Cardiovascular Diseases; Coronary Disease; Cardiomyopathies; Heart Failure; Heart Valve Diseases; Atrial Fibrillation; Atrial Flutter; Statistics; Brazil
About these statistics
Abbreviations Used in ‘About These Statistics’ and Highlights
| AF | Atrial Fibrillation |
| AMI | Acute Myocardial Infarction |
| CABG | Coronary Artery Bypass Grafting |
| CI | Confidence Interval |
| CV | Cardiovascular |
| CVD | Cardiovascular Disease |
| DALY | Disability-Adjusted Life Year |
| FU | Federative Unit |
| GBD | Global Burden of Disease |
| GDP | Gross Domestic Product |
| HR | Hazard Ratio |
| HS | Hemorrhagic Stroke |
| IBGE | Brazilian Institute of Geography and Statistics (in Portuguese, Instituto Brasileiro de Geografia e Estatística ) |
| ICD | International Statistical Classification of Diseases and Related Health Problems |
| IHD | Ischemic Heart Disease |
| IHME | Institute for Health Metrics and Evaluation |
| Int$ | International dollars |
| IPCA | Brazilian Consumer Price Index (in Portuguese, Índice de Preços ao Consumidor Amplo ) |
| IRR | Incidence Rate Ratio |
| IS | Ischemic Stroke |
| NRVD | Non-Rheumatic Valvular Heart Disease |
| OR | Odds Ratio |
| PCI | Percutaneous Coronary Intervention |
| PNS | National Health Survey (in Portuguese, Pesquisa Nacional de Saúde ) |
| PPP | Purchasing Power Parity |
| R$ | Reais , Brazilian currency |
| RHD | Rheumatic Heart Disease |
| SAH | Subarachnoid Hemorrhage |
| SDI | Sociodemographic Index |
| SIH | Brazilian Hospital Information System (in Portuguese, Sistema de Informações Hospitalares ) |
| SIM | Brazilian Mortality Information System (in Portuguese, Sistema de Informações sobre Mortalidade ) |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| UI | Uncertainty Interval |
| US$ | US dollars |
| YLD | Year Lived with Disability |
| YLL | Year of Life Lost |
This is the 2021 edition of the Cardiovascular Statistics - Brazil , a multi-institutional effort to periodically provide updated information on the epidemiology of heart diseases and stroke in Brazil. The report incorporates official statistics provided by the Brazilian Ministry of Health and other government agencies, by the GBD project led by the IHME of the University of Washington, as well as data generated by other sources and scientific studies, such as cohorts and registries, on CVDs and their risk factors. The document is directed to researchers, clinicians, patients, healthcare policy makers, media professionals, the public, and others who seek comprehensive national data available on heart disease and stroke.
The Cardiovascular Statistics – Brazil 2021 is an updated and expanded version of the Cardiovascular Statistics – Brazil 2020 , 11. Oliveira GMM, Brant LCC, Polanczyk CA, Biolo A, Nascimento BR, Malta DC, Souza MFM, Soares GP, Xavier GF Jr, Machline-Carrion MJ, Bittencourt MS, Pontes Neto OM, Silvestre OM, Teixeira RA, Sampaio RO, Gaziano TA, Roth GA, Ribeiro ALP. Cardiovascular Statistics - Brazil 2020. Arq Bras Cardiol. 2020;115(3):308-439. doi: 10.36660/abc.20200812. published last year in the ABC Cardiol. It includes the most recent data on CVD as a group of conditions and five specific CVDs covered by the 2020 document, in addition to new chapters on CV risk behaviors and factors, specifically hypertension, diabetes, dyslipidemia, obesity, and smoking and tobacco use. The work was conducted by volunteer researchers from several Brazilian Universities and research institutions led by a steering committee of five members (ALPR, CAP, DCM, GMMO, and LCCB), with the support of the Brazilian Society of Cardiology and the collaboration of the GBD Brazil Network 22. Malta DC, Passos VMA, Machado ÍE, Marinho Souza MF, Ribeiro ALP. The GBD Brazil Network: Better Information for Health Policy Decision-Making in Brazil. Popul Health Metr. 2020;18(Suppl 1):23. doi: 10.1186/s12963-020-00224-1. and of an International Committee (GAR, PP, and TAG). The document follows the methodology used by the American Heart Association to produce the annual Heart Disease & Stroke Statistics Update , 33. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):254-743. doi: 10.1161/CIR.0000000000000950. which emphasizes epidemiological and public health data. The Cardiovascular Statistics – Brazil neither gives information on pathophysiological mechanisms nor makes treatment recommendations. Unlike guidelines and position papers, it intends to present the newest and best health-related metrics of CVD statistics of the Brazilian population.
Data used in the present document have four different sources: (a) the Brazilian Mortality and Hospital Information Systems, provided by the government; (b) the GBD 2019 estimates; 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. (c) the systematic review of the literature with emphasis on the publications of the last 10 years; (d) the health care utilization costs, based on the reimbursement tables from the Public Health System, adjusted for inflation and reported in both original currency units (Reais or US dollars in a specific year) and international dollars. The international dollars were converted to PPP adjusted to US$ 2019 (Int$ 2019) using the Campbell and Cochrane Economics Methods Group and the Evidence for Policy and Practice Information and Coordinating Centre cost converter. 55. Shemilt I, Thomas J, Morciano M. A Web-Based Tool for Adjusting Costs to a Specific Target Currency and Price Year. Evid. Policy. 2010;6(1):51-9. doi:10.1332/174426410X482999. Better explanation on how mortality rate estimates can vary depending on the source used (mortality information system or GBD datasets) can be seen elsewhere. 66. Malta DC, Teixeira R, Oliveira GMM, Ribeiro ALP. Cardiovascular Disease Mortality According to the Brazilian Information System on Mortality and the Global Burden of Disease Study Estimates in Brazil, 2000-2017. Arq Bras Cardiol. 2020;115(2):152-160. doi: 10.36660/abc.20190867.
https://doi.org/10.36660/abc.20190867...
As expected, different or discordant metrics are sometimes presented for a single condition, considering that studies may have distinct methodologies or were conducted in different time periods, locations, and age ranges. These differences are unavoidable, and their possible reasons are always discussed in this document. Since many studies cover a long period of time and life expectancy increased in Brazil in the last decades, we used age-standardized rates, i.e., a weighted average of the age-specific rates per 100 000 persons, in which the weights are the proportions of people in the corresponding age groups of a standard population. The GBD age-standardization uses a global age pattern, although other sources may have used different reference populations. For most studies, race/skin color was used according to the IBGE definition, i.e., white, black, brown, yellow (oriental), and indigenous.
Cardiovascular disease is still responsible for nearly one third of deaths in Brazil and affects disproportionally the most vulnerable stratum of the population, which has marked difficulties in accessing high quality health care. 77. Castro MC, Massuda A, Almeida G, Menezes-Filho NA, Andrade MV, Noronha KVMS, Rocha R, Macinko J, Hone T, Tasca R, Giovanella L, Malik AM, Werneck H, Fachini LA, Atun R. Brazil’s Unified Health System: The First 30 Years and Prospects for the Future. Lancet. 2019;394(10195):345-56. doi: 10.1016/S0140-6736(19)31243-7. , 88. Ribeiro ALP, Duncan BB, Brant LCC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular Health in Brazil: Trends and Perspectives. Circulation. 2016;133(4): 422-33. doi: https://doi.org/10.1161/CIRCULATIONAHA.114.008727 .
https://doi.org/10.1161/CIRCULATIONAHA.1...
To have representative, reliable and extensive national data on CVD, risk behaviors and factors is an obligatory step towards overcoming these inequalities and providing the best possible CV care to all Brazilians. This study gathers this information, essential to individual care and to plan the next steps of health policy in Brazil. 99. Ribeiro ALP, Oliveira GMM. Toward a Patient-Centered, Data-Driven Cardiology. Arq Bras Cardiol. 2019;112(4):371-3. doi: 10.5935/abc.20190069. In addition, it points out gaps in the knowledge to be filled with further studies. We all aspire for people to live longer and better. Knowing more about CV statistics to help tackle CVD is a good start to this goal.
Main Brazilian Data Sources
A. For the present version of the Cardiovascular Statistics - Brazil document, the main Brazilian data sources were the Brazilian Mortality and Hospital Information Systems, periodic health surveys, such as the National Health Survey, and official population estimates. Brazilian Mortality Information System: In Brazil, the SIM, created in 1975 by the Brazilian Ministry of Health, is responsible for collecting, storing, managing, and disseminating national mortality data. This health information system represented a major advance in the country’s epidemiological surveillance, since its main task is to record all deaths occurring in the Brazilian territory. The Brazilian Ministry of Health implemented a Standard Certificate of Death model, a document for collecting information on death, that uses the ICD to code the causes of death. In addition, a flow of collection, processing, and distribution of death information has been implemented in all 5570 municipalities across the country. 1010. Brasil. Ministério da Saúde. Manual de Instruções para o Preenchimento da Declaração de Óbito. Brasília: Ministério da Saúde; 2011. , 1111. Jorge MH, Laurenti R, Gotlieb SL. Análise da Qualidade das Estatísticas Vitais Brasileiras: A Experiência de Implantação do SIM e do SINASC. Cien Saude Colet. 2007;12(3):643-54. doi: 10.1590/s1413-81232007000300014. The quality of statistics on causes of death in Brazil significantly improved in the last two decades, but data from the beginning of the 2000 decade are still of low quality, specifically in some parts of the country. 1212. França E, Abreu DX, Rao C, Lopez AD. Evaluation of Cause-of-Death Statistics for Brazil, 2002-2004. Int J Epidemiol. 2008;37(4):891-901. doi: 10.1093/ije/dyn121. Knowing the heterogeneity of these indicators in Brazil, the Brazilian Cardiovascular Statistics report treated data to estimate information closer to real, by correcting for underreporting and redistribution of ill-defined causes of death. More details can be found in the article by Malta et al . 66. Malta DC, Teixeira R, Oliveira GMM, Ribeiro ALP. Cardiovascular Disease Mortality According to the Brazilian Information System on Mortality and the Global Burden of Disease Study Estimates in Brazil, 2000-2017. Arq Bras Cardiol. 2020;115(2):152-160. doi: 10.36660/abc.20190867.
https://doi.org/10.36660/abc.20190867...
B. Brazilian Hospital Information System: The aim of the SIH database is to register all hospitalizations funded by the SUS. The SIH-SUS compiles the hospitalizations at the municipal level through the “Hospital Admission Authorization”, which has information about the diseases leading to hospitalization (using ICD-10), length of stay, procedures, and costs. 1313. Escosteguy CC, Portela MC, Medronho RA, Vasconcellos MT. O Sistema de Informações Hospitalares e a Assistência ao Infarto Agudo do Miocárdio. Rev Saude Publica. 2002;36(4):491-9. doi: 10.1590/s0034-89102002000400016. The SIH-SUS information allows the development of methodologies and the definition of indicators to identify geographical disparities related to hospital resources. 1414. Rocha TAH, Silva NCD, Amaral PVM, Barbosa ACQ, Vissoci JRN, Thomaz EBAF, Queiroz RCS, Harris M, Facchini LA. Geolocation of Hospitalizations Registered on the Brazilian National Health System’s Hospital Information System: A Solution Based on the R Statistical Software. Epidemiol Serv Saude. 2018;27(4):e2017444. doi: 10.5123/S1679-49742018000400016.
C. National Health Survey: When the statistics for CV risk factors are cited, a preference for the PNS survey was made. The PNS is a household-based epidemiological survey, representative of Brazil, its large regions, FUs, metropolitan regions, capitals, and other municipalities in each FU. The PNS 2013 sample was composed of 64 348 households. The survey was carried out by the IBGE in partnership with the Ministry of Health. Most health topics were included, such as noncommunicable diseases, risk factors, elderly, women, children, use of health services, health inequalities, anthropometric features, laboratory tests, and blood pressure measurements. 1515. Malta DC, Stopa SR, Szwarcwald CL, Gomes NL, Silva JB Jr, Reis AA. Surveillance and Monitoring of Major Chronic Diseases in Brazil - National Health Survey, 2013. Rev Bras Epidemiol. 2015;18(Suppl 2):3-16. doi: 10.1590/1980-5497201500060002. The PNS data are used by the GBD in its estimates for Brazil.
D. For population estimates, the most updated population estimates generated by the IBGE (www.ibge.gov.br) were used in the denominator. For the hospitalizations and cost analyses, the resident population estimated for the National Audit Office yearly, from 2008 to 2019, was used.
GBD 2019
The GBD Study ( http://www.healthdata.org/gbd ) is the most comprehensive worldwide observational epidemiological study to date. It describes mortality and morbidity from major diseases, injuries, and risk factors to health at global, national, and regional levels. Examining trends from 1990 to the present and making comparisons across populations enable us to understand the changing health challenges faced by people across the world in the 21st century. The GBD 2019 is the latest publicly available dataset. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1616. GBD 2019 Viewpoint Collaborators. Five Insights From the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1135-59. doi: 10.1016/S0140-6736(20)31404-5.
https://doi.org/10.1016/S0140-6736(20)31...
The GBD Brazil network has been collaborating with the IHME, which leads the project in the world, in the identification and provision of datasets, revision of models and estimates, and validation and publication of the results for Brazil. 2020. França EB, Passos VMA, Malta DC, Duncan BB, Ribeiro ALP, Guimarães MDC, Abreu DMX, Vasconcelos AMN, Carneiro M, Teixeira R, Camargos P, Melo APS, Queiroz BL, Schmidt MI, Ishitani L, Ladeira RM, Morais-Neto OL, Bustamante-Teixeira MT, Guerra MR, Bensenor I, Lotufo P, Mooney M, Naghavi M. Cause-Specific Mortality for 249 Causes in Brazil and States During 1990-2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Popul Health Metr. 2017;15(1):39. doi: 10.1186/s12963-017-0156-y. , 2121. GBD 2016 Brazil Collaborators. Burden of Disease in Brazil, 1990-2016: A Systematic Subnational Analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10149):760-75. doi: 10.1016/S0140-6736(18)31221-2.
https://doi.org/10.1016/S0140-6736(18)31...
Details on how the estimates are calculated can be obtained in the capstone papers of the GBD Study and in the IHME website ( http://www.healthdata.org/acting-data/what-we-measure-and-why ). We summarize below the main estimates used in this document:
A. Estimates of deaths and causes of deaths. The main source of information is the SIM, a database from the Brazilian Ministry of Health, adjusted to other national and international sources. The IHME used methods for correcting for underreporting of deaths and “garbage codes” deaths according to previously published algorithms, 2222. Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for Enhancing Public Health Utility of National Causes-of-Death Data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. updated in the newer versions of the study ( http://www.healthdata.org/acting-data/determining-causes-death-how-we-reclassify-miscoded-deaths ).
B. The YLLs are years lost due to premature mortality. The YLLs are calculated by subtracting the age at death from the longest possible life expectancy for a person at that age. For example, if the longest life expectancy for men in a given country is 75 years, and a man dies of cancer at 65, this would be 10 years of life lost due to cancer.
C. The YLDs can also be described as years lived in less-than-ideal health. This includes conditions such as influenza, which may last for only a few days, or epilepsy, which can last a lifetime. It is measured by taking the prevalence of the condition multiplied by the disability weight for that condition. Disability weights reflect the severity of different conditions and are developed through surveys with the general population.
D. The DALY is a universal metric that allows researchers and policymakers to compare very different populations and health conditions across time. The DALYs equal the sum of YLLs and YLDs. One DALY equals one lost year of healthy life. The DALYs allow us to estimate the total number of years lost due to specific causes and risk factors at the country, regional, and global levels.
Systematic Review of the Literature
Descriptors for the elaboration of search strategies were selected in MeSH and DeCS, the controlled vocabularies from MEDLINE and LILACS, respectively. Embase’s plan was designed with Emtree descriptors associated with MeSH. Free terms were also used, that is, significant keywords and their synonyms, spelling variations, and acronyms that are essential for searching in the searched domain, but which are not controlled descriptors (or are not in the synonym list of these descriptors). Importantly, to maintain search uniformity, the same descriptors were used in all search strategies. However, search strategies were customized according to the specifics of each database. In addition, it is worth noting that the terms related to “Brazil” were generally searched in all fields of research (subject, author, title, institutional affiliation, journal name, etc.).
The selected bases for research were MEDLINE/PubMed, Embase, LILACS, CINAHL, Cochrane Library Scopus, and Web of Science. The following bibliographic research filters and limits were used: period of publication (2004-2020); languages (Portuguese, English and Spanish); type of study/publication (Review, Meta-Analysis, Clinical Trial, Randomized Controlled Trial, Comparative Study, Practice Guideline, Guideline, Systematic Review, Evaluation Studies, Government Publications, and Multicenter Study). All references were managed using EndNote Web. From the search, articles were included if the study were population- or community-based; nation- or state-wide studies were preferred. Moreover, articles set at health services or hospitals were included if the study was multicenter and had an adequate sample size (>200 participants was the suggested cut-off), preferably. In addition to the articles identified by the systematic search, the authors could include other studies found in the references of the searched articles or other articles they were aware of in their area of expertise, if the studies fulfilled the criteria above mentioned. Finally, which studies should be described in each chapter was mostly a decision of the experts commissioned to the specific theme.
Healthcare Utilization
Healthcare costing studies have expressive methodologic variability and need to be carefully interpreted. In the present document, most of the cost data were gathered from the Public Health System reimbursement tables from 2008 to 2019. During this period, adjustment for inflation was performed neither regularly nor homogeneously across the CVD groups or procedures, thus the crude values presented were not adjusted to actual inflation.
To minimize biases in reporting and interpreting cost data, a systematic approach was applied to all chapters. Overall costing studies were described in original units (Reais or US dollars in a specific year) and international dollars. International dollars were converted to PPP adjusted to 2019 US dollars (Int$ 2019) using the Campbell and Cochrane Economics Methods Group and the Evidence for Policy and Practice Information and Coordinating Centre cost converter (https://eppi.ioe.ac.uk/costconversion/default.aspx). A two-stage approach is applied in this method. First, it adjusts the original estimate of cost from the original price-year to a target price-year, using a GDP deflator index (GDPD values). Second, it converts the price-year adjusted cost estimate in the original currency to a target currency, using conversion rates based on PPP for GDP (PPP values). 55. Shemilt I, Thomas J, Morciano M. A Web-Based Tool for Adjusting Costs to a Specific Target Currency and Price Year. Evid. Policy. 2010;6(1):51-9. doi:10.1332/174426410X482999. For original economic studies, when the base year of the currency was not reported or could not be inferred from the manuscript (e.g. the last year of data collection), the recommendation was to assume the year before the publication of the paper.
Highlights
Total Cardiovascular Disease
• According to both the GDB Study 2019 and the SUS database, CVDs are the number 1 cause of death in Brazil. Of the CVDs, IHD was the leading cause of death in the country, followed by stroke in 1990 and 2019.
• According to the GBD Study 2019, CVD prevalence was estimated in 6.1% of the population and has increased from 1990 due to population growth and aging. However, the age-standardized CVD prevalence and incidence rate in Brazil decreased in the same period.
• A reduction in age-adjusted mortality rate from 1990 to 2019 was observed in all FUs, although less impressive in the North and Northeastern as compared to the other regions.
• Age-standardized DALY rates in Brazil decreased from 1990 to 2019, and there was a correlation between the percent decline in DALY rates and the increase in the SDI: the higher the SDI, the greater the decline in DALYs due to CVD.
• Data from the SUS database showed a significant number of clinical and surgical CV procedures paid, led by heart failure, cerebrovascular diseases, and acute coronary syndrome. Hospitalizations for PCI significantly increased in the last decades, while surgical procedures remained stable.
Stroke
• According to a community-based study performed in the city of Matão in 2003-2004 and 2015-2016, the age-adjusted stroke incidence decreased by 39% (IRR 0.61; 95% CI, 0.46–0.79) and mortality by 50% (IRR 0.50; 95% CI, 0.31– 0.94). The mean age of stroke patients increased by 9%, from 65.2 (95% CI, 62.6–67.8) to 71.0 (95% CI, 68.1–73.8) years. The 1-year case fatality was 26%; approximately 56% of the patients were functionally independent, while 7% had a recurrent stroke.
• Regarding the distribution of stroke subtypes, according to the Joinvasc Registry performed in the city of Joinville, from 1995 to 2013, the proportion of IS increased 12%, whereas that of HS decreased 16%. Meanwhile, the proportion of SAH remained relatively stable, ranging from 7.5% in 1995 to 6% in 2012–2013. In the last 8 years, the incidences of IS and HS showed significant decreases of 15% (95% CI, 1–28) and 60% (95% CI, 13–86), respectively.
• According to data from the GBD Study 2019, the age-standardized mortality rate from stroke per 100 000 in 1990 was 137.8 (127.8 to 144) and, in 2019, 58.1 (52.6 to 61.8), representing a percent change of -57.8 (-60.4 to -0.6). The highest percent change occurred in Goiás, -65.9 (-71.8 to -0.6), and the lowest in Maranhão, -22.7 (-37.2 to 0). For adults, the highest percent change was observed among people aged 50-69 years, -61 (-603.6 to -0.6).
• Considering the burden of stroke in Brazil, the GBD Study 2019 also observed a prominent decrease in YLL: the age-standardized YLL rates due to stroke per 100 000 in 1990 was 2778.6 (2659.5 to 2879.2) and, in 2019, 1098.7 (1025.8 to 1153.7), representing a percent change of -60.5 (-62.7 to -0.6). For adults, the highest percent change was observed among people aged 50-59 years, -61.7 (-64.3 to -0.6).
Acute and Chronic Coronary Artery Disease
• According to the GBD Study 2019, the number of individuals with IHD (AMI, stable angina, or ischemic heart failure) in Brazil increased from 1.48 million in 1990 to more than 4 million in 2019, and the crude IHD prevalence rate increased from 0.99% to 1.85% in the period, although age-standardized prevalence rates remained stable.
• In 2019, there were 171 246 deaths due to IHD in Brazil, corresponding to 12% of total deaths in the country and 43% of all CVD deaths. IHD was the number one cause of death in Brazil in all but two FUs. A reduction in age-adjusted mortality rate from 1990 to 2019 was observed in all FUs, although less impressive in the Northeastern as compared to the other regions.
• According to the SUS database, the number of hospitalizations due to AMI in the public system increased by 54% from 2008 to 2019, adjusted for the population. Non-primary PCIs per inhabitants doubled, while primary PCIs increased by 31%. Meanwhile, the total number of CABGs remained stable in the period. The in-hospital mortality rate for AMI decreased from 15.9% in 2008 to 12.9% in 2019; for acute coronary syndrome, rates were stable during that period, as well as for PCI and CABG procedures.
Cardiomyopathy and Heart Failure
• According to GBD Study 2019 estimates, the age-standardized prevalence of cardiomyopathy and myocarditis decreased in Brazil from 76.6 (95% UI, 53.4-107.2) in 1990 to 73.0 (95% UI, 51.1-100.1) in 2019, a decrease of 4.7% (95% UI, - 9.5 to 0.8) in the period. In absolute numbers, estimates of the prevalence of cardiomyopathy and myocarditis in Brazil increased from less than 60 000 in 1990 to over 160 000 in 2019, mainly due to population growth and aging. The cardiomyopathy and myocarditis prevalence was greater in men (98.9; 95% UI, 69.5-137.2) than in women (54.1; 95% UI, 38.4-73.8) in 2019.
• In the NIH REDS-II Chagas retrospective cohort study, initially healthy blood donors with an index T. cruzi -seropositive donation and age, sex, and period-matched seronegative donors were followed up for 20 years. The differential incidence of cardiomyopathy was 1.85 per 100 person-years attributable to T. cruzi infection in the first 10 years of follow-up, and 0.9 per 100 person-years in the following 10 years. A T. cruzi antibody level in the second visit was associated with the development of cardiomyopathy (adjusted OR, 1.4; 95% CI 1.1-1.8) in the last visit.
• According to the GBD Study 2019, the number of deaths due to Chagas disease in Brazil decreased from 7903 (95% UI, 2438-10 073) in 1990 to 6523 (95% UI, 3350-11 226) in 2019. The age-standardized mortality rate showed a more striking decrease (-67.5% change), from 8.6 (95% UI, 2.8-10.9) deaths per 100 000 inhabitants in 1990 to 2.8 (95% UI, 1.8-4.8) per 100 000 inhabitants in 2019, accounting for 1.6% of all CV deaths in the country.
• According to data from the SUS, there were 3 085 359 hospitalizations due to heart failure from 2008 to 2019. This number represents one-third of total clinical admissions related to CV conditions in the period studied, when there was a reduction in the number of clinical admissions due to heart failure from 298 474 (157 per 100 000) in 2008 to 222 620 (105 per 100 000) in 2019, with an even reduction over the years. Despite that reduction in the number of admissions, unadjusted healthcare expenditure estimates from the direct payment for the care of heart failure patients increased from 2008 to 2019 by almost 32%, from R$ 272 280 662 (2019 Int$ 267 102 469) in 2008 to R$ 359 301 691 (2019 Int$ 173 659 589) in 2019. Heart failure accounted for most costs related to clinical admissions due to CVD.
Valvular Heart Disease
• According to the GBD Study 2019, the pattern of valvular heart disease has been changing in Brazil: age-standardized prevalence was stable from 1990 to 2019 for RHD, but a marked increase of over 50% was observed for NRVD, especially for men and older age groups. Among specific valve diseases, there was a marked 201.8% increase of calcific aortic valve disease, reinforcing the impact of population aging.
• RHD showed a marked decrease in age standardized mortality (-59.4%) from 1990 to 2019, while a milder decrease was observed for NRVD, 16.2% (95% UI, 10.3-22.5). However, crude mortality rates increased significantly for older ages (>70 years), associated with degenerative aortic valve disease, suggesting a growing burden to the health systems and urging specific actions to minimize impacts.
• The burden attributable to valvular heart disease in Brazil remains socioeconomically driven, with significant negative correlations between changes in the age-standardized mortality rates associated with RHD and the SDI in 1990 and 2019, in addition to positive correlations between NRVD mortality rates and the SDI in both years.
• Expenses with valvular heart disease by the Brazilian public health system decreased proportionally from 2008 to 2019 (-6.3% and -28% for clinical and interventional admissions, respectively), due to inflation and monetary correction. This constraint urges discussions towards a budgetary revision, avoiding the deferral or restriction of interventional and surgical procedures and allowing for the incorporation of new technologies and devices.
• Despite the improvement in the past decades, RHD remains as an important cause of morbidity and mortality in Brazil: data from the SUS database show that besides being the etiology of nearly half of the valve surgeries in the public health system – associated with higher hospital mortality – the prevalence of subclinical disease among schoolchildren proved to be high (4.5%), with the implementation of large-scale screening programs in 2014. Thus, coordinated actions for early diagnosis and prophylaxis are needed to avoid disease progression and late sequelae.
Atrial Fibrillation
• According to the GBD Study 2019, the age-standardized prevalence rates due to AF and atrial flutter increased slightly in Brazil from 519 (95% UI, 393-669) in 1990 to 537 (95% UI, 409-692) in 2019, per 100 000 inhabitants, for both sexes, with 3.5% (95% UI, 1.8-5.1) change in the period.
• In a 10-year follow-up of 1462 individuals aged ≥ 60 years (mean age, 69 years; 61% women) included in the Bambuí Cohort Study in 1997, AF or flutter was independently associated with an increase in all-cause mortality (HR, 2.35; 95% CI, 1.53-3.62) among patients with and without Chagas disease.
• Data from the Telehealth Network of Minas Gerais with ECGs of 1 558 421 individuals (mean age, 51±18 years; 40.2% men) performed between 2010 and 2017 revealed in multivariable models adjusted for age and sex that the following self-reported comorbidities and risk factors related to the presence of AF: Chagas disease (OR 3.08; 95% CI, 2.91-3.25), previous myocardial infarction (OR 1.74; 95% CI, 1.56-1.93), chronic obstructive pulmonary disease (OR 1.48; 95% CI, 1.33-1.66), hypertension (OR 1.31; 95% CI, 1.27-1.34), and dyslipidemia (OR 1.09; 95% CI, 1.03-1.16). Current smoking and diabetes were not associated with prevalent AF.
• Of all 429 cases of stroke (87.2% ischemic strokes) that occurred in the city of Joinville in 2015 and were included in a registry, AF was detected in 11.4% of all patients and in 58% of the cardioembolic strokes. Similarly, AF was detected in 58% of 359 patients with cardioembolic stroke from a single-center, consecutive sample in the city of Curitiba, Brazil.
Hypertension
• Analysis of the 2013 PNS showed a 22.8% prevalence of measured hypertension in individuals older than 18 years in a sample of 59 402 individuals. In those older than 75 years, the estimated prevalence was 47.1%. In the age groups between 18 and 74 years, the prevalence was higher in men, while women showed a slight predominance only in the age group above 75 years. The analysis by region showed that the Southeastern (25%) and Southern (25%) regions had the highest prevalence for both sexes.
• Using data from the 2013 PNS, 36% of the Brazilians included had a previous diagnosis and/or measured blood pressure ≥140/90 mm Hg. Of these, 89% had contacted the health system in the previous 2 years, but only 65% were aware of their condition. From those aware of their hypertensive condition, 62% regularly sought care, 92% of whom had been prescribed medications. Of those who reported receiving medications, only 56% reported that ongoing care for their condition was free of barriers and included advice about managing important risk factors and behavior. Of the entire hypertensive population, about 33% had their blood pressure under control.
• According to data from participants in the Brazilian Study of Cardiovascular Risks in Adolescents (ERICA), of 73 399 students evaluated, 55.4% were female and the mean age was 14.7 ± 1.6 years. The prevalence of hypertension was 9.6%, with the lowest in the Northern (8.4%) and Northeastern regions (8.4%), and the highest, in the Southern region (12.5%). Obese adolescents had a higher prevalence of hypertension (28.4%) than overweight (15.4%) or eutrophic adolescents (6.3%). The proportion of hypertension due to obesity was estimated in 17.8%.
• In the ELSA-Brasil cohort study, which included 7063 patients with a mean age of 58.9 years at baseline (2008-2010), hypertension was associated with the greatest decline in memory, fluency, and global cognitive score. Prehypertension was also an independent predictor of greater decline in the verbal fluency test and global cognitive score. Moreover, among treated individuals, blood pressure control at baseline was inversely associated with the decline in both global cognitive and memory test scores.
Diabetes mellitus
• Considering the International Diabetes Federation data published in 2019, Brazil ranked 5th regarding the number of adults with diabetes worldwide, totaling 16.8 million (95% CI, 15.0 – 18.7) people, 46% of whom were not aware of their disease. The prevalence of prediabetes was 9.5% (15.1 million people).
• According to GBD 2019, mortality from CVD attributable to diabetes for all ages in Brazil increased in absolute numbers from 50 812 deaths (95% UI, 35 649 -73 137) in 1990 to 80 754 (95% UI, 55 922 – 118 175) in 2019. However, the age-standardized mortality rates per 100 000 inhabitants decreased from 70.4 (95% UI, 47.4 – 106.1) in 1990 to 35.9 (95% UI, 24.5 – 53.0) in 2019, a reduction of -49.0% (95% UI, -53.4 to -43.9).
• Regarding the burden of CVD attributable to diabetes, the age-standardized DALY rates decreased by -47.4% (95% UI, -52.2 to -41.9) per 100 000 inhabitants from 1990 to 2019, despite the increase in the total number of DALYs from 1 072 309 (95% UI: 784 276 - 1 484 959) to 1 571 116 (95% UI: 1 140 912 – 2 203 188) in the same period. There was a heterogeneous reduction in the age-standardized DALY rates attributable to diabetes among the Brazilian FUs and regions.
Dyslipidemia
• According to the PNS 2014-2015, the prevalence of dyslipidemia in Brazil is still high: total cholesterol ≥ 200 mg/dL in 32.7% (95% CI, 31.5 - 34.1) of the general population; low HDLc in 31.8% (95% CI, 30.5 – 33.1), and high LDLc in 18.6% (95% CI, 17.5 – 19.7). Greater level of education was related to lower prevalence of high total cholesterol, high LDLc, and low HDLc.
• According to the GBD Study 2019, when analyzing trends from 1990 to 2019, an increase was observed in the absolute numbers of deaths, YLLs, and DALYs, with a decrease in the age-standardized rates for those same metrics in all states and at national level.
• A Brazilian cohort (ELSA-Brasil study) assessed familial hypercholesterolemia and showed a prevalence of 1 in 263 individuals, but data on burden of disease and impact on cost are still lacking.
• Awareness of dyslipidemia according to the ELSA-Brasil is also low (58.1% of individuals with elevated LDLc), with only 42.3% of those individuals receiving medical treatment. Only 58.3% of the individuals on some kind of lipid-lowering medication achieved target serum lipid level.
Obesity and Overweight
• According to data from IBGE, in Brazil, the percentages of adults (age ≥18 years) with excess weight and obesity in 2019 were, respectively, 57.5% (95% CI, 54.8 – 60.2) and 21.8 % (95% CI, 19.2 – 24.7) for men, and 62.6% (95% CI, 59.1 – 66.0) and 29.5% (95% CI, 25.4 – 34.0) for women. Progressive increase of obesity was observed with age increase, ranging from 10.7% (95% CI, 7.7 – 14.7) [male: 7.9% (95% CI, 4.8 – 12.8); female: 13.5% (95% CI, 8.8 – 20.4)] in the age group of 18-24 years to 34.4% (95% CI, 29.7 – 39.4) [male: 30.2% (95% CI, 24.8 – 36.3); female: 38.0% (95% CI, 32.3 - 44.0)] in the age group of 40-59 years. It is worth noting the higher prevalence of excess weight and obesity in the female sex for all age groups.
• From 1990 to 2019, there was a negative change in the mortality rates from CVD attributable to high body mass index for women [-33.9 (-43.7; -16.7)], which was higher than that for men [-22.8 (-35.9;6.2)]. The highest decreases in the percentage of mortality occurred in the FUs with higher income in Brazil.
• Most FUs had a decrease in the age-standardized rates of DALYs due to CVD attributed to high body mass index for women in the period. Similar behavior was observed in those rates for men, with a percent decrease of obesity from 1990 to 2019.
• Most public policies have failed to reduce obesity in adults and children, probably because obesity is multifactorial and involves many socioeconomic interests. Obesity is a pandemic, with impact on both developed and developing countries and consequences for the individual, social, familial, and financial levels. Nationwide registries of measured obesity should be built to enable the development of more effective public policies to control obesity, which has been increasing in Brazil in both sexes and several age groups.
Smoking and Tobacco Use
• PNS 2019 data indicate that 12.8% (95% CI, 12.4 - 13.2%) of adults use some tobacco product, being the use higher among males (16.2%; 95% CI, 15.6 - 16.9%) than among females (9.9%; 95% CI, 9.3 - 10.3%). Considering the Vigitel household survey, there was a significant decrease in the prevalence of smoking in the adult population, with a 37.6% reduction from 2006 to 2019. However, there was a 0.5% increase in the prevalence from 2018 to 2019, suggesting a change in the trend and calling for attention.
• According to the GBD Study 2019, there was a reduction of 58.8% (95% UI, 56.2 - 61.1) in the smoking-attributable total mortality rate in Brazil from 1990 to 2019. The same trend was observed for both men and women, and in all Brazilian FUs. Likewise, the smoking-attributable CV mortality reduced by near 70% in the same period.
• The tobacco CV burden of disease decreased from 1990 to 2019, with a 69% (95% UI, 56 - 61) reduction in the age-standardized DALY rate. There was a heterogeneous reduction in the age-standardized DALY rates attributed to tobacco in the different FUs and regions of Brazil, more pronounced in the Southeastern, Southern and West-Central FUs, with a modest reduction in the Northern FUs and an even more discreet reduction in most Northeastern FUs.
• In a study using Markov probabilistic microsimulation economic model, the total direct cost of tobacco was estimated at US$ 11.8 billion per year, 70% corresponding to the direct cost associated with health care and the remainder associated with the indirect cost due to loss of productivity due to premature death and inability. Tobacco represented 22% of the direct costs of CVD in Brazil and 17% of the direct costs of stroke.
1. TOTAL CARDIOVASCULAR DISEASES
ICD-9 390 to 459; ICD-10 I00 to I99.
See Table 1-1 through 1-13 and Charts 1-1 through 1-16
Abbreviations Used in Chapter 1
| AHA | American Heart Association |
| AMI | Acute Myocardial Infarction |
| CABG | Coronary artery bypass grafting |
| CI | Confidence Interval |
| CVD | Total Cardiovascular Diseases |
| DALYs | Disability-Adjusted Life Years |
| DATASUS | Brazilian Unified Health System Database |
| ELSA-Brasil | The Brazilian Longitudinal Study of Adult Health (in Portuguese , Estudo Longitudinal de Saúde do Adulto ) |
| FHP | Family Health Program |
| FU | Federative Units |
| GBD | Global Burden of Disease |
| GDP | Gross Domestic Product |
| HDI | Human Development Index |
| HDIm | Municipal Human Development Index |
| HF | Heart Failure |
| IBGE | Brazilian Institute of Geography and Statistics |
| ICD | International Statistical Classification of Diseases and Related Health Problems |
| IHD | Ischemic Heart Disease |
| NCD | Noncommunicable Chronic Diseases |
| NHS | National Health System |
| OR | Odds Ratio |
| PAR | Population Attributable Risks |
| RR | Relative Risk |
| SDI | Sociodemographic Index |
| SIDRA | IBGE Automated Retrieval System (in Portuguese, Sistema IBGE de Recuperação Automática) |
| SIM | Brazilian Mortality Information System (in Portuguese, Sistema de Informações sobre Mortalidade ) |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| UI | Uncertainty Interval |
– Number of prevalent cases and age-standardized prevalence rates of cardiovascular diseases, per 100 000 inhabitants, and percent change of rates, according to age group and sex, in Brazil, in 1990 and 2019.
– Number of incident cases, age-standardized incidence rates of cardiovascular diseases (per 100 000 inhabitants), and percent change of rates in Brazil and its Federative Units, in 1990 and 2019.
– Number of deaths, age-standardized mortality rates due to cardiovascular diseases (per 100 000 inhabitants), and percent change of rates in Brazil and its Federative Units, in 1990 and 2019.
– Proportional mortality from cardiovascular diseases (CVD), ischemic heart diseases (IHD) and stroke by Brazilian Region and Federative Unit, and in Brazil, in 2019.
– Number of DALYs, age-standardized DALY rates due to cardiovascular diseases (per 100 000 inhabitants), and percent change of rates in Brazil and its Federative Units, in 1990 and 2019.
– Number of YLLs, age-standardized YLL rates due to cardiovascular diseases (per 100 000 inhabitants), and percent change of rates, according to age group, in Brazil, in 1990 and 2019.
– Number of YLDs, age-standardized YLD rates due to cardiovascular diseases (per 100 000 inhabitants), and percent change of rates, according to age group, in Brazil, in 1990 and 2019.
– Total number of hospitalizations for clinical procedures for cardiovascular diseases by competence year, Brazil, 2008 to 2019.
– Total number of hospitalizations for surgical procedures for cardiovascular diseases by competence year, Brazil, 2008 to 2019.
– Total value (in Reais) of clinical procedures for cardiovascular diseases by competence year, Brazil, 2008 to 2019.
– Total value (in Int$2019) of clinical procedures for cardiovascular diseases by competence year, Brazil, 2008 to 2019.
– Total value (in Reais) of surgical procedures for cardiovascular diseases by competence year, Brazil, 2008 to 2019.
– Total value (in Int$2019) of surgical procedures for cardiovascular diseases by competence year, Brazil, 2008 to 2019.
– Ranking of causes of death in Brazil, 1990 and 2019, according to age-standardized mortality rates per 100 000 inhabitants, both sexes, 1990 and 2019, and percent change of rates.
– Ranking of causes of cardiovascular death in Brazil, 1990 and 2019, according to age-standardized mortality rate per 100 000 inhabitants, both sexes, 1990 and 2019, and percent change of rates.
– Ranking of causes of cardiovascular death per Brazilian Federative Unit in 1990, according to age-standardized mortality rates per 100 000 inhabitants, both sexes.
– Ranking of causes of cardiovascular death per Brazilian Federative Unit in 2019, according to age-standardized mortality rates per 100 000 inhabitants, both sexes.
– Age-standardized prevalence rate of cardiovascular disease, per 100 000 inhabitants, by sex, Brazil, 1990-2019.
– Age-standardized mortality rate from cardiovascular disease, per 100 000 inhabitants, by sex, Brazil, 1990-2019.
– Geographic distribution of mortality rates per 100 000 inhabitants, standardized by age in the Federative Units of Brazil, according to sex, 2000 and 2019.
– Age-standardized mortality rates from cardiovascular disease, per 100 000 inhabitants, by Brazilian region, for females, 1990-2019.
– Age-standardized mortality rate from cardiovascular disease, per 100 000 inhabitants, by Brazilian regions, for males, 1990-2019.
– Correlation between percent change of age-standardized mortality rates 2019/1990 and the 2019 sociodemographic index (SDI 2019).
– Age-standardized rates of DALYs due to cardiovascular diseases, per 100 000 inhabitants, 1990-2019, Brazil and its regions.
– Correlation between percent change of age-standardized DALY rates 2019/1990 and the 2019 sociodemographic index (SDI 2019).
– Total number of hospitalizations for clinical procedures due to cardiovascular diseases, by competence year, Brazil, 2008 to 2019.
– Total number of hospitalizations for surgical procedures due to cardiovascular diseases, by competence year, Brazil, 2008 to 2019.
Overview
• Noncommunicable chronic diseases comprise the world’s leading group of causes of death, responsible for premature deaths, loss of quality of life, and adverse economic and social impacts. The NCD are responsible for approximately 70% of global deaths, equivalent to more than 38 million deaths annually, significantly exceeding deaths from external causes and infectious diseases. 2323. World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013-2020. Geneva: WHO Library Cataloguing-In-Publication Data; 2013. Of all deaths due to NCD worldwide, nearly 45%, over 17 million, result from CVD. A similar distribution is observed in Brazil, where 72% of deaths are due to NCD, of which 30% are due to CVD, and 16% to neoplasms (Chart 1-1). 2121. GBD 2016 Brazil Collaborators. Burden of Disease in Brazil, 1990-2016: A Systematic Subnational Analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10149):760-75. doi: 10.1016/S0140-6736(18)31221-2.
https://doi.org/10.1016/S0140-6736(18)31...
, 2727. Nascimento BR, Brant LCC, Oliveira GMM, Malachias MVB, Reis GMA, Teixeira RA, Malta DC, França E, Souza MFM, Roth GA, Ribeiro ALP. Cardiovascular Disease Epidemiology in Portuguese-Speaking Countries: data From the Global Burden of Disease, 1990 to 2016. Arq Bras Cardiol. 2018;110(6):500-11. doi: 10.5935/abc.20180098. , 2828. Malta DC, Bernal RT, Souza MF, Szwarcwald CL, Lima MG, Barros MB. Social Inequalities in the Prevalence of Self-Reported Chronic Non-Communicable Diseases in Brazil: National Health Survey 2013. Int J Equity Health. 2016;15(1):153. doi: 10.1186/s12939-016-0427-4.
• The definition of CVD may vary according to the study, from including all diseases listed in ICD-10 Chapter IX to just grouping together the 3 main causes (IHD, stroke, and HF). For the GBD, the definition of total CVD comprises 10 causes: rheumatic heart disease, IHD, cerebrovascular disease, hypertensive heart disease, cardiomyopathy, myocarditis, atrial fibrillation and flutter, aortic aneurysm, peripheral vascular disease, and endocarditis. 2929. Brant LCC, Nascimento BR, Passos VMA, Duncan BB, Bensenõr IJM, Malta DC, Souza MFM, Ishitani LH, França E, Oliveira MS, Mooney M, Naghavi M, Roth G, Ribeiro ALP. Variations and Particularities in Cardiovascular Disease Mortality in Brazil and Brazilian States in 1990 and 2015: Estimates From the Global Burden of Disease. Rev Bras Epidemiol. 2017;20(Suppl 01):116-28. doi: 10.1590/1980-5497201700050010.
• Cardiovascular diseases are the number 1 cause of death in Brazil. According to the GBD Study 2019 estimates, of the CVD, IHD was the leading cause of death in the country, followed by stroke in both 1990 and 2019 (Chart 1-2). In fact, in 2019, IHD was the leading cause of death in all Brazilian FUs, except for the state of Amazonas, in the Northern region. Three states in that region, Acre, Amapá, and Pará, showed no significant difference regarding the mortality rates due to IHD and stroke (Charts 1-3 and 1-4).
Prevalence
• Gonçalves et al. published in 2019 a cross-sectional study from the Brazilian National Health Survey conducted in 2013 on a sample of 60 202 adults aged over 18 years, stratified by sex and age groups, using a hierarchical binary logistic regression model. The self-reported diagnosis of heart disease in Brazil was 4.2% (95% CI, 4.0 - 4.3) and associated with the female sex (OR = 1.1; 95% CI, 1.1 - 1.1), individuals 65 years and older (OR = 4.7; 95% CI, 3.3 – 5), hypertension (OR = 2.4; 95% CI, 2.2 – 2.7), elevated cholesterol (OR = 1.6; 95% CI, 1.5 – 1.8), overweight (OR = 1.5; 95% CI, 1.4 – 1.8) or obesity (OR = 2.0; 95% CI, 1.7 – 2.2), sedentary behavior (OR = 1.5; 95% CI, 1.02 – 2.1), and tobacco use (OR = 1.2; 95% CI, 1.03 – 1.3). 3030. Gonçalves RPF, Haikal DS, Freitas MIF, Machado ÍE, Malta DC. Self-Reported Medical Diagnosis of Heart Disease and Associated Risk Factors: National Health Survey. Rev Bras Epidemiol. 2019;22(Suppl 2):E190016.SUPL.2. doi:10.1590/1980-549720190016.supl.2.
• In the ELSA-Brasil, a cohort study that included 15 105 civil servants from 6 academic institutions (54% women, 35-74 years, with baseline assessment between 2008 and 2010), the self-reported prevalence was as follows: coronary heart disease, 4.7% (men=5.7%, women=4.0%); HF, 1.5% (men=1.9%, women=1.5%); stroke, 1.3% for both sexes; rheumatic fever, 2.9% (men=2.2%, women=3.4%); and Chagas disease, 0.4%, for both sexes. 3131. Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM, Aquino EM, Passos VM, Matos SM, Molina Mdel C, Carvalho MS, Bensenor IM. Cohort Profile: Longitudinal Study of Adult Health (ELSA-Brasil). Int J Epidemiol. 2015;44(1):68-75. doi: 10.1093/ije/dyu027.
• The prevalence of CVD increases significantly with age. In a longitudinal study in the elderly over 60 years of age, from the state of São Paulo in 2000, 2006 and 2010, the prevalence of CVD was defined as a positive response to the question: “Have you ever been told by a doctor or nurse you had a heart attack, coronary heart disease, angina, congestive disease, or other heart problems?”. The CVD prevalence was 17.9%, 22.2% and 22.9% for 2000, 2006, and 2010, respectively. The presence of CVD was associated with older age, smoking history, diabetes, and hypertension. 3232. Massa KHC, Duarte YAO, Chiavegatto Filho ADP. Análise da Prevalência de Doenças Cardiovasculares e Fatores Associados em Idosos, 2000-2010. Cien Saude Colet. 2019;24(1):105-14. doi: 10.1590/1413-81232018241.02072017.
• According to the GBD Study 2019, the CVD prevalence was 6.1% of the population in 2019 and has increased from 1990 due to population growth and aging. However, the age-standardized CVD prevalence rate in Brazil decreased in the same period, from 6138 (95% UI, 5762 - 6519) to 5454 (95% UI, 5082 - 5838) per 100 000 inhabitants (Table 1-1).
• As compared to females, in 2019 males had a higher age-standardized prevalence rate (Charts 1-5 and 1-6) and, from 1990 to 2019, a prevalence rate decline of -8,7 (-10.2 to -7.2), lower than that of females (-12.8, 95% UI, -14.1 to -11.3) in the same period (Chart 1-6 and Table 1-1). Considering the total number in 2019, 12 946 932 (95% UI, 11 899 752 – 13 617 524) individuals had prevalent CVD in Brazil, and 51% of them were men. The prevalence rate declined among the elderly and increased among males and females aged 15-49 years (Table 1-1).
Incidence
• According to the GBD Study 2019, the age-standardized incidence rate of CVD in Brazil, in 2019, was 475 (95% UI, 447-507) per 100 000 inhabitants. From 1990 to 2019, that rate decreased -20% (-22 to -18) (Table 1-2).
• The age-standardized CVD incidence rate did not differ significantly among the FUs in 2019, varying from 441 in the state of Piauí to 486 in the state of Pernambuco. From 1990 to 2019, all FUs had a reduction in the age-standardized CVD incidence rate, and the state of Rio de Janeiro showed the highest percent change among them (-25.5%; 95% UI, -27.7 to -23.5) (Table 1-2).
Mortality
• In Brazil, Mansur et al . have shown that the age-standardized CVD mortality rate has declined significantly in recent decades. A 2016 study analyzed CVD mortality rates from the age of 30 years and older, by sex, per 100 000 inhabitants. The annual variations in cardiovascular mortality for the periods 1980-2006 and 2007-2012 were, respectively: for both sexes: -1.5% and -0.8%; men: -1.4% and -0.6%; women: -1.7% and -1.0%. 3333. Mansur AP, Favarato D. Mortality Due to Cardiovascular Diseases in Women and Men in the Five Brazilian Regions, 1980-2012. Arq Bras Cardiol. 2016;107(2):137-46. doi: 10.5935/abc.20160102.
• Baptista et al . investigated how age composition and age-specific mortality rates are related to the observed difference in deaths from CVD in the adult population, by sex, in Brazilian microregions from 1996 to 2015. They suggested, after correcting for underreporting of death counts, that there was a decline in the rates of deaths from CVD in the period studied. However, the main driver of the change in mortality rates was heterogeneous across Brazilian microregions. In general, in the most socioeconomically developed areas, the age structure was more importantly related to the mortality rates, with older populations dying from CVD. Interestingly, there were differences in the main drivers of CVD mortality even within the Brazilian regions and FUs. 3434. Baptista E, Queiroz B, Rigotti J. Decomposition of Mortality Rates From Cardiovascular Disease in the Adult Population: A Study for Brazilian Micro-Regions Between 1996 and 2015. Rev. Bras. Estud. Popul. 2018;35(2):e00050. doi: 10.20947/S102-3098a0050.
• Data from the GBD Study 2019 reveal that, although mortality rates from CVD in Brazil significantly decreased over the past few years, the total number of deaths due to CVD increased, as a result of population growth and aging. There were 269 722.7 (95% UI, 257 743.7 - 277 272.1) and 397 993 (95% UI, 361 776.4 – 417 773.2) deaths from CVD in the country in 1990 and 2019, respectively. The age-standardized mortality rate, per 100 000 inhabitants, was 355.4 (332.5 - 367.6) in 1990 and 175.7 (159 - 184.8) in 2019, decreasing by -50.6% (-52.7 to -0.5) in the period (Chart 1-7). Although the age-standardized mortality rates were higher for men throughout the whole period, the percent decrease was similar for both sexes, 48% for men and 52% for women (Chart 1-8).
• Table 1-3 shows the number of deaths, the age-standardized mortality rate due to CVD per 100 000 inhabitants, and the percent change of rates, by FU, in Brazil, in 1990-2019. The states of Maranhão and Alagoas had the highest risk for mortality, above the country average. The FUs with the greatest percent reductions in the period were Rondônia, Minas Gerais, Distrito Federal, Paraná, Santa Catarina, and São Paulo, in that order.
• Chart 1-9 shows the geographical distribution of mortality rates per 100 000 inhabitants, standardized by age in the Brazilian FUs, by sex, in 2000 and 2019, according to the SIM, and using the IBGE population. There was a decrease in the standardized mortality rates for both sexes, except for males from the states of Roraima, Piauí and Alagoas, despite the redistribution of ill-defined causes and correction of underreporting according to the GBD 2019 coefficients. Malta et al. compared historical series of CVD mortality rates in Brazil using SIM database with and without correction and the GBD 2017 estimates between 2000 and 2017. The authors pointed out that the increase in mortality rates observed in 2017 in some Northern and Northeastern FUs was due to the improvement in death registration and in the definition of underlying causes of death in recent years. 66. Malta DC, Teixeira R, Oliveira GMM, Ribeiro ALP. Cardiovascular Disease Mortality According to the Brazilian Information System on Mortality and the Global Burden of Disease Study Estimates in Brazil, 2000-2017. Arq Bras Cardiol. 2020;115(2):152-160. doi: 10.36660/abc.20190867.
https://doi.org/10.36660/abc.20190867...
• Brant et al. , analyzing GBD 2015 data, observed a decrease in age-standardized CVD mortality rate from 429.5 (1990) to 256.0 (2015) per 100 000 inhabitants (-40.4%), with marked differences across the FUs. That decrease was more pronounced in the FUs of the Southeastern and Southern regions and the Distrito Federal, regions that concentrate the largest populations and income, and more modest in most Northern and Northeastern states. 2929. Brant LCC, Nascimento BR, Passos VMA, Duncan BB, Bensenõr IJM, Malta DC, Souza MFM, Ishitani LH, França E, Oliveira MS, Mooney M, Naghavi M, Roth G, Ribeiro ALP. Variations and Particularities in Cardiovascular Disease Mortality in Brazil and Brazilian States in 1990 and 2015: Estimates From the Global Burden of Disease. Rev Bras Epidemiol. 2017;20(Suppl 01):116-28. doi: 10.1590/1980-5497201700050010.
• Importantly, the annual reduction in CVD mortality rates in Brazil was lower in the final years when considering the 1990-2019 period, for males and females.
• Regarding the trend by age group, the largest reductions in the CVD mortality rates per 100 000, between 1990 and 2019, were observed in the ‘under 5’ age group [-60.9 (-70.7 to -48.9)], followed by the 50-69 years age group [-50.6 (-52.7 to -48.4)].
• The FHP coverage was associated with a reduction in hospitalizations and mortality from CVD that were included in the national ambulatory care-sensitive list in Brazil, and its effect increased according to the duration of the FHP implementation in the municipality. Rasella et al . observed reductions in the mortalities from cerebrovascular disease and heart disease of 0.82 (95% CI, 0.79 - 0.86) and 0.79 (95% CI, 0.75 - 0.80) respectively, reaching 0.69 (0.66 - 0.73) and 0.64 (0.59 - 0.68), respectively, when the FHP coverage was consolidated during all 8 years studied. 3535. Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of Primary Health Care on Mortality From Heart and Cerebrovascular Diseases in Brazil: A Nationwide Analysis of Longitudinal Data. BMJ. 2014;349:g4014. doi: 10.1136/bmj.g4014.
• According to the SIM database, in 2019, CVD corresponded to 27.0% of total deaths, with the highest proportion in the Southeastern region and lowest in the Northern region. Ischemic heart disease accounted for 32.3% of total deaths from CVD in Brazil, and stroke was responsible for 27.8% of those deaths. The highest proportion of IHD mortality occurred in the states of Mato Grosso do Sul, Pernambuco, and São Paulo, while the highest proportion of stroke deaths occurred in the states of Amazonas, Pará, and Amapá, and the Distrito Federal (Table 1-4).
• The proportion of deaths due to CVD decreased for men (from 30.1% to 27.6%) and for women (from 31.1% to 29.9%) from 2000-2002 to 2015-2017. Moreover, Lotufo noted a constant excess of premature male deaths due to CVD during that period, with a male-to-female ratio of 2:1. 3636. Lotufo PA. Trends in Cardiovascular Diseases and Heart Disease Death Rates Among Adults Aged 45-64: Brazil, 2000-2017. Sao Paulo Med J. 2019;137(3):213-5. doi: 10.1590/1516-3180.2019.1373.220719.
There is a significant correlation of the SDI, an estimate of the socioeconomic level, with the CVD burden. Chart 1-12 shows the correlation of a greater reduction in the percent change of age-standardized CVD mortality rates, between 1990 and 2019, with a higher 2019 SDI, suggesting that the decrease in mortality from CVD followed the improvement in the local socioeconomic conditions, as observed in other studies. 55. Shemilt I, Thomas J, Morciano M. A Web-Based Tool for Adjusting Costs to a Specific Target Currency and Price Year. Evid. Policy. 2010;6(1):51-9. doi:10.1332/174426410X482999. , 3737. Villela PB, Klein CH, de Oliveira GMM. Socioeconomic factors and mortality due to cerebrovascular and hypertensive disease in Brazil. Rev Port Cardiol. 2019;38(3):205-12. doi: 10.1016/j.repc.2018.07.007.
• Lotufo et al . compared three different household income levels (high, middle, and low) with mortality rates due to CVD, in the city of São Paulo, from 1996 to 2010. The annual percent change and 95% CI for men living in the high, middle-, and low-income areas were -4.1 (-4.5 to -3.8), -3.0 (-3.5 to -2.6), and -2.5 (-2.8 to -2.1), respectively. The trend rates of women living in the high-income areas were -4.4 (-4.8 to -3.9) in 1996-2005 and -2.6 (-3.8 to -1.4) in 2005-2010. The reduction in deaths due to CVD was more significant for men and women living in the wealthiest neighborhoods, with a greater declining risk of death gradient for those living in the wealthiest areas as compared to the most deprived neighborhoods. 4040. Lotufo PA, Fernandes TG, Bando DH, Alencar AP, Benseñor IM. Income and Heart Disease Mortality Trends in Sao Paulo, Brazil, 1996 to 2010. Int J Cardiol. 2013;167(6):2820-3. doi: 10.1016/j.ijcard.2012.07.006.
• An inverse association of the HDIm and the supplementary health coverage with mortality due to CVD was observed, suggesting a relationship between socioeconomic factors and CVD. 3737. Villela PB, Klein CH, de Oliveira GMM. Socioeconomic factors and mortality due to cerebrovascular and hypertensive disease in Brazil. Rev Port Cardiol. 2019;38(3):205-12. doi: 10.1016/j.repc.2018.07.007. The HDIm increased between 2000 and 2010 in all FUs, in half of which it was 0.7 or higher. Supplementary health coverage increased in the country during the study period and was inversely associated with mortality due to CVD between 2004 and 2013. 3737. Villela PB, Klein CH, de Oliveira GMM. Socioeconomic factors and mortality due to cerebrovascular and hypertensive disease in Brazil. Rev Port Cardiol. 2019;38(3):205-12. doi: 10.1016/j.repc.2018.07.007.
• Soares et al . observed a decrease in CVD mortality in the states of Rio de Janeiro, São Paulo, and Rio Grande do Sul that preceded improvement in the socioeconomic index. The GDP per capita evolution, the child mortality decline, a higher educational level (represented by the schooling years of individuals over the age of 25 years), and the HDIm showed a high correlation with the reduction in the CVD mortality rate. A reduction in the mortality rates due to DCV, stroke, and IHD in the state of Rio de Janeiro State in past decades was preceded by an increase in the HDI. An increment of 0.1 in the HDI correlated with the following reductions in the number of deaths per 100 000 inhabitants: 53.5 for DCV; 30.2 for stroke; and 10.0 for IHD. 3838. Soares GP, Klein CH, Silva NA, Oliveira GM. Progression of Mortality due to Diseases of the Circulatory System and Human Development Index in Rio de Janeiro Municipalities. Arq Bras Cardiol. 2016;107(4):314-22. doi: 10.5935/abc.20160141. , 3939. Soares GP, Brum JD, Oliveira GM, Klein CH, Silva NAS. Evolution of Socioeconomic Indicators and Cardiovascular Mortality in Three Brazilian States. Arq Bras Cardiol. 2013;100(2):147-56. doi: 10.5935/abc.20130028.
• Baptista et al . investigated the relationship between CVD mortality rate and economic development over time and space, measured by GDP per capita, in Brazilian microregions from 2001 to 2015. They used the databases of the SIM (DATASUS) and of the SIDRA (IBGE). The authors observed a rapid decline in CVD mortality in the Southern and Southeastern microregions and a slower decline in the West-Central region. On the other hand, the Northern and Northeastern regions had an increase in CVD mortality over time, maybe due to lower access to healthcare and socioeconomic factors. 4141. Baptista E, Queiroz B. The Relation Between Cardiovascular Mortality and Development: Study for Small Areas in Brazil, 2001–2015. Demographic Res. 2019;41(51):1437-52. doi: 10.4054/DemRes.2019.41.51.
• Silveira et al ., studying the effect of ambient temperature on cardiovascular mortality in 27 Brazilian cities, observed a higher number of cardiovascular deaths associated with low and high temperatures in most of the Brazilian cities and the West-Central, Northern, Southern, and Southeastern regions. The overall RR for Brazil was 1.26 (95% CI, 1.17–1.35) for the 1stpercentile of temperature and 1.07 (95% CI, 1.01–1.13) for the 99thpercentile of temperature versus the 79thpercentile (27.7 °C), in which RR was the lowest. 4242. Silveira IH, Oliveira BFA, Cortes TR, Junger WL. The Effect of Ambient Temperature on Cardiovascular Mortality in 27 Brazilian Cities. Sci Total Environ. 2019;691:996-1004. doi: 10.1016/j.scitotenv.2019.06.493.
Burden of Disease
• Age-standardized DALY rates in Brazil were 6907 (95% UI, 6783-7039) per 100 000 inhabitants in 1990 and decreased to 3735 (95% UI, 3621-3849) per 100 000 inhabitants in 2019. The DALY rates declined in all five regions, with different patterns, faster in the South and Southeast and slower in the Northeast (Chart 1-13). There was a correlation between the percent decline in DALY rates and the increase in the SDI: the higher the SDI, the greater the decline in DALYs due to CVD. Distrito Federal, and the states of Rio de Janeiro and Santa Catarina had higher SDI and a great decline in DALY rates, while, the states of Alagoas, Piauí and Ceará had small declines in DALY rates and low SDI (Chart 1-14 and Table 1-5).
• Regarding YLLs, 8 130 233 years of life were lost in 2019 due to CVD mortality. It was higher among individuals aged 50-69 years as compared to the other age groups. The YLL rates have declined since 1990 for all age groups (Table 1-6). Age-standardized YLL rates decreased by 51.5% (95% UI, -53.4 to -49.7) from 1990 to 2019 (Table 1-6).
• Disability caused by CVD did not decline as observed with mortality. The age-standardized YLD rate declined by 15% from 1990 to 2019 (Table 1-7). The ‘50-69 years’ group had the greatest number of YLDs, followed close by the ‘15-49 years’ group. All age groups had a small decline in the age-standardized rates, and the ‘15-49 years’ group had the smallest (-0.7%) (Table 1-7).
Health Care Utilization and Cost
• In Brazil, from 2008 to 2019, the main groups of clinical and surgical cardiovascular procedures corresponded to 8 743 403 procedures paid by SUS. Of these, 7 462 563 were clinical procedures, led by HF, with 41.3% (3 085 359) of the admissions, followed by cerebrovascular diseases, 30.2% (2 253 344), acute coronary syndrome, 11.5% (855 125), and AMI with clinical approach, 10.1% (757 081) (Tables 1-8 and 1-9).
• Hospital admissions for clinical conditions of CVD decreased by 13 289 from 2008 to 2019 (Table 1-8), although the absolute numbers through the years were stable. In 2008, each clinical admission costed R$890 on average, and, in 2019, that cost was R$1488, a 67% increase (Table 1-10).
• Of the 1 280 840 cardiovascular surgical procedures performed from 2008 to 2019, 755 411 (58.9%) were coronary angioplasties, followed by 265 123 CABG surgeries (20.1%), and 151 902 valve surgeries (11.9%). The angioplasty/CABG ratio in 2008 was 1.8, increasing to 4.1 in 2019.
