no 21o dia, sem seqüelas.
Coma; Fenobarbital; Imunofluorescência; Microscopia de fluorescência; Toxicologia
CASE REPORT
Coma blisters after poisoning caused by central nervous system depressants: case report including histopathological findings* * This study was carried out at the UNICAMP Poison Control Center and the Departments of Dermatology and Pathology, School of Medical Sciences, UNICAMP - Campinas (SP), Brazil.
Bolhas do coma pós-intoxicação por depressores do sistema nervoso central: relato de caso incluindo achados histopatológicos
Maira Migliari BrancoI; Eduardo Mello De CapitaniII; Maria Letícia CintraIII; Stephen HyslopIV; Adriana Camargo CarvalhoV; Fabio BucaretchiVI
IResidency in Pediatrics - Physician at the Campinas Poison Control Center of the Medical Science School, State University of Campinas (Centro de Controle de Intoxicações da Faculdade de Ciências Médicas da Universidade Estadual de Campinas - FCM-UNICAMP) - Campinas (SP), Brazil
IIPhD - Associate Professor of the Department of Internal Medicine and of the Campinas Poison Control Center of the Medical Science School, State University of Campinas (Centro de Controle de Intoxicações da Faculdade de Ciências Médicas da Universidade Estadual de Campinas - FCM-UNICAMP) - Campinas (SP), Brazil
IIIPhD - Assistant Professor of the Department of Anatomical Pathology of the Medical Science School, State University of Campinas (Centro de Controle de Intoxicações da Faculdade de Ciências Médicas da Universidade Estadual de Campinas - FCM-UNICAMP) - Campinas (SP), Brazil
IVPhD - Assistant Professor of the Department of Pharmacology of the Medical Science School, State University of Campinas (Faculdade de Ciências Médicas da Universidade Estadual de Campinas - FCM-UNICAMP) - Campinas (SP), Brazil
VMaster's degree - Nurse at the Clinical Skills Laboratory of the Medical Science School, State University of Campinas (Faculdade de Ciências Médicas da Universidade Estadual de Campinas - FCM-UNICAMP) - Campinas (SP), Brazil
VIhD - Assistant Professor of the Department of Pediatrics and of the Campinas Poison Control Center of the Medical Science School, State University of Campinas (Centro de Controle de Intoxicações da Faculdade de Ciências Médicas da Universidade Estadual de Campinas - FCM-UNICAMP) - Campinas (SP), Brazil
Mailing address Mailing address: Maira Migliari Branco Rua Carlos Chagas, 150 13083-970 Campinas, SP E-mail: mairinha_branco@hotmail.com
ABSTRACT
Blister formation and eccrine sweat gland necrosis is a cutaneous manifestation associated with states of impaired consciousness, most frequently reported after overdoses of central nervous system depressants, particularly phenobarbital. The case of a 45-year-old woman who developed "coma blisters" at six distinct anatomic sites after confirmed (laboratory) phenobarbital poisoning, associated with other central nervous system depressants (clonazepam, promethazine, oxcarbazepine and quetiapine), is presented. A biopsy from the left thumb blister taken on day 4 revealed focal necrosis of the epidermis and necrosis of sweat gland epithelial cells; direct immunofluorescence was strongly positive for IgG in superficial blood vessel walls but negative for IgM, IgA, C3 and C1q. The patient was discharged on day 21 with no sequelae.
Keywords: Coma; Fluorescent antibody technique; Microscopy, fluorescence; Phenobarbital; Toxicology
RESUMO
Formação de bolhas e necrose de glândula sudoríparas écrinas é uma manifestação cutânea associada com estados de diminuição da consciência, mais frequentemente relatada após superdosagens de depressores do sistema nervoso central, particularmente fenobabital. Relatamos o caso de uma paciente de 45 anos que desenvolveu "bolhas do coma" após tentativa de suicídio por fenobarbital (confirmada laboratorialmente), associada a outros depressores do sistema nervoso central (clonazepam, prometazina, oxcarbazepina e quetiapina). Biópsia da bolha do 1o quirodáctilo esquerdo no 4o dia de internação revelou necrose focal da epiderme e necrose de células epiteliais de glândula sudorípara; a imunofluorescência direta foi fortemente positiva para IgG na parede superficial dos vasos sanguíneos, mas negativa para IgM, IgA, C3 e C1q. A paciente teve alta no 21o dia, sem seqüelas.
Palavras-chave: Coma; Fenobarbital; Imunofluorescência; Microscopia de fluorescência; Toxicologia
INTRODUCTION
Blister formation and eccrine sweat gland necrosis is an infrequent cutaneous manifestation associated with states of impaired consciousness, most frequently reported after overdoses of central nervous system (CNS) depressants, particularly phenobarbital.1-7 In general, lesions are few in number, are predominantly found on skin overlying the bony prominences, appear within 24 h and resolve within 10-14 days.6 More rarely, blister formation and eccrine sweat gland necrosis have also been described in non-comatose patients.8,9 Reviewing the literature, no previous reports of similar cases have been reported in Brazil. Therefore, we describe one more case of druginduced coma blisters, with histopathological and immunofluorescence findings.
