Abstract
Cyclophosphamide is an alkylating agent widely used for the treatment of malignant neoplasia and which can be used in the treatment of multiple rheumatic diseases. Medication administration errors may lead to its reduced efficacy or increased drug toxicity. Many errors occur in the administration of injectable drugs. The present study aimed at structuring a routine for cyclophosphamide use, as well as creating a document with pharmacotherapeutic guidelines for the patient. The routine is schematized in three phases: pre-chemotherapy, administration of cyclophosphamide, and post-chemotherapy, taking into account the drugs to be administered before and after cyclophosphamide in order to prevent adverse effects, including nausea and hemorrhagic cystitis. Adverse reactions can alter laboratory tests; thus, this routine included clinical management for changes in white blood cells, platelets, neutrophils, and sodium, including cyclophosphamide dose adjustment in the case of kidney disease. Cyclophosphamide is responsible for other rare - but serious - side effects, for instance, hepatotoxicity, severe hyponatremia and heart failure. Other adverse reactions include hair loss, amenorrhea and menopause. In this routine, we also entered guidelines to post-chemotherapy patients. The compatibility of injectable drugs with the vehicle used has been described, as well as stability and infusion times. The routine aimed at the rational use of cyclophosphamide, with prevention of adverse events and relapse episodes, factors that may burden the health care system.
Keywords:
Cyclophosphamide; Antiemetics; Chemotherapy; Cystitis
Resumo
A ciclofosfamida (CFM) é um agente alquilante vastamente usado para o tratamento de neoplasias malignas e pode ser usado no tratamento de diversas doenças reumatológicas. O erro de administração de medicamentos pode levar à diminuição da eficácia ou ao aumento da toxicidade medicamentosa. Diversos erros ocorrem na administração de medicamentos injetáveis. O trabalho objetivou a estruturação de uma rotina do uso de ciclofosfamida, bem como a criação de um documento de orientações farmacoterapêuticas para o paciente. A rotina foi esquematizada em três fases, a pré-quimioterapia (pré-QT), a administração da ciclofosfamida e a pós-quimioterapia (pós-QT), que levaram em consideração os medicamentos que devem ser administrados antes e depois da ciclofosfamida para prevenção aos efeitos adversos, incluindo náusea e cistite hemorrágica. As reações adversas podem alterar os exames laboratoriais e a rotina incluiu manejo clínico para alteração clínica dos leucócitos, das plaquetas, dos neutrófilos e do sódio incluindo o ajuste de dose de ciclofosfamida em caso de insuficiência renal. A ciclofosfamida é responsável por outras reações adversas raras, mas sérias, como hepatotoxicidade, hiponatremia severa e falência cardíaca. Outras reações adversas incluem perda de cabelo, amenorreia e menopausa. A rotina foi composta também por orientações ao paciente pós-QT. A compatibilidade dos medicamentos injetáveis com o veículo foi descrita, bem como o tempo de estabilidade e o tempo de infusão. A rotina visou ao uso racional da ciclofosfamida e prevenir os efeitos adversos e os episódios de recidiva, os quais podem onerar o sistema de saúde.
Palavras-chave:
Ciclofosfamida; Antieméticos; Quimioterapia; Cistite
Introduction
Cyclophosphamide (CPM) is an alkylating agent widely used for the treatment of malignancies such as breast cancer,11 Burkard ME, Wisinski KB, Njiaju UO, Donohue S, Hegeman R, Stella A, et al. Feasibility of 4 cycles of docetaxel and cyclophosphamide every 14 days as an adjuvant regimen for breast cancer: a Wisconsin Oncology Network study. Clin Breast Cancer. 2014;14:205-11. multiple myeloma,22 Huang BT, Tan Y, Zhao WH, Zeng QC, Li BS, Chen RL. How to determine bortezomib-based regimen for elderly patients with multiple myeloma: PAD versus CBd, an observational study. J Cancer Res Clin Oncol. 2014;140:303-9. renal diseases including nephrotic syndrome refractory to corticosteroid and focal segmental glomerulonephritis, and this drug can be used in the treatment of multiple rheumatic diseases,33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9.
4 Munyangango EM, Le Roux-Villet C, Doan S, Pascal F, Soued I, Alexandre M, et al. Oral cyclophosphamide without corticosteroids to treat mucous membrane pemphigoid. Br J Dermatol. 2013;168:381-90.-55 Mota LM, Cruz BA, Brenol CV, Pereira IA, Rezende-Fronza LS, Bertolo MB, et al. Consenso 2012 da Sociedade Brasileira de Reumatologia para o tratamento da artrite reumatoide. Rev Bras Reumatol. 2012;52:152-74. including cicatricial pemphigoid (also called pemphigoid mucous membrane),44 Munyangango EM, Le Roux-Villet C, Doan S, Pascal F, Soued I, Alexandre M, et al. Oral cyclophosphamide without corticosteroids to treat mucous membrane pemphigoid. Br J Dermatol. 2013;168:381-90. rheumatoid arthritis,55 Mota LM, Cruz BA, Brenol CV, Pereira IA, Rezende-Fronza LS, Bertolo MB, et al. Consenso 2012 da Sociedade Brasileira de Reumatologia para o tratamento da artrite reumatoide. Rev Bras Reumatol. 2012;52:152-74. juvenile dermatomyositis,66 Rosa Neto NS, Goldenstein-Schainberg C. Dermatomiosite juvenil: revisão e atualização em patogênese e tratamento. Rev Bras Reumatol. 2010;503:299-312. systemic sclerosis,77 Broad K, Pope JE. The efficacy of treatment for systemic sclerosis interstitial lung disease: results from a meta-analysis. Med Sci Monit. 2010;16:RA187-90.,88 Appenzeller S, Sampaio-Barros PD, Samara AM, Marques Neto JF. Crise renal como manifestação inicial de esclerose sistêmica sine scleroderma. Rev Bras Reumatol. 2004;44:87-9. interstitial lung disease,77 Broad K, Pope JE. The efficacy of treatment for systemic sclerosis interstitial lung disease: results from a meta-analysis. Med Sci Monit. 2010;16:RA187-90. lupus vasculopathy,99 Chu H, Wu LH, Song D, Yu F, Zhao MH. Noninflammatory necrotizing vasculopathy in lupus nephritis: a single-center experience. Lupus. 2014;23:20-30. systemic vasculitis, and refractory treatment of lupus-associated thrombocytopenic purpura.1010 Campos LM, Spadoni MS, Michelin CM, Jesus AA, Carneiro JD, da Silva CA. Thrombotic thrombocytopenic purpura at presentation of juvenile systemic lupus erythematosus patients. Rev Bras Reumatol. 2013;53:120-6. In addition to other indications of cyclophosphamide, the treatment of neuromyelitis optica can also be included.1111 Yaguchi H, Sakushima K, Takahashi I, Nishimura H, Yashima-Yamada M, Nakamura M, et al. Efficacy of intravenous cyclophosphamide therapy for neuromyelitis optica spectrum disorder. Intern Med. 2013;52:969-72.
In children, cyclophosphamide may be used in the treatment of nephrotic syndrome and systemic lupus erythematosus.1212 Hobbs DJ, Barletta GM, Rajpal JS, Rajpal MN, Weismantel DP, Birmingham JD, et al. Severe paediatric systemic lupus erythematosus nephritis - a single-centre experience. Nephrol Dial Transplant. 2010;25:457-63.,1313 Lehman TJ, Singh C, Ramanathan A, Alperin R, Adams A, Barinstein L, et al. Prolonged improvement of childhood onset systemic lupus erythematosus following systematic administration of rituximab and cyclophosphamide. Pediatri Rheumatol Online J. 2014;12:3.
Cyclophosphamide can be administered by oral or intravenous route.1414 Suarez-Almazor ME, Belseck E, Shea B, Wells G, Tugwell P. Cyclophosphamide for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2000;:CD001157. The intravenous administration is more frequent in the field of rheumatology, taking into account studies showing an efficacy similar to that of oral treatment, but with less toxicity, for example, a decrease in premature ovarian failure, less severe infection, and lower overall exposure of the urinary tract to acrolein, a toxic metabolite of cyclophosphamide.1515 Cox PJ. Cyclophosphamide cystitis - identification of acrolein as the causative agent. Biochem Pharmacol. 1979;28:2045-9. Cyclophosphamide is orally administered QD (24-24 h), while the intravenous route is administered in pulses, and the dose is adjusted according to hematologic and renal toxicities.1616 Mavragani CP, Moutsopoulos HM. Lupus nephritis: current issues. Ann Rheum Dis. 2003;62:795-8.
The administration of cyclophosphamide in pulses may follow a weekly or monthly basis, in combination with a corticosteroid and other chemotherapeutic agents, provided that the attending physician takes into account the minimum blood count (NADIR) for the administration of cyclophosphamide.1616 Mavragani CP, Moutsopoulos HM. Lupus nephritis: current issues. Ann Rheum Dis. 2003;62:795-8.