• Hospitalizations for surgical CVD procedures from 2008 to 2019 increased by 64% (Table 1-9). On average, each surgical procedure was reimbursed R$7036 in 2008, showing an unadjusted increase of 18% in 2019 as compared to 2008, at a cost of R$8319 per procedure (Table 1-12).
• Over the last 12 years, in Brazil, there has been a significant reduction in hospitalizations for HF and an increase in annual hospitalizations for AMI and cerebrovascular diseases, and flat trends in other groups of clinical procedures (Chart 1-15). Regarding the surgical approaches in the same years, there was a great increase in the annual number of coronary angioplasties and a trend towards stability in the number of other surgical procedures (Chart 1-16).
• Tables 1-10 and 1-11 show the amounts in Reais and International Dollars for the year 2019 (Int$2019), respectively, paid by the public health system for clinical cardiovascular admissions, in Brazil, from 2008 to 2019. The total amount spent on those hospitalizations was R$ 9 378 278, corresponding to Int$ 6 170 381 in 2019. Heart failure, cerebrovascular diseases and coronary artery disease syndromes were responsible for most of those values.
• The amounts paid for surgical procedures for CVD are shown in Reais in Table 1-12 and in Int$2019 in Table 1-13. Although they represent a smaller number as compared to clinical procedures, they were responsible for higher expenses, with R$ 10 524 044 spent, equivalent to Int$2019 6 853 635. The procedures used for the treatment of IHD, including coronary angioplasty and CABG, accounted for the largest fraction of those expenses.
Future Research
• The SIM, implemented in 1975, is an essential tool for monitoring mortality statistics in Brazil, because the registration of all deaths is mandatory in the FUs, with 98% coverage of the national territory in 2017, that coverage being lower in the Northern region than in the Southern region. The Northeastern region has the poorest coverage, still under 95%. 4343. Brasil. Ministério da Saúde. DATASUS. Informações de Saúde, Morbidade e Informações Epidemiológicas [Internet]. Brasília: Ministério da Saúde; 2016 [cited 2021 Nov 09]. Available From: http://datasus.saude.gov.br/informacoes-de-saude/tabnet/epidemiologica .
http://datasus.saude.gov.br/informacoes-...
Although SIM has improved through specific Ministry of Health projects, 4444. Frias PG, Szwarcwald CL, Morais Neto OL, Leal MD, Cortez-Escalante JJ, Souza PR Jr, Almeida WD, Silva JB Jr. Utilização das Informações Vitais para a Estimação de Indicadores de Mortalidade no Brasil: Da Busca Ativa de Eventos ao Desenvolvimento de Métodos. Cad Saude Publica. 2017;33(3):e00206015. doi: 10.1590/0102-311X00206015. , 4545. Almeida WDS, Szwarcwald CL. Adequacy of Mortality Data and Correction of Reported Deaths From the Proactive Search of Deaths. Cien Saude Colet. 2017;22(10):3193-203. doi: 10.1590/1413-812320172210.12002016. problems persist, such as ill-defined causes (around 6%), garbage codes and underreporting of deaths, which generate biases that may disrupt the metrics presented. As such, further research is needed to promote methodological adjustments for coverage, redistribution of ill-defined causes, especially in the older years of the historical series. On the other hand, the estimates from the GBD Study need additional research to implement models with better distribution of garbage codes adapted to local realities.
• It is worth mentioning that there is a lack of primary incidence data (cohorts) in Brazil, requiring research that allows us to understand how to face CVD in states and populations with low socioeconomic indices.
• Because of the reduction in the decline trend of age-standardized CVD mortality in the last 5 years, novel strategies to tackle CVD mortality must be studied. Understanding of the drivers of this change is essential to implement effective policies, particularly facing population aging, which will increase the number of individuals with CVD in the country.
2. STROKE (CEREBROVASCULAR DISEASES)
ICD-9 430 to 438; ICD-10 I60 to I69
See Tables 2-1 through 2-12 and Charts 2-1 through 2-3
Abbreviations Used in Chapter 2
| ACEI/ARB | Angiotensin Converting Enzyme Inhibitor/Angiotensin Receptor Blocker |
| CHD | Coronary Heart Disease |
| CI | Confidence Interval |
| DALYs | Disability-Adjusted Life Years |
| DATASUS | Brazilian Unified Health System Database |
| GBD | Global Burden of Disease |
| HS | Hemorrhagic Stroke |
| ICD | International Statistical Classification of Diseases and Related Health Problems |
| ICD-9 | International Statistical Classification of Diseases and Related Health Problems, 9thRevision |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems, 10thRevision |
| ICH | Intracerebral Hemorrhage |
| IMPACT-AF | Improve Treatment with Anticoagulants in Patients with Atrial Fibrillation |
| INR | International Normalized Ratio |
| IRR | Incidence Rate Ratio |
| IS | Ischemic Stroke |
| MAPS | Matão Preventing Stroke Study |
| MELAS | Mitochondrial Encephalomyopathy, Lactic Acidosis and Stroke-Like Episodes |
| NOAC | Non-Vitamin K Antagonist Oral Anticoagulant |
| OR | Odds Ratio |
| PNS | National Health Survey (in Portuguese, Pesquisa Nacional de Saúde ) |
| PURE | Prospective Urban Rural Epidemiological Study |
| RR | Relative Risk |
| SAH | Subarachnoid Hemorrhage |
| SD | Standard Deviation |
| SDI | Sociodemographic Index |
| SIM | Brazilian Mortality Information System (in Portuguese, Sistema de Informações sobre Mortalidade ) |
| SSQOL | Stroke Specific Quality of Life Scale) |
| TIA | Transient Ischemic Attack |
| UI | Uncertainty Interval |
| VKA | Vitamin K Antagonist |
| WHO | World Health Organization |
| YLDs | Years Lived with Disability |
| YLLs | Years of Life Lost |
– Number of cases and age-standardized prevalence rates (per 100 000) of ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil and its Federative Units.
– Number of cases and age-standardized prevalence rates (per 100 000) of stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil, according to age group.
– Number of cases and age-standardized incidence rates (per 100 000) of stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil and its Federative Units.
– Number of cases and age-standardized incidence rates (per 100 000) of stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil, according to age group.
– Number of deaths and age-standardized mortality rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil and its Federative Units.
– Number of deaths and age-standardized mortality rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil, according to age group.
– Number of YLLs and age-standardized YLL rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil and its Federative Units.
– Number of YLLs and age-standardized YLL rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil, according to age group.
– Number of YLDs and age-standardized YLD rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil and its Federative Units.
– Number of YLDs and age-standardized YLD rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil, according to age group.
– Number of DALYs and age-standardized DALY rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil and its Federative Units.
– Number of DALYs and age-standardized DALY rates (per 100 000) due to stroke, ischemic stroke, subarachnoid hemorrhage, and intracerebral hemorrhage in 1990 and 2019, and percent change of rates, in Brazil, according to age group.
– Age-standardized prevalence rates of stroke (A), ischemic stroke (B), intracerebral hemorrhage (C), and subarachnoid hemorrhage (D) (per 100 000 inhabitants), 1990-2019. Data derived from Global Burden of Disease Study 2019. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Age-standardized incidence rates of stroke, (A), ischemic stroke (B), intracerebral hemorrhage (C), and subarachnoid hemorrhage (D) (per 100 000 inhabitants), 1990-2019. Data derived from Global Burden of Disease Study 2019. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Age-standardized mortality rates due to stroke (A), ischemic stroke (B), intracerebral hemorrhage (C), and subarachnoid hemorrhage (D) (per 100 000 inhabitants), 1990-2019. Data derived from Global Burden of Disease Study 2019. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Prevalence
• Stroke prevalence estimates may differ slightly between studies because each study selects and recruits a sample of participants to represent the target study population (e.g., state, region, or country).
• In a community-based study in Brazil, using a questionnaire applied to 4496 individuals aged over 35 years, living in a deprived neighborhood in the city of São Paulo in 2011, Abe et al . found 243 individuals initially screened positive for stroke. The age-adjusted prevalence rate for men was 4.6% (95% CI, 3.5-5.7) and, for women, 6.5% (95% CI, 5.5-7.5). 4747. Abe IM, Lotufo PA, Goulart AC, Benseñor IM. Stroke Prevalence in a Poor Neighbourhood of São Paulo, Brazil: Applying a Stroke Symptom Questionnaire. Int J Stroke. 2011;6(1):33-9. doi: 10.1111/j.1747-4949.2010.00538.x.
• Using a screening tool, the Stroke Symptom Questionnaire, Fernandes et al. studied stroke prevalence in the town of Coari, in the Brazilian Amazon Basin, and compared stroke prevalence in riverside inhabitants to that in the urban population of the same municipality. Out of 4897 respondents in the urban area and 1028 in the rural area, the authors found a 6.3% crude prevalence of stroke in the rural area and 3.7% in the urban area, with differences maintained after sex and age adjustment. 4848. Fernandes TG, Benseñor IM, Goulart AC, Tavares BM, Alencar AP, Santos IS, Lotufo PA. Stroke in the Rain Forest: Prevalence in a Ribeirinha Community and an Urban Population in the Brazilian Amazon. Neuroepidemiology. 2014;42(4):235-42. doi: 10.1159/000362210.
• Using the WHO Stepwise Approach to Stroke Surveillance, Goulart et al. conducted a study to verify stroke mortality and morbidity rates in an area of São Paulo, Brazil. The questionnaire determining stroke prevalence was applied door to door in a family-health-program neighborhood (Step 3). Out of 3577 subjects over the age of 35 years evaluated at home, 244 (6.82%) cases of stroke survivors were identified via the questionnaire validated by a board-certified neurologist. 4949. Goulart AC, Bustos IR, Abe IM, Pereira AC, Fedeli LM, Benseñor IM, Lotufo PA. A Stepwise Approach to Stroke Surveillance in Brazil: The EMMA (Estudo de Mortalidade e Morbidade do Acidente Vascular Cerebral) Study. Int J Stroke. 2010;5(4):284-9. doi: 10.1111/j.1747-4949.2010.00441.x.
• Benseñor et al. analyzed a community-based epidemiological survey (PNS - 2013) with a Brazilian representative sample to assess the absolute numbers with respective prevalence rates of stroke and post-stroke disabilities. The authors estimated 2 231 000 strokes and 568 000 stroke cases with severe disabilities. The point prevalence estimates for stroke were 1.6% and 1.4% in men and women, respectively. 5050. Bensenor IM, Goulart AC, Szwarcwald CL, Vieira ML, Malta DC, Lotufo PA. Prevalence of Stroke and Associated Disability in Brazil: National Health Survey--2013. Arq Neuropsiquiatr. 2015;73(9):746-50. doi: 10.1590/0004-282X20150115.
• According to data from the GBD Brazil Group, the age-standardized prevalence rates of IS per 100 000 were 1327.6 (1151.2 to 1516) in 1990 and 870.1 (761.1 to 992.8) in 2019, representing a percent change of -34.5 (-36.7 to -0.3) (Table 2-1 and Chart 2-1). The highest percent change occurred in the state of Rondônia -41.7 (-46.2 to -0.4) and the lowest in the state of Amapá -23.4 (-28.6 to -0.2) (Table 2-1). For adults, the highest percent change was observed among people aged 50-69 years, -39.5 (-42.6 to -0.4) (Table 2-2). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized prevalence rates of ICH per 100 000 were 507.5 (438.9 to 584.1) in 1990 and 315.9 (275 to 361.4) in 2019, representing a percent change of -37.7 (-40.5 to -0.3) (Table 2-1 and Chart 2-1). For adults, the highest percent change was observed among people aged 50-69 years, -44.8 (-47.4 to -0.4) (Table 2-2). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized prevalence rates of SAH per 100 000 were 158.6 (131.7 to 192.4) in 1990 and 124.8 (104.2 to 150.1) in 2019, representing a percent change of -21.3 (-24.3 to -0.2) (Chart 2-1 and Table 2-1). For adults, the highest percent change was observed among people aged 50-69 years, -21.1 (-24.4 to -0.2) (Table 2-2). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Incidence
Stroke Subtypes
• Data from the Joinville community-based study showed that, when comparing different time periods (1995, 2005-2006, 2010-2011, and 2012-2013), the stroke incidence decreased. Over the last 18 years, the overall stroke (e.g., all major stroke types) incidence in Joinville decreased by 37% (95% CI, 32 - 42). 5151. Cabral NL, Cougo-Pinto PT, Magalhaes PS, Longo AL, Moro CH, Amaral CH, Costa G, Reis FI, Gonçalves AR, Nagel V, Pontes-Neto OM. Trends of Stroke Incidence From 1995 to 2013 in Joinville, Brazil. Neuroepidemiology. 2016;46(4):273-81. doi: 10.1159/000445060.
• The incidence of first ever stroke adjusted to the Brazilian population was 86.6 per 100 000 (95% CI, 80.5 - 93.0) in 2005-2006 and 113.46 per 100 000 (95% CI, 101.5 - 126.8) in 1995. 5252. Cabral NL, Gonçalves AR, Longo AL, Moro CH, Costa G, Amaral CH, Souza MV, Eluf-Neto J, Fonseca LA. Trends in Stroke Incidence, Mortality and Case Fatality Rates in Joinville, Brazil: 1995-2006. J Neurol Neurosurg Psychiatry. 2009;80(7):749-54. doi: 10.1136/jnnp.2008.164475. The overall incidence, age-adjusted to world population per 100 000 person-years was 143.7 (95% CI, 128.4–160.3) in 1995, fell to 105.4 (95% CI, 98.0–113.2) in 2005–2006, and then to 90.9 (95% CI, 85.1–96.9) in 2012-2013. The age-standardized incidence of first-ever stroke stratified by gender and age also decreased significantly over time. The reduction was 11% greater in men (42%; 95% CI, 35–49) than in women (31%; 95% CI, 23–39), and 16% greater in young people (≤ 44 years: 54%; 95% CI, 41–66) than in older people (>44 years: 38%; 95% CI, 33–43). 5151. Cabral NL, Cougo-Pinto PT, Magalhaes PS, Longo AL, Moro CH, Amaral CH, Costa G, Reis FI, Gonçalves AR, Nagel V, Pontes-Neto OM. Trends of Stroke Incidence From 1995 to 2013 in Joinville, Brazil. Neuroepidemiology. 2016;46(4):273-81. doi: 10.1159/000445060.
• From 1995 to 2013, the proportion of IS increased by 12%, whereas that of HS decreased by 16%. Meanwhile, the proportion of SAH remained relatively stable, ranging from 7.5% in 1995 to 6% in 2012-2013. The weight of the decrease in age-adjusted stroke incidence was proportionally higher for HS than for IS, whereas that of SAH remained stable. In the last 8 years, the incidences of IS and HS showed significant absolute decreases of 15% (95% CI, 1–28) and 60% (95% CI, 13–86), respectively. Meanwhile, the incidence of SAH showed a 29% nonsignificant absolute decrease (95% CI, 15–92). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In the second Matão stroke registry study, all incident stroke events (81 cases) that occurred between August 1, 2015, and July 31, 2016, were registered. The mean age increased by 9%, from 65.2 (95% CI, 62.6–67.8) to 71.0 (95% CI, 68.1–73.8) years. Between 2003-2004 and 2015-2016, the age-adjusted incidence decreased by 39% (IRR 0.61; 95% CI, 0.46–0.79) and mortality by 50% (IRR 0.50; 95% CI, 0.31– 0.94). The 1-year case fatality was 26%; approximately 56% of the patients were functionally independent, while 7% had a recurrent stroke. 5353. Minelli C, Cabral NL, Ujikawa LT, Borsetti Neto FA, Chiozzini EML, Reis GC, Borin LA, Carvalho CC. Trends in the Incidence and Mortality of Stroke in Matão, Brazil: The Matão Preventing Stroke (MAPS) Study. Neuroepidemiology. 2020;54(1):75-82. doi: 10.1159/000503005. Compared with the results of the previous Matão stroke registry study, 5454. Minelli C, Fen LF, Minelli DP. Stroke Incidence, Prognosis, 30-Day, and 1-Year Case Fatality Rates in Matão, Brazil: A Population-Based Prospective Study. Stroke. 2007;38(11):2906-11. doi: 10.1161/STROKEAHA.107.484139. these outcomes did not differ significantly.
• Data from the GBD Brazil Group show that the age-standardized incidence rates per 100 000 of stroke were 224.6 (201.6 to 251.8) in 1990 and 127 (113.8 to 142.1) in 2019, representing a percent change of -43.5 (-44.7 to -0.4) (Table 2-3 and Chart 2-2). The highest percent change occurred in Distrito Federal, -47.7 (-49.7 to -0.5), and the lowest in the state of Ceará, -30.6 (-33.2 to -0.3) (Table 2-3). The highest percent change was observed among people aged 15-49 years, -38.1 (-40.9 to -0.4) (Table 2-4). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized incidence rates of IS per 100 000 were 136.6 (115.7 to 163.1) in 1990 and 78.2 (66.1 to 93) in 2019, representing a percent change of -42.7 (-44.3 to -0.4) (Table 2-3 and Chart 2-2). For adults, the highest percent change was observed among people aged 50-69 years, -48 (-49.9 to -0.5) (Table 2-4). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized incidence rates of ICH per 100 000 were 66 (56.1 to 77.9) in 1990 and 31.6 (26.6 to 37.3) in 2019, representing a percent change of -52.1 (-53.5 to -0.5) (Table 2-3 and Chart 2-2). For adults, the highest percent change was observed among people aged 50-69 years, -53.2 (-55.3 to -0.5) (Table 2-4). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized incidence rates of SAH per 100 000 were 22.1 (18.6 to 26.3) in 1990 and 17.2 (14.4 to 20.6) in 2019, representing a percent change of -22.2 (-25.1 to -0.2) (Table 2-3 and Chart 2-2). For adults, the highest percent change was observed among people aged 15-49 years, -23.6 (-27.8 to -0.2) (Table 2-4). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Mortality
• In the stroke population-based study known as MAPS, between 2003–2004 and 2015–2016, mortality increased by 50% (IRR 0.50; 95% CI, 0.31–0.94). The 1-year case fatality was 26%. Approximately 56% of the patients were functionally independent, while 7% had a recurrent stroke. 5353. Minelli C, Cabral NL, Ujikawa LT, Borsetti Neto FA, Chiozzini EML, Reis GC, Borin LA, Carvalho CC. Trends in the Incidence and Mortality of Stroke in Matão, Brazil: The Matão Preventing Stroke (MAPS) Study. Neuroepidemiology. 2020;54(1):75-82. doi: 10.1159/000503005. Compared with the results from the first Matão stroke registry study, 5454. Minelli C, Fen LF, Minelli DP. Stroke Incidence, Prognosis, 30-Day, and 1-Year Case Fatality Rates in Matão, Brazil: A Population-Based Prospective Study. Stroke. 2007;38(11):2906-11. doi: 10.1161/STROKEAHA.107.484139. these rates did not differ significantly.
• Results from a study assessing the association between the mortality due to cerebrovascular diseases and the Municipal Human Development Index and extent of supplementary health coverage in the Brazilian Federative Units, between 2004 and 2013, showed that the percentage of supplementary health coverage in Brazil increased in that period and had an inverse relationship with mortality. Additionally, the correlation coefficient between Municipal Human Development Index scores and the mortality rates weighted by ill-defined causes and standardized by age showed and inverse association. Thus, both increased Municipal Human Development Index and health coverages were associated with decreased mortalities. 3737. Villela PB, Klein CH, de Oliveira GMM. Socioeconomic factors and mortality due to cerebrovascular and hypertensive disease in Brazil. Rev Port Cardiol. 2019;38(3):205-12. doi: 10.1016/j.repc.2018.07.007.
• Data from the GBD Brazil Group show that the age-standardized mortality rates from stroke per 100 000 were 137.8 (127.8 to 144) in 1990 and 58.1 (52.6 to 61.8) in 2019, representing a percent change of -57.8 (-60.4 to -0.6) (Table 2-5 and Chart 2-3). The highest percent change occurred in the state of Goiás, -65.9 (-71.8 to -0.6), and the lowest, in the state of Maranhão, -22.7 (-37.2 to 0) (Table 2-5). For adults, the highest percent change was observed among people aged 50-69 years, -61 (-63.6;-0.6) (Table 2-6). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized mortality rates from IS per 100 000 were 80 (72.5 to 84.3) in 1990 and 33.9 (29.7 to 36.6) in 2019, representing a percent change of -57.6 (-60.9 to -0.5) (Table 2-5 and Chart 2-3). For adults, the highest percent change was observed among people aged 15-49 years, -66.1 (-70.5 to -0.6) (Table 2-6). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized mortality rates from ICH per 100 000 were 49.8 (47.1 to 52.2) in 1990 and 18.6 (17.3 to 19.8) in 2019, representing a percent change of -62.6 (-65.3 to -0.6) (Table 2-5 and Chart 2-3). For adults, the highest percent change was observed among people aged 50-69 years, -63.1 (-65.7 to -0.6) (Table 2-6). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized mortality rates from SAH per 100 000 were 8 (7.3 to 8.4) in 1990 and 5.5 (5 to 5.9) in 2019, representing a percent change of -30.3 (-36.2 to -0.2) (Table 2-6 and Chart 2-3). For adults, the highest percent change was observed among people aged 15-49 years, -40.8 (-46 to -0.3) (Table 2-6). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Temporal Trends
• The estimates from the GBD 2015 used to analyze the magnitude and trends of mortality rates and DALYs from cerebrovascular disease (ICD-10: I60-I69) in the 27 Brazilian Federative Units between 1990 and 2015, showed that, despite the increase in the absolute number of deaths due to cerebrovascular disease, the proportion of deaths under the age of 70 years was halved between 1990 and 2015. From 1990 to 2015, the risk of death attributable to stroke decreased for both men (-2.41% per year) and women (-2.51% per year). Nevertheless, the annual reduction in mortality rates adjusted for age, for both sexes, slowed between 2005 and 2015 when compared to the previous period of 1990-2005. States in the lower SDI tertile had less significant reductions (-1.23 and -1.84% per year) as compared to those in the middle (-1.94 and - 2.22%) and upper (-2.85 and -2.82%) SDI tertiles for men and women, respectively. In addition, the YLDs decreased among states, but less expressively. 5555. Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, Ribeiro ALP, Bensenõr IJM. Cerebrovascular Disease in Brazil From 1990 to 2015: Global Burden of Disease 2015. Rev Bras Epidemiol. 2017;20(Suppl 1):129-141. doi: 10.1590/1980-5497201700050011.
• A study on age-adjusted stroke mortality trends among adults (30-69 years-old) from Brazilian regions between 1996 and 2011 evaluated the influence of the methods used to correct death rates in the final estimates. Corrections were implemented by reallocation of deaths with non-registered sex or age, redistribution of garbage codes and redistribution of ill-defined causes of deaths, and changed significantly the observed age-adjusted stroke mortality rates in 1996 and 2011, pre- and post-correction, respectively: 1) for men: in 1996, 82.9 and 113.6; and, in 2011, 49.6 and 60.9; and 2) for women: in 1996, 58.2 and 84.4; and, in 2011, 34.7 and 42.3. 5656. Passos VM, Ishitani LH, Franco GC, Lana GC, Abreu DM, Marinho MF, França EB. Consistent Declining Trends in Stroke Mortality in Brazil: Mission Accomplished? Arq Neuropsiquiatr. 2016;74(5):376-81. doi: 10.1590/0004-282X20160055.
• A study assessing regional differences in mortality transition and using data from the SIM from 1990 to 2012 showed a –48.05% variation in the mortality coefficient for stroke. Most regions showed a reduction in mortality rates: –61.99% in the Southeast, –55.49% in the South, –26.91% in the West-Central, and –20.78% in the North. Only the Northeast showed increased mortality rates (13.77%). 5757. Guimarães RM, Andrade SS, Machado EL, Bahia CA, Oliveira MM, Jacques FV. Diferenças regionais na transição da mortalidade por doenças cardiovasculares no Brasil, 1980 a 2012. Rev Panam Salud Publica. 2015;37(2):83-9.
• In the city of São Paulo, from 1996 to 2011, 77 848 stroke deaths were confirmed with 51.4% of them among persons aged 35–74 years old. In that period, age-adjusted mortality rates from cerebrovascular diseases decreased by 46.6% in men and by 47.8% in women. For men in high-income neighborhoods, the downward trend was constant; in the middle-income area, there was a sharp decline from 1996 to 2000, followed by a slower pace between 2000 and 2011. In the low-income area, the annual percent change was higher between 1996 and 2002, with a mild decline in 2002–2011. For women in high income areas, there was a sharp decline from 1996 to 2003, and a lower decrease in the last half of the period; in the low- and middle-income areas, the decline was constant during all periods. For the full period, both sexes and age group of 35–74 years, the decline in age-adjusted rates were more pronounced among those residing in the wealthiest area as compared to those living in the poorest area. This same pattern, but with a decline in magnitude, was observed in people aged ≥75 years in all areas as compared to other age groups, for both sexes. Additionally, the temporal evolution of the ratios of age-adjusted rates between people aged 35–74 years living in low- and high-income areas was as follows: for men, from 1996 to 1998, the rate ratio was 2.03, and, from 2009 to 2011, 2.34; for women, from 1996 to 1998, the rate ratio was 2.09, and, from 2009 to 2011, 2.58. The trends of the ratios of age-adjusted rates between those areas showed an annual percent change growth of 1.4 (0.5–2.4) for men and 1.1 (0.1–2.0) for women. 5858. Fernandes TG, Bando DH, Alencar AP, Benseñor IM, Lotufo PA. Income Inequalities and Stroke Mortality Trends in Sao Paulo, Brazil, 1996-2011. Int J Stroke. 2015;10(100):34-7. doi: 10.1111/ijs.12526.
Global Burden of Cerebrovascular Diseases
YLL
• Data from the GBD Brazil Group show that the age-standardized YLL rates due to stroke per 100 000 were 2778.6 (2659.5 to 2879.2) in 1990 and 1098.7 (1025.8 to 1153.7) in 2019, representing a percent change of -60.5 (-62.7 to -0.6) (Table 2-7). For adults, the highest percent change was observed among people aged 50-69 years, -61,7 (-64,3 to -0,6) (Table 2-8). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized YLL rates due to IS per 100 000 were 1211.1 (1133.8 to 1268.9) in 1990 and 479.7 (435.1 to 510.8) in 2019, representing a percent change of -60.4 (-63.5 to -0.6) (Tables 2-7 and 2-8). For adults, the highest percent change was observed among people aged 15-49 years, -66,6 (-71,1 to -0,6) (Table 2-8). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized YLL rates due to ICH per 100 000 were 1283.5 (1227.7 to 1351) in 1990 and 449.2 (423.3 to 472.5) in 2019, representing a percent change of -65 (-67.6 to -0.6) (Tables 2-7 and 2-8). For adults, the highest percent change was observed among people aged 50-69 years, -63,9 (-66,5 to -0,6) (Table 2-8). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized YLL rates due to SAH per 100 000 were 284 (253.8 to 297.2) in 1990 and 169.8 (158.3 to 180.8) in 2019, representing a percent change of -40.2 (-44.9 to -0.3) (Tables 2-7 and 2-8). For adults, the highest percent change was observed among people aged 15-49 years, -42,8 (-47,7 to -0,3) (Table 2-8). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
YLD
• Data from the GBD Brazil Group show that the age-standardized YLD rates due to stroke per 100 000 were 180.4 (133.2 to 228.8) in 1990 and 120.9 (88.7 to 152.6) in 2019, representing a percent change of -33 (-34.8 to -0.3) (Tables 2-9 and 2-10). The highest percent change occurred in the state of Rondônia, -39.5 (-43.8 to -0.4), and the lowest in the state of Amapá, -23 (-27.3 to -0.2) (Table 2-9). For adults, the highest percent change was observed among people aged 50-69 years, -38.7 (-40.9 to -0.4) (Table 2-10). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized YLD rates due to IS per 100 000 were 122.2 (88 to 156.8) in 1990 and 81.2 (58.3 to 104) in 2019, representing a percent change of -33.5 (-35.9 to -0.3) (Tables 2-9 and 2-10). For adults, the highest percent change was observed among people aged 50-69 years, -39 (-42.1 to -0.4) (Table 2-10). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized YLD rates due to ICH per 100 000 were 44.3 (32.3 to 56.6) in 1990 and 28.5 (20.7 to 36.9) in 2019, representing a percent change of -35.7 (-38.8 to -0.3) (Tables 2-9 and 2-10). For adults, the highest percent change was observed among people aged 50-69 years, -43.8 (-47.2 to -0.4) (Table 2-10). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized YLD rates due to SAH per 100 000 were 13.9 (9.7 to 18.6) in 1990 and 11.2 (7.9 to 15) in 2019, representing a percent change of -19.5 (-23.7 to -0.2) (Tables 2-9 and 2-10). For adults, the highest percent change was observed among people aged 50-69 years, -19.9 (-26.1 to -0.1) (Table 2-10). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
DALY
• Data from the GBD Brazil Group show that the age-standardized DALY rates due to stroke per 100 000 were 2959 (2829.6 to 3063) in 1990 and 1219.6 (1142 to 1285.5) in 2019, representing a percent change of -58.8 (-61 to -0.6) (Tables 2-11 and 2.12). The highest percent change occurred in the state of Santa Catarina -67.8 (-71.1 to -0.6) and the lowest in the state of Maranhão -31.7 (-45.2 to -0.1) (Table 2-11). For adults, the highest percent change was observed among people aged 50-69 years, -60.3 (-62.8 to -0.6) (Table 2-12). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized DALY rates due to IS per 100 000 were 1333.3 (1244.5 to 1403.6) in 1990 and 561 (510.4 to 599.8) in 2019, representing a percent change of -57.9 (-61 to -0.6) (Tables 2-11 and 2-12). For adults, the highest percent change was observed among people aged 50-69 years, -63.5 (-66.5 to -0.6) (Table 2-12). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized DALY rates due to ICH per 100 000 were 1327.8 (1274 to 1397.3) in 1990 and 477.6 (450.9 to 503.8) in 2019, representing a percent change of -64 (-66.6 to -0.6) (Tables 2-11 and 2-12). For adults, the highest percent change was observed among people aged 50-69 years, -63.3 (-65.9 to -0.6) (Table 2-12). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-standardized DALY rates due to SAH per 100 000 were 297.9 (267.5 to 312.7) in 1990 and 181 (169.4 to 192.8) in 2019, representing a percent change of -39.2 (-43.8 to -0.3) (Tables 2-11 and 2-12). For adults, the highest percent change was observed among people aged 15-49 years, -41.5 (-46.4 to -0.3) (Table 2-12). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Healthcare Utilization
Hospital Admissions
• Using time-series analysis, Katz et al. evaluated the relationship between stroke-related unemployment rate and hospital admission in Brazil over a recent 11-year span. Data on monthly hospital admissions due to stroke from March 2002 to December 2013 were extracted from the DATASUS, revealing 1 581 675 admissions due to stroke in the period. The unemployment rate decreased from 12.9% in 2002 to 4.3% in 2013, while admissions due to stroke increased. However, the adjusted model showed no positive association between the unemployment rate and admissions due to stroke (estimate coefficient=2.40±4.34; p=0.58). 5959. Katz M, Bosworth HB, Lopes RD, Dupre ME, Morita F, Pereira C, Franco FG, Prado RR, Pesaro AE, Wajngarten M. A Time-Series Analysis of the Relation Between Unemployment Rate and Hospital Admission for Acute Myocardial Infarction and Stroke in Brazil Over More Than a Decade. Int J Cardiol. 2016;224:33-6. doi: 10.1016/j.ijcard.2016.08.309.
• Using data from the SIH, the SIM and the Brazilian Institute of Geography and Statistics, Adami et al. analyzed rates of stroke-related mortality and incidence of hospital admissions in Brazilians aged 15-49 years, according to region and age group, between 2008 and 2012. Stroke was defined according to the ICD-10 (I60-I64). Crude and standardized mortality (WHO reference) and incidence of hospital admissions per 100 000 inhabitants, stratified by region and age group, were estimated. The authors found 131 344 hospital admissions due to stroke in Brazilians aged 15-49 years between 2008 and 2012. During the same time, the rate of hospital admissions stabilized: 24.67 (95% CI, 24.66 - 24.67) in 2008 and 25.11 (95% CI, 25.10 - 25.11) in 2012 (β = 0.09, p = 0.692, r2 = 0.05). 6060. Adami F, Figueiredo FW, Paiva LS, Sá TH, Santos EF, Martins BL, Valenti VE, Abreu LC. Mortality and Incidence of Hospital Admissions for Stroke among Brazilians Aged 15 to 49 Years between 2008 and 2012. PLoS One. 2016;11(6):e0152739. doi: 10.1371/journal.pone.0152739.
• Dantas et al. performed a study to assess stroke-related hospitalizations in the Brazilian Unified Health System from 2009 to 2016. The authors selected hospitalization registries according to the stroke diagnosis codes from the ICD-10. From 2009 to 2016, the number of admissions increased from 131 122 to 146 950, and the absolute number of in-hospital deaths increased from 28 731 to 31 937. Younger age and male sex were significantly associated with patient survival. The annual age-adjusted hospitalization and in-hospital mortality rates decreased by 11.8% and 12.6%, respectively, but the case-fatality rate increased for patients older than 70 years. 6161. Dantas LF, Marchesi JF, Peres IT, Hamacher S, Bozza FA, Neira RAQ. Public Hospitalizations for Stroke in Brazil From 2009 to 2016. PLoS One. 2019;14(3):e0213837. doi: 10.1371/journal.pone.0213837.
• In a retrospective study using data from DATASUS and assessing the six leading causes of hospital admissions in elders from 2005 and 2015, stroke was the third cause of admissions in 2015 for both genders and the age group of 60-79 years, with a -2.6 variation. 6262. Rossetto C, Soares JV, Brandão ML, Rosa NGD, Rosset I. Causes of Hospital Admissions and Deaths Among Brazilian Elders Between 2005 and 2015. Rev Gaucha Enferm. 2019;40:e20190201. doi: 10.1590/1983-1447.2019.20190201.
Healthcare and Quality Indicators
• An analysis of the expansion trends of the family health strategy and hospitalization for conditions sensitive to primary care in Rio de Janeiro, between 1998 and 2015, showed a 7.6% decrease in hospitalizations for cerebrovascular diseases. 6363. Pimenta L, Dutra VGP, Castro ALB, Guimarães RM. Analysis of Conditions Sensitive to Primary Care in a Successful Experience of Primary Healthcare Expansion in Brazil, 1998-2015. Public Health. 2018;162:32-40. doi: 10.1016/j.puhe.2018.05.011.
• A study assessing sociodemographic factors related to lack of hospital care for cerebrovascular disease deaths in the state of São Paulo in the periods of 1996-1998 and 2013-2015 showed that, of the 127 319 people who died due to stroke during the mentioned periods, 19 362 (15.2%) had no hospital care. In the latter period, a higher risk for death without care was identified for individuals of yellow race (RR = 1.48; 95% CI, 1.25-1.77), and a lower risk for black individuals (RR = 0,86; 95% CI, 0.76-0.95), married people (RR = 0.70; 95% CI, 0.64-0.75), and for those living in the city of São Paulo (RR = 0.92; 95% CI, 0.86-0.98). 6464. Santos EFS, Antunes JLF. Fatores Associados à Falta de Assistência Hospitalar nos Óbitos por Doença Cerebrovascular, São Paulo, Brasil: Análise Comparativa entre 1996-1998 e 2013-2015. Cad Saude Publica. 2020;36(4):e00227718. doi: 10.1590/0102-311X00227718.
• Data from a hospital-based study evaluating 2407 consecutive patients (mean age, 67.7 ± 14.4 years; 51.8% females) admitted to 19 hospitals in the city of Fortaleza showed that IS was the most frequent subtype (72.9%), followed by intraparenchymal hemorrhage (15.2%), SAH (6.0%), TIA (3%), and undetermined stroke (2.9%). The median time from symptom onset to hospital admission was 12.9 (3.8 –32.5) hours. Hypertension was the most common risk factor. Only 1.1% of the patients with IS received thrombolysis. The median time from hospital admission to neuroimaging was 3.4 (1.2–26.5) hours. 6565. Carvalho JJ, Alves MB, Viana GÁ, Machado CB, Santos BF, Kanamura AH, Lottenberg CL, Neto MC, Silva GS. Stroke Epidemiology, Patterns of Management, and Outcomes in Fortaleza, Brazil: A Hospital-Based Multicenter Prospective Study. Stroke. 2011;42(12):3341-6. doi: 10.1161/STROKEAHA.111.626523.
• A study evaluating factors that influence temporal trends in quality indicators for IS in a tertiary hospital, certified by the Joint Commission International as a primary stroke center, assessed 551 patients discharged with IS from January 2009 to December 2013 (median age 77.0 years, interquartile range: 64.0-84.0; 58.4% men). Ten predefined performance measures selected by the Get With the Guidelines-Stroke program were assessed. The quality indicators that improved with time were the use of cholesterol lowering therapy (P = 0.02) and stroke education (P = 0.04). The median composite perfect care did not consistently improve throughout the period (P = 0.13). After a multivariable adjustment, only thrombolytic treatment (OR 2.06, P < 0.01), dyslipidemia (OR 2.03, P < .01), and discharge in a Joint Commission International visit year (OR 1.8, P < 0.01) remained as predictors of a perfect care index of 85% or higher. The quality indicators with worse performance (anticoagulation for atrial fibrillation and cholesterol reduction) were similar in the tertiary and secondary community hospitals. The overall perfect care measure did not improve and was influenced by being discharged in a Joint Commission International visit year, having dyslipidemia, and having undergone thrombolytic treatment. 6666. Alves MB, Silva GS, Miranda RCA, Massaud RM, Vaccari AMH, Cendoroglo-Neto M, Diccini S. Patterns of Care and Temporal Trends in Ischemic Stroke Management: A Brazilian Perspective. J Stroke Cerebrovasc Dis. 2017;26(10):2256-63. doi: 10.1016/j.jstrokecerebrovasdis.2017.05.008.
• An analysis of the stroke units in two centers from the cities of Curitiba and Botucatu, for the key performance indicators required by the Ministry of Health in Brazil, including the percentage of patients admitted to the stroke unit, venous thromboembolism prophylaxis in the first 48 hours after admission, pneumonia and hospital mortality due to stroke, and hospital discharge on antithrombotic therapy in patients without cardioembolic mechanism, showed that both centers admitted over 80% of the patients in their stroke unit. The incidence of venous thromboembolism prophylaxis was > 85% and that of in-hospital pneumonia was < 13%. The rate of in-hospital mortality from stroke was < 15% and that of hospital discharge on antithrombotic therapy was > 70%. 6767. Lange MC, Braga GP, Nóvak EM, Harger R, Felippe MJDB, Canever M, Dall’Asta I, Rauen J, Bazan R, Zetola V. Key Performance Indicators for Stroke From the Ministry of Health of Brazil: Benchmarking and Indicator Parameters. Arq Neuropsiquiatr. 2017;75(6):354-8. doi: 10.1590/0004-282X20170051.
• A before and after study assessed the effect on mortality rates of the implementation of a dedicated cardiovascular and stroke unit in an emergency department of a tertiary public hospital in the city of Porto Alegre. The period prior to that unit implementation (2002 through 2005) included 4164 patients, and the vascular unit period (2007 to 2010) included 6280 patients. Overall, the case-fatality rate for acute vascular conditions decreased from 9% to 7.3% with the vascular unit implementation (p = 0.002). The in-hospital mortality rates from acute coronary syndrome dropped from 6% to 3.8% (p = 0.003) and from acute pulmonary embolism dropped from 32.1% to 10.8% (p < 0.001). The stroke case-fatality rate did not decrease despite improvements in the quality of stroke healthcare indicators. 6868. Nasi LA, Ferreira-Da-Silva AL, Martins SC, Furtado MV, Almeida AG, Brondani R, Wirth L, Kluck M, Polanczyk CA. Implementation of a Dedicated Cardiovascular and Stroke Unit in a Crowded Emergency Department of a Tertiary Public Hospital in Brazil: Effect on Mortality Rates. Acad Emerg Med. 2014;21(1):40-6. doi: 10.1111/acem.12291.
• A cluster randomized trial assessed the effect of a multifaceted quality improvement intervention on adherence to evidence-based therapies for the care of patients with acute IS and TIA (including case management, reminders, a roadmap and checklist for the therapeutic plan, educational materials, and periodic audit and feedback reports to each intervention cluster). The study evaluated 1624 patients from 36 hospitals covering all Brazilian regions. The primary outcome was a composite adherence score for acute IS and TIA performance measures, and the secondary outcomes included an all-or-none composite endpoint of performance measures. The overall mean (SD) age of the patients enrolled in the study was 69.4 (13.5) years, and 913 (56.2%) were men. Overall mean (SD) composite adherence score for the 10 performance measures in the intervention group hospitals as compared to the control group hospitals was 85.3% (20.1%) vs. 77.8% (18.4%) (mean difference, 4.2%; 95% CI, -3.8% to 12.2%). As a secondary endpoint, 402 of 817 patients (49.2%) at the intervention group hospitals received all the therapies they were eligible for vs. 203 of 807 (25.2%) in the control group hospitals (OR, 2.59; 95% CI, 1.22-5.53; P = 0.01). The intervention did not result in a significant increase in the composite adherence score for evidence-based therapies in patients with acute IS or TIA. However, when using an all-or-none approach, the intervention resulted in improved adherence to evidence-based therapies and in improved thrombolysis rates. 6969. Machline-Carrion MJ, Santucci EV, Damiani LP, Bahit MC, Málaga G, Pontes-Neto OM, Martins SCO, Zétola VF, Normilio-Silva K, Freitas GR, Gorgulho A, Salles A, Silva BGP, Santos JY, Jesuíno IA, Bueno PRT, Cavalcanti AB, Guimarães HP, Xian Y, Bettger JP, Lopes RD, Peterson ED, Berwanger O; BRIDGE-Stroke Investigators. Effect of a Quality Improvement Intervention on Adherence to Therapies for Patients With Acute Ischemic Stroke and Transient Ischemic Attack: A Cluster Randomized Clinical Trial. JAMA Neurol. 2019;76(8):932-41. doi: 10.1001/jamaneurol.2019.1012.
Complications
Disability
• Benseñor et al. analyzed a community-based epidemiological survey (PNS - 2013) with a Brazilian representative sample to assess the absolute numbers with respective prevalence rates of stroke and post-stroke disabilities. The authors estimated 2 231 000 strokes and 568 000 stroke cases with severe disabilities. The point prevalence estimates for stroke were 1.6% and 1.4% in men and women, respectively. The prevalence of post-stroke disabilities was 29.5% for men and 21.5% for women. Stroke prevalence rates increased with aging, low education level, among people living in urban areas, and showed no difference according to self-reported skin color. The degree of post-stroke disability was not statistically different according to sex, race, education level or living area. 5050. Bensenor IM, Goulart AC, Szwarcwald CL, Vieira ML, Malta DC, Lotufo PA. Prevalence of Stroke and Associated Disability in Brazil: National Health Survey--2013. Arq Neuropsiquiatr. 2015;73(9):746-50. doi: 10.1590/0004-282X20150115.
• In a subsequent assessment based on the PNS - 2013, access to rehabilitation is deficient: only 0.27% of the individuals underwent physical therapy for stroke and 0.12% performed some type of rehabilitation treatment, which impairs the user’s functional status. 7070. Schmidt MH, Selau CM, Soares PS, Franchi EF, Piber VD, Quatrin LB. Acidente Vascular Cerebral e Diferentes Limitações: Uma Análise Interdisciplinar. Arq Ciênc Saúde UNIPAR. 2019;23(2):139-44. doi: 10.25110/arqsaude.v23i2.2019.6404.
• Carvalho-Pinto et al. conducted a retrospective observational study that collected data from medical records and home visits of post-stroke patients followed in a primary healthcare unit in the city of Belo Horizonte, Brazil, between May 2013 and May 2014. Data included health status, care received following stroke, personal and environmental contextual factors, functioning and disability, organized according to the International Classification of Functioning, Disability and Health conceptual framework. Most participants had good self-perception of manual ability (2.39 [SD, 2.29] logits) and limited walking ability (88%), were capable of improving natural gait speed, had a change in balance (51.43%) and functional mobility (54.16%) with risk of falling, and had a negative self-perception of quality of life (average score of 164.21 [SD, 35.16] points in the SSQOL-Brazil). 7171. Carvalho-Pinto BP, Faria CD. Health, Function and Disability in Stroke Patients in the Community. Braz J Phys Ther. 2016;20(4):355-66. doi: 10.1590/bjpt-rbf.2014.0171.
Cost
• A cost-effectiveness study assessing thrombolytic drugs in Brazil reported that, for a 1-year result, for men, the cost of treatment with rt-PA was higher than that of the conservative treatment. This result is mainly directed by the cost of the medication. Part of this additional cost is compensated by the lower cost of rehabilitation and less productivity losses as early as the first 2 years, because the patients treated with rt-PA presented fewer sequelae than those who received conservative treatment. After the second post-stroke year, for both sexes, treatment with rt-PA (alteplase), considering direct and indirect costs, started to have a lower cost when compared to conservative treatment. From this time horizon onward, the additional cost of the medication starts to be more than compensated by the smaller productivity losses and lower social security and patient rehabilitation costs. 7272. Araújo DV, Teich V, Passos RB, Martins SC. Analysis of the Cost-Effectiveness of Thrombolysis With Alteplase in Stroke. Arq Bras Cardiol. 2010;95(1):12-20. doi: 10.1590/s0066-782x2010005000067.
Genetics/Family History
• Mitochondrial disorders, such as MELAS, may be responsible for up to one third of cryptogenic ISs in young patients. Stroke-like episodes can appear at any age in MELAS and occur in around 50% of the patients with the A3243G mitochondrial DNA mutation. The A3243G mutation has been reported in approximately 80% of the cases of MELAS, and other mitochondrial DNA mutations, such as T3271C, have also been described. In an investigation conducted by Conforto et al. both mutations were assessed in three groups of patients aged less than 46 years (Group 1: 15 patients with cryptogenic strokes; Group 2: 3 patients diagnosed with MELAS syndrome, including stroke-like episodes; Group 3: 20 healthy subjects). The A3243G mutation was absent in all subjects in Groups 1 and 3 but was present in all subjects in Group 2. Thus, these results do not support screening for those mutations to diagnose oligosymptomatic forms of MELAS in cryptogenic strokes in the absence of other features of the syndrome. 7373. Conforto AB, Yamamoto FI, Oba-Shinjo SM, Pinto JG, Hoshino M, Scaff M, Marie SK. Screening for MELAS Mutations in Young Patients With Stroke of Undetermined Origin. Arq Neuropsiquiatr. 2007;65(2B):371-6. doi: 10.1590/s0004-282x2007000300001.
Prevention
• The PURE study examined rates and predictors of use of evidence-based secondary prevention medications (ACEI/ARB, antiplatelets, statins, and beta-blockers) in patients with cardiovascular diseases, including CHD and stroke in South American countries, including Brazil. The study showed that fewer stroke patients received antiplatelets (24.3%), ACEI/ARB (37.6%), and statins (9.8%) as compared with CHD patients (30.1%, 36.0%, and 18.0%, respectively). This underutilization of therapies in stroke patients varied substantially among countries, with the lowest use in Colombia (no prescription of statins). When CHD and stroke patients were combined, the proportion of utilization of antiplatelets was highest in Chile (38.1%) and lowest in Argentina (23.0%). The use of ACEI/ARB and statins was higher in Brazil (46.4% and 26.4%) and lower in Colombia (26.4% and 1.4%), respectively. Among CHD and stroke participants, the use was higher in those with higher education level relative to those with none, primary, or unknown education [35.6% vs. 23.6% for antiplatelets (p = 0.002); 20.6% vs. 10.9% for statins (p = 0.0007)]. Former smokers with CHD or stroke were more likely to receive proven therapies than current smokers or those who had never smoked (35.2% vs. 26.6% and 27.7%, respectively, for antiplatelets [p = 0.039]; 19.9% vs. 10.6% and 13.0% for statins [p = 0.004]). Only 4.1% of the patients received all 4 therapies (antiplatelets, beta-blockers, ACEI/ARB, and statins), with the highest rate in Brazil (5.5%), and the lowest in Colombia (0.5%) (p = 0.02). Moreover, the use of no medication was observed in 30% of Brazilian stroke patients. 7474. Avezum A, Oliveira GBF, Lanas F, Lopez-Jaramillo P, Diaz R, Miranda JJ, Seron P, Camacho-Lopez PA, Orlandini A, Bernabe-Ortiz A, Mattos AC, Islam S, Rangarajan S, Teo K, Yusuf S. Secondary CV Prevention in South America in a Community Setting: The PURE Study. Glob Heart. 2017;12(4):305-13. doi: 10.1016/j.gheart.2016.06.001.
• The IMPACT-AF, a clustered randomized trial to IMProve treatment with AntiCoagulanTs in patients with Atrial Fibrillation, a leading cause of stroke, conducted in Argentina, Brazil, China, India, and Romania, showed that, overall, two-thirds of patients were on oral anticoagulation at baseline, 83% were on a VKA, and 15% were on NOACs. Patients from Brazil were most often on oral anticoagulation at baseline (91%), whereas only 38% of patients from China were on anticoagulation at baseline. Of all patients taking VKAs in Brazil, 40.3% had INR values between 2 and 3 prior to the baseline visit. 7575. Vinereanu D, Al-Khalidi HR, Rao MP, He W, Lopes RD, Bahit CM, Ciobanu AO, Fox KA, Pokorney SD, Xian Y, Jiang J, Kamath DY, Berwanger O, Tajer C, Huo Y, Xavier D, Granger CB. Regional Differences in Presentation and Antithrombotic Treatment of Patients With Atrial Fibrillation: Baseline Characteristics From a Clustered Randomized Trial to IMProve Treatment With AntiCoagulanTs in Patients With Atrial Fibrillation (IMPACT-AF). Am Heart J. 2017;192:38-47. doi: 10.1016/j.ahj.2017.07.004.
Awareness, treatment, control
• Several studies have shown alarming lack of knowledge about stroke risk factors, stroke treatment, and recognition of stroke symptoms as a medical emergency. In a community-based study, Pontes-Neto et al. interviewed subjects in public places of four major cities in Brazil between July 2004 and December 2005, using a structured, open-ended questionnaire in Portuguese, based on a case presentation of a typical patient with acute stroke at home. The authors found 28 different Portuguese terms to name stroke. Twenty-two percent of the interviewees did not recognize any warning signs of stroke. Only 34.6% of the interviewees answered the correct nationwide emergency telephone number in Brazil (#192). Only 51.4% of the interviewees reported they would call an ambulance for a relative with symptoms of stroke. 7676. Pontes-Neto OM, Silva GS, Feitosa MR, Figueiredo NL, Fiorot JA Jr, Rocha TN, Massaro AR, Leite JP. Stroke Awareness in Brazil: Alarming Results in a Community-Based Study. Stroke. 2008;39(2):292-6. doi: 10.1161/STROKEAHA.107.493908.
• Falavigna A et al. used a closed-ended, self-administered questionnaire to assess the knowledge about stroke among 952 residents of the city of Caxias do Sul, Brazil. Lower income and lower educational level were independent predictors of inability to recognize that stroke affects the brain. Lower income and age < 50 years were independent predictors of lack of knowledge about stroke risk factors. 7777. Falavigna A, Teles AR, Vedana VM, Kleber FD, Mosena G, Velho MC, Mazzocchin T, Silva RC, Lucena LF, Santin JT, Roth F. Awareness of Stroke Risk Factors and Warning Signs in Southern Brazil. Arq Neuropsiquiatr. 2009;67(4):1076-81. doi: 10.1590/s0004-282x2009000600022.
• In a community-based and cross-sectional study, Pitton Rissardo et al. applied a stroke knowledge survey to a convenience sample of 633 passers-by of a public square from December 2015 to October 2016, in the city of Santa Maria, state of Rio Grande do Sul. Of the respondents, 33% correctly reported the meaning of the acronym “AVC” (in Portuguese, acidente vascular cerebral ), the most recommended term to name stroke in Portuguese by the Brazilian Society of Cerebrovascular Diseases. Around 30% of subjects incorrectly localized stroke in the heart. Only 50% of the respondents correctly reported a warning sign of stroke. Individuals with a higher level of education were more likely to call an ambulance for a relative with stroke symptoms. 7878. Rissardo JP, Caprara ALF, Prado ALC. Stroke Literacy in a South Brazilian City: A Community Based Survey. J Stroke Cerebrovasc Dis. 2018;27(9):2513-8. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.006.
• In recent years, there have been several initiatives to improve public stroke awareness in Brazil, mainly around the World Stroke Day (October 29th) annual campaigns led by the World Stroke Organization. Despite these efforts, only 30–40% of patients with stroke are hospitalized within 4 hours of symptom onset. 7979. Martins SCO, Sacks C, Hacke W, Brainin M, Figueiredo FA, Marques Pontes-Neto O, Germain PML, Marinho MF, Wiegering AH, McGhie DV, Cruz-Flores S, Ameriso SF, Villareal WMC, Durán JC, Passos JEF, Nogueira RG, Carvalho JJF, Silva GS, Moro CHC, Oliveira-Filho J, Gagliardi R, Sousa EDG, Soares FF, Campos KP, Teixeira PFP, Gonçalves IP, Carquin IRS, Collazos MM, Romero GEP, Figueredo JIM, Barboza MA, López MÁC, Góngora-Rivera F, Cantú-Brito C, Novarro-Escudero N, Velázquez Blanco MÁ, Morvil CAAR, Bareiro ABO, Rojas GM, Flores A, Hancco-Saavedra JA, Pérez Jimenez V, Argomedo CA, Kadota LR, Crosa R, Cuervo DLM, Souza AC, Carbonera LA, Guzmán TFÁ, Maldonado N, Cabral NL, Anderson C, Lindsay P, Hennis A, Feigin VL. Priorities to Reduce the Burden of Stroke in Latin American Countries. Lancet Neurol. 2019;18(7):674-83. doi: 10.1016/S1474-4422(19)30068-7.
Future Research
• The Brazilian research portfolio in vascular neurology has evolved largely in recent years, as illustrated by the foundation of the Brazilian Stroke Research Network. Still, there are several opportunities for improvement. The most expressive community studies on stroke prevalence and incidence derive mostly from two cities. While both examples represent a major achievement in stroke epidemiology, there is still a need for a broader assessment comprising a representation of all geographical regions, diverse cultures, income levels, and ethnicities.
• Additionally, there are inherent constrains related to studies relying on stroke identification using ICD codes. It is not uncommon for users to apply a broader code on admission, that might not be adjusted during hospital stay, thus not representing the actual stroke subtype (e.g., an IS might be coded as non-specified stroke or even as TIA). With the dawn of the big data technologies (e.g., text mining), additional clinical information from admission or discharge records could provide a reliable cross-reference source, thus confirming or correcting a given code.
3. ACUTE AND CHRONIC CORONARY HEART DISEASE
ICD-9-CM 410 to 414; ICD-10 I10 to I25
See Tables 3-1 through 3-3 and Charts 3-1 through 3-20
Abbreviations Used in Chapter 3
| ACCEPT/SBC | Brazilian Registry of Clinical Practice in Acute Coronary Syndromes of the Brazilian Society of Cardiology |
| ACS | Acute Coronary Syndrome |
| AMI | Acute Myocardial Infarction |
| ASA | Acetylsalicylic Acid |
| BRACE | Brazilian Registry in Acute Coronary Syndromes |
| BRIDGE-ACS | Brazilian Intervention to Increase Evidence Usage in Acute Coronary Syndromes |
| BYPASS | Brazilian Registry of Adult Patients Undergoing Cardiovascular Surgery |
| CABG | Coronary Artery Bypass Grafting |
| CCS | Chronic Coronary Syndrome |
| CENIC | Brazilian Nationwide PCI Registry (in Portuguese, Central Nacional de Intervenções Cardiovasculares ) |
| CHD | Coronary Heart Disease |
| CI | Confidence Interval |
| CVD | Cardiovascular Diseases |
| DALYs | Disability-Adjusted Life Years |
| DATASUS | Brazilian Unified Health System Database |
| ERICO | Strategy of Registry of Acute Coronary Syndrome (in Portuguese, Estudo de Registro de Insuficiência Coronariana ) |
| GBD | Global Burden of Disease |
| IHD | Ischemic Heart Disease |
| MASS | Medicine, Angioplasty, or Surgery Study |
| OR | Odds Ratio |
| PCI | Percutaneous Coronary Intervention |
| PNS | National Health Survey (in Portuguese, Pesquisa Nacional de Saúde ) |
| RBSCA | Brazilian Registry of Acute Coronary Syndrome (in Portuguese, Registro Brasileiro de Síndrome Coronariana Aguda ) |
| REPLICCAR-I | São Paulo's Cardiovascular Surgery Registry (in Portuguese, Registro Paulista de Cirurgia Cardiovascular ) |
| RESISST | STEMI Registry from Salvador (in Portuguese, Registro Soteropolitano de Infarto Agudo do Miocárdio com Supra de ST ) |
| SDI | Sociodemographic Index |
| SIH | Brazilian Hospital Information System (in Portuguese, Sistema de Informações Hospitalares ) |
| STEMI | ST-Elevation Myocardial Infarction |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| UI | Uncertainty Interval |
| VICTIM | Via Crucis for the Treatment of Myocardial Infarction |
| YLDs | Years Lived with Disability |
| YLLs | Years of Life Lost |
– Number of cases, age-standardized prevalence rates (per 100 000) of ischemic heart disease in 1990 and 2019, and percent change of rates in the period, in Brazil and its Federative Units.
– Number of deaths, age-standardized mortality rate (per 100 000) due to ischemic heart disease in 1990 and 2019, and percent change of rates in the period, in Brazil and its Federative Units.
– Number of DALYs, age-standardized DALY rates (per 100 000) due to ischemic heart disease in 1990 and 2019, and percent change of rates in the period, in Brazil and its Federative Units.
– Crude and age-standardized prevalence rates (per 100 000) of ischemic heart disease in Brazil, 1990-2019. Shaded areas show 95% uncertainty intervals.
– Prevalence rate (per 100 000) of ischemic heart disease according to sex and age in Brazil, 2019. Error bars show 95% uncertainty intervals.
– Incidence rate (per 100 000) of ischemic heart disease according to sex and age. Brazil, 2019. Error bars show 95% uncertainty intervals.
– Mortality rate (per 100 000) due to ischemic heart disease according to sex and age in Brazil, 2019. Error bars show 95% uncertainty intervals.
– Crude and age-standardized mortality rates (per 100 000) due to ischemic heart disease in Brazil, 1990-2019. Shaded areas show 95% uncertainty intervals.
– Age-standardized mortality rate (per 100 000) from ischemic heart disease by Brazilian regions, 1990-2019.
– Correlation between the percent change in age-standardized mortality rates due to ischemic heart disease from 1990 to 2019 and the 2019 Sociodemographic Index (SDI).
– In-hospital mortality rate due to acute coronary syndrome (ACS), acute myocardial infarction (AMI), percutaneous coronary intervention (PCI), and coronary artery bypass graft (CABG) surgery in the public health system of Brazil, 2008-2019.
– Correlation between the in-hospital mortality rate due to acute coronary syndrome (ACS) in the public health system in 2019 and the 2019 Sociodemographic Index (SDI).
– Correlation between the in-hospital mortality rate due to acute myocardial infarction (AMI) in the public health system in Brazil in 2019 and the 2019 Sociodemographic Index (SDI).
– Crude and age-standardized DALY rates (per 100 000) due to ischemic heart disease in Brazil, 1990-2019. Shaded areas show 95% uncertainty intervals.
– Age-standardized DALY rates (per 100 000) due to ischemic heart disease by Brazilian regions, 1990-2019.
– Correlation between the percent change of age-standardized DALY rates due to ischemic heart disease from 1990 to 2019 and the 2019 Sociodemographic Index (SDI).
– Number of hospital admissions for acute coronary syndrome (ACS), acute myocardial infarction (AMI), and chronic coronary syndrome (CCS) to the public health system in Brazil, 2008-2019.
– Number of hospital admissions for primary percutaneous coronary intervention (PCI), non-primary PCI, and coronary artery bypass graft (CABG) surgery to the public health system in Brazil, 2008-2019.
– Percentage of percutaneous coronary intervention (PCI) and coronary artery bypass graft surgery (CABG) out of myocardial revascularization procedures in the Brazilian public health system, 2008-2019.
– Total amount in international dollars (Int$ 2019) reimbursed for hospital admissions due to acute coronary syndrome (ACS), acute myocardial infarction (AMI), and chronic coronary syndrome (CCS) to the public health system in Brazil, 2008-2019.
– Average amount in international dollars (Int$ 2019) reimbursed per hospital admission due to acute coronary syndrome (ACS), acute myocardial infarction (AMI), and chronic coronary syndrome (CCS) to the public health system in Brazil, 2008-2019.
– Total amount in international dollars (Int$ 2019) reimbursed for hospital admissions due to primary percutaneous coronary intervention (PCI), non-primary PCI, and coronary artery bypass graft (CABG) surgery to the public health system in Brazil, 2008-2019.
– Average amount in international dollars (Int$ 2019) reimbursed per hospital admission due to primary percutaneous coronary intervention (PCI), non-primary PCI, and coronary artery bypass graft (CABG) surgery to the public health system in Brazil, 2008-2019.
Overview and Prevalence
• Ischemic heart disease, also known as CHD, comprises a spectrum of symptomatic and asymptomatic clinical conditions typically related to a reduction in blood flow to the heart muscle. The most common cause is atherosclerotic disease in the coronary arteries, a chronic condition with varied presentations, progressing from a long asymptomatic phase to stable angina, AMI, and unstable angina. Ischemic heart disease is a common cause of heart failure, with reduced or preserved left ventricular ejection fraction, ventricular arrhythmias, and sudden cardiac arrest.
• Ischemic heart disease was the leading cause of death in Brazil in the last decade, for men and women. Because of its wide range of clinical presentations, the reported IHD prevalence, incidence, and mortality vary widely, depending on the population and healthcare setting studied.
Ischemic Heart Disease
• According to data from the GBD study, the number of individuals living with IHD, defined as those with previous AMI, stable angina, or ischemic heart failure, in Brazil increased from 1.48 million in 1990 to more than 4 million in 2019 (Table 3-1), and the crude IHD prevalence increased from 0.99% to 1.85% in the period (Chart 3-1). These rates sharply increased with aging: 0.4%, 4.4%, and 14.0% among individuals aged 15-49 years, 50-69 years, and 70 years or older, respectively, in 2019. In all age strata, IHD was more frequent in males than in females (Chart 3-2). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The continuous increase in the number of IHD cases can be explained by the population growth and aging, because the age-standardized prevalence rate remained stable from 1990 to 2019 (percent change: -1%, Table 3-1 and Chart 3-1). In 2019, the age-standardized IHD prevalence was 1709 (95% UI, 1466-1994) per 100 000 inhabitants in the total population (Table 3-1), 1046 (95% UI, 905-1209) per 100 000 females and 2534 (95% UI, 2170-2975) per 100 000 males. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In general, there was a difference in the age-standardized IHD prevalence among the Brazilian regions in 2019, with the highest prevalence rates observed in the Southeastern and Southern regions (state of Minas Gerais: 1878 per 100 000 inhabitants; states of Paraná and Santa Catarina: ~1750 per 100 000), and the lowest prevalence rates in the Northern region (state of Amapá: 1496 per 100 000, Table 3-1). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The self-reported prevalence of IHD was 2.7% in the baseline assessment of the ELSA-Brasil cohort in 2008-2010. This cohort was composed of more than 15 000 civil servants aged 35-74 years from six cities (Salvador, Vitória, Belo Horizonte, Rio de Janeiro, São Paulo, and Porto Alegre). The prevalence was higher in males and individuals in the lower socioeconomic level. 8080. Birck MG, Goulart AC, Lotufo PA, Benseñor IM. Secondary Prevention of Coronary Heart Disease: A Cross-Sectional Analysis on the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Sao Paulo Med J. 2019;137(3):223-33. doi: 10.1590/1516-3180.2018.0531140319.
