Introduction
Takayasu's arteritis chiefly affects the aorta and its major branches, including the pulmonary artery. Clinical presentations of TA are protean and not specific, the vast majority of patients presented vascular insufficiency such as stenosis, occlusion, or aneurysm. Such features confuse TA with those of chronic thromboembolic diseases, fibrosing mediastinitis or neoplasia, resulting in an erroneous initial diagnosis.11 Kerr KM, Auger WR, Fedullo PF, Channick RH, Yi ES, Moser KM. Large vessel pulmonary arteritis mimicking chronic thromboembolic disease. Am J Respir Crit Care Med. 1995;152:367-73. PMID: 7599847. The median delay of the diagnosis of disease was 10 months after the onset of first symptoms.22 Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takayasu's arteritis. Ann Intern Med. 1994;120:919-29. PMID: 7909656. Severe hypertension, severe functional disability, and evidence of cardiac involvement were good predictors for either death or major event on follow-up, which help the prognosis assessment and elective interventions.33 Subramanyan R, Joy J, Balakrishnan KG. Natural history of aortoarteritis (Takayasu's disease). Circulation. 1989;80:429-37. PMID: 2569946.
Case report
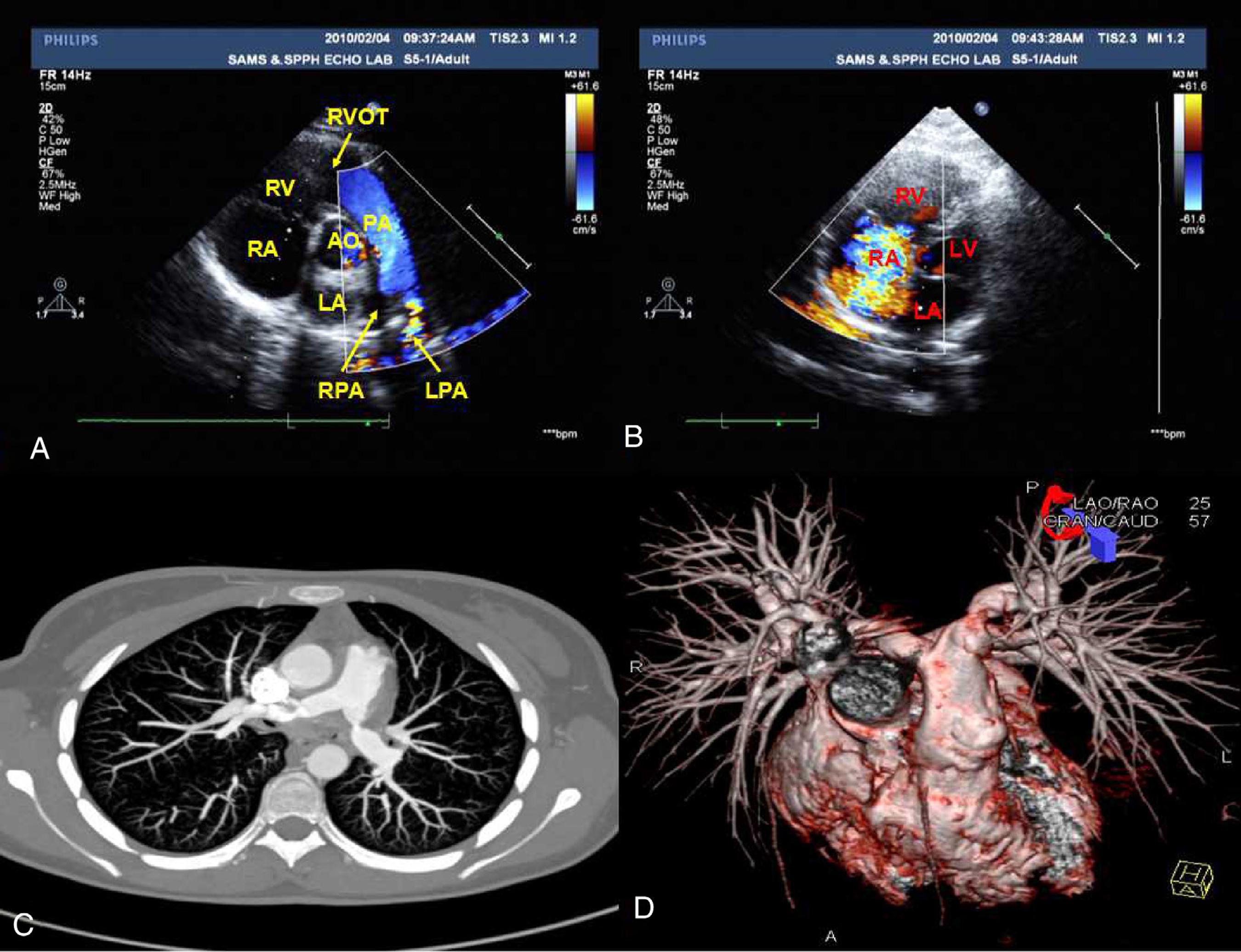
An 18-year-old yellow Asian female patient had been suffering from fatigue on effort, chest stuffiness, chest pain, and dyspnea for 8 months. Two months ago, she was admitted to the department of cardiology in our hospital. Blood pressure was 126/83 mmHg without difference between bilateral arms. The echocardiography (ECHO) showed excessive stenosis of both branches of pulmonary artery, the initial portion of the right branch with a lumen of 14 mm and the left 16 mm, and a significantly high pulmonary artery pressure of 118 mmHg (Fig. 1A-B). Dual source computed tomography (DSCT) verified a considerable partial stenosis of both branches of pulmonary artery and no evidence of aorta involvement (Fig. 1C-D). All the clinical manifestations of this patient demonstrated critical pulmonary artery hypertension with stenosis followed by left heart involvement. Therefore, she was diagnosed with congenital heart disease from these findings.
(A-B) Echocardiography 6 months after symptom onset. It showed colorful blood flow in left branch of pulmonary artery due to the stenotic lesion (A) and remarked tricuspid regurgitation (B). (C-D) Dual source computed tomography of pulmonary artery 4 months after symptom onset. It revealed the considerably stenosis of both branches of pulmonary artery (arrows) and no evidence of aorta involvement. LV, left ventricle; LA, left atrium; RV, right ventricle; RA, right atrium; AO, aorta; PA, pulmonary artery; LPA, left branch of pulmonary artery; RPA, right branch of pulmonary artery; RVOT, right ventricular outflow tract.