17 Dupuis LL, Boodhan S, Holdsworth M, Robinson PD, Hain R, Portwine C, et al. Guideline for the prevention of acute nausea and vomiting due to antineoplastic medication in pediatric cancer patients. Pediatr Blood Cancer. 2013;60:1073-82.-1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. Cyclophosphamide may cause some adverse events, and when these effects are related to the drug, are classified as an adverse drug reaction.1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
The adverse drug reaction can be conceptualized as an unintended and harmful reaction into the body, occurring in those routinely used doses in humans for prophylaxis, diagnosis, disease therapy, or for changes of physiological functions.1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
A reaction that occurs in a small percentage of the population, but that, if not avoided, may cause irreversible damage to the patient, such as death, congenital abnormalities, birth defects or conditions that require permanent hospitalization, is classified as "severe reaction".1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
Some adverse reactions related to the administration of cyclophosphamide are bone marrow suppression, susceptibility to infections, sterility and amenorrhea,1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. as well as nephrotoxicity and cystitis,1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67.,1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
and also cardiovascular complications, for instance, sinus bradycardia, pericarditis, myocarditis and heart failure.2020 Lotan E, Leader A, Lishner M, Gottfried M, Pereg D. Unrecognized renal insufficiency and chemotherapy associated adverse effects among breast cancer patients. Anticancer Drugs. 2012;23:991-5. Children and adolescents treated with high doses of cyclophosphamide are more likely to develop dental disorders and a decreased salivary flow. Cyclophosphamide is also teratogenic.2121 Hsieh SG, Hibbert S, Shaw P, Ahern V, Arora M. Association of cyclophosphamide use with dental developmental defects and salivary gland dysfunction in recipients of childhood antineoplastic therapy. Cancer. 2011;117:2219-27. A long term reaction of cyclophosphamide is malignacies.1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. One can observe an increase in the incidence of bladder cancer and esophageal and lung adenocarcionoma, which customarily occur after two years of treatment.1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67.
In addition to adverse drug reactions of cyclophosphamide, it is critical that the physician adopt all precautionary measures, because these adverse reactions may be more important in cases where cyclophosphamide is administered intravenously, given that, with this route of administration, the drug is not absorbed, the onset of its action is faster and, because the drug does not undergo first-pass metabolism, the bioavailability, i.e. the bioavailable concentration to exert a pharmacological action, becomes proportionally higher versus oral administration of cyclophosphamide.2222 Andrade ED. Terapêutica medicamentosa em odontologia: procedimentos clínicos e uso de medicamentos nas principais situações da prática odontológica. São Paulo: Artes Médicas; 1998.,2323 Fuchs FD, Wannamacher L. Farmacologia clínica: fundamentos da terapêutica racional. Rio de Janeiro: Guanabara Koogan; 1992. Another important aspect to consider concerns the errors associated with the administration of injectable drugs.2424 Wannmacher L. Erros: evitar o evitável. Uso racional de medicmanetos: tema selecionados, vol. 2; 2005. p. 1–6. Available at: http://www.saudedireta.com.br/docsupload/1284734732novo_erro_medico.pdf [accessed 08.08.14].
http://www.saudedireta.com.br/docsupload...
It is known that the use of injections is often associated with medication errors classified as serious events.2222 Andrade ED. Terapêutica medicamentosa em odontologia: procedimentos clínicos e uso de medicamentos nas principais situações da prática odontológica. São Paulo: Artes Médicas; 1998. Intravenous-route administration errors represent 21.1% of all errors, with possible risk of errors of contamination, administration rate, and dilution.2525 Melo LR, Pedreira MLG. Erros de medicação em pediatria: análise da documentação de enfermagem no prontuário do paciente. Rev Bras Enferm. 2005;58:180-5. Such parenteral drug administration errors, especially those by intravenous route, can cause an adverse drug reaction.1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
In addition to health-related problems, it is required that the costs resulting from drug administration errors are taken into account. In Brazil, it is estimated that the annual cost with the use of chemotherapeutic drugs exceed 1.1 billion reais, and this value can increase in cases of injectable drug administration errors.2424 Wannmacher L. Erros: evitar o evitável. Uso racional de medicmanetos: tema selecionados, vol. 2; 2005. p. 1–6. Available at: http://www.saudedireta.com.br/docsupload/1284734732novo_erro_medico.pdf [accessed 08.08.14].
http://www.saudedireta.com.br/docsupload...
Thus, one must bear in mind that these costs may be magnified by the occurrence of adverse events.2626 Allué N, Chiarello P, Bernal Delgado E, Castells X, Giraldo P, Martínez N, et al. Impacto económico de los eventos adversos en los hospitales españoles a partir del Conjunto Mínimo Básico de Datos. Gac Sanit. 2014;28:48-54. An adverse event is any untoward medical occurrence that affects the patient being medicated, but without a direct causal relationship with his/her treatment.1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
Thus, it is important to standardize the administration of parenteral drugs and provide their rational use, which can be defined as the patient's need to receive the appropriate drug in the correct dosage for an adequate length of time and with the lowest cost.2727 Medeiros EFF, Moraes CF, Karnikowski M, Nóbrega OT, Karnikowski MGdO. Intervenção interdisciplinar enquanto estratégia para o Uso Racional de Medicamentos em idosos. Ciênc Saúde Coletiva. 2011;16:3139-49.
Taking into account the rational use of drugs, it is important to standardize rules for the parenteral administration of cyclophosphamide. The objectives of this study are proposing a cyclophosphamide administration routine in Rheumatology units, and the creation of a document containing pharmacotherapeutic guidelines for the patient, in order to maximize the efficiency of treatment based on a literature review.
Methods
Cyclophosphamide routine
An infusion routine for cyclophosphamide was developed in order to increase the bioavailability (effectiveness) of this drug while minimizing adverse reactions, thus rendering the treatment more tolerable for the patient. The protocol was divided into stages to facilitate the comprehension of the health staff and the replication of the cyclophosphamide dosing schedule. The drugs of the first (pre-ChT) and third (post-ChT) steps correspond to the administration of pharmaceuticals in order to prevent the main adverse reactions resulting from the administration of cyclophosphamide (second phase), including nausea, vomiting, and hemorrhagic cystitis. The clinical management of adverse reactions that change laboratory tests was described, as well as the clinical management of cyclophosphamide in renal failure. The rare, but serious, adverse reactions were also highlighted.
The most common adverse reactions were emphasized so that the attending physician could provide guidance with respect to the main care that the patient should take in his/her home, after administration of cyclophosphamide. These precautions are essential to prevent or minimize adverse effects and increase treatment adherence.
In addition, the compatibility of these injectable drugs with the vehicle, stability time, and infusion time was ascertained. The sequence of administration of these drugs has been prepared in order to increase the efficacy of cyclophosphamide and diminish the onset of adverse reactions to the drugs administered.
Results
The routine administration of cyclophosphamide was developed in three phases: pre-ChT, cyclophosphamide administration, and post-ChT. With a view to the prevention of hemorrhagic cystitis, intravenous hydration with a blood volume expander (a crystalloid: 0.9% saline) was standardized.2828 Schuchter LM, Hensley ML, Meropol NJ, Winer EP. Update of recommendations for the use of chemotherapy and radiotherapy protectants: clinical practice guidelines of the American Society of Clinical Oncology, Chemotherapy, and Radiotherapy. J Clin Oncol. 2002;20:2895-903. In addition, the drug administration sequence, the amount of diluent, the need (or otherwise) for dilution, infusion and administration times, and laboratory tests which should be monitored before and after the infusion of cyclophosphamide were indicated, as well as the guidelines to the patient.
Fig. 133 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9.,55 Mota LM, Cruz BA, Brenol CV, Pereira IA, Rezende-Fronza LS, Bertolo MB, et al. Consenso 2012 da Sociedade Brasileira de Reumatologia para o tratamento da artrite reumatoide. Rev Bras Reumatol. 2012;52:152-74.,2020 Lotan E, Leader A, Lishner M, Gottfried M, Pereg D. Unrecognized renal insufficiency and chemotherapy associated adverse effects among breast cancer patients. Anticancer Drugs. 2012;23:991-5.,2929 Shepherd JD, Pringle LE, Barnett MJ, Klingemann HG, Reece DE, Phillips GL. Mesna versus hyperhydration for the prevention of cyclophosphamide-induced hemorrhagic cystitis in bone marrow transplantation. J Clin Oncol. 1991;9:2016-20.
30 Hawthorn J, Cunningham D. Dexamethasone can potentiate the anti-emetic action of a 5HT3 receptor antagonist on cyclophosphamide induced vomiting in the ferret. Br J Cancer. 1990;61:56-60.
31 Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143-50.
32 Turner N, Stewart J, Barnett F, White S. Syndrome of inappropriate anti-diuretic hormone secretion secondary to carboplatin after docetaxel-carboplatin-trastuzumab combination for early stage HER-2 positive breast cancer. Asia Pac J Clin Oncol. 2012;8:e9-11.