Myocardial Infarction
• The reported prevalence of AMI was 4.0% in the May Measurement Month 2017 cross-sectional survey of 7260 individuals from different ethnicities and regions of Brazil. Participants (56% women; mean age, 51.6±16.1 years) were mainly recruited from hospitals and indexed clinics. 8181. Barbosa E, Eibel B, Brandão AA, Feitosa ADM, Miranda RD, Kobeissi E, Beaney T, Poulter NR, Mota-Gomes MA, Barroso WKS. May Measurement Month 2017: Brazilian Results-Americas. Eur Heart J Suppl. 2019;21(Suppl D):25-7. doi: 10.1093/eurheartj/suz079.
Types of Acute Coronary Syndrome
• The large prospective ACCEPT registry, planned by the Brazilian Society of Cardiology, enrolled 4782 patients with ACS in 53 institutions (public hospitals, health maintenance organizations, and private services) from the five Brazilian regions. The sites were mostly tertiary, with high availability of PCI and cardiac surgery. Participants were included between 2010 and 2014. The percentages of patients with unstable angina, non-STEMI, and STEMI were 30%, 34%, and 36%, respectively. 8282. Silva PGMBE, Berwanger O, Santos ESD, Sousa ACS, Cavalcante MA, Andrade PB, Neuenschwander FC, Vargas Filho H, Guimarães JI, Andrade J, Paola AAV, Malachias MVB, Mattos LAPE, Precoma DB, Bacal F, Dutra OP. One Year Follow-up Assessment of Patients Included in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2020;114(6):995-1003. doi: 10.36660/abc.20190879.
• The BRACE study, a cross-sectional, epidemiological registry of ACS patients, used a stratified “cluster sampling” methodology to select services that were representative of all hospitals with intensive care or cardiology unit in Brazil. Among 1150 patients from 72 hospitals included in the study from 2007 to 2009, 54% had STEMI. Among the remaining patients with non-ST elevation ACS, 67% had non-STEMI, while 33% had unstable angina. 8383. Franken M, Giugliano RP, Goodman SG, Baracioli LM, Godoy LC, Furtado RHM, Lima FG, Nicolau JC. Performance of Acute Coronary Syndrome Approaches in Brazil: A Report From the BRACE (Brazilian Registry in Acute Coronary SyndromEs). Eur Heart J Qual Care Clin Outcomes. 2020;6(4):284-92. doi: 10.1093/ehjqcco/qcz045. , 8484. Nicolau JC, Franken M, Lotufo PA, Carvalho AC, Marin Neto JA, Lima FG, Dutra O, Knobel E, de Oliveira CC, Timerman S, Stefanini E. Use of Demonstrably Effective Therapies in the Treatment of Acute Coronary Syndromes: Comparison Between Different Brazilian Regions. Analysis of the Brazilian Registry on Acute Coronary Syndromes (BRACE). Arq Bras Cardiol. 2012 Apr;98(4):282-9. doi: 10.1590/s0066-782x2012000400001.
• In the ERICO study, a prospective cohort of patients admitted with ACS in a university hospital in the city of São Paulo, among 964 participants recruited from 2009 to 2012, the initial diagnosis was unstable angina in 33%, non-STEMI in 39%, and STEMI in 28% of the cases. 8585. Santos IS, Goulart AC, Brandão RM, Santos RC, Bittencourt MS, Sitnik D, Pereira AC, Pastore CA, Samesima N, Lotufo PA, Bensenor IM. One-year Mortality after an Acute Coronary Event and its Clinical Predictors: The ERICO Study. Arq Bras Cardiol. 2015;105(1):53-64. doi: 10.5935/abc.20150044.
• The BRIDGE-ACS trial was a cluster-randomized study involving 1150 patients with ACS recruited from general public hospitals in Brazilian major urban areas in 2011. The rates of diagnosis of unstable angina, non-STEMI, and STEMI were 24%, 36%, and 40%, respectively. 8686. Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, Santucci EV, Victor E, Tenuta M, Carvalho V, Mira VL, Pieper KS, Weber B, Mota LH, Peterson ED, Lopes RD; Bridge-Acs Investigators. Effect of a Multifaceted Intervention on Use of Evidence-Based Therapies in Patients With Acute Coronary Syndromes in Brazil: The BRIDGE-ACS Randomized Trial. JAMA. 2012;307(19):2041-9. doi: 10.1001/jama.2012.413.
Stable Angina
• Regional population surveys conducted in 2007, applying the Angina Rose questionnaire, reported a prevalence of angina of 12.3% among adults aged ≥30 years in the city of Ribeirão Preto, and of 8.2% among individuals aged ≥40 years in the city of Pelotas. 8787. Moraes SA, Freitas IC. Doença Isquêmica do Coração e Fatores Associados em Adultos de Ribeirão Preto, SP. Rev Saude Publica. 2012;46(4):591-601. doi: 10.1590/s0034-89102012005000056.
https://doi.org/10.1590/s0034-8910201200...
, 8888. Alves L, Cesar JA, Horta BL. Prevalence of Angina Pectoris in Pelotas, South of Brazil. Arq Bras Cardiol. 2010;95(2):179-85. doi: 10.1590/s0066-782x2010005000075.
• According to the 2013 PNS, an epidemiological home-based survey, country-wide representative, the overall prevalence rates of class I and class II angina were 7.6% (95% CI, 7.2%-8.0%) and 4.2% (95% CI, 3.9%-4.5%), respectively. 8989. Lotufo PA, Malta DC, Szwarcwald CL, Stopa SR, Vieira ML, Bensenor IM. Prevalence of Angina Pectoris in the Brazilian Population From the Rose Questionnaire: Analysis of the National Health Survey, 2013. Rev Bras Epidemiol. 2015;18(Suppl 2):123-31. doi: 10.1590/1980-5497201500060011.
• Self-reported angina pectoris was more prevalent in females than in males in all studies described.
• It is important to note the higher prevalence rates observed in prospective surveys as compared to national statistics. Self-reported assessments of angina are very sensitive but not specific to CHD, because they require neither confirmatory exams nor health reports. In addition, national statistics might underrepresent the true epidemiology of CHD, considering its asymptomatic nature.
Incidence
• The GBD study estimated an incidence of 260 661 (95% UI, 230 100 - 293 617) IHD events (mainly myocardial infarction) in Brazil in 2019. As expected, the incidence rate was strongly associated with aging: 29 (95% UI, 23-36), 323 (95% UI, 268-386), and 737 (95% UI, 625-868) per 100 000 individuals aged 15-49 years, 50-69 years, and 70 years or older, respectively. In all age groups, IHD was more incident in males than in females (Chart 3-3). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In 2019, the age-standardized incidence rate was 110 (95% UI, 97-124) per 100 000 inhabitants in the whole population, 78 (95% UI, 69-88) per 100 000 females, and 148 (95% UI, 130-166) per 100 000 males. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• While the crude IHD incidence rate continuously increased from 1990 to 2019, the age-standardized rate slightly decreased (-15%) from 1990 to 2000, remaining stable thereafter (percent change from 2000 to 2019: 3%). From 1990 to 2019, the percent change in the age-adjusted incidence rate of IHD was -12% (95% UI, -15% to -10%) in the total population, and 7% (95% UI, 1% to 12%), 2% (95% UI, -1% to 6%), and -19% (95% UI, -22% to -16%) among individuals aged 15-49 years, 50-69 years, and 70 years or older, respectively. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In a systematic review from public health data in 2012, the incidence rates of AMI and ACS per 100 000 inhabitants were 29.8 and 38, respectively. 88. Ribeiro ALP, Duncan BB, Brant LCC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular Health in Brazil: Trends and Perspectives. Circulation. 2016;133(4): 422-33. doi: https://doi.org/10.1161/CIRCULATIONAHA.114.008727 .
https://doi.org/10.1161/CIRCULATIONAHA.1...
Mortality
• According to the GBD estimates, there were 171 246 deaths due to IHD in Brazil in 2019 (Table 3-2), corresponding to 12% (11%-13%) of total deaths in the country and 43% of all CVD deaths. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The crude mortality rate attributed to IHD was 79 (95% UI, 72-83) per 100 000 inhabitants in 2019. The rates increased with aging: 11 (95% UI, 11-12), 149 (95% UI, 142-156), and 751 (95% UI, 651-807) per 100 000 individuals aged 15-49 years, 50-69 years, and 70 years or older, respectively. In all age groups, the mortality rate was higher in males than in females (Chart 3-4). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In 2019, the age-standardized mortality rate due to IHD was 75 (95% UI, 68-79) per 100 000 inhabitants in the total population (Table 3-2), 58 (95% UI, 51-63) per 100 000 females and 96 (95% UI, 88-101) per 100 000 males. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In 2019, IHD ranked as the number one cause of death in Brazil in all but two Federative Units (states of Amazonas and Amapá, where IHD was the second most frequent cause of death). In addition, IHD was the main cause of death in both females and males over 50 years of age, and the third cause of fatalities among men aged 15-49 years (after interpersonal violence and road injuries). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• According to the GBD study, the unadjusted mortality rate due to IHD mildly increased from ~2005 to 2019, while the age-standardized rate continuously decreased from 1990 to 2019 (cumulative percent change: -53%, Table 3-2 and Chart 3-5). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The decrease in the mortality rate from 1990 to 2019 was less pronounced in individuals aged 15-49 years (-34.9%, 95% UI, -38.5% to -31,1%) as compared to those aged 50-69 years (-47.8%, 95% UI, -50.6% to -45,0%) or 70 years or older (-46.5%, 95% UI, -50.1% to -43,7%). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Regional differences in age-adjusted mortality rates and trends over time were noted. In 1990, rates were higher in the Southern and Southeastern regions, and lower in the Northern and Northeastern states. From 1990 to 2019, a reduction in mortality rates was observed in all states (less impressive in the Northeastern) and the heterogeneity among regions was progressively attenuated (Chart 3-6). The mildest variations occurred in the states of Ceará (-17%) and Maranhão (-21%), whereas the most pronounced decreases were detected in the Distrito Federal (-65%) and the states of Minas Gerais (-63%) and São Paulo (-62%, Table 3-2). A negative correlation was observed between the change in age-standardized mortality rate from IHD in the period and the 2019 SDI ( r 20.61, p-value < 0.01, Chart 3-7). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
, 9090. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. Seattle: Institute for Health Metrics and Evaluation; 2020. In 2019, the lowest death rates were observed in the states of Amazonas (56 per 100 000) and Minas Gerais (59 per 100 000), whereas the highest rates were noted in the states of Maranhão (104 per 100 000) and Pernambuco (102 per 100 000, Table 3-2). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In a temporal analysis of data from the Brazilian Ministry of Health, the coefficient of death related to IHD remained stable for women in the Northern and West-Central regions between 1981 and 2001, whereas it decreased in the Southern and Southeastern regions, and increased in the Northeastern. For males, there was a trend towards a decrease in events in the Southern and Southeastern regions. 9191. Souza MF, Alencar AP, Malta DC, Moura L, Mansur AP. Serial Temporal Analysis of Ischemic Heart Disease and Stroke Death Risk in Five Regions of Brazil From 1981 to 2001. Arq Bras Cardiol. 2006;87(6):735-40. doi: 10.1590/s0066-782x2006001900009.
• An analysis conducted in the DATASUS from 1990 to 2009 demonstrated a reduction in the age-adjusted mortality rate due to IHD in Brazil. The rate reduced from 195 to 149 per 100 000 males (variation: -23.4%) and from 120 to 84 per 100 000 females (variation: -29.5%). 9292. Mansur AP, Favarato D. Mortality Due to Cardiovascular Diseases in Brazil and in the Metropolitan Region of São Paulo: A 2011 Update. Arq Bras Cardiol. 2012;99(2):755-61. doi: 10.1590/s0066-782x2012005000061.
• The proportion of deaths caused by CVD has remained stable over the last decades, with reports ranging from 26% to 32%, according to the year. An ecologic study in the city of Porto Alegre, including individuals aged 45-64 years, demonstrated that CVD was responsible for 28.5% of all deaths in 2009. Of those, 40% were related to IHD, whose proportion was higher among those with a lower socioeconomic status (42.7%) than those with a higher socioeconomic status (26.3%). 9393. Bassanesi SL, Azambuja MI, Achutti A. Premature Mortality Due to Cardiovascular Disease and Social Inequalities in Porto Alegre: From Evidence to Action. Arq Bras Cardiol. 2008;90(6):370-9. doi: 10.1590/s0066-782x2008000600004.
• In a national ecologic study including individuals aged 35-64 years, the rate of death related to IHD was 84 ± 30 per 100 000 inhabitants from 1999 to 2001. The incidence of events was directly related to the poverty rate and lower educational attainment. Importantly, there was wide variability in the results across the 98 participating cities, probably due to data quality. 9494. Ishitani LH, Franco GC, Perpétuo IH, França E. Desigualdade Social e Mortalidade Precoce por Doenças Cardiovasculares no Brasil. Rev Saude Publica. 2006;40(4):684-91. doi: 10.1590/s0034-89102006000500019.
Mortality Related to Acute Coronary Syndromes
• According to the SIH/SUS, the in-hospital mortality rate among patients treated for ACS in the public service setting remained stable from 2008 to 2019 [2.2% (1404 deaths out of 63 913 admissions) and 2.1% (1449 out of 70 013), respectively] (Chart 3-8). There was a modest negative correlation between the in-hospital mortality rate during treatment for ACS in 2019 and the SDI ( r 20.27, p-value = 0.01), with higher rates detected in the Northeastern and Northern states (Chart 3-9). 9090. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. Seattle: Institute for Health Metrics and Evaluation; 2020. , 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• Among individuals admitted with AMI, the in-hospital mortality rate decreased from 15.9% (7627 deaths in 48 114 admissions) in 2008 to 12.9% (10 445 deaths in 80 944 admissions) in 2019, a percent change of -19% (Chart 3-8). A mild negative correlation between the in-hospital mortality rate during hospitalization for AMI in 2019 and the SDI was observed ( r 20.18, p-value = 0.03, Chart 3-10). 9090. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. Seattle: Institute for Health Metrics and Evaluation; 2020. , 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• Several Brazilian ACS registries reported the outcomes of individuals admitted with ACS. In general, the mortality rate in registries is lower than that reported in the SIH/SUS. Several studies highlighted regional differences in treatment practices and mortality, as well as poorer outcomes in patients treated in public services as compared to those admitted to private hospitals. 8282. Silva PGMBE, Berwanger O, Santos ESD, Sousa ACS, Cavalcante MA, Andrade PB, Neuenschwander FC, Vargas Filho H, Guimarães JI, Andrade J, Paola AAV, Malachias MVB, Mattos LAPE, Precoma DB, Bacal F, Dutra OP. One Year Follow-up Assessment of Patients Included in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2020;114(6):995-1003. doi: 10.36660/abc.20190879.
• In the ACCEPT registry, among 2485 ACS patients recruited from 47 Brazilian hospitals in 2010/2011, the all-cause mortality at 30 days was 1.8% for unstable angina, 3.0% for non-STEMI, and 3.4% for STEMI. 9797. Mattos LAP, Berwanger O, Santos ES, Reis HJ, Romano ER, Petriz JL, Sousa AC, Neuenschwander FC, Guimarães JI, Andrade JP. Clinical Outcomes at 30 days in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2013;100(1):6-13. doi: 10.1590/s0066-782x2013000100003.
• In a subsequent report from the ACCEPT registry analyzing a total of 4782 patients recruited up to 2014, the rate of major cardiovascular events was 13.6% after 1 year of follow-up. Events occurred more frequently among patients from the SUS (16.6 per 100 patients/year), as compared to private patients or those with health insurance (9.1 per 100 patients/year). In addition, a regional discrepancy in the rate of death at 1 year was noted, with higher numbers in the Northern region (19.8%; 95% CI, 12.6%-27.0%) and lower rates in the Northeastern region (5.6%; 95% CI, 3.7%-7.5%). 8282. Silva PGMBE, Berwanger O, Santos ESD, Sousa ACS, Cavalcante MA, Andrade PB, Neuenschwander FC, Vargas Filho H, Guimarães JI, Andrade J, Paola AAV, Malachias MVB, Mattos LAPE, Precoma DB, Bacal F, Dutra OP. One Year Follow-up Assessment of Patients Included in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2020;114(6):995-1003. doi: 10.36660/abc.20190879.
• In the BRACE cross-sectional registry, the overall in-hospital mortality was 5.2% among 1150 ACS patients recruited from 2007 to 2009 in 72 hospitals representative of all national services with intensive care or cardiology unit. 8383. Franken M, Giugliano RP, Goodman SG, Baracioli LM, Godoy LC, Furtado RHM, Lima FG, Nicolau JC. Performance of Acute Coronary Syndrome Approaches in Brazil: A Report From the BRACE (Brazilian Registry in Acute Coronary SyndromEs). Eur Heart J Qual Care Clin Outcomes. 2020;6(4):284-92. doi: 10.1093/ehjqcco/qcz045. , 8484. Nicolau JC, Franken M, Lotufo PA, Carvalho AC, Marin Neto JA, Lima FG, Dutra O, Knobel E, de Oliveira CC, Timerman S, Stefanini E. Use of Demonstrably Effective Therapies in the Treatment of Acute Coronary Syndromes: Comparison Between Different Brazilian Regions. Analysis of the Brazilian Registry on Acute Coronary Syndromes (BRACE). Arq Bras Cardiol. 2012 Apr;98(4):282-9. doi: 10.1590/s0066-782x2012000400001.
• The RBSCA registry enrolled 2693 patients between 2003 and 2008, including 45% of AMI cases. The in-hospital mortality rate was 3.1% for those with unstable angina and 7.7% for those with AMI, leading to an overall rate of 5.5%. 9898. Piegas LS, Avezum A, Guimarães HP, Muniz AJ, Reis HJ, Santos ES, Knobel M, Souza Rd. Acute Coronary Syndrome Behavior: Results of a Brazilian Registry. Arq Bras Cardiol. 2013;100(6):502-10. doi: 10.5935/abc.20130101.
• In a retrospective, multicenter study of 3745 patients admitted for ACS between 2010 and 2015, the in-hospital all-cause mortality was 3.3%, and 454 (12.2%) patients experienced at least one major adverse event (reinfarction, shock, bleeding, stroke, or death). 9999. Soeiro AM, Silva PGMBE, Roque EAC, Bossa AS, Biselli B, Leal TCAT, Soeiro MCFA, Pitta FG, Serrano CV Jr, Oliveira MT Jr. Prognostic Differences Between Men and Women With Acute Coronary Syndrome. Data From a Brazilian Registry. Arq Bras Cardiol. 2018;111(5):648-53. doi: 10.5935/abc.20180166.
• In the ERICO study, the mortality rate was 4.4% at 30 days and 12% at 1 year among 964 patients admitted with ACS from 2009 to 2012. 8585. Santos IS, Goulart AC, Brandão RM, Santos RC, Bittencourt MS, Sitnik D, Pereira AC, Pastore CA, Samesima N, Lotufo PA, Bensenor IM. One-year Mortality after an Acute Coronary Event and its Clinical Predictors: The ERICO Study. Arq Bras Cardiol. 2015;105(1):53-64. doi: 10.5935/abc.20150044.
• In an observational longitudinal study undertaken from 2011 to 2014 in a high-complexity hospital in the city of Belo Horizonte, the in-hospital mortality was 9.1% among 788 patients with STEMI and 7.6% among 341 patients with non-STEMI. 100100. Lana MLL, Beaton AZ, Brant LCC, Bozzi ICRS, Magalhães O, Castro LRA, Silva FCT Jr, Silva JLP, Ribeiro ALP, Nascimento BR. Factors Associated With Compliance to AHA/ACC Performance Measures in a Myocardial Infarction System of Care in Brazil. Int J Qual Health Care. 2017;29(4):499-506. doi: 10.1093/intqhc/mzx059.
• In a study from the Minas Telecardio 2 Project, conducted in 2013 and 2014 in six emergency units in the city of Montes Claros, among 593 patients with ACS, the in-hospital mortality was 9.4%, ranging from 4.9% for unstable angina to 17% for STEMI cases. 101101. Marino BC, Marcolino MS, Reis RS Jr, França AL, Passos PF, Lemos TR, Antunes IO, Ferreira CG, Antunes AP, Ribeiro ALP. Epidemiological Profile and Quality Indicators in Patients With Acute Coronary Syndrome in Northern Minas Gerais - Minas Telecardio 2 Project. Arq Bras Cardiol. 2016;107(2):106-15. doi: 10.5935/abc.20160095.
• In the RESISST registry, 520 STEMI patients were admitted to public healthcare units interconnected through a Regional Integrated Care Network, from January 2011 to June 2013. Only 41% of the patients underwent reperfusion therapy, and the 30-day mortality rate was 15.3%. 102102. Filgueiras Filho NM, Feitosa Filho GS, Solla DJF, Argôlo FC, Guimarães PO, Paiva Filho IM, Carvalho LGM, Teixeira LS, Rios MNO, Câmara SF, Novais VO, Barbosa LS, Ballalai CS, De Lúcia CV, Granger CB, Newby LK, Lopes RD. Implementation of a Regional Network for ST-Segment-Elevation Myocardial Infarction (STEMI) Care and 30-Day Mortality in a Low- to Middle-Income City in Brazil: Findings From Salvador’s STEMI Registry (RESISST). J Am Heart Assoc. 2018;7(14):e008624. doi: 10.1161/JAHA.118.008624.
• In the VICTIM Registry, statewide data from the state of Sergipe collected from 2014 to 2017 identified 707 cases of STEMI with in-hospital mortality of 10.9%. There was a significantly higher mortality rate for those admitted to public hospitals compared to those admitted to private services (11.9% versus 5.9%, respectively). 9696. Oliveira JC, Almeida-Santos MA, Cunha-Oliveira J, Oliveira LCS, Barreto IDC, Lima TCRM, Arcelino LAM, Prado LFA, Silveira FS, Nascimento TAS, Ferreira EJP, Barreto RV, Moraes EV, Mendonça JT, Sousa ACS, Barreto-Filho JA; VICTIM Register Investigators. Disparities in Access and Mortality of Patients With ST-Segment-Elevation Myocardial Infarction Using the Brazilian Public Healthcare System: VICTIM Register. J Am Heart Assoc. 2019;8(20):e013057. doi: 10.1161/JAHA.119.013057.
• Among 1263 non-STEMI patients admitted to a private hospital in the city of São Paulo from 2014 to 2018, the in-hospital mortality rate was 1.3%. 103103. Guimarães PO, Sampaio MC, Malafaia FL, Lopes RD, Fanaroff AC, Silva PGMB, Santos TM, Okada MY, Mouallem ARE, Diniz MDS, Custódio JV, Garcia JCT, Furlan V. Clinical Outcomes and Need for Intensive Care After Non-ST-Segment-Elevation Myocardial Infarction. Eur J Intern Med. 2020;76:58-63. doi: 10.1016/j.ejim.2020.02.008.
• Among 1852 STEMI patients admitted to municipal emergency rooms in the city of São Paulo from 2010 to 2016 and undergoing a pharmaco-invasive treatment, the in-hospital mortality was 4.0% among patients aged <75 years and 18.2% among those aged ≥75 years. 104104. Helber I, Alves CMR, Grespan SM, Veiga ECA, Moraes PIM, Souza JM, Barbosa AH, Gonçalves I Jr, Fonseca FAH, Carvalho ACC, Caixeta A. The Impact of Advanced Age on Major Cardiovascular Events and Mortality in Patients With ST-Elevation Myocardial Infarction Undergoing a Pharmaco-Invasive Strategy. Clin Interv Aging. 2020;15:715-22. doi: 10.2147/CIA.S218827.
• Mortality rates were reported in a registry of 542 consecutive patients admitted with STEMI and undergoing primary PCI between March 2011 and February 2017 in a tertiary university hospital in the city of Porto Alegre. In-hospital death occurred in 10.7% during the study period and was stable from 2011 to 2016. The 1-year mortality rate was 16.6% with a decreasing trend from 2011 to 2016. 105105. Machado GP, Pivatto F Jr, Wainstein R, Araujo GN, Carpes CK, Lech MC, Valle FH, Bergoli LCC, Gonçalves SC, Wainstein MV. An Overview of Care Change in the Last 6 year in Primary PCI in ST-Elevation Myocardial Infarction in a Tertiary University Brazilian Hospital. Int. J. Cardiovasc. Sci. 2019;32(2):125-33. doi: 10.5935/2359-4802.20180090.
•A 21-year time series study explored trends in AMI-related mortality according to sex, regions of Brazil, and type of city (state capital versus non-capital). Mortality data were retrieved from the Mortality Information System of the Brazilian Ministry of Health and the authors applied procedures to correct mortality rates for ill-defined causes, use of garbage codes, and underreporting. From 1996 to 2016, the age-standardized mortality rate from AMI declined 44% in the country, with substantial regional differences (percent changes: +5% in the North, +11% in the Northeast, -35% in the West-Central, -68% in the Southeast, and -85% in the South). Moreover, temporal changes were more pronounced in females than in males, and in capital cities than in non-capital cities. The corrected age-standardized mortality rate from AMI decreased 49% and 23% in females living in capital cities and in other municipalities, respectively, from 1996 to 2016. Among males, the respective declines were 43% and 17%. Importantly, improvements in the quality of data (e.g., decrease in underreporting) have occurred over the years; this phenomenon is more recent in the Northern and Northeastern regions and in non-capital cities. 106106. Ferreira LCM, Nogueira MC, Carvalho MS, Teixeira MTB. Mortality Due to Acute Myocardial Infarction in Brazil From 1996 to 2016: 21 Years of Disparities in Brazilian Regions. Arq Bras Cardiol. 2020;115(5):849-59. doi: 10.36660/abc.20190438.
https://doi.org/10.36660/abc.20190438...
Mortality Related to Percutaneous Coronary Intervention
• According to the SIH/SUS, the in-hospital mortality rate among patients undergoing any PCI in public hospitals remained fairly stable from 2008 to 2019 [2.4% (1112 deaths out of 46 683 admissions) and 2.7% (2625 out of 96 930), respectively], with a percent change of 14% (Chart 3-8). In 2019, these rates ranged from 2.4% in the Southeastern to 3.5% in the Northeastern region. Among those who underwent primary PCI, the in-hospital mortality was 6.8% (765 fatalities out of 11 270 procedures), ranging from 5.9% in the Northern, Southern, and West-Central regions to 7.3% in the Southeastern region. 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• In a cohort study undertaken from 2009 to 2013 (Brazilian PCI multicenter registry), among 4806 patients undergoing PCI (69% with recent AMI) in eight tertiary referral medical centers, the in-hospital mortality rate was 2.6%. 107107. Lodi-Junqueira L, Silva JL, Ferreira LR, Gonçalves HL, Athayde GR, Gomes TO, Borges JC, Nascimento BR, Lemos PA, Ribeiro ALP. In-Hospital Mortality Risk Prediction After Percutaneous Coronary Interventions: Validating and Updating the Toronto Score in Brazil. Catheter Cardiovasc Interv. 2015;86(6):239-46. doi: 10.1002/ccd.25916.
• In another PCI registry including 1249 consecutive patients in 2009, the total mortality rate was 2.3%, ranging from 0.2% for patients with stable angina to 6.1% for those with STEMI. 108108. Paula LJC, Lemos PA, Medeiros CR, Marin-Neto JA, Figueiredo GL, Polanczyk CA, Wainstein MV, Ribeiro ALP, Lodi-Junqueira L, Oliveira FRA, Sarmento-Leite R, Mattos LA, Cantarelli MJC, Brito FS Jr, Carvalho ACC, Barbosa MR. Construção e validação de um sistema integrado de dados de intervenção coronária percutânea no Brasil (Registro ICP-BR): Perfil clínico dos primeiros 1.249 pacientes incluídos]. Rev Bras Cardiol Inv. 2010;18:256-62.
• In a study that evaluated PCIs in public hospitals from 2005 to 2008, 166 514 procedures were performed in 180 hospitals. The average in-hospital mortality was 2.3%, ranging from 0% to 11.4%. This rate was lower in the Southeastern region (2.0%) and higher in the Northern region (3.6%). The in-hospital mortality rate was 2.3% in high-volume hospitals, accounting for 101 218 (60.8%) PCIs, 2.3% in medium-volume hospitals, and 2.5% in low-volume hospitals. Mortality rate was higher among females and patients older than 65 years. 109109. Piegas LS, Haddad N. Percutaneous Coronary Intervention in Brazil: Results From the Brazilian Public Health System. Arq Bras Cardiol. 2011;96(4):317-24. doi: 10.1590/s0066-782x2011005000035.
• Most reports originate from public institutions, and data from private hospitals are limited. An analysis of 440 procedures performed in a public and another private hospital in the city of Rio de Janeiro between 2013 and 2014 showed low mortality (0.5%), with similar rates in both institutions. 110110. Ferreira RM, Souza E Silva NA, Salis LHA. Complications After Elective Percutaneous Coronary Interventions: A Comparison Between Public and Private Hospitals. Indian Heart J. 2018;70(1):32-6. doi: 10.1016/j.ihj.2017.06.012.
• Differences in in-hospital mortality after PCI according to femoral or radial access were retrospectively analyzed in 158 363 patients enrolled in the CENIC Registry between 2006 and 2016 (52% with stable CHD). Use of radial access progressively increased from 12% in 2006 to 50% in 2016 and was associated with lower in-hospital mortality rate as compared to femoral access in an analysis with propensity score matching (0.4% versus 0.7%; OR, 0.59; 95% CI, 0.47-0.74; p < 0.001; n = 54 242 patients). 111111. Pinton F, Prado G, Bezerra C, Mariani J, Campos C, Caixeta A, Franken M, Lemos PA. TCT-795 Trends in the Prevalence and In-Hospital Outcomes of Radial Versus Femoral Access in Percutaneous Coronary Intervention: A Report With 158,363 Patients From the Brazilian Nationwide PCI Registry (CENIC). J Am Coll Cardiol. 2019;74(13):779. doi:10.1016/j.jacc.2019.08.942.
• In 847 patients older than 90 years undergoing PCI (68% with ACS) and included in the CENIC Registry between 2006 and 2016, the in-hospital mortality rate was 4.8%. 112112. Pinton F, Prado G, Bezerra C, Mariani J, Campos C, Caixeta A, Franken M, Lemos PA. TCT-422 Clinical Outcomes and Predictors of Mortality Among 847 Nonagenarians Undergoing Percutaneous Coronary Intervention: Insights From a Brazilian Nationwide PCI Registry (CENIC Registry). J Am Coll Cardiol. 2019;74(13):418. doi:10.1016/j.jacc.2019.08.513.
• There are scarce data on long-term survival rates of patients undergoing PCI. In an analysis from procedures performed in the state of Rio de Janeiro between 1999 and 2000 in all public hospitals including 19 263 individuals, 1-year survival was 93% and 15-year survival was 57%. In that study, women, as compared to men, had a higher survival rate within 15 years after PCI. 113113. Silva CGSE, Klein CH, Godoy PH, Salis LHA, Silva NASE. Up to 15-Year Survival of Men and Women after Percutaneous Coronary Intervention Paid by the Brazilian Public Healthcare System in the State of Rio de Janeiro, 1999-2010. Arq Bras Cardiol. 2018;111(4):553-61. doi: 10.5935/abc.20180184.
Mortality Related to Coronary Artery Bypass Graft Surgery
• According to the SIH/SUS, the in-hospital mortality rate among patients undergoing CABG surgery in public institutions was 7.0% (1566 deaths in 22 537 procedures) in 2008 and 6.1% (1432 in 23 488 admissions) in 2019, a percent change of -12% (Chart 3-8). In 2019, the lowest rate was observed in the Northeastern region (4.4%), while the highest rate was found in the West-Central region (10.0%). 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• The BYPASS registry is an ongoing database established in 2015 by the Brazilian Society of Cardiovascular Surgery and involves 17 institutions representing all Brazilian regions. Among 2292 patients enrolled until November 2018 who underwent isolated or combined CABG, the in-hospital mortality rate was 2.8%, while 5.3% stayed on mechanical ventilation for more than 24 hours and 1.2% had an in-hospital stroke. 114114. Gomes WJ, Moreira RS, Zilli AC, Bettiati LC Jr, Figueira FAMDS, D’ Azevedo SSP, Soares MJF, Fernandes MP, Ardito RV, Bogdan RAB, Campagnucci VP, Nakasako D, Kalil RAK, Rodrigues CG, Rodrigues AB Jr, Cascudo MM, Atik FA, Lima EB, Nina VJDS, Heluy RA, Azeredo LG, Henrique OS Jr, Mendonça JT, Silva KKOG, Pandolfo M, Lima JD Jr, Faria RM, Santos JG, Paez RP, Coelho GHB, Pereira SN, Senger R, Buffolo E, Caputi GM, Santo JADE, Oliveira JAB, Berwanger O, Cavalcanti AB, Jatene FB. The Brazilian Registry of Adult Patient Undergoing Cardiovascular Surgery, the BYPASS Project: Results of the First 1,722 Patients. Braz J Cardiovasc Surg. 2017;32(2):71-6. doi: 10.21470/1678-9741-2017-0053. , 115115. Paez RP, Hossne NA Jr, Santo JADE, Berwanger O, Santos RHN, Kalil RAK, Jatene FB, Cavalcanti AB, Zilli AC, Bettiati LC Jr, Figueira FAMDS, D’Azevedo SSP, Soares MJF, Fernandes MP, Ardito RV, Bogdan RAB, Campagnucci VP, Nakasako D, Rodrigues CG, Rodrigues AB Jr, Cascudo MM, Atik FA, Lima EB, Nina VJDS, Heluy RA, Azeredo LG, Henrique OS Jr, Mendonça JT, Silva KKOG, Pandolfo M, Lima Júnior JD, Faria RM, Santos JGD, Coelho GHB, Pereira SN, Senger R, Buffolo E, Caputi GM, Oliveira JAB, Gomes WJ; BYPASS Registry Study Group. Coronary Artery Bypass Surgery in Brazil: Analysis of the National Reality Through the BYPASS Registry. Braz J Cardiovasc Surg. 2019;34(2):142-8. doi: 10.21470/1678-9741-2018-0313.
• The MASS II trial was a single-center randomized clinical trial designed to compare the long-term effects of medical therapy, angioplasty, or surgical strategies for the treatment of multivessel CAD with stable angina and preserved ventricular function conducted before 2007. The in-hospital mortality rates for PCI and CABG were 2.4% and 2.5%, respectively. 116116. Hueb W, Lopes NH, Gersh BJ, Soares P, Machado LA, Jatene FB, Oliveira SA, Ramires JA. Five-Year Follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): A Randomized Controlled Clinical Trial of 3 Therapeutic Strategies for Multivessel Coronary Artery Disease. Circulation. 2007;115(9):1082-9. doi: 10.1161/CIRCULATIONAHA.106.625475. The 10-year survival rates were not significantly different between the groups: 75% for CABG, 75% for PCI, and 69% for medical therapy (p=0.089). 117117. Hueb W, Lopes N, Gersh BJ, Soares PR, Ribeiro EE, Pereira AC, Favarato D, Rocha AS, Hueb AC, Ramires JA. Ten-Year Follow-up Survival of the Medicine, Angioplasty, or Surgery Study (MASS II): A Randomized Controlled Clinical Trial of 3 Therapeutic Strategies for Multivessel Coronary Artery Disease. Circulation. 2010;122(10):949-57. doi: 10.1161/CIRCULATIONAHA.109.911669. In another trial of the same group (MASS III), similar 10-year survival rates were described. 118118. Hueb W, Rezende PC, Gersh BJ, Soares PR, Favarato D, Lima EG, Garzillo CL, Jatene FB, Ramires JAF, Filho RK. Ten-Year Follow-Up of Off-Pump and On-Pump Multivessel Coronary Artery Bypass Grafting: MASS III. Angiology. 2019;70(4):337-44. doi: 10.1177/0003319718804402.
• In the REPLICCAR-I Registry, 2961 patients underwent isolated CABG in 10 hospitals between 2013 and 2016. The all-cause mortality rate was 3.4% at 30 days and 5.3% at 4 years of follow-up. 119119. Gonzales-Tamayo L, Campos CM, Lisboa LAF, Dallan LAO, Jatene FB, Mejia OAV. Choosing the Best Mortality Predictor for Isolated Cabg in Complex Coronary Artery Disease Patients: Performance Comparison of STS, Euroscore II, and Syntax Score II. J Am Coll Cardiol. 2019;73(9):2129. doi:10.1016/S0735-1097(19)32735-4.
• Several other single-center experiences, with both retrospective and prospective analyses, described short-term mortality for patients who underwent CABG ranging from 1.9% to 11.7%. 120120. Buffolo E, Branco JN, Gerola LR, Aguiar LF, Teles CA, Palma JH, Catani R. Off-Pump Myocardial Revascularization: Critical Analysis of 23 Years’ Experience in 3,866 Patients. Ann Thorac Surg. 2006;81(1):85-9. doi: 10.1016/j.athoracsur.2005.07.032.
Burden of Disease
• The GBD 2019 estimated a rate of 1563 (95% UI, 1472-1636) DALYs lost per 100 000 individuals due to IHD (Table 3-3). This DALY rate was equivalent to 5.7% (95% UI, 5.1%-6.3%) of all DALYs, meaning that IHD was the second most common cause of DALYs in Brazil among females (after neonatal disorders) and males (after interpersonal violence) in 2019. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• From 1990 to 2019, the total number of DALYs attributable to IHD continuously increased, the crude DALY rate per 100 000 remained fairly stable, and the age-standardized DALY rate per 100 000 gradually declined 50% in the period (Table 3-3, Chart 3-11). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
•When considering the Brazilian regions, the trend of age-standardized DALY rate from 1990 to 2019 resembles what was observed for mortality rates. In 1990, the highest rates were in the Southern and Southeastern regions, whereas the lowest rates were in the Northern and Northeastern regions. All states showed reductions in the age-adjusted DALY rate in the period, with variations of smaller magnitude in the Northern and Northeastern regions, so that the heterogeneity among the regions diminished (Chart 3-12). The states with the least pronounced decreases were Ceará (-16%), Paraíba (-25%), and Alagoas (-26%, Table 3-3). There was a negative correlation between the change in age-standardized DALY rate from IHD in the period and the SDI ( r 20.59, p-value < 0.01, Chart 3-13). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
, 9090. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. Seattle: Institute for Health Metrics and Evaluation; 2020. In 2019, the lowest DALY rate was reported in the state of Amazonas (1106 per 100 000), whereas the highest rates were noted in the states of Maranhão (2157 per 100 000) and Pernambuco (2163 per 100 000, Table 3-3). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Most of the DALYs associated with IHD were due to YLLs. The age-standardized rate of YLL was 1501 (95% UI, 1408-1574) per 100 000. These YLLs represented 9.1% (95% UI, 8.6%-9.6%) of all YLLs in 2019. This rate halved from 1990 to 2019, with a percent change of -50.8% (95% UI, -53.1% to -48.5%). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The age-adjusted rate of YLDs attributable to CHD was 63 (95% UI, 41-89) per 100 000. From 1990 to 2019, this rate reduced by 5% (95% UI, -7% to -3%). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Healthcare Utilization and Cost
• According to SIH/SUS administrative data, the absolute number of hospital admissions for ACS to public institutions remained stable from 2008 to 2019 (Chart 3-14). In 2019, there were 70 204 hospital admissions (33.4 per 100 000 inhabitants) due to ACS in the country. The number of hospitalizations due to AMI increased from 47 358 in 2008 to 80 614 in 2019 (percent change: 70%) or from 25.0 to 38.4 per 100 000 inhabitants (percent change: 54%, Chart 3-14). Hospital admissions due to CCSs decreased from 12 393 (6.5 per 100 000) in 2008 to 6703 (3.2 per 100 000) in 2019 (Chart 3-14). 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
•Hospital admissions in the public service for non-primary PCIs more than doubled from 2008 (n= 38 635) to 2019 (n= 85 518, Chart 3-15), while primary PCIs for AMI management increased by 45% (from 7 648 to 11 099). Considering rates per 100 000 inhabitants, the values for non-primary PCI were 20.4 in 2008 and 40.7 in 2019 (percent change: 100%) and those for primary PCI were 4.0 in 2008 and 5.3 in 2019 (percent change: 31%). Meanwhile, the total number of CABGs remained stable in the period (Chart 3-15), totalizing 21 018 procedures (10.0 per 100 000 inhabitants) in 2019. As a consequence, percutaneous myocardial revascularization increased as compared to surgery, from 69% of all procedures in 2008 to 82% in 2019 (Chart 3-16). 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• Most PCIs performed in public hospitals in the last years were categorized as non-primary PCIs. The percentage of primary PCIs among all PCIs remained stable from 2009 to 2019 (between 9% and 13%). 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• In 2019, the average lengths of hospital stay for ACS, AMI, PCI and CABG surgery in public hospitals were 5.4, 8.7, 3.8, and 12.0 days, respectively, remaining stable since 2008. 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• According to the SIH/SUS, the unadjusted annual cost associated with all admissions due to ACS to public hospitals increased from R$ 44 710 681 in 2008 to R$ 81 167 005 in 2019. In the same period, the annual cost related to hospitalizations for AMI increased from R$ 65 019 331 to R$ 151 123 021, while the cost associated with CCSs decreased from R$ 7 798 578 to R$ 6 475 644. Converting to purchasing power parity-adjusted Int$ 2019, the amount associated with treatment for ACS has slightly decreased in recent years, reaching Int$ 39 230 065 in 2019; this expenditure has remained stable in the setting of AMI (Int$ 73 041 576 in 2019) and diminished for CCS (Int$ 3 129 842 in 2019, Chart 3-17). 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
•In international dollars, the average reimbursed amount per hospital admission due to ACS, AMI, or CCS decreased from 2008 to 2019 (Chart 3-18). In 2019, the average expenditures per admission were R$ 1156 (Int$ 559), R$ 1875 (Int$ 906), and R$ 966 (Int$ 467) for ACS, AMI, and CCS, respectively. 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• The SUS administrative database showed that the total amount reimbursed for non-primary PCIs was R$ 546 132 199 (Int$ 263 959 497) in 2019. The correspondent cost for primary PCIs was R$ 74 907 756 (Int$ 36 204 812). The average expenditure paid per patient was R$ 6386 (Int$ 3087) for non-primary PCI and R$ 6749 (Int$ 3262) for primary PCI. Regarding CABG, the total amount reimbursed was R$ 278 544 224 (Int$ 134 627 464), corresponding to a mean value of R$ 13 253 (Int$ 6406) per surgical procedure. 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
•In international dollars, the total annual cost due to non-primary PCI increased in recent years, while the annual cost related to primary PCI remained stable and the CABG expenditure declined (Chart 3-19). The average amount reimbursed per hospital admission has decreased for both PCI and CABG since 2008 (Chart 3-20). 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• A global modeling approach was performed in 2015 to assess the economic impact (health system and productivity) of four heart conditions in Brazil (hypertension, heart failure, AMI, and atrial fibrillation), providing estimates of the annual cost for the year 2015. The four heart conditions were estimated to affect ~45.7 million people in Brazil, corresponding to 32% of the adult population. AMI posed the greatest financial cost, with an estimated prevalence of 0.2% (334 978 cases), a health system cost per case of US$ 48 118, and a productivity cost of US$ 18 678. 124124. Stevens B, Pezzullo L, Verdian L, Tomlinson J, George A, Bacal F. The Economic Burden of Heart Conditions in Brazil. Arq Bras Cardiol. 2018;111(1):29-36. doi: 10.5935/abc.20180104.
• The annualized cost for an individual with chronic CHD was estimated to be around R$ 2733 ± 2307 by the SUS, with the outpatient cost being responsible for 54% of the total. For private insurance plans, the cost was estimated to be R$ 6788 ± 7842, with 69% of which related to inpatient costs. For outpatient costs, medications were responsible for R$ 1154, representing, for public and private payers, 77% and 55% of the outpatient costs and 42% and 17% of the total cost, respectively. 125125. Azambuja MI, Foppa M, Maranhão MF, Achutti AC. Economic Burden of Severe Cardiovascular Diseases in Brazil: An Estimate Based on Secondary Data. Arq Bras Cardiol. 2008;91(3):148-71. doi: 10.1590/s0066-782x2008001500005.
• In a report from a CHD clinic of a public hospital, the mean annual cost per outpatient was US$ 1521 (2015 currency). The mean cost per hospitalization was US$ 1976, and the expenses were higher in the first and last years of follow-up. Unstable angina, revascularization procedures, diabetes, hypertension, and obesity were predictors of higher hospitalization costs. 126126. Schlatter RP, Hirakata VN, Polanczyk CA. Estimating the Direct Costs of Ischemic Heart Disease: Evidence From a Teaching Hospital in BRAZIL, A Retrospective Cohort Study. BMC Cardiovasc Disord. 2017;17(1):180. doi: 10.1186/s12872-017-0615-1.
• Data from 2008 to 2014 estimated that 4 653 884 diagnostic tests were performed for CVD in Brazil, including 3 015 993 electrocardiograms, 862 627 invasive angiographies, and 669 969 nuclear tests, leading to an overall cost of US$ 271 million. In this national geospatial evaluation of health access, ACS mortality was associated with lower income, fewer nuclear tests, and an increase in exercise electrocardiogram tests and cardiac catheterization procedures. 127127. Hertz JT, Fu T, Vissoci JR, Rocha TAH, Carvalho E, Flanagan B, Andrade L, Limkakeng AT, Staton CA. The Distribution of Cardiac Diagnostic Testing for Acute Coronary Syndrome in the Brazilian Healthcare System: A national Geospatial Evaluation of Health Access. PLoS One. 2019;14(1):e0210502. doi: 10.1371/journal.pone.0210502.
• A study using micro costing methodology evaluated the costs associated with PCI in 40 patients from two public teaching hospitals in 2017. The median cost of PCI was R$ 4579 in one hospital and R$ 3156 in the other. Most of the expenditure was due to the prosthesis cost (72% and 81% of the total cost). 128128. Schlatter R, Etges AP, Neyeloff JL, Cruz LN, Kopittke L, Moreira L, Polanczyk CA. PCV51 a Microcosting study for Angioplasty Procedure: real world data in southern Brazil. Value in Health 2019;22:128. doi: 10.1016/j.jval.2019.04.487.
• In a quantitative, descriptive, and cross-sectional study carried out in a philanthropic hospital in the city of São Paulo, assessing 1913 consecutive patients who underwent CABG in 2012, the average cost per patient was US$ 7993 (median US$ 6463). The amount paid by the public health system was US$ 3450 (median US$ 3159), resulting in a deficit of 51% of the total cost for the providers. 129129. Silva GSD, Colósimo FC, Sousa AG, Piotto RF, Castilho V. Coronary Artery Bypass Graft Surgery Cost Coverage by the Brazilian Unified Health System (SUS). Braz J Cardiovasc Surg. 2017;32(4):253-9. doi: 10.21470/1678-9741-2016-0069.
• A retrospective analysis of medical claims of beneficiaries of health insurance plans was performed considering hospitalization costs for patients admitted with ACS between 2010 and 2012. The mean cost per patient on medical therapy only was R$ 18 262, for those undergoing PCI, R$ 30 611, and for those undergoing CABG, R$ 37 455. 130130. Teich V, Piha T, Fahham L, Squiassi HB, Paloni EM, Miranda P, Araújo DV. Acute Coronary Syndrome Treatment Costs From the Perspective of the Supplementary Health System. Arq Bras Cardiol. 2015;105(4):339-44. doi: 10.5935/abc.20150129.
• An analysis of 240 patients undergoing isolated CABG in a reference hospital in 2013 showed an average hospitalization cost of R$ 22 647 ± 28 106 (R$ 35 400 ± 40 509 for those with some complication and of R$ 13 997 ± 5 801 for those without complication). 131131. Barbosa JL, Thiers CA, Silva AFR, Vianna MM, Gedeon POPR, Neto LM, Moreira, MBUD, Faria LF, Tura, BR. Impact of Complications of Myocardial Revascularization Surgery on Expenses During Hospital Stay. Int. J. Cardiovasc. Sci. 2019;32(1):28-34. doi: 10.5935/2359-4802.20180083.
• A cost analysis of 101 patients undergoing PCI at the SUS in 2014/2015 showed a median cost of R$ 6705 ± 3116 per patient. Costs were lower for elective PCI (R$ 5085 ± 16) than for PCI due to ACS (R$ 6854 ± 3396). 132132. Neto AFCB, Campos FZ, Gonçalves RB, Gomes IC, Sternick EB, Almeida AM. Costs and Clinical Outcomes in Percutaneous Coronary Intervention by the Brazilian National Health System. Int J Cardiovasc Sci. 2016;29(6):431-42. doi: 10.5935/2359-4802.20170007. doi: 10.5935/2359-4802.20170007.
Quality of Care
• Several publications addressed the quality of care in ACS in Brazil. 8282. Silva PGMBE, Berwanger O, Santos ESD, Sousa ACS, Cavalcante MA, Andrade PB, Neuenschwander FC, Vargas Filho H, Guimarães JI, Andrade J, Paola AAV, Malachias MVB, Mattos LAPE, Precoma DB, Bacal F, Dutra OP. One Year Follow-up Assessment of Patients Included in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2020;114(6):995-1003. doi: 10.36660/abc.20190879. , 8383. Franken M, Giugliano RP, Goodman SG, Baracioli LM, Godoy LC, Furtado RHM, Lima FG, Nicolau JC. Performance of Acute Coronary Syndrome Approaches in Brazil: A Report From the BRACE (Brazilian Registry in Acute Coronary SyndromEs). Eur Heart J Qual Care Clin Outcomes. 2020;6(4):284-92. doi: 10.1093/ehjqcco/qcz045. , 8585. Santos IS, Goulart AC, Brandão RM, Santos RC, Bittencourt MS, Sitnik D, Pereira AC, Pastore CA, Samesima N, Lotufo PA, Bensenor IM. One-year Mortality after an Acute Coronary Event and its Clinical Predictors: The ERICO Study. Arq Bras Cardiol. 2015;105(1):53-64. doi: 10.5935/abc.20150044. , 8686. Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, Santucci EV, Victor E, Tenuta M, Carvalho V, Mira VL, Pieper KS, Weber B, Mota LH, Peterson ED, Lopes RD; Bridge-Acs Investigators. Effect of a Multifaceted Intervention on Use of Evidence-Based Therapies in Patients With Acute Coronary Syndromes in Brazil: The BRIDGE-ACS Randomized Trial. JAMA. 2012;307(19):2041-9. doi: 10.1001/jama.2012.413. , 9696. Oliveira JC, Almeida-Santos MA, Cunha-Oliveira J, Oliveira LCS, Barreto IDC, Lima TCRM, Arcelino LAM, Prado LFA, Silveira FS, Nascimento TAS, Ferreira EJP, Barreto RV, Moraes EV, Mendonça JT, Sousa ACS, Barreto-Filho JA; VICTIM Register Investigators. Disparities in Access and Mortality of Patients With ST-Segment-Elevation Myocardial Infarction Using the Brazilian Public Healthcare System: VICTIM Register. J Am Heart Assoc. 2019;8(20):e013057. doi: 10.1161/JAHA.119.013057. , 100100. Lana MLL, Beaton AZ, Brant LCC, Bozzi ICRS, Magalhães O, Castro LRA, Silva FCT Jr, Silva JLP, Ribeiro ALP, Nascimento BR. Factors Associated With Compliance to AHA/ACC Performance Measures in a Myocardial Infarction System of Care in Brazil. Int J Qual Health Care. 2017;29(4):499-506. doi: 10.1093/intqhc/mzx059. These studies highlight the opportunities for healthcare improvement, as well as the regional differences and heterogeneity of public and private services that may impact the outcomes as described above. Moreover, some publications reported on the implementation of strategies to optimize the quality of care in ACS. 8686. Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, Santucci EV, Victor E, Tenuta M, Carvalho V, Mira VL, Pieper KS, Weber B, Mota LH, Peterson ED, Lopes RD; Bridge-Acs Investigators. Effect of a Multifaceted Intervention on Use of Evidence-Based Therapies in Patients With Acute Coronary Syndromes in Brazil: The BRIDGE-ACS Randomized Trial. JAMA. 2012;307(19):2041-9. doi: 10.1001/jama.2012.413. , 102102. Filgueiras Filho NM, Feitosa Filho GS, Solla DJF, Argôlo FC, Guimarães PO, Paiva Filho IM, Carvalho LGM, Teixeira LS, Rios MNO, Câmara SF, Novais VO, Barbosa LS, Ballalai CS, De Lúcia CV, Granger CB, Newby LK, Lopes RD. Implementation of a Regional Network for ST-Segment-Elevation Myocardial Infarction (STEMI) Care and 30-Day Mortality in a Low- to Middle-Income City in Brazil: Findings From Salvador’s STEMI Registry (RESISST). J Am Heart Assoc. 2018;7(14):e008624. doi: 10.1161/JAHA.118.008624. , 133133. Marino BCA, Ribeiro ALP, Alkmim MB, Antunes AP, Boersma E, Marcolino MS. Coordinated Regional Care of Myocardial Infarction in a Rural Area in Brazil: Minas Telecardio Project 2. Eur Heart J Qual Care Clin Outcomes. 2016;2(3):215-24. doi: 10.1093/ehjqcco/qcw020. , 134134. Marcolino MS, Brant LCC, Araujo JG, Nascimento BR, Castro LR, Martins P, Lodi-Junqueira L, Ribeiro ALP. Implementation of the Myocardial Infarction System of Care in City of Belo Horizonte, Brazil. Arq Bras Cardiol. 2013;100(4):307-14.
• In the prospective registry ACCEPT, the rate of full adherence to guideline-recommended medications (dual antiplatelet therapy, parenteral anticoagulants, statins, and beta-blockers) was 62% soon after admission for ACS. Among patients with STEMI (n=1714), 82% were treated with either fibrinolysis or primary PCI. Rates of reperfusion therapies for AMI differed according to the region of the country: 87%, 85%, 73%, 67%, and 66% in the Southern, Southeastern, Northeastern, West-Central, and Northern regions, respectively. Acetylsalicylic acid was prescribed in 95% of the cases on discharge and 86% at 12 months of follow-up. P2Y12 receptor inhibitors were prescribed in 92% of the instances on admission, 79% on discharge, and 47% after 12 months. Statins were recommended to 93% of the patients on discharge and 83% after 12 months. Therapy considered incomplete and hospitalization in a public institution, among other factors, were associated with major cardiovascular events. 8282. Silva PGMBE, Berwanger O, Santos ESD, Sousa ACS, Cavalcante MA, Andrade PB, Neuenschwander FC, Vargas Filho H, Guimarães JI, Andrade J, Paola AAV, Malachias MVB, Mattos LAPE, Precoma DB, Bacal F, Dutra OP. One Year Follow-up Assessment of Patients Included in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2020;114(6):995-1003. doi: 10.36660/abc.20190879.
• In the BRACE cross-sectional analysis, the quality of care in ACS was measured by a performance score that included ASA prescription on hospital admission, ASA/beta-blocker/statin prescription on discharge, and reperfusion therapy to STEMI patients within 12 hours from symptom onset, among other factors. Importantly, lower scores were independently associated with a higher risk for hard outcomes and in-hospital death. The score was lower in the Northern and Northeastern regions than in the rest of the country both within the first 24 hours and on hospital discharge. Higher scores were observed in teaching versus non-teaching hospitals. No significant difference in the scores was detected between public and private institutions, although reperfusion therapy for STEMI was more frequent in private hospitals (86% versus 75%), while ASA/statin prescription on discharge was more common in public hospitals. Overall, the percentages of patients prescribed ASA, statin, and beta-blocker at discharge were 86%, 82%, and 69%, respectively. 8383. Franken M, Giugliano RP, Goodman SG, Baracioli LM, Godoy LC, Furtado RHM, Lima FG, Nicolau JC. Performance of Acute Coronary Syndrome Approaches in Brazil: A Report From the BRACE (Brazilian Registry in Acute Coronary SyndromEs). Eur Heart J Qual Care Clin Outcomes. 2020;6(4):284-92. doi: 10.1093/ehjqcco/qcz045.
• Among participants included in the ERICO study between 2009 and 2012, reperfusion therapy was performed in 72% of STEMI cases. The rates of medical treatment during hospitalization were as follows: 98% for ASA, 96% for clopidogrel and heparin, 92% for statins, and 84% for beta-blockers. 8585. Santos IS, Goulart AC, Brandão RM, Santos RC, Bittencourt MS, Sitnik D, Pereira AC, Pastore CA, Samesima N, Lotufo PA, Bensenor IM. One-year Mortality after an Acute Coronary Event and its Clinical Predictors: The ERICO Study. Arq Bras Cardiol. 2015;105(1):53-64. doi: 10.5935/abc.20150044.
• In the VICTIM study, the mean time between symptom onset and hospital admission was longer in the context of the public service as compared to private hospitals (25 ± 37 versus 9 ± 21 hours; respectively, P <0.001). The rate of primary PCI was lower in public services than in private hospitals (45% versus 78%, respectively, P <0.001). 9696. Oliveira JC, Almeida-Santos MA, Cunha-Oliveira J, Oliveira LCS, Barreto IDC, Lima TCRM, Arcelino LAM, Prado LFA, Silveira FS, Nascimento TAS, Ferreira EJP, Barreto RV, Moraes EV, Mendonça JT, Sousa ACS, Barreto-Filho JA; VICTIM Register Investigators. Disparities in Access and Mortality of Patients With ST-Segment-Elevation Myocardial Infarction Using the Brazilian Public Healthcare System: VICTIM Register. J Am Heart Assoc. 2019;8(20):e013057. doi: 10.1161/JAHA.119.013057.
• In a university hospital in the city of Belo Horizonte, compliance with 13 pre-specified performance measures was evaluated in 1129 patients with STEMI or non-STEMI hospitalized between 2011 and 2014. The median compliance was 83% and the treatment of 67% of the patients reached at least 80% of the quality measures. The rate of reperfusion therapy in STEMI cases was 56%. 100100. Lana MLL, Beaton AZ, Brant LCC, Bozzi ICRS, Magalhães O, Castro LRA, Silva FCT Jr, Silva JLP, Ribeiro ALP, Nascimento BR. Factors Associated With Compliance to AHA/ACC Performance Measures in a Myocardial Infarction System of Care in Brazil. Int J Qual Health Care. 2017;29(4):499-506. doi: 10.1093/intqhc/mzx059.
• In a study from the Minas Telecardio 2 Project, 593 patients with ACS were included between 2013 and 2014. Among individuals with STEMI, 46% received reperfusion therapy, mostly primary PCI. The door-to-balloon time was greater than 90 minutes in 37.5% of those patients. Overall, the rates of ASA, P2Y12 inhibitor, and statin prescriptions were 97%, 86%, and 81% within 24 hours, and 93%, 69%, and 86% on discharge, respectively. 101101. Marino BC, Marcolino MS, Reis RS Jr, França AL, Passos PF, Lemos TR, Antunes IO, Ferreira CG, Antunes AP, Ribeiro ALP. Epidemiological Profile and Quality Indicators in Patients With Acute Coronary Syndrome in Northern Minas Gerais - Minas Telecardio 2 Project. Arq Bras Cardiol. 2016;107(2):106-15. doi: 10.5935/abc.20160095.
• In another publication from the Minas Telecardio Project 2, the quality of care for STEMI was evaluated before (n = 214) and after (n = 143) the implementation of a coordinated management protocol that took place between 2014 and 2015. The rate of reperfusion therapy increased from 71% to 81% (P = 0.045), while the percentage of patients being prescribed ASA and P2Y12 inhibitors increased from 94% and 88%, respectively, to 100% in both cases. In addition, a non-significant decrease in the odds of in-hospital death was reported (OR, 0.73; 95% CI, 0.34–1.60). 133133. Marino BCA, Ribeiro ALP, Alkmim MB, Antunes AP, Boersma E, Marcolino MS. Coordinated Regional Care of Myocardial Infarction in a Rural Area in Brazil: Minas Telecardio Project 2. Eur Heart J Qual Care Clin Outcomes. 2016;2(3):215-24. doi: 10.1093/ehjqcco/qcw020.
• In a retrospective observational study of public services in the city of Belo Horizonte, the in-hospital mortality rate reduced after the implementation of an AMI management system, including tele-electrocardiography (12% in 2009 and 7% in 2011, P < 0.001). 134134. Marcolino MS, Brant LCC, Araujo JG, Nascimento BR, Castro LR, Martins P, Lodi-Junqueira L, Ribeiro ALP. Implementation of the Myocardial Infarction System of Care in City of Belo Horizonte, Brazil. Arq Bras Cardiol. 2013;100(4):307-14.
• The RESISST study reported outcomes in STEMI before and after the implementation of an integrated regional network supported by telemedicine in the city of Salvador, Bahia state. The authors reported an increase in the rates of primary reperfusion (from 29% to 54%, P <0.001), a decrease in the 30-day mortality rate (from 20% to 5%, P <0.001), and an increase in the use of dual antiplatelet therapy and statins. 102102. Filgueiras Filho NM, Feitosa Filho GS, Solla DJF, Argôlo FC, Guimarães PO, Paiva Filho IM, Carvalho LGM, Teixeira LS, Rios MNO, Câmara SF, Novais VO, Barbosa LS, Ballalai CS, De Lúcia CV, Granger CB, Newby LK, Lopes RD. Implementation of a Regional Network for ST-Segment-Elevation Myocardial Infarction (STEMI) Care and 30-Day Mortality in a Low- to Middle-Income City in Brazil: Findings From Salvador’s STEMI Registry (RESISST). J Am Heart Assoc. 2018;7(14):e008624. doi: 10.1161/JAHA.118.008624.
• The BRIDGE-ACS trial was a cluster-randomized study that evaluated a multifaceted quality improvement program for the treatment of patients with ACS. Compared to routine practice, the intervention, which included educational materials for clinicians, reminders, algorithms, and case manager training, increased the odds of receiving eligible medications. Moreover, the rates of in-hospital cardiovascular event were 5.5% in the intervention group and 7.0% in the control group (population average OR [ORPA], 0.72 [95% CI, 0.36-1.43]), whereas the 30-day all-cause mortality rates were 7.0% and 8.4% in the intervention and control groups, respectively (ORPA, 0.79 [95% CI, 0.46-1.34]). 8686. Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, Santucci EV, Victor E, Tenuta M, Carvalho V, Mira VL, Pieper KS, Weber B, Mota LH, Peterson ED, Lopes RD; Bridge-Acs Investigators. Effect of a Multifaceted Intervention on Use of Evidence-Based Therapies in Patients With Acute Coronary Syndromes in Brazil: The BRIDGE-ACS Randomized Trial. JAMA. 2012;307(19):2041-9. doi: 10.1001/jama.2012.413.
Future Research
• Additional data are needed for further understanding of the epidemiological distribution of CHD in Brazil, in particular:
1. development of nationwide databases aiming at gathering accurate and real-time information on the epidemiology of distinct clinical presentations of CHD, including delivery of care, performance, and outcome measurements;
2. systematic reviews of prevalence and mortality rates of ACS, stable angina, PCI, and CABG, including representative samples of all geographical areas of the country;
3. assessment of the effectiveness of structured nationwide programs for quality and performance measurement of different providers (public, non-for-profit, and for-profit) to understand the current situation, as well as for designing strategies aimed at reducing CVD morbidity and mortality;
4. additional economic and cost-effectiveness analyses of the impact of CHD and its diagnostic and therapeutic interventions, from a macro level and using micro costing methods for both the public and private healthcare systems;
5. development of structured programs to assess the prevalence, incidence, and clinical and economic impact of chronic CHD in the outpatient setting.