One month ago, tricuspid valve annuloplasty and branch pulmonary arteries angioplasty were given in another hospital due to exacerbated symptoms. Laboratory tests postoperative pointed out immunological aberration. Erythrocyte sedimentation rate is 89.0 mm/h, and rheumatoid factor is 9.1 IU/mL.
Subsequently the patient was admitted to the department of rheumatology of our hospital. Diagnosis of TA was suspected, and as such a complete aortogram was made but proved to be normal. Repeated ECHO showed reduction of tricuspid regurgitation and pulmonary artery pressure, and a normal aortic arch and its branches (bilateral internal and external carotid artery, and bilateral subclavian artery). Digital subtraction angiography (DSA) findings referred to no vascular lesions of the aorta and branches, presented as stenosis, narrowing, occlusion and irregularity of wall (Fig. 2A). Anti-nuclear antibody (ANA) was positive in a titer of 1:40, and perinuclear anti-neutrophil cytoplasmic antibody (p-ANCA) positive in 1:10. On admission, she was diagnosed as TA. Prednisone 30 mg/day and aspirin 50 mg/day were added.
(A) Digital subtraction angiography of the aorta and branches after tricuspid valve annuloplasty. Images of thoracic aorta, abdominal aorta and iliac artery were integrated into one figure. It referred to no vascular lesions that involved the aorta and branches. (B) Computed tomography arteriograms of the aorta and branches 42 months after TA diagnosis. Considerably remarkable stenosis of the right brachiocephalic trunk (large arrow), left common carotid artery (small arrow) and subclavian artery was noted.
Six months later, the patient suffered from pulmonary tuberculosis. Treatment with isoniazid, rifampicin, ethambutol and pyrazinamide for 3 months was ineffective, and then turned to 4-aminosalicylic acid, protionamide, moxifloxacin and clarithromycin intermittent for 15 months, eventually achieving relief. Prednisone administration persisted throughout the procedure. During the follow-up, she developed great depression and was successfully rescued after taking 20 mg digoxin once herself. Forty-two months later, the patient returned again, being attacked by cervicodynia and dizziness for 4 months. Computed tomography angiography (CTA) revealed a considerable stenosis of the right brachiocephalic trunk, left common carotid artery and subclavian artery (Fig. 2B). Consultation for department of cardiovascular surgery was required and angioplasty will be undergone.