33 Trissel LA. Handbook on injectable drugs. 17th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2013.
34 Haubitz M, Bohnenstengel F, Brunkhorst R, Schwab M, Hofmann U, Busse D. Cyclophosphamide pharmacokinetics and dose requirements in patients with renal insufficiency. Kidney Int. 2002;61:1495-501.
35 Mardegan LC, Soledade C, Sachetto Z, Bertolo MB, Amstalden EMI, Sâmara AM, et al. Síndrome de Churg Strauss: uma vasculite rara. Rev Bras Reumatol. 2004;44:179-84.
36 Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs. 2011;22:468-72.
37 Salido M, Macarron P, Hernandez-Garcia C, D'Cruz DP, Khamashta MA, Hughes GR. Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus. Lupus. 2003;12:636-9.
38 Calixto-Lima L, Martins de Andrade E, Gomes AP, Geller M, Siqueira-Batista R. Dietetic management in gastrointestinal complications from antimalignant chemotherapy. Nutr Hosp. 2012;27:65-75.
39 Zahn KL, Wong G, Bedrick EJ, Poston DG, Schroeder TM, Bauman JE. Relationship of protein and calorie intake to the severity of oral mucositis in patients with head and neck cancer receiving radiation therapy. Head Neck. 2012;34:655-62.
40 Milman N. Anemia - still a major health problem in many parts of the world!. Ann Hematol. 2011;90:369-77.
41 McDermid JM, Lönnerdal B. Iron Adv Nutr. 2012;3:532-3.-4242 Centro de Oncologia Unimed Birigui. Cuidados com o paciente em quimioterapia. Available at: http://www.unimedbirigui.net.br/oncologia/downloads/manual_cuidados_com_o_paciente_em_puimioterapia.pdf [acessed 08.08.14].
http://www.unimedbirigui.net.br/oncologi...
, lists the routine data, and Fig. 2
4444 Instituto Estadual de Hematologia Arthur de Siqueira Cavalcanti (Hemorio). Rio de Janeiro: Manual do paciente em quimioterapia; 2006. Available at: http://www.hemorio.rj.gov.br/Html/pdf/Manuais/quimioterapia.pdf [accessed 08.08.14].
http://www.hemorio.rj.gov.br/Html/pdf/Ma...
45 Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5.
46 González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6.
47 Otero López MJ. Errores de medicación y gestión de riesgos. Rev Esp Salud Pública. 2003;77:527-40.
48 Medeiros-Souza P, Santos-Neto L, Kusano LTE, Pereira MG. Diagnosis and control of polypharmacy in the elderly. Rev Saúde Pública. 2007;41:1049-53.
49 Mesna. In: UpToDate Inc. [base de dados da Internet]. Waltham, (MA); 2013. Available at: http://www.uptodate.com [accessed 01.07.14]. Requer assinatura.
http://www.uptodate.com...
-5050 Taketomo CK, Hodding JH, Kraus DM. Pediatric dosage jandbook. Cleveland: Lexi-Comp Inc.; 1992. describes the guidelines for the patient. Severe and uncommon adverse reactions which should be monitored are hepatotoxicity,33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. hyponatremia4545 Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5. (in this case, serum sodium level = 135 mmol/L [sodium is an univalent element; thus, 1 mmol/L = 1 mEq/L)],4545 Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5. and cardiovascular failure due to cyclophosphamide cardiotoxicity.3636 Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs. 2011;22:468-72.
Cyclophosphamide administration routine in autoimmune rheumatic diseases.Sources: aShepherd et al.2929 Shepherd JD, Pringle LE, Barnett MJ, Klingemann HG, Reece DE, Phillips GL. Mesna versus hyperhydration for the prevention of cyclophosphamide-induced hemorrhagic cystitis in bone marrow transplantation. J Clin Oncol. 1991;9:2016-20.; bHawthorn; eCunningham3030 Hawthorn J, Cunningham D. Dexamethasone can potentiate the anti-emetic action of a 5HT3 receptor antagonist on cyclophosphamide induced vomiting in the ferret. Br J Cancer. 1990;61:56-60.; cJordan et al.3131 Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143-50.; dTurner et al.3232 Turner N, Stewart J, Barnett F, White S. Syndrome of inappropriate anti-diuretic hormone secretion secondary to carboplatin after docetaxel-carboplatin-trastuzumab combination for early stage HER-2 positive breast cancer. Asia Pac J Clin Oncol. 2012;8:e9-11.; eTrissel3333 Trissel LA. Handbook on injectable drugs. 17th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2013.; fHaubitz et al.3434 Haubitz M, Bohnenstengel F, Brunkhorst R, Schwab M, Hofmann U, Busse D. Cyclophosphamide pharmacokinetics and dose requirements in patients with renal insufficiency. Kidney Int. 2002;61:1495-501.; gMardegan et al.3535 Mardegan LC, Soledade C, Sachetto Z, Bertolo MB, Amstalden EMI, Sâmara AM, et al. Síndrome de Churg Strauss: uma vasculite rara. Rev Bras Reumatol. 2004;44:179-84.; hDi Lisi et al.3636 Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs. 2011;22:468-72.; iSalido et al.3737 Salido M, Macarron P, Hernandez-Garcia C, D'Cruz DP, Khamashta MA, Hughes GR. Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus. Lupus. 2003;12:636-9.; jCalixto-Lima et al.3838 Calixto-Lima L, Martins de Andrade E, Gomes AP, Geller M, Siqueira-Batista R. Dietetic management in gastrointestinal complications from antimalignant chemotherapy. Nutr Hosp. 2012;27:65-75.; kLotan et al.2020 Lotan E, Leader A, Lishner M, Gottfried M, Pereg D. Unrecognized renal insufficiency and chemotherapy associated adverse effects among breast cancer patients. Anticancer Drugs. 2012;23:991-5.; lZahn et al.3939 Zahn KL, Wong G, Bedrick EJ, Poston DG, Schroeder TM, Bauman JE. Relationship of protein and calorie intake to the severity of oral mucositis in patients with head and neck cancer receiving radiation therapy. Head Neck. 2012;34:655-62.; mMilman4040 Milman N. Anemia - still a major health problem in many parts of the world!. Ann Hematol. 2011;90:369-77.; nMota et al.55 Mota LM, Cruz BA, Brenol CV, Pereira IA, Rezende-Fronza LS, Bertolo MB, et al. Consenso 2012 da Sociedade Brasileira de Reumatologia para o tratamento da artrite reumatoide. Rev Bras Reumatol. 2012;52:152-74.; ºMcDermid and Lönnerdal4141 McDermid JM, Lönnerdal B. Iron Adv Nutr. 2012;3:532-3.; pCentro de Oncologia Unimed Birigui4242 Centro de Oncologia Unimed Birigui. Cuidados com o paciente em quimioterapia. Available at: http://www.unimedbirigui.net.br/oncologia/downloads/manual_cuidados_com_o_paciente_em_puimioterapia.pdf [acessed 08.08.14].
http://www.unimedbirigui.net.br/oncologi... ; qSubramaniam et al.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9.; rMota et al.4343 Mota DM, Silva MG, Sudo EC, Ortún V. Uso racional de medicamentos: uma abordagem econômica para tomada de decisões. Ciênc Saúde Coletiva. 2008;13(Suppl.):589-601.