4. CARDIOMYOPATHY AND HEART FAILURE
ICD-10 I42; I50; B57.2
See Tables 4-1 through 4-12 and Charts 4-1 through 4-10
Abbreviations Used in Chapter 4
| BREATHE | Brazilian Registry of Heart Failure |
| ChCM | Chagas Cardiomyopathy |
| ChD | Chagas Disease |
| CI | Confidence Interval |
| DALY | Disability-Adjusted Life Years |
| FU | Federative Unit |
| GBD | Global Burden of Disease |
| HCM | Hypertrophic Cardiomyopathy |
| HF | Heart Failure |
| HF-PEF | Preserved Ejection Fraction Heart Failure |
| HF-REF | Reduced Ejection Fraction Heart Failure |
| HR | Hazard Ratio |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems, 10thRevision |
| IQR | Interquartile Range |
| NChC | Non-Chagas Cardiomyopathies |
| OR | Odds Ratio |
| PAR | Population Attributable Risk |
| REMADHE | Repetitive Education at Six-Month Intervals and Monitoring for ADherence in Heart Failure Outpatients trial |
| SDI | Sociodemographic Index |
| SEADE | Data Analysis State System Foundation (in Portuguese, Fundação Sistema Estadual de Análise de Dados ) |
| SIM | Brazilian Mortality Information System (in Portuguese, Sistema de Informações sobre Mortalidade ) |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| UI | Uncertainty Interval |
| US | United States of America |
| YLD | Years Lived with Disability |
| YLL | Years of Life Lost |
– Number of prevalence cases, age-standardized prevalence rates (per 100 000) of cardiomyopathy and myocarditis, and percent change of rates, in Brazil and its Federative Units, 1990 and 2019.
– Number of incidence cases, age-standardized incidence rate (per 100 000) of cardiomyopathy and myocarditis, and percent change of rates, in Brazil and its Federative Units, 1990 and 2017.
– Incidence rates of cardiomyopathy and myocarditis (per 100 000) and percent change of rates, by age and sex, Brazil, 1990 and 2019.
– Number of deaths, age-standardized mortality rates (per 100 000) of cardiomyopathy and myocarditis, and percent change of rates, in Brazil and its Federative Units, 1990 and 2019.
– Mortality rates of cardiomyopathy and myocarditis (per 100 000) and percent change of rates, by age and sex, Brazil, 1990-2019.
– Number of DALYs, age-standardized DALY rates (per 100 000) due to cardiomyopathy and myocarditis, and percent change of rates, in Brazil and its Federative Units, 1990 and 2019.
– Rates of DALYs due to cardiomyopathy and myocarditis (per 100 000) and percent change of rates, by age and sex, Brazil, 1990 and 2019.
– Number of deaths, age-standardized mortality rates (per 100 000) of Chagas disease, and percent change of rates, in Brazil and its Federative Units, 1990 and 2019.
– Number of prevalence cases, age-standardized prevalence rates (per 100 000) of heart failure from all causes, and percent change of rates, in Brazil and its Federative Units, 1990 and 2017.
– Prevalence rates of heart failure (per 100 000) and percent change of rates, by age and sex, Brazil, 1990 and 2017.
– Number and age-standardized rates of YLDs (per 100 000) due to heart failure from all causes, and percent change of rates, in Brazil and its Federative Units, 1990 and 2017.
– Rates of YLDs due to heart failure (per 100 000) and percent change of rates, by age and sex, Brazil, 1990 and 2017.
– Prevalence rate (A) and crude prevalence rate (B) of cardiomyopathy and myocarditis, per 100 000 inhabitants, Brazil, 1990-2019.
– Age-standardized and all ages mortality rate due to cardiomyopathy and myocarditis, per 100 000 inhabitants, Brazil, 1990-2019.
– Correlation between the sociodemographic index (SDI) and the age-standardized mortality rate due to cardiomyopathy and myocarditis, per 100 000 inhabitants, 1990 and 2019.
– Age-standardized and all ages rates of DALYs attributable to cardiomyopathy and myocarditis, per 100 000 inhabitants, in Brazil, from 1990 to 2017.
Data derived from Global Burden of Disease Study 2017 (GBD 2017). 152152. Global Burden of Disease Study 2017 (GBD 2017) results. Global Health Data Exchange website. Seattle, WA: Institute for Health Metrics and Evaluation (IHME), University of Washington; 2017. [cited 2021 Nov 09]. Available From: http://ghdx.healthdata.org/g .
http://ghdx.healthdata.org/g...
– Age-standardized and all ages mortality rates attributable to Chagas Disease, per 100 000 inhabitants, in Brazil from 1990 to 2019.
– Correlation between percent change in age-standardized mortality rates due to Chagas disease, per 100 000 inhabitants, from 1990 to 2019 and the Sociodemographic Index (SDI) in 1990 and in 2019.
– Spatial distribution of mean mortality rates related to Chagas disease, per 100 000 inhabitants, based on multiple causes of death by municipality, Brazil, 1999–2007.
– Standardized mortality rate due to Chagas disease in Brazil according to age range (in years) and year of occurrence, from 2000 to 2010.
– Trends of mortality from heart failure, from 2007 to 2016, in Brazil (BR), in the state of Rio Grande do Sul (RS), and in the city of Porto Alegre (POA).
Cardiomyopathy and Myocarditis
Prevalence and Incidence
• According to GBD Study 2019 estimates, the age-standardized prevalence of cardiomyopathy and myocarditis decreased in Brazil, from 76.6 (95% UI, 53.4-107.2) in 1990 to 73.0 (95% UI, 51.1-100.1) in 2019, a decrease of 4.7% (95% UI, - 9.5 to 0.8) in the period (Chart 4-1.A and Table 4-1). In absolute numbers, estimates of the prevalence of cardiomyopathy and myocarditis in Brazil increased from less than 60 000 in 1990 to over 160 000 in 2019, mainly due to population growth and aging (Chart 4-1.B). The cardiomyopathy and myocarditis prevalence was greater in men (98.9; 95% UI, 69.5-137.2) than in women (54.1; 95% UI, 38.4-73.8) in 2019, although there was a prevalence decrease of 5 (95% UI, -11.6 - 0) for women and of 2.9 (95% UI, -9.1 - 0) for men in that period. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• According to GBD Study 2019 estimates, the prevalence of cardiomyopathy and myocarditis is highly variable amongst Brazilian FUs, and the percent change varied unevenly between 1990 and 2019 (Table 4-1). In 2019, the highest rates were observed in São Paulo, Paraíba, and Roraima. From 1990 to 2019, increased age-standardized prevalence rates were observed in Goiás and Maranhão, while age-standardized prevalence decreased in all other FUs. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Regarding age-standardized incidence rates per 100 000 per-year, the GBD Study 2019 estimates were 15.8 (95% UI, 12.7-19.2) in 1990, and 15.8 (95% UI, 12.7-19.2) in 2019, with a small change of -0.2% (95% UI, -0.3 to -0.2) during that period (Table 4-2). Absolute numbers of incident cases were 18 583 (95% UI, 14 825-22 718) in 1990 and 35 863 (95% UI, 28 946-43 756) in 2019; that increase is related to population growth and aging. Table 4-3 depicts the incidence rates of cardiomyopathy and myocarditis per 100 000 inhabitants, by age, for both sexes, in 1990 and 2019, and the percent change of the rates. In 1990 and 2019, the highest rates were observed in the ‘70+ years’ group. From 1990 to 2019, the incidence increased in the ‘15-49 years’ and the ‘70+ years’ age groups for both women and men. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Mortality
• According to the GBD Study 2019 estimates, the mortality rates due to cardiomyopathy and myocarditis seemed to increase in the 1990s but decreased in the following 2 decades (Chart 4-2). As shown in Table 4-4, the mortality rates were 15.9 (95% UI, 12.4-17.1) in 1990 and 9.4 (95% UI, 8.3-11.1) in 2019, per 100 000 inhabitants, a decrease of 40.8% (95% UI, -46.6 to -25.4). Despite this decrease in mortality rates, the number of deaths from cardiomyopathy and myocarditis increased in that period due to population growth and aging. Cardiomyopathy and myocarditis were responsible for 13 408 (95% UI, 8417-10 163) deaths in 1990, rising to 21 425 (95% UI, 17 885-21 745) deaths in 2019. The GBD Study 2019 estimates of mortality rates due to cardiomyopathy refer to cases with cardiomyopathy listed as an underlying cause of death. Death due to HF related to other specific causes are attributed to the underlying disease, i.e., deaths related to ischemic cardiomyopathy are coded as due to ischemic heart disease. Moreover, for the GBD project, HF is not considered a primary cause of death, and all deaths coded as related to HF are recoded to the baseline condition (see below). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Table 4-4 also depicts the total number of deaths and age-standardized mortality rate (per 100 000 inhabitants) due to cardiomyopathy and myocarditis, as well as the percent change of rates, by FU, in Brazil, in 1990 and 2019. All FU had decreased mortality rates, with the highest percentages of reductions observed between 1990 and 2019 in the states of Goiás and Paraná. In 2019, the FUs with the lowest mortality rates (below 6.0) were the states of Amazonas, Rio Grande do Norte and Pará.
• Table 4-5 shows mortality rates due to cardiomyopathy and myocarditis according to sex and by age groups, from the GBD Study 2019 estimates. Women had lower age-standardized mortality rates, as well as a more pronounced reduction from 1990 to 2019. Rates in women were 13.5 (95% UI, 9.9-14.7) in 1990 and 7.2 (95% UI, 6.2 - 9) in 2019, a reduction of 46.6% (95% UI, -54.8 to -0.2). Rates in men were 18.7 (95% UI, 13.2 - 20.4) in 1990 and 12.1 (95% UI, 10 - 15.1) in 2019, a variation of -35.4% (95% UI, -43.3 to -0.1). As expected, the highest mortality rate was observed in the 70+ years group, with rates of 127.2 (95% UI, 96.5-138.3) in 1990 and of 84.6 (95% UI, 72.1-104) in 2019 per 100 000. For the 50-69 years group, rates were 29.2 (95% UI, 22 – 31.4) per 100 000 in 1990 and 17.2 (95% UI, 15.1 - 20) in 2019. Overall, mortality rates decreased from 1990 to 2019 in all age groups. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The GBD Study 2019 uses the SDI as an estimate of the socioeconomic level of a location. Chart 4-3 depicts the correlation between the SDI and the age-standardized mortality rate due to cardiomyopathy and myocarditis, per 100 000, both in 1990 and 2019. There was no correlation between age-standardized mortality rates and the SDI in 1990 (R = - 0.36, p=0.068). However, there was a significant correlation between age-standardized mortality rates and the SDI in 2019 (R = 0.4, p=0.041). 9090. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. Seattle: Institute for Health Metrics and Evaluation; 2020.
• In a study reporting data from the SEADE, from the state of São Paulo, cardiomyopathies were responsible for a total of 3571 deaths, representing 23.3% of HF-related deaths in 2006: dilated cardiomyopathy accounted for 17.2% of the deaths; alcoholic cardiomyopathy, for 0.45%; and restrictive cardiomyopathies, for 0.37%. Chagas disease and alcoholic cardiomyopathy were responsible for 7.8% and 0.45% of the HF-related deaths, respectively. 135135. Bocchi EA. Heart Failure in South America. Curr Cardiol Rev. 2013;9(2):147-56. doi: 10.2174/1573403x11309020007.
• Data on specific cardiomyopathies are scarce. A cohort study of 214 patients with HCM reported data from a 7-year follow-up in a tertiary hospital in São Paulo, Brazil. The mean age was 37±16 years, and 52% were women. There were 22 deaths (10%), 15 directly related to HCM (11 sudden deaths). The cumulative survival rates were 94.5% at 5 years, 91% at 10 years, and 87.9% at 15 years, with an annual mortality rate of 1%, which is low, considering that the study was conducted in a referral center. 136136. Arteaga E, Ianni BM, Fernandes F, Mady C. Benign Outcome in a Long-Term Follow-up of Patients With Hypertrophic Cardiomyopathy in Brazil. Am Heart J. 2005;149(6):1099-105. doi: 10.1016/j.ahj.2004.09.049.
Burden of Disease
• According to the GBD 2019 estimates, the trends of age-standardized DALY rates due to cardiomyopathy and myocarditis were similar to those of mortality, with a small increase in the 1990s and a decrease during the following decades. As shown in Table 4-6, age-standardized DALY rates were 399.4 (95% UI, 319.6-426.4) in 1990 and 238.6 (95% UI, 213-272.3) in 2019, per 100 000 inhabitants, a decrease of 40.3% (95% UI, -45.8 to -27.9). These changes are similar to those observed in the mortality rates. Despite that decrease in DALY rates, cardiomyopathy and myocarditis resulted in 431 381 (95% UI, 349,546-465,068) DALYs in Brazil in 1990 and in 545 772 (95% UI, 484 988-621 356) in 2019, which represents 0.62% of all DALYs. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Table 4-7 shows DALY rates due to cardiomyopathy and myocarditis according to sex and by age groups, from the GBD Study 2019 estimates. The age-standardized DALY rates were lower in women, and the reduction from 1990 to 2019 was also more pronounced in women. The DALY rates for women were 321.1 (95% UI, 237.7-346.2) in 1990 and 165.7 (95% UI, 147.3 - 198) in 2019, a reduction of 48.4% (95% UI, -55 to – 0.2). The DALY rates for men were 484.8 (95% UI, 353.6 – 528.5) in 1990 and 320.4 (95% UI, 257.7 – 371.8) in 2019, a reduction of 33.9% (95% UI, -41.8 to -0.1). As expected, the highest DALY rate was observed in the 70+ years group, followed by that of the 50-69 years group. Overall, DALY rates decreased from 1990 to 2019 in all age groups (Chart 4-4). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Chronic Chagas Disease and Chagas Cardiomyopathy
Prevalence and Incidence
• The 2010 prevalence of ChD in Brazil was estimated at 1 156 821 by the World Health Organization, 137137. Chagas disease in Latin America: An Epidemiological Update Based on 2010 Estimates. Wkly Epidemiol Rec. 2015;90(6):33-43. which is the last official available estimate, published in 2015. According to that statement, the estimated number of individuals with ChCM in Brazil is 231 364 subjects. 137137. Chagas disease in Latin America: An Epidemiological Update Based on 2010 Estimates. Wkly Epidemiol Rec. 2015;90(6):33-43. Those numbers reveal a significant decreasing trend of ChD human cases in Brazil in relation to previous estimates, which was attributed to various factors, mainly the almost complete interruption of the vectorial and transfusion-related transmission in Brazil.
• According to the GBD Study 2019 estimates, the age-standardized prevalence of ChD markedly reduced in Brazil, by 37.7% (95% UI, -40.2 to -35.2) from 1990 to 2019: from 1463 (95% UI, 1240-1711) in 1990 to 912 (95% UI, 788-1048) in 2019 per 100 000 inhabitants. The prevalence of ChD in Brazil in 2019 was higher in men [987 (95% UI, 856.4 – 1141.3)] than in women [841 (95% UI, 723.2-962)]. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• In a systematic review of population-based studies on ChD prevalence in Brazil, performed from 1980 until September 2012, 42 articles with relevant prevalence data were identified from a total of 4985 references. 138138. Martins-Melo FR, Ramos AN Jr, Alencar CH, Heukelbach J. Prevalence of Chagas Disease in Brazil: A Systematic Review and Meta-Analysis. Acta Trop. 2014;130:167-74. doi: 10.1016/j.actatropica.2013.10.002. The pooled estimate of ChD prevalence across studies for the entire period was 4.2% (95% CI, 3.1-5.7), ranging from 4.4% (95% CI, 2.3-8.3) in the 1980s to 2.4% (95% CI: 1.5-3.8) after 2000. The estimated ChD prevalence for males and females was similar (4.1% [95% CI, 2.6-6.6], 4.2% [95% CI, 2.6-6.8], respectively). The highest pooled prevalence was observed in individuals aged >60 years (17.7%; 95% CI, 11.4-26.5), and in the Northeastern (5.0%; 95% CI, 3.1-8.1) and Southeastern (5.0%; 95% CI, 2.4-9.9) regions and in mixed (urban/rural) areas (6.4%; 95% CI, 4.2-9.4). About 4.6 million (95% CI, 2.9-7.2 million) people are estimated to have been infected with T. cruzi in 2010. These estimates are much higher than those from the World Health Organization for 2010. 137137. Chagas disease in Latin America: An Epidemiological Update Based on 2010 Estimates. Wkly Epidemiol Rec. 2015;90(6):33-43. The authors observed a high degree of heterogeneity in most pooled estimates (I(2)>75%; p<0.001).
• In the NIH REDS-II Chagas retrospective cohort study, initially healthy blood donors with an index T. cruzi -seropositive donation and age, sex, and period-matched seronegative donors were followed up for 10 years. 139139. Sabino EC, Ribeiro ALP, Salemi VM, Oliveira CDL, Antunes AP, Menezes MM, Ianni BM, Nastari L, Fernandes F, Patavino GM, Sachdev V, Capuani L, Almeida-Neto C, Carrick DM, Wright D, Kavounis K, Goncalez TT, Carneiro-Proietti AB, Custer B, Busch MP, Murphy EL; National Heart, Lung, and Blood Institute Retrovirus Epidemiology Donor Study-II (REDS-II), International Component. Ten-year Incidence of Chagas Cardiomyopathy Among Asymptomatic Trypanosoma Cruzi-Seropositive Former Blood Donors. Circulation. 2013;127(10):1105-15. doi: 10.1161/CIRCULATIONAHA.112.123612. The differential incidence of cardiomyopathy was 1.85 per 100 person-years attributable to T. cruzi infection in the first 10 years of follow-up, and 0.9 per 100 person-years in the following 10 years. T. cruzi antibody level in the second visit was associated with development of cardiomyopathy (adjusted OR of 1.4, 95% CI 1.1-1.8) in the last visit. 140140. Nunes MCP, Buss LF, Silva JLP, Martins LNA, Oliveira CDL, Cardoso CS, Brito BOF, Ferreira AM, Oliveira LC, Bierrenbach AL, Fernandes F, Busch MP, Hotta VT, Martinelli LMB, Almeida Soeiro MCF, Brentegani A, Salemi VMC, Menezes MM, Ribeiro ALP. Incidence and Predictors of Progression to Chagas Cardiomyopathy: Long-Term Follow-Up of Trypanosoma Cruzi Seropositive Individuals. Circulation. 2021;144:1553–66. doi: 10.1161/circulationaha.121.055112.
Mortality
• According to the GBD Study 2019, the number of deaths due to ChD in Brazil has decreased over the past decades (Chart 4-5). In the 1990s, ChD was responsible for 7903 (95% UI, 2438-10 073) deaths, reducing to 6523 (95% UI, 3350-11 226) deaths in 2019. The age-standardized mortality rate showed more striking decrease (-67.5% change), from 8.6 (95% UI, 2.8-10.9) deaths per 100 000 inhabitants in 1990 to 2.8 (95% UI, 1.8-4.8) per 100 000 inhabitants in 2019, accounting for 1.6% of all cardiovascular deaths in the country. In 2019, men had higher age-standardized mortality rates than women (3.5, 95% UI, 1.4-6.2; and 2.2, 95% UI, 0.9-4.3, respectively). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Table 4-8 demonstrates the total number of deaths and age-standardized mortality rates due to ChD (per 100 000 inhabitants), for both sexes, and the percent change of rates, by FU, in Brazil, in 1990 and in 2019. There is striking variability among the FUs regarding the number of deaths and death rates for both years. In 1990, higher mortality rates (> 10 per 100 000 inhabitants) were observed in the Brazilian central FUs of Goiás, Distrito Federal, Minas Gerais and Bahia, with a peak in Goiás (52.3 per 100 000, 95% UI, 3.3-82.4). All FUs showed a reduction in mortality rates, varying from 39.9% (95% UI, 67.7 to 15.5) in the state of Ceará to 79.6% (95% UI, -84.3 to -5.8) in the state of Goiás.
• The estimated mortality in children under 5 years is practically zero. In the other age groups, the reduction in mortality rates was more pronounced (76.2 % change, UI -86.5 to 29.5) in the age group of 15-49 years, from 2.6 (UI 0.6-3.5) to 0.6 (UI 0.4-1.3) per 100 000 inhabitants. Most deaths occurred in individuals aged 70+ years, who presented the lowest percent reduction (-54.7%, UI -65-6.3) during the 1990-2019 period: from 53 (UI 19.2-66.3) to 24 (10.4-36.1) per 100 000 inhabitants. The decrease in age-standardized mortality rate per 100 000 inhabitants correlates with the SDI of Brazilian FUs in 1990 (R = - 0.56, p=0.003) and in 2019 (R = - 0.63, p<0.001) (Chart 4-6).
• Several population-based studies showed a reduction in mortality due to ChD in Brazil in the last decades. Martins-Melo et al . 141141. Martins-Melo FR, Alencar CH, Ramos AN Jr, Heukelbach J. Epidemiology of Mortality Related to Chagas’ Disease in Brazil, 1999-2007. PLoS Negl Trop Dis. 2012;6(2):e1508. doi: 10.1371/journal.pntd.0001508. reported that nationwide standardized mortality rates reduced gradually, from 3.78 (1999) to 2.78 (2007) deaths/year per 100 000 inhabitants (-26.4%). Nobrega et al . 142142. Nóbrega AA, Araújo WN, Vasconcelos AMN. Mortality Due to Chagas Disease in Brazil According to a Specific Cause. Am J Trop Med Hyg. 2014;91(3):528-33. doi: 10.4269/ajtmh.13-0574. showed that the nationwide standardized mortality rate decreased by 32.4%, from 3.4% in 2000 to 2.3% in 2010. The mortality rate due to cardiac involvement decreased in all regions of Brazil, except for the Northern region, where it increased by 1.6%. The Northeastern region had the smallest and the West-Central had the largest decrease. Simões et al . 143143. Simões TC, Borges LF, Assis ACP, Silva MV, Santos J, Meira KC. Chagas Disease Mortality in Brazil: A Bayesian Analysis of Age-Period-Cohort Effects and Forecasts for Two Decades. PLoS Negl Trop Dis. 2018;12(9):e0006798. doi: 10.1371/journal.pntd.0006798. studied the evolution of ChD mortality in Brazil from 1980 to 2014 and forecasted the mortality from years 2015 to 2034. Those authors estimated a progressive decline in ChD mortality, which would be highest among the young. The expected average reduction was 76.1% as compared to the last period observed (2010-2014) and the last period predicted (2030-2034). The West-Central, Southeastern, and Southern regions had a reduction in the rate of ChD deaths between 2000 and 2014. The mortality rate in the Northeastern region did not statistically differ in any period analyzed, while, in the Northern region, it showed an increasing trend.
• In a study analyzing all death certificates of individuals who died between 1999 and 2007 in Brazil, 141141. Martins-Melo FR, Alencar CH, Ramos AN Jr, Heukelbach J. Epidemiology of Mortality Related to Chagas’ Disease in Brazil, 1999-2007. PLoS Negl Trop Dis. 2012;6(2):e1508. doi: 10.1371/journal.pntd.0001508. based on the nationwide SIM, ChD was mentioned in 53 930 (0.6%) death certificates, as an underlying cause in 44 537 (82.6%) death certificates, and as an associated cause of death in 9387 (17.4%) death certificates. Acute ChD was responsible for 2.8% of the deaths. The mean standardized mortality rate was 3.36 per 100 000 inhabitants/year. This is 21% higher than the mortality rate considering merely the underlying cause of death (2.78 deaths per 100 000 inhabitants/year). The proportional mortality considering multiple causes of death was 0.6%. Individuals who died from ChD were predominantly males (57%), aged over 60 years (62.8%), and residing in the Southeastern region (53.6%). The West-Central region showed the highest proportional mortality of all regions (2.17%). 141141. Martins-Melo FR, Alencar CH, Ramos AN Jr, Heukelbach J. Epidemiology of Mortality Related to Chagas’ Disease in Brazil, 1999-2007. PLoS Negl Trop Dis. 2012;6(2):e1508. doi: 10.1371/journal.pntd.0001508.
• In the same database, calculating the mean mortality rate for each municipality of residence and using Empirical Bayesian smoothing, the spatial analysis identified a large cluster of high risk for mortality by ChD, involving nine states in the central region of Brazil (Chart 4-7). 144144. Martins-Melo FR, Ramos AN Jr, Alencar CH, Lange W, Heukelbach J. Mortality of Chagas’ disease in Brazil: Spatial Patterns and Definition of High-Risk Areas. Trop Med Int Health. 2012;17(9):1066-75. doi: 10.1111/j.1365-3156.2012.03043.x.
• Nobrega et al ., in a descriptive study using data from the SIM of all individuals who died of ChD in Brazil between 2000 and 2010, observed that, in the 2000-2010 period, most of the deaths due to ChD (85.9%) occurred in males aged > 60 years and were caused by cardiac involvement. During the studied period, the mortality rate decreased in all age groups, except for that of 80 years and over (Chart 4-8). 142142. Nóbrega AA, Araújo WN, Vasconcelos AMN. Mortality Due to Chagas Disease in Brazil According to a Specific Cause. Am J Trop Med Hyg. 2014;91(3):528-33. doi: 10.4269/ajtmh.13-0574.
• In a retrospective cohort study, probabilistic linkage was used to identify among blood donors from 1996 to 2000 (2842 seropositive and 5684 seronegative for ChD) those who died until 2010. 145145. Capuani L, Bierrenbach AL, Alencar AP, Mendrone A Jr, Ferreira JE, Custer B, Ribeiro ALP, Sabino EC. Mortality Among Blood Donors Seropositive and Seronegative for Chagas Disease (1996-2000) in São Paulo, Brazil: A Death Certificate Linkage Study. PLoS Negl Trop Dis. 2017;11(5):e0005542. doi: 10.1371/journal.pntd.0005542. The authors identified 159 deaths among the 2842 seropositive blood donors (5.6%) and 103 deaths among the 5684 seronegative blood donors (1.8%). Chagas seropositive donors had a 2.3 times higher risk of death due to all causes (95% CI, 1.8-3.0) than seronegative donors. Among seropositive donors, only 26 had the ICD-10 code indicating ChD as the underlying cause of death (B57.0/B57.5). 145145. Capuani L, Bierrenbach AL, Alencar AP, Mendrone A Jr, Ferreira JE, Custer B, Ribeiro ALP, Sabino EC. Mortality Among Blood Donors Seropositive and Seronegative for Chagas Disease (1996-2000) in São Paulo, Brazil: A Death Certificate Linkage Study. PLoS Negl Trop Dis. 2017;11(5):e0005542. doi: 10.1371/journal.pntd.0005542. The authors concluded that ChD is an underreported cause of death in the Brazilian mortality database.
• Ayub-Ferreira et al . compared the mechanism of death in HF due to ChCM with that of other etiologies in a prospective clinical trial, the REMADHE trial, which included patients aged 18 years or older with irreversible chronic HF of at least 6 months and left ventricular ejection fraction of less than 50%. Of the 342 patients analyzed, 185 (54.1%) died. Death occurred in 56.4% of ChD patients and in 53.7% of non-ChD patients. Of all ChD group deaths, 48.4% were related to HF worsening, 25.7% to sudden death, and 6.4% to stroke. The cumulative incidence of all-cause mortality and HF mortality was significantly higher in ChD patients as compared to non-ChD patients. 146146. Ayub-Ferreira SM, Mangini S, Issa VS, Cruz FD, Bacal F, Guimarães GV, Chizzola PR, Conceição-Souza GE, Marcondes-Braga FG, Bocchi EA. Mode of Death on Chagas Heart Disease: Comparison With Other Etiologies. A Subanalysis of the REMADHE Prospective Trial. PLoS Negl Trop Dis. 2013;7(4):e2176. doi: 10.1371/journal.pntd.0002176. There was no difference in the cumulative incidence of sudden death mortality between the two groups. In severe Chagas heart disease, progressive HF is the most important mechanism of death.
• In the Bambuí Cohort Study, a large population-based cohort study of elderly residing in an area where ChD is endemic, 1479 subjects aged 60 years and over (38.1% positive T. cruzi test) were followed up from 1997 to 2007. During a mean 8.72-year follow-up, 567 participants died. T. cruzi infection was a predictor of mortality among cohort members, and this association remained largely significant after adjustments for age, sex, and conventional cardiovascular risk factors (HR = 1.56; 95% CI, 1.32-1.85). Overall, the PAR for mortality due to T. cruzi infection was 13.2% (95% CI, 9.8-16.4). 147147. Lima-Costa MF, Peixoto SV, Ribeiro ALP. Chagas Disease and mortality in Old Age as an Emerging Issue: 10 Year Follow-Up of the Bambuí Population-Based Cohort Study (Brazil). Int J Cardiol. 2010;145(2):362-3. doi: 10.1016/j.ijcard.2010.02.036.
• Nadruz et al . studied the temporal trends in PAR of ChCM for 2-year mortality among patients with HF enrolled in 2002-2004 (era 1) and in 2012-2014 (era 2) in a Brazilian university hospital. They prospectively studied 362 (15% with ChCM) and 582 (18% with ChCM) HF patients with ejection fraction ≤50% in eras 1 and 2, respectively, and estimated the PAR of ChCM for 2-year mortality. Although the absolute death rates decreased over time in the ChCM and NChC groups, the PAR of ChCM for mortality increased among patients with HF [PAR(era 1)= 11.0 (95% CI, 2.8-18.5%); PAR(era 2)= 21.9 (95% CI, 16.5-26.9)%; p=0.023 versus era 1], driven by increases in the HR associated with ChD. 148148. Nadruz W Jr, Gioli-Pereira L, Bernardez-Pereira S, Marcondes-Braga FG, Fernandes-Silva MM, Silvestre OM, Sposito AC, Ribeiro ALP, Bacal F, Fernandes F, Krieger JE, Mansur AJ, Pereira AC. Temporal Trends in the Contribution of Chagas Cardiomyopathy to Mortality Among Patients With Heart Failure. Heart. 2018;104(18):1522-1528. doi: 10.1136/heartjnl-2017-312869.
• In a cohort study, 298 ChD patients were followed up from March 1995 to September 2019 in the municipality of Virgem da Lapa, located in the state of Minas Gerais, Brazil. In the 24-year study period, 113 (37.9%) deaths were recorded in the cohort, 107 (35.9%) of which were attributed to heart disease: only 10 (11.6%) occurred in the 86 patients without cardiomyopathy, 49 (31.4%) in the 156 patients with cardiomyopathy, and 48 (85.7%) in the 56 patients with left ventricle aneurysm. The risk of death was 7.4 times significantly higher in patients with left ventricle aneurysms. 149149. Borges-Pereira J, Coura JR, Zauza PL, Pirmez C, Xavier SS. Chagas Disease in Virgem da Lapa, Minas Gerais, Brazil: Left Ventricle aneurysm and the Risk of Death in the 24-Year Interval. Mem Inst Oswaldo Cruz. 2020;115:e200056. doi: 10.1590/0074-02760200056.
• In a cohort study that followed up 1637 ChD patients residing in 21 municipalities in which ChD is endemic, for two years, 205 (12.5%) patients showed new cardiovascular events, 134 of whom (8.2%) died, 28 (1.7%) developed atrial fibrillation, and 43 (2.6%) required pacemaker implantation. Individuals living in municipalities with a larger rural population had protection against cardiovascular events (OR = 0.5; 95% CI, 0.4-0.7), while those residing in municipalities with fewer physicians per 1000 inhabitants (OR = 1.6; 95% CI, 1.2-2.5) and those living in municipalities with lower primary health care coverage (OR = 1.4; 95% CI, 1.1-2.1) had higher chances of experiencing cardiovascular events. 150150. Ferreira AM, Sabino ÉC, Oliveira LC, Oliveira CDL, Cardoso CS, Ribeiro ALP, Damasceno RF, Nunes MDCP, Haikal DSA. Impact of the Social Context on the Prognosis of Chagas Disease Patients: Multilevel Analysis of a Brazilian Cohort. PLoS Negl Trop Dis. 2020;14(6):e0008399. doi: 10.1371/journal.pntd.0008399.
• In a cohort study including 1551 patients with ChCM from the state of Minas Gerais, Brazil, a score to predict 2-year mortality was developed. The score included simple variables, such as age, New York Heart Association functional class, heart rate, QRS duration, and abnormal NT-proBNP adjusted by age. The observed mortality rates in the low-, intermediate-, and high-risk groups were 0%, 3.6%, and 32.7%, respectively, in the derivation cohort, and 3.2%, 8.7%, and 19.1%, respectively, in the validation cohort, with C statistics of 0.82 and 0.71, respectively. It seems to be a helpful and simple score that could be used in remote areas with limited technological resources. 151151. Oliveira CL, Nunes MCP, Colosimo EA, de Lima EM, Cardoso CS, Ferreira AM, de Oliveira LC, Moreira CHV, Bierrenbach AL, Haikal DSA, Peixoto SV, Lima-Costa MF, Sabino EC, Ribeiro ALP. Risk Score for Predicting 2-Year Mortality in Patients With Chagas Cardiomyopathy From Endemic Areas: SaMi-Trop Cohort Study. J Am Heart Assoc. 2020;9(6):e014176. doi: 10.1161/JAHA.119.014176.
Burden of Disease
In the GBD Study 2019, 174 194 DALYs (95% UI, 109 039-302 974) due to ChD were estimated in Brazil, with a relative reduction of 32.1% as compared to that of 1990 (256 380 DALYs, 95% UI, 81 697-328 720). Age-standardized DALY rates declined at national level (-70.5%) and in all Brazilian FUs between 1990 and 2019, but with different regional patterns ( Chart 4-9 ). The decrease in the DALY rates was driven primarily by a consistent reduction in the YLL rates, the main component of total DALYs for ChD. The highest fatal and non-fatal burden due to ChD was observed among males, the elderly, and in the Brazilian FUs encompassing important endemic areas of vectorial transmission in the past, such as the states of Goiás, Tocantins, Minas Gerais, Bahia, and the Distrito Federal. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Age-standardized rates of DALYs due to Chagas disease, per 100 000 population, in Brazil, in 2016. Source: Martins-Melo et al. 144144. Martins-Melo FR, Ramos AN Jr, Alencar CH, Lange W, Heukelbach J. Mortality of Chagas’ disease in Brazil: Spatial Patterns and Definition of High-Risk Areas. Trop Med Int Health. 2012;17(9):1066-75. doi: 10.1111/j.1365-3156.2012.03043.x.
Heart Failure
• Because HF is not considered an underlying cause of death (i.e., garbage code) in the GBD study, all deaths attributed to HF in death certificates are reclassified and/or redistributed to other causes, according to the GBD method. As such, there is no data from GBD on mortality from HF. Because HF is classified by GBD as an “impairment”, the only indicators we have for HF from the GBD are prevalence and YLDs, which is the morbidity component of DALYs.
Prevalence and Incidence
• According to the GBD Study 2017 estimates, age-standardized prevalence of HF changed in Brazil from 818 (95% UI, 718-923) in 1990 to 772 (95% UI, 680-875) in 2017, with a decrease of 5% (95% UI, -7.1 to -3) in the period (Table 4-9). In absolute numbers, estimates for the prevalence of HF in Brazil rose from 0.67 million in 1990 to almost 1.7 million in 2017, mainly due to population growth and aging. The prevalence of HF is variable amongst Brazilian FUs, and the percentage of change varied unevenly between 1990 and 2017 (Table 4-9). In 2017, the highest rates were observed in the state of Rio Grande do Norte, and the lowest, in the state of Acre. From 1990 to 2017, decreased age-standardized prevalence rates were observed in most FUs, and increases in rates occurred in 8 FUs, mostly in the Northeastern region. 152152. Global Burden of Disease Study 2017 (GBD 2017) results. Global Health Data Exchange website. Seattle, WA: Institute for Health Metrics and Evaluation (IHME), University of Washington; 2017. [cited 2021 Nov 09]. Available From: http://ghdx.healthdata.org/g .
http://ghdx.healthdata.org/g...
• Table 4-10 depicts HF prevalence according to sex and age groups, from the GBD Study 2017 estimates. HF prevalence was higher in women (795; 95% UI, 694-901) than in men (751; 95% UI, 656-845) in 2017, and the reduction in prevalence from 1990 to 2017 was more pronounced in men [the percentage of decrease was 7.5 (95% UI, -10.2 to -4.8) for men and 3.2 (95% UI, -6.5 to -0.1) for women]. Regarding age groups, there is a 10-fold increase in the incidence rates from the ‘15-49 years’ group to the ‘50-69 years’ group, as well a 6-fold increase from the latter to the ‘70+ years’ group, and these increases are similar for women and men. From 1990 to 2017, the prevalence increased only in the ‘15-49 years’ group, while decreased in the others, probably associated with increased ischemic events in that age group. 152152. Global Burden of Disease Study 2017 (GBD 2017) results. Global Health Data Exchange website. Seattle, WA: Institute for Health Metrics and Evaluation (IHME), University of Washington; 2017. [cited 2021 Nov 09]. Available From: http://ghdx.healthdata.org/g .
http://ghdx.healthdata.org/g...
• A systematic review evaluated the burden of HF in Latin America and included 143 articles published between January 1994 and June 2014, with at least 50 participants aged ≥ 18 years; most studies included (64%) were from Brazil. 153153. Ciapponi A, Alcaraz A, Calderón M, Matta MG, Chaparro M, Soto N, Bardach A. Burden of Heart Failure in Latin America: A Systematic review and Meta-Analysis. Rev Esp Cardiol. 2016;69(11):1051-60. doi: 10.1016/j.rec.2016.04.054. The patients’ mean age was 60±9 years, and the mean ejection fraction was 36±9%. The prevalence of HF was 1% (95% CI, 0.1-2.7). Of the studies included, only one assessed incidence, with 1091 individuals identified through multistage probability sampling in the city of Porto Alegre, Brazil. The mean age was 42.8±16.9 years, and 55% were women. The incidence of HF in the single population study providing this information was 199 cases per 100 000 person-years. 154154. Moraes RS, Fuchs FD, Moreira LB, Wiehe M, Pereira GM, Fuchs SC. Risk Factors for Cardiovascular Disease in a Brazilian Population-Based Cohort Study. Int J Cardiol. 2003;90(2-3):205-11. doi: 10.1016/s0167-5273(02)00556-9.
• In a population-based study in primary care of a medium-sized city in Brazil, 633 individuals aged ≥45 years were randomly selected and registered in a primary care program of a medium-sized city in Brazil. The mean age was 59.6±10.4 years, and 62% were females; the prevalence of symptomatic HF (stage C) was 9.3%, and the prevalence of stage B HF (structural abnormalities) was 42.7%. Of the patients with HF, 59% presented with HF-PEF and 41%, with HF-REF. 155155. Jorge AL, Rosa ML, Martins WA, Correia DM, Fernandes LC, Costa JA, Moscavitch SD, Jorge BA, Mesquita ET. The Prevalence of Stages of Heart Failure in Primary Care: a Population-Based Study. J Card Fail. 2016;22(2):153-7. doi: 10.1016/j.cardfail.2015.10.01.
https://doi.org/10.1016/j.cardfail.2015....
• A study from the Brazilian National Health Survey held in 2013, with data on 59 655 adults (≥ 18 years), found a prevalence of self-rated HF of 1.1%, which would represent about 1.7 million people. In those aged over 60 years, the prevalence was 3.3%. 156156. Nogueira IDB, Nogueira PAMS, Fonseca AMC, Santos, TZM, Souza DE, Ferreira GMH. Prevalência de Insuficiência Cardíaca e Associação com Saúde Autorreferida no Brasil: Pesquisa Nacional de Saúde – 2013. Acta Fisiátrica. 2019;26(2):95-101. doi: 10.11606/issn.2317-0190.v26i2a164952
• Another population-based study of residents in Zona da Mata, state of Minas Gerais, involved 7113 frail elderly. The mean age was 72.4 ± 8.0 years, 67.6% were women, and the prevalence of HF was 7.9%. 157157. Fochat RC, Polonini HC, Barbosa SEM, Chicourel EL, Raposo NRB. Prevalence of Major Public Health Impact Diseases Among Frail Elderly Residents in the Zona da Mata region in the State of Minas Gerais. Rev APS. 2016;19(2):268-76.
• In a study that included 166 patients from the rural area of Valença, state of Rio de Janeiro, the mean age was 61±14 years, and 51% were men. The main etiologies were hypertensive and ischemic, and 51% of the patients had HF-REF, showing characteristics similar to those of cohorts from non-rural tertiary centers. 158158. Balieiro HM, Osugue RK, Rangel SP, Brandão R, Balieiro TL, Bernardez S, Mesquita ET. Clinical and Demographic Profile and Quality Indicators for heart Failure in a Rural Area. Arq Bras Cardiol. 2009;93(6):637-42. doi: 10.1590/s0066-782x2009001200020.
Mortality
• In a study evaluating data from the SIM, from 2008 to 2012, HF was a frequently used garbage code in Brazil. It was listed as the underlying causes of death in 123 268 (3.7%) of those records and as a multiple cause of death in 233 197 (7%). By using two redistribution methods to specific causes of death, only 38.7-44.8% could be reclassify to a defined cause of death with the principal diagnosis, depending on the reclassification method. 159159. Bierrenbach AL, Alencar GP, Martinez C, Souza M de FM de, Policena GM, França EB. Redistribution of Heart Failure Deaths Using Two Methods: Linkage of Hospital Records With Death Certificate Data and Multiple Causes of death data. Cad Saude Publica. 2019;35(5):e00135617. doi:10.1590/0102-311x00135617. Although HF should not be considered the underlying cause of deaths and rather be in the chain of events that led to death, any analysis of SIM data that uses HF as the underlying cause of death from death certificates must be interpreted with caution, because it may be wrongly estimating the true burden of HF.
• Data obtained from the SEADE for mortality in the state of São Paulo in 2006 evaluated 242 832 deaths in estimated 41 654 020 inhabitants. 135135. Bocchi EA. Heart Failure in South America. Curr Cardiol Rev. 2013;9(2):147-56. doi: 10.2174/1573403x11309020007. Heart failure and etiologies associated with HF (except primary valvular disease) were responsible for 6.3% of the total deaths. For these data, there was neither distribution nor reclassification of the underlying causes of death, and all etiologies associated with HF were included when considering the impact of HF on total mortality.
• A study of mortality due to HF in three states of Brazil (Rio de Janeiro, São Paulo, and Rio Grande do Sul) included data from 2 960 857 death certificates from 1999 to 2005. The percentages of deaths due to HF were 3.0% in the restricted form (HF as the underlying cause of death) and 9.0% in the comprehensive form (HF mentioned in any line of the death certificate) in 1999. The percentages decreased over time and were 2.4% and 8.6%, respectively, in 2005. The mortality rates decreased in most age groups, except for the group aged 80 years or older. The rates increased with age and were clearly higher among men up to 80 years of age. 160160. Gaui EN, Klein CH, Oliveira GM. Mortality due to Heart Failure: Extended Analysis and Temporal Trend in Three States of Brazil. Arq Bras Cardiol. 2010;94(1):55-61. doi: 10.1590/s0066-782x2010000100010.
• A Brazilian cohort study showed data of 1220 outpatients in a specialized HF clinic followed up for 26±26 months from 1991 to 2000. Patients were in functional classes III and IV, had a mean age of 45.5±11 years, and 78% were men. The main etiologies were dilated cardiomyopathy (37%), ChD (20%), and ischemic cardiomyopathy (17%). In the follow-up period of 26±26 months, 415 (34%) patients died, and 71 (6%) patients underwent heart transplantation. Chagas disease was a predictor of poor prognosis. 161161. Freitas HF, Chizzola PR, Paes AT, Lima AC, Mansur AJ. Risk Stratification in a Brazilian Hospital-Based Cohort of 1220 Outpatients With Heart Failure: Role of Chagas’ Heart Disease. Int J Cardiol. 2005;102(2):239-47. doi: 10.1016/j.ijcard.2004.05.025.
• More recent data from 700 consecutive patients with HF-REF from the outpatient clinic of a tertiary health center in São Paulo, Brazil, showed 1-year mortality of 6.8% (47 patients). The composite outcome of death and hospitalization was 17.7% (123 patients) and 1% (7 patients) underwent heart transplantation. The patients’ mean age was 55.4±12.2 years, and 67% were men. The main etiologies were hypertensive (26.0%), ischemic (21.9%), and Chagasic (17.0%) forms of cardiomyopathy. High levels of blood urea nitrogen and brain natriuretic peptide, as well as low systolic blood pressure, were independent predictors of 1-year overall mortality in this sample. 162162. Gioli-Pereira L, Marcondes-Braga FG, Bernardez-Pereira S, Bacal F, Fernandes F, Mansur AJ, Pereira AC, Krieger JE. Predictors of One-Year Outcomes in Chronic Heart Failure: The Portrait of a Middle Income Country. BMC Cardiovasc Disord. 2019;19(1):251. doi: 10.1186/s12872-019-1226-9.
• In a study reporting data from a National Database of Multisite Pacemaker including 3526 patients from 2002 to 2007 cared for at the SUS, the patients’ mean age was 59.8±13.3 years, and 66% were men. The overall survival of patients submitted to cardiac resynchronization therapy in Brazil was 80.1% (95% CI, 79.4–80.8) in 1 year and 55.6% (95% CI, 54.6–56.6) in 5 years, whereas the median overall survival was 30.3 months (IQR, 16.1–50.9). Furthermore, improved survival was observed in the cohort studied, from 2002 throughout 2007 (p=0.055). 163163. Abreu CD, Xavier RM, Nascimento JS, Ribeiro ALP. Long-Term Outcome After Cardiac Resynchronization Therapy: A Nationwide Database. Int J Cardiol. 2012;155(3):492-3. doi: 10.1016/j.ijcard.2011.12.083.
Hospitalizations
• Hospital admissions are the main consequences of decompensated HF, resulting in worse prognosis and increasing costs. The BREATHE Study evaluated a sample of patients admitted due to acute decompensated HF. A total of 1263 patients were included from 51 centers from different Brazilian regions in 2011 and 2012. In-hospital mortality was 12.6%, and care quality indicators based on hospital discharge recommendations were reached in less than 65% of the patients. 164164. Albuquerque DC, Souza Neto JD, Bacal F, Rohde LE, Bernardez-Pereira S, Berwanger O, Almeida DR; Investigadores Estudo BREATHE. I Brazilian Registry of Heart Failure - Clinical Aspects, Care Quality and Hospitalization Outcomes. Arq Bras Cardiol. 2015;104(6):433-42. doi: 10.5935/abc.20150031.
• Other studies reporting mortality rates before the BREATHE Study 165165. Tavares LR, Victer H, Linhares JM, de Barros CM, Oliveira MV, Pacheco LC, Viana CH, Pereira SB, Silva GP, Mesquita ET. Epidemiology of Decompensated Heart Failure in the City of Niterói: EPICA - Niterói Project. Arq Bras Cardiol. 2004;82(2):125-8. doi: 10.1590/s0066-782x2004000200003. , 166166. Wajner A, Zuchinali P, Olsen V, Polanczyk CA, Rohde LE. Causes and Predictors of in-Hospital Mortality in Patients Admitted With or for Heart Failure at a Tertiary Hospital in Brazil. Arq Bras Cardiol. 2017;109(4):321-30. doi: 10.5935/abc.20170136. showed similar rates of in-hospital mortality, ranging from 9% to 17%. 165165. Tavares LR, Victer H, Linhares JM, de Barros CM, Oliveira MV, Pacheco LC, Viana CH, Pereira SB, Silva GP, Mesquita ET. Epidemiology of Decompensated Heart Failure in the City of Niterói: EPICA - Niterói Project. Arq Bras Cardiol. 2004;82(2):125-8. doi: 10.1590/s0066-782x2004000200003.
• In a comparison of decompensated HF patients in tertiary care teaching hospitals in Brazil and in the US, US patients were older (p < 0.01) and had higher prevalence of the ischemic etiology (p < 0.01). Length-of-stay was significantly shorter (5 [IQR, 3-9] vs. 11 [IIQ, 6-19] days; p < 0.001) and in-hospital mortality was lower (2.4% vs. 13%; p < 0.001) in the US cohort, but fewer clinical events within 3 months after discharge were observed in the Brazilian patients (42% vs. 54%; p = 0.02). That study highlights the importance of improving knowledge about HF in Brazilian patients to improve care and outcomes. 167167. Rohde LE, Clausell N, Ribeiro JP, Goldraich L, Netto R, William Dec G, DiSalvo TG, Polanczyk CA. Health Outcomes in Decompensated Heart Failure: A Comparison of Tertiary Hospitals in Brazil and United States. Int J Cardiol. 2005;102:71-7. doi: 10.1016/j.i.
• In the previously cited systematic review that evaluated the burden of HF in Latin America (64% included studies from Brazil), 153153. Ciapponi A, Alcaraz A, Calderón M, Matta MG, Chaparro M, Soto N, Bardach A. Burden of Heart Failure in Latin America: A Systematic review and Meta-Analysis. Rev Esp Cardiol. 2016;69(11):1051-60. doi: 10.1016/j.rec.2016.04.054. the hospital admission rates were 33%, 28%, 31%, and 35% at 3, 6, 12, and 24 to 60 months of follow-up, respectively. The median hospital length of stay was 7.0 [IQR, 5.20-11.00] days. In-hospital mortality was 11.7% (95% CI, 10.4%-13.0%), and the rate was higher in patients with a reduced ejection fraction, ischemic heart disease, or ChD. The 1-year mortality rate was 24.5% (95% CI, 19.4-30.0).
• Using data from the SUS, the numbers of hospitalizations and deaths due to HF were described in São Paulo, Brazil, from 1992 to 2010. The in-hospital mortality rate due to HF was 15%. Comparing the 1992-1993 and 2008-2009 periods, there was a 32% decrease in the number of hospitalizations due to HF (p = 0.002), a 15% increase in mortality (p = 0.004), and increased hospital length of stay due to HF (from 8.8 to 11.3 days, p = 0.001). 168168. Godoy HL, Silveira JA, Segalla E, Almeida DR. Hospitalization and Mortality Rates for Heart Failure in Public Hospitals in São Paulo. Arq Bras Cardiol. 2011;97(5):402-7. doi: 10.1590/s0066-782x2011005000096.
• Another study with data from the DATASUS evaluated HF admissions over a 10-year period (2007 to 2016) in Brazil as compared to those in the state of Rio Grande do Sul and in the city of Porto Alegre (a city with several referral centers). As depicted in Chart 4-10, that study showed a decline in in-hospital mortality rates from 2007 to 2016, in both Brazil (19% decline) and the state of Rio Grande do Sul (25% decline), and a more pronounced decline in the city of Porto Alegre (65%). 169169. Nicolao CZ, Ferreira JB, Paz AA, Linch GFC, Rover M, Souza EN. Heart Failure: An Overview of Morbidity and Mortality in Rio Grande do Sul. Int J Cardiovac Sci. 2019;32(6):596-604. doi: 10.5935/2359-4802.20190032.
• In 2020, a more recent study with data from the DATASUS evaluating HF admissions between 2008 and 2017 in Brazil, described 51 172 HF hospitalizations in the period, representing the main cause of hospitalizations for cardiovascular diseases (29.4%). Similarly to the study mentioned above, this study showed a reduction in hospitalizations in the period (34%; p = 0.004). When stratified by age, individuals aged over 60 years accounted for 73% of all cases of HF hospitalization in Brazil. The mortality rate due to HF between 2008 and 2015 was 14.0 per 100 000 (± 0.53), with a 7.7% reduction in the observed period. 170170. Fernandes ADF, Fernandes GC, Mazza MR, Knijnik LM, Fernandes GS, Vilela AT, Badiye A, Chaparro SV. A 10-Year Trend Analysis of Heart Failure in the Less Developed Brazil. Arq Bras Cardiol. 2020;114(2):222-31. doi: 10.36660/abc.20180321.
Burden of Disease
• According to the GBD 2017 estimates (Table 4-11), the age-standardized YLD rates due to HF were 112 (95% UI, 83-141) in 1990 and 109 (95% UI, 81-134) in 2017, per 100 000 inhabitants, corresponding to a decrease of 3% (95% UI, -6.7 to 0.3). These changes are similar to the observed in the HF prevalence rates. Despite this decrease in YLD rates, HF resulted in 88 114 (95% UI, 64 078-112 624) DALYs in Brazil in 1990 and in 234 169 (95% UI, 174 338-291 188) in 2017, due to population growth and aging. 152152. Global Burden of Disease Study 2017 (GBD 2017) results. Global Health Data Exchange website. Seattle, WA: Institute for Health Metrics and Evaluation (IHME), University of Washington; 2017. [cited 2021 Nov 09]. Available From: http://ghdx.healthdata.org/g .
http://ghdx.healthdata.org/g...
• Table 4-12 shows YLD rates due to HF according to sex and by age groups, from the GBD Study 2017 estimates. The age-standardized YLD rates were similar in women and men in 1990, but the 2017 rates were 105 (95% UI, 82-127) for men and 111 (95% UI, 80-1416) for women, due to a 6.8% reduction (95% UI, 110.9 to -2.6) for men as compared to almost no reduction for women (-0.3%; 95% CI, -4.9 to 4.2). As expected, the highest YLD rate was observed in the ‘70+ years’ group, followed by the ‘50-69 years’ group. Similarly to the changes observed in prevalence, from 1990 to 2017, the greatest YLD increases were observed in the ‘15-49 years’ group. 152152. Global Burden of Disease Study 2017 (GBD 2017) results. Global Health Data Exchange website. Seattle, WA: Institute for Health Metrics and Evaluation (IHME), University of Washington; 2017. [cited 2021 Nov 09]. Available From: http://ghdx.healthdata.org/g .
http://ghdx.healthdata.org/g...
Health Care Utilization and Cost
(Refer to Tables 1-6 through 1-9 and Charts 1-15 through 1-1 6)
• According to data from the SUS, there were 3 085 359 hospitalizations due to HF from 2008 to 2019. This number represents one-third of total clinical admissions related to cardiovascular conditions in the period studied. Unadjusted costs were R$ 3 957 126 308. In international dollars, adjusted total values converted to purchasing power parity for 2019US$ were $ 2 651 479 951. 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
• During the period observed, there was a reduction in the number of clinical admissions due to HF from 298 474 (157 per 100 000) in 2008 to 222 620 (105 per 100 000) in 2019, with an even reduction over the years. Despite that reduction in the number of admissions, unadjusted healthcare expenditure estimates from the direct payment for the care of HF patients increased from 2008 to 2019 by almost 32%, from R$ 272 280 662 (2019 Int$ 267 102 469) in 2008 to R$ 359 301 691 (2019 Int$ 173 659 589) in 2019. The decreased number of admissions and increased expenditure represent higher costs per admission throughout the observed period (R$ 912 in 2008 to R$ 1568 in 2018). Heart failure accounted for most costs related to clinical admissions due to cardiovascular diseases.
• The economic burden of HF in Brazil was assessed using the standard cost of illness framework in 2015. The analysis assessed the prevalence and associated expenditures on healthcare treatment, productivity losses from reduced employment, costs of providing formal and informal care, and lost wellbeing. The study found that HF imposes a financial cost of R$ 22.1 billion/US$ 6.8 billion, the second out of four major heart conditions in Brazil: myocardial infarction, HF, hypertension, and atrial fibrillation. 124124. Stevens B, Pezzullo L, Verdian L, Tomlinson J, George A, Bacal F. The Economic Burden of Heart Conditions in Brazil. Arq Bras Cardiol. 2018;111(1):29-36. doi: 10.5935/abc.20180104.
• In the study by Nicolao et al ., 169169. Nicolao CZ, Ferreira JB, Paz AA, Linch GFC, Rover M, Souza EN. Heart Failure: An Overview of Morbidity and Mortality in Rio Grande do Sul. Int J Cardiovac Sci. 2019;32(6):596-604. doi: 10.5935/2359-4802.20190032. the DATASUS data on HF admissions over a 10-year period (2007 to 2016) showed a 97% increase in the mean per-patient cost of HF-related hospitalizations from 2007 to 2016. Data from the city of Porto Alegre (a city with several referral hospitals) showed an even more pronounced increase (135%), but also a more pronounced decrease in mortality as compared to overall data of Brazil (see above).
Open Heart Transplantation and Assist Device Placement
• The number of heart transplantations performed in Brazil increased from 149 in 2006 to 357 in 2016. Although the number of heart transplantations increased significantly in that period, it represents approximately one-fifth of the estimated population need. The 1-year survival was 73% (data for survival collected from 2010). 171171. Registro Brasileiro de Transplantes. Dimensionamento dos transplantes no Brasil e em cada estado (2009-2016). São Paulo: Associação Brasileira de Transplante de Órgãos; 2016.
• An analysis of cost for heart transplantation in Brazil, of all consecutive heart transplant recipients at a single center from July 2015 to June 2017, showed an average total cost for the 27 patients included of US$ 74 341, which is lower than those reported for developed countries, but exceeds the reimbursement value per patient by 60%. 172172. Goldraich LA, Neyeloff JL, Etges APBS, Zeilmann LG, Hastenteufel LT, Ghisleni EC, Clausell N. Heart Transplantation Cost Composition in Brazil: A Patient-Level Microcosting Analysis and Comparison With International Data. J Card Fail. 2018;24(12):860-3. doi: 10.1016/j.cardfail.2018.10.011.
• In a descriptive study of a public reference hospital in cardiology, located in the city of Fortaleza, Brazil, 16 patients were submitted to ventricular assist device implantation from 2008 to 2015. Mean age was 40.1 ± 3.4 years, and 87.5% were men. Chagas heart disease was the main etiology (37.5%). All patients experienced complications during the use of the device, bleeding being the most frequent (11 [68.8%]). Regarding the clinical outcome, 10 patients (62.5%) underwent cardiac transplantation and 5 patients (31.3%) died. 173173. Cestari V, Pessoa VL, Souza Neto JD, Moreira T, Florêncio R, Vasconcelos GG, Souza L, Braga A, Sobral MG. Clinical Evolution of Patients Using Ventricular Assist Devices as a Bridge for Transplantation. Transplant Proc. 2018;50(3):796-803. doi: 10.1016/j.transproceed.2018.02.014.
Future Research
• Because HF is considered a garbage code when assigned as the underlying cause of death, studies investigating the better method to reclassify and redistribute this cause are needed to reduce bias and promote better data comparability to enhance health policies.
• Brazilian cohort studies for cardiomyopathies are scarce, and some clinical studies in Brazil reported HF data, but there are few multicenter studies with Brazilian population data. It is worth noting the importance of having data for both HF and cardiomyopathy and for both outpatients and hospitalized ones, in addition to fully understanding the increasing burden of HF on cardiovascular diseases. More multicenter large-scale studies are needed to better describe the burden, outcomes, and costs of HF in the Brazilian population.
• In addition, studies exploring quality of care and costs in HF would help develop health policies to improve awareness, access to life-saving interventions, organ donation, and the better use of resources in this complex and demanding disease.
• Mortality rates due to ChD decreased substantially in the last decades and they are expected to continue to decline in the coming years. Indeed, there is evidence that ChD is an underreported cause of death, and, probably, of hospitalization as well. More data on the hospitalization rates and outcomes in ChCM patients are needed.
5. VALVULAR HEART DISEASE
ICD-9 424; ICD-10 I34 to I38
See Table 5-1 through 5-5 and Charts 5-1 through 5-11
Abbreviations Used in Chapter 5
| AF | Atrial Fibrillation |
| ARF | Acute Rheumatic Fever |
| CABG | Coronary Artery Bypass Graft |
| CAD | Coronary Artery Disease |
| CI | Confidence Interval |
| DALYs | Disability-Adjusted Life Years |
| ECG | Electrocardiogram |
| FU | Federative Unit |
| GBD | Global Burden of Disease |
| HIC | High-Income Countries |
| ICD | International Statistical Classification of Diseases and Related Health Problems |
| IL | Interleukine |
| NRVD | Non-rheumatic Valvular Heart Disease |
| RHD | Rheumatic Heart Disease |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| TAVI | Transcatheter Aortic Valve Implantation |
| UI | Uncertainty Interval |
| YLLs | Years of Life Lost |
– Age-standardized prevalence rates of valvular heart disease per 100 000, in 1990 and 2019, and percent change of rates, in Brazil and its Federative Units.
– Death and DALY rates per 100 000 in 1990 and 2019, and percent change of rates, by age, sex, and cause of death, Brazil.
– Number of deaths, age-standardized mortality rate (per 100 000) in 1990 and 2019, and percent change of rates, by cardiovascular groups of causes of death, in Brazil and its Federative Units.
– Number of DALY, age-standardized DALY rates (per 100 000) in 1990 and 2019, and percent change of rates, by cardiovascular groups of causes of death, in Brazil and its Federative Units.
– Total number of admissions and associated costs in Brazilian Reais (R$) and International Dollars 2019 (Int$) for surgical and clinical procedures to treat valvular heart disease in Brazil, from 2008 to 2019.
– A: Age-standardized and crude prevalence rates of Rheumatic Heart Disease in Brazil from 1990 to 2019. B: Total prevalent cases of Rheumatic Heart Disease in Brazil from 1990 to 2019.
– A: Age-standardized and crude prevalence rates of Non-Rheumatic Valvular Heart Disease in Brazil from 1990 to 2019. B: Number of prevalent cases of Non-Rheumatic Valvular Heart Disease in Brazil from 1990 to 2019.
– A: Age-standardized and crude mortality rates attributable to Rheumatic Heart Disease in Brazil from 1990 to 2019. B: Total number of deaths attributable to Rheumatic Heart Disease in Brazil from 1990 to 2019.
– Correlation between the percent change in age-standardized mortality rates associated with Rheumatic Heart Disease and the Sociodemographic Index (SDI) in the Brazilian Federative Units in 1990 (A) and 2019 (B).
– A: Age-standardized and crude mortality rates attributable to Non-Rheumatic Valvular Heart Disease in Brazil from 1990 to 2019. B: Total number of deaths attributable to Non-Rheumatic Valvular Heart Disease in Brazil from 1990 to 2019.
– Correlation between the age-standardized mortality rates attributable to calcific aortic valve disease and the Sociodemographic Index (SDI) in the Brazilian Federative Units in 1990 (A) and 2019 (B).
– A: Age-standardized death rates attributable to Rheumatic Heart Disease in Brazil and each region from 1990 to 2019. B: Age-standardized DALY rates attributable to Rheumatic Heart Disease in Brazil and each region from 1990 to 2019.
– Correlation between the percent change in DALY rates attributable to Rheumatic Heart Disease from 1990 to 2019 and the Sociodemographic Index (SDI) in the Brazilian Federative Units in 1990 (A) and 2019 (B).
– A: Age-standardized death rates attributable to Non-Rheumatic Valvular Heart Disease in Brazil and each region from 1990 to 2019. B: Age-standardized DALY rates attributable to Non-Rheumatic Valvular Heart Disease in Brazil and each region from 1990 to 2019.
– Correlation between the age-standardized DALY rates attributable to Non-Rheumatic Valvular Heart Disease and the Sociodemographic Index (SDI) in the Brazilian Federative Units in 1990 (A) and 2019 (B).
– Expenses associated with the surgical treatment of cardiovascular diseases in Brazil, according to the type in SUS, from 2008 to 2020 (Currency: International Dollars). 9595. Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
http://tabnet.datasus.gov.br/...