Discussion
TA affects generally the aorta and its main branches. An analysis of 108 Takayasu's arteritis patients in Korea demonstrated that in TA patients, according to the number of involved vascular lesions, the most commonly involved branches of the aorta is the subclavian artery (33.7%), the renal artery (25.3%) and the common carotid artery (21.7%), and the pulmonary artery comprised only 0.8%.44 Park MC, Lee SW, Park YB, Chung NS, Lee SK. Clinical characteristics and outcomes of Takayasu's arteritis: analysis of 108 patients using standardized criteria for diagnosis, activity assessment, and angiographic classification. Scand J Rheumatol. 2005;34:284-92. PMID: 16195161.
16195161...
Another report in 1994 of 60 patients seen at the National Institutes of Health (NIH) pointed out that two thirds of patients (65%) had aortic lesions, the most common site was in the carotid vessels (70%), and 4 of 60 patients (15%) had pulmonary artery stenosis and hypertension.22 Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takayasu's arteritis. Ann Intern Med. 1994;120:919-29. PMID: 7909656. While in Mexico, right heart catheterization and pulmonary angiography pointed out 50% pulmonary involvement in 22 patients.55 Lupi E, Sanchez G, Horwitz S, Gutierrez E. Pulmonary artery involvement in Takayasu's arteritis. Chest. 1975;67:69-74. PMID: 14812. Therefore, pulmonary arteritis involvement is not rare in the course of TA. Pulmonary artery involvement coexists generally with damage of the most common arteries such as described above. Nevertheless, it presented as the initial isolated presentation is seldom seen. One literature review performed in the Medline/PubMed database from 1975 to 2009 eventually found 14 patients with isolated pulmonary vasculitis and 8 patients with pulmonary involvement was the initial presentation.66 Toledano K, Guralnik L, Lorber A, Ofer A, Yigla M, Rozin A, et al. Pulmonary arteries involvement in Takayasu's arteritis: two cases and literature review. Semin Arthritis Rheum. 2011;41:461-70. PMID: 21803399.
21803399...
This patient experienced other new arteries involvement of the right brachiocephalic trunk, left common carotid artery and subclavian artery, 50 months after the first presenting manifestations.
Atypical presentations of TA with pulmonary symptoms contribute to an incorrect initial diagnosis. Clinical manifestations of systemic artery involvement appeared after several years, just as this case we report that vasculitis of brachiocephalic trunk, common carotid artery and subclavian artery appeared 3 years after the first presentation, resulting in an erroneous initial diagnosis. The pulmonary artery involvement confused TA with those of chronic thromboembolic diseases and pulmonary diseases leading to a misdiagnosis.77 Karadag B, Kilic H, Duman D, Ongen Z, Vural VA, Yazici H. Takayasu's disease with prominent pulmonary artery involvement: confusion with pulmonary disease leading to delayed diagnosis. Mod Rheumatol. 2008;18:507-510. PMID:18504527.
18504527...
Diseases of pulmonary vasculitis are classified into three categories according to imaging findings, localized nodular and patchy opacities (angiitis granulomatosis group), diffuse air space consolidation (diffuse pulmonary hemorrhage due to capillaritis), and aneurysm or stenosis of the large pulmonary arteries such as Takayasu's arteritis, Behcet's disease.88 Seo JB, Im JG, Chung JW, Song JW, Goo JM, Park JH, et al. Pulmonary vasculitis: the spectrum of radiological findings. Br J Radiol. 2000;73:1224-31. PMID: 11144805.9
11144805...
Despite the initial presentations of this patient are not specific, in a young female presenting with a clinical picture of acute pulmonary embolism and an elevated erythrocyte sedimentation rate (ESR) and CRP, with no risk factors for thromboembolic disease and no evidence of other systemic vasculitides of large vessels, TA must be considered in the differential diagnosis. The effective method to an early and accurate diagnosis should be considering TA in the differential diagnosis and active screening. Patients of TA without specific symptoms of vasculitis showed inflammatory activity in the vessel walls of the aorta for PET-CT with (18)F-FDG.99 Cabrera A, Caicedo AL, Elena A, Garrastachu MP, Caňete F, Ramirez R. PET-CT with 18F-FDG in the diagnosis of Takayasu's arteritis and the assessment of response to therapy. Rev Esp Med Nucl Imagen Mol. 2014;33:302-5. PMID: 24950891.
24950891...