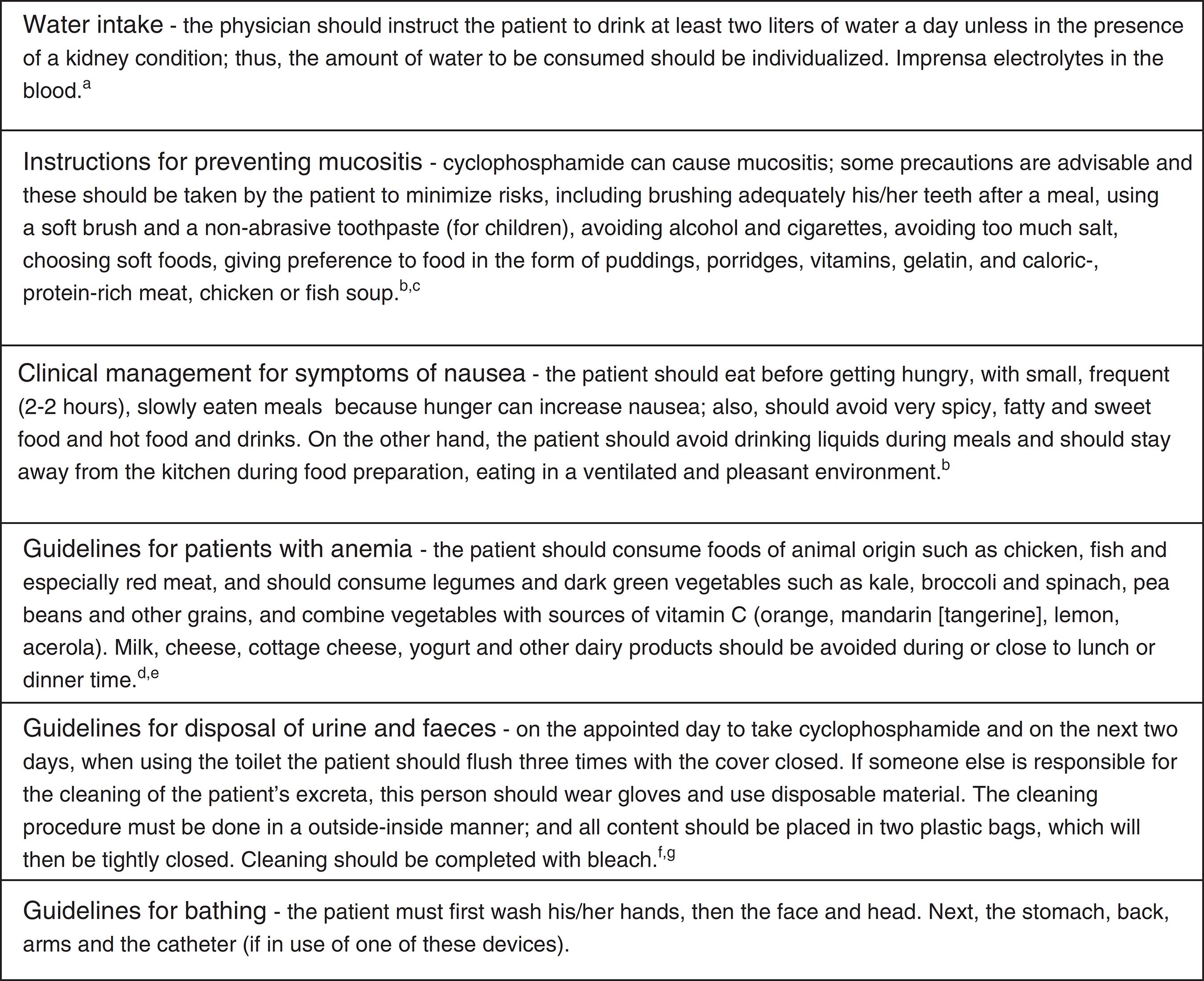
Guidelines for the patient taking cyclophosphamide.Sources: aInstituto Estadual de Hematologia Arthur de Siqueira4444 Instituto Estadual de Hematologia Arthur de Siqueira Cavalcanti (Hemorio). Rio de Janeiro: Manual do paciente em quimioterapia; 2006. Available at: http://www.hemorio.rj.gov.br/Html/pdf/Manuais/quimioterapia.pdf [accessed 08.08.14].
http://www.hemorio.rj.gov.br/Html/pdf/Ma... ; bBruining et al.4545 Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5.; cGonzález et al.4646 González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6.; dOtero López4747 Otero López MJ. Errores de medicación y gestión de riesgos. Rev Esp Salud Pública. 2003;77:527-40.; eMedeiros-Souza et al.4848 Medeiros-Souza P, Santos-Neto L, Kusano LTE, Pereira MG. Diagnosis and control of polypharmacy in the elderly. Rev Saúde Pública. 2007;41:1049-53.; fMesna4949 Mesna. In: UpToDate Inc. [base de dados da Internet]. Waltham, (MA); 2013. Available at: http://www.uptodate.com [accessed 01.07.14]. Requer assinatura.
http://www.uptodate.com... ; gTaketomo et al.5050 Taketomo CK, Hodding JH, Kraus DM. Pediatric dosage jandbook. Cleveland: Lexi-Comp Inc.; 1992..
Other adverse reactions from cyclophosphamide are amenorrhea,1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. early menopause,4646 González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6. and hair loss.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9.
Discussion
Drug administration errors can decrease the effectiveness of the pharmacological treatment and increase both the occurrence of adverse reactions and the financial costs of treatment.2424 Wannmacher L. Erros: evitar o evitável. Uso racional de medicmanetos: tema selecionados, vol. 2; 2005. p. 1–6. Available at: http://www.saudedireta.com.br/docsupload/1284734732novo_erro_medico.pdf [accessed 08.08.14].
http://www.saudedireta.com.br/docsupload...
A retrospective study conducted in hospitals in Spain between 2008 and 2010 evaluated the incidence of cost and adverse event. 245,320 episodes were identified, with an overall cost of 1,308,791.97 euros. Approximately 6.8% of patients experienced adverse events, representing a rise of 16.2% in costs. Six of the ten adverse events that burdened more significantly the hospital system occurred in the operating room, corresponding to an increase of expenses around 6.7% to the health system.2626 Allué N, Chiarello P, Bernal Delgado E, Castells X, Giraldo P, Martínez N, et al. Impacto económico de los eventos adversos en los hospitales españoles a partir del Conjunto Mínimo Básico de Datos. Gac Sanit. 2014;28:48-54.
A prospective study conducted between August and November 1999 and between January and May 2000 notified 1800 errors in 1663 patients. The number of notifications resulting from drug-related problems (including those probable and possible ones) was 215 (11.9%). Of these notifications, 108 (50.2%) were filled up due to adverse reactions, 100 (46.5%) came out of therapeutic failure related to dosing, and seven (3.3%) were due to intoxication. According to the criteria (modified) of Schumock and Tornton, 68.4% of drug-related problems are considered as preventable.4747 Otero López MJ. Errores de medicación y gestión de riesgos. Rev Esp Salud Pública. 2003;77:527-40.
The cyclophosphamide dosing schedule took into account the most common adverse reactions, the administration's strategy in the case of kidney failure, and the sequence in the administration of pre-ChT drugs, cyclophosphamide, and post-ChT drugs; to this end, the dosage of all medications used, their dilution and infusion time also were included.
The main clinical strategies in the face of adverse reactions from cyclophosphamide use included the care of hemorrhagic cystitis, nausea, and vomiting.1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. The administration of these drugs corresponds to what is defined as a qualitative polypharmacy, wherein the administration of a medication is performed to correct the adverse reaction of another medication.4848 Medeiros-Souza P, Santos-Neto L, Kusano LTE, Pereira MG. Diagnosis and control of polypharmacy in the elderly. Rev Saúde Pública. 2007;41:1049-53.
Several clinical strategies have been proposed to avoid hemorrhagic cystitis, including increased hydration of the patient and the administration of mesna and furosemide.2828 Schuchter LM, Hensley ML, Meropol NJ, Winer EP. Update of recommendations for the use of chemotherapy and radiotherapy protectants: clinical practice guidelines of the American Society of Clinical Oncology, Chemotherapy, and Radiotherapy. J Clin Oncol. 2002;20:2895-903.,2929 Shepherd JD, Pringle LE, Barnett MJ, Klingemann HG, Reece DE, Phillips GL. Mesna versus hyperhydration for the prevention of cyclophosphamide-induced hemorrhagic cystitis in bone marrow transplantation. J Clin Oncol. 1991;9:2016-20. In those cases in which the patient suffers of a severe kidney impairment, it is preferable to administer mesna in place of hydration, due to the patient's water restriction.2020 Lotan E, Leader A, Lishner M, Gottfried M, Pereg D. Unrecognized renal insufficiency and chemotherapy associated adverse effects among breast cancer patients. Anticancer Drugs. 2012;23:991-5.,2929 Shepherd JD, Pringle LE, Barnett MJ, Klingemann HG, Reece DE, Phillips GL. Mesna versus hyperhydration for the prevention of cyclophosphamide-induced hemorrhagic cystitis in bone marrow transplantation. J Clin Oncol. 1991;9:2016-20.
For the prevention of hemorrhagic cystitis, mesna is administered in a dose equivalent to 60% of cyclophosphamide, divided into three doses - 20% 15 min before the administration of cyclophosphamide, 20% after cyclophosphamide, and 20% 4 or 8 h after cyclophosphamide.2828 Schuchter LM, Hensley ML, Meropol NJ, Winer EP. Update of recommendations for the use of chemotherapy and radiotherapy protectants: clinical practice guidelines of the American Society of Clinical Oncology, Chemotherapy, and Radiotherapy. J Clin Oncol. 2002;20:2895-903. Mesna reduces the deposit of acrolein (a metabolite of cyclophosphamide) in the bladder, thus preventing hemorrhagic cystitis and bladder cancer.1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67.
In order to decrease the exposure of the urinary tract to acrolein, the patient should be well hydrated before, during and after the administration of cyclophosphamide. Thus, at the time of his/her admission, the patient should receive, through a venous access, 1 L of a blood volume expander (a crystalloid: saline 0.9%) for 1 h, 60 min before the administration of cyclophosphamide.5151 Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221-32.