Prevalence
Rheumatic Heart Disease
• According to the Global Atlas on Cardiovascular Disease Prevention and Control, updated by the GBD 2019, RHD is estimated to currently affect about 40.5 million people worldwide, accounting for 1-1.5% (306 000 deaths) of all cardiovascular deaths. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 174174. Thomas H, Diamond J, Vieco A, Chaudhuri S, Shinnar E, Cromer S, Perel P, Mensah GA, Narula J, Johnson CO, Roth GA, Moran AE. Global Atlas of Cardiovascular Disease 2000-2016: The Path to Prevention and Control. Glob Heart. 2018;13(3):143-63. doi: 10.1016/j.gheart.2018.09.511. Until the middle of the 20th century, RHD was the leading cause of heart valve disease in the world. Improved health conditions, early identification of Streptococcus pyogenes infections, and antibiotic use have significantly decreased RHD prevalence in HIC. Published data from 2016 estimate that RHD is the primary cause of 2.5% of valvular heart diseases in the United States and Canada, reaching up to 22% in Europe. 175175. Iung B, Vahanian A. Epidemiology of Acquired Valvular Heart Disease. Can J Cardiol. 2014;30(9):962-70. doi: 10.1016/j.cjca.2014.03.022. Even higher rates have been reported in Brazil, accounting for about 50% of the heart valve surgeries in SUS. 176176. Nascimento BR, Beaton AZ, Nunes MC, Diamantino AC, Carmo GA, Oliveira KK, Oliveira CM, Meira ZM, Castilho SR, Lopes EL, Castro IM, Rezende VM, Chequer G, Landay T, Tompsett A, Ribeiro ALP, Sable C; PROVAR (Programa de RastreamentO da VAlvopatia Reumática) Investigators. Echocardiographic Prevalence of Rheumatic Heart Disease in Brazilian Schoolchildren: Data From the PROVAR study. Int J Cardiol. 2016;219:439-45. doi: 10.1016/j.ijcard.2016.06.088.
• In low- to middle-income countries, the prevalence of RHD remains around 444 per 100 000 inhabitants. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 179179. Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, Forouzanfar MH, Longenecker CT, Mayosi BM, Mensah GA, Nascimento BR, Ribeiro ALP, Sable CA, Steer AC, Naghavi M, Mokdad AH, Murray CJL, Vos T, Carapetis JR, Roth GA. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990-2015. N Engl J Med. 2017;377(8):713-722. doi: 10.1056/NEJMoa1603693. In Brazil, it persists as the main etiology of valvular heart disease, especially in patients from the SUS. Previous evaluations have shown prevalence of 360 per 100 000 in our country. 180180. Alves Meira ZM, de Castilho SR, Lins Barros MV, Maria Vitarelli A, Diniz Capanema F, Moreira NS, Moreira Camargos PA, Coelho Mota CC. Prevalence of rheumatic fever in children From a public high school in Belo Horizonte. Arq Bras Cardiol. 1995;65(4):331-4. Other evaluations have found a prevalence ranging from 100 to 700 per 100 000 schoolchildren. 181181. Tarasoutchi F, Montera MW, Grinberg M, Piñeiro DJ, Sánchez CR, Bacelar AC, Lopes AS, Fernandes JR, Pires LJ, Moraes RC, Accorsi TA, Colafranceschi AS, Kiyose AT, Fiorelli AI, Bacelar AC, Lopes AS, Ramos AI, Boer BN, Abdulmassih Neto C, Sánchez CR, Esteves CA, Weksler C, Piñeiro DJ, Kruczan DD, Rossi EG, Mesquita ET, Brito FS Jr, Bacal F, Bosh F, Urzua FF, Moraes F, Tarasoutchi F, Costa FD, Barbosa GV, Spina GS, Murad H, Hernández HM, Fernandes JR, Mangione JA, Brito JC, Murillo JR, Plana JC, Paganini JJ, Krauss J, Moura LA, Pires LJ, Carvalho LA, Cardoso LF, Katz M, Vieira ML, Montera MW, Barbosa Mde M, Barbosa Mde R, Grinberg M, Villagrán OA, Pomerantzeff PM, Lavitola Pde L, Moraes RC, Leite RE, Sampaio RO, Franco S, Martins SM, Bordignon S, Accorsi TA, David TE, Duré VR, Rossei V, Ávila WS. Brazilian Guidelines for Valve Disease - SBC 2011 / I Guideline Inter-American Valve Disease - 2011 SIAC. Arq Bras Cardiol. 2011;97(Suppl 1):1-67. doi: 10.1590/s0066-782x2011002000001.
https://doi.org/10.1590/s0066-782x201100...
• In Brazil, of 174 patients presenting with acute valvular heart disease to the emergency room at the São Paulo Heart Institute, rheumatic involvement was observed in 60%, followed by degenerative aortic valve disease (15%), and mitral valve prolapse (13%). At total, 27.5% of the patients had isolated mitral regurgitation and 11% had mitral stenosis, with aortic valve disease present in the remaining patients. 182182. Moraes RC, Katz M, Tarasoutchi F. Clinical and Epidemiological Profile of Patients With Valvular Heart Disease Admitted to the Emergency Department. Einstein. 2014;12(2):154-8. doi: 10.1590/s1679-45082014ao3025.
• A recent study in Brazil has shown that the regression rates of valvular heart disease, especially in patients with moderate/severe ARF, may be lower than previously described. Only 22/69 patients had total regression of mitral regurgitation after rheumatic carditis (31.9%). Aortic regurgitation also has a lower total regression rate than those observed in studies prior to the echocardiographic era (18%). However, most cases persisted with mild mitral or residual aortic regurgitation. 183183. Carvalho LMA, Araujo FDR, Meira ZMA. Doppler Echocardiographic Follow-Up of Mitral and Aortic Regurgitation in Children and Adolescents With Subclinical and Mild Rheumatic Carditis. Int J Cardiovasc Sciences. 2017;30(5):391-400. doi: 10.5935/2359-4802.20170065. In another study involving 258 children and adolescents with ARF followed up from 2 to 15 years, valve lesions healed in 25% of the patients with mild carditis, in 2.5% of those with moderate carditis, while no healing was observed in those with severe carditis. 184184. Meira ZM, Goulart EM, Mota C. Comparative Study of Clinical and Doppler Echocardiographic Evaluations of the Progression of Valve Diseases in Children and Adolescents With Rheumatic Fever. Arq Bras Cardiol. 2006;86(1):32-8. doi: 10.1590/s0066-782x2006000100006.
• Regarding disease progression, an echocardiographic risk score for prediction of mid-term outcomes in children with echo-detected RHD has been derived from a Brazilian cohort, 185185. Nunes MCP, Sable C, Nascimento BR, Lima EM, da Silva JLP, Diamantino AC, Oliveira KKB, Okello E, Aliku T, Lwabi P, Colosimo EA, Ribeiro ALP, Beaton AZ. Simplified Echocardiography Screening Criteria for Diagnosing and Predicting Progression of Latent Rheumatic Heart Disease. Circ Cardiovasc Imaging. 2019;12(2):e007928. doi: 10.1161/CIRCIMAGING.118.007928. with good discrimination in a second screening sample in the country 186186. Bechtlufft BM, Nascimento BR, Sable C, Fraga CL, Barbosa MM, Reis SD, Diamantino AC, Meira ZMA, Castilho SRT, Arantes NF, Oliveira KK, Silva JLP, Rezende BF, Costa WAA, Mata MD, Pereira AF, Ribeiro ALP, Beaton AZ, Pereira Nunes MC. Validation of a Simplified Score for Predicting Latent Rheumatic Heart Disease Progression Using a Prospective Cohort of Brazilian Schoolchildren. BMJ Open. 2020;10(5):e036827. doi: 10.1136/bmjopen-2020-036827. (C-statistic=0.71, 95% CI, 0.63 - 0.80) and in pooled cohorts from 3 other countries (C-statistic=0.70, 95% CI, 0.64 - 0.76). Its application may be useful for detecting individuals at higher risk for late sequelae. 187187. Nascimento BR, Nunes MCP, Lima EM, Sanyahumbi AE, Wilson N, Tilton E, Rémond MGW, Maguire GP, Ribeiro ALP, Kazembe PN, Sable C, Beaton AZ; Programa de Rastreamento da Valvopatia Reumática (PROVAR) Investigators. Outcomes of Echocardiography-Detected Rheumatic Heart Disease: Validating a Simplified Score in Cohorts From Different Countries. J Am Heart Assoc. 2021;10(18):e021622. doi: 10.1161/JAHA.121.021622.
• In addition to the echo score, other markers of unfavorable outcomes of latent and clinical RHD (noticeably progression to clinically prevalent disease and the need for valve intervention, respectively) have been evaluated in Brazil. Among individuals with latent RHD, IL-4, IL-8 and IL-1RA seem to be the best predictors of clinical disease. In addition, the co-regulated expression of IL-6 and TNF-α is associated with severe valve dysfunction, whereas high IL-10 and IL-4 levels predicted subsequently adverse outcomes in individuals with established disease. 188188. Soares ACd, Passos LSA, Sable C, Beaton A, Ribeiro VT, Gollob KJ, Dutra WO, Nunes MCP. Circulating Cytokines Predict Severity of Rheumatic Heart Disease. Int J Cardiol. 2019;289:107-9. doi: 10.1016/j.ijcard.2019.04.063.
• In another genetic study comparing samples from individuals with latent and clinical RHD and controls, clinical disease associated with higher levels of all cytokines, IL-4, CXCL8 and IL-1RA being its strongest predictors compared to latent RHD. An association of polymorphisms in IL-2, IL-4, IL-6 and IL-10 genes and clinical RHD was observed, and gene polymorphism and phenotypic expression of IL-4 accurately discriminate latent versus clinical RHD, and may potentially guide clinical management in the future. 189189. Tormin JPAS, Nascimento BR, Sable CA, da Silva JLP, Brandao-de-Resende C, Rocha LPC, Pinto CHR, Neves EGA, Macedo FVB, Fraga CL, Oliveira KKB, Diamantino AC, Ribeiro ALP, Beaton AZ, Nunes MCP, Dutra WO; PROVAR (Programa de RastreamentO da VAlvopatia Reumática) investigators. Cytokine Gene Functional Polymorphisms and Phenotypic Expression as Predictors of Evolution From Latent to Clinical Rheumatic Heart Disease. Cytokine. 2021;138:155370. doi: 10.1016/j.cyto.2020.155370.
• According to the GBD 2019, from 1990 to 2019, the age-standardized prevalence of RHD had a slight 2.1% (95% UI, 0.2 – 4.0) increase, from 899.6 (95% UI, 699.8 – 1119.1) to 918.5 (95% UI, 716 – 1142.5) per 100 000, remaining higher in women than in men in the whole period (Table 5-1 and Chart 5-1.A). Although small for both sexes, the percent increase was numerically more pronounced in women (3.5%) than in men, who had a stable trend (0.1%, 95% UI, -2.4 – 2.8). The percent increases were higher in the states of Alagoas, Bahia, and Sergipe, from the lowest-income Northeastern region. Although the central estimates were higher in these states, the 95% UIs were wide, and overlap with those of other FUs (Table 5-1). 190190. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, Regional, and National Incidence, Prevalence, and Years Lived With Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-858. doi: 10.1016/S0140-6736(18)32279-7.
https://doi.org/10.1016/S0140-6736(18)32...
However, it may be hypothesized that the small increase of RHD prevalence observed in the period may reflect the progress of epidemiological data collection and health statistics, as well as the systematic inclusion of definite subclinical RHD. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• The crude prevalence of RHD, however, increased 6.8% (95% UI, 1.7 – 12.5%) from 1990 to 2019, from 908.8 (95% UI, 699.1 - 1139.4) to 970.2 (95% UI, 756.6 - 1202.9) per 100 000, also remaining higher in women in the whole period (Chart 5-1.B). Similarly to the trend observed for age-standardized prevalence rates, the increase in crude prevalence was more pronounced for women than for men (8.4% vs. 4.2%). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• Even with the relatively stable trends depicted by the GBD 2019 modeling, RHD is the most prevalent cause of mitral valve disease in Brazil according to published data, when both mitral stenosis (over 90%) and mitral regurgitation (about 55-60%) are considered. 182182. Moraes RC, Katz M, Tarasoutchi F. Clinical and Epidemiological Profile of Patients With Valvular Heart Disease Admitted to the Emergency Department. Einstein. 2014;12(2):154-8. doi: 10.1590/s1679-45082014ao3025.
• Mitral stenosis occurs in a much higher frequency in women than in men, in a ratio of 3:2. It is a frequent sequela of ARF, reaching more than 85% of cases even in HIC, such as those in Europe, 191191. Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E, Ravaud P, Vahanian A. A prospective Survey of Patients With Valvular Heart Disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24(13):1231-43. doi: 10.1016/s0195-668x(03)00201-x. with a similar pattern still observed in Brazil. 178178. Ribeiro GS, Tartof SY, Oliveira DW, Guedes AC, Reis MG, Riley LW, Ko AI. Surgery for Valvular Heart Disease: A Population-Based Study in a Brazilian Urban Center. PLoS One. 2012;7(5):e37855. doi: 10.1371/journal.pone.0037855. , 182182. Moraes RC, Katz M, Tarasoutchi F. Clinical and Epidemiological Profile of Patients With Valvular Heart Disease Admitted to the Emergency Department. Einstein. 2014;12(2):154-8. doi: 10.1590/s1679-45082014ao3025. More rarely, mitral stenosis associates with other diseases, such as mitral annulus calcification, mucopolysaccharidosis, rheumatoid arthritis, and congenital carcinoid syndrome. 175175. Iung B, Vahanian A. Epidemiology of Acquired Valvular Heart Disease. Can J Cardiol. 2014;30(9):962-70. doi: 10.1016/j.cjca.2014.03.022. , 182182. Moraes RC, Katz M, Tarasoutchi F. Clinical and Epidemiological Profile of Patients With Valvular Heart Disease Admitted to the Emergency Department. Einstein. 2014;12(2):154-8. doi: 10.1590/s1679-45082014ao3025.
• Recent large-scale screening study looking at subclinical RHD has shown a prevalence of 42 per 1000 in schoolchildren (mean age of 11 years) in the Southeastern state of Minas Gerais: 37 per 1000 borderline RHD and 5 per 1000 definite RHD. In that study, higher prevalence was observed in females (48 per 1000 vs. 35 per 1000) and in children older than 12 years. 176176. Nascimento BR, Beaton AZ, Nunes MC, Diamantino AC, Carmo GA, Oliveira KK, Oliveira CM, Meira ZM, Castilho SR, Lopes EL, Castro IM, Rezende VM, Chequer G, Landay T, Tompsett A, Ribeiro ALP, Sable C; PROVAR (Programa de RastreamentO da VAlvopatia Reumática) Investigators. Echocardiographic Prevalence of Rheumatic Heart Disease in Brazilian Schoolchildren: Data From the PROVAR study. Int J Cardiol. 2016;219:439-45. doi: 10.1016/j.ijcard.2016.06.088. The same project has concluded that primary care centers are the ideal scenario for RHD screening, considering the higher population participation and involvement rates. 192192. Nascimento BR, Sable C, Nunes MCP, Diamantino AC, Oliveira KKB, Oliveira CM, Meira ZMA, Castilho SRT, Santos JPA, Rabelo LMM, Lauriano KCA, Carmo GAL, Tompsett A, Ribeiro ALP, Beaton AZ; PROVAR (Rheumatic Valve Disease Screening Program) Investigators. Comparison Between Different Strategies of Rheumatic Heart Disease Echocardiographic Screening in Brazil: Data From the PROVAR (Rheumatic Valve Disease Screening Program) Study. J Am Heart Assoc. 2018;7(4):e008039. doi: 10.1161/JAHA.117.008039.
• Echo screening in the primary care setting has also been tested as an additional tool, on top of clinical variables, to predict major abnormalities in standard echo (including significant valve disease and RHD) and prioritize referrals in Brazil. The combined score – derived from 603 patients in waiting lists for echocardiography, and validated in a similar sample of 1526 individuals – had good discrimination, with C-statistic = 0.72, sensitivity = 99% and negative predictive value = 97%, and emerges as a promising tool for early diagnosis of valve disease/RHD, estimation of disease burden and priority referrals. 193193. Diamantino AC, Nascimento BR, Nunes MCP, Sable CA, Oliveira KKB, Rabelo LC, Franco J, Diamantino LC, Barbosa MM, Reese AT, Olivieri L, de Lima EM, Martins LNA, Colosimo EA, Beaton AZ, Ribeiro ALP; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática e outras Doenças Cardiovasculares) investigators. Impact of Incorporating Echocardiographic Screening Into a Clinical Prediction Model to Optimise Utilisation of Echocardiography in Primary Care. Int J Clin Pract. 2021;75(3):e13686. doi: 10.1111/ijcp.13686.
• One additional tool for estimating the prevalence of subclinical RHD is artificial intelligence. The machine learning system (Convolutional Neural Network) currently under development in Brazil from screening studies has shown good accuracy (normal=72.8±10.2; borderline RHD=64.3±12.2; and definite RHD=85.8±11.3) and may help broaden the availability of early echocardiographic diagnosis in the future. 194194. Nascimento BR, Martins JFBS, Nascimento ER, Pappa GL, Sable CA, Beaton AZ, Gomes PR, Nunes MC, Oliveira KKB, Franco J, Pereira AFC, Rezende BDF, Mata MDO, AL Ribeiro, Meira W. Deep learning for automatic identification of Rheumatic Heart Disease in Echoca. J Am Coll Cardiol. 2020;75(11):3577.
Non-rheumatic Valvular Heart Disease
• According to the GBD 2019, the age-standardized prevalence of NRVD had a marked increase in Brazil from 1990 to 2019, with a significant 54.3% increase from 25.3 (95% UI, 22.4 - 27.8) per 100 000 in 1990 to 39 (95% UI, 33.9 - 44.6) per 100 000 in 2019. The percent change was considerably higher for men compared to women (105.9% vs. 20.9%) (Chart 5-2.A). The increasing trend was mostly driven by calcific aortic valve disease (201.8%), from 7.9 (95% UI, 6.3 - 9.6) per 100 000 in 1990 to 23.7 (95% UI, 19.1 - 29) per 100 000 in 2019, for both men (218.8%) and women (182.2%). Conversely, for mitral degenerative valve disease the age-standardized prevalence was stable, with a slight percent change: -2.3% (95% UI, -4 to -0.4) (Table 5-1). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• Aligned with age-standardized rates, the crude prevalence of NRVD showed a marked 149.3% (95% UI, 126.7 - 173.3) increase from 1990 [17.6 (95% UI, 15.7 - 19.4)] to 2019 [44 (95% UI, 38.2 - 50.3)] per 100 000 (Table 5-1 and Chart 5-2.B). Again, the increase was more pronounced for men than for women, and the steeper inclination compared to age-standardized rates suggests that prevalence is increasing disproportionally in the elderly (Chart 5-2.B). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• Unlike mitral valve disease, aortic valve disease is predominantly degenerative or calcific. Observational studies show that aortic stenosis is seen in 4.5% of the population >75 years in HIC, such as the United States. 195195. Freeman RV, Otto CM. Spectrum of Calcific Aortic Valve Disease: Pathogenesis, Disease Progression, and Treatment Strategies. Circulation. 2005;111(24):3316-26. doi: 10.1161/CIRCULATIONAHA.104.486738. According to observational studies 182182. Moraes RC, Katz M, Tarasoutchi F. Clinical and Epidemiological Profile of Patients With Valvular Heart Disease Admitted to the Emergency Department. Einstein. 2014;12(2):154-8. doi: 10.1590/s1679-45082014ao3025. , 196196. Grinberg M, Accorsi TA. Aortic stenosis in the elderly: a Brazilian perspective. Arq Bras Cardiol. 2009 Feb;92(2):e9-12. doi: 10.1590/s0066-782x2009000200016. and the GBD 2019 data, 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
in Brazil, as well as in the rest of the world, an increasing trend towards degenerative aortic valve disease has been observed as compared to other etiologies, such as RHD.
• Thus, the increase in all-age prevalence of NRVD has been mostly driven by calcific aortic valve disease [396.6% (95% UI, 353.1 – 450.0)], especially for older age groups (>70 years) (Table 5-2), but increasing trends have been also significant for mitral degenerative valve disease [54.1% (95% UI, 50.4 – 58.0)] and other NRVDs, although data quality remains limited for the latter, despite the improvement of data sources (Table 5-1). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• Contrary to that observed for the rheumatic etiology, there has been an increase in mitral valve prolapse as the etiology of primary mitral regurgitation in Brazil: although in the overall population it reaches rates around 1-2.5%, with good prognosis in most cases, of the patients admitted with valve disease in a Brazilian emergency department in 2009 (56±17 years, 54% female), 13% had that etiology. 181181. Tarasoutchi F, Montera MW, Grinberg M, Piñeiro DJ, Sánchez CR, Bacelar AC, Lopes AS, Fernandes JR, Pires LJ, Moraes RC, Accorsi TA, Colafranceschi AS, Kiyose AT, Fiorelli AI, Bacelar AC, Lopes AS, Ramos AI, Boer BN, Abdulmassih Neto C, Sánchez CR, Esteves CA, Weksler C, Piñeiro DJ, Kruczan DD, Rossi EG, Mesquita ET, Brito FS Jr, Bacal F, Bosh F, Urzua FF, Moraes F, Tarasoutchi F, Costa FD, Barbosa GV, Spina GS, Murad H, Hernández HM, Fernandes JR, Mangione JA, Brito JC, Murillo JR, Plana JC, Paganini JJ, Krauss J, Moura LA, Pires LJ, Carvalho LA, Cardoso LF, Katz M, Vieira ML, Montera MW, Barbosa Mde M, Barbosa Mde R, Grinberg M, Villagrán OA, Pomerantzeff PM, Lavitola Pde L, Moraes RC, Leite RE, Sampaio RO, Franco S, Martins SM, Bordignon S, Accorsi TA, David TE, Duré VR, Rossei V, Ávila WS. Brazilian Guidelines for Valve Disease - SBC 2011 / I Guideline Inter-American Valve Disease - 2011 SIAC. Arq Bras Cardiol. 2011;97(Suppl 1):1-67. doi: 10.1590/s0066-782x2011002000001.
https://doi.org/10.1590/s0066-782x201100...
Conversely, in a hospital registry of heart surgeries in one of the largest capitals of the country (city of Salvador), from 2002 to 2005, only a small proportion of cases was associated with mitral prolapse, 178178. Ribeiro GS, Tartof SY, Oliveira DW, Guedes AC, Reis MG, Riley LW, Ko AI. Surgery for Valvular Heart Disease: A Population-Based Study in a Brazilian Urban Center. PLoS One. 2012;7(5):e37855. doi: 10.1371/journal.pone.0037855. similarly to the results of a study with 78 808 patients utilizing 2 large national databases (the Brazilian Hospital Information System and the Mortality Information System) from 2001 to 2007, in which only 0.24% (187) of the cases reported that undelaying cause. 197197. Xavier RMA, Azevedo VMP, Godoy PH, Migowski A, Ribeiro ALP, Chaves RBM, Correia MG, Xavier CA, Hashimoto LA, Weksler C, Silva NASE. Medium-Term Outcomes of 78,808 Patients after Heart Valve Surgery in a Middle-Income Country: A Nationwide Population-Based Study. BMC Cardiovasc Disord. 2017;17(1):302. doi: 10.1186/s12872-017-0725-9. However, data may be biased by the absence of coding for etiologies of valvular haert disease in the public and most of the private health systems.
Incidence
• According to a study based on in-hospital medical charts in Northeastern Brazil from 2002 to 2005 (1320 surgeries), the mean annual incidence for cardiac valve surgeries was 4.75 per 100 000 residents and positively associated with age. The mean annual incidence of RHD and degenerative valvular disease were 2.86 and 0.73 per 100 000, respectively. 178178. Ribeiro GS, Tartof SY, Oliveira DW, Guedes AC, Reis MG, Riley LW, Ko AI. Surgery for Valvular Heart Disease: A Population-Based Study in a Brazilian Urban Center. PLoS One. 2012;7(5):e37855. doi: 10.1371/journal.pone.0037855.
Rheumatic Heart Disease
• For RHD, the age-specific incidence followed a bimodal distribution according to the source of surgery reimbursement, increasing almost linearly by 1 case per 100 000 population for each decade of life until the age of 40–49 years, peaking at 4.85 cases per 100 000 population. Following a decline, a second peak occurred at 60–69 years of age (6.54 cases per 100 000 population). 178178. Ribeiro GS, Tartof SY, Oliveira DW, Guedes AC, Reis MG, Riley LW, Ko AI. Surgery for Valvular Heart Disease: A Population-Based Study in a Brazilian Urban Center. PLoS One. 2012;7(5):e37855. doi: 10.1371/journal.pone.0037855.
• The incidence of RHD remained stable [percent increase: 0.5% (95% UI, -1.2 - 2.6)] in Brazil, ranging from 53.9 (95% UI, 40.4 - 67.5) per 100 000 (95 299 cases) in 1990 to 54.2 (95% UI, 40.7 - 68.5) per 100 000 (108 204 cases) in 2019, according to GBD 2019 data. This stable trend was relatively homogeneous across the country, with overlapping 95% UIs even in the lower resourced states of the Northern and Northeastern regions. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• In general, a significant reduction in the incidence of RHD was observed in the age group 15 – 49 years [-12.7% (95% UI, -17.2 to -6.8)], while trends were stable in the other age groups. This pattern may be associated with improved disease diagnosis and prevention in younger groups (noticeably 5 – 18 years, the peak of ARF incidence) in past decades, resulting in a lower incidence in teenagers and adults. However, the decrease in the age group 5 – 14 years was not captured by the model, presumably influenced by the lack of data on subclinical RHD prior to 2014. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
Non-Rheumatic Valvular Heart Disease
• In a different pattern as compared to that of RHD, the NRVD age-standardized incidence rates had a significant 11.1% (95% UI, 6.5 - 16.4) increase from 3.6 (95% UI, 3.3 – 4.0) per 100 000 in 1990 to 4.0 (95% UI, 3.6 - 4.5) per 100 000 in 2019, according to the GBD 2019 estimates. This increase was mostly driven by the 20.1% (95% UI, 12.9 - 28.4) increase in calcific aortic valve disease, markedly in individuals aged 50 - 69 years [56.9% (95% UI, 39.8 - 75.6)]. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• However, the aforementioned increasing incidence of calcific aortic valve disease in middle-age individuals [15 – 49 years: 56.9% (95% UI, 39.8 - 75.6)] is atypical, considering the disease epidemiology, and may be cautiously interpreted as a possible limitation of the GBD modeling, 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
, 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
because primary data for this cause are scarce in Brazil. In addition, a non-expected stable pattern in individuals >70 years was modelled. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010.
Mortality
• Valvular heart disease is one of the leading causes of cardiovascular death in Brazil, particularly in economically underserved regions, and RHD – the most socially driven etiology – ranked as the 8th/9thcause in past decades. 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
In the most underserved setting, RHD has been playing an important role for decades, with decreasing trends – not always adequately captured by statistical modeling – following socioeconomic improvement. 174174. Thomas H, Diamond J, Vieco A, Chaudhuri S, Shinnar E, Cromer S, Perel P, Mensah GA, Narula J, Johnson CO, Roth GA, Moran AE. Global Atlas of Cardiovascular Disease 2000-2016: The Path to Prevention and Control. Glob Heart. 2018;13(3):143-63. doi: 10.1016/j.gheart.2018.09.511. , 179179. Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, Forouzanfar MH, Longenecker CT, Mayosi BM, Mensah GA, Nascimento BR, Ribeiro ALP, Sable CA, Steer AC, Naghavi M, Mokdad AH, Murray CJL, Vos T, Carapetis JR, Roth GA. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990-2015. N Engl J Med. 2017;377(8):713-722. doi: 10.1056/NEJMoa1603693. , 197197. Xavier RMA, Azevedo VMP, Godoy PH, Migowski A, Ribeiro ALP, Chaves RBM, Correia MG, Xavier CA, Hashimoto LA, Weksler C, Silva NASE. Medium-Term Outcomes of 78,808 Patients after Heart Valve Surgery in a Middle-Income Country: A Nationwide Population-Based Study. BMC Cardiovasc Disord. 2017;17(1):302. doi: 10.1186/s12872-017-0725-9.
• Although nationwide data are still scarce, the sub-analysis of a multicenter cohort with 920 patients who underwent heart valve surgeries (isolated aortic valve replacement, 34%; isolated mitral valve replacement, 25%; 81% covered by the public health system) showed an acceptable surgical mortality rate (7.3%) 198198. Zilli AC, Guizilini S, Rocco IS, Santo JADE, Berwanger O, Kalil RAK, Jatene FB, Cavalcanti AB, Santos RHN, Gomes WJ. Valve Heart Surgery in Brazil - The BYPASS Registry Analysis. Braz J Cardiovasc Surg. 2020;35(1):82-90. doi: 10.21470/1678-9741-2019-0408. as compared to previous series (11.9%). 178178. Ribeiro GS, Tartof SY, Oliveira DW, Guedes AC, Reis MG, Riley LW, Ko AI. Surgery for Valvular Heart Disease: A Population-Based Study in a Brazilian Urban Center. PLoS One. 2012;7(5):e37855. doi: 10.1371/journal.pone.0037855.
Rheumatic Heart Disease
• Contrasting with the increasing trend of prevalence, age-standardized mortality rates attributable to RHD significantly decreased by 59.4% in Brazil, from 2.8 (95% UI, 2.7 – 3.0) to 1.2 (95% UI, 1.1 - 1.2) per 100 000, according to the GBD 2019 study. The percent decrease was similar for men (62.0%) and women (58.1%) (Table 5-3 and Chart 5-3.A). A similar trend was observed for the crude mortality rates (Chart 5-3.B). During the period, the total number of deaths decreased from 3088 (95% UI, 2939 - 3256) to 2715 (95% UI, 2505 - 2913) in 1990 and 2019, respectively, despite population growth (Table 5-3). These trends may reflect improvement in health conditions, and better and earlier access to healthcare. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• In 1990, RHD ranked 10thamong the causes of death in Brazil (9thto 12thin different states), and moved to 12thin 2019 (10thto 13thin most states, and 14thonly in the West-Central state of Mato Grosso do Sul). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• The more compelling decrease in mortality rates was observed in lower ages, especially in the ‘5-14 years’ and ‘15-49 years’ age groups: -78.1% (95% UI, -81.9 to -73.6) and -64.6% (95% UI, -68.3 to -60.4) per 100 000, respectively (Table 5-2). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
This may be associated with the better treatment of pharyngitis, ARF, and early presentations of RHD, while chronic sequelae still persist as a challenge. 199199. GBD 2019 Universal Health Coverage Collaborators. Measuring Universal Health Coverage Based on an Index of Effective Coverage of Health Services in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1250-84. doi: 10.1016/S0140-6736(20)30750-9.
https://doi.org/10.1016/S0140-6736(20)30...
, 200200. Dougherty S, Beaton A, Nascimento BR, Zühlke LJ, Khorsandi M, Wilson N. Prevention and Control of Rheumatic Heart Disease: Overcoming Core Challenges in Resource-Poor Environments. Ann Pediatr Cardiol. 2018;11(1):68-78. doi: 10.4103/apc.APC_135_17.
• According to the GBD 2019 data, there was a significant negative correlation between the percent change in age-standardized mortality rates and SDI in 1990 (Chart 5-4) (r=-0.41, p=0.03) and in 2019 (r=-0.44, p=0.02). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
Considering RHD as the most socially-driven etiology of valvular disease, this antecipated pattern differed from the GBD 2017 estimates, which did not reach statistical significance in 2017. This may suggest that, despite the undoubtable socioeconomic improvements observed in all Brazilian regions since 1990, which impacted different aspects of disease prevention and healthcare and significantly reduced the sociodemographic gap, inequality still plays an important role in RHD mortality. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
Non-rheumatic Valvular Heart Disease
• According to the GBD 2019 study, age-standardized mortality rates attributable to NRVD showed a 16.2% (95% UI, 10.3 - 22.5) decrease from 1990 to 2019 (Table 5-3 and Chart 5-5.A). However, for crude mortality rates a significant increase was observed [51.9% (95% UI, 39.8 - 62.7)], with a considerable contribution of older ages, markedly over 70 years [17.2% (95% UI, 5.4 - 27.4)] (Table 5-3 and Chart 5-5.B). The patterns were similar for men and women. Similar trends were observed for calcific aortic valve disease mortality rates, with a marked 17% (95% UI, 2.0 - 38.5) increase in the elderly (≥70 years), reflecting the association with population aging and prevalent cardiovascular risk factors (Table 5-2). For mitral degenerative valve disease, the age-standardized mortality rates decreased 19.0% (95% UI, 5.8 - 34.8 ), as opposed to a 36.2% increase in the crude prevalence (Tables 5-1 and 5-3), as a result of the increasing rates [16.5% (95% UI, -18.5 - 48.7)] in septuagenarians and older (Table 5-2), however with wide UIs. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
, 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• The increasing mortality rates in older ages due to NRVD noticeably contrasts with the trends observed for RHD, possibly reflecting a higher prevalence and, consequently, mortality in the age groups >70 years, for both aortic and mitral NRVD (Table 5-2). From 1990 to 2019, an increasing burden of calcific aortic valve disease, in both males and females, associated with an increase in mortality in that age group. The 95% UIs are overall wide for NRVD mortality estimates, especially for each specific valvular involvement in separate. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• In 1990 NRVD ranked 10thamong causes of death in Brazil (8thto 11thin different states), and proportionally increased to 9thin 2019 (8thto 10thin most states), the opposite trend of RHD (Chart 5-4). 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• GBD 2019 data demonstrated significant correlations between the changes in age-standardized mortality rates of NRVD in general and SDI in 1990 (r= -0.55, p=0.003) and 2019 (r= -0.58, p=0.001), and a similar pattern for calcific aortic valve disease (1990: r= -0.51, p=0.007; 2019: r= -0.54, p=0.003). Strong positive correlations were observed between age-standardized mortality and SDI in both 1990 (r=0.80, p<0.001) and 2019 (r=0.70, p<0.001) (Chart 5-6). As socioeconomic development correlates with epidemiological transition and life expectancy, a higher SDI associates with more elderly individuals at risk for degenerative valvular conditions and less prone to infectious etiologies, such as RHD. However, in Brazil, socioeconomic conditions – and possibly access to optimal healthcare – still played an important role on changes in NRVD mortality over time. 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• Similar correlations were observed for degenerative mitral valve disease. On the other hand, for other NRVDs, no significant correlation was observed between age-standardized mortality rates – and their percent changes over time – and SDI. 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
Burden of Disease
Rheumatic Heart Disease
• According to GBD 2019 data, the age-standardized DALY rate attributable to RHD significantly decreased 45.1% in Brazil, from 144.6 (95% UI, 126.8 - 167.3) per 100 000 in 1990 to 79.3 (95% UI, 61.6 - 102.6) per 100 000 in 2019 (Chart 5-7.A). The decreasind rates observed in the period were similar for men and women, -46.7% (95% UI, -54.4 to -39.3) and -44.2% (95% UI, -51.1 to -36.9), respectively (Table 5-4). 201201. GBD 2017 DALYs and HALE Collaborators. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 359 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859-922. doi: 10.1016/S0140-6736(18)32335-3.
https://doi.org/10.1016/S0140-6736(18)32...
• Age-standardized DALY rates decreased in all Brazilian states, with a steeper trend in the regions with highest rates in 1990: the West-Central and Southeast (Table 5-2). The Southeastern and West-Central regions had the highest age-standardized DALY rates and proportional DALYs in 1990, while four states of the Northeast (Sergipe, Bahia, Alagoas, and Pernambuco), one from the South (Paraná), and one from the West-Central (Goiás) topped the list in 2019. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• A similar downward pattern was observed for the age-standardized YLL rates due to RHD, which ranged from 102.1 (95% UI, 97.5 - 107.3) per 100 000 in 1990 to 35.8 (95% UI, 33.5 - 38.4) per 100 000 in 2019, with a 64.9% (95% UI, 61.6 - 67.9) decrease. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• The GBD 2019 estimates showed no correlation between age-standardized DALY rates due to RHD and SDI in 1990 or in 2019. Similarly, the SDI did not correlate with the percent change in age-standardized DALY rates in 1990 (r= -0.36, p=0.06), and a weak correlation was observed in 2019 (r= -0.41, p=0.03) (Chart 5-8), suggesting that the effects of socioeconomic development were less pronounced over morbidity, compared to mortality.
Non-rheumatic Valvular Heart Disease
• According to the GBD 2019, the age-standardized DALY rates of NRVD decreased (30%) in Brazil, from 62.8 (95% UI, 60.3 - 65.2) per 100 000 in 1990 to 44 (95% UI, 40.7 - 47) per 100 000 in 2019 (Table 5-4 and Chart 5-9.B). The decrease pattern observed in the period was similar for men (-31%) and women (-28%). Regarding specific diseases, rates decreased equally for mitral degenerative valve disease [-30.7% (95% UI, -41.6 to -22.6)] as compared to calcific aortic valve disease [-30.3% (95% UI, -36.3 to -21.3)]. For other NRVD, the age-standardized rates tended to increase [19.1% (95% UI, -21.1 - 68.5)], although UIs were considerably wide, including the 0, in this case. The trends observed for YLLs were similar. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• The downward trend was relatively homogeneous accross Brazilian states, and the age-standardized DALY rates remained higher for the Southern and Southeastern regions during the whole period, in addition to the Northeastern state of Pernambuco (5thplace in 2019) (Chart 5-9.B). The most significant decrease was also observed in the Southeastern and West-Central regions (Distrito Federal and the states of São Paulo, Minas Gerais, Goiás and Rio de Janeiro) in addition to the Northern state of Rondônia (which lacks primary data for most estimates). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• Similarly to that observed for mortality, the decreasing age-standardized DALY rates of NRVD contrast with the slight increase of crude rates [7.3% (95% UI, 0 - 15.1)] in the period (1990 – 2019), driven by the >70 age-group (+5%) and again suggesting that morbidity associated with NRVD is shifting to the elderly, presumably following changes in the population age composition. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 1818. GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
https://doi.org/10.1016/S0140-6736(20)30...
• The proportional DALY rates in Brazil increased, and, from 1990 to 2019, the Southern and Southeastern regions accounted for the highest DALY proportions in the period, according to GBD estimates. 201201. GBD 2017 DALYs and HALE Collaborators. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 359 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859-922. doi: 10.1016/S0140-6736(18)32335-3.
https://doi.org/10.1016/S0140-6736(18)32...
,202201
• In addition, according to GBD 2019 data, there were significant positive correlations between the age-standardized DALY rates of NRVD in general and the SDI in 1990 (r=0.80, p<0.001) and in 2019 (r=0.55, p<0.001) (Chart 5-10). Percent changes in age-standardized DALY rates (1990 – 2019) also correlated with the SDI in 1990 (r= -0.72, p<0.001) and in 2019 (r= -0.72, p<0.001). For calcific aortic valve disease, significant correlations were observed between DALYs and the SDI in 1990 (r2=0.80, p<0.001) and in 2019 (r2=0.62, p<0.001), as well as between percent changes in DALY rates and the SDI in both years, suggesting that socioeconomic development is also a determinant of degenerative NRVD, linked to aging and risk factors.
• For degenerative mitral valve disease, a positive correlation between age-standardized DALY rates and the SDI was observed in 1990, but not in 2019, whereas percent changes in DALY rates correlated negatively with the SDI in 1990 and in 2019, suggesting some impact of socioeconomic markers on this condition.
Complications and Associated Diseases
Arrhythmias Associated with Valve Disease
• For patients with valvular heart disease, AF is also an aggravating factor and usually occurrs in those with more advanced natural history. It is more commonly associated with mitral valve disease, especially mitral stenosis. In a cohort of 427 patients (mean age 50±16 years, 84% female) with severe mitral stenosis, AF was observed in 34% of them, being more frequent in those who died during follow-up (27 of 41; 66%) as compared to survivors (114 of 378; 30%), reinforcing its role as a prognosis marker in valve disease. 203203. Nunes MCP, Tan TC, Elmariah S, Lodi-Junqueira L, Nascimento BR, Lago R, Silva JLP, Reis RCP, Zeng X, Palacios IF, Hung J, Levine RA. Net Atrioventricular Compliance is an Independent Predictor of Cardiovascular Death in Mitral Stenosis. Heart. 2017;103(23):1891-1898. doi: 10.1136/heartjnl-2016-310955.
• In addition, AF can develop in severe aortic valve disease, especially in older and postoperative patients. In a retrospective cohort of 348 patients (mean age, 76.8±4.6 years), postoperative AF was observed in 114 (32.8%), but rates were higher in patients ≥ 80 years as compared to 70-79-year-old patients (42.9% vs. 28.8%, p=0.017). 204204. Pivatto F jR, Teixeira Filho GF, Sant’anna JR, Py PM, Prates PR, Nesralla IA, Kalil RA. Advanced age and Incidence of Atrial Fibrillation in the Postoperative Period of Aortic Valve Replacement. Rev Bras Cir Cardiovasc. 2014;29(1):45-50. doi: 10.5935/1678-9741.20140010.
• In another retrospective assessment conducted in the state of Pernambuco (Northeastern Brazil), involving 491 consecutive patients after heart valve surgery, the incidence of AF was 31.2% and was associated with age >70 years (OR=6.82; 95% CI, 3.34 - 14.10, p <0.001), mitral valve disease (OR=3.18; 95% CI, 1.83 - 5.20, p<0.001), and no postoperative use of beta-blockers, among other factors. 205205. Sá MP, Sá MV, Albuquerque AC, Silva BB, Siqueira JW, Brito PR, Ferraz PE, Lima Rde C. Predicting Risk of Atrial Fibrillation After Heart Valve Surgery: Evaluation of a Brazilian Risk Score. Rev Bras Cir Cardiovasc. 2012;27(1):117-22. doi: 10.5935/1678-9741.20120017.
• Valvular heart disease (17.5%) and arrhythmias (AF and atrial flutter, 50.7%) were the main cardioembolic sources of stroke in a study involving 256 patients (60.2 ± 6.9 years, 132 males) in the Southern region of Brazil. 206206. Marrone LCP, Brunelli JPf, Saute Rl, Tomasi Gh, Madeira Bc, Martins WA, Rohr RD, Heck AP, Botton LR, Castro MM, Bodanese R, Bodanese LC, Marrone ACH, Costa JC. Cardioembolic Sources in Stroke Patients in South of Brazil. Thrombosis. 2014;2014:753-780. doi: 10.1155/2014/753780.
• In the BYPASS registry, a multicenter cohort, of the patients undergoing valve heart surgeries, the most frequent postoperative complications were arrhythmias (22.6%), followed by infections (5.7%), and low-output syndrome (5.1%). 198198. Zilli AC, Guizilini S, Rocco IS, Santo JADE, Berwanger O, Kalil RAK, Jatene FB, Cavalcanti AB, Santos RHN, Gomes WJ. Valve Heart Surgery in Brazil - The BYPASS Registry Analysis. Braz J Cardiovasc Surg. 2020;35(1):82-90. doi: 10.21470/1678-9741-2019-0408.
Association Between Valvular Heart Disease and Coronary Artery Disease
• Due to the increased surgical risk of combined valve procedures and coronary revascularization, it is essential to recognize the prevalence of obstructive CAD in association with valvular heart disease. Studies have shown a lower prevalence of CAD in patients with RHD as compared to those with NRVD, possibly as a reflection of the lower median age of RHD patients and the higher prevalence of coronary risk factors in NRVD. 207207. Sampaio RO, Jonke VM, Falcão JL, Falcão S, Spina GS, Tarasoutchi F, Grinberg M. Prevalence of Coronary Artery Disease and Preoperative Assessment in Patients With Valvopathy. Arq Bras Cardiol. 2008;91(3):183-6. doi: 10.1590/s0066-782x2008001500010.
• In a study in Rio de Janeiro (Southeastern Brazil) including 1412 candidates for cardiac surgery of any indication, 294 with primary valvular heart disease of rheumatic and non-rheumatic etiologies were selected. All 294 patients were ≥40 years-old and had coronary angiography performed. The prevalence of obstructuve CAD in RHD and NRVD patients was 4% and 33.6% (p <0.0001), respectively. Characteristics and risk factors, such as age, typical chest pain, hypertension, diabetes mellitus, and dyslipidemia, were significantly associated with obstructive CAD. 208208. Kruczan DD, Silva NA, Pereira Bde B, Romão VA, Correa Filho WB, Morales FE. Coronary Artery Disease in Patients With Rheumatic and Non-Rheumatic Valvular Heart Disease Treated at a Public Hospital in Rio de Janeiro. Arq Bras Cardiol. 2008;90(3):197-203. doi: 10.1590/s0066-782x2008000300010.
• In another study in Brazil, evaluating 712 patients with valvular heart disease (mean age, 58±13 years), the incidence of obstructive CAD was 20%. However, in younger patients (<50 years) prevalence was much lower (3.3%). 209209. Cazelli JG, Camargo GC, Kruczan DD, Weksler C, Felipe AR, Gottlieb I. Prevalence and Prediction of Obstructive Coronary Artery Disease in Patients Undergoing Primary Heart Valve Surgery. Arq Bras Cardiol. 2017;109(4):348-356. doi: 10.5935/abc.20170135. These data are similar to those observed in another study that included 3736 patients (mean age, 43.7 years), in which prevalence of obstructive CAD combined with valvular heart disease was 3.42%. 207207. Sampaio RO, Jonke VM, Falcão JL, Falcão S, Spina GS, Tarasoutchi F, Grinberg M. Prevalence of Coronary Artery Disease and Preoperative Assessment in Patients With Valvopathy. Arq Bras Cardiol. 2008;91(3):183-6. doi: 10.1590/s0066-782x2008001500010.
Healthcare Utilization and Cost
• According to the SUS administrative database, the total crude expenses (reimbursement) with hospital admissions for clinical treatment of valvular heart disease in Brazil showed a significant 90% increase, from R$ 1 051 959 in 2008 to R$ 1 999 540 in 2019 in an almost-linear pattern. Ajusting and converting these values to international dollars in 2019, the total costs for the public system were $ 1 031 953, in 2008, and $ 966 428, in 2019, for the treatment of hospitalization due to valvular conditions, a 6.3% reduction. 210210. Rede Interagencial de Informação para a Saúde. Indicadores e Dados Básicos de Saúde [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2020 Nov 09]. Available From: https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ .
https://datasus.saude.gov.br/acesso-a-in...
• Similarly, unadjusted costs associated with valvular surgical/interventional procedures (codes related to valve surgery, percutaneous mitral commissurotomy, other types of valvuloplasty) also increased from 2008 to 2019, from R$ 130 588 598 (2019 Int$ 128 105 083) to R$ 190 771 771 (2019 Int$ 92 204 819), although with less magnitude as compared to clinical admissions (46% vs. 90%). After adjustment for Int$, a remarkable 28.0% reduction was observed. The total expense with surgical procedures for the SUS in this time series (2008 – 2019) was R$ 10 524 044 511 (Int$ 6 853 635 725) (Table 5-5 and Chart 5-11). 210210. Rede Interagencial de Informação para a Saúde. Indicadores e Dados Básicos de Saúde [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2020 Nov 09]. Available From: https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ .
https://datasus.saude.gov.br/acesso-a-in...
• The number of surgical/interventional admissions related to valve diseases remained relatively stable in Brazil from 2008 to 2019, ranging from 12 679 in 2008 to 14 294 in 2019. This is presumably associated with the growing complexity and costs of interventions (markedly, hospital costs, devices and prostheses) and denotes the economic burden posed by the incorporation of new procedures and technologies, but it is also a marked effect of inflation on healthcare costs – considering the lower values in 2019 when adjusted to Int$. In this scenario, the future incorporation of well established therapies not yet reimbused by the SUS, such as TAVI, will contribute to increase the economic burden, although expenses with judicial demands may easily overcome ordinary costs. 211211. Lopes MACQ, Nascimento BR, Oliveira GMM. Treatment of Aortic Stenosis in Elderly Individuals in Brazil: How Long Can We Wait? Arq Bras Cardiol. 2020;114(2):313-18. doi: 10.36660/abc.2020003.
• The total number of hospital admissions due to valve disease (clinical and surgical) in this period was 196 922, and most of them occurred in the Southeastern region (41.2%), followed by the Northeastern (25.7%), Southern (20.2%), West-Central (7.5%), and Northern (5.4%) regions (Table 5-5). 210210. Rede Interagencial de Informação para a Saúde. Indicadores e Dados Básicos de Saúde [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2020 Nov 09]. Available From: https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ .
https://datasus.saude.gov.br/acesso-a-in...
• A dramatic drop was observed for some types of procedures, despite their growing indications, such as the percutaneous mitral commissurotomy. For this specific procedure, the downward numbers may be associated with the lagged reimbursement tables of the SUS, limiting the number of hospitals that perform this intervention. The absolute number of open heart valve surgeries remained stable, from 12 201 in 2008 to 12 771 in 2019, despite the growing number of cases of valvular heart disease – especially NRVD – and the growing burden in the elderly, as population ages. 190190. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, Regional, and National Incidence, Prevalence, and Years Lived With Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-858. doi: 10.1016/S0140-6736(18)32279-7.
https://doi.org/10.1016/S0140-6736(18)32...
, 211211. Lopes MACQ, Nascimento BR, Oliveira GMM. Treatment of Aortic Stenosis in Elderly Individuals in Brazil: How Long Can We Wait? Arq Bras Cardiol. 2020;114(2):313-18. doi: 10.36660/abc.2020003.
• In none of the periods, the increase in the number of admissions paralleled the increasing expenses, suggesting not only a progressive complexity – and, consequently, cost – of the procedures to treat heart valve disease, but also inflation over medical devices and associated hospital costs (considering the Int$ values) (Table 5-5 and Chart 11). 210210. Rede Interagencial de Informação para a Saúde. Indicadores e Dados Básicos de Saúde [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2020 Nov 09]. Available From: https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ .
https://datasus.saude.gov.br/acesso-a-in...
• From the SUS administrative database, valve procedures associated with RHD sequelae cannot be differentiated from those associated with other etiologies, since no specific coding is available, and the reporting of the ICD coding is imprecise. 210210. Rede Interagencial de Informação para a Saúde. Indicadores e Dados Básicos de Saúde [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2020 Nov 09]. Available From: https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ .
https://datasus.saude.gov.br/acesso-a-in...
• Interestingly, observational studies have reinforced that RHD remains as the main etiology associated with cardiac surgery in young people in Brazil, reaching up to 60% in a study performed in the city of Salvador, Bahia (Northeastern Brazil). 178178. Ribeiro GS, Tartof SY, Oliveira DW, Guedes AC, Reis MG, Riley LW, Ko AI. Surgery for Valvular Heart Disease: A Population-Based Study in a Brazilian Urban Center. PLoS One. 2012;7(5):e37855. doi: 10.1371/journal.pone.0037855. At the São Paulo Heart Institute (Southeastern region), the number of heart valve surgeries associated with RHD increased substantially over the past 10 years, from around 400 surgeries/year in 1990 to over 600 after 2000. 121121. Lisboa LA, Moreira LF, Mejia OV, Dallan LA, Pomerantzeff PM, Costa R, Puig LB, Jatene FB, Marcial MB, Stolf NA. Evolution of Cardiovascular Surgery at the Instituto do Coração: Analysis of 71,305 surgeries. Arq Bras Cardiol. 2010;94(2):162-8, 174-81, 164-71. doi: 10.1590/s0066-782x2010000200006. Between 2008 and 2015, there were 26 054 hospital admissions due to ARF sequelae, 45% of which due to heart disease, leading to a possibly underestimated total cost of US$ 3.5 million annually. 177177. Santos JPAD, Carmo GALD, Beaton AZ, Lourenço TV, Diamantino AC, Nunes MDCP, Sable C, Nascimento BR. Challenges for the Implementation of the First Large-Scale Rheumatic Heart Disease Screening Program in Brazil: The PROVAR Study Experience. Arq Bras Cardiol. 2017;108(4):370-374. doi: 10.5935/abc.20170047. , 210210. Rede Interagencial de Informação para a Saúde. Indicadores e Dados Básicos de Saúde [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2020 Nov 09]. Available From: https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ .
https://datasus.saude.gov.br/acesso-a-in...
• According to observational studies and hospital-based registries, overall valve diseases of rheumatic origin account for about 90% of the cardiac surgeries in children and for over 30% of the cardiac surgeries in adults, most of them in young ages. 135135. Bocchi EA. Heart Failure in South America. Curr Cardiol Rev. 2013;9(2):147-56. doi: 10.2174/1573403x11309020007. However, few epidemiological studies estimated the cause-specific burden of valve diseases in Brazil.
• Echocardiographic screening for latent RHD has proven to be cost-effective in one study conducted in Brazil. A strategy based on task-shifting, with imaging acquisition by non-physicians utilizing handheld devices and remote telemedicine interpretation by experts, resulted in an Incremental Cost-Effectiveness Ratio of $10 148.38 per DALY averted, below the estimated threshold of 3 times the gross domestic product per capita, suggested by the World Health Organization. 212212. Ubels J, Sable C, Beaton AZ, Nunes MCP, Oliveira KKB, Rabelo LC, Teixeira IM, Ruiz GZL, Rabelo LMM, Tompsett AR, Ribeiro ALP, Sahlen KG, Nascimento BR; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática e Outras Doenças Cardiovasculares) investigators. Cost-Effectiveness of Rheumatic Heart Disease Echocardiographic Screening in Brazil: Data From the PROVAR+ Study: Cost-effectiveness of RHD screening in Brazil. Glob Heart. 2020;15(1):18. doi: 10.5334/gh.529.
• Data from the national database of the SUS (DATASUS) show that from 2008 to 2017 there were 42 720 and 78 966 hospital admissions due to ARF and chronic RHD, respectively, accounting for 0.4% and 0.7% of cardiovascular admissions in the country, respectively. This analysis, however, lacks data from specific NRVD. 213213. Fonseca LGA, Lima INDF, Gualdi LP. Characterization of Brazilian Hospital Admissions due to Cardiovascular Diseases: A Longitudinal Study. BMC Cardiovasc Disord. 2020;20(1):311. doi: 10.1186/s12872-020-01588-w.
Mitral Valve Disease
• Based on SUS administrative data from 2001 to 2007 and regarding mitral valve surgery, in a retrospective series of 78 808 consecutive surgical patients, the mean age was 50.0 years (35.9 - 62.5) and 40 106 were females (50.9%). Again, RHD was the main etiology, accounting for 53.7% of the total patients undergoing surgery and for over 94% of those undergoing procedures due to mitral stenosis. Mitral stenosis was the largest single surgical indication, accounting for 38.9% of the total. Overall, valve replacement was done in 69.1% of the surgeries. In-hospital mortality was 7.6%. 197197. Xavier RMA, Azevedo VMP, Godoy PH, Migowski A, Ribeiro ALP, Chaves RBM, Correia MG, Xavier CA, Hashimoto LA, Weksler C, Silva NASE. Medium-Term Outcomes of 78,808 Patients after Heart Valve Surgery in a Middle-Income Country: A Nationwide Population-Based Study. BMC Cardiovasc Disord. 2017;17(1):302. doi: 10.1186/s12872-017-0725-9.
• Surgical mortality was slightly higher in women than in men (7.8% vs. 7.3%; p <0.001), and considerably higher in people ≥80 years. On the other hand, the lowest mortality was observed for those between 20 and 39.9 years (p <0.001). Patients with combined aortic and mitral surgeries (reflecting rheumatic etiology) were the youngest (median, 43.3 years). Surgery for aortic stenosis was more common in older individuals (median, 58.0 years) (p <0.001). Valve repair had lower mortality (3.5%) as compared to valve replacement (6.9%), multiple valve repair and/or replacement (8.2%), and concomitant CABG (14.6%) (p<0.001). Associated CABG occurred in 7147 patients (9.1% of the sample). 197197. Xavier RMA, Azevedo VMP, Godoy PH, Migowski A, Ribeiro ALP, Chaves RBM, Correia MG, Xavier CA, Hashimoto LA, Weksler C, Silva NASE. Medium-Term Outcomes of 78,808 Patients after Heart Valve Surgery in a Middle-Income Country: A Nationwide Population-Based Study. BMC Cardiovasc Disord. 2017;17(1):302. doi: 10.1186/s12872-017-0725-9.
• Regarding percutaneous mitral commissurotomy, studies in Brazil show a much higher proportion of females (85%) – coincident with the epidemiology of RHD and noticeably mitral stenosis – and of young people (<40 years). 214214. Cardoso LF, Ayres CV, Bento AM, Tarasoutchi F, Vieira ML, Grinberg M. Immediate and Late Results of Percutaneous Mitral Valve Repair in Patients With Mitral Stenosis. Arq Bras Cardiol. 2010;94(3):383-90, 406-13. doi: 10.1590/s0066-782x2010000300020. , 215215. Peixoto A, Linhares L, Scherr P, Xavier R, Siqueira SL, Pacheco TJ, Venturinelli G. Rheumatic Fever: Systematic Review. Rev Bras Clin Med. 2011;9(3):234-8. As local expertise in this procedure develops, technical aspects are being investigated, such as the routine utilization of conscious sedation (low-dose midazolam and fentanyl) resulting in anxiolysis and analgesia, without hemodynamic effects. 216216. Alcici ME, Lodi-Junqueira L, Sant’Anna Athayde GR, Soares JR, Gomes Tiago DA, Tavares PL, Saad GP, Ferreira de Sales I, Okello E, Rwebembera J, Esteves WAM, Nunes MCP. The Importance of Conscious Sedation for Life-Saving Valve Procedures in Patients With Rheumatic Heart Disease From Low- to Middle-Income Countries. Glob Heart. 2019;14(3):311-16. doi: 10.1016/j.gheart.2019.07.003. Furthermore, there are continuous efforts to define predictors of long-term clinical outcomes, such as changes in invasive and non-invasive atrioventricular compliance. 217217. Athayde GRS, Nascimento BR, Elmariah S, Lodi-Junqueira L, Soares JR, Saad GP, Silva JLP, Tan TC, Hung J, Palacios IF, Levine RA, Nunes MCP. Impact of Left Atrial Compliance Improvement on Functional Status After Percutaneous Mitral Valvuloplasty. Catheter Cardiovasc Interv. 2019;93(1):156-63. doi: 10.1002/ccd.27831.
• In a retrospective study aimed at evaluating mitral valve repair in 54 Brazilian children (<16 years) with early chronic RHD, no perioperative death was recorded. The most frequent late (>7 days) outcomes were residual mitral lesion (n=11) and need for reoperation (n=3). Thus, mitral repair remains a reasonable strategy for RHD at younger ages. 218218. Cruz RCC, Cordeiro BS, Santos FS, Fernandes CR, Gama JMA, Ladeia AMT. Predictors of Unfavourable Outcomes in Children and Adolescents Submitted to Surgical Mitral Valvuloplasty Secondary to Chronic Rheumatic Heart Disease. Arq Bras Cardiol. 2019;113(4):748-56. doi: 10.5935/abc.20190184.
Aortic Valve Disease
• A cohort of 724 consecutive patients, who underwent cardiac surgery at the São Paulo Heart Institute, has evidenced, similarly to other studies, a higher percentage of women (55%) and predominance of RHD (60%). However, in that series, there was a great proportion of aortic valve disease (396 cases) over mitral valve disease (306 cases) as compared to other series. Of the patients with mitral valve disease, 39.9% had stenosis, 38.4% regurgitation, and 21.7% mitral prosthesis dysfunction. In patients undergoing aortic valve interventions, stenosis was observed in 51.6%, regurgitation in 29.3%, and prosthesis dysfunction in 19.1%. The study suggests an increase in aortic valve disease as compared to mitral valve disease in a tertiary hospital in the Southeastern region of Brazil. 219219. Grinberg M, Jonke VM, Sampaio RO, Spina GS, Tarasoutchi F. Validation of a New Surgical Risk Score For Heart Valve Surgery: VMCP. Arq Bras Cardiol. 2009;92(4):320-5. doi: 10.1590/s0066-782x2009000400012.
• Another retrospective cohort study has been conducted in the city of Porto Alegre (Southern Brazil) with 1065 patients (mean age, 61.4 ± 11.8 years; 38% women). Aortic valve replacement was done in 18.8% and mitral valve replacement, in 13.4%. Concomitant coronary revascularization was performed in 60.3% of the sample, and valve surgeries in 32.7%. Overall in-hospital mortality was 7.8%, being lower for isolated CABG (5.9%), intermediate for valve surgery (aortic and/or mitral and/or tricuspid = 8.6%), and higher for combined valve and CABG procedures (20.0%). 220220. Garofallo SB, Machado DP, Rodrigues CG, Bordim O Jr, Kalil RA, Portal VL. Applicability of Two International Risk Scores in Cardiac Surgery in a Reference Center in BRAZIL. Arq Bras Cardiol. 2014;102(6):539-48. doi: 10.5935/abc.20140064.
Transcatheter Aortic Valve Implantation in Brazil
• As in other countries, TAVI gained importance in Brazil in the past 20 years. It is estimated that over 100 000 percutaneous aortic valve implantations have been performed worldwide to date. 196196. Grinberg M, Accorsi TA. Aortic stenosis in the elderly: a Brazilian perspective. Arq Bras Cardiol. 2009 Feb;92(2):e9-12. doi: 10.1590/s0066-782x2009000200016. , 211211. Lopes MACQ, Nascimento BR, Oliveira GMM. Treatment of Aortic Stenosis in Elderly Individuals in Brazil: How Long Can We Wait? Arq Bras Cardiol. 2020;114(2):313-18. doi: 10.36660/abc.2020003. The first TAVI in Brazil occurred in 2008. The Brazilian TAVI registry reported 418 TAVI in 18 centers until 2014, and this number has grown exponentially since then. Femoral access was the choice in 96.2% of the procedures, and the prostheses used were CoreValve® (86.1%) and Sapien XT® (13.9%). Of that initial experience, all-cause mortality at 30 days and 1 year were 9.1 and 21.5%, respectively. 221221. Brito FS Jr, Carvalho LA, Sarmento-Leite R, Mangione JA, Lemos P, Siciliano A, Caramori P, São Thiago L, Grube E, Abizaid A; Brazilian TAVI Registry Investigators. Outcomes and Predictors of Mortality After Transcatheter Aortic Valve Implantation: Results of the Brazilian registry. Catheter Cardiovasc Interv. 2015;85(5):153-62. doi: 10.1002/ccd.25778.
• Data from the TAVI registry updated in 2017 revealed a total of 819 patients under clinical follow-up, demonstrating that the procedure has a low incidence of complications – especially early hard cliical outcomes – and highlighting rates of postprocedural renal failure around 18%. 222222. Nunes Filho ACB, Katz M, Campos CM, Carvalho LA, Siqueira DA, Tumelero RT, Portella ALF, Esteves V, Perin MA, Sarmento-Leite R, Lemos Neto PA, Tarasoutchi F, Bezerra HG, Brito FS Jr. Impact of Acute Kidney Injury on Short- and Long-term Outcomes After Transcatheter Aortic Valve Implantation. Rev Esp Cardiol. 2019;72(1):21-29. doi: 10.1016/j.rec.2017.11.024. , 223223. Monteiro C, Ferrari ADL, Caramori PRA, Carvalho LAF, Siqueira DAA, Thiago LEKS, Perin M, Lima VC, Guérios E, Brito FS Jr. Permanent Pacing After Transcatheter Aortic Valve Implantation: Incidence, Predictors and Evolution of Left Ventricular Function. Arq Bras Cardiol. 2017;109(6):550-59. doi: 10.5935/abc.20170170.