Although clinically significant palliation usually occurred after angioplasty or bypass of severely stenotic vessels, restenosis was common.22 Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takayasu's arteritis. Ann Intern Med. 1994;120:919-29. PMID: 7909656.,1010 Hecht T, Esmaeili A, Behnke-Hall K. Balloon angioplasty of the bilateral renal arteries by Takayasu's arteritis with a paclitaxel-eluting balloon. Cardiol Young. 2014;8:1-4. PMID:25296292.
25296292...
,1111 Li D, Ma S, Li G, Chen J, Tang B, Zhang X, et al. Endovascular stent implantation for isolated pulmonary arterial stenosis caused by Takayasu's arteritis. Clin Res Cardiol. 2010;99:573-5. PMID: 20405135.
20405135...
Whereas, treatment of tricuspid valve annuloplasty and balloon dilatation in this patient pulse prolonged glucocorticoid administration have palliated both the pulmonary and cardiac conditions and stenotic bilateral pulmonary artery during 3-year follow-up, although stenosis of the right brachiocephalic trunk, left common carotid artery and subclavian artery occurred. Arteries reconstructed after surgical bypass may have superior patency to those reconstructed by endovascular treatment.1212 Kim YW, Kim DI, Park YJ, Yang SS, Lee GY, Kim DK, et al. Surgical bypass vs endovascular treatment for patients with supra-aortic arterial occlusive disease due to Takayasu's arteritis. J Vasc Surg. 2012;55:693-700. PMID: 22119246.
22119246...
Biologic therapy such as anti-TNF and anti-IL-6 receptor agents may be a useful adjunct to steroids.1313 Hoffman GS, Merkel PA, Brasington RD, Lenschow DJ, Liang P. Anti-tumor necrosis factor therapy in patients with difficult to treat Takayasu's arteritis. Arthritis Rheum. 2004;50:2296-304. PMID: 15248230.
15248230...
14 Nishimoto N, Nakahara H, Yoshio-Hoshino N, Mima T. Successful treatment of a patient with Takayasu's arteritis using a humanized anti-interleukin-6 receptor antibody. Arthritis Rheum. 2008;58:1197-200. PMID: 18383395.
18383395...
15 Tombetti E, Di Chio MC, Sartorelli S, Bozzolo E, Sabbadini MG, Manfredi AA, et al. Anti-cytokine treatment for Takayasu's arteritis: state of the art. Intractable Rare Dis Res. 2014;3:29-33. PMID: 25343124.
25343124...
-1616 Serra R, Grande R, Buffone G, Scarcello E, Tripodi F, Rende P, et al. Effects of glucocorticoids and tumor necrosis factor-alpha inhibitors on both clinical and molecular parameters in patients with Takayasu's arteritis. J Pharmacol Pharmacother. 2014;5:193-6. PMID: 25210399.
25210399...
In addition, this patient of TA suffered from pulmonary tuberculosis 6 months after the definite diagnosis of TA. A possible relationship between TA and infection with Mycobacterium tuberculosis has been suggested, but not proven.1717 van Timmeren MM, Heeringa P, Kallenberg CG. Infectious triggers for vasculitis. Curr Opin Rheumatol. 2014;26:416-23. PMID: 24827750.
24827750...
Positive purified protein derivation (PPD) tests for tuberculin were found high in TA patients.1818 Pantell RH, Goodman BW. Takayasu's arteritis: the relationship with tuberculosis. Pediatrics. 1981;67:84-8. PMID:6113574.M. tuberculosis may contribute to the development of TA via its production of superantigens and the elevated proinflammatory cytokines.1919 Castillo-Martínez D, Amezcua-Guerra LM. Self-reactivity against stress-induced cell molecules: the missing link between Takayasu's arteritis and tuberculosis?. Med Hypotheses. 2012;78:485-8. PMID: 22285197.
22285197...
Further study of the relationship between TA and tuberculosis may show the exact role of M. tuberculosis in the pathogenesis of Takayasu's arteritis.
References
-
1Kerr KM, Auger WR, Fedullo PF, Channick RH, Yi ES, Moser KM. Large vessel pulmonary arteritis mimicking chronic thromboembolic disease. Am J Respir Crit Care Med. 1995;152:367-73. PMID: 7599847.
-
2Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, et al. Takayasu's arteritis. Ann Intern Med. 1994;120:919-29. PMID: 7909656.
-
3Subramanyan R, Joy J, Balakrishnan KG. Natural history of aortoarteritis (Takayasu's disease). Circulation. 1989;80:429-37. PMID: 2569946.