Cyclophosphamide per se can be administered at any time. In turn, the infusion of mesna depends on the administration of cyclophosphamide.2828 Schuchter LM, Hensley ML, Meropol NJ, Winer EP. Update of recommendations for the use of chemotherapy and radiotherapy protectants: clinical practice guidelines of the American Society of Clinical Oncology, Chemotherapy, and Radiotherapy. J Clin Oncol. 2002;20:2895-903. Mesna may be administered by oral or parenteral (subcutaneous or intravenous) route.2828 Schuchter LM, Hensley ML, Meropol NJ, Winer EP. Update of recommendations for the use of chemotherapy and radiotherapy protectants: clinical practice guidelines of the American Society of Clinical Oncology, Chemotherapy, and Radiotherapy. J Clin Oncol. 2002;20:2895-903.
The oral administration of mesna has the advantage of a convenient dosage schedule; however, its use brings some disadvantages, for instance, a higher frequency of nausea and vomiting.4949 Mesna. In: UpToDate Inc. [base de dados da Internet]. Waltham, (MA); 2013. Available at: http://www.uptodate.com [accessed 01.07.14]. Requer assinatura.
http://www.uptodate.com...
,5050 Taketomo CK, Hodding JH, Kraus DM. Pediatric dosage jandbook. Cleveland: Lexi-Comp Inc.; 1992. Another limiting factor of the use of this drug orally is the decreased bioavailability versus parenteral route, due to first-pass metabolism, in addition to the potential decrease in its absorption as a result of frequent episodes of vomiting caused by the treatment with cyclophosphamide.3131 Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143-50. Taking into account the concepts that guide the rational use of pharmaceuticals, including the reduction of treatment costs for both the patient and society, oral administration of mesna would have also the advantage of a likely decrease in expenses, due the lower bed occupancy time and less workload of the nursing team.5151 Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221-32. Still in this context, another possible disadvantage is the patient's non-compliance; thus, one cannot be sure that the patient has taken, or otherwise, the last dose of mesna PO.5252 Dewulf NL, Monteiro RA, Passos AD, Vieira EM, Troncon LE. Adesão ao tratamento medicamentoso em pacientes com doenças gastrintestinais crônicas acompanhados no ambulatório de um hospital universitário. Rev Bras Ciênc Farm. 2006;42:575-84.
The advantage of the use IV mesna is that there is no need of absorption, and the onset of action of this drug is faster, compared with oral administration.2222 Andrade ED. Terapêutica medicamentosa em odontologia: procedimentos clínicos e uso de medicamentos nas principais situações da prática odontológica. São Paulo: Artes Médicas; 1998.,2323 Fuchs FD, Wannamacher L. Farmacologia clínica: fundamentos da terapêutica racional. Rio de Janeiro: Guanabara Koogan; 1992.,5353 Golan DE. Princípios de farmacologia: a base fisiopatológica da farmacoterapia. Rio de Janeiro: Guanabara Koogan; 2009. The disadvantage of the parenteral route is the greater risk of contamination, administration errors, less dosing convenience, and increase of the patient's hospital stay.2323 Fuchs FD, Wannamacher L. Farmacologia clínica: fundamentos da terapêutica racional. Rio de Janeiro: Guanabara Koogan; 1992.,5353 Golan DE. Princípios de farmacologia: a base fisiopatológica da farmacoterapia. Rio de Janeiro: Guanabara Koogan; 2009.
However, mesna administration with a view to the prevention of hemorrhagic cystitis in patients using cyclophosphamide in therapeutic doses for rheumatic diseases is controversial; thus, mesna may be replaced by a suitable hydration with 6 L of water per day, plus a diuretic drug, or the use of hydration with a volume of 3 L/m2 per day.5454 Monach PA, Arnold LM, Merkel PA. Incidence and prevention of bladder toxicity from cyclophosphamide in the treatment of rheumatic diseases: a data-driven review. Arthritis Rheum. 2010;62:9-21.
Furosemide is administered after cyclophosphamide infusion at a dose of 20 mg, in order to stimulate diuresis that, in synergism with mesna, decreases the exposure of urothelium to the action of acrolein.5555 Mesna: Tampa (FL): Gold Standard; 2014. Available at: http://www.clinicalpharmacology.com [accessed 08.08.14]. Requer assinatura.
http://www.clinicalpharmacology.com...
The maximum concentration of furosemide is 10 mg/mL administered in bolus, achieving a therapeutic concentration of 10 mg/mL per minute.5555 Mesna: Tampa (FL): Gold Standard; 2014. Available at: http://www.clinicalpharmacology.com [accessed 08.08.14]. Requer assinatura.
http://www.clinicalpharmacology.com...
The second dose of mesna (20% of cyclophosphamide dose) is administered in the interval between 15 and 30 min after the administration of cyclophosphamide.2828 Schuchter LM, Hensley ML, Meropol NJ, Winer EP. Update of recommendations for the use of chemotherapy and radiotherapy protectants: clinical practice guidelines of the American Society of Clinical Oncology, Chemotherapy, and Radiotherapy. J Clin Oncol. 2002;20:2895-903.
Nausea and vomiting are considered as common adverse reactions in chemotherapy, and this also occurs with cyclophosphamide3131 Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143-50. which, in turn, participates of many chemotherapeutic regimens. In this case, a routine has been proposed for the treatment of rheumatic diseases. Nausea caused by the exclusive administration of cyclophosphamide (without a therapeutic scheme) is classified as a late-onset nausea.5656 Jeong SW, Cho JW, Hwang JS, Song JD, Shin S, Jang JY, et al. The antiemetic effect of a novel tropisetron patch in anticancer agents-induced kaolin pica model using rats. Environ Toxicol Pharmacol. 2005;20:167-74. Thus, ondansetron was not required to prevent this effect.5656 Jeong SW, Cho JW, Hwang JS, Song JD, Shin S, Jang JY, et al. The antiemetic effect of a novel tropisetron patch in anticancer agents-induced kaolin pica model using rats. Environ Toxicol Pharmacol. 2005;20:167-74. A decrease in effectiveness is another reason for not using ondansetron prior to cyclophosphamide.5757 de Jonge ME, Huitema AD, van Dam SM, Rodenhuis S, Beijnen JH. Effects of co-medicated drugs on cyclophosphamide bioactivation in human liver microsomes. Anticancer Drugs. 2005;16:331-6.
This reduction in efficacy occurs because ondansetron is an inhibitor of CYP2B.5858 Goodman L. Goodman & Gilman: as bases farmacológicas da terapêutica. Rio de Janeiro: McGraw-Hill; 2001.59 This occurs because cyclophosphamide is a prodrug that must be activated by CYP2B, resulting in 4-hydroxycyclophosphamide and aldophosphamide. These metabolites are transported to the site of action, where they undergo spontaneous cleavage, producing phosphoramide mustard, responsible for the pharmacological effects of the drug.5858 Goodman L. Goodman & Gilman: as bases farmacológicas da terapêutica. Rio de Janeiro: McGraw-Hill; 2001.59
Moreover, dexamethasone was added prior to chemotherapy, as a prophylactic agent to anaphylactic shock and also as an antiemetic.5959 Andrews PL, Sanger GJ. Nausea and the quest for the perfect anti-emetic. Eur Pharmacol. 2014;722:108-21. Preferably, dexamethasone should be administered so that its peak coincides with the peak of physiological corticosteroids, which normally occurs at 8 a.m. and 16 p.m.5858 Goodman L. Goodman & Gilman: as bases farmacológicas da terapêutica. Rio de Janeiro: McGraw-Hill; 2001.59 A peak in dexamethasone plasma concentration occurs within 60 min, and its action begins in 30 min.5555 Mesna: Tampa (FL): Gold Standard; 2014. Available at: http://www.clinicalpharmacology.com [accessed 08.08.14]. Requer assinatura.
http://www.clinicalpharmacology.com...
,6060 Dexamethasone. In: UpToDate Inc. [base de dados da Internet]. Waltham, (MA); 2013. Available at: http://www.uptodate.com [accessed 01.07.14]. Requer assinatura.
http://www.uptodate.com...
Thus, the administration of dexamethasone should be started in the morning, 30 min before the administration of cyclophosphamide, preferably at 7:30 a.m.5858 Goodman L. Goodman & Gilman: as bases farmacológicas da terapêutica. Rio de Janeiro: McGraw-Hill; 2001.59
After the emesis caused by cyclophosphamide was classified as a delayed-type,5656 Jeong SW, Cho JW, Hwang JS, Song JD, Shin S, Jang JY, et al. The antiemetic effect of a novel tropisetron patch in anticancer agents-induced kaolin pica model using rats. Environ Toxicol Pharmacol. 2005;20:167-74. and in view of the decrease of cyclophosphamide efficacy when ondansetron is administered prior to this chemotherapeutic agent, ondansetron (8 mg PO3131 Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143-50.,6161 Cagnoni PJ, Matthes S, Day TC, Bearman SI, Shpall EJ, Jones RB. Modification of the pharmacokinetics of high-dose cyclophosphamide and cisplatin. Bone Marrow Transplant. 1999;24:1-4. administered at 6 and 14 or 8 and 16 h post-ChT, and with a maximum dose of 16 mg after chemotherapy, not exceeding 32 mg per day) was the last drug used for the prophylaxis of emesis caused by cyclophosphamide.3131 Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143-50.