• In another assessment performed in the city of Rio de Janeiro, of 136 patients undergoing TAVI [median age, 83 (80-87) years; 51% males], perioperative mortality was 1.5%; 30-day mortality, 5.9%; in-hospital mortality, 8.1%; and 1-year mortality, 15.5%. 224224. Souza AL, Salgado CG, Mourilhe-Rocha R, Mesquita ET, Lima LC, Mattos ND, Rabischoffsky A, Fagundes FE, Colafranceschi AS, Carvalho LA. Transcatheter Aortic Valve Implantation and Morbidity and Mortality-Related Factors: A 5-Year Experience in Brazil. Arq Bras Cardiol. 2016;106(6):519-27. doi: 10.5935/abc.20160072.
• Of 819 percutaneous aortic valves implanted until 2017, 135 patients (20.1%) required permanent pacemaker implantation. These patients were older (82.5 vs. 81.1 years; p=0.047), predominantly male (59.3% vs 45%; p=0.003), and had previous right bundle-branch block (OR=6.19, 95% CI, 3.56 - 10.75, p≤0.001). The use of CoreValve® prosthesis (OR=3.16, 95% CI, 1.74 - 5.72, p≤0.001) and baseline transaortic gradient >50 mm Hg (OR=1.86, 95% CI, 1.08 - 3.20, p=0.025) were independent predictors of permanent pacemaker implantation. 223223. Monteiro C, Ferrari ADL, Caramori PRA, Carvalho LAF, Siqueira DAA, Thiago LEKS, Perin M, Lima VC, Guérios E, Brito FS Jr. Permanent Pacing After Transcatheter Aortic Valve Implantation: Incidence, Predictors and Evolution of Left Ventricular Function. Arq Bras Cardiol. 2017;109(6):550-59. doi: 10.5935/abc.20170170.
Future Research
• Even considering the noticeable improvement in past decades, there is still paucity of primary data about the epidemiology of valvular heart disease in Brazil, and room for future research.
• Administrative data collection should be included, with the development of specific coding to allow for discrimination of variables, such as the valve involved, type of valvular dysfunction, type of prosthesis, and, especially, etiology and association with systemic diseases. This is especially important in the SUS.
• In addition, the development of nationwide registries on valve disease and procedures is warranted. Refining the coding system and implementing mandatory clinical and surgical reports – as previously done for percutaneous coronary interventions – may be an initial step to improve data acquisition.
• As the country has significant cohorts of patients with valvular heart disease, mid- and long-term follow-up of these samples are warranted. Of note, there are research initiatives that require incentives and funding for their continuation, such as ongoing studies on long-term prognosis of subclinical RHD in children and adolescents, 176176. Nascimento BR, Beaton AZ, Nunes MC, Diamantino AC, Carmo GA, Oliveira KK, Oliveira CM, Meira ZM, Castilho SR, Lopes EL, Castro IM, Rezende VM, Chequer G, Landay T, Tompsett A, Ribeiro ALP, Sable C; PROVAR (Programa de RastreamentO da VAlvopatia Reumática) Investigators. Echocardiographic Prevalence of Rheumatic Heart Disease in Brazilian Schoolchildren: Data From the PROVAR study. Int J Cardiol. 2016;219:439-45. doi: 10.1016/j.ijcard.2016.06.088. , 192192. Nascimento BR, Sable C, Nunes MCP, Diamantino AC, Oliveira KKB, Oliveira CM, Meira ZMA, Castilho SRT, Santos JPA, Rabelo LMM, Lauriano KCA, Carmo GAL, Tompsett A, Ribeiro ALP, Beaton AZ; PROVAR (Rheumatic Valve Disease Screening Program) Investigators. Comparison Between Different Strategies of Rheumatic Heart Disease Echocardiographic Screening in Brazil: Data From the PROVAR (Rheumatic Valve Disease Screening Program) Study. J Am Heart Assoc. 2018;7(4):e008039. doi: 10.1161/JAHA.117.008039. genetic and immune determinants of response to streptococcal infections leading to RHD, 225225. Guilherme L, Kalil J. Rheumatic Fever and Rheumatic Heart Disease: Cellular Mechanisms Leading Autoimmune Reactivity and Disease. J Clin Immunol. 2010;30(1):17-23. doi: 10.1007/s10875-009-9332-6. clinical and procedural predictors of short- and long-term events after percutaneous mitral commissurotomy, 203203. Nunes MCP, Tan TC, Elmariah S, Lodi-Junqueira L, Nascimento BR, Lago R, Silva JLP, Reis RCP, Zeng X, Palacios IF, Hung J, Levine RA. Net Atrioventricular Compliance is an Independent Predictor of Cardiovascular Death in Mitral Stenosis. Heart. 2017;103(23):1891-1898. doi: 10.1136/heartjnl-2016-310955. , 226226. Nunes MC, Tan TC, Elmariah S, Lago R, Margey R, Cruz-Gonzalez I, Zheng H, Handschumacher MD, Inglessis I, Palacios IF, Weyman AE, Hung J. The Echo Score Revisited: Impact of Incorporating Commissural Morphology and Leaflet Displacement to the Prediction of Outcome For Patients Undergoing Percutaneous Mitral Valvuloplasty. Circulation. 2014;129(8):886-95. doi: 10.1161/CIRCULATIONAHA.113.001252. and a national TAVI registry. 221221. Brito FS Jr, Carvalho LA, Sarmento-Leite R, Mangione JA, Lemos P, Siciliano A, Caramori P, São Thiago L, Grube E, Abizaid A; Brazilian TAVI Registry Investigators. Outcomes and Predictors of Mortality After Transcatheter Aortic Valve Implantation: Results of the Brazilian registry. Catheter Cardiovasc Interv. 2015;85(5):153-62. doi: 10.1002/ccd.25778.
• One study suggests that echo screening for RHD is cost-effective in Brazil, 212212. Ubels J, Sable C, Beaton AZ, Nunes MCP, Oliveira KKB, Rabelo LC, Teixeira IM, Ruiz GZL, Rabelo LMM, Tompsett AR, Ribeiro ALP, Sahlen KG, Nascimento BR; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática e Outras Doenças Cardiovasculares) investigators. Cost-Effectiveness of Rheumatic Heart Disease Echocardiographic Screening in Brazil: Data From the PROVAR+ Study: Cost-effectiveness of RHD screening in Brazil. Glob Heart. 2020;15(1):18. doi: 10.5334/gh.529. thus, its application outside research and integration into health systems should be investigated in large-scale programs.
• In addition, continuing efforts have been directed to the development of vaccines for streptococcal infections, 225225. Guilherme L, Kalil J. Rheumatic Fever and Rheumatic Heart Disease: Cellular Mechanisms Leading Autoimmune Reactivity and Disease. J Clin Immunol. 2010;30(1):17-23. doi: 10.1007/s10875-009-9332-6. and collaborative studies on their efficacy and clinical application to reduce RHD burden are warranted.
• As reimbursement for TAVI has just been approved in the Brazilian private health system, its incorporation in the Brazilian SUS seems to be close, 211211. Lopes MACQ, Nascimento BR, Oliveira GMM. Treatment of Aortic Stenosis in Elderly Individuals in Brazil: How Long Can We Wait? Arq Bras Cardiol. 2020;114(2):313-18. doi: 10.36660/abc.2020003. and a comprehensive evaluation of its actual clinical, budgetary and social impact on public healthcare outcomes requires extensive research and funding.
• Finally, promising strategies to provide early diagnosis and prioritization of referrals in low-resourced areas should be further investigated in Brazil. As an example, the availability of imaging modalities for the management of valvular heart disease – markedly echocardiography – is limited and unequally distributed in the country. In this scenario, the implementation of tele-echocardiography, with task-shifting of imaging acquisition to non-physicians (still not allowed by Brazilian healthcare regulations outside research) and remote reading, has already been evaluated, and implementation should be considered. 227227. Nascimento BR, Beaton AZ, Nunes MCP, Tompsett AR, Oliveira KKB, Diamantino AC, Barbosa MM, Lourenço TV, Teixeira IM, Ruiz GZL, Rios JPP, Ribeiro ALP, Sable C; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática and Other Cardiovascular Diseases) Investigators. Integration of Echocardiographic Screening by Non-Physicians With Remote Reading in Primary Care. Heart. 2019;105(4):283-290. doi: 10.1136/heartjnl-2018-313593. Despite its good overall diagnostic performance and discrimination of patients at higher cardiovascular risk, 227227. Nascimento BR, Beaton AZ, Nunes MCP, Tompsett AR, Oliveira KKB, Diamantino AC, Barbosa MM, Lourenço TV, Teixeira IM, Ruiz GZL, Rios JPP, Ribeiro ALP, Sable C; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática and Other Cardiovascular Diseases) Investigators. Integration of Echocardiographic Screening by Non-Physicians With Remote Reading in Primary Care. Heart. 2019;105(4):283-290. doi: 10.1136/heartjnl-2018-313593. the impact on clinical outcomes and cost-effectiveness of the strategy are yet to be explored.
• There is room for improvement of remote cardiac diagnosis in Brazil, through the expansion of tele-ECG, AF screening, 228228. Diamantino AC, Nascimento BR, Beaton AZ, Nunes MCP, Oliveira KKB, Rabelo LC, Barbosa MM, Tompsett AR, Olivieri L, Mata MD, Costa WAA, Pereira AF, Diamantino LC, Ribeiro ALP, Sable C, Brant LCC. Atrial Fibrillation Detection With a Portable Device During Cardiovascular Screening in Primary Care. Heart. 2020;106(16):1261-66. doi: 10.1136/heartjnl-2019-316277. remote consultations – including those for infective conditions, such as COVID-19 229229. Nascimento BR, Brant LCC, Castro ACT, Froes LEV, Ribeiro ALP, Cruz LV, Araújo CB, Souza CF, Froes ET, Souza SD. Impact of a Large-Scale Telemedicine Network on Emergency Visits and Hospital Admissions During the Coronavirus Disease 2019 Pandemic in Brazil: Data From the UNIMED-BH System. J Telemed Telecare. 2020:1357633X20969529. doi: 10.1177/1357633X20969529. – and the incorporation of imaging innovations to improve access to cardiovascular care. Extensive discussions are required, based on robust scientific evidence.
6. ATRIAL FIBRILLATION AND ATRIAL FLUTTER
ICD-10 I48
See Tables 6-1 through 6-5 and Charts 6-1 through 6-3
Abbreviations Used in Chapter 6
| AF | Atrial Fibrillation |
| BNP | B-type Natriuretic Peptide |
| CABG | Coronary Artery Bypass Grafting |
| ChD | Chagas Disease |
| CI | Confidence Interval |
| DALYs | Disability-Adjusted Life Years |
| ECG | Electrocardiogram |
| ELSA-Brasil | The Brazilian Longitudinal Study of Adult Health |
| FU | Federative Unit |
| GARFIELD-AF | The Global Anticoagulant Registry in the FIELD-AF |
| GBD | Global Burden of Disease |
| HF | Heart Failure |
| HR | Hazard Ratio |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems, 10thRevision |
| IMPACT-AF | A Multifaceted Intervention to Improve Treatment With Oral Anticoagulants in Atrial Fibrillation |
| INR | International Normalized Ratio |
| NOAC | New Oral Anticoagulants |
| OR | Odds Ratio |
| PPP | Purchasing Power Parity |
| SDI | Sociodemographic Index |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| TIA | Transient Ischemic Attack |
| TTR | Time in Therapeutic Range |
| UI | Uncertainty Interval |
| VKA | Vitamin K Antagonists |
| YLDs | Years Lived with Disability |
| YLLs | Years of Life Lost |
– Number of prevalent cases and age-standardized prevalence rates (per 100 000 inhabitants) of atrial fibrillation and flutter in 1990 and 2019, with percent change of rates, according to sex and age group, in Brazil
– Number of prevalent cases and age-standardized prevalence rate (per 100 000 inhabitants) of atrial fibrillation and flutter in 1990 and 2019, with percent change of rates, in Brazil and Brazilian Federative Units
– Number of deaths and age-standardized mortality rates (per 100 000 inhabitants) due to atrial fibrillation and flutter in 1990 and 2019, with percent change of rates, according to sex and age group, in Brazil
– Number of deaths and age-standardized mortality rate (per 100 000 inhabitants) due to atrial fibrillation and flutter in 1990 and 2019, with percent change of rates, in Brazil and Brazilian Federative Units
– Number of DALYs and age-standardized DALY rates (per 100 000 inhabitants) due to atrial fibrillation and flutter in 1990 and 2019, with percent change of rates, according to sex and age group, in Brazil
– All ages and age-standardized rates of atrial fibrillation/flutter between 1990 and 2019, in Brazil. A. Prevalence, B. Incidence, C. Deaths, D. YLLs, D. DALYs, E. YLDs. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Correlation of the 2019 Sociodemographic Index (SDI) and the percent change in age-standardized mortality rates due to atrial fibrillation and flutter per 100 000 inhabitants from 1990 to 2019
– Deaths (per 100 000) due to atrial fibrillation and flutter attributable to risk factors in Brazil in 1990 and 2019, and percent change, for both sexes, males, and females.
Prevalence and Incidence
• According to the GBD Study 2019 estimates, the age-standardized prevalence rates due to AF and atrial flutter increased slightly in Brazil from 519 (95% UI, 393-669) in 1990 to 537 (95% UI, 409-692) in 2019, per 100 000 inhabitants, for both sexes, with 3.5% (95% UI, 1.8-5.1) change in this period. The prevalence of AF and atrial flutter was higher in men [in 1990, 619 (95% UI, 468-792); in 2019, 643 (95% UI, 489-829)] than in women [in 1990, 499 (95% UI, 418-587); in 2019, 522 (95% UI, 440-610)], although the percent change was similar for both sexes (women, 4.0%; 95% UI, 1.9-6.5; and men, 4.0%; 95% UI, 1.9-6.0) in this period. In absolute numbers, estimates for the prevalence of AF and atrial flutter in Brazil rose from 0.4 million in 1990 to 1.2 million in 2019, mainly due to population growth and aging (Table 6-1 and Chart 6-1), as suggested by growing crude prevalence rates. In 2019, the proportion of subjects with prevalent AF was 0.59% (95% UI, 0.45-0.76). Stratifying by Brazilian FUs, the prevalence rate of AF and atrial flutter is similar in most Brazilian FUs, except for Minas Gerais, whose rate is nearly twice that of other states (Table 6-2). Importantly, Minas Gerais is the only state for which the Institute for Health Metrics and Evaluation has primary data, what may explain this difference and suggest that the AF prevalence may be even higher in Brazil than that estimated by the GBD. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Regarding the age-standardized incidence rate, per 100 000, per-year, the GBD Study 2019 estimates were 44 (95% UI, 33-56) in 1990 and 45 (95% UI, 34-58) in 2019, also higher for men in both time periods [women, 1990: 37 (95% UI, 28-48) and 2017: 39 (95% UI, 29-50); men: 1990: 50 (95% UI, 38-64) and 2017: 52 (95% UI, 39-67)].
• Data from population-based studies showed prevalence varying from 0.3% to 2.4%. In the ELSA-Brasil cohort study, which included 14 424 adults with valid ECG (45.8% men; age range, 35-74 years), the AF and atrial flutter prevalence was 0.3% (men, 0.5%; women, 0.2%), with the highest prevalence in the age range of 65-74 years (women: OR, 17; 95% CI, 2.1-135.9; men: OR, 52.3; 95% CI, 3.1-881.8). There was no difference in prevalence according to self-reported race, for both sexes. 230230. Pinto-Filho MM, Brant LCC, Foppa M, Garcia-Silva KB, Oliveira RAM, Fonseca MJM, Alvim S, Lotufo PA, Mill JG, Barreto SM, Macfarlane PW, Ribeiro ALP. Major Electrocardiographic Abnormalities According to the Minnesota Coding System Among Brazilian Adults (From the ELSA-Brasil Cohort Study). Am J Cardiol. 2017;119(12):2081-87. doi: 10.1016/j.amjcard.2017.03.043. In a cross-sectional study with 1524 elderly in São Paulo, the prevalence of AF or atrial flutter was 2.4% (men 3.9%; women, 2.0%). 231231. Kawabata-Yoshihara LA, Benseñor IM, Kawabata VS, Menezes PR, Scazufca M, Lotufo PA. Prevalence of Electrocardiographic Findings in Elderly Individuals: the Sao Paulo Aging & Health Study. Arq Bras Cardiol. 2009;93(6):602-7, 651-6. doi: 10.1590/s0066-782x2009001200015.
https://doi.org/10.1590/s0066-782x200900...
• Data from telehealth centers across Brazil have provided information on the prevalence of AF and atrial flutter based on ECG from primary care. 232232. Santos JPAD, Ribeiro ALP, Andrade-Junior D, Marcolino MS. Prevalence of Electrocardiographic Abnormalities in Primary Care Patients According to Sex and Age Group. A Retrospective Observational Study. Sao Paulo Med J. 2018;136(1):20-28. doi: 10.1590/1516-3180.2017.0222290817. In the ECG dataset of the Telehealth Network of Minas Gerais including 1 558 421 individuals (mean age, 51±18 years; 40.2% men) with ECG performed between 2010 and 2017, the AF prevalence was 1.33%, higher in men (1.81% vs. 1.02%), and increasing with age (OR 1.08, CI 95% 1.08-1.08), reaching 7.0% in octogenarians (8.4% in men vs. 5.9% in women). 236236. Paixão GMM, Silva LGS, Gomes PR, Lima EM, Ferreira MPF, Oliveira DM, Ribeiro MH, Ribeiro AH, Nascimento JS, Canazart JA, Ribeiro LB, Benjamin EJ, Macfarlane PW, Marcolino MS, Ribeiro ALP. Evaluation of Mortality in Atrial Fibrillation: Clinical Outcomes in Digital Electrocardiography (CODE) Study. Glob Heart. 2020;15(1):48. doi: 10.5334/gh.772.
• Data from 676 621 ECG (mean age, 51±19 years; 57.5% women) performed from 2009 to 2016 were analyzed at the Federal University of São Paulo telemedicine center and revealed a 7-year AF prevalence of 2.2% and a countrywide 2025 projected AF prevalence of 1.7%. 234234. Moraes ERFL, Cirenza C, Lopes RD, Carvalho AC, Guimaraes PO, Rodrigues AAE, Paola AAV. Prevalence of Atrial Fibrillation and Stroke Risk Assessment Based on Telemedicine Screening Tools in a Primary Healthcare Setting. Eur J Intern Med. 2019;67:36-41. doi: 10.1016/j.ejim.2019.04.024.
• The GARFIELD-AF is a hospital-based registry that included patients (≥18 years) with AF diagnosed within the previous 6 weeks and at least one additional risk factor for stroke. In Brazil, 41 sites included 1065 patients with non-valvular AF between 2010 and 2014 (mean age, 68±13 years; 55% males). New-onset AF diagnosed within the previous 6 weeks was recorded in 52% of the patients, paroxysmal in 25%, persistent in 14%, and permanent in 8%. 237237. Jerjes-Sanchez C, Corbalan R, Barretto ACP, Luciardi HL, Allu J, Illingworth L, Pieper KS, Kayani G; GARFIELD-AF Investigators. Stroke prevention in patients From Latin American Countries With Non-Valvular Atrial Fibrillation: Insights From the GARFIELD-AF Registry. Clin Cardiol. 2019;42(5):553-60. doi: 10.1002/clc.23176.
Mortality
• In the GBD Study 2019, the number of deaths from AF in Brazil has increased over the past few years, due to population growth and aging. In the 1990s, AF was responsible for 2659 (95% UI, 2263-3342) deaths, which rose to 10 811 (95% UI, 8636-12801) in 2019. However, the age-standardized mortality rate due to AF remained stable in the period, 4.8 (95% UI, 4.0-6.0) deaths per 100 000 inhabitants in 1990 and 5.0 (95% UI, 4.0-6.0) per 100 000 inhabitants in 2019, accounting for 0.8% (95% UI, 0.6-0.9) of all deaths in the country. Although age-standardized prevalence rates were consistently higher in men, women had a higher age-standardized mortality rate in 2019 [(women, 5.2 (95% UI, 3.9-6.0); men, 4.8 (95% UI, 3.2-6.4)], consistent with data from other countries. 238238. Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of Atrial Fibrillation on the Risk of Death: the Framingham Heart Study. Circulation. 1998;98(10):946-52. doi: 10.1161/01.cir.98.10.946. , 239239. Emdin CA, Wong CX, Hsiao AJ, Altman DG, Peters SA, Woodward M, Odutayo AA. Atrial Fibrillation as Risk Factor for Cardiovascular Disease and Death in Women Compared With Men: Systematic Review and Meta-Analysis of Cohort Studies. BMJ. 2016;532:h7013. doi: 10.1136/bmj.h7013. For individuals > 70 years old, the mortality rate increased from 1990 (51, 95% UI, 43-65) to 2019 (73, 95% UI, 57-87) (Table 6-3). Of note, because mortality based on vital registration data alone provides an implausibly steep increase over time possibly due to changes in ascertainment rather than AF epidemiology, the GBD Study 2019 assumes, a priori, that age and sex-specific mortality rates are neither increasing nor decreasing over time. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. As such, the small changes over time herein reported are intentionally lower than the real changes in raw data.
• Chart 6-1 shows that, although age-standardized mortality rates are stable, crude mortality rates are rising because of population aging and the growing number of individuals living longer with chronic heart diseases. Moreover, the YLL, a metric used in GBD for premature death, is also rising when not standardized to age.
• Table 6-4 shows the total number of deaths and the age-standardized mortality rates (per 100 000 inhabitants) due to AF and flutter, in 1990 and 2019, and percent change, for both sexes, in Brazil and its FUs. The FU with the highest mortality rates in 2019 were Distrito Federal, Maranhão, and Roraima, while those with the lowest were Piauí, Amazonas, and Paraíba. However, due to reporting issues, these data can be inconsistent and should be interpreted with caution.
• The GBD Study 2019 uses the SDI as an estimate of the socioeconomic level of a location. As demonstrated in Chart 6-2, there was a modest association of higher SDI in 2019 and greater percent change in AF age-standardized mortality rate from 1990 to 2019 (r=-0.44, p=0.02), revealing that the most developed FUs had a greater reduction in mortality, possibly due to health investments and a greater reduction in the cardiovascular disease burden as a whole.
• From a dataset of 1 558 421 ECGs from primary care patients (Telehealth Network of Minas Gerais) linked to the Brazilian Mortality Information System, the overall mortality rate was 3.34% in a mean follow-up of 3.68 years. After adjusting for age and comorbidities, patients living with AF had a higher risk of overall (HR 2.10; 95% CI, 2.03–2.17) and cardiovascular (HR 2.06; 95% CI, 1.86–2.29) death, with increased risk in women, who lost their survival advantage over men when AF was present. 236236. Paixão GMM, Silva LGS, Gomes PR, Lima EM, Ferreira MPF, Oliveira DM, Ribeiro MH, Ribeiro AH, Nascimento JS, Canazart JA, Ribeiro LB, Benjamin EJ, Macfarlane PW, Marcolino MS, Ribeiro ALP. Evaluation of Mortality in Atrial Fibrillation: Clinical Outcomes in Digital Electrocardiography (CODE) Study. Glob Heart. 2020;15(1):48. doi: 10.5334/gh.772.
• In a 10-year follow-up of 1462 individuals aged ≥ 60 years (mean age, 69 years; 61% women) included in 1997 in the Bambuí Cohort Study, AF or flutter was independently associated with an increase in all-cause mortality (HR, 2.35; 95% CI, 1.53-3.62) among patients with and without ChD (HR,1.92; 95% CI, 1.05-3.51). 240240. Ribeiro ALP, Marcolino MS, Prineas RJ, Lima-Costa MF. Electrocardiographic Abnormalities in Elderly Chagas Disease Patients: 10-Year Follow-Up of the Bambui Cohort Study of Aging. J Am Heart Assoc. 2014;3(1):e000632. doi: 10.1161/JAHA.113.000632.
• In the GARFIELD-AF, a worldwide hospital-based study that included 1061 patients in Brazil (≥18 years) who had AF diagnosed within the previous 6 weeks and at least one additional risk factor for stroke, the all-cause mortality rate per 100-person-years was 6.19 (CI 95%, 4.83-7.94), and 38.7% were cardiovascular deaths. 237237. Jerjes-Sanchez C, Corbalan R, Barretto ACP, Luciardi HL, Allu J, Illingworth L, Pieper KS, Kayani G; GARFIELD-AF Investigators. Stroke prevention in patients From Latin American Countries With Non-Valvular Atrial Fibrillation: Insights From the GARFIELD-AF Registry. Clin Cardiol. 2019;42(5):553-60. doi: 10.1002/clc.23176.
Burden of Disease
• According to GBD 2019 estimates, AF resulted in 230 116 (95% UI, 189 167 – 279 885) DALYs in Brazil in 2019, representing 0.35% of all DALYs. The age-standardized DALY rate was 103 (95% UI, 84-125) per 100 000 in 2019, greater for men (110; 95% UI 86-138) than for women (96; 95% UI, 78-115), although the proportion of DALYs is higher for women (0.42%; 95% UI, 0.35-0.48) than for men (0.30%; 95% UI, 0.24-0.37) (Table 6-5).
• Chart 6-1 and Table 6-4 reveal the same pattern for mortality rates: while the age-standardized mortality rate remained stable from 1990 to 2019, the crude rate increased.
Complications
Stroke
• Of all 429 cases of stroke (87.2% ischemic strokes) that occurred in the city of Joinville in 2015 and were included in a registry, AF was detected in 11.4% of all patients and in 58% of the cardioembolic strokes. 241241. Amaral CHD, Amaral AR, Nagel V, Venancio V, Garcia AC, Magalhaes PS, Longo AL, Moro CH, Reis FI, D’Avila A, Cabral NL. Incidence and Functional Outcome of Atrial Fibrillation and Non-Atrial Fibrillation- Related Cardioembolic Stroke in Joinville, Brazil: A Population-Based Study. Arq Neuropsiquiatr. 2017;75(5):288-94. doi: 10.1590/0004-282X20170039. Similarly, AF was detected in 58% of 359 patients with cardioembolic stroke from a one-center, consecutive sample in the city of Curitiba, Brazil. 242242. Lange MC, Ribas G, Scavasine V, Ducci RD, Mendes DC, Zétola VHF, Cabral N, Rundek T. Stroke Recurrence in the Different Subtypes of Ischemic Stroke. The Importance of the Intracranial Disease. Arq Neuropsiquiatr. 2018;76(10):649-53. doi: 10.1590/0004-282X20180095.
• Age (OR=1.04; 95% CI, 1.02-1.08), National Institutes of Health Stroke Scores on admission (OR=1.10; 95% CI, 1.05-1.16), and the presence of left atrial enlargement (OR=2.5; 95% CI, 1.01-6.29) were predictors of AF (C-statistic, 0.76; 95% CI, 0.69-0.83) among patients hospitalized for acute ischemic stroke or TIA in a Brazilian cohort. 243243. Figueiredo MM, Rodrigues AC, Alves MB, Cendoroglo Neto M, Silva GS. Score for Atrial Fibrillation Detection in Acute Stroke and Transient Ischemic Attack Patients in a Brazilian Population: the Acute Stroke Atrial Fibrillation Scoring System. Clinics. 2014;69(4):241-6. doi: 10.6061/clinics/2014(04)04.
• In a cohort of 1121 ischemic stroke patients in a 12-year follow-up, AF was independently associated with increased overall (HR 1.82; 95% CI, 1.43-2.31) and cardiovascular (HR 2.07; 95% CI, 1.36-3.14) mortality. 244244. Goulart AC, Olmos RD, Santos IS, Tunes G, Alencar AP, Thomas N, Lip GY, Lotufo PA, Benseñor IM. The Impact of Atrial Fibrillation and Long-Term Oral Anticoagulant Use on All-Cause and Cardiovascular Mortality: A 12-Year Evaluation of the Prospective Brazilian Study of Stroke Mortality and Morbidity. Int J Stroke. 2021:1747493021995592. doi: 10.1177/1747493021995592.
Dementia
• In a cross-sectional study with 1524 participants aged >65 years, dementia was diagnosed in 11% of those with AF versus 4% among those without AF (p=0.07); the authors found an odds ratio of dementia of 2.8 (95% CI, 1.0-8.1; p = 0.06) among subjects with AF. 245245. Kawabata-Yoshihara LA, Scazufca M, Santos Ide S, Whitaker A, Kawabata VS, Benseñor IM, Menezes PR, Lotufo PA. Atrial Fibrillation and Dementia: Results From the Sao Paulo Ageing & Health Study. Arq Bras Cardiol. 2012;99(6):1108-14. doi: 10.1590/s0066-782x2012005000106.
https://doi.org/10.1590/s0066-782x201200...
Association of Risk Factors for AF/Flutter
• According to the GBD Study 2019, AF deaths were attributed to six risk factors in 1990 and 2019: high blood pressure, high body mass index, dietary risks, alcohol use, tobacco, and other environmental risks. For both sexes, high systolic blood pressure was the most important risk factor for death due to AF, accounting for 35.8% (95% UI, 29.7-42.2) of deaths for men and 34.4% (95% UI, 27.5-41.7) for women in 2019. High body mass index ranked 2 for both sexes and was responsible for 23.9% of AF deaths (95% UI, 12-38) in men and 28.8% (95% UI, 16.7-43.2%) in women, in 2019. Importantly, while the risk attributed to high blood pressure increased slightly from 1990 to 2019 (7.1% change for men and 10.7% for women), the AF deaths attributable to high body mass index are increasing steeply (74.4% change for men and 79.5% for women). The risk for death from AF attributable to alcohol use is also rising, particularly for women (Chart 6-3).
• Data from the Telehealth Network of Minas Gerais with ECGs of 1 558 421 individuals (mean age, 51±18 years; 40.2% men) performed between 2010 and 2017 revealed in multivariable models adjusted for age and sex that the following self-reported comorbidities related to the presence of AF: ChD (OR 3.08; 95% CI, 2.91-3.25), previous myocardial infarction (OR 1.74; 95% CI, 1.56-1.93), chronic obstructive pulmonary disease (OR 1.48; 95% CI, 1.33-1.66), hypertension (OR 1.31; 95% CI, 1.27-1.34), dyslipidemia (OR 1.09; 95% CI, 1.03-1.16). Current smoking and diabetes were not associated with prevalent AF. 236236. Paixão GMM, Silva LGS, Gomes PR, Lima EM, Ferreira MPF, Oliveira DM, Ribeiro MH, Ribeiro AH, Nascimento JS, Canazart JA, Ribeiro LB, Benjamin EJ, Macfarlane PW, Marcolino MS, Ribeiro ALP. Evaluation of Mortality in Atrial Fibrillation: Clinical Outcomes in Digital Electrocardiography (CODE) Study. Glob Heart. 2020;15(1):48. doi: 10.5334/gh.772.
• A cross-sectional study comparing AF subjects with healthy controls found a higher frequency of sleep apnea in the AF group than in the control group (81.6% versus 60%, p = 0.03). 246246. Braga B, Poyares D, Cintra F, Guilleminault C, Cirenza C, Horbach S, Macedo D, Silva R, Tufik S, Paola AA. Sleep-Disordered Breathing and Chronic Atrial Fibrillation. Sleep Med. 2009;10(2):212-6. doi: 10.1016/j.sleep.2007.12.007.
Associated Comorbidities
Atrial Fibrillation and Other Heart Diseases
• The incidence of AF among 300 elderly patients (mean age, 75±8 years; 56% women) monitored with pacemakers, free from AF at baseline, was 22% in a 435-day follow-up 247247. Lima C, Martinelli M, Peixoto GL, Siqueira SF, Wajngarten M, Silva RT, Costa R, Filho R, Ramires JA. Silent Atrial Fibrillation in Elderly Pacemaker Users: A Randomized Trial Using Home Monitoring. Ann Noninvasive Electrocardiol. 2016;21(3):246-55. doi: 10.1111/anec.12294. and reached 85% of the patients with pacemakers and chronic kidney disease in a 1-year follow-up. 248248. Kiuchi MG, Chen S, Silva GR, Paz LMR, Souto GLL. Register of Arrhythmias in Patients With Pacemakers and Mild to Moderate Chronic Kidney Disease (RYCKE): Results From an Observational Cohort Study. Relampa. 2016;29(2):49-56.
• On echocardiogram, AF was associated with heart disease (OR = 3.9; 95% CI, 2.1 - 7.2, p <0.001) in 1518 patients (mean age, 58±16 years; 66% female) from a waiting list for echocardiogram in primary care, who were also screened for AF with a portable device (AF prevalence of 6.4%). The authors suggest that AF screening could be a useful primary care tool to stratify risk and prioritize echocardiography. 228228. Diamantino AC, Nascimento BR, Beaton AZ, Nunes MCP, Oliveira KKB, Rabelo LC, Barbosa MM, Tompsett AR, Olivieri L, Mata MD, Costa WAA, Pereira AF, Diamantino LC, Ribeiro ALP, Sable C, Brant LCC. Atrial Fibrillation Detection With a Portable Device During Cardiovascular Screening in Primary Care. Heart. 2020;106(16):1261-66. doi: 10.1136/heartjnl-2019-316277.
• Heart failure and AF coexist in many patients as they share similar pathophysiological pathways. In a retrospective study of 659 patients hospitalized for decompensated HF in 2011, the AF prevalence was 40% (73% permanent AF), and AF was associated with increasing age (p < 0.0001), non-ischemic etiology (p = 0.02), right ventricular dysfunction (p = 0.03), lower systolic blood pressure (p = 0.02), higher ejection fraction (p < 0.0001), and enlarged left atrium (p < 0.0001). Patients with AF had longer hospital length of stay (20.5 ± 16 days versus 16.3 ± 12, p = 0.001). 249249. Mendes FS, Atié J, Garcia MI, Gripp EA, Sousa AS, Feijó LA, Xavier SS. Atrial Fibrillation in Decompensated Heart Failure: Associated Factors and In-Hospital Outcome. Arq Bras Cardiol. 2014;103(4):315-22. doi: 10.5935/abc.20140123.
• Of the patients with cardiovascular disease visiting the emergency department, the prevalence of AF was 40% among patients with decompensated HF 2222. Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for Enhancing Public Health Utility of National Causes-of-Death Data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. and 44% among those with valvular heart disease. 182182. Moraes RC, Katz M, Tarasoutchi F. Clinical and Epidemiological Profile of Patients With Valvular Heart Disease Admitted to the Emergency Department. Einstein. 2014;12(2):154-8. doi: 10.1590/s1679-45082014ao3025.
• A study including critically ill patients found an AF incidence of 11% during their intensive care unit stay. 250250. Duarte PAD, Leichtweis GE, Andriolo L, Delevatti YA, Jorge AC, Fumagalli AC, Santos LC, Miura CK, Saito SK. Factors Associated With the Incidence and Severity of New-Onset Atrial Fibrillation in Adult Critically Ill Patients. Crit Care Res Pract. 2017;2017:8046240. doi: 10.1155/2017/8046240.
Perioperative Atrial Fibrillation and Cardiovascular Surgery
• Of patients undergoing cardiac surgery, 12% to 33% had AF in the postoperative period. 204204. Pivatto F jR, Teixeira Filho GF, Sant’anna JR, Py PM, Prates PR, Nesralla IA, Kalil RA. Advanced age and Incidence of Atrial Fibrillation in the Postoperative Period of Aortic Valve Replacement. Rev Bras Cir Cardiovasc. 2014;29(1):45-50. doi: 10.5935/1678-9741.20140010. , 251251. Barbieri LR, Sobral ML, Gerônimo GM, Santos GG, Sbaraíni E, Dorfman FK, Stolf NA. Incidence of Stroke and Acute Renal Failure in Patients of Postoperative Atrial Fibrillation After Myocardial Revascularization. Rev Bras Cir Cardiovasc. 2013;28(4):442-8. doi: 10.5935/1678-9741.20130073. , 252252. Bohatch MS Jr, Matkovski PD, Di Giovanni FJ, Fenili R, Varella EL, Dietrich A. Incidence of Postoperative Atrial Fibrillation in Patients Undergoing On-Pump and Off-Pump Coronary Artery Bypass Grafting. Rev Bras Cir Cardiovasc. 2015;30(3):316-24. doi: 10.5935/1678-9741.20150040. Surgeries for valve replacement were associated with a higher occurrence of AF (31-33%) as compared to CABG (12-16%) during hospitalization.
• Advanced age, mitral valve disease, and no beta-blocker use were associated with postoperative AF in valvular surgery. 205205. Sá MP, Sá MV, Albuquerque AC, Silva BB, Siqueira JW, Brito PR, Ferraz PE, Lima Rde C. Predicting Risk of Atrial Fibrillation After Heart Valve Surgery: Evaluation of a Brazilian Risk Score. Rev Bras Cir Cardiovasc. 2012;27(1):117-22. doi: 10.5935/1678-9741.20120017. Among those who underwent CABG, the postoperative AF incidence was associated with left atrial > 40.5mm and age > 64.5 years. 253253. Folla CO, Melo CC, Silva RC. Predictive Factors of Atrial Fibrillation After Coronary Artery Bypass Grafting. Einstein. 2016;14(4):480-85. doi: 10.1590/S1679-45082016AO3673.
Atrial Fibrillation and Chagas Disease
• AF has been consistently associated with ChD and increases the risk of death in ChD patients. 254254. Marcolino MS, Palhares DM, Ferreira LR, Ribeiro ALP. Electrocardiogram and Chagas Disease: A Large Population Database of Primary Care Patients. Glob Heart. 2015;10(3):167-72. doi: 10.1016/j.gheart.2015.07.001. In the Bambuí Cohort Study, 1462 participants aged ≥ 60 years (mean age, 69 years; ChD n=557, 38.1%), with baseline ECG, were followed up for 10 years. AF was more frequently observed in ChD subjects [6.1% vs 3.4% (OR: 3.43; 95% CI, 1.87-6.32, adjusted for age, sex, and clinical variables)], in whom it was an independent risk factor for death (HR: 2.35; 95% CI, 1.53-3.62 adjusted for age, sex, clinical variables and BNP levels). 240240. Ribeiro ALP, Marcolino MS, Prineas RJ, Lima-Costa MF. Electrocardiographic Abnormalities in Elderly Chagas Disease Patients: 10-Year Follow-Up of the Bambui Cohort Study of Aging. J Am Heart Assoc. 2014;3(1):e000632. doi: 10.1161/JAHA.113.000632.
• In a large sample of 264 324 patients undergoing tele-ECG in primary health care units in 2011, ChD was self-reported by 7590 (2.9%). The mean age of ChD subjects was 57.0 ± 13.7 years, while that of non-ChD subjects was 50.4 ± 19.1 years, with 5% of octogenarians in both groups. AF was observed in 5.35% of the ChD subjects and in 1.65% of non-ChD ones (OR: 3.15; 95% CI, 2.83-3.51, adjusted for age, sex, and self-reported comorbidities). 254254. Marcolino MS, Palhares DM, Ferreira LR, Ribeiro ALP. Electrocardiogram and Chagas Disease: A Large Population Database of Primary Care Patients. Glob Heart. 2015;10(3):167-72. doi: 10.1016/j.gheart.2015.07.001.
• Rojas et al . evaluated, in a systematic review and meta-analysis, the frequency of electrocardiographic abnormalities in ChD in the general population. Forty-nine studies were selected, including 34 023 individuals (12 276 ChD and 21 747 non-ChD). The AF prevalence was significantly higher in ChD patients (OR: 2.11; 95% CI, 1.40-3.19). 256256. Rojas LZ, Glisic M, Pletsch-Borba L, Echeverría LE, Bramer WM, Bano A, Stringa N, Zaciragic A, Kraja B, Asllanaj E, Chowdhury R, Morillo CA, Rueda-Ochoa OL, Franco OH, Muka T. Electrocardiographic Abnormalities in Chagas Disease in the General Population: A Systematic Review and Meta-Analysis. PLoS Negl Trop Dis. 2018;12(6):e0006567. doi: 10.1371/journal.pntd.0006567.
• In a sample of 424 ChD patients under the age of 70 years (41.7% female; mean age, 47±11 years), followed up for 7.9 ± 3.2 years, Rassi et al . found an AF prevalence of 13.3±3.1% and a strong association with the risk of death [HR: 5.43 (2.91–10.13)] on univariate analysis. 257257. Rassi A Jr, Rassi A, Little WC, Xavier SS, Rassi SG, Rassi AG, Rassi GG, Hasslocher-Moreno A, Sousa AS, Scanavacca MI. Development and Validation of a Risk Score for Predicting Death in Chagas’ Heart Disease. N Engl J Med. 2006;355(8):799-808. doi: 10.1056/NEJMoa053241.
Health Care Utilization and Cost
(Refer to Tables 1-6 through 1-9 and Charts 1-15 and 1-16)
• From 2008 to 2019, there were 354 619 hospitalizations for AF, and 1413 ablation procedures for AF and atrial flutter were performed by the SUS, with unadjusted costs of R$ 260 593 600 and R$ 7 912 561, respectively. After adjusting for Brazilian inflation, the costs were R$ 451 530 532 and R$ 13 710 094, respectively, and, in international dollars, converted to PPP-adjusted to US$ 2019, $ 169 076 584 and $ 5 047 822, respectively.
• An analysis of the economic burden of heart conditions in Brazil estimated an AF prevalence of 0.8% (n=1 202 151 cases) in 2015. The authors estimated a total cost for AF of R$ 3.921 billion (US$ 1.2 billion), 94% due to direct healthcare costs. 124124. Stevens B, Pezzullo L, Verdian L, Tomlinson J, George A, Bacal F. The Economic Burden of Heart Conditions in Brazil. Arq Bras Cardiol. 2018;111(1):29-36. doi: 10.5935/abc.20180104.
• A study on data from a private outpatient clinic regarding anticoagulation analyzed the annual cost per AF patient (n=1220; mean age, 64 years) and found that 64% of all costs (US$ 10 679) during a 1.5-year follow-up were attributed to inpatient costs. 258258. Silva PGMBE, Sznejder H, Vasconcellos R, Charles GM, Mendonca-Filho HTF, Mardekian J, Nascimento R, Dukacz S, Fusco MD. Anticoagulation Therapy in Patients With Non-valvular Atrial Fibrillation in a Private Setting in Brazil: A Real-World Study. Arq Bras Cardiol. 2020 Mar;114(3):457-466. doi: 10.36660/abc.20180076.
Awareness, Treatment, and Control
Anticoagulation
• There was a high variation in the use of anticoagulation in patients with AF, from 1.5% to 91%. Studies with samples from primary care were more likely to have low anticoagulation use as compared to samples recruited from tertiary centers or cardiologists, as detailed below.
• Of the 4638 subjects with AF in primary care centers of 658 municipalities of the Minas Gerais state (mean age, 70±14 years; 54% men), who underwent ECG using telehealth in 2011, VKA use was reported by 1.5% and aspirin, by 3.1%. 233233. Marcolino MS, Palhares DM, Benjamin EJ, Ribeiro ALp. Atrial Fibrillation: Prevalence in a Large Database of Primary Care Patients in Brazil. Europace. 2015;17(12):1787-90. doi: 10.1093/europace/euv185.
• Of 125 primary care centers from nine states in four Brazilian regions, from January 2009 to April 2016, a subset of 301 patients had AF, 189 (63%) of whom were at high risk for stroke; only 28 (15%) were regular oral anticoagulant users, and 102 (54%) were on aspirin. 234234. Moraes ERFL, Cirenza C, Lopes RD, Carvalho AC, Guimaraes PO, Rodrigues AAE, Paola AAV. Prevalence of Atrial Fibrillation and Stroke Risk Assessment Based on Telemedicine Screening Tools in a Primary Healthcare Setting. Eur J Intern Med. 2019;67:36-41. doi: 10.1016/j.ejim.2019.04.024.
• In the GARFIELD-AF registry, of the 1061 patients included (82.3% by cardiologists) in Brazil between 2010 and 2014 (mean age, 68±13 years; 55% males), 86% had CHA2DS2-VASc score ≥ 2, 19% were not using anticoagulation therapy at baseline, 26% were only receiving antiplatelet therapy, 29% were using VKA, and 26% were receiving NOAC. 237237. Jerjes-Sanchez C, Corbalan R, Barretto ACP, Luciardi HL, Allu J, Illingworth L, Pieper KS, Kayani G; GARFIELD-AF Investigators. Stroke prevention in patients From Latin American Countries With Non-Valvular Atrial Fibrillation: Insights From the GARFIELD-AF Registry. Clin Cardiol. 2019;42(5):553-60. doi: 10.1002/clc.23176.
• The IMPACT-AF, 259259. Vinereanu D, Lopes RD, Bahit MC, Xavier D, Jiang J, Al-Khalidi HR, He W, Xian Y, Ciobanu AO, Kamath DY, Fox KA, Rao MP, Pokorney SD, Berwanger O, Tajer C, Silva PGMB, Roettig ML, Huo Y, Granger CB; IMPACT-AF Investigators. A Multifaceted Intervention to Improve Treatment With Oral Anticoagulants in Atrial Fibrillation (IMPACT-AF): An International, Cluster-Randomised Trial. Lancet. 2017;390(10104):1737-1746. doi: 10.1016/S0140-6736(17)32165-7.
https://doi.org/10.1016/S0140-6736(17)32...
a clustered randomized trial to improve treatment with anticoagulants in patients with AF conducted in Argentina, Brazil, China, India, and Romania, showed that two-thirds of the patients were on oral anticoagulation at baseline: 83% were on a VKA and 15% were on NOAC. The patients from Brazil (n=360) were most often on oral anticoagulation at baseline (91%) and 27% were on NOAC. Of all patients taking VKA in Brazil, 40.3% had INR values between 2 and 3 prior to the baseline visit.
• A stroke registry in the city of Joinville described all 429 cases of stroke that occurred in 2015, and AF was detected in 49 (11.4%) patients. Of the 26 patients with known prior AF, 19 (73%) were not anticoagulated, 20 (77%) had a CHA2DS2-VASc score ≥ 3, and 21 (81%) had a HAS-BLED score < 3. 241241. Amaral CHD, Amaral AR, Nagel V, Venancio V, Garcia AC, Magalhaes PS, Longo AL, Moro CH, Reis FI, D’Avila A, Cabral NL. Incidence and Functional Outcome of Atrial Fibrillation and Non-Atrial Fibrillation- Related Cardioembolic Stroke in Joinville, Brazil: A Population-Based Study. Arq Neuropsiquiatr. 2017;75(5):288-94. doi: 10.1590/0004-282X20170039.
• In a cohort of 1121 ischemic stroke patients, 200 of whom had AF, anticoagulation for AF was inversely associated with all-cause mortality (oral anticoagulant time-dependent effect: multivariable HR, 0.47; 95% CI, 0.30–0.50) and stroke mortality (oral anticoagulant time-dependent effect ≥ 6 months: multivariable OR, 0.09; 95% CI, 0.01–0.65), but not with cardiovascular mortality. 244244. Goulart AC, Olmos RD, Santos IS, Tunes G, Alencar AP, Thomas N, Lip GY, Lotufo PA, Benseñor IM. The Impact of Atrial Fibrillation and Long-Term Oral Anticoagulant Use on All-Cause and Cardiovascular Mortality: A 12-Year Evaluation of the Prospective Brazilian Study of Stroke Mortality and Morbidity. Int J Stroke. 2021:1747493021995592. doi: 10.1177/1747493021995592.
• The quality of warfarin therapy has been evaluated using the parameter TTR in different samples in Brazil. The TTR of anticoagulation for AF has ranged from 31% to 67% in the studies. 258258. Silva PGMBE, Sznejder H, Vasconcellos R, Charles GM, Mendonca-Filho HTF, Mardekian J, Nascimento R, Dukacz S, Fusco MD. Anticoagulation Therapy in Patients With Non-valvular Atrial Fibrillation in a Private Setting in Brazil: A Real-World Study. Arq Bras Cardiol. 2020 Mar;114(3):457-466. doi: 10.36660/abc.20180076. , 260260. Silva RMFLD, Silva PAE, Lima MC, Sant’Anna LT, Silva TC, Moreira PHV, Gandra RM, Cavalcanti TR, Mourão PHV. Thromboembolism and Bleeding Risk Scores and Predictors of Cardiac Death in a Population With Atrial Fibrillation. Arq Bras Cardiol. 2017;109(1):5-13. doi: 10.5935/abc.20170064. Anticoagulation Therapy in Patients with Non-valvular Atrial Fibrillation in a Private Setting in Brazil: A Real-World Study 258258. Silva PGMBE, Sznejder H, Vasconcellos R, Charles GM, Mendonca-Filho HTF, Mardekian J, Nascimento R, Dukacz S, Fusco MD. Anticoagulation Therapy in Patients With Non-valvular Atrial Fibrillation in a Private Setting in Brazil: A Real-World Study. Arq Bras Cardiol. 2020 Mar;114(3):457-466. doi: 10.36660/abc.20180076. , 260260. Silva RMFLD, Silva PAE, Lima MC, Sant’Anna LT, Silva TC, Moreira PHV, Gandra RM, Cavalcanti TR, Mourão PHV. Thromboembolism and Bleeding Risk Scores and Predictors of Cardiac Death in a Population With Atrial Fibrillation. Arq Bras Cardiol. 2017;109(1):5-13. doi: 10.5935/abc.20170064. Age >65 years, but not health literacy, was associated with a higher TTR value. 262262. Marcatto LR, Sacilotto L, Darrieux FC, Hachul DT, Scanavacca MI, Krieger JE, Pereira AC, Santos PC. Age is Associated With Time in Therapeutic Range for Warfarin Therapy in Patients With Atrial Fibrillation. Oncotarget. 2016;7(34):54194-99. doi: 10.18632/oncotarget.10944. In a retrospective analysis of 1220 patients from the private setting, those with low TTR had more severe bleeding and 40% higher health costs in a median 1.5-year follow-up. 258258. Silva PGMBE, Sznejder H, Vasconcellos R, Charles GM, Mendonca-Filho HTF, Mardekian J, Nascimento R, Dukacz S, Fusco MD. Anticoagulation Therapy in Patients With Non-valvular Atrial Fibrillation in a Private Setting in Brazil: A Real-World Study. Arq Bras Cardiol. 2020 Mar;114(3):457-466. doi: 10.36660/abc.20180076.
Rhythm or Rate Control (Medication, Cardioversion, Catheter Ablation)
• A cross-sectional study with 167 AF patients found that rate control was more common than rhythm control as treatment strategy (79% vs. 21%; p < 0.001). Among those in rhythm control, amiodarone (43%), sotalol (16%), and propafenone (14%) were the most prescribed drugs. Beta-blockers were prescribed in 81% of the patients on rate control. 264264. Oliveira LH, Mallmann FB, Botelho FN, Paul LC, Gianotto M, Abt RB, Silva NJ, Luize CM, Nogueira FL, Carvalho RS, Paola AA, Cirenza C. Cross-Sectional Study of Treatment Strategies on Atrial Fibrillation. Arq Bras Cardiol. 2012;98(3):195-202. doi: 10.1590/s0066-782x2012005000020. Amiodarone was mentioned by 83% of doctors as the choice for the rhythm control strategy. 265265. van der Sand CR, Leiria TL, Kalil RA. Assessment of the Adherence of Cardiologists to Guidelines for the Treatment of Atrial Fibrillation. Arq Bras Cardiol. 2013;101(2):127-33. doi: 10.5935/abc.20130148.
• Data from 125 primary care centers showed that of 301 patients with AF, 91 (30.2%) were receiving neither rate nor rhythm control therapy. Of the remaining 210 patients undergoing treatment, 147 (70%) used rate control agents (beta-blockers, digoxin, diltiazem, or verapamil) and 25 (12%) used at least one antiarrhythmic drug (amiodarone or propafenone). The simultaneous use of antiarrhythmic drugs and beta-blockers was reported by 36 (17%). 234234. Moraes ERFL, Cirenza C, Lopes RD, Carvalho AC, Guimaraes PO, Rodrigues AAE, Paola AAV. Prevalence of Atrial Fibrillation and Stroke Risk Assessment Based on Telemedicine Screening Tools in a Primary Healthcare Setting. Eur J Intern Med. 2019;67:36-41. doi: 10.1016/j.ejim.2019.04.024.
Future Research
• Ongoing cohort studies have the potential to fill information gaps on incidence, risk factors, risk prediction, and prevention of AF in Brazil. To our knowledge, there is no original published study with information on the AF incidence in Brazil or longitudinal data on risk factors.
• Studies designed to screen AF in population-based or selected populations using ECG or screening devices are ongoing and should bring information on the relevance of including this strategy in primary care or specialized centers.
• The First Brazilian Cardiovascular Registry of Atrial Fibrillation, the RECALL study, finished the inclusion of 4584 patients in 2019 and its results are awaited. It will be the largest Brazilian registry regarding AF patient characteristics and treatment from 73 centers from all Brazilian geographic regions. 266266. Lopes RD, Paola AA, Lorga Filho AM, Consolim-Colombo FM, Andrade J, Mattos LAP, Bernardez-Pereira S, Berwanger O, Figueiredo MJO; RECALL Steering Committee and Investigators. Rationale and Design of the First Brazilian Cardiovascular Registry of Atrial Fibrillation: The RECALL study. Am Heart J. 2016;176:10-6. doi: 10.1016/j.ahj.2016.03.001.
• Implementation strategies to enhance anticoagulation use among AF patients should be encouraged, particularly in primary care settings.
• Studies using artificial intelligence to diagnose or predict AF may be a tool to improve AF diagnosis and personalize screening strategies.
7. HYPERTENSION
ICD-10 - I10
See Tables 7-1 through 7-6 and Charts 7-1 through 7-7
| CI | Confidence Interval |
| CVD | Cardiovascular Disease |
| DALYs | Disability-Adjusted Life Years |
| DBP | Diastolic Blood Pressure |
| ELSA | English Longitudinal Study of Ageing |
| ELSA-Brasil | Brazilian Longitudinal Study of Adult Health (in Portuguese , Estudo Longitudinal de Saúde do Adulto ) |
| ERICA | Brazilian Study of Cardiovascular Risk in Adolescents (in Portuguese, Estudo dos Riscos Cardiovasculares em Adolescentes ) |
| FU | Federative Unit |
| GBD | Global Burden of Disease |
| HIPERDIA | SUS’ Program for Arterial Hypertension and Diabetes |
| HR | Hazard Ratio |
| HRQOL | Health-Related Quality of Life |
| IBGE | Brazilian Institute of Geography and Statistics (in Portuguese, Instituto Brasileiro de Geografia e Estatística ) |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems, 10thRevision |
| IPAQ | International Physical Activity Questionnaire |
| OR | Odds Ratio |
| PR | Prevalence Ratio |
| SBC | Brazilian Society of Cardiology (in Portuguese, Sociedade Brasileira de Cardiologia) |
| SBP | Systolic Blood Pressure |
| SDI | Sociodemographic Index |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| UI | Uncertainty Interval |
| YLD | Years Lived with Disability |
| YLL | Years of Life Lost |
– Rates of self-reported hypertension in individuals aged 18 years or more and 95% confidence intervals, by sex, in Brazil, its regions, Federative Units and residence areas (urban or rural), 2019.
– Rates of self-reported hypertension in individuals aged 18 years or more and 95% confidence intervals, according to sociodemographic variables, Brazil, 2019.
– Number of deaths, age-standardized mortality rates (per 100 000) due to high systolic blood pressure from all causes, and percent change of rates, Brazil, 1990 and 2019.
– Age-standardized mortality rates (per 100 000) due to high systolic blood pressure from all causes, and percent change of rates, by sex, in Brazil and its Federative Units, 1990 and 2019.
– Number of deaths, age-standardized mortality rates (per 100 000) due to high systolic blood pressure from cardiovascular diseases, and percent change of rates, by age group. Brazil, 1990 and 2019.
– Number of deaths (A) and mortality rates (B) attributable to high systolic blood pressure in Brazil, 1990-2019.
– Proportional mortality due to high systolic blood pressure according to age groups, by sex, in Brazil, 2019.
– Age-standardized mortality rates of diseases attributable to high systolic blood pressure, stratified by all causes, in Brazil, 1990 and 2019.
– Age-standardized mortality rates of diseases attributable to elevated systolic blood pressure, stratified by cardiovascular diseases, in Brazil, 1990 and 2019.
– Correlation between the 2019 sociodemographic index (SDI) and the percent change of mortality rates from cardiovascular disease attributable to high systolic blood pressure from 1990 to 2019, in Brazil.
– Absolute number of YLLs (A), YLDs (B), and DALYs (C) due to hypertension, in Brazil, 1990-2020.
Overview
• For standardization purposes, in this document arterial hypertension was characterized as sustained blood pressure levels equal to or greater than 140 mm Hg for SBP and/or equal to or greater than 90 mm Hg for DBP. 267267. Barroso WKS, Rodrigues CIS, Bortolotto LA, Mota-Gomes MA, Brandão AA, Feitosa ADM, Machado CA, Poli-de-Figueiredo CE, Amodeo C, Mion D Jr, Barbosa ECD, Nobre F, Guimarães ICB, Vilela-Martin JF, Yugar-Toledo JC, Magalhães MEC, Neves MFT, Jardim PCBV, Miranda RD, Póvoa RMDS, Fuchs SC, Alessi A, Lucena AJG, Avezum A, Sousa ALL, Pio-Abreu A, Sposito AC, Pierin AMG, Paiva AMG, Spinelli ACS, Nogueira ADR, Dinamarco N, Eibel B, Forjaz CLM, Zanini CRO, Souza CB, Souza DDSM, Nilson EAF, Costa EFA, Freitas EV, Duarte EDR, Muxfeldt ES, Lima Júnior E, Campana EMG, Cesarino EJ, Marques F, Argenta F, Consolim-Colombo FM, Baptista FS, Almeida FA, Borelli FAO, Fuchs FD, Plavnik FL, Salles GF, Feitosa GS, Silva GVD, Guerra GM, Moreno Júnior H, Finimundi HC, Back IC, Oliveira Filho JB, Gemelli JR, Mill JG, Ribeiro JM, Lotaif LAD, Costa LSD, Magalhães LBNC, Drager LF, Martin LC, Scala LCN, Almeida MQ, Gowdak MMG, Klein MRST, Malachias MVB, Kuschnir MCC, Pinheiro ME, Borba MHE, Moreira Filho O, Passarelli Júnior O, Coelho OR, Vitorino PVO, Ribeiro RM Jr, Esporcatte R, Franco R, Pedrosa R, Mulinari RA, Paula RB, Okawa RTP, Rosa RF, Amaral SLD, Ferreira-Filho SR, Kaiser SE, Jardim TSV, Guimarães V, Koch VH, Oigman W, Nadruz W. Brazilian Guidelines of Hypertension - 2020. Arq Bras Cardiol. 2021;116(3):516-658. doi: 10.36660/abc.20201238.
https://doi.org/10.36660/abc.20201238...
The percentage prevalence values will be presented, followed by 95% CIs or 95% UIs, as available in the cited studies.
• In population studies, hypertension can be either measured or self-reported. The former derives from direct blood pressure measurement using standardized techniques and is described in each document, while self-reported hypertension is characterized by a positive answer to a question about the presence of that medical diagnosis or by a positive answer regarding the use of antihypertensive medications, 268268. Malta DC, Gonçalves RPF, Machado ÍE, Freitas MIF, Azeredo C, Szwarcwald CL. Prevalence of Arterial Hypertension According to Different Diagnostic Criteria, National Health Survey. Rev Bras Epidemiol. 2018;21(Suppl 1):e180021. doi: 10.1590/1980-549720180021.supl.1. depending, therefore, on the patient’s access to the diagnosis and understanding of this information.
• When the GBD Study is the data source, the risk is attributable to high SBP, as described in a previous publication. 269269. Brant LCC, Nascimento BR, Veloso GA, Gomes CS, Polanczyk CA, Oliveira GMM, Ribeiro ALP, malta DC. Burden of Cardiovascular Diseases Attributable to Risk Factors in Brazil: Data From the Global Burden of Disease 2019. Rev Soc Bras Med Trop. 2021;2021(54). Epub ahead of print.
Prevalence and Incidence
Incidence
• In a 2021 study by Lopes et al. analyzing 8154 participants from the ELSA-Brasil study, the incidence of hypertension per 1000 person-years was 43.2, 51.6 in men and 37.3 in women. Still, the incidence per 1000 person-years was higher in the ‘70-74 years’ age group (88.8), in black (55.9), obese (79.7), or diabetic (91.4) individuals, and in those with lower socioeconomic status (58.9). 270270. Lopes JAS, Giatti L, Griep RH, Lopes AADS, Matos SMA, Chor D, Fonseca MJM, Barreto SM. Life Course Socioeconomic Position, Intergenerational Social Mobility, and Hypertension Incidence in ELSA-Brasil. Am J Hypertens. 2021;34(8):801-9. doi: 10.1093/ajh/hpab029.
Prevalence
• Data on the prevalence of hypertension may differ between studies, depending on the type of research and the study population, especially in a country with continental dimensions and substantial miscegenation like Brazil.
Measured Hypertension
• According to Malta et al ., in an analysis of the 2013 National Health Survey data, the prevalence of measured hypertension in individuals older than 18 years was 22.8% (95% CI, 22.1 - 23.4%) in a sample of 59 402 individuals. 271271. Malta DC, Santos NB, Perillo RD, Szwarcwald CL. Prevalence of High Blood Pressure Measured in the Brazilian Population, National Health Survey, 2013. Sao Paulo Med J. 2016;134(2):163-70. doi: 10.1590/1516-3180.2015.02090911. In individuals older than 75 years, the estimated prevalence was 47.1% (95% CI, 44.1 - 50.2%), and, in an analysis stratified by sex, in the age groups between 18 years and 74 years, the prevalence was higher in men, with women showing a slight predominance only in the age group ‘above 75 years’ (47.8%, 95% CI, 43.9 -51.7 versus 46.2%, 95% CI, 41.3 - 51.3%), revealing a possible survival bias. The analysis by region showed that the Southeastern (25%, 95% CI, 23.8 - 26.1%) and Southern (25%, 95% CI, 23.5 - 26.5%) regions had the highest prevalence in both sexes. 271271. Malta DC, Santos NB, Perillo RD, Szwarcwald CL. Prevalence of High Blood Pressure Measured in the Brazilian Population, National Health Survey, 2013. Sao Paulo Med J. 2016;134(2):163-70. doi: 10.1590/1516-3180.2015.02090911.
• In the ELSA study, Chor et al . observed a hypertension prevalence of 40.1% in men and 32.2% in women, with a progressive increase with age, reaching 63.7% in individuals aged 65 years to 74 years. 66. Malta DC, Teixeira R, Oliveira GMM, Ribeiro ALP. Cardiovascular Disease Mortality According to the Brazilian Information System on Mortality and the Global Burden of Disease Study Estimates in Brazil, 2000-2017. Arq Bras Cardiol. 2020;115(2):152-160. doi: 10.36660/abc.20190867.
https://doi.org/10.36660/abc.20190867...
In addition, there was a lower prevalence in individuals with postgraduation (28.4%), when compared with those without a complete secondary education (44%), and in those with a per capita family income above USD $1000.00 (30.7%), when compared with those with an income below USD $500.00 (40.9%). The evaluation by race showed a higher prevalence among blacks (49.3%) as compared to other race/color categories. 272272. Chor D, Ribeiro ALP, Sá Carvalho M, Duncan BB, Lotufo PA, Nobre AA, Aquino EM, Schmidt MI, Griep RH, Mdel CM, Barreto SM, Passos VM, Benseñor IJ, Matos SM, Mill JG. Prevalence, Awareness, Treatment and Influence of Socioeconomic Variables on Control of High Blood Pressure: Results of the ELSA-Brasil Study. PLoS One. 2015;10(6):e0127382. doi: 10.1371/journal.pone.0127382.