CASE REPORT
A 45-year-old woman was found unresponsive at home by family members. Tablets of her current medications (clonazepam, promethazine, oxcarbazepine, quetiapine and phenobarbital) were found beside her. She was admitted to the local Emergency Department with a Glasgow coma scale of 5, bilateral myosis, HR = 98 bpm, and BP = 90/50 mmHg; initial procedures included endotracheal intubation, gastric lavage and a single dose of activated charcoal. The patient was subsequently referred to the university hospital, where the presence of bullous lesions over the right knee and left thumb was noticed (Figure 1). Laboratory results at admission revealed a plasma phenobarbital level of 63 µg/dL (by polarized immunofluorescence; reference value= 10-25 µg/dL) and a serum total CK level of 3,581 U/L (reference value < 145 U/L); the serum levels of the other medications were not quantified. Since these findings indicated mild rhabdomyolysis and phenobarbital poisoning, the patient was treated with fluids replacement, multiple doses of activated charcoal and urinary alkalinization. During evolution, four new blisters with the same characteristics as those on the knee and thumb were noted (one each on the left hand, left shoulder, right lower-arm and right foot).
A biopsy from the left thumb blister taken on day 4 revealed focal necrosis of the epidermis, a subepidermal blister partially filled with fibrin, and necrosis of sweat gland epithelial cells (Figure 2). Direct immunofluorescence was strongly positive for IgG in superficial blood vessel walls but was negative for IgM, IgA, C3 and C1q (Figure 3).
The patient remained on mechanical ventilation for 12 days and was discharged on day 21, with no sequelae. At discharge, she confirmed the inten-tional ingestion of an overdose of all her current medications.
DISCUSSION
Coma blisters are not so uncommon after barbiturates overdose; in a large case series, such lesions were noted in 6.5% of 290 patients who suffered acute barbiturate poisoning, within as early as 4h postingestion.1 The most significant structural changes have been identified in eccrine sweat glands and ducts, which may show partial or total necrosis, even in early lesions, with little or no epidermal changes, as herein reported.3,5,6
The pathogenesis of coma blisters remains unclear, and their distribution cannot be explained simply by pressure effects in comatose patients.5 According to Sánchez et al (1993), vascular changes correlate proportionately with epidermal damage and consist of a neutrophilic inflammatory infiltrate and blood vessel wall damage, mainly involving arterioles.5 In addition, hypotension, hypoxia, direct local toxic effects and autonomic instabilities may also contribute to blister formation and sweat gland necrosis.4,5,6
The immunofluorescence findings in cutaneous lesions of drug-induced coma have rarely been studied.3,5,10 Patchy intercellular staining for IgG, IgA and C3 and deposits of IgM and C3 in dermal vessel walls and epidermal keratinocytes have already been described.3,5,10 The interpretation of direct immunofluorescence results in these cases remains controversial, particularly because they may reflect a nonspecific interaction rather than a direct
immune-mediated pathogenic mechanism. Since the epidermis is the last cutaneous epithelium to suffer necrosis, and since dermal inflammation and blood vessel wall damage correlate with epidermal damage, the vascular involvement in these cases is probably more a consequence than a causative factor of the cutaneous lesions. 5
In conclusion, poisoning by CNS depressants, particularly phenobarbital, should always be considered as a possible etiologic agent in comatose patients who develop bullous lesions.
Received on 11.04.2011.
Approved by the Advisory Board and accepted for publication on 01.06.2011.
Conflict of interest: None
Financial funding: None
- 1. Beveridge GW, Lawson AAH. Occurrence of bullous lesions in acute barbiturate intoxication. Br Med J. 1965;1:835-7.
- 2. Matthew H. Barbiturates. Clin Toxicol. 1975;8:495-513.
- 3. Rocamora A, Matarredona J, Sendagorta E, Ledo A. Sweat gland necrosis in druginduced coma: a light and direct immunofluorescence study. J Dermatol. 1986;13:49-53.
- 4. Dunn C, Held JL, Spitz J, Silvers DN, Grossman ME, Kohn SR. Coma blisters: report and review. Cutis. 1990;45:423-6.
- 5. Sanchéz Yus R, Requena L, Simón P, Hospital M. Histopathology of cutaneous changes in drug-induced coma. Am J Dermatopathol. 1993;15:208-16.
- 6. Setterfeld JF, Robinson R, MacDonald D, Calonje E. Coma-induced bullae and sweat gland necrosis following clobazam. Clin Exp Dermatol. 2000;25:215-8.
- 7. Basu A, Brown S, Kirkham N, Ramesk V, Leech S, Devli A. Coma blisters in 2 children on anticonvulsivant medication. J Child Neurol. 2009;24:1021-5.
- 8. Ferrel C, Sullica VI, Aste N, Atzori L, Pinna M, Biggio P. Drug-induced sweat gland necrosis in a non-comatose patient: a case presentation. J Eur Acad Dermatol Venereol. 2003;17:443-5.
- 9. Piede J, Wallace E. Coma bullae: associations beyond medications. Mayo Clin Proc. 2011;86:e5.
- 10. Reilly GD, Harrington CI. Positive immunofluorescence in bullous lesions in druginduced coma. Br J Dermatol. 1983;109:720.
Publication Dates
-
Publication in this collection
10 Aug 2012 -
Date of issue
Aug 2012
History
-
Received
11 Apr 2011 -
Accepted
01 June 2011