Other important adverse effects of cyclophosphamide include hematologic toxicity,1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. kidney failure,2020 Lotan E, Leader A, Lishner M, Gottfried M, Pereg D. Unrecognized renal insufficiency and chemotherapy associated adverse effects among breast cancer patients. Anticancer Drugs. 2012;23:991-5. hyponatremia,4545 Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5.,6262 Gilbar PJ, Richmond J, Wood J, Sullivan A. Syndrome of inappropriate antidiuretic hormone secretion induced by a single dose of oral cyclophosphamide. Ann Pharmacother. 2012;46:23. neurological impairment,4545 Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5. amenorrhea,1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. early menopause,4646 González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6. hair loss,33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. hepatotoxicity (rare),33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. and late-onset cancer.1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67. The dose of cyclophosphamide for the treatment of systemic lupus erythematosus, including those patients with neuropsychiatric and/or hematologic disorders, with class IV lupus nephritis, and with other serious manifestations of systemic lupus erythematosus, is 0.5-1 g/m2 IV monthly,55 Mota LM, Cruz BA, Brenol CV, Pereira IA, Rezende-Fronza LS, Bertolo MB, et al. Consenso 2012 da Sociedade Brasileira de Reumatologia para o tratamento da artrite reumatoide. Rev Bras Reumatol. 2012;52:152-74.,6262 Gilbar PJ, Richmond J, Wood J, Sullivan A. Syndrome of inappropriate antidiuretic hormone secretion induced by a single dose of oral cyclophosphamide. Ann Pharmacother. 2012;46:23. with dosage adjustment in patients with hematological toxicity and kidney failure.2020 Lotan E, Leader A, Lishner M, Gottfried M, Pereg D. Unrecognized renal insufficiency and chemotherapy associated adverse effects among breast cancer patients. Anticancer Drugs. 2012;23:991-5.,6363 Abdul Rasool Hassan B, Yusoff ZB, Bin Othman S. Association of neutropenia onset and severity with chemotherapy regimens and schedules. Asian Pac J Cancer Prev. 2011;12:1425-8. Adverse hematologic reactions caused by cyclophosphamide are classified as serious, as they cause high morbidity.1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
,6464 Vieira FP, Rediguieiri CF, Rediguieiri CF. A regulação de medicamentos no Brasil. Porto Alegre: Artmed; 2013. p. 672. NADIR is the minimum hematologic counting that must be observed to see if the patient may or may not embark on another chemotherapeutic cycle.6565 Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532-43. The main hematological tests include platelets, neutrophils, white blood cells and neutrophil counts. Neutropenia is defined as a decrease in absolute neutrophil count <1500 cells/µL.6565 Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532-43. The main causes of neutropenia include hematologic disorders, autoimmune diseases, infection, adverse drug reaction, chemotherapy, and radiotherapy.6565 Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532-43. Thrombocytopenia occurs when the platelet count is <100,000/mm3.6565 Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532-43. In a patient with a platelet count <81,000/mm3 concomitantly experiencing leukopenia, the treatment should be discontinued until the platelet count increase to 99,000/mm3.6565 Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532-43. However, cyclophosphamide can be used in the treatment of refractory thrombocytopenic purpura, and in this case, among the hematologic disorders, thrombocytopenia, and microangiopathic hemolytic anemia are included. Leukopenia1010 Campos LM, Spadoni MS, Michelin CM, Jesus AA, Carneiro JD, da Silva CA. Thrombotic thrombocytopenic purpura at presentation of juvenile systemic lupus erythematosus patients. Rev Bras Reumatol. 2013;53:120-6. is defined as a white cell count <3500/mm3.6565 Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532-43.
Hepatotoxicity is an adverse reaction caused by cyclophosphamide that normally occurs at high doses.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. When hepatotoxicity occurs at low doses, the reaction is classified as a rare, but serious, event.1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
,6464 Vieira FP, Rediguieiri CF, Rediguieiri CF. A regulação de medicamentos no Brasil. Porto Alegre: Artmed; 2013. p. 672. Acute liver failure with low-dose cyclophosphamide (200 mg) was described in a case report of a male Chinese aged 48 years with progressive glomerulonephritis secondary to Wegener's granulomatosis, 24 h after the administration of cyclophosphamide.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. The diagnosis of granulomatosis with polyangiitis was established by pathological examination and c-ANCA.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. The patient was being treated with high-dose methylprednisolone, plasmapheresis, intermittent hemodialysis and low intravenous doses of cyclophosphamide.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. Other factors that may be associated with hepatotoxicity have been excluded, including antifungals, HIV, and hepatitis B and C.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. Alanine transaminase increased from 41 U/L to 336 U/L at the day of administration of 200 mg of cyclophosphamide; in the next day, a peak of 566 U/L was reached.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. Two weeks later, the patient was treated with another pulse of 200 mg of cyclophosphamide (second dose), and the concentration of alanine transaminase reached 1253 U/L.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. A liver biopsy was not possible, because the patient had a clotting disorder.33 Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9. Another laboratory parameter to be monitored is sodium concentration. Hyponatremia is considered as an electrolyte disorder identified in clinical practice.4545 Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5. Although many cases are mild or relatively symptomatic, hyponatremia is regarded as a clinically important finding, with high morbidity and mortality. Neurological symptoms of hyponatremia occur at sodium levels <125 mmol/L.6666 Letmaier M, Painold A, Holl AK, Vergin H, Engel R, Konstantinidis A, et al. Hyponatraemia during psychopharmacological treatment: results of a drug surveillance programme. Int J Neuropsychopharmacol. 2012;15:739-48. Among the complications of hyponatremia, one can mention central nervous system disorders such as seizures, and even a permanent damage to the central nervous system, and death.6666 Letmaier M, Painold A, Holl AK, Vergin H, Engel R, Konstantinidis A, et al. Hyponatraemia during psychopharmacological treatment: results of a drug surveillance programme. Int J Neuropsychopharmacol. 2012;15:739-48. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) was described in a case report in which this syndrome was associated with the use of IV cyclophosphamide in a dose of 500-1000 mg/m2, with a serum sodium level <120 mmol/L in a patient presenting neurological complications.6262 Gilbar PJ, Richmond J, Wood J, Sullivan A. Syndrome of inappropriate antidiuretic hormone secretion induced by a single dose of oral cyclophosphamide. Ann Pharmacother. 2012;46:23.
Cyclophosphamide may also cause cardiotoxicity. Routinely, echocardiography, a noninvasive method, is used to monitor cardiovascular function in patients treated with immunosuppressants.3636 Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs. 2011;22:468-72. Other non-invasive methods most widely used are electrocardiography and 24-h (ECG) Holter monitoring.3636 Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs. 2011;22:468-72. Invasive methods such as scintigraphy, magnetic resonance imaging and cardiac biopsy are also procedures that can be used in cases of adverse reactions classified as serious.3636 Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs. 2011;22:468-72.
Other adverse reactions caused by cyclophosphamide include amenorrhea, menopause, and late-onset cancer, including esophageal, lung and bladder adenocarcinoma.1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67.,4646 González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6. Cyclophosphamide was administered at a dose of 750-1000 mg/m2 body surface in LUMINA (Lupus in minorities, nature versus nurture), a multicenter study performed including 567 women aged under 51 years.4646 González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6. A decrease in gonadal function was found, and gonadal failure was defined as the occurrence of amenorrhea for more than six months without a history of hysterectomy.4646 González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6. Cyclophosphamide has also been associated with teratogenicity.1818 Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67.
As to cyclophosphamide dose adjustment in patients with kidney failure, this is only done in severe cases, that is, with a creatinine clearance <10 mL/min. The therapeutic regimen of cyclophosphamide should be modified, its dose should be reduced by 25%, and supplemented with 50% after dialysis.3434 Haubitz M, Bohnenstengel F, Brunkhorst R, Schwab M, Hofmann U, Busse D. Cyclophosphamide pharmacokinetics and dose requirements in patients with renal insufficiency. Kidney Int. 2002;61:1495-501.
The dilution of the drugs used in cyclophosphamide routine was carried out with the goal of maintaining the highest possible concentration of the drug in its non-ionized form.5858 Goodman L. Goodman & Gilman: as bases farmacológicas da terapêutica. Rio de Janeiro: McGraw-Hill; 2001.59 Thus, two parameters were taken into account: drug compatibility with the vehicle (saline, dextrose or ringer lactate) and its stability time in the vehicle; preference was given to those drugs whose stability time was longer, in order to ensure a more effective treatment.3333 Trissel LA. Handbook on injectable drugs. 17th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2013.
When the drugs used have proved compatible and stable with the same vehicle, preference was given to the choice of the same vehicle, as this facilitates their administration by the nursing staff and prevents pharmacokinetic interaction, which would cause ionization of the drugs and a decrease in their efficacy.6767 Brasil. Ministério da Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Assistência Farmacêutica e Insumos Estratégicos. Formulário terapêutico nacional 2010: Rename 2010. 2a. ed. Brasília: Ministério da Saúde; 2010. Série B. Textos Básicos de Saúde.
Another important aspect that should be addressed is the education of the patient on the treatment to what he/she is being submitted. A study in the city of Natal with 40 women diagnosed with systemic lupus erythematosus at the Hospital Onofre has shown that patients showing greater adherence were those who understood correctly the treatment and also the disease; thus, these women satisfactorily understood the adverse events and the clinical management, in order to minimize these adverse drug reactions.6868 Faria DA, Revoredo LS, Vilar MJ, Maia EM. Resilience and treatment adhesion in patients with systemic lupus erythematosus. Open Rheumatol J. 2014;8:1-8.
Publications on adverse events are important tools for drug safety monitoring after their release for marketing purposes by the health authorities of each country.6969 Kelly WN, Arellano FM, Barnes J, Bergman U, Edwards IR, Fernandez AM, et al. Guidelines for submitting adverse event reports for publication. Pharmacoepidemiol Drug Saf. 2007;16:581-7. This review of medication administration intended to standardize the administration of cyclophosphamide by health professionals, in order to minimize the adverse events caused by drugs, the so-called adverse drug reaction.1919 US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
http://www.fda.gov/downloads/Drugs/…/Gui...
Conclusion
The routine was developed in order to increase the area under the curve (AUC) for cyclophosphamide, and to attain an appropriate clinical management to minimize the adverse drug reactions that, if not properly prevented, will cause damage to the patient, for instance, an increased prevalence of vomiting, and acrolein deposition in the bladder. The clinical management of adverse reactions that alter laboratory tests was described in order to guide the application of these tests. Adverse reactions, even being rare, were highlighted because these events can cause high morbidity. Thus, the rational use of cyclophosphamide increases the safety of the treatment and reduces the cost of administration of this chemotherapeutic agent, since our goal is to avoid error.
-
☆
Study conducted at the Serviço de Reumatologia, Hospital Universitário, Universidade de Brasília, Brasília, DF, Brazil.
References
-
1Burkard ME, Wisinski KB, Njiaju UO, Donohue S, Hegeman R, Stella A, et al. Feasibility of 4 cycles of docetaxel and cyclophosphamide every 14 days as an adjuvant regimen for breast cancer: a Wisconsin Oncology Network study. Clin Breast Cancer. 2014;14:205-11.
-
2Huang BT, Tan Y, Zhao WH, Zeng QC, Li BS, Chen RL. How to determine bortezomib-based regimen for elderly patients with multiple myeloma: PAD versus CBd, an observational study. J Cancer Res Clin Oncol. 2014;140:303-9.
-
3Subramaniam SR, Cader RA, Mohd R, Yen KW, Ghafor HA. Low-dose cyclophosphamide-induced acute hepatotoxicity. Am J Case Rep. 2013;14:345-9.
-
4Munyangango EM, Le Roux-Villet C, Doan S, Pascal F, Soued I, Alexandre M, et al. Oral cyclophosphamide without corticosteroids to treat mucous membrane pemphigoid. Br J Dermatol. 2013;168:381-90.
-
5Mota LM, Cruz BA, Brenol CV, Pereira IA, Rezende-Fronza LS, Bertolo MB, et al. Consenso 2012 da Sociedade Brasileira de Reumatologia para o tratamento da artrite reumatoide. Rev Bras Reumatol. 2012;52:152-74.
-
6Rosa Neto NS, Goldenstein-Schainberg C. Dermatomiosite juvenil: revisão e atualização em patogênese e tratamento. Rev Bras Reumatol. 2010;503:299-312.
-
7Broad K, Pope JE. The efficacy of treatment for systemic sclerosis interstitial lung disease: results from a meta-analysis. Med Sci Monit. 2010;16:RA187-90.
-
8Appenzeller S, Sampaio-Barros PD, Samara AM, Marques Neto JF. Crise renal como manifestação inicial de esclerose sistêmica sine scleroderma. Rev Bras Reumatol. 2004;44:87-9.
-
9Chu H, Wu LH, Song D, Yu F, Zhao MH. Noninflammatory necrotizing vasculopathy in lupus nephritis: a single-center experience. Lupus. 2014;23:20-30.
-
10Campos LM, Spadoni MS, Michelin CM, Jesus AA, Carneiro JD, da Silva CA. Thrombotic thrombocytopenic purpura at presentation of juvenile systemic lupus erythematosus patients. Rev Bras Reumatol. 2013;53:120-6.
-
11Yaguchi H, Sakushima K, Takahashi I, Nishimura H, Yashima-Yamada M, Nakamura M, et al. Efficacy of intravenous cyclophosphamide therapy for neuromyelitis optica spectrum disorder. Intern Med. 2013;52:969-72.
-
12Hobbs DJ, Barletta GM, Rajpal JS, Rajpal MN, Weismantel DP, Birmingham JD, et al. Severe paediatric systemic lupus erythematosus nephritis - a single-centre experience. Nephrol Dial Transplant. 2010;25:457-63.
-
13Lehman TJ, Singh C, Ramanathan A, Alperin R, Adams A, Barinstein L, et al. Prolonged improvement of childhood onset systemic lupus erythematosus following systematic administration of rituximab and cyclophosphamide. Pediatri Rheumatol Online J. 2014;12:3.
-
14Suarez-Almazor ME, Belseck E, Shea B, Wells G, Tugwell P. Cyclophosphamide for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2000;:CD001157.
-
15Cox PJ. Cyclophosphamide cystitis - identification of acrolein as the causative agent. Biochem Pharmacol. 1979;28:2045-9.
-
16Mavragani CP, Moutsopoulos HM. Lupus nephritis: current issues. Ann Rheum Dis. 2003;62:795-8.
-
17Dupuis LL, Boodhan S, Holdsworth M, Robinson PD, Hain R, Portwine C, et al. Guideline for the prevention of acute nausea and vomiting due to antineoplastic medication in pediatric cancer patients. Pediatr Blood Cancer. 2013;60:1073-82.
-
18Furst DE, Tseng CH, Clements PJ, Strange C, Tashkin DP, Roth MD, et al. Adverse events during the Scleroderma Lung Study. Am J Med. 2011;124:459-67.
-
19US Department of Health and Human Services. Food and Drug Administration. Guidance for industry and investigators: safety reporting requirements for INDs and BA/BE Studies. MD: Silver Spring; 2012. p. 29. Available at: http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf [accessed 08.08.14].
» http://www.fda.gov/downloads/Drugs/…/Guidances/UCM227351.pdf -
20Lotan E, Leader A, Lishner M, Gottfried M, Pereg D. Unrecognized renal insufficiency and chemotherapy associated adverse effects among breast cancer patients. Anticancer Drugs. 2012;23:991-5.
-
21Hsieh SG, Hibbert S, Shaw P, Ahern V, Arora M. Association of cyclophosphamide use with dental developmental defects and salivary gland dysfunction in recipients of childhood antineoplastic therapy. Cancer. 2011;117:2219-27.
-
22Andrade ED. Terapêutica medicamentosa em odontologia: procedimentos clínicos e uso de medicamentos nas principais situações da prática odontológica. São Paulo: Artes Médicas; 1998.
-
23Fuchs FD, Wannamacher L. Farmacologia clínica: fundamentos da terapêutica racional. Rio de Janeiro: Guanabara Koogan; 1992.
-
24Wannmacher L. Erros: evitar o evitável. Uso racional de medicmanetos: tema selecionados, vol. 2; 2005. p. 1–6. Available at: http://www.saudedireta.com.br/docsupload/1284734732novo_erro_medico.pdf [accessed 08.08.14].
» http://www.saudedireta.com.br/docsupload/1284734732novo_erro_medico.pdf -
25Melo LR, Pedreira MLG. Erros de medicação em pediatria: análise da documentação de enfermagem no prontuário do paciente. Rev Bras Enferm. 2005;58:180-5.
-
26Allué N, Chiarello P, Bernal Delgado E, Castells X, Giraldo P, Martínez N, et al. Impacto económico de los eventos adversos en los hospitales españoles a partir del Conjunto Mínimo Básico de Datos. Gac Sanit. 2014;28:48-54.
-
27Medeiros EFF, Moraes CF, Karnikowski M, Nóbrega OT, Karnikowski MGdO. Intervenção interdisciplinar enquanto estratégia para o Uso Racional de Medicamentos em idosos. Ciênc Saúde Coletiva. 2011;16:3139-49.