• In a cross-sectional study carried out in a population from the semiarid region of the state of Pernambuco, Santiago et al. observed that the prevalence of measured hypertension was similar among individuals who were white (28.9%, 95% CI, 19.8 - 39.4%) versus those who were brown or black (27%, 95% CI, 22.3 - 32.2%). 77. Castro MC, Massuda A, Almeida G, Menezes-Filho NA, Andrade MV, Noronha KVMS, Rocha R, Macinko J, Hone T, Tasca R, Giovanella L, Malik AM, Werneck H, Fachini LA, Atun R. Brazil’s Unified Health System: The First 30 Years and Prospects for the Future. Lancet. 2019;394(10195):345-56. doi: 10.1016/S0140-6736(19)31243-7. When the education level was considered in the analysis, the prevalence was 44.6% (95% CI, 36.4 - 53%) in those who had never attended school, almost twice as high as in those who had completed elementary or secondary/higher education. The assessment by employment status showed a higher prevalence in individuals without any work activity (30.3%, 95% CI, 24.4 - 36.7%) when compared with those who worked (23.9%, 95% CI, 18.0 - 30.7%). Still, the prevalence was higher in individuals belonging to the upper and middle classes (20.5%, 95% CI, 15.3 - 26.4%) compared with those belonging to the lower class (35.2%, 95% CI, 28.5 - 42.3%). 273273. Santiago ERC, Diniz ADS, Oliveira JS, Leal VS, Andrade MIS, Lira PIC. Prevalence of Systemic Arterial Hypertension and Associated Factors Among Adults From the Semi-Arid Region of Pernambuco, Brazil. Arq Bras Cardiol. 2019;113(4):687-695. doi: 10.5935/abc.20190145.
• Barbosa et al . estimated the prevalence of hypertension and its associated factors in the less developed regions of Brazil in a cross-sectional study carried out with 835 individuals >18 years of age, who completed a structured household questionnaire. 274274. Barbosa JB, Silva AA, Santos AM, Monteiro F Jr, Barbosa MM, Barbosa MM, Figueiredo Neto JA, Soares Nde J, Nina VJ, Barbosa JN. Prevalence of Arterial Hypertension and Associated Factors in Adults in São Luís, State of Maranhão. Arq Bras Cardiol. 2008;91(4):236-42. doi: 10.1590/s0066-782x2008001600009. Measurements of blood pressure, weight, height, and waist circumference were taken, and other risk factors for CVD were assessed. Age varied from 18 to 94 years (mean age, 39.4 years), 293 (35.1%) individuals were normotensive and 313 (37.5%) were prehypertensive. The hypertension prevalence was 27.4% (95% CI, 24.4% - 30.6%) and higher among men (32.1%) than among women (24.2%). In the adjusted analysis, the following variables remained independently associated with hypertension: male sex (PR 1.52, 95% CI, 1.25 - 1.84); age ≥ 30 years (PR 6.65, 95% CI, 4.40 - 10.05 for ≥60 years of age); overweight (PR 2.09, 95% CI, 1.64 - 2.68); obesity (PR 2.68, 95% CI, 2.03 - 3.53); and diabetes (PR 1.56, 95% CI, 1.24 - 1.97). 274274. Barbosa JB, Silva AA, Santos AM, Monteiro F Jr, Barbosa MM, Barbosa MM, Figueiredo Neto JA, Soares Nde J, Nina VJ, Barbosa JN. Prevalence of Arterial Hypertension and Associated Factors in Adults in São Luís, State of Maranhão. Arq Bras Cardiol. 2008;91(4):236-42. doi: 10.1590/s0066-782x2008001600009.
Self-reported Hypertension
• Self-report is the most frequently used criterion to assess the prevalence of hypertension in Brazil. Picon et al ., in a meta-analysis involving 120 018 individuals, demonstrated that, despite different criteria for hypertension diagnosis in the 1980s and 1990s, the prevalence of hypertension reduced from 36.1% (95% CI, 28.7 - 44.2%) to 28.7% (95% CI, 26.2 - 31.4%) over 30 years. 274274. Barbosa JB, Silva AA, Santos AM, Monteiro F Jr, Barbosa MM, Barbosa MM, Figueiredo Neto JA, Soares Nde J, Nina VJ, Barbosa JN. Prevalence of Arterial Hypertension and Associated Factors in Adults in São Luís, State of Maranhão. Arq Bras Cardiol. 2008;91(4):236-42. doi: 10.1590/s0066-782x2008001600009. However, in the early 2000s, the prevalence estimate on telephone inquiries was still 20.6% (95% CI, 19.0 - 22.4%). 275275. Picon RV, Fuchs FD, Moreira LB, Riegel G, Fuchs SC. Trends in Prevalence of Hypertension in Brazil: A Systematic Review With Meta-Analysis. PLoS One. 2012;7(10):e48255. doi: 10.1371/journal.pone.0048255.
• An analysis of data from the 2013 National Health Survey showed a prevalence of hypertension in men of 18.3% (95% CI, 17.5 - 19.1%), according to the self-reported criterion, of 25.8% (95% CI, 24.8 - 26.7%), when measured by an instrument, and of 33% (95% CI, 32.1 - 34.0%), when measured by an instrument and/or use of antihypertensive medication reported. In women, the observed percentages were higher according to the self-reported criterion [24.2% (95% CI, 23.4 - 24.9%)] and lower according to all other diagnostic criteria: 20% (95% CI, 19.3 - 20.8%), when measured by an instrument, and 31.7% (95% CI, 30.9 - 32.5%), when measured by an instrument and/or use of antihypertensive medication reported. 268268. Malta DC, Gonçalves RPF, Machado ÍE, Freitas MIF, Azeredo C, Szwarcwald CL. Prevalence of Arterial Hypertension According to Different Diagnostic Criteria, National Health Survey. Rev Bras Epidemiol. 2018;21(Suppl 1):e180021. doi: 10.1590/1980-549720180021.supl.1. These differences can be explained by the fact that women seek health services more frequently and are more likely to be diagnosed with hypertension. The Southeastern and Southern regions and the urban areas of the country had the highest prevalence when the geographic regions and the area of residence were analyzed, respectively. 268268. Malta DC, Gonçalves RPF, Machado ÍE, Freitas MIF, Azeredo C, Szwarcwald CL. Prevalence of Arterial Hypertension According to Different Diagnostic Criteria, National Health Survey. Rev Bras Epidemiol. 2018;21(Suppl 1):e180021. doi: 10.1590/1980-549720180021.supl.1.
• In the VIGITEL study, 276276. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2019: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília: Ministério da Saúde; 2019. based on telephone interviews carried out in 26 capitals and in the Distrito Federal in 2019, the prevalence of hypertension was 24.5%, specifically 27.3% in women and 21.2% in men. The highest prevalence was observed in the Distrito Federal (29.6%) and the cities of Porto Alegre (27.2%) and Recife (26%) for men, and in the cities of Rio de Janeiro (32.8%), Recife (30.2%), and Salvador (30%) for women. 276276. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2019: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília: Ministério da Saúde; 2019. In addition, that study assessed the relation to level of education and found that, in individuals with up to 8 years of schooling, hypertension prevalence was approximately three times higher than that of individuals with at least 12 years of schooling, for both sexes. 276276. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2019: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília: Ministério da Saúde; 2019.
• Using estimates from the GBD Study 2017, Nascimento et al . reported an increased prevalence in age-standardized high SBP from 16.9% (95% UI, 16.5 - 17.3%) in 1990 to 18.9% (95% UI, 18.5 - 19.3%) in 2017, which was higher among men throughout the study period. Furthermore, the growth rate in the country was +0.4% per year among adults older than 25 years. 1111. Jorge MH, Laurenti R, Gotlieb SL. Análise da Qualidade das Estatísticas Vitais Brasileiras: A Experiência de Implantação do SIM e do SINASC. Cien Saude Colet. 2007;12(3):643-54. doi: 10.1590/s1413-81232007000300014. When analyzed by sex, the highest prevalence in 2017 was observed in the state of Santa Catarina (28.8%, 95% UI, 26.6-31%) in the male sex and in the state of Sergipe (19.8%, 95% UI, 17.7-21.9%) in the female sex. 277277. Nascimento BR, Brant LCC, Yadgir S, Oliveira GMM, Roth G, Glenn SD, Mooney M, Naghavi M, Passos VMA, Duncan BB, Silva DAS, Malta DC, Ribeiro ALP. Trends in Prevalence, Mortality, and Morbidity Associated With High Systolic Blood Pressure in Brazil From 1990 to 2017: Estimates From the “Global Burden of Disease 2017” (GBD 2017) study. Popul Health Metr. 2020;18(Suppl 1):17. doi: 10.1186/s12963-020-00218-z.
• Table 7-1 shows the prevalence of self-reported hypertension in Brazil according to sex in adults aged 18 years or more in 2019, as reported by the IBGE. The prevalence of hypertension was 23.9% in the country and higher in the female as compared to the male sex (26.4% versus 21.1%, respectively). There was a higher prevalence in urban areas as compared to rural ones (24.0% versus 23.2%, respectively), and in the Southeastern region for both sexes (23.1% for men and 28.3% for women).
• Table 7-2 shows the prevalence of self-reported hypertension according to sociodemographic variables, as reported by the IBGE. Of note, the highest prevalence rates were observed in individuals older than 75 years (62.1%), in those who had no education or few schooling years (36.6%), and in black (25.8%) and unemployed (38.7%) individuals. In contrast, when the income criterion was used, those with lower income had a lower prevalence of hypertension (18.7%), probably reflecting the lack of access to the health care system.
Mortality
Total Mortality Attributable to Hypertension
• Oliveira et al . compared the all-cause mortality attributable to hypertension in two population groups, a Brazilian and an English. The data used were obtained from the ELSA cohort, with 3205 individuals, and from the Bambuí cohort, with 1382 participants, all of them older than 60 years. Of note, the sociodemographic characteristics were different between the two cohorts, and the levels of education and family income were higher in the English cohort, while the rates of smoking and diabetes were higher in the Brazilian cohort. Regarding relative risks, in the English cohort, there was no difference when hypertension was assessed alone, while in the Brazilian cohort, hypertension conferred a relative risk of 1.43 (95% CI, 1.06 - 1.94, p=0.028) for mortality in 6 years. Furthermore, deaths attributable to hypertension in the Brazilian cohort were 25.3% (95% CI, 8.2 - 39.3%), far surpassing the English cohort, in which the result was borderline and without adequate statistical precision. 278278. Oliveira C, Marmot MG, Demakakos P, Mambrini JVM, Peixoto SV, Lima-Costa MF. Mortality Risk Attributable to Smoking, Hypertension and Diabetes Among English and Brazilian Older Adults (The ELSA and Bambui Cohort Ageing Studies). Eur J Public Health. 2016;26(5):831-5. doi: 10.1093/eurpub/ckv225.
• Table 7-3 shows the number of deaths and the age-standardized mortality rates attributable to high SBP from all causes according to the GBD Study 2019 data. Note that in older age groups, the number of deaths and the mortality rate are higher, as expected for this disease. However, the mortality rate attributable to high SBP in 2019 was 104.8 per 100 000 inhabitants; there was a 46.9% reduction over the study period, which may represent a lower incidence and greater therapeutic control of hypertension, as well as an improvement in the socioeconomic conditions observed in the period. 3737. Villela PB, Klein CH, de Oliveira GMM. Socioeconomic factors and mortality due to cerebrovascular and hypertensive disease in Brazil. Rev Port Cardiol. 2019;38(3):205-12. doi: 10.1016/j.repc.2018.07.007. , 279279. Villela PB, Klein CH, Oliveira GM. Trends in Mortality From Cerebrovascular and Hypertensive Diseases in Brazil Between 1980 and 2012. Arq Bras Cardiol. 2016;107(1):26-32. doi: 10.5935/abc.20160092.
• Table 7-4, depicting the age-standardized mortality rates attributable to high SBP from all causes according to sex and Brazilian FUs, shows an almost 50% decrease in mortality rates between 1990 and 2019 for both sexes, and the reduction was higher in women as compared to men (49.6% versus 43.8%, respectively). However, for women, except for the state of Rondônia — which had the greatest percentage reduction in mortality rate attributed to high SBP — the greatest reductions were found in the FUs of the Southeastern and Southern regions, and in the Distrito Federal. The state of Maranhão was the only FU that showed an increase in the rates during the study period. Among men, all FUs showed a reduction in mortality attributed to high SBP, with the largest percentage decreases recorded in the FUs of the Southern and Southeastern regions, as observed for women (Table 7-4) .
• Chart 7-1 shows the number of deaths (A) and mortality rates (B) attributable to high SBP between 1990 and 2019. With increasing life expectancy, the consequent aging of the population, and the data observed in the previous tables, the number of deaths related to high SBP was also expected to increase, as shown in Chart 7-1A. However, when the effect of age was mitigated by age-standardization of the rates, a decrease in mortality rate was observed over time (1B).
• The proportional mortality by age groups in 2019 is shown in Chart 7-2. Of note, there is a greater proportion of deaths in the groups between 55 years and 74 years for women; however, for men, the greatest proportion is observed in the age groups 10 years younger (45 years to 64 years). Importantly, the age groups ‘above 75 years’ for women and ‘above 65 years’ for men may have other concurrent diseases; therefore, the proportion of deaths from high SBP tends to decrease due to competitive causes, which may, at least in part, explain the data described above.
• Chart 7-3 presents the age-standardized mortality rates of diseases attributable to high SBP, stratified for all causes, between 1990 and 2019. As shown, most deaths are related to major CVDs, i.e., ischemic heart disease, cerebrovascular disease, and hypertensive diseases, all three of which decreased between 1990 and 2019. Notably, hypertensive diseases showed the smallest reduction when compared with the other two diseases. This may be related to the rules for the selection of the underlying cause of death in death certificates, in which, because of the use of specific algorithms, hypertensive disease is rarely selected as the underlying cause of death. 280280. Villela PB, Klein CH, Oliveira GMM. Cerebrovascular and Hypertensive Diseases as Multiple Causes of Death in Brazil From 2004 to 2013. Public Health. 2018;161:36-42. doi: 10.1016/j.puhe.2018.04.006.
Cardiovascular Mortality Attributable to Hypertension
• Regarding cardiovascular mortality attributable to high SBP, Table 7-5 shows the number of deaths, mortality rates, and the percent change of rates between 1990 and 2019 according to GBD estimates. There was a decrease by almost 50% in the period, from 186.1 per 100 000 inhabitants in 1990 to 93.4 per 100 000 inhabitants in 2019 (Table 7-5), and, similarly to all-cause mortality, the highest rates were observed in the older age groups.
• Table 7-6 presents the mortality from CVDs attributed to high SBP by FU and sex, indicating a trend similar to that shown in Tables 7-3 and 7-4, both of which show mortality from all causes and include evaluation by age group and FU. Thus, there was a reduction in the cardiovascular mortality attributable to hypertension by 52.5% among women and by 46.8% among men between 1990 and 2019 in Brazil. For females, the FUs with the greatest reductions were the states of Rondônia, Minas Gerais, Paraná, and Rio de Janeiro, and the Distrito Federal, with 62.9%, 60.4%, 59.3%, 59.1%, and 58%, respectively (Table 7-6), while, for males, the greatest reductions were observed in the Distrito Federal, and the states of Minas Gerais, São Paulo, Santa Catarina, and Rio de Janeiro, with 61.3%, 58%, 56.1%, 55.1%, and 54.2%, respectively.
• Chart 7-4 shows the age-standardized mortality rates of diseases attributable to elevated SBP, stratified by CVDs, between 1990 and 2019. The mortality rates from chronic kidney disease remained stable, while those from ischemic heart diseases, stroke, hypertensive diseases, and cardiomyopathies and myocarditis decreased over that period.
• Finally, Chart 7-5 shows the relationship between the 2019 SDI and the percent change in deaths from CVD attributable to high SBP from 1990 to 2019, in Brazil, by FU. Chart 7-5 shows that the greatest reductions in age-standardized mortality rate occurred in those FUs with the highest SDI values in an almost linear relationship, with a correlation coefficient of 0.78 and p-value=0.
Burden of Disease
• Chart 7-6 shows the absolute number of YLLs (A), YLDs (B), and DALYs (C) related to hypertension between 1990 and 2020. It is worth noting the trend towards an increase in YLLs (A) and mainly in YLDs (B), with a consequent impact on the DALYs curve (A). These observations can be justified, at least partially, by population growth and aging.
• In contrast, the age-standardized rates in Chart 7-7 show a reduction in YLLs (A) and in YLDs (B) with a consequent impact on DALYs (C). These curves reflect the attenuation of the population aging effect on the disease burden, with a smaller influence on YLDs, which may be partially explained by the inequality of access to the healthcare system, hindering the treatment of more severe diseases, with a consequent impact on YLDs.
Impact on Cardiovascular Health
•Fuchs et al. investigated the association between clustering of risk factors and self-reported CVD among 1007 women living in the city of Porto Alegre, Southern Brazil. 281281. Fuchs SC, Moreira LB, Camey SA, Moreira MB, Fuchs FD. Clustering of Risk Factors for Cardiovascular Disease Among Women in Southern Brazil: A Population-Based Study. Cad Saude Publica. 2008;24(Suppl 2):S285-93. doi: 10.1590/s0102-311x2008001400013. The prevalence of hypertension, diabetes, physical activity, and the diet pattern were evaluated regarding their association, in a clustered fashion, with CVD, which was defined as the self-report of history of myocardial infarction, heart failure, stroke or coronary artery bypass surgery. The investigators found hypertension and diabetes as the main cluster associated with CVD, accounting for an independent risk ratio of 8.5 (95% CI, 3.0 - 24.5).
• Carvalho et al. , evaluating, in a sample of 333 individuals with treated hypertension or without hypertension, the association between hypertension and quality of life measured by the SF-36, showed that hypertensive patients had lower quality of life than their normotensive counterparts. 282282. Carvalho MV, Siqueira LB, Sousa AL, Jardim PC. The Influence of Hypertension on Quality of life. Arq Bras Cardiol. 2013;100(2):164-74. doi: 10.5935/abc.20130030. They found that normotensive individuals have higher HRQOL questionnaire scores as compared to hypertensive patients in all domains except for the ‘Emotional Aspect’. With respect to ‘Grouped Physical Component’, male hypertensive patients scored 298.4±72.6 as compared to 333.1±52.1 of normotensive males (P<0.01), and female hypertensive patients scored 243.8±84.0 as compared to 318.7±58.5 of normotensive females (P<0.01). Among males, the difference was significant for the ‘Functional Capacity’, ‘Social Aspect’, and ‘Mental Health’ domains of the SF-36, and, among females, the difference was observed for the ‘Emotional Aspect’ domain.
• To investigate the association of hypertension, prehypertension, age, duration of diagnosis, and blood pressure, Menezes et al . used the ELSA-Brasil data, which included 7063 patients, with a mean age of 58.9 years at baseline (2008-2010). The authors verified that hypertension was associated with the greatest decline in memory, fluency, and global cognitive score. Prehypertension was also an independent predictor of greater decline in the verbal fluency test and global cognitive score. Moreover, among treated individuals, blood pressure control at baseline was inversely associated with the decline in both global cognitive and memory test scores. 283283. Menezes ST, Giatti L, Brant LCC, Griep RH, Schmidt MI, Duncan BB, Suemoto CK, Ribeiro ALP, Barreto SM. Hypertension, Prehypertension, and Hypertension Control: Association With Decline in Cognitive Performance in the ELSA-Brasil Cohort. Hypertension. 2021;77(2):672-81. doi: 10.1161/HYPERTENSIONAHA.120.16080.
The association of CVD (coronary artery disease, myocardial infarction, and stroke) with diabetes, hypertension, and diabetes plus hypertension was investigated by Santos et al. in 2691 patients enrolled in the HIPERDIA program in the city of Fortaleza. 284284. Santos JC, Moreira TM. Risk Factors and Complications in Patients With Hypertension/Diabetes in a Regional Health District of Northeast Brazil. Rev Esc Enferm USP. 2012;46(5):1125-32. doi: 10.1590/s0080-62342012000500013. The authors confirmed a significant association of hypertension with stroke, coronary artery disease, and myocardial infarction (P<0.001).
Costs and Healthcare Utilization
• Estimating the costs of hypertension, diabetes, and obesity in SUS patients in 2018, Nilson et al. noticed that the total cost of hypertension, diabetes, and obesity paid by the SUS reached R$ 3.45 billion (95% CI, 3.15 - 3.75), more than US$890 million. Of that total amount, 59% was spent with hypertension, 30% with diabetes, and 11% with obesity. When obesity was considered separately a risk factor for hypertension and diabetes, the cost attributable to this disease reached R$ 1.42 billion (95% CI, 0.98 - 1.87), corresponding to 41% of the total cost. 285285. Nilson EAF, Andrade RDCS, Brito DA, Oliveira ML. Costs attributable to obesity, hypertension, and diabetes in the Unified Health System, Brazil, 2018. Rev Panam Salud Publica. 2020;44:e32. doi: 10.26633/RPSP.2020.32.
https://doi.org/10.26633/RPSP.2020.32...
• Marinho et al. , investigating healthcare costs of patients with diabetes and hypertension, compared the direct costs of outpatient procedures with the amount reimbursed by the SUS. Their study’s main conclusion was that direct costs of the operation was higher than what SUS had been reimbursing, characterizing a public healthcare underfunding in real life that may compromise the quality of the control of cardiovascular risk factors. Of the costs, that with medications was the highest, followed by outsourced services and human resources. 286286. Marinho MG, Cesse EÂ, Bezerra AF, Sousa IM, Fontbonne A, Carvalho EF. Analysis of Health Care Costs of Patients With Diabetes Mellitus and Hypertension in a Public Health Reference Unit in Recife--Brazil. Arq Bras Endocrinol Metabol. 2011;55(6):406-11. doi: 10.1590/s0004-27302011000600007.
• Queiroz et al . investigated the association between the number of cardiovascular risk factors or CVD and hospitalizations among 514 users of the SUS in the city of Presidente Prudente, São Paulo state. They concluded that hypertension, arrythmias, lower levels of physical activity, and myocardial infarction were associated with the number of days of hospitalization. In addition, they reported that the number of cardiovascular risk factors or CVD per patient was associated with the number of days of hospitalization. Nevertheless, rates of hospitalization in the last 12 months were independently higher only for those with arrythmias (OR 3.04, 95% CI, 1.74 - 5.31) and history of myocardial infarction (OR 3.07, 95% CI, 1.34 - 7.01). 287287. Queiroz DC, Cantarutti DC, Turi BC, Fernandes RA, Codogno J. Association between Cardiovascular Diseases and Hospitalization Among Patients Users of the Brazilian National Health System. Medicina. 2016;49(1):52-9. doi: 10.11606/issn.2176-7262.v49i1p52-59.
Hypertension Awareness, Treatment, and Control
• Using data from the 2013 National Health Survey, Macinko et al . estimated that about 36% of the Brazilian population (51.4 million) had a previous diagnosis and/or measured blood pressure of 140/90 mm Hg or more. Of these, 89% had contacted the health system in the previous 2 years, but only 65% were aware of their condition. From those aware of their hypertensive condition, 62% regularly sought care, 92% of whom had been prescribed medications. Of those who reported receiving medications, only 56% reported that ongoing care for their condition was free of barriers and included advice about managing important risk factors and behavior. Of the entire hypertensive population, about 33% had their blood pressure under control. 288288. Macinko J, Leventhal DGP, Lima-Costa MF. Primary Care and the Hypertension Care Continuum in Brazil. J Ambul Care Manage. 2018;41(1):34-46. doi: 10.1097/JAC.0000000000000222.
• To estimate prevalence, awareness, types of anti-hypertensive treatment, and the association of hypertension control with social status, data from the ELSA-Brasil baseline (2008-2010) were collected in 15 103 individuals. 273273. Santiago ERC, Diniz ADS, Oliveira JS, Leal VS, Andrade MIS, Lira PIC. Prevalence of Systemic Arterial Hypertension and Associated Factors Among Adults From the Semi-Arid Region of Pernambuco, Brazil. Arq Bras Cardiol. 2019;113(4):687-695. doi: 10.5935/abc.20190145. Blood pressure was measured by the oscillometric method, and 35.8% of those individuals were classified as hypertensive, and 76.8% of them were on anti-hypertensive medication. Women were more aware than men (84.8% versus 75.8%) and more often on medication (83.1% versus 70.7%). Use of at least one anti-hypertensive drug was reported by 76.8% (n = 4147) of the participants classified as having hypertension and was also more frequent among women in all age groups. Of the users of anti-hypertensives, 69.4% showed controlled blood pressure levels (65.5% of the men and 72.9% of the women). Considering all the hypertensive individuals, about 53% showed appropriate blood pressure levels. Among those on drug treatment, controlled blood pressure was more likely in the higher educated group than among participants with less than secondary school education (PR 1.21; 95% CI, 1.14 - 1.28), and among Asian (PR 1.21; 95% CI, 1.12 - 1.32) and Whites (PR 1.19; 95% CI, 1.12 -1.26) as compared to Blacks.
• In a cross-sectional population-based study, carried out through a household survey and randomized cluster sampling, from the Health Status of the Elderly Population of the Municipality of Goiânia, state of Goiás, investigating 912 non-institutionalized elderly (≥ 60 years) living in urban areas, Sousa et al . reported a 74.9% prevalence of hypertension, higher (78.6%) among men (OR 1.4, 95% CI, 1.04 - 1.92). The treatment rate was 72.6%, with higher rates observed among smokers (OR 2.06, 95% CI, 1.28 - 3.33). The rate of hypertension control was 50.8%, higher among women (OR 1.57, 95% CI, 1.19 - 2.08). 289289. Sousa ALL, Batista SR, Sousa AC, Pacheco JAS, Vitorino PVO, Pagotto V. Hypertension Prevalence, Treatment and Control in Older Adults in a Brazilian Capital City. Arq Bras Cardiol. 2019;112(3):271-8. doi: 10.5935/abc.20180274.
• In a cross-sectional study investigating 502 users of the Family Health Strategy to control hypertension, Rocha et al . compared three different instruments to measure patient’s adherence to hypertension treatment (the Morisky and Green test, the Qualiaids team’s Medication Adherence Questionnaire, and the Haynes’ Questionnaire). The authors reported the following non-adherence prevalence rates: 29.28%, measured by the Morisky and Green test; 60.16%, by the Qualiaids Questionnaire; and 13.15%, by the Haynes questionnaire. This indicates room for improvement even in a structured program such as the Family Health Strategy. Despite the great variability in the adherence rates depending on the instrument used to measure it, the authors noticed a significant association of adherence to treatment and blood pressure control. 290290. Rocha TPO, Figueredo-Neto JA, Fernandes DR, Santana EEC, Abreu JER, Cardoso RLS, Melo JB. A Comparative Study among Different Treatment Adherence Methods in Hypertensive Patients. Int J Cardiovasc Sci. 2015;28(2):122-129. doi: 10.5935/2359-4802.20150015.
• To assess the evolution of hypertension prevalence, awareness, and control for over 10 years in the state of Pernambuco, two cross-sectional studies were conducted based on random samples of urban and rural households in 2006 and 2015/2016, involving adults aged 20 years or older. Approximately one third of the adult population of Pernambuco had hypertension in 2006 and this prevalence was maintained in 2015/2016. In rural areas, awareness concerning hypertension rose from 44.8% in 2006 to 67.3% in 2015/2016, and control, from 5.3% to 27.1%, so that awareness and control were similar in urban and rural areas in 2015/2016. A logistic regression analysis was conducted to estimate the influence of the social, behavioral, and anthropometric determinants on hypertension. Although social and behavioral factors improved in the 10-year period, overweight and abdominal obesity increased. After an adjustment for potential confounding factors, the likelihood of having hypertension more than doubled among men (OR 2.03; p < 0.001), young adults (OR 4.41; p < 0.001), the elderly (OR 14.44; p < 0.001), and those with abdominal obesity (OR 2.04; p < 0.001) in urban areas, as well as among young adults (OR 2.56; p < 0.001), and less educated (OR 2.21; p = 0.006) and overweight individuals (OR 2.23; p < 0.001) in rural areas. 291291. Souza NP, Cesse EÂP, Souza WV, Fontbonne A, Barreto MNSC, Goff ML, Batista Filho M, Féart C, Lira PIC. Temporal Variation in Prevalence, Awareness and Control of Hypertension in Urban and Rural Areas in Northeast Brazil between 2006 and 2016. Cad Saude Publica. 2020;36(4):e00027819. doi: 10.1590/0102-311X00027819.
• In a prospective study, Krieger et al . investigated the prevalence of resistant hypertension in a cohort of 1597 patients with stage 2 hypertension submitted to a step drug protocol. From 1597 patients recruited, 187 (11.7%) fulfilled the resistant hypertension criteria, defined as the lack of hypertension control evaluated by office blood pressure ≥140/90 mm Hg and mean 24-hour ambulatory blood pressure monitoring ≥ 130/80 mm Hg despite treatment with three drugs (enalapril or losartan, amlodipine and chlorthalidone) for 12 weeks. In addition, investigating the clinical predictors of hypertension, they noticed that history of stroke, diabetes mellitus, and office blood pressure ≥ 180/110 mm Hg at study entry were independently associated with resistant hypertension. 292292. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, Mill JG, Lotufo PA, Amodeo C, Batista MC, Bodanese LC, Carvalho ACC, Castro I, Chaves H, Costa EAS, Feitosa GS, Franco RJS, Fuchs FD, Guimarães AC, Jardim PC, Machado CA, Magalhães ME, Mion D Jr, Nascimento RM, Nobre F, Nóbrega AC, Ribeiro ALP, Rodrigues-Sobrinho CR, Sanjuliani AF, Teixeira MDCB, Krieger JE; ReHOT Investigators. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90. doi: 10.1161/HYPERTENSIONAHA.117.10662.
• In the HealthRise, a program of community-based interventions for the detection and management of hypertension and diabetes in underserved communities implemented in 2017-2018, more patients met treatment targets for hypertension [45.9% (43.0%–48.9%)] at endline than at baseline [35.4% (32.6%–38.6%), p<0.001], in the city of Vitória da Conquista, Bahia state. In the other city included in the project, Teófilo Otoni, Minas Gerais state, more patients met hypertension treatment targets at endline [52.2% (49.3–55%)] as compared to baseline [48.3% (45.5–51.2%); p<0.05], suggesting that these community-based interventions have the potential to improve hypertension control. 293293. Flor LS, Wilson S, Bhatt P, Bryant M, Burnett A, Camarda JN, Chakravarthy V, Chandrashekhar C, Chaudhury N, Cimini C, Colombara DV, Narayanan HC, Cortes ML, Cowling K, Daly J, Duber H, Kavinkare VE, Endlich P, Fullman N, Gabert R, Glucksman T, Harris KP, Bouskela MAL, Maia J, Mandile C, Marcolino MS, Marshall S, McNellan CR, Medeiros DS, Mistro S, Mulakaluri V, Murphree J, Ng M, Oliveira JAQ, Oliveira MG, Phillips B, Pinto V, Ngwato TP, Radant T, Reitsma MB, Ribeiro ALP, Roth G, Rumel D, Sethi G, Soares DA, Tamene T, Thomson B, Tomar H, Ugliara Barone MT, Valsangkar S, Wollum A, Gakidou E. Community-Based Interventions for Detection and Management of Diabetes and Hypertension in Underserved Communities: A Mixed-Methods Evaluation in Brazil, India, South Africa and the USA. BMJ Glob Health. 2020;5(6):e001959. doi: 10.1136/bmjgh-2019-001959.
Risk Factors and Prevention
• Treff CA Jr, in his dissertation, investigated the relationship between hypertension and physical activity levels according to the ‘leisure’ and ‘transportation’ domains of the IPAQ questionnaire. By using the databank of the ELSA-Brasil study, that author observed that leisure-time physically active individuals had lower SBP (p=0.007) and DBP (p=0.001) levels. On the other hand, no relationship was identified between hypertension and the levels of physical activity performed as a form of transportation. 294294. Treff CA Jr. Physical Activity in Leisure and in Transportation Associated With Hypertension in the Longitudinal Study of Adult Health (ELSA-Brazil) [dissertation]. São Paulo: Faculdade de Medicina, Universidade de São Paulo; 2015.
• Investigating the potential role of diet leading to blood pressure elevation and expression of other cardiovascular risk factors, Pavan et al . studied 1110 subjects aged 22–89 years divided into three matched groups by sex and age (370 from Tanzania and Uganda, 370 from the Amazonian region of Brazil, and 370 from northern Italy; 111 men and 259 women in each group). The SBP of Africans eating a low-salt ‘fish and vegetable’ diet was lower than that of Brazilians, whose diet was based on cereals and meat, and that of highly urbanized Italians (144.1±21.9, 155.4±26.8, and 159.7±22.9 mm Hg, respectively, < 0.0001). The same occurred for DBP (83.2±11.8, 94.5±15.5, 94.7±11.6 mm Hg, respectively, < 0.0001). The SBP was correlated to the body mass index of all three populations, but with age only for the Brazilians and Italians. Total cholesterol level and body mass index, both of which are low among Africans, increased progressively with increasing economic level. Transition from a rural to an urbanized lifestyle seems to be accompanied by a rise in rates of cardiovascular risk factors; in addition, environmental, rather than racial factors, have a crucial impact on the risk pattern of populations. 295295. Pavan L, Casiglia E, Pauletto P, Batista SL, Ginocchio G, Kwankam MM, Biasin R, Mazza A, Puato M, Russo E, Pessina AC. Blood Pressure, Serum Cholesterol and Nutritional State in Tanzania and in the Amazon: Comparison With an Italian Population. J Hypertens. 1997;15(10):1083-90. doi: 10.1097/00004872-199715100-00006.
• In a descriptive, observational, cross-sectional population-based study, Jardim et al . evaluated 1739 individuals and observed that hypertension was prevalent in 36.4% of the total population, and higher among males (41.8%) than females (31.8%). Hypertension was positively correlated to age ≥60 years versus age of 18-29 years (OR 8.92, 5.94 – 14.11; P<0.000), male gender (OR 1.86, 1.47–2.35; P<0.000), and body mass index (OR 1.44, 1.13 – 1.83; P=0.004). Prevalences of overweight and obesity were 30.0% and 13.6%, respectively. Overweight was higher among females and obesity among males. The prevalence of smoking was 20.1%, higher among males (27.1%) as compared to females (16.4%). A sedentary lifestyle was observed in 62.3% of the population, with no difference between genders. Regular alcohol consumption was reported by 44.4% of the individuals, being more frequent among males. 296296. Jardim PC, Gondim MR, Monego ET, Moreira HG, Vitorino PV, Souza WK, Scala LC. High Blood Pressure and Some Risk Factors in a Brazilian capital. Arq Bras Cardiol. 2007;88(4):452-7. doi: 10.1590/s0066-782x2007000400015.
• Using data from the VIGITEL survey, Moreira et al . tried to identify and measure the relationships of sociodemographic and behavioral characteristics, food consumption characteristics, and health indicators related to hypertension and diabetes. The independent variables analysed in the study were selected based on their importance for determining the total burden of disease, as estimated by the World Health Organization for the Americas region. 297297. Moreira APL, Malta DC, Vianna RP de T, Moreira PVL, Carvalho AT de. Risk and protection factors for self-reported hypertension and diabetes in João Pessoa, Brazil. The VIGITEL survey, 2014. A cross-sectional study. Sao Paulo Med J. 2017;135(5):450-461. doi:10.1590/1516-3180.2017.0044250517. The adjusted analysis relating to the women’s data showed that age ≥ 65 years (PR 1.3; 1.0-1.7), excessive body weight (PR 1.7; 1.3-2.2), self-rated poor health (PR 1.3; 1.0-1.8), and a previous medical diagnosis of dyslipidemia (PR 1.5; 1.2-1.8) remained independently associated with higher prevalence of hypertension. Consuming whole-fat milk remained associated with lower prevalence of hypertension in women (PR 0.7; 0.6-0.9). In the adjusted analysis for men, overweight (PR 1.7; 1.1-2.5) and self-rated poor health were independently associated with hypertension (PR 1.9; 1.4-2.5).
• Investigating whether blood pressure response to salt intake would be sex-specific, Mill et al . studied the changes in blood pressure according to different salt intake by men and women in 12 813 individuals with a validated 12-hour overnight urine collection in which salt intake was estimated. A set of questionnaires, clinical examination, and laboratory tests were carried out during a single visit. Salt intake was 12.9 ± 5.9 g/d among men and 9.3 ± 4.3 g/d among women. As expected, the authors concluded that blood pressure increased as salt intake increased, regardless of using blood pressure-lowering medication. Nevertheless, the slope of increase in blood pressure elicited by salt intake was significantly higher in women than in men. They concluded that salt intake was elevated in this large sample of Brazilian adults and only a few participants were compliant with the guidelines’ recommendations. Moreover, the higher responsiveness to salt intake observed in women as compared to men, even after controlling for confounders, indicates higher salt sensitivity and may have pathophysiological implications. 298298. Mill JG, Baldo MP, Molina MDCB, Schmidt MI, Barreto SM, Chor D, Griep RH, Matos SM, Ribeiro ALP, Duncan BB, Aquino EM, Lotufo PA, Bensenor I. Sex-Specific Patterns in the Association Between Salt Intake and Blood Pressure: The ELSA-Brasil study. J Clin Hypertens. 2019;21(4):502-509. doi: 10.1111/jch.13509.
Children and Adolescents
• Hypertension, obesity, poor diet, and physical inactivity in childhood and adolescence are an emerging epidemiological concern. Moreover, early identification and intervention may prevent premature CVD in adult life.
• To estimate the prevalence of hypertension and obesity and the role of obesity in hypertension in Brazilian adolescents, data from participants in the ERICA Study were evaluated by Bloch et al . Prevalence and 95% CI of arterial hypertension and obesity, both on a national basis and in the Brazilian regions, were estimated by sex and age groups, as was the proportion of hypertension due to obesity in the population. The study assessed 73 399 students, 55.4% female, mean age of 14.7 ± 1.6 years. The prevalence of hypertension was 9.6% (95% CI, 9.0 - 10.3), the lowest being in the Northern (8.4%; 95% CI, 7.7 - 9.2) and Northeastern (8.4%; 95% CI, 7.6 - 9.2) regions, and the highest in the Southern region (12.5%; 95% CI, 11.0 - 14.2). The mean prevalence of obesity was 8.4% (95% CI, 7.9 - 8.9), which was lower in the Northern region and higher in the Southern region. The prevalences of hypertension and obesity were higher among males. Obese adolescents presented a higher prevalence of hypertension, 28.4% (95% CI, 25.5 - 31.2), than overweight adolescents, 15.4% (95% CI, 17.0 - 13.8), or eutrophic adolescents, 6.3% (95% CI, 5.6 - 7.0), as commonly noticed. The proportion of hypertension due to obesity was estimated at 17.8%. The authors concluded that the control of obesity could lower the prevalence of hypertension among Brazilian adolescents by approximately 20%. 299299. Bloch KV, Klein CH, Szklo M, Kuschnir MC, Abreu Gde A, Barufaldi LA, da Veiga GV, Schaan B, da Silva TL, de Vasconcellos MT, Moraes AJ, Borges AL, de Oliveira AM, Tavares BM, de Oliveira CL, Cunha Cde F, Giannini DT, Belfort DR, Santos EL, de Leon EB, Fujimori E, Oliveira ER, Magliano Eda S, Vasconcelos Fde A, Azevedo GD, Brunken GS, Guimarães IC, Faria Neto JR, Oliveira JS, de Carvalho KM, Gonçalves LG, Monteiro MI, Santos MM, Jardim PC, Ferreira PA, Montenegro RM Jr, Gurgel RQ, Vianna RP, Vasconcelos SM, Goldberg TB. ERICA: Prevalences of Hypertension and Obesity in Brazilian Adolescents. Rev Saude Publica. 2016;50(Suppl 1):9s. doi: 10.1590/S01518-8787.2016050006685.
• Christofaro et al . analysed the relationship between hypertension of adolescents and their parents’ sociodemographic characteristics and lifestyle. For this task, 1231 adolescents, 1202 mothers, and 871 fathers were investigated. The prevalence of hypertension was higher among adolescents with older parents, with both parents reporting hypertension, and with overweight mothers. In multivariate analysis, adolescents with older mothers (OR 2.36; 95% CI, 1.12 - 4.98), hypertensive mothers (OR 2.22; 95% CI, 1.26 - 3.89), and hypertensive fathers (OR 1.70; 95% CI, 1.03 - 2.81) were more likely to have hypertension. In the analysis that considered clusters of health risk factors, higher risks of hypertension were observed in adolescents whose mothers had four or more aggregated risk factors (OR 2.53; 95% CI, 1.11 - 5.74). 300300. Christofaro DGD, Mesas AE, Ritti Dias RM, Fernandes RA, Saraiva BTC, Palma MR, Silva DAS, Andrade SM. Association Between Hypertension in Adolescents and the Health Risk Factors of Their Parents: An Epidemiological Family Study. J Am Soc Hypertens. 2018;12(3):182-9. doi: 10.1016/j.jash.2017.12.011.
• To estimate the presence of cardiovascular risk (obesity and hypertension) in schoolchildren and its potential interactions with cardiorespiratory fitness, Burgos et al . performed a cross-sectional study conducted in 1666 schoolchildren, aged 7-17 years, 873 (52.4%) of them males. The following variables were evaluated: SBP, DBP, body mass index, body fat percentage, and cardiorespiratory fitness. Systolic blood pressure and DBP were correlated with waist circumference, waist-hip ratio, sum of skin folds, and cardiorespiratory fitness. The authors reported that 26.7% of them were overweight or obese, and 35.9% had body fat percentage over moderately high. They also found that 13.9% and 12.1% of the students were borderline or hypertensive, for SBP and DBP, respectively. There was a significant correlation of SBP and DBP with all variables, and a weak to moderate correlation with age, weight, height, body mass index, and waist circumference. These data indicate a cluster of hypertension, obesity, and lack of cardiorespiratory fitness in early life and must elicit the development of effective prevention programs to reduce CVD in adulthood. 301301. Burgos MS, Reuter CP, Burgos LT, Pohl HH, Pauli LT, Horta JA, Reckziegel MB, Franke SI, Prá D, Camargo M. Comparison Analysis of Blood Pressure, Obesity, and Cardio-Respiratory Fitness in Schoolchildren. Arq Bras Cardiol. 2010;94(6):788-93. doi: 10.1590/s0066-782x2010005000046.
• Schommer et al . investigated the association between anthropometric variables and blood pressure levels in schoolchildren from 5th to 8th grade to identify which parameter more strongly correlated with blood pressure levels. Using a cross-sectional study with probabilistic population-based cluster sampling of schoolchildren, they enrolled schoolchildren from 5th to 8th grade in public elementary schools of the city of Porto Alegre. The participants’ mean age was 12.6 ± 1.6 years, and 55.2% of them were females. Abnormal blood pressure levels were found in 11.3% of the sample and borderline values, in 16.2%. Of the anthropometric variables analyzed, hip circumference showed the strongest correlation with increased blood pressure (r = 0.462, p < 0.001), followed by waist circumference (r = 0.404, p < 0.001) and abdominal skinfold (r = 0.291, p < 0.001). 302302. Schommer VA, Barbiero SM, Cesa CC, Oliveira R, Silva AD, Pellanda LC. Excess Weight, Anthropometric Variables and Blood Pressure in Schoolchildren Aged 10 to 18 Years. Arq Bras Cardiol. 2014;102(4):312-8. doi: 10.5935/abc.20140038.
Future Research
• Because of its prevalence and impact, hypertension is the leading cardiovascular risk factor for disability and death around the globe and in Brazil. Despite this current knowledge, more representative and comprehensive data is lacking to better quantify the current incidence, the trends of hypertension, the life course trajectories and their determinants, and the morbidity and mortality related to hypertension, stratified by regions, sex, age, and socioeconomic status in Brazil.
• Planning to decrease cardiovascular burden in Brazil, there is a huge gap regarding a deeper and more integrated knowledge about how to improve hypertension prevention, awareness, treatment, and control, as well as its relationship with other cardiovascular unfavorable behaviors and risk factors, such as proposed by the American Heart Association with the seven metrics to measure cardiovascular health at the population level. 303303. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD; American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction: The American Heart Association’s Strategic Impact Goal Through 2020 and Beyond. Circulation. 2010;121(4):586-613. doi: 10.1161/CIRCULATIONAHA.109.192703. The current understanding points out to the global cardiovascular risk, at the population level, as the main determinant of cardiovascular morbidity and mortality nationwide. Therefore, better data on outcomes and health service research to measure population end-results and healthcare system performance, and on implementation science investigating strategies of how to improve these outcomes are urgently needed in Brazil. 304304. Oliveira JC, Barreto-Filho JA. Public health policy based on “made-in-Brazil” Science: a challenge for the Arquivos Brasileiros de Cardiologia. Arq Bras Cardiol. 2015;105(3):211-213. doi:10.5935/abc.20150120.
• Moreover, we must move on from only generating evidence to a model of continuously translating the evidence into good health care policies. 305305. Krumholz HM. Outcomes research: generating evidence for best practice and policies. Circulation. 2008;118(3):309-318. doi:10.1161/CIRCULATIONAHA.107.690917. National population strategies with effective campaigns to promote healthy habits (i.e.: decrease salt in diet, taxation of unhealthy foods, increase in physical activity), allied to more effective identification and treatment of the individuals at greater cardiovascular risk, and objective surveillance of results must be more disseminated to all levels of our healthcare system.
• Another theme that deserves better research is related to disparities regarding access, timelines, and outcomes of hypertensive patients using the SUS as compared to patients using private healthcare services. 9696. Oliveira JC, Almeida-Santos MA, Cunha-Oliveira J, Oliveira LCS, Barreto IDC, Lima TCRM, Arcelino LAM, Prado LFA, Silveira FS, Nascimento TAS, Ferreira EJP, Barreto RV, Moraes EV, Mendonça JT, Sousa ACS, Barreto-Filho JA; VICTIM Register Investigators. Disparities in Access and Mortality of Patients With ST-Segment-Elevation Myocardial Infarction Using the Brazilian Public Healthcare System: VICTIM Register. J Am Heart Assoc. 2019;8(20):e013057. doi: 10.1161/JAHA.119.013057. Considering that more than three-quarters of Brazilians are SUS users, it is imperative to measure continuously the outcomes of hypertension programs implemented by the SUS, such as the Family Health Strategy, and to compare to those reached by the private healthcare system.
8. DIABETES MELLITUS
ICD-10 E10 to E14; ICD-10-CM E8 to E13
See Tables 8-1 to 8-5 and Charts 8-1 through 8-4
Abbreviations used in Chapter 8
| BMI | Body Mass Index |
| CI | Confidence Interval |
| CVD | Cardiovascular Diseases |
| DALYs | Disability-Adjusted Life Years |
| ELSA-Brazil | Longitudinal Study of Adult Health - Brazil |
| ERICA | Brazilian Study of Cardiovascular Risk in Adolescents (in Portuguese, Estudo dos Riscos Cardiovasculares em Adolescentes ) |
| FU | Federative Unit |
| GBD | Global Burden of Disease |
| HbA1c | Glycosylated Hemoglobin |
| HDL | High Density Lipoprotein |
| HR | Hazard Ratio |
| IBGE | Brazilian Institute of Geography and Statistics (in Portuguese, Instituto Brasileiro de Geografia e Estatística ) |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems, 10thRevision |
| IDF | International Diabetes Federation |
| LDL | Low Density Lipoprotein |
| MASS | The Medicine, Angioplasty or Surgery Registry (in Portuguese, Registro de Medicina, Angioplastia ou Cirurgia ) |
| OR | Odds Ratio |
| PNAUM | Survey on the Access, Utilization and Promotion of Rational Use of Medications in Brazil (in Portuguese, Pesquisa Nacional sobre o Acesso, Utilização e Promoção do Uso Racional de Medicamentos no Brasi l) |
| PNS | National Health Survey (in Portuguese, Pesquisa Nacional de Saúde ) |
| PR | Prevalence Ratio |
| REACT | Registry of Clinical Practice in Patients at High Cardiovascular Risk (in Portuguese, Registro do Paciente de Alto Risco Cardiovascular na Prática Clínica ) |
| SBC | Brazilian Society of Cardiology (in Portuguese, Sociedade Brasileira de Cardiologia ) |
| SDI | Sociodemographic Index |
| SF-36 | Short Form 36 quality of life questionnaire |
| SIM | Brazilian Mortality Information System (in Portuguese, Sistema de Informações sobre Mortalidade ) |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| UI | Uncertainty Interval |
| VIGITEL | Surveillance System of Risk and Protection Factors for Chronic Diseases by Telephone Survey (in Portuguese, Sistema de Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico ) |
| YLDs | Years Lived with Disability |
| YLLs | Years of Life Lost |
– Prevalence of diabetes mellitus (glycosylated hemoglobin ≥ 6.5% or use of antidiabetic drugs): total, according to sex and Brazilian regions.
– Prevalence of diabetes mellitus (glycosylated hemoglobin ≥ 6.5% or use of antidiabetic drugs) according to age range and sociodemographic characteristics.
– Number of deaths and age-standardized mortality rate (per 100 000) from cardiovascular disease attributable to diabetes for both sexes, in Brazil and its Federative Units, 1990 and 2019.
– Age-standardized mortality rate (per 100 000) from cardiovascular disease attributable to diabetes, for men and women, in Brazil and its Federative Units, 1990 and 2019.
– Number of DALYs and age-standardized DALY rates (per 100 000) from cardiovascular disease attributable to diabetes for both sexes, in Brazil and its Federative Units, 1990 and 2019.
– Total number of deaths due to diabetes (A). From cardiovascular disease attributable to diabetes: number of deaths (B), age-standardized mortality rate (per 100 000) (C), and DALY rate (D). Brazil, 2019.
– Proportional mortality from cardiovascular diseases attributable to diabetes according to sex and age group. Brazil, 2019
– Deaths attributable to diabetes stratified by all causes and by cardiovascular diseases. Brazil, 2019.
– Correlation between the sociodemographic index (SDI) of 2019 and the percent change in deaths from cardiovascular disease attributable to diabetes from 1990 to 2019, in Brazil and its Federative Units.
Introduction
• Diabetes mellitus is a chronic and progressive disease, characterized by metabolic changes due to persistent hyperglycemia resulting from defects in the secretion and/or action of the insulin produced by the pancreatic beta cells. In the long run, persistent hyperglycemia causes microvascular (retinopathy, nephropathy, neuropathy) and macrovascular (coronary artery disease, cerebrovascular disease, and peripheral artery occlusive disease) complications. Prediabetes (reduced glucose tolerance and impaired fasting plasma glucose) refers to the condition in which glycemia is elevated as compared to normal parameters, but without meeting the diagnostic criteria for diabetes. The identification of prediabetes is important because it increases the risk for diabetes and CVD; in addition, interventions related to lifestyle changes have proven to reduce the risk of diabetes in those individuals.
• The classification of diabetes is based on its etiology. The most prevalent types are type 2 and type 1 diabetes, representing 90-95% and 5-10% of the cases, respectively. Type 2 diabetes usually occurs in adults over the age of 30-40 years, has a complex and multifactorial etiology, involving polygenic inheritance and influence of familial and environmental factors – unhealthy food habits, physical inactivity, and sedentary lifestyle. Its pathophysiology involves insulin resistance and initial increase in insulin production, followed over the years by pancreatic failure to produce that hormone. 307307. Kahn CR, Ferris HA, O’NEILL BT. Pathophysiology of Type 2 Diabetes Mellitus. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A. Williams Textbook of Endocrinology. 14th ed. Philadelphia: Elsevier; 2019. Chapter 34.
• Type 1 diabetes usually affects children, adolescents, or young adults, has an autoimmune, polygenic etiology resulting from the destruction of pancreatic beta cells and complete insulin deficiency. It can occur in adults (former LADA – latent autoimmune diabetes in adults, currently known as type 1 adult diabetes). It is subdivided into types 1A and 1B depending on the presence of autoantibodies. Autoantibodies are detected in type 1A diabetes, as well as a genetic predisposition associated with environmental factors that trigger the immune response (viral infections, components of the diet and of the intestinal microbiota). Type 1B diabetes is autoantibody-negative and its etiology is idiopathic. Cardiovascular disease is the major cause of death in patients with diabetes, who have twice the risk of major cardiovascular events as compared to the population without the disease, in addition to worse response to treatment and worse outcomes after a cardiovascular event (acute myocardial infarction, stroke). The classic cardiovascular risk factors [smoking, arterial hypertension, high levels of LDL-cholesterol, low levels of HDL-cholesterol] maximize that risk, the duration of diabetes, and the coexistence of microvascular complications. The cardiovascular complications of diabetes include coronary artery disease, cerebrovascular disease, and peripheral artery disease. 308308. Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241(19):2035-2038. doi:10.1001/jama.241.19.2035. , 309309. MICHAEL BROWNLEE, LLOYD P. AIELLO, JENNIFER K. SUN, MARK E. COOPER, EVA L. FELDMAN, JORGE PLUTZKY, AND ANDREW J.M. BOULTON. Complications of Diabetes Mellitus. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A. Williams Textbook of Endocrinology. 14th.
• Diabetes directly affects the quality of life, productivity, and survival, in addition to having an important economic impact on health systems. Meeting glycemic targets and control of other cardiovascular risk factors are known to contribute to prevent and delay the progression of the disease’s chronic complications. The systemic impairment of several organs and the disease’s complexity require global care for the patient, comprising several aspects of the treatment. 309309. MICHAEL BROWNLEE, LLOYD P. AIELLO, JENNIFER K. SUN, MARK E. COOPER, EVA L. FELDMAN, JORGE PLUTZKY, AND ANDREW J.M. BOULTON. Complications of Diabetes Mellitus. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A. Williams Textbook of Endocrinology. 14th.
• In this chapter, diabetes mellitus is approached as a cardiovascular risk factor, as it has been identified since the classic Framingham study. 308308. Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241(19):2035-2038. doi:10.1001/jama.241.19.2035. The presence of diabetes mellitus in association with smoking, systemic arterial hypertension, and dyslipidemia increases by two to three times the risk of CVD. 310310. Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16(2):434-444. doi:10.2337/diacare.16.2.434.
Prevalence
• Teló et al ., in a systematic review with meta-analysis of Brazilian observational studies from 1980 to 2015, including 50 articles, have shown the increasing prevalence of diabetes in recent decades. The prevalence of diabetes was as follows: 5.6% (95% CI: 5.0 – 6.3) by self-report (36 studies); 6.6% (95% CI: 4.8 – 8.9) by fasting plasma glucose (7 studies); and 11.9% (95% CI: 7.7 – 17.8) by oral glucose tolerance test (7 studies). In trend analyses, increase in the prevalence of diabetes was observed over time, the biggest increase being observed in studies using the oral glucose tolerance test in the diagnosis: 7.4% (95% CI: 7.1 – 7.7) in the 1980s, 12.1% (95% CI: 10.5 – 13.8) in the 1990s, 14.5% (95% CI: 13.1 – 16.0) in the 2000s, and 15.7% (95% CI: 9.8 – 24.3) in the 2010s. 311311. Telo GH, Cureau FV, de Souza MS, Andrade TS, Copês F, Schaan BD. Prevalence of diabetes in Brazil over time: a systematic review With meta-analysis. Diabetol Metab Syndr. 2016;8(1):65. doi:10.1186/s13098-016-0181-1.
• Considering the IDF data published in 2019, Brazil ranked 5th regarding the number of adults with diabetes worldwide, totaling 16.8 million (95% CI: 15.0 – 18.7) people with that disease, 46% of whom did not know they had the disease. The prevalence of prediabetes was 9.5% (15.1 million people). 312312. International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: International Diabetes Federation; 2019.
• Data from the PNS (2014 to 2015) have shown the following prevalence of diabetes according to different criteria: 6.6% (95% CI: 5.9 – 7.2) [HbA1c ≥ 6.5%]; 8.4% (95% CI: 7.6 – 9.1) [HbA1c ≥ 6.5% or use of antidiabetic drugs]; 9.4% (95% CI: 8.6 – 10.1) [HbA1c ≥ 6.5% or history of diabetes], and 7.5% (95% CI: 6.7 – 8.2) [history of diabetes]. That information is presented according to sex, Brazilian geographical regions (Table 8-1), age range, educational level, self-reported skin color, and BMI (Table 8-2), considering the most comprehensive criterion (HbA1c ≥ 6.5% or use of antidiabetic drugs). For all criteria, the prevalence was higher in women, individuals aged over 30 years, and among those with overweight or obesity. Higher educational level was associated with lower prevalence of diabetes, and the West-Central region had the highest prevalence of all Brazilian regions. 2828. Malta DC, Bernal RT, Souza MF, Szwarcwald CL, Lima MG, Barros MB. Social Inequalities in the Prevalence of Self-Reported Chronic Non-Communicable Diseases in Brazil: National Health Survey 2013. Int J Equity Health. 2016;15(1):153. doi: 10.1186/s12939-016-0427-4.
• Malta et al. , in a cross-sectional study including self-reported data of 60 202 Brazilians, have analyzed the inequalities in the self-reported prevalence of noncommunicable diseases, including diabetes. The prevalence of diabetes was higher among illiterate individuals or those with incomplete elementary education and those with incomplete secondary education [9.61% (PR 1.42, 95% CI: 1.13-1.77) and 5.36% (PR 1.59, 95% CI: 1.23-2.06), respectively], while those with higher education had a 4.18% prevalence. 2828. Malta DC, Bernal RT, Souza MF, Szwarcwald CL, Lima MG, Barros MB. Social Inequalities in the Prevalence of Self-Reported Chronic Non-Communicable Diseases in Brazil: National Health Survey 2013. Int J Equity Health. 2016;15(1):153. doi: 10.1186/s12939-016-0427-4.
• Iser et al. have shown, using data from the PNS (2014 to 2015), that the prevalence of prediabetes was 18.5% (95% CI: 17.4 – 19.7), according to the American Diabetes Association (HbA1c: 5.7-6.4%), and 7.5% (95% CI: 6.7 – 8.3), according to the World Health Organization criterion (HbA1c: 6.0-6.4%). 313313. Iser BPM, Pinheiro PC, Malta DC, Duncan BB, Schmidt MI. Prediabetes and intermediate hyperglycemia prevalence in adults and associated factors, Health National Survey. Cien Saude Colet. 2021;26(2):531-540. doi:10.1590/1413-81232021262.34852020.
• In 2019, Teló et al. have published the results of a big cross-sectional study developed in a representative sample of Brazilian students aged 12 to 17 years showing that, of the 37 854 young individuals enrolled, 3.3% (95% CI: 2.9 – 3.7) had type 2 diabetes (HbA1c: ≥6.5% or fasting plasma glucose ≥ 126 mg/dL or history of diabetes) and 22.0% (95% CI: 20.6 – 23.4) had prediabetes (HbA1c: between 5.7% and 6.5% or fasting plasma glucose between 100 and 126 mg/dL). 314314. Telo GH, Cureau F V, Szklo M, Bloch K V, Schaan BD. Prevalence of type 2 diabetes among adolescents in Brazil: Findings From Study of Cardiovascular Risk in Adolescents (ERICA). Pediatr Diabetes. 2019;20(4):389-396. doi:10.1111/pedi.12828.
Incidence
• Most studies on the incidence of diabetes have reported data from high-income countries, and usually from the adult population, thus reflecting mainly the incidence of type 2 diabetes. In children and adolescents, type 2 diabetes has been increasing in several countries because of the increase in the prevalence of overweight, obesity, physical inactivity, and sedentary lifstyle. 312312. International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: International Diabetes Federation; 2019.
• Schmidt et al. have recruited from 2008 to 2010 and followed up for 3.7 ± 0.63 years 11 199 civil servants without diabetes from the Brazilian multicenter study, the ELSA-Brazil Study. Diabetes was diagnosed in the follow-up if fasting plasma glucose ≥ 126 mg/dL or glycemia after oral glucose tolerance test ≥ 200 mg/dL or HbA1c ≥ 6.5%. The cumulative incidence of diabetes was 2.0 per 100 person-years (95% CI: 1.8 – 2.1), similar in men and women, higher in individuals over the age of 65 years [2.8%; 95% CI: 2.3 – 3.4], obese (3.8%; 95% CI: 3.4 – 4.3) and those with lower educational level (3.0%; 95% CI: 2.6 – 3.6). 315315. Schmidt MI, Bracco PA, Yudkin JS, Bensenor IM, Griep RH, Barreto SM, Castilhos CD, Duncan BB. Intermediate Hyperglycaemia to Predict Progression to Type 2 Diabetes (ELSA-Brasil): An Occupational Cohort Study in Brazil. Lancet Diabetes Endocrinol. 2019;7(4):267-77. doi: 10.1016/S2213-8587(19)30058-0.
• Sitnik et al ., in a prospective cohort of 1536 individuals without diabetes in 1998 (fasting plasma glucose collection date), civil servants of the University of São Paulo, participants of the ELSA-Brazil Study, aged 23-63 years, have assessed the association of fasting plasma glucose, incidence of diabetes, subclinical atherosclerosis and cardiovascular events. The adjusted diabetes incidence rate was 9.8/1000 person-years (95% CI: 7.7 – 13.6 /1000 person-years). 316316. Sitnik D, Santos IS, Goulart AC, Staniak HL, Manson JE, Lotufo PA, Bensenor IM. Fasting Glucose Levels, Incident Diabetes, Subclinical Atherosclerosis and Cardiovascular Events in Apparently Healthy Adults: A 12-year Longitudinal Study. Diab Vasc Dis Res. 2016;13(6):429-37. doi: 10.1177/1479164116653356.
• The number of children and adolescents with type 1 diabetes has increased worldwide, approximately 3% per year, although with important regional differences. 312312. International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: International Diabetes Federation; 2019. , 317317. Group DP. Incidence and trends of childhood Type 1 diabetes worldwide 1990-1999. Diabet Med. 2006;23(8):857-866. doi:10.1111/j.1464-5491.2006.01925.x. ,3186, 1212. França E, Abreu DX, Rao C, Lopez AD. Evaluation of Cause-of-Death Statistics for Brazil, 2002-2004. Int J Epidemiol. 2008;37(4):891-901. doi: 10.1093/ije/dyn121. , 1313. Escosteguy CC, Portela MC, Medronho RA, Vasconcellos MT. O Sistema de Informações Hospitalares e a Assistência ao Infarto Agudo do Miocárdio. Rev Saude Publica. 2002;36(4):491-9. doi: 10.1590/s0034-89102002000400016. Brazil ranks third in the number of new cases of children and adolescents aged 0-14 years with type 1 diabetes (7.3 cases per 1000/year), in addition to the prevalence of the disease in that same age range (51.1 per 1000). 312312. International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: International Diabetes Federation; 2019.
• Negrato et al. have described the annual incidence of type 1 diabetes from 1986 to 2015 in the city of Bauru, São Paulo state, in children ≤ 14 years of age, using individual case report and capture and recapture method. In that period, 302 cases were identified, an incidence of 12.8 per 100 000 inhabitants (95% CI: 11.2 – 14.4), ranging from 2.8 per 100 000 inhabitants in 1987 to 25.6 per 100 000 inhabitants in 2013, without difference between sexes. 319319. Negrato CA, Lauris JRP, Saggioro IB, Corradini MCM, Borges PR, Crês MC, Leal A Jr, Guedes MFS, Gomes MB. Increasing Incidence of Type 1 Diabetes Between 1986 and 2015 in Bauru, Brazil. Diabetes Res Clin Pract. 2017;127:198-204. doi: 10.1016/j.diabres.2017.03.014.
Mortality
Overall Mortality Attributable to Diabetes
• Klafke et al. have described trends in mortality from acute complications of diabetes (ketoacidosis, hyperosmolarity and hypoglycemia) in Brazil, for all ages, from 1991 to 2010, when the SUS was implemented. Using data from the IBGE and the SIM, over that period, 694 769 deaths from diabetes were registered, of which 81 208 (11.7%) were due to acute complications. In 1991, 2070 men died from acute complications of diabetes, with an age-adjusted mortality rate per 100 000 inhabitants of 7.4 (95% CI: 7.2 – 7.6), while 2832 women died, with mortality rate of 9.7 per 100 000 inhabitants (95% CI: 9.1 – 9.6), yielding a woman/man mortality rate of 1.3. As compared to 1991, in 2010, 1600 men died from acute complications of diabetes, with mortality rate of 2.4 per 100 000 inhabitants (95% CI: 2.3 – 2.5), while 2141 women died, with mortality rate of 2.5 per 100 000 inhabitants (95% CI: 2.4 – 2.6), yielding a woman/man mortality rate of 1.0. Thus, mortality from complications of diabetes in 20 years decreased 70.9% (95% CI: 67.2 – 74.5), from 8.42 (95% CI: 8.3 – 8.6) deaths per 100 000 inhabitants in 1991 for both sexes to 2.45 per 100 000 inhabitants (95% CI: 2.4 – 2.5) in 2010. That reduction occurred in both sexes, all ages, and in all Brazilian regions. 320320. Klafke A, Duncan BB, Stevens A, Rosa Rdos S, Moura L, Malta D, Schmidt MI. The Decline in Mortality Due to Acute Complications of Diabetes Mellitus in Brazil, 1991-2010. BMC Public Health. 2015;15:772. doi: 10.1186/s12889-015-2123-5.
• Malhão et al. have assessed the diabetes mortality trends in Brazil, per sex, in adults ≥ 20 years of age, from 1980 to 2012, using data from IBGE and SIM. From 1980 to 2012, 955 455 individuals had diabetes as their underlying cause of death, and 551 016 were women (57.7%) and 404 439, men (42.3%). In that period, the age-standardized mortality rate per 100 000 inhabitants increased from 20.8 (95% CI: 20.2 – 21.5) to 47.6 (95% CI: 47.0 – 48.2) for men, and from 28.7 (95% CI: 27.9 – 29.4) to 47.2 (95% CI: 46.7 – 47.7) for women. Considering the entire period analyzed, that rate increased 2.9% per year for men (mean annual percent change of 2.9; 95% CI: 2.6 – 3.1) and 1.7% for women (mean annual percent change of 1.7; 95% CI: 1.5 – 1.9). Considering diabetes as the underlying or associated cause of death from 2001 to 2012, there were 1 076 434 deaths [603 686 women (56.1%); 472 748 men (43.9%)]. In that period, the age-standardized mortality rate increased from 76.1 per 100 000 inhabitants (95% CI: 75.2 – 77.0) to 95.6 per 100 000 inhabitants (95% CI: 94.8 – 96.5) in men, and from 83.7 per 100 000 inhabitants (95% CI: 82.9 – 84.6) to 93.3 per 100 000 inhabitants (95% CI: 92.6 – 94.1) in women. 321321. Malhão TA, Brito ADS, Pinheiro RS, Cabral C da S, Camargo TMCR de, Coeli CM. Sex Differences in Diabetes Mellitus Mortality Trends in Brazil, 1980-2012. PLoS One. 2016;11(6):e0155996. doi:10.1371/journal.pone.0155996.
• Duncan et al. , using data on diabetes and hyperglycemia from the GBD Study 2015 for all ages, have shown that in Brazil, in 2015, the diabetes mortality rate was 26.8 per 100 000 inhabitants (95% CI: 25.0 – 28.5) for men and 33.2 per 100 000 inhabitants (95% CI: 31.1 – 35.2) for women. 322322. Duncan BB, França EB, Passos VMA, Cousin E, Ishitani LH, Malta DC, Naghavi M, Mooney M, Schmidt MI. The Burden of Diabetes and Hyperglycemia in Brazil and its States: Findings From the Global Burden of Disease Study 2015. Rev Bras Epidemiol. 2017;20(Suppl 01):90-101. doi: 10.1590/1980-5497201700050008.
• Duncan et al. , using data on diabetes and hyperglycemia from the GBD Study 2016-2017 for all ages, have shown that, in that period, type 1 diabetes age-standardized mortality rate decreased by more than 50% for women and about 10% for men, thus the sex-specific mortality rates, which were different in the beginning of the period, converged. Age-standardized mortality rates for type 2 diabetes, however, remained stable during the period, with a slight reduction for women and slight increase for men. When considering the crude overall rates, however, mortality from type 2 diabetes increased dramatically, basically doubling in the period. In addition, those authors have shown that the highest mortality rates from diabetes in 2017 occurred mainly in the Northeastern states, and the highest increases in mortality from 1990 to 2017 were observed in the Northern, Northeastern and West-Central regions, and the greatest reductions in the Southeastern region. 323323. Duncan BB, Cousin E, Naghavi M, Afshin A, França EB, Passos VMA, Malta D, Nascimento BR, Schmidt MI. The Burden of Diabetes and Hyperglycemia in Brazil: A Global Burden of Disease Study 2017. Popul Health Metr. 2020;18(Suppl 1):9. doi: 10.1186/s12963-020-00209-0.
• Data from the GBD Study 2019 have shown that, although the age-standardized mortality rates from diabetes have substantially decreased in recent years in Brazil, the total number of deaths from diabetes has increased (Chart 8-3A). There were 87 644 (95% CI: 71 924 -110 625) and 174 198 (95% CI: 142 704 – 217 111) deaths from diabetes in Brazil in 1990 and 2019, respectively (Chart 8-1A). Age-standardized mortality rate per 100 000 inhabitants was 116.8 (95% CI: 92.8 – 152.0) in 1990 and 77.0 (95% CI: 63.0 – 96.7) in 2019, decreasing by 34% (95% CI: -40.1 to -28.1) in that period. That reduction was not homogeneous in the Brazilian regions and FUs, being more pronounced in the Southeastern, West-Central and Southern regions and the Distrito Federal, with a slight to small reduction in several Northern FUs. It is worth noting that the reduction trend in age-standardized mortality rate from diabetes occurred in all age groups, but more significantly in the age group from 5 to 14 years (-45.8%; 95% CI: -57.2 to -33.1) and less significantly in the age group from 15 to 49 years (-24.8%; 95% CI: -30.7 to -18.5), with intermediate reductions in the age groups > 70 years (-26%; 95% CI: -33.2 to -18.2) and 50-69 years (-33.2%; 95% CI: -40.1 to -26.4). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Cardiovascular Mortality Attributable to Diabetes
• Mortality from CVD attributable to diabetes for all ages in Brazil, according to GBD 2019 data, increased in absolute numbers from 50 812 deaths (95% CI: 35 649 -73 137) in 1990 to 80 754 (95% CI: 55 922 – 11 8175) in 2019 (Table 8-3 and Chart 8-1B). However, the age-standardized mortality rates per 100 000 inhabitants decreased from 70.4 (95% CI: 47.4 – 106.1) in 1990 to 35.9 (95% CI: 24.5 – 53.0) in 2019, a reduction of -49.0% (95% CI: -53.4 to -43.9) (Chart 8-1C). This reduction trend occurred in a non-uniform way in the FUs, with a more significant reduction in most FUs of the Southern, Southeastern, West-Central and Northern regions and the Distrito Federal, and only modest reductions in the FUs of the Northeastern region. When comparing between sexes, women had greater mortality rate reductions than men in most Brazilian FUs regarding data from 1990 and 2019, except for the states of Maranhão and Piauí and the Distrito Federal (Table 8-4). Regarding the trend according to age group, the reduction in the mortality rate from CVD attributable to diabetes occurred in all age groups: 15 to 49 years (-37.3%; 95% CI: -46.8 to -25.3), 50 to 69 years (-46.0%; 95% CI: -54.2 to -35.5), and > 70 years (-43.5%; 95% CI: -50.3 a -36.7). It is worth noting that, in 2019, when comparing sex and age groups (Chart 8-2), women had lower proportional mortality rates from CVD attributable to diabetes in almost all age groups described. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Although data from the GBD Study 2019 showed that the total number of deaths attributable to diabetes for all ages and stratified for all causes increased in Brazil from 1990 to 2019 (Chart 8-3A), the age-standardized mortality rate per 100 000 inhabitants decreased in the same period from 116.8 (95% CI: 92.8 – 152.0) to 77 (95% CI: 63.0 – 96.7). It is worth noting that more than 85% of that reduction occurred due to the decrease in the rates of ischemic heart disease, from 39.8% (95% CI: 21.3 - 65.3) in 1990 to 20.9% (95% CI: 11.6 – 34.4) in 2019, and of stroke, from 30.3% (95% CI: 18.2 – 54.8) in 1990 to 14.7% (95% CI: 8.6 – 25.6) in 2019 (Chart 8-3B). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• The SDI is an estimate of the socioeconomic level of a certain place and Chart 8-4 shows the relation of that index in 2019 and the percent change in deaths from CVD attributable to diabetes from 1990 to 2019. The data show the correlation between the greater percent change in the age-standardized mortality rate from 1990 to 2019 and the SDI in 2019, suggesting that the reduction in CVD mortality followed the improvement in socioeconomic conditions. The FUs with lower SDI had smaller percent changes in deaths (more deaths), except for Roraima and Rondônia, while the FUs with higher SDI had higher percent changes in deaths (less deaths), such as São Paulo, Rio de Janeiro, and the Distrito Federal.
Burden of Disease
Burden of Disease Attributable to Diabetes
• Data from the GBD Study 2019 estimated a reduction in the age-standardized DALY rates per 100 000 inhabitants attributable to diabetes in Brazil of -26.1% (95% CI: -31.7 to -20.9) from 1990 to 2019, despite the increase in the total number of DALYs from 2 448 714.5 (95% CI: 2 087 403.6 – 2 919 735.6) to 4 778 225.9 (95% CI: 4 017 716.8 – 5 709 063.5) in the period. The reduction in the DALY rate, although occurring in all age groups, was more pronounced in the FUs of the Southeastern, Southern and West-Central regions and the Distrito Federal, being less significant in many FUs of the Northern and Northeastern regions, including the increase in the DALY rate in the states of Amapá, Ceará, and Maranhão. When comparing between sexes, the DALY rate reduction was more significant in women (-37.7%; 95% CI: 44.2 to -31.1) than in men (-29.9%; 95% CI: 36.9 to -22.3) for the same period. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Burden of Cardiovascular Disease Attributable to Diabetes
• Data from the GBD Study 2019 regarding the burden of CVD estimated a reduction in the age-standardized DALY rates attributable to diabetes in Brazil (Chart 8-1D and Table 8-5) of -47.4% (95% CI: -52.2 to -41.9) per 100 000 inhabitants from 1990 to 2019, despite the increase in the total number of DALYs from 1 072 309 (95% CI: 784 276 - 1 484 959) to 1 571 116 (95% CI: 1 140 912 – 2 203 188) in the period. This rate reduction occurred due to the reduction in the YLLs of -33.4% (95% CI: -42.5 to -15) from 1990 to 2019. In the same period, there was an increase in the YLDs of 17.6% (95% CI: 0.4 – 50.5). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• There was a heterogeneous reduction in the age-standardized DALY rates attributable to diabetes among the Brazilian FUs and regions, more marked in the FUs of the Southeastern, Southern, and West-Central regions and the Distrito Federal, with a mild reduction in the FUs of the Northern region and an even milder reduction in most FUs of the Northeastern region.
• Data from the GBD Study 2019 showed that the reduction in the age-standardized DALY rates attributable to diabetes from 1990 to 2019 occurred in all age groups: 15-49 years (-36.5%; 95% CI: -46.0 to -24.5), 50-69 years (-45.5%; 95% CI: -53.4 to -35.2) and > 70 years (-46.2%; 95% CI: -52.5 to -39.1). For men of all ages, the variation was -43.1% (95% CI: -49.4 to -35.1), and for women of all ages, the variation was -52.0% (95% CI: -58.5 to -44.5). Only in the states of Maranhão and Piauí, men had a higher reduction as compared to women. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Impact on Cardiovascular Health
• Fuchs et al. , in a cross-sectional study carried out in 2005 in the city of Porto Alegre, Rio Grande do Sul state, with adults (18 to 90 years of age), assessed the association of clustering of risk factors and self-reported CVD. The participants were interviewed at home about the presence of diabetes, physical activity, and diet pattern, in addition to assessed regarding the presence of systemic arterial hypertension. The sample consisted of 1007 women, mostly white (73.0%), mean age of 44.8±0.8 years, and mean schooling of 9.3±0.3 years. Arterial hypertension, diabetes, obesity, low fruit and vegetable intake, and lack of vigorous or moderate physical activity were clustered into a combination of risk factors, which independently associated with the self-reported CVD. The major cluster included the presence of arterial hypertension and diabetes, representing an independent risk ratio of 8.5 (95% CI: 3.0 – 24.5). 281281. Fuchs SC, Moreira LB, Camey SA, Moreira MB, Fuchs FD. Clustering of Risk Factors for Cardiovascular Disease Among Women in Southern Brazil: A Population-Based Study. Cad Saude Publica. 2008;24(Suppl 2):S285-93. doi: 10.1590/s0102-311x2008001400013.
• Cardoso el al. reported the results of a prospective observational study carried out in Rio de Janeiro from August 2004 to December 2008 with 620 adults with type 2 diabetes, followed up until August 2013 in a diabetes outpatient clinic from a Brazilian university-affiliated hospital. Those authors aimed to relate the HbA1c levels with cardiovascular outcomes. The HbA1c levels were measured at baseline and 3-4 times per year during follow-up. The primary endpoints were a composite of total fatal and nonfatal cardiovascular events, major cardiovascular events, and all-cause mortality. Cardiovascular and noncardiovascular mortalities were the secondary endpoints. The sample’s mean age was 60.4±9.4 years, 37.1% were men, 55% Caucasians. After a median follow-up of 79 [59-93] months, 125 total cardiovascular events occurred (90 major events), with a total of 111 deaths (64 due to CVD). After statistical adjustment to other cardiovascular risk factors, baseline HbA1c and mean HbA1c in the first year were predictors of total cardiovascular events (HR 1.13; 95% CI: 1.04 – 1.23 and HR 1.26; 95% CI: 1.12 – 1.41, respectively), of major cardiovascular events (HR 1.15; 95% CI: 1.04 – 1.28 and HR 1.27; 95% CI: 1.11 –1.45, respectively), of all-cause mortality (HR 1.10; 95% CI: 1.00 – 1.21 and HR 1.18; 95% CI: 1.04 – 1.35, respectively) and cardiovascular mortality (HR 1.14; 95% CI: 1.01 – 1.27 and HR 1.27; 95% CI: 1.08 – 1.50, respectively). Every 1% increase in the mean HbA1c in the first year increased by 27.0% (95% CI: 11.0 – 45.0) the risk of major cardiovascular events. Cardiovascular protection was observed up to HbA1c levels lower than 6.5%. On the second year, however, HbA1c was not a predictor of any endpoint (HR 1.12; 95% CI: 0.98 – 1.28; p=0.09 for total cardiovascular events; HR 1.09; 95% CI: 0.92 – 1.29; p=0.32 for major cardiovascular events). 324324. Cardoso CRL, Leite NC, Salles GF. Prognostic Importance of C-Reactive Protein in High Cardiovascular Risk Patients With Type 2 Diabetes Mellitus: The Rio de Janeiro Type 2 Diabetes Cohort Study. J Am Heart Assoc. 2016;5(11). doi:10.1161/JAHA.116.004554.
• Sitnik et al. , in a prospective cohort of 1536 individuals without diabetes in 1998 (fasting plasma glucose collection date), civil servants of the University of São Paulo, participants of the ELSA-Brazil Study, aged 23-63 years, aimed to assess the association of fasting plasma glucose and incidence of diabetes with subclinical atherosclerosis and cardiovascular events. Fasting plasma glucose levels of 110-125mg/dL were associated with higher carotid intima-media thickness (β 0.028; 95% CI: 0.003 – 0.053). Excluding the individuals who developed diabetes in the follow-up, there was a borderline association between higher carotid intima-media thickness and fasting plasma glucose levels of 110-125mg/dL (β 0.030; 95% CI: -0.005 to 0.065). Diabetes was associated with higher carotid intima-media thickness (β 0.034; 95% CI: 0.015 – 0.053), coronary artery calcium scores ≥ 400 (OR 2.84; 95% CI: 1.17 – 6.91) and the combined outcome of coronary artery calcium score ≥ 400 or cardiovascular event (OR 3.50; 95% CI: 1.60 – 7.65). 316316. Sitnik D, Santos IS, Goulart AC, Staniak HL, Manson JE, Lotufo PA, Bensenor IM. Fasting Glucose Levels, Incident Diabetes, Subclinical Atherosclerosis and Cardiovascular Events in Apparently Healthy Adults: A 12-year Longitudinal Study. Diab Vasc Dis Res. 2016;13(6):429-37. doi: 10.1177/1479164116653356.
• Schaan et al. , analyzing data from the REACT Study, a Brazilian multicenter registry, carried out from July 2010 to May 2016, aimed to establish the long-term risk for clinical events of patients at high cardiovascular risk in Brazil. The project was idealized and coordinated by the SBC, with the participation of private and public centers from all Brazilian regions, respecting the population distribution according to IBGE data. A total of 5006 individuals aged ≥ 45 years were included and divided in the following four groups: no diabetes and no previous cardiovascular event (n = 430); diabetes and no previous cardiovascular event (n = 1138); no diabetes and previous cardiovascular event (n = 1747); and diabetes and previous cardiovascular event (n = 1691). Previous cardiovascular event was defined as evidence of coronary artery disease, stroke or transient ischemic accident, peripheral artery disease, presence of three cardiovascular risk factors – except for diabetes (arterial hypertension, dyslipidemia, age > 70 years, family history of coronary artery disease, asymptomatic carotid artery disease). Major clinical events (all-cause mortality, nonfatal myocardial infarction, nonfatal cardiopulmonary arrest, and nonfatal stroke) were observed in 332 patients during the 1-year follow-up. Previous cardiovascular event was associated with a higher risk for another event during follow-up (HR 2.31; 95% CI: 1.74 – 3.05, p<0.001), as was the presence of diabetes (HR 1.28; 95% CI: 1.10 – 1.73, p=0.005). Patients with diabetes, failing to meet the HbA1c target, had worse event-free survival as compared to patients with good metabolic control (HR 1.70; 95% CI: 1.01 – 2.84, p=0.044). 325325. . Diabetes and cardiovascular events in high-risk patients: Insights From a multicenter registry in a middle-income country Beatriz D Schaan 1, Jose Albuquerque de Figueiredo Neto 2, Leila Beltrami Moreira 3, Priscila Ledur 4, Luiz Alberto P Mattos 5, Danie.
• Rezende et al. , in a retrospective cohort study, included 888 patients with type 2 diabetes and multivessel coronary artery disease in the MASS Registry from the Instituto do Coração of the University of São Paulo from January 2003 to December 2007. The patients were followed-up with outpatient visits every 6 months and prospectively assessed for cardiovascular events. Of the 888 patients, 725 (81.6%) had complete clinical and HbA1c data for analysis. The sample’s characteristics were as follows: median age, 62.4 years (55.7 – 68.0); 467 men (64.4%); median follow-up, 10.0 years (8.0 – 12.3); and a mean amount of 9.5±3.8 HbA1c values for each patient. The composite endpoint of death, myocardial infarction or ischemic stroke occurred in 262 patients (36.1%). An increase of 1 point in the longitudinal HbA1c value was significantly associated with a 14% higher risk of the combined endpoint of all-cause mortality, myocardial infarction, and ischemic stroke (HR 1.14; 95% CI: 1.04 – 1.24; p=0.002) in the unadjusted analysis. After adjusting for baseline factors (age, sex, 2-vessel or 3-vessel coronary artery disease, initial coronary artery disease treatment, ejection fraction, creatinine and LDL-cholesterol levels), a 1-point increase in the longitudinal HbA1c value was associated with a 22% higher risk of the combined endpoint (HR 1.22; 95% CI: 1.12 – 1.35; p<0.001). 326326. Rezende PC, Hlatky MA, Hueb W, Garcia RMR, Selistre LS, Lima EG, Garzillo CL, Scudeler TL, Boros GAB, Ribas FF, Serrano CV Jr, Ramires JAF, Kalil Filho R. Association of Longitudinal Values of Glycated Hemoglobin With Cardiovascular Events in Patients With Type 2 Diabetes and Multivessel Coronary Artery Disease. JAMA Netw Open. 2020;3(1):e1919666. doi: 10.1001/jamanetworkopen.2019.19666.
Knowledge, Treatment and Control Diabetes
• The treatment of diabetes is based on three pillars: diet, physical exercise, and drugs (oral antidiabetic drugs and insulin). A cross-sectional multicenter study published in 2016 by Gomes and Negrato 327327. Gomes MB, Negrato CA. Adherence to insulin therapeutic regimens in patients With type 1 diabetes. A nationwide survey in Brazil. Diabetes Res Clin Pract. 2016;120:47-55. doi:10.1016/j.diabres.2016.07.011. with a convenience sample of 1698 patients with type 1 diabetes from 10 Brazilian cities, assessed adherence to treatment (Morisky medication scale questionnaire), which was maximal in 9.8% of them, moderate in 42.2%, and minimal in 48.0%. Lower adherence was associated with higher HbA1c values (9.2 ± 2.2%, 8.9 ± 2.0%, and 8.6 ± 1.9%, respectively) for each group cited. 327327. Gomes MB, Negrato CA. Adherence to insulin therapeutic regimens in patients With type 1 diabetes. A nationwide survey in Brazil. Diabetes Res Clin Pract. 2016;120:47-55. doi:10.1016/j.diabres.2016.07.011.
• A randomized clinical trial involving 238 patients with type 2 diabetes has compared an empowerment program for selfcare based on a behavior change protocol and its effect on glycemic control, and showed that the group randomized for the intervention had lower Hba1c levels (7.5 ± 1.7% vs. 8.1 ± 2.2%). 328328. Cortez DN, Macedo MM, Souza DA, Santos JC, Afonso GS, Reis IA, Torres HC. Evaluating the Effectiveness of an Empowerment Program for Self-Care in Type 2 Diabetes: A Cluster Randomized Trial. BMC Public Health. 2017;17(1):41. doi: 10.1186/s12889-016-3937-5.
• In 2017, Meiners et al. , based on data from a household population-based survey (PNAUM) with cross-sectional design and a probabilistic sample of the Brazilian population, have assessed the access and adherence to treatment of 2624 patients with diabetes aged > 20 years. Total access to the medications studied was 98%, while adherence was probable in 71% (95% CI: 67.2 – 74.5), probably low in 9.8% (95% CI: 8.0 – 12.0), and low in 17.2% (95% CI: 14.6 – 20.1), with better adherence rates in the West-Central region. 329329. Meiners MMMA, Tavares NUL, Guimarães LSP, Bertoldi AD, Pizzol TDSD, Luiza VL, Mengue SS, Merchan-Hamann E. Access and Adherence to Medication Among People With Diabetes in Brazil: Evidences From PNAUM. Rev Bras Epidemiol. 2017;20(3):445-59. doi: 10.1590/1980-5497201700030008.
• Self-reported adherence to treatment and its associated factors were assessed by Marinho et al. in 2018 in a cross-sectional study with 476 patients with diabetes in a tertiary hospital. Good adherence was 93.5% for medication use, 59.3% for foot care, 56.1% for glycemic monitoring, 29.2% for diet, and 22.5% for physical exercise. The following were associated with good adherence: younger age, lower BMI, presence of macrovascular complications, better occupational performance and emotional domain of SF-36. 330330. Marinho FS, Moram CBM, Rodrigues PC, Leite NC, Salles GF, Cardoso CRL. Treatment Adherence and Its Associated Factors in Patients With Type 2 Diabetes: Results From the Rio de Janeiro Type 2 Diabetes Cohort Study. J Diabetes Res. 2018;2018:8970196. doi:10.1155/2018/8970196.
• In 2018, Silva et al. conducted a household survey in 63 municipalities of Minas Gerais state, selected by convenience, aimed at assessing the use of drugs in patients with diabetes. The study assessed 2619 patients with diabetes (83.7% with type 2 diabetes and 10.4% with type 1 diabetes, mean age of 61.3 ± 16.4 years) and reported the use of 13 629 drugs, 35% were generic drugs and 60% acquired in public drugstores. The most frequently used drugs were metformin, losartan, glybenclamide, and simvastatin. Polypharmacy (use of five or more drugs) was identified in 56.5% (95% CI: 3.4) of the respondents. The factors associated with the occurrence of polypharmacy were age group of 40-59 years (OR 2.46; 95% CI: 1.68 – 3.61), age > 60 years (OR 4.58; 95% CI: 3.18 – 6.60), self-perception of poor or very poor health (OR 1.75; 95% CI: 1.26 – 2.38), presence of five or more comorbidities (OR 3.45; 95% CI: 2.84 – 4.19), mean time of diagnosis > 10 years (OR 1.64; 95% CI: 1.36 – 1.98), having at least four medical visits within the past year (OR 1.79; 95% CI: 1.48 – 2.16), lack of regular physical activity (OR 1.47; 95% CI: 1.22 – 1.78), interruption of the usual activities in the past 15 days (OR 1.30; 95% CI: 1.03 – 1.64), and having private health insurance (OR 1.39; 95% CI: 1.13 – 1.70). 331331. Silva MRRD, Diniz LM, Santos JBRD, Reis EA, Mata ARD, Araújo VE, Álvares J, Acurcio FA. Drug Utilization and faCtors Associated With Polypharmacy in Individuals With Diabetes Mellitus in Minas Gerais, Brazil. Cien Saude Colet. 2018;23(8):2565-2574. doi: 10.1590/1413-81232018238.10222016.
• Leitão et al. , in a cross-sectional population-based study with individuals aged ≥ 20 years, reporting a medical diagnosis of diabetes and interviewed over the telephone (VIGITEL System) from 2012 to 2018, estimated the prevalence of use and distribution of sources of oral antidiabetic drugs in Brazil, according to sociodemographic variables. The prevalence of the use of oral antidiabetic drugs in Brazil increased from 77.4% (95% CI: 74.3 – 80.1) in 2012 to 85.2% (95% CI: 82.8 – 87.2) in 2018, and, in the Southern region, that use increased from 73.4% (95% CI: 67.8 – 78.4) in 2012 to 84.9% (95% CI: 79.7 – 88.9) in 2018. There was a decrease in the access to oral antidiabetic drugs in the public health system (SUS) pharmacies and an increase in the access to those drugs in popular pharmacies, without significant changes in that access in private drugstores. 332332. Leitão VBG, Francisco PMSB, Malta DC, Costa KS. Tendency of use and sources for obtaining oral antidiabetic drugs for treatment of diabetes in Brazil From 2012 to 2018: analysis of the Vigitel survey. Rev Bras Epidemiol. 2021;24:e210008. doi:10.1590/1980-549720210008.
• A cross-sectional study with convenience sampling from 20 Brazilian medical centers, regarding healthcare provided between 2006 and 2007, described the glycemic control of 5692 patients with diabetes > 18 years (1904 men and 3788 women). Of those, 72% of the men and 74% of the women had HbA1c levels > 7.0%. 333333. Duarte FG, Moreira SS, Almeida MDCC, Souza Teles CA, Andrade CS, Reingold AL, Moreira ED Jr. Sex Differences and Correlates of Poor Glycaemic Control in Type 2 Diabetes: A Cross-Sectional Study in Brazil and Venezuela. BMJ Open. 2019;9(3):e023401. doi: 10.1136/bmjopen-2018-023401.
• Schneiders et al ., in a retrospective cohort with 488 patients of primary (n=192) and tertiary (n=192) healthcare, have assessed the following diabetes care quality indicators in patients whose HbA1c level had been assessed in the past year: annual assessment of diabetic nephropathy, retinopathy and neuropathy, lipid profile, nutritional assessment, and inquiry about tobacco use. From the included patients, only 14 (7.3%) in primary healthcare and 52 (27.0%) in tertiary healthcare had at least 50% of those quality indicators covered. The major differences between the healthcare provided to patients in primary and tertiary healthcare were: assessment of diabetic nephropathy (84.8% vs. 95.8%, respectively), retinopathy (13.2% vs. 35.9%, respectively) and neuropathy (9.5% vs. 58.9%), in addition to nutritional assessment (17.2% vs. 38.0%, respectively). 334334. Schneiders J, Telo GH, Bottino LG, Pasinato B, Neyeloff JL, Schaan BD. Quality indicators in type 2 diabetes patient care: analysis per care-complexity level. Diabetol Metab Syndr. 2019;11:34. doi:10.1186/s13098-019-0428-8.
• Alessi et al . have conducted a cross-sectional multicenter study on primary and tertiary healthcare to elderly with type 2 diabetes (>65 years, n=322, 160 in primary and 162 in tertiary healthcare) to assess the number of patients with proper glycemic control considering the need for individualized glycemic targets in a good part of that population. Patients meeting the glycemic targets were those with the following characteristics: HbA1c of 7.0-7.5% for an estimated life expectancy >10 years; HbA1c of 7.5-8.0% for an estimated life expectancy of 5-10 years; and HbA1c of 8.0-8.5% for an estimated life expectancy <5 years. In primary and tertiary healthcare, HbA1c level was over the target in 49.1% and 50.3% of the patients, respectively. In the entire sample, 42.2% of the patients were over the HbA1c target, 28.9% met the target, and 28.9% were below the target. 335335. Alessi J, Telo GH, Oliveira GB, Schneiders J, Zanella MJB, Schaan BD. The Rational Treatment of Diabetes Mellitus in Older Adults: The adequacy of Treatment Decisions Based on Individualized Glycemic Targets in Primary and Tertiary Care. J Diabetes Complications. 2021;35(4):107835. doi: 10.1016/j.jdiacomp.2020.107835.
Risk Factors and Prevention
• Obesity, diet pattern, physical inactivity and sedentary lifestyle are well-known risk factors for the development of type 2 diabetes. The prevalence of diabetes clearly increases as the prevalence of obesity increases. 336336. Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, Lifestyle, and the Risk of Type 2 Diabetes Mellitus in Women. N Engl J Med. 2001;345(11):790-7. doi: 10.1056/NEJMoa010492. Diabetes can be prevented or its onset postponed with lifestyle changes, diet pattern changes, and use of drugs, mostly oral antidiabetic drugs.
• A systematic review with meta-analysis published by Sbaraini et al. in 2021 included 151 studies on the prevalence of overweight and obesity in Brazilian adolescents aged 10-19 years. They reported an increase in overweight prevalence as follows: 8.2% (95% CI: 7.7 – 8.7) up to 2000, 18.9% (95% CI: 14.7 – 23.2) from 2000 to 2009, and 25.1% (95% CI: 23.4 – 26.8) from 2010 onwards, a pattern similar to that of the prevalence of obesity. The Southeastern and Southern regions had higher prevalence of overweight and obesity, without difference between the sexes. 337337. Sbaraini M, Cureau FV, Ritter JDA, Schuh DS, Madalosso MM, Zanin G, Goulart MR, Pellanda LC, Schaan BD. Prevalence of Overweight and Obesity Among Brazilian Adolescents Over Time: A Systematic Review and Meta-Analysis. Public Health Nutr. 2021:1-12. doi: 10.1017/S1368980021001464.
• Those same authors have shown that of 37 892 adolescents enrolled in the ERICA Study, 17.2% were overweight, 5.6% were obese, and 1.3% were severely obese, increasing the chance of adverse cardiometabolic outcomes according to higher BMI, including higher fasting plasma glucose [RP 5.30 (95% CI: 1.94 – 14.50)] and HbA1c (2.04; 95% CI: 1.29 – 3.25). 338338. Sbaraini M, Cureau FV, Sparrenberger K, Teló GH, Kuschnir MCC, Oliveira JS, Leal VS, Bloch KV, Schaan BD. Severity of Obesity is Associated With Worse Cardiometabolic Risk Profile in Adolescents: Findings From a Brazilian National Study (ERICA). Nutrition. 2020;75-6:110758. doi: 10.1016/j.nut.2020.110758.
• Flor et al. have estimated the relation of type 2 diabetes in adults aged > 20 years and its percentage attributable to overweight and obesity in Brazil (Burden of Disease Project 2008 – Brazil). The results showed that 49.2%, 58.3% and 70.6% of diabetes in women were attributable to overweight, obesity, and excess weight, respectively. Regarding men, those percentages were 40.5%, 45.4%, and 60.3%, respectively. Differences were observed in the different Brazilian regions, and the most developed ones, South and Southeast, showed high percentages of diabetes attributable to obesity, while, in the Northern region, diabetes was related to overweight. This behavior might be related to a late epidemiological transition in less favored regions. 339339. Flor LS, Campos MR, Oliveira AF, Schramm JM. Diabetes Burden in Brazil: Fraction Attributable to Overweight, Obesity, and Excess Weight. Rev Saude Publica. 2015;49:29. doi: 10.1590/s0034-8910.2015049005571.
• In the baseline of the ELSA-Brasil Study, the analysis of 14 912 Brazilian civil servants has shown higher prevalence of diabetes among individuals with BMI of 25-29.9 kg/m2(18.9%; 95% CI: 18.0 – 19.9%) and above 30 kg/m2(32.1%; 95% CI: 30.6 – 33.6%) as compared to those with BMI ≤ 24.9 kg/m2(11.7; 95% CI: 10.9 – 12.6%). 340340. Lotufo PA, Santos RD, Figueiredo RM, Pereira AC, Mill JG, Alvim SM, Fonseca MJ, Almeida MC, Molina MC, Chor D, Schmidt MI, Ribeiro ALP, Duncan BB, Bensenor IM. Prevalence, Awareness, Treatment, and Control of High Low-Density Lipoprotein Cholesterol in Brazil: Baseline of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Clin Lipidol. 2016;10(3):568-76. doi: 10.1016/j.jacl.2015.12.029.
• In a cross-sectional population-based study (VIGITEL, 2014), Moreira et al . have assessed the sociodemographic, behavioral, and dietary characteristics of 867 adults aged > 45 years in the city of João Pessoa, Paraíba state, and their associations with the presence of systemic arterial hypertension and diabetes. In an adjusted analysis, the prevalence of diabetes was higher among women with lower educational level (0-4 years of schooling, PR 3.3; 95% CI: 1.4 – 7.5) and no regular consumption of beans (PR 1.6; 95% CI: 1.0 – 2.8). Among men, the age ranges of 55-64 years (PR 5.1; 95% CI: 1.9 – 13.4) and ≥ 65 years (PR 4.0; 95% CI: 1.4 – 10.9) and being married (PR 17.7; 95% CI: 2.0 – 153.0) were associated with a higher prevalence of diabetes. 297297. Moreira APL, Malta DC, Vianna RP de T, Moreira PVL, Carvalho AT de. Risk and protection factors for self-reported hypertension and diabetes in João Pessoa, Brazil. The VIGITEL survey, 2014. A cross-sectional study. Sao Paulo Med J. 2017;135(5):450-461. doi:10.1590/1516-3180.2017.0044250517.
• In a cross-sectional population-based study conducted from 2006 to 2016 (VIGITEL, 2014), 297297. Moreira APL, Malta DC, Vianna RP de T, Moreira PVL, Carvalho AT de. Risk and protection factors for self-reported hypertension and diabetes in João Pessoa, Brazil. The VIGITEL survey, 2014. A cross-sectional study. Sao Paulo Med J. 2017;135(5):450-461. doi:10.1590/1516-3180.2017.0044250517. Oliveira et al . assessed the sociodemographic, behavioral, and dietary characteristics of 572 437 adults aged >18 years from the Brazilian capitals and Distrito Federal and their association with self-reported diabetes. Individuals with diabetes had fewer risky and more protective behaviors as follows: higher intake of fruits and vegetables [34.0% (95% CI: 33.8 – 34.3) in controls and 40.7% (95% CI: 39.7 – 41.8) in individuals with diabetes, adjusted PR 1.05]; lower consumption of meat with excess fat [24.3% (95% CI: 23.3 – 25.2) vs. 32.3% (95% CI: 31.9 – 32.5), adjusted PR 0.95], of whole milk [44.5% (95% CI: 43.5 – 45.5) vs. 55.4% (95% CI: 55.1 – 55.7%), adjusted PR 0.87] and of soft drinks and sugar-sweetened beverages [9.5% (95% CI: 8.5 – 10.5) vs. 25% (95% CI: 24.6 – 25.4), adjusted PR 0.57]. Individuals with diabetes reported lower consumption of alcoholic beverages [15.9% (95% CI: 14.7 – 17.1) vs. 26.8% (95% CI: 26.4 – 27.2), adjusted PR 0.86] and less leisure-time physical activity [24.0% (95% CI: 23.1 – 25.0) vs. 34.6% (95% CI: 34.3 – 34.9), adjusted PR 0.92] than individuals without diabetes. 341341. Oliveira AP, Maia EG, Silva FM, Martins APB, Claro RM. Needed Improvements in Diabetes Prevention and Management in Brazil. Prev Chronic Dis. 2018;15:E153. doi: 10.5888/pcd15.180269.
• In a cross-sectional analysis of the ELSA-Brazil Study, an adjusted model has shown an inverse association of diabetes and the intake of at least four servings per day of dairy products [0.76 (95% CI: 0.59 – 0.97)] in 10 010 adults. 342342. Drehmer M, Pereira MA, Schmidt MI, Molina MDCB, Alvim S, Lotufo PA, Duncan BB. Associations of Dairy Intake With Glycemia and Insulinemia, Independent of Obesity, in Brazilian Adults: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Am J Clin Nutr. 2015;101(4):775-82. doi: 10.3945/ajcn.114.102152.
• Considering leisure-time physical activity, the ELSA-Brazil Study has shown a lower chance of diabetes in active men and women as compared to inactive ones: 0.73 (95% CI: 0.61 – 0.87) and 0.83 (95% CI: 0.67 – 1.03), respectively. 343343. Lin X, Alvim SM, Simoes EJ, Bensenor IM, Barreto SM, Schmidt MI, Ribeiro ALP, Pitanga F, Almeida MC, Liu S, Lotufo PA. Leisure Time Physical Activity and Cardio-Metabolic Health: Results From the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Am Heart Assoc. 2016;5(6):e003337. doi: 10.1161/JAHA.116.003337.
• Werneck et al ., in 2018, based on data from the PNS-2013, have assessed the self-reported levels and patterns of television watching of 60 202 Brazilian adults and their association with type 2 diabetes. Television watching for more than 4 hours per day increased the likelihood of developing diabetes for men (1.64; 95% CI: 1.23 – 2.17) and women (1.33; 95% CI: 1.09 – 1.63) as compared to those watching television less than 2 hours per day. 344344. Werneck AO, Cyrino ES, Collings PJ, Ronque ERV, Szwarcwald CL, Sardinha LB, Silva DR. TV Viewing in 60,202 Adults From the National Brazilian Health Survey: Prevalence, Correlates, and Associations With Chronic Diseases. J Phys Act Health. 2018;15(7):510-5. doi: 10.1123/jpah.2017-0317.
• Teló et al ., in a cross-sectional study with 37 854 adolescents, have shown a higher likelihood of type 2 diabetes in those with obesity (OR 1.59; 95% CI: 1.20 – 2.11) and increased waist circumference (OR 1.51; 95% CI: 1.13 – 2.01), with no association with physical inactivity (< 60 min/day). 314314. Telo GH, Cureau F V, Szklo M, Bloch K V, Schaan BD. Prevalence of type 2 diabetes among adolescents in Brazil: Findings From Study of Cardiovascular Risk in Adolescents (ERICA). Pediatr Diabetes. 2019;20(4):389-396. doi:10.1111/pedi.12828.
Future Research
• The evidence is still insufficient whether diabetes prevention through lifestyle changes would also prevent cardiovascular and microvascular complications of the disease.
• Studies on the incidence of type 1 and type 2 diabetes with national representativity, aimed at social and behavioral determinants are required.
• Considering the SUS coverage and the possibility of reaching many patients with type 1 and type 2 diabetes, studies focused on assessing the efficacy and effectiveness of the care provided to these patients in Brazil are required.
• Considering the several publications on the increase of the overweight and obesity incidence in the Brazilian population in all age ranges, mostly in the lower socioeconomic levels, efficient public policies to prevent obesity should be prioritized to reduce new cases of diabetes and its complications. Some exemples are: 1. Taxation of high caloric foods; 2. Mandatory labeling of food products; 3. Creation of programs to prevent and treat obesity in communities, rescuing individuals predisposed to diabetes by using simple tools (questionnaires); 4. Training of multiprofessional teams to engage in lifestyle change programs to prevent and treat diabetes; 5. Integration of physical education professionals into those programs.
9. DYSLIPIDEMIA
CID-10 E78 (E78.0 – E78.9); CID-10-CM E78 (E78.0 – E78.9)
See Tables 9-1 through 9-8 and Charts 9-1 through 9-5
| AMI | Acute Myocardial Infarction |
| CI | Confidence Interval |
| CVD | Cardiovascular Diseases |
| DALYs | Disability-Adjusted Life Years |
| ELSA-Brasil | The Brazilian Longitudinal Study of Adult Health |
| ERICA | Brazilian Study of Cardiovascular Risk in Adolescents (in Portuguese, Estudo dos Riscos Cardiovasculares em Adolescentes ) |
| FU | Federative Unit |
| GBD 2019 | Global Burden of Disease 2019 |
| HDLc | High-Density-Lipoprotein Cholesterol |
| LDLc | Low-Density-Lipoprotein Cholesterol |
| OR | Odds Ratio |
| PNAUM | Study on the Access to, Use, and Promotion of Rational Use of Medicines in Brazil (in Portuguese, Pesquisa Nacional sobre Acesso, Utilização e Promoção do Uso Racional de Medicamentos no Brasil ) |
| PNS | National Health Survey (in Portuguese, Pesquisa Nacional de Saúde ) |
| SDI | Sociodemographic Index |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| TC | Total Cholesterol |
| TG | Triglycerides |
| UI | Uncertainty Interval |
| YLDs | Years Lived with Disability |
| YLLs | Years of Life Lost |
– Mean plasma lipid levels, prevalence of borderline and high levels, and estimated population with abnormal levels, by sex and age group. ERICA-Brasil, 2013-2014.
– Prevalence of total cholesterol ≥ 200 mg/dL according to sex, age group, educational level, skin color, and country region. Brazil, PNS 2014-2015.
– Prevalence of low HDL-cholesterol (< 40 mg/dL) according to sex, age group, educational level, skin color, and Brazilian region, PNS 2014-2015.
– Prevalence of high LDL-cholesterol (> 130 mg/dL) according to sex, age group, educational level, skin color, and Brazilian region, PNS 2014-2015.
– Numbers of deaths and age-standardized mortality rates attributable to high LDL-cholesterol levels in 1990 and 2019, and percent change of rates, in Brazil and Federative Units.
– Mortality rate (age-standardized) attributable to high LDL-cholesterol levels in 1990 and 2019, and percent change of rates, stratified by sex, in Brazil and its Federative Units.
– Numbers and rates of deaths, DALYs, YLLs, YLDs attributable to high LDL-cholesterol levels in 1990 and 2019, and percentage change of rates, by age group, in Brazil.
– Change in age-standardized mortality rates due to ischemic heart disease and stroke attributable to high LDL-cholesterol levels between 1990 and 2019.
– Correlation between the percent change in age-standardized mortality rate from 1990 to 2019 and the 2019 Sociodemographic Index of each federative unit.
– Proportional mortality attributable to high LDL-cholesterol levels by age group, Brazil, 2019.
– Numbers of deaths and YLLs and age-standardized rates of mortality and YLLs attributable to high LDL-cholesterol levels between 1990 and 2019.
– Numbers and age-standardized rates of DALYs and YLDs attributable to high LDL-cholesterol levels between 1990 and 2019.
Introduction
• Dyslipidemia is defined as abnormal serum lipid levels, including cholesterol, its subfractions and/or TG. Dyslipidemia is a well-defined risk factor for CVD, in which its causal role has been unequivocally established. 346346. Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, Daemen MJ, Demer LL, Hegele RA, Nicholls SJ, Nordestgaard BG, Watts GF, Bruckert E, Fazio S, Ference BA, Graham I, Horton JD, Landmesser U, Laufs U, Masana L, Pasterkamp G, Raal FJ, Ray KK, Schunkert H, Taskinen MR, van de Sluis B, Wiklund O, Tokgozoglu L, Catapano AL, Ginsberg HN. Low-Density Lipoproteins Cause Atherosclerotic Cardiovascular Disease: Pathophysiological, Genetic, and Therapeutic Insights: A Consensus Statement From the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2020;41(24):2313-30. doi: 10.1093/eurheartj/ehz962. Its treatment, even in primary prevention, has been shown to effectively reduce CVD. 347347. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):596-646. doi: 10.1161/CIR.0000000000000678. Data on mean cholesterol levels and prevalence of dyslipidemia were obtained for adults primarily from the PNS 2015 and for adolescents from the ERICA Study. Smaller prevalence studies (regionally based) were also used when appropriate.
• Throughout this chapter we will usually describe data on TC, LDLc, HDLc, and TG when available. Definitions of dyslipidemia vary historically and according to the positions of local cardiology societies. In this chapter, for the purpose of classification and unless stated otherwise, we will use the term dyslipidemia as follows: for adults, TC ≥ 200 mg/dL, LDLc ≥ 130 mg/dL, HDLc < 40 mg/dL, and TG ≥ 150 mg/dL; 348348. Malta DC, Szwarcwald CL, Machado ÍE, Pereira CA, Figueiredo AW, Sá ACMGN, Velasquez-Melendez G, Santos FMD, Souza PB Jr, Stopa SR, Rosenfeld LG. Prevalence of Altered total Cholesterol and Fractions in the Brazilian Adult Population: National Health Survey. Rev Bras Epidemiol. 2019;22(Suppl 2):E190005.SUPL.2. doi: 10.1590/1980-549720190005.
https://doi.org/10.1590/1980-54972019000...
and for children and adolescents, TC ≥ 170 mg/dL, LDLc ≥ 130 mg/dL, HDLc < 45 mg/dL, and TG ≥ 130 mg/dL. 349349. Faria Neto JR, Bento VF, Baena CP, Olandoski M, Gonçalves LG, Abreu Gde A, Kuschnir MC, Bloch KV. ERICA: Prevalence of Dyslipidemia in Brazilian Adolescents. Rev Saude Publica. 2016;50(Suppl 1):10s. doi: 10.1590/S01518-8787.2016050006723.
Prevalence
Youth
• In the nationwide ERICA Study, Faria Neto et al . 349349. Faria Neto JR, Bento VF, Baena CP, Olandoski M, Gonçalves LG, Abreu Gde A, Kuschnir MC, Bloch KV. ERICA: Prevalence of Dyslipidemia in Brazilian Adolescents. Rev Saude Publica. 2016;50(Suppl 1):10s. doi: 10.1590/S01518-8787.2016050006723. evaluated 38 069 schoolchildren (60% girls) aged 12 to 17 years from the capitals of the 27 Brazilian FUs, in addition to five sets of municipalities with more than 100 000 inhabitants, in all five Brazilian geographic regions. 349349. Faria Neto JR, Bento VF, Baena CP, Olandoski M, Gonçalves LG, Abreu Gde A, Kuschnir MC, Bloch KV. ERICA: Prevalence of Dyslipidemia in Brazilian Adolescents. Rev Saude Publica. 2016;50(Suppl 1):10s. doi: 10.1590/S01518-8787.2016050006723. Mean TC was 148 mg/dL (95% CI, 147-149 mg/dL), LDLc 85 mg/dL (95% CI, 84-86 mg/dL), HDLc 47 mg/dL (95% CI, 47-48 mg/dL) and TG 78 mg/dL (95% CI, 76-79 mg/dL). Regarding the prevalence of abnormal values, 20.1% (95% CI, 19-21.3%) showed an increase in TC, 3.5% (95% CI, 3.2-4%) in LDLc, and 7.8% (95% CI, 7.1-8.6%) in TG. The prevalence of low HDLc was 47% (95% CI, 45-49%). Such data stratified by age and sex can be seen in Table 9-1 .
• For children aged 6 to 12 years, there data is scanty. In a study conducted in Santa Catarina with 1011 students aged 6 to 14 years (52.4% girls), the following mean levels were reported: TC, 172 (± 27) mg/dL in girls, 170 (± 28) mg/dL in boys; LDLc, 104 (± 24) mg/dL in girls, 104 (± 27) mg/dL in boys; HDLc, 49 (± 11) mg/dL in girls, 49 (± 11) mg/dL in boys; and TG, 80 (24-459) mg/dL in girls, 77 (14-752) mg/dL in boys. 350350. Rosini N, Machado MJ, Webster IZ, Moura SA, Cavalcante LS, Silva EL. Simultaneous Prediction of Hyperglycemia and Dyslipidemia in School Children in Santa Catarina State, Brazil Based on Waist Circumference Measurement. Clin Biochem. 2013;46(18):1837-41. doi: 10.1016/j.clinbiochem.2013.08.015.
• A study conducted in the city of Vitória with 511 children (age, 6 to 9 years; 46.77% boys) found high TC in 32.7% of them, high LDLc in 9.2%, low HDLc in 27%, and elevated TG levels in 4.1%. 351351. Almeida PCD, Silva JP, Pinasco GC, Hegner CC, Mattos DC, Potratz MO, Bravin LS, Silva VR, Lamounier JA. Lipid Profile in Schoolchildren in Vitória – Brazil. J Hum Growth Dev. 2016;26(1):61-6. doi: doi.org/10.7322/jhgd.110989. In the city of Salvador, of 1131 children evaluated (age, 7 to 15 years; 50.1% boys), 25.5% (95% CI, 22.7 – 28.3) were found to be dyslipidemic (TC ≥ 170 mg/dL and/or TG ≥ 130 mg/dL). Dyslipidemia was associated with excess body weight (OR: 3.40; 95% CI, 2.07-5.58) and moderate to high consumption of high-risk food (OR: 1.49; 95% CI, 1.01-2.19). 352352. Alcântara Neto OD, Silva RC, Assis AM, Pinto Ede J. Factors Associated With Dyslipidemia in Children and Adolescents Enrolled in Public Schools of Salvador, Bahia. Rev Bras Epidemiol. 2012;15(2):335-45. doi: 10.1590/s1415-790x2012000200011.
Adults
• According to a study by Malta et al . 348348. Malta DC, Szwarcwald CL, Machado ÍE, Pereira CA, Figueiredo AW, Sá ACMGN, Velasquez-Melendez G, Santos FMD, Souza PB Jr, Stopa SR, Rosenfeld LG. Prevalence of Altered total Cholesterol and Fractions in the Brazilian Adult Population: National Health Survey. Rev Bras Epidemiol. 2019;22(Suppl 2):E190005.SUPL.2. doi: 10.1590/1980-549720190005.
https://doi.org/10.1590/1980-54972019000...
using data from the PNS 2014-2015, in the Brazilian adult population, the prevalence of high TC was 32.7%, of high LDLc, 18.6%, and of low HDLc, 31.8%. In that study, the mean levels were as follows: TC, 185 mg/dL; LDLc, 105 mg/dL; and HDLc, 46 mg/dL. While the prevalence of high TC was higher in women, the prevalence of low HDLc was higher in men. Detailed information on the prevalence of elevated TC and LDLc and of low HDLc stratified by sex, for different age groups, educational attainment, skin color and country region are presented in Tables 9-2 to 9-4. In general, higher levels of education were related to lower prevalence of high TC and LDLc and of low HDLc. Older age groups had higher prevalence of elevated TC and LDLc. Residing in the Southern and Southeastern regions of Brazil were related to lower prevalence of low HDLc. An association between self-reported skin color and lipid profile was less clear, but black women had a lower prevalence of low HDLc. 348348. Malta DC, Szwarcwald CL, Machado ÍE, Pereira CA, Figueiredo AW, Sá ACMGN, Velasquez-Melendez G, Santos FMD, Souza PB Jr, Stopa SR, Rosenfeld LG. Prevalence of Altered total Cholesterol and Fractions in the Brazilian Adult Population: National Health Survey. Rev Bras Epidemiol. 2019;22(Suppl 2):E190005.SUPL.2. doi: 10.1590/1980-549720190005.
https://doi.org/10.1590/1980-54972019000...
Other factors associated with lipid profile changes that have been reported in the Brazilian population include physical activity 353353. Silva RC, Diniz MF, Alvim S, Vidigal PG, Fedeli LM, Barreto SM. Physical Activity and Lipid Profile in the ELSA- Brasil Study. Arq Bras Cardiol. 2016;107(1):10-9. doi: 10.5935/abc.20160091. and seasonal variations. 354354. Moura FA, Dutra-Rodrigues MS, Cassol AS, Parra ES, Zago VH, Panzoldo NB, Alexandre F, Vieira IC, Vendrame F, Virginio VW, Castanho VS, Danelon MR, Nunes VS, Leança CC, Saraiva FK, Coelho OR, Nakandakare E, Quintão EC, de Faria EC, Sposito AC. Impact of Seasonality on the Prevalence of Dyslipidemia: A Large Population Study. Chronobiol Int. 2013;30(8):1011-5. doi: 10.3109/07420528.2013.793698.
• The ELSA-Brasil study found the following percentages in women and men, respectively: high LDLc, 57.6% and 58.8%; low HDLc, 20.7% and 14.7%; and hypertriglyceridemia, 23.2% and 40.7%. In addition, the ELSA-Brasil study reported small differences, whose clinical impact seem to be limited, in the lipid profile according to skin color. 355355. Santos RD, Bensenor IM, Pereira AC, Lotufo PA. Dyslipidemia According to Gender and Race: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Clin Lipidol. 2016;10(6):1362-8. doi: 10.1016/j.jacl.2016.08.008.
• In 2003, Martinez et al . reported on the evaluation of 81 262 individuals (51% male; 44.7 ± 15.7 years) from 13 large Brazilian cities. 356356. Martinez TL, Santos RD, Armaganijan D, Torres KP, Loures-Vale A, Magalhães ME, Lima JC, Moriguchi E, Amodeo C, Ortiz J. National Alert Campaign About Increased Cholesterol: Determination of Cholesterol Levels in 81,262 Brazilians. Arq Bras Cardiol. 2003;80(6):635-8, 631-4. doi: 10.1590/s0066-782x2003000600006. Mean TC was 199.0 ± 35.0 mg/dL and 13% of the sample had a TC above 240 mg/dL.
Attributable Risk
Mortality
• The absolute number of deaths and mortality rates countrywide and by FU (including percent change) can be seen in Table 9-5. According to the GBD Study 2019 estimates, between 1990 and 2019, the cardiovascular mortality attributable to high levels of LDLc in Brazil increased in absolute numbers, from 68 327 (95% CI, 55 097 - 83 768) to 99 375 (95% CI, 78 039 - 126 143), but had a 51.3% reduction in the age-standardized rate [88.6 (95% CI, 67.8 - 114.8) to 43.1 (95% CI, 33.4 - 55.9) per 100,000], as a result of population aging. Of the states, Minas Gerais had the highest reduction in mortality rate (-63%) and Ceará, the lowest (-15%).
• Table 9-6 describes the mortality rates attributable to elevated LDLc stratified by sex. For women, the rate went from 72.9 (54.2-97.8) in 1990 to 33.8 (25-45.1) in 2019, a reduction of 53.7% (-56.9 to -50.4) at national level. The greatest reduction was observed in the state of Rondônia (-66.1%) and the smallest, in the state of Maranhão (-1%). For men, the overall percent change was -48.8% (-52.1 to -44.9), from 105.7 (82.4-133.6) in 1990 to 54.2 (42.3-68.4) in 2019, and Distrito Federal had the greatest reduction (-61.9%) and Ceará, the lowest (-10.1%).
• The specific causes of death attributable to high LDLc followed the same trend. Mortality from ischemic heart disease went from 57 020 (95% CI, 46 252 - 68 541) to 83 759 (95% CI, 65 742 - 101 543) and cerebrovascular from 11 306 (95% CI, 5 270 - 21 619) to 15 615 (95% CI, 5 522 - 32 805) with a reduction in the age-standardized mortality rate for both. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
The change in the age-standardized mortality rate due to ischemic heart disease and stroke attributable to high LDLc, from 1990 to 2019, is represented in Chart 9-1.
• The SDI is a composite index that measures per capita income, fertility, education, and sociodemographic development. The SDI allows the comparison of states and countries according to their development. The reduction in age-standardized mortality rate was greater in the FUs with higher SDI (Distrito Federal, São Paulo, Santa Catarina, Rio de Janeiro), and smaller in those with lower SDI, such as the FUs in the Northeastern region (Chart 9-2).
• Absolute numbers of deaths and mortality rates by age group are demonstrated in Table 9-7. There was a reduction in the mortality rate for all age groups. The age group of 50-69 years experienced the highest reduction in the mortality rate (-48.5%). Chart 9-3 depicts the proportion of mortality by age group attributable to high LDLc. This risk factor seems to have greater impact on those aged 40 to 64 years.
Years of Life Lost
• The same phenomenon observed for mortality rates can be evidenced for the metric of YLLs, which varied in absolute numbers from 1 759 130 (95% CI, 1 501 507 – 2 056 575) to 2 230 747 (95% CI, 1 880 847 – 2 617 317). The age-standardized rate varied from 1874.3 (95% CI, 1561 - 2235) to 926 (95% CI, 773-1094). 1212. França E, Abreu DX, Rao C, Lopez AD. Evaluation of Cause-of-Death Statistics for Brazil, 2002-2004. Int J Epidemiol. 2008;37(4):891-901. doi: 10.1093/ije/dyn121. The increase in the number of deaths and YLLs attributable to LDLc and the reduction in the age-standardized rates of both between 1990 and 2019 are shown in Chart 9-4. The absence of a reduction in the mortality rate, when removing the age-standardization, is explained by population aging.
Burden of Disease
• In addition to the fatal complications of CVD attributable to dyslipidemia, non-fatal complications, such as non-fatal AMI and non-fatal stroke, can be partially attributed to dyslipidemia. The impact of these conditions can be measured by YLDs and DALYs, the latter being the sum of YLLs and YLDs. Between 1990 and 2019, the absolute number of YLDs increased from 62 670 (95% CI, 41 368 - 87 015) to 132 393 (95% CI, 87 121 - 184 089), with rate (per 100,000) ranging from 65.7 (95% CI, 42.2-92.3) to 55.4 (36.3-77.7), a negative variation of 15.8% (Table 9-7). 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
• Regarding DALYs, following the same trend of that of mortality, there was an increase in the absolute numbers of DALYs, from 1 821 799 (95% CI, 1 548 456 - 2 139 063) to 2 363 141 (95% CI, 1 985 655 - 2 781 318). This increase was accompanied by a reduction in its age-standardized rate [1940.1 (95% CI, 1614.4 - 2322.9) to 981.3 (95% CI, 817.1 - 1162.4)], a percent change of -49.4%. These changes are illustrated in Chart 9-5.
• Table 9-8 shows the age-standardized DALY rates attributable to high LDLc levels in 1990 and 2019, and the percent change in the period, stratified by sex, in Brazil and FUs. In women, the national rate went from 1425.8 (1165.2 - 1745.1) in 1990 to 692.2 (567-842.5) in 2019, a percent change of -51.5% (-54.8 to -47.9). The greatest change was seen in Distrito Federal, -64.2% (-70.5 to -57.9), and the smallest, in the state of Maranhão, -8.9% (-30.8 to -26.9). For men, the rate of DALYs went from 2496 (2090.2 - 2980.2) to 1310.6 (1097.4 - 1543), with a change of -47.5% (-50.9 to -43.8) in Brazil. The FU with the greatest improvement was the Distrito Federal, -61.9% (-67.4 to -54.6), while the state of Ceará showed the smallest percent change, -10.1% (-32.7 to -23).
• Table 9-7 shows the numbers and rates of deaths, DALYs, YLLs, YLDs attributable to high LDLc in 1990 and 2019, with their respective percent changes, by age group.
Familial Dyslipidemia
• The prevalence of familial dyslipidemia diagnosed by the Dutch Lipid Clinic Network (DLCN) criteria was assessed in the ELSA-Brasil study, with a documented prevalence of 1 in 263 individuals. This condition was more prevalent in blacks (1 in 156) and brown races (mixed ethnicity; 1 in 204) than in white people (1 in 417). 357357. Harada PH, Miname MH, Benseñor IM, Santos RD, Lotufo PA. Familial Hypercholesterolemia Prevalence in an Admixed Racial Society: Sex and Race Matter. The ELSA-Brasil. Atherosclerosis. 2018;277:273-7. doi: 10.1016/j.atherosclerosis.2018.08.021.
• Despite controversies on the use of cascade screening to identify relatives of individuals with familial dyslipidemia, a Brazilian study demonstrated that 59% of the relatives of individuals with mutations were also carriers of such mutations, suggesting a high prevalence of familial dyslipidemia in this selected subgroup. 358358. Jannes CE, Santos RD, Silva PRS, Turolla L, Gagliardi AC, Marsiglia JD, Chacra AP, Miname MH, Rocha VZ, Salgado Filho W, Krieger JE, Pereira AC. Familial Hypercholesterolemia in Brazil: Cascade Screening Program, Clinical and Genetic Aspects. Atherosclerosis. 2015;238(1):101-7. doi: 10.1016/j.atherosclerosis.2014.11.009.
Awareness and Statin Use in Brazil
• An analysis conducted in the ELSA-Brasil study, including 15 096 adults aged 35-74 years, explored the prevalence of high LDLc (according to the NCEP-ATP-III criteria) and the proportion of participants aware of this diagnosis. 340340. Lotufo PA, Santos RD, Figueiredo RM, Pereira AC, Mill JG, Alvim SM, Fonseca MJ, Almeida MC, Molina MC, Chor D, Schmidt MI, Ribeiro ALP, Duncan BB, Bensenor IM. Prevalence, Awareness, Treatment, and Control of High Low-Density Lipoprotein Cholesterol in Brazil: Baseline of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Clin Lipidol. 2016;10(3):568-76. doi: 10.1016/j.jacl.2015.12.029. The frequency of participants with elevated LDLc was 45.5%, of which only 58.1% were aware of the diagnosis. Among those participants with elevated LDLc, 42.3% were using some lipid-lowering medications as treatment and 58.3% reached the target defined by the NCEP-ATP-III panel.
• In an analysis based on the PNAUM between 2014 and 2015, the use of statins in SUS primary care in the five Brazilian regions was assessed. 359359. Santos RD, Pereira C, Cesena F, Laurinavicius AG, Tabone V, Bittencourt MS. Cardiovascular Risk Misperception and Low Awareness of Familial Hypercholesterolemia in Individuals With Severe Hypercholesterolemia. Arq Bras Cardiol. 2021;116(4):706-12. doi: 10.36660/abc.20190516. Among the 8803 respondents, the prevalence of statin use was 9.3%, and 81.4% of these users reported having dyslipidemia. Simvastatin was the most widely used statin (90.3%), followed by atorvastatin (4.7%) and rosuvastatin (1.9%).
• Regarding familial dyslipidemia awareness and treatment, Santos et al . reported results from a database of 70 000 individuals undergoing a mandatory employer-sponsored routine health evaluation in a private hospital in São Paulo. 359359. Santos RD, Pereira C, Cesena F, Laurinavicius AG, Tabone V, Bittencourt MS. Cardiovascular Risk Misperception and Low Awareness of Familial Hypercholesterolemia in Individuals With Severe Hypercholesterolemia. Arq Bras Cardiol. 2021;116(4):706-12. doi: 10.36660/abc.20190516. Among 70 000 patients, 1987 met the established criteria for familial dyslipidemia (LDLc ≥ 190 mg/dL or LDLc ≥ 160 mg/dL on statin). A sample of 200 was selected to complete a questionnaire. From the 200