-
4Park MC, Lee SW, Park YB, Chung NS, Lee SK. Clinical characteristics and outcomes of Takayasu's arteritis: analysis of 108 patients using standardized criteria for diagnosis, activity assessment, and angiographic classification. Scand J Rheumatol. 2005;34:284-92. PMID: 16195161.
» 16195161 -
5Lupi E, Sanchez G, Horwitz S, Gutierrez E. Pulmonary artery involvement in Takayasu's arteritis. Chest. 1975;67:69-74. PMID: 14812.
-
6Toledano K, Guralnik L, Lorber A, Ofer A, Yigla M, Rozin A, et al. Pulmonary arteries involvement in Takayasu's arteritis: two cases and literature review. Semin Arthritis Rheum. 2011;41:461-70. PMID: 21803399.
» 21803399 -
7Karadag B, Kilic H, Duman D, Ongen Z, Vural VA, Yazici H. Takayasu's disease with prominent pulmonary artery involvement: confusion with pulmonary disease leading to delayed diagnosis. Mod Rheumatol. 2008;18:507-510. PMID:18504527.
» 18504527 -
8Seo JB, Im JG, Chung JW, Song JW, Goo JM, Park JH, et al. Pulmonary vasculitis: the spectrum of radiological findings. Br J Radiol. 2000;73:1224-31. PMID: 11144805.9
» 11144805 -
9Cabrera A, Caicedo AL, Elena A, Garrastachu MP, Caňete F, Ramirez R. PET-CT with 18F-FDG in the diagnosis of Takayasu's arteritis and the assessment of response to therapy. Rev Esp Med Nucl Imagen Mol. 2014;33:302-5. PMID: 24950891.
» 24950891 -
10Hecht T, Esmaeili A, Behnke-Hall K. Balloon angioplasty of the bilateral renal arteries by Takayasu's arteritis with a paclitaxel-eluting balloon. Cardiol Young. 2014;8:1-4. PMID:25296292.
» 25296292 -
11Li D, Ma S, Li G, Chen J, Tang B, Zhang X, et al. Endovascular stent implantation for isolated pulmonary arterial stenosis caused by Takayasu's arteritis. Clin Res Cardiol. 2010;99:573-5. PMID: 20405135.
» 20405135 -
12Kim YW, Kim DI, Park YJ, Yang SS, Lee GY, Kim DK, et al. Surgical bypass vs endovascular treatment for patients with supra-aortic arterial occlusive disease due to Takayasu's arteritis. J Vasc Surg. 2012;55:693-700. PMID: 22119246.
» 22119246 -
13Hoffman GS, Merkel PA, Brasington RD, Lenschow DJ, Liang P. Anti-tumor necrosis factor therapy in patients with difficult to treat Takayasu's arteritis. Arthritis Rheum. 2004;50:2296-304. PMID: 15248230.
» 15248230 -
14Nishimoto N, Nakahara H, Yoshio-Hoshino N, Mima T. Successful treatment of a patient with Takayasu's arteritis using a humanized anti-interleukin-6 receptor antibody. Arthritis Rheum. 2008;58:1197-200. PMID: 18383395.
» 18383395 -
15Tombetti E, Di Chio MC, Sartorelli S, Bozzolo E, Sabbadini MG, Manfredi AA, et al. Anti-cytokine treatment for Takayasu's arteritis: state of the art. Intractable Rare Dis Res. 2014;3:29-33. PMID: 25343124.
» 25343124 -
16Serra R, Grande R, Buffone G, Scarcello E, Tripodi F, Rende P, et al. Effects of glucocorticoids and tumor necrosis factor-alpha inhibitors on both clinical and molecular parameters in patients with Takayasu's arteritis. J Pharmacol Pharmacother. 2014;5:193-6. PMID: 25210399.
» 25210399 -
17van Timmeren MM, Heeringa P, Kallenberg CG. Infectious triggers for vasculitis. Curr Opin Rheumatol. 2014;26:416-23. PMID: 24827750.
» 24827750 -
18Pantell RH, Goodman BW. Takayasu's arteritis: the relationship with tuberculosis. Pediatrics. 1981;67:84-8. PMID:6113574.
-
19Castillo-Martínez D, Amezcua-Guerra LM. Self-reactivity against stress-induced cell molecules: the missing link between Takayasu's arteritis and tuberculosis?. Med Hypotheses. 2012;78:485-8. PMID: 22285197.
» 22285197
Publication Dates
-
Publication in this collection
Nov-Dec 2017
History
-
Received
3 Apr 2015 -
Accepted
13 Oct 2015