Abstracts
PURPOSE: This 3D-finite elements method study evaluated the effect of bone resorption on the stress distribution in overdentures with bone loss surrounding implants and resorption of the distal ridge. METHODS: Tridimensional models were built from the images of a computerized tomography of a mandible and 3D laser digitalization of implants, abutments, mucosa, and complete denture. The geometric models of implants and abutments were mounted at the canine region to build reference model 1 - absence of bone resorption. To build the test models the mandible geometric solid was modified to simulate 2-mm vertical bone loss surrounding the implants (model 2) and resorption of the distal ridge (model 3). Finite elements models were generated, and a 100 N static load was applied at the first molar region of each model to compare the von Mises stress distributions in selected points. RESULTS: Von Mises stresses increased on the bone surrounding implants and on the prosthetic components in the model with 2-mm vertical bone loss. The combination of 2-mm vertical bone loss and resorption of the distal ridge did not increase the stresses compared with the model with only bone loss surrounding implants. The highest stress concentration at marginal bone and implants occurred on the same side of the vertical load application for all models. CONCLUSION: The results suggest that the bone loss surrounding implants increases stress concentration in dental implants, abutments, and marginal bone independently from the bone resorption of the distal ridge.
Dental implants; overdenture; biomechanics; finite element analysis
OBJETIVO: Avaliar, através da análise por elementos finitos com modelo tridimensional, o efeito da reabsorção óssea na distribuição de tensões em prótese tipo overdenture, em situações de perda óssea ao redor dos implantes e reabsorção do rebordo posterior. METODOLOGIA: Foram construídos modelos tridimensionais de uma mandíbula e de intermediários protéticos, prótese total, placa resiliente e implante. Os modelos geométricos dos implantes e intermediários protéticos foram montados na região dos caninos, constituindo o modelo 1. Para a construção dos modelos experimentais, o contorno do modelo geométrico da mandíbula foi alterado para simular a perda óssea nos implantes (modelo 2) e a reabsorção do rebordo posterior associada à perda óssea marginal nos implantes (modelo 3). Para gerar a malha de elementos finitos os materiais foram considerados homogêneos, isotrópicos e linearmente elásticos. Uma carga de 100 N foi aplicada indiretamente, sobre uma simulação de bolo alimentar, na região de primeiro molar inferior direito em cada um dos três modelos. Foram analisadas as distribuições de tensão de von Mises em pontos pré-determinados. RESULTADOS: A reabsorção óssea do rebordo posterior associada à perda óssea do osso periimplantar promoveu maior concentração de tensões nos implantes, nos componentes protéticos e no tecido ósseo marginal. Houve maior concentração de tensões no osso periimplantar e nos implantes no mesmo lado de aplicação da carga. CONCLUSÃO: Os resultados sugerem que a perda óssea periimplantar aumenta a concentração de tensões nos implantes, pilares e osso marginal independentemente da reabsorção óssea na crista distal.
Implantes dentários; sobredentadura; biomecânica; análise por elementos finitos
ORIGINAL ARTICLE
Stresses in implant-supported overdentures with bone resorption: a 3-D finite element analysis
Tensões em sobredentaduras com reabsorção óssea: análise por elementos finitos tridimensional
Luiz Oscar Honorato MarianoI; Evandro Afonso SartoriI; Josué Ricardo BroiloI; Rosemary Sadami ShinkaiI; Leandro CorsoII; Rogério José MarczakIII
IGraduate Program in Dentistry, Pontifical Catholic University of RioGrande do Sul, Porto Alegre, RS, Brazil
IIDepartment of Engineering, University of Caxias do Sul, Caxias do Sul, RS, Brazil
IIIDepartment of Mechanical Engineering, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil
Correspondence Correspondence: Luiz Oscar Honorato Mariano Universidade do Sul de Santa Catarina Departamento de Ciências Biológ. e da Saúde e de Ciências Soc. Aplicadas Avenida José Acácio Moreira, 787 Dehon Tubarão, SC Brasil 88704-900 E-mail: luizoscarhm@hotmail.com
ABSTRACT
PURPOSE: This 3D-finite elements method study evaluated the effect of bone resorption on the stress distribution in overdentures with bone loss surrounding implants and resorption of the distal ridge.