-
28Schuchter LM, Hensley ML, Meropol NJ, Winer EP. Update of recommendations for the use of chemotherapy and radiotherapy protectants: clinical practice guidelines of the American Society of Clinical Oncology, Chemotherapy, and Radiotherapy. J Clin Oncol. 2002;20:2895-903.
-
29Shepherd JD, Pringle LE, Barnett MJ, Klingemann HG, Reece DE, Phillips GL. Mesna versus hyperhydration for the prevention of cyclophosphamide-induced hemorrhagic cystitis in bone marrow transplantation. J Clin Oncol. 1991;9:2016-20.
-
30Hawthorn J, Cunningham D. Dexamethasone can potentiate the anti-emetic action of a 5HT3 receptor antagonist on cyclophosphamide induced vomiting in the ferret. Br J Cancer. 1990;61:56-60.
-
31Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143-50.
-
32Turner N, Stewart J, Barnett F, White S. Syndrome of inappropriate anti-diuretic hormone secretion secondary to carboplatin after docetaxel-carboplatin-trastuzumab combination for early stage HER-2 positive breast cancer. Asia Pac J Clin Oncol. 2012;8:e9-11.
-
33Trissel LA. Handbook on injectable drugs. 17th ed. Bethesda, MD: American Society of Health-System Pharmacists; 2013.
-
34Haubitz M, Bohnenstengel F, Brunkhorst R, Schwab M, Hofmann U, Busse D. Cyclophosphamide pharmacokinetics and dose requirements in patients with renal insufficiency. Kidney Int. 2002;61:1495-501.
-
35Mardegan LC, Soledade C, Sachetto Z, Bertolo MB, Amstalden EMI, Sâmara AM, et al. Síndrome de Churg Strauss: uma vasculite rara. Rev Bras Reumatol. 2004;44:179-84.
-
36Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs. 2011;22:468-72.
-
37Salido M, Macarron P, Hernandez-Garcia C, D'Cruz DP, Khamashta MA, Hughes GR. Water intoxication induced by low-dose cyclophosphamide in two patients with systemic lupus erythematosus. Lupus. 2003;12:636-9.
-
38Calixto-Lima L, Martins de Andrade E, Gomes AP, Geller M, Siqueira-Batista R. Dietetic management in gastrointestinal complications from antimalignant chemotherapy. Nutr Hosp. 2012;27:65-75.
-
39Zahn KL, Wong G, Bedrick EJ, Poston DG, Schroeder TM, Bauman JE. Relationship of protein and calorie intake to the severity of oral mucositis in patients with head and neck cancer receiving radiation therapy. Head Neck. 2012;34:655-62.
-
40Milman N. Anemia - still a major health problem in many parts of the world!. Ann Hematol. 2011;90:369-77.
-
41McDermid JM, Lönnerdal B. Iron Adv Nutr. 2012;3:532-3.
-
42Centro de Oncologia Unimed Birigui. Cuidados com o paciente em quimioterapia. Available at: http://www.unimedbirigui.net.br/oncologia/downloads/manual_cuidados_com_o_paciente_em_puimioterapia.pdf [acessed 08.08.14].
» http://www.unimedbirigui.net.br/oncologia/downloads/manual_cuidados_com_o_paciente_em_puimioterapia.pdf -
43Mota DM, Silva MG, Sudo EC, Ortún V. Uso racional de medicamentos: uma abordagem econômica para tomada de decisões. Ciênc Saúde Coletiva. 2008;13(Suppl.):589-601.
-
44Instituto Estadual de Hematologia Arthur de Siqueira Cavalcanti (Hemorio). Rio de Janeiro: Manual do paciente em quimioterapia; 2006. Available at: http://www.hemorio.rj.gov.br/Html/pdf/Manuais/quimioterapia.pdf [accessed 08.08.14].
» http://www.hemorio.rj.gov.br/Html/pdf/Manuais/quimioterapia.pdf -
45Bruining DM, van Roon EN, de Graaf H, Hoogendoorn M. Cyclophosphamide-induced symptomatic hyponatraemia. Neth J Med. 2011;69:192-5.
-
46González LA, Pons-Estel GJ, Zhang JS, McGwin G, Roseman J, Reveille JD, et al. Effect of age, menopause and cyclophosphamide use on damage accrual in systemic lupus erythematosus patients from LUMINA, a multiethnic US cohort (LUMINA LXIII). Lupus. 2009;18:184-6.
-
47Otero López MJ. Errores de medicación y gestión de riesgos. Rev Esp Salud Pública. 2003;77:527-40.
-
48Medeiros-Souza P, Santos-Neto L, Kusano LTE, Pereira MG. Diagnosis and control of polypharmacy in the elderly. Rev Saúde Pública. 2007;41:1049-53.
-
49Mesna. In: UpToDate Inc. [base de dados da Internet]. Waltham, (MA); 2013. Available at: http://www.uptodate.com [accessed 01.07.14]. Requer assinatura.
» http://www.uptodate.com -
50Taketomo CK, Hodding JH, Kraus DM. Pediatric dosage jandbook. Cleveland: Lexi-Comp Inc.; 1992.
-
51Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010;363:221-32.
-
52Dewulf NL, Monteiro RA, Passos AD, Vieira EM, Troncon LE. Adesão ao tratamento medicamentoso em pacientes com doenças gastrintestinais crônicas acompanhados no ambulatório de um hospital universitário. Rev Bras Ciênc Farm. 2006;42:575-84.
-
53Golan DE. Princípios de farmacologia: a base fisiopatológica da farmacoterapia. Rio de Janeiro: Guanabara Koogan; 2009.
-
54Monach PA, Arnold LM, Merkel PA. Incidence and prevention of bladder toxicity from cyclophosphamide in the treatment of rheumatic diseases: a data-driven review. Arthritis Rheum. 2010;62:9-21.
-
55Mesna: Tampa (FL): Gold Standard; 2014. Available at: http://www.clinicalpharmacology.com [accessed 08.08.14]. Requer assinatura.
» http://www.clinicalpharmacology.com -
56Jeong SW, Cho JW, Hwang JS, Song JD, Shin S, Jang JY, et al. The antiemetic effect of a novel tropisetron patch in anticancer agents-induced kaolin pica model using rats. Environ Toxicol Pharmacol. 2005;20:167-74.
-
57de Jonge ME, Huitema AD, van Dam SM, Rodenhuis S, Beijnen JH. Effects of co-medicated drugs on cyclophosphamide bioactivation in human liver microsomes. Anticancer Drugs. 2005;16:331-6.
-
58Goodman L. Goodman & Gilman: as bases farmacológicas da terapêutica. Rio de Janeiro: McGraw-Hill; 2001.59
-
59Andrews PL, Sanger GJ. Nausea and the quest for the perfect anti-emetic. Eur Pharmacol. 2014;722:108-21.
-
60Dexamethasone. In: UpToDate Inc. [base de dados da Internet]. Waltham, (MA); 2013. Available at: http://www.uptodate.com [accessed 01.07.14]. Requer assinatura.
» http://www.uptodate.com -
61Cagnoni PJ, Matthes S, Day TC, Bearman SI, Shpall EJ, Jones RB. Modification of the pharmacokinetics of high-dose cyclophosphamide and cisplatin. Bone Marrow Transplant. 1999;24:1-4.
-
62Gilbar PJ, Richmond J, Wood J, Sullivan A. Syndrome of inappropriate antidiuretic hormone secretion induced by a single dose of oral cyclophosphamide. Ann Pharmacother. 2012;46:23.
-
63Abdul Rasool Hassan B, Yusoff ZB, Bin Othman S. Association of neutropenia onset and severity with chemotherapy regimens and schedules. Asian Pac J Cancer Prev. 2011;12:1425-8.
-
64Vieira FP, Rediguieiri CF, Rediguieiri CF. A regulação de medicamentos no Brasil. Porto Alegre: Artmed; 2013. p. 672.
-
65Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532-43.
-
66Letmaier M, Painold A, Holl AK, Vergin H, Engel R, Konstantinidis A, et al. Hyponatraemia during psychopharmacological treatment: results of a drug surveillance programme. Int J Neuropsychopharmacol. 2012;15:739-48.
-
67Brasil. Ministério da Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Assistência Farmacêutica e Insumos Estratégicos. Formulário terapêutico nacional 2010: Rename 2010. 2a. ed. Brasília: Ministério da Saúde; 2010. Série B. Textos Básicos de Saúde.
-
68Faria DA, Revoredo LS, Vilar MJ, Maia EM. Resilience and treatment adhesion in patients with systemic lupus erythematosus. Open Rheumatol J. 2014;8:1-8.
-
69Kelly WN, Arellano FM, Barnes J, Bergman U, Edwards IR, Fernandez AM, et al. Guidelines for submitting adverse event reports for publication. Pharmacoepidemiol Drug Saf. 2007;16:581-7.
Publication Dates
-
Publication in this collection
Nov-Dec 2017
History
-
Received
2 Aug 2013 -
Accepted
7 Apr 2016