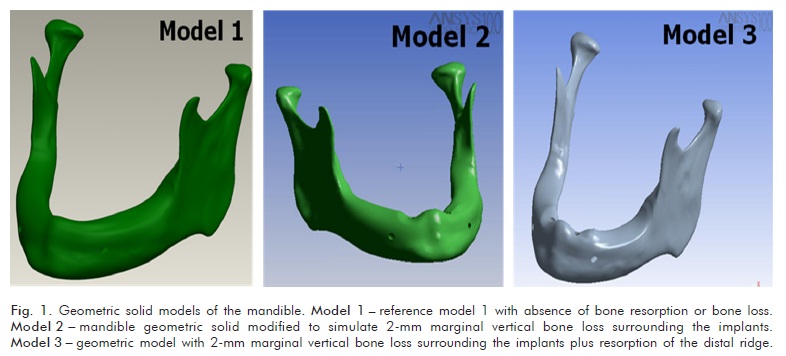
METHODS: Tridimensional models were built from the images of a computerized tomography of a mandible and 3D laser digitalization of implants, abutments, mucosa, and complete denture. The geometric models of implants and abutments were mounted at the canine region to build reference model 1 - absence of bone resorption. To build the test models the mandible geometric solid was modified to simulate 2-mm vertical bone loss surrounding the implants (model 2) and resorption of the distal ridge (model 3). Finite elements models were generated, and a 100 N static load was applied at the first molar region of each model to compare the von Mises stress distributions in selected points.
RESULTS: Von Mises stresses increased on the bone surrounding implants and on the prosthetic components in the model with 2-mm vertical bone loss. The combination of 2-mm vertical bone loss and resorption of the distal ridge did not increase the stresses compared with the model with only bone loss surrounding implants. The highest stress concentration at marginal bone and implants occurred on the same side of the vertical load application for all models.
CONCLUSION: The results suggest that the bone loss surrounding implants increases stress concentration in dental implants, abutments, and marginal bone independently from the bone resorption of the distal ridge.
Key words: Dental implants; overdenture; biomechanics; finite element analysis
RESUMO
OBJETIVO: Avaliar, através da análise por elementos finitos com modelo tridimensional, o efeito da reabsorção óssea na distribuição de tensões em prótese tipo overdenture, em situações de perda óssea ao redor dos implantes e reabsorção do rebordo posterior.
METODOLOGIA: Foram construídos modelos tridimensionais de uma mandíbula e de intermediários protéticos, prótese total, placa resiliente e implante. Os modelos geométricos dos implantes e intermediários protéticos foram montados na região dos caninos, constituindo o modelo 1. Para a construção dos modelos experimentais, o contorno do modelo geométrico da mandíbula foi alterado para simular a perda óssea nos implantes (modelo 2) e a reabsorção do rebordo posterior associada à perda óssea marginal nos implantes (modelo 3). Para gerar a malha de elementos finitos os materiais foram considerados homogêneos, isotrópicos e linearmente elásticos. Uma carga de 100 N foi aplicada indiretamente, sobre uma simulação de bolo alimentar, na região de primeiro molar inferior direito em cada um dos três modelos. Foram analisadas as distribuições de tensão de von Mises em pontos pré-determinados.
RESULTADOS: A reabsorção óssea do rebordo posterior associada à perda óssea do osso periimplantar promoveu maior concentração de tensões nos implantes, nos componentes protéticos e no tecido ósseo marginal. Houve maior concentração de tensões no osso periimplantar e nos implantes no mesmo lado de aplicação da carga.
CONCLUSÃO: Os resultados sugerem que a perda óssea periimplantar aumenta a concentração de tensões nos implantes, pilares e osso marginal independentemente da reabsorção óssea na crista distal.
Palavras-chave: Implantes dentários; sobredentadura; biomecânica; análise por elementos finitos
Introduction
The main complaint reported by edentulous patients refers to the instability of the complete denture particularly in the mandible. Complete oral rehabilitation including dental implants is a viable clinical treatment option for total edentulous patients, with good acceptance on functional, comfort and social aspects. However, the implant-supported fixed prostheses are an expensive treatment due to the complexity of surgical and prosthetic phases, cost of implants and prosthetic components and laboratory fees. The overdenture is an alternative to fixed implant-supported prosthesis for its relatively low cost and clinical indication in cases of impossibility of placing multiple implants with appropriate number and arrangement in the arch to support a fixed prosthesis (1).
The traditional implant-supported overdenture has a minimum of two implants inserted in the region of the mandibular canines (2). This type of treatment helps reducing the resorption rate of the anterior ridge and increasing denture retention and stability, so that patients with overdentures report greater satisfaction than with conventional complete dentures (3-7). Another point in favor of overdentures is the increased proprioception during speech and mastication with greater movement of the tongue and facial muscles and improved patient confidence (8). In comparison with an implant-supported fixed prosthesis, the overdenture also has the advantage of allowing easier cleaning as they are removable and supported by fewer number of implants (9).
The mandibular bone loss inevitably occurs after the extraction of teeth, and the resorption of the posterior ridge is not prevented with the installation of implants in the anterior region (10-12). A marginal periimplantar bone loss of approximately 1 mm in the first year and of additional 0.1 mm annually has been reported as normal in the literature (13-15). This rate of bone loss can vary due to unfavorable conditions of masticatory loading and plaque accumulation on the implant sites, which could compromise the prognosis of the oral rehabilitation treatment over the years since it is related to the preservation of the supporting tissues. The literature is scarce about the influence of posterior ridge resorption combined with periimplantar bone loss on the biomechanics of implants and overdentures when subjected to masticatory loads. The finite element method is a computer-based simulation of the biomechanical behavior of complex structures by means of numerical analysis and may help to understand some patterns of stress distribution under function (16,17).
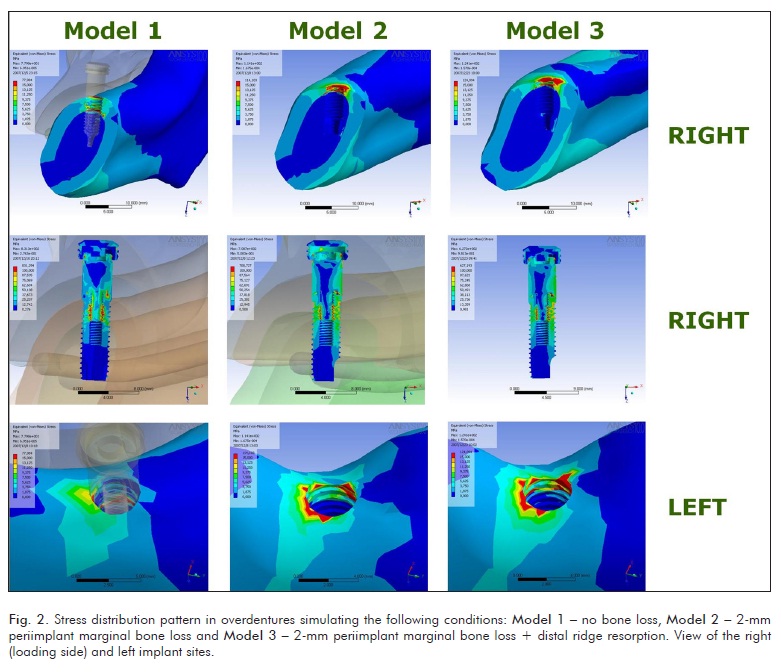
This study used a finite element analysis with three-dimensional model to evaluate the effect of bone resorption on stress distribution in mandibular overdentures under a vertical static load. This study has a comparative, descriptive design to evaluate stress distribution pattern in overdentures simulating the following conditions: 1) no loss of marginal bone around dental implants, 2) marginal bone loss of 2mm around the implants, and 3) resorption of the posterior ridge of the mandible associated with marginal bone loss 2 mm around the implants. The a priori hypothesis was that posterior ridge resorption associated with marginal periimplantar bone loss affects the biomechanics of the overdenture system and modify the stress distribution pattern in the bone, implant and prosthetic components.
Materials and methods
The research protocol was approved by the Institutional Review Board of the Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil.
Generation of 3D geometric solid models
The materials used to obtain the solid models were: a dry edentulous mandible from the collection of the Discipline of Dental Radiology, a 4.0 × 11.5 mm standard implant (3i Implant Innovations, Palm Beach, Florida, USA), a 4 mm Locator® attachment (3i Implant Innovations, Palm Beach, Florida, USA), a conventional complete denture and a 3 mm-thick resilient silicone mucosa simulation.
Seventy 1 mm-thick slices of the mandible were obtained by means of a helical computed tomography using a spiral CT GE HiSpeed CTI System Series 6.4 (GE Healthcare, Waukesha, USA). The tridimensional images with 1 mm of gap between sections were scanned using the softwares programs Matlab® (The MathWorks, Natick, Massachusetts, USA) and Rhynoceros 3D® version 3.0 (McNeel and Associates, Seattle, USA) to extract the coordinates of points necessary for the creation of images of the geometric surface of the mandible, which had been worked into the program SolidWorks® 2005 (SolidWorks Corporation, Concord, Massachusetts, USA) for smoothing and generation of a continuous model (predictive engineering) made internally by cortical and cancellous bone. The assembly of the computational geometric model was performed only for half of the sections generated by the CT scan, and by symmetry it was generated the entire mandibular 3D geometric model without bone loss (model 1 reference model). For the construction of the test models, the outline of the geometric model of the mandible was altered to simulate the 2 mm periimplantar bone loss (model 2) and the bone resorption of the posterior ridge of the mandible associated with 2 mm periimplant bone loss (model 3) (Fig. 1).
The 3D models of the complete denture, resilient mucosa simulation, implant and components were created using a laser scanning system (Digimil 3D Tecnodrill®, Novo Hamburgo, RS, Brazil). A computer file was generated with extension. "Txt" from coordinates x, y, z from each point of the scanned external surfaces. This file was opened in Geomagic® software v. 7.0 (Raindrop, Research Triangle Park, USA), where a cloud of points with 0.07 mm between each point was obtained. In the software the images were cleaned beforehand, and then 3D images of the prototypes of the research began to be visualized. A second and final cleaning was done (removal of islands of solid) so that small imperfections in the shape of the structures or digitized artifacts were corrected and a treatment of the cloud of points with the software tools. After this, a new file format was created with the extension ".STL" where only the outer 3D shape of material used was available. The images were saved in ".iges" and exported to Rhynoceros® software version 3.0 (McNeel and Associates, Seattle, USA), in which the manipulation of images allowed the design of the study prototypes. The geometric models of implants and prosthetic components were mounted in the canines region of the mandibular model with the mucosa simulation.
Generation of the 3D finite element models and stress analysis
The final ".iges" geometric models were exported to a software (ANSYS 10.0, ANSYS Inc., Houston, Texas, USA) to generate the finite element mesh. Isoparametric quadratic tetrahedral elements were used (four triangular faces and 10 nodes) for the discretization of the mandibles, implants and prosthetic components. In relation to contact between the components of the model, it was adopted a situation of perfect contact between implants and bone tissue. To impose restrictions on movement of the rigid body model, restrictions have been adopted for all degrees of freedom for each node found in the articular surface of the condyles and the regions of insertion of the masticatory muscles (masseter, temporalis, medial pterygoid and lateral pterygoid) (16,17). The physical properties of the materials used were extracted from the literature (Table 1), and the materials were considered homogeneous, isotropic and linearly elastic.
A load of 100 N was applied to the model indirectly over a simulation of a masticatory bolus, which was shaped as a semi-sphere in contact with the right first molar. The distributions of von Mises stresses induced by the applied loads on the three models were qualitatively analyzed in selected areas: 1) periimplant cortical bone and 2) implants and prosthetic components.
Results
Figure 2 displays the stress distribution pattern in selected areas of the models 1, 2 and 3. For all models the highest stress concentration at marginal bone and implants occurred on the same side of the vertical load application (right side).
The Von Mises stresses increased on the periimplant marginal bone and in the prosthetic components in the model with 2-mm vertical bone loss. As the layer of cortical bone was thinner in the models with periimplant bone loss (models 2 and 3), the stresses were located closer to the platform of the implant in comparison with model 1. Thus, the right and left implants in the models 2 and 3 showed larger area of high stress and also maximum values than model 1. There was a similar stress distribution pattern in the periimplant region of the models 2 and 3. Only the left periimplant region of the model without bone loss (model 1) did not show stress values considered critical, which are represented by areas in red color.
Discussion
After completion of treatment with overdentures, changes in the support structures of implants and prostheses may occur over time, mainly periimplantar marginal bone loss and ridge resorption (5,18,19). In the tested models of implant-supported overdentures, the periimplant marginal bone loss increased stress concentration in dental implants, abutments, and marginal bone independently from the bone resorption of the distal ridge. The combination of 2-mm vertical bone loss and resorption of the distal ridge (model 3) did not substantially modify the stress distribution pattern and magnitude compared with the model with only periimplant marginal bone loss (model 2). This finding indicates that an overdenture supported by two implants may not have a negative biomechanical prognosis for patients with distal ridge resorption if adequate support is given by the denture bearing area.
Previous studies (14,20) related the progressive marginal bone loss with increasing values of tension in the cervical area of the implant and the support bone tissue. In the present research, the thickness of cortical bone tissue was reduced in the region of periimplantar bone loss, since the layer of cortical bone tissue narrows as bone remodeling occurs due to the occlusal stimuli that promote progressive marginal bone loss (20). Thus, this may have been one of the causes on the wider distribution of tension in the cortical layer, since the area for dissipation of the applied force decreased. This explanation is consistent with the finite elements study by Sevimay et al. (21), in which the authors found that implants placed in the region of small thickness of cortical bone and poor quality of cancellous bone showed higher micromovement under occlusal loads and higher concentration of stresses in the adjacent bone tissue. Another possible explanation for the tensions to be higher in the region of periimplant bone loss would be the dislocation to the apex of the fulcrum of rotation in the cervical implant region due to lower insertion of the latter in the bone tissue.
Only Von Mises stresses of low magnitude were observed in the cancellous bone tissue, whereas different patterns of stress concentration occurred in cortical bone tissue. This happens because the elasticity modulus of the two types of bone is very different, and the stress distribution is also modified in the cancellous bone with variable bone density (22). The high values of stress concentration in the cortical bone may indicate increased participation in the absorption of functional loads transmitted by the implant-supported prosthesis (17).
For the current study, it was simulated an application of a vertical load of 100 N, which is considered a physiological value in edentulous patients and sufficient to obtain significant results in previous studies with finite element (16). It was observed that the largest gradient forces in the bone periimplantar marginal regions occurred on the right side, close to the place of application of vertical loading, corresponding to the right first molar. Probably the prosthesis loading in other places and in different angulation may produce a different behavior of the stress distribution in bone tissue and implants (16). Although the greatest concentrations of stresses have been observed in the right implant models with bone resorption, the right implant of the model without bone loss presented visually wider distribution of high values of tension along its structure than the left implant model with periimplant bone loss. This fact showed that the implant closest to the point of load application on the prosthesis always suffers greater mechanical stress in overdentures, both in great deployment situations as after marginal bone loss.
The analysis of the stresses transmitted to the structures of the implants and bone by three-dimensional finite element method has shown similar results when compared with mechanical tests (17,23). However, the results of computer simulations do not reflect the clinical reality even with a precise geometric modeling and refinement of the mathematical model (23). Regarding the elements used to generate the mesh, it was used the geometry of quadratic isoparametric tetrahedron, since this form has allowed better representation of the contour of the surfaces of solids of the study, and has simple approaches, enabling its use in greater numbers to obtain a solution with higher precision. The use of CT scan images of the entire mandible contributed to the precise reconstruction of the geometric model faster than other methods using histological slices (24). The refinement of the model was carried out to remove unnecessary irregularities, since the more complex geometry, the more complex the mesh generation. It was necessary to adopt simplifying assumptions in accordance with the requirements of computational resources and the impossibility of perfectly copying the functioning of human structures because of the variation within subjects. Another limitation is related to the physical properties of the tested materials, which were considered homogeneous, isotropic and linearly elastic. Also, a linear analysis was used with load application statically, concentrated, and axial. However, bone is heterogeneous and anisotropic, i.e., it presents different mechanical properties throughout its structure and viscoelastic characteristics that vary according to the direction of the load application.
In summary, this study showed that the Von Mises stresses increased on the periimplant marginal bone and prosthetic components in the model with 2-mm vertical bone loss (model 2). However, the combination of 2-mm vertical bone loss and resorption of the distal ridge (model 3) did not increase the stresses compared with the model with only periimplant marginal bone loss (model 2). The results of this study are consistent with the studies of Kitamura et al. (14) and Akca and Cehreli (20), in which the authors stated that in implants with marginal bone loss and subjected to non-axial forces there is a greater concentration of tension in both the neck of implant and the adjacent bone. Another important finding was that bone resorption of the posterior ridge did not promote a great increase in the gradient of stresses around the implants. Likewise, there is no scientific data indicating that the resorption of the posterior ridge increases the stress concentration in the implant. This is a reminder of the need for periodic checkups that include plaque control, relining and occlusal evaluation of the prosthesis in order to minimize or eliminate risk factors that would lead to marginal bone loss of implants, altering the biomechanics of the system (25). This would eliminate a continuous cycle where bone loss is a consequence of stress concentration, and the converse is also true, that would jeopardize the longevity of implants by the progressive and accelerated loss of marginal bone tissue.
Although they have limitations, computer simulations allow the analysis of complex biomechanical systems that can be easily modified and tested without risk to patients to justify the clinical use of new forms of treatment. Therefore, further studies should evaluate other factors related to the biomechanics of implant-supported overdentures aiming to increase the predictability of long-term success of this treatment modality.
Acknowledgements
This study was partially supported by the Brazilian Ministry of Education/CAPES. This paper is derived from the Masters dissertation by Dr. Luiz O. Mariano at the Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil, and the related poster was presented at the 2010 IADR Annual Meeting in Barcelona, Spain.
- 1. Batenburg RH, Meijer HJ, Raghoebar GM, Vissink A. Treatment concept for mandibular overdentures supported by endosseous implants: a literature review. Int J Oral Maxillofac Implants 1998;13:539-45.
- 2. Jemt T. Implant treatment in elderly patients. Int J Prosthodont 1993;6:456-61.
- 3. Naert I, Gizani S, Vuylsteke M, Van Steenberghe D. A 5-year prospective randomized clinical trial on the influence of splinted and unsplinted oral implants retaining a mandibular overdenture: prosthetic aspects and patient satisfaction. J Oral Rehabil 1999;26:195-202.
- 4. Sadowsky S. Mandibular implant-retained overdentures: a literature review. J Prosthet Dent 2001;86:468-73.
- 5. Wright PS, Glantz PO, Randow K, Watson RM. The effects of fixed and removable implant-stabilised prostheses on posterior mandibular residual ridge resorption. Clin Oral Implants Res 2002;13:169-74.
- 6. Walton JN, MacEntee MI, Glick N. One-year prosthetic outcomes with implant overdentures: a randomized clinical trial. Int J Oral Maxillofac Implants 2002;17:391-8.
- 7. Visser A, Meijer HJ, Raghoebar GM, Vissink A. Implant-retained mandibular overdentures versus conventional overdentures: 10 years of case and aftercare. Int J Prosthodont 2006;19:271-8.
- 8. Truhlar RS, Casino AJ, Cancro JJ. Treatment planning in the elderly implant patient. Dental Clin North Am 1997;41:847-61.
- 9. Parel SM, Balshi TJ, Sullivan DY. Modifications of existing prosthesis with osseointegrated implants. J Prosthet Dent 1986;56:195-202.
- 10. Suenaga K, Sato T, Nishigawa G, Minagi S. Relationship between size of denture foundation area and resorption of alveolar ridge in the edentulous mandible. J Oral Rehabil 1997;24:315-9.
- 11. Burns DR. Mandibular implant overdenture treatment: Consensus and Controversy. J Prosthodont 2000;9:37-46.
- 12. Kordatzis K, Wright PS, Meijer HJ. Posterior mandibular residual ridge resorption in patients with conventional dentures and implant overdentures. . Int J Oral Maxillofac Implants 2003;18:447-52.
- 13. Jung YC, Han CH, Lee KW. A 1-year radiographic evaluation of marginal bone around dental implants. . Int J Oral Maxillofac Implants 1996;11:811-8.
- 14. Kitamura E, Stegaroiu R, Nomura S, Miyakawa O. Influence of marginal bone resorption on stress around an implant a three-dimensional finite element analysis. J Oral Rehabil 2005;32:279-86.
- 15. Meijer HJ, Raghoebar GM, Van't Hof MA, Visser A. A controlled clinical trial of implant-retained mandibular overdentures: 10 years results of clinical aspects and aftercare of IMZ implants and Branemark implants. Clin Oral Implants Res 2000;11:441-7.
- 16. Daas M, Dubois G, Bonnet AS, Lipinski P, Rignon-Bret C. A complete finite element model of a mandibular implant-retained overdenture with two implants: Comparison between rigid and resilient attachment configurations. Med Eng Physics 2008;2:1-8.
- 17. Natali AN, Pavan PG, Ruggero AL. Analysis of bone-implant interaction phenomena by using a numerical approach. Clin Oral Implants Res 2006;17:67-74.
- 18. van Steenberghe D, Quirynen M, Naert I, Maffei G, Jacobs R. Marginal bone loss around implants retaining mandibular overdentures at 4-, 8-, and 12-years follow-up. J Clin Periodontol 2001;28:628-33.
- 19. Blum IR, McCord JF. A clinical investigation of the morphological changes in the posterior mandible when implant-retained overdentures are used. Clin Oral Impl Res 2004;15:700-8.
- 20. Akca K, Cehreli MK. Biomechanical consequences of progressive marginal bone loss around oral implants: a finite element stress analysis. Med Biol Eng Comput 2006;44:527-35.
- 21. Sevimay M, Turhan F, Kiliçarslan MA, Eskitascioglu G. Three-dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. J Prosthet Dent 2005;93:227-34.
- 22. Correia A, Piloto P, Campos JC, Vaz M. Finite element analysis of the mechanical behavior of a partially edentulous mandible as a function of cancellous bone density. Rev Odonto Cienc 2009;24:22-27.
- 23. Merz BR, Hunenbart S, Belser UC. Mechanics of the implant abutment connection: an 8-degree taper compared to a butt joint connection. . Int J Oral Maxillofac Implants 2000;15:519-26.
- 24. Sato Y, Teixeira ER, Tsuga K, Shindoi N. The effectiveness of a new algorithm on a three-dimensional finite element model construction of bone trabeculae in implant biomechanics. J Oral Rehabil 1999;26:640-3.
- 25. Atwood DA. Some clinical factors related to rate of resorption of residual ridges. J Prosthet Dent 2001;86:119-25.
Correspondence:
Publication Dates
-
Publication in this collection
24 May 2012 -
Date of issue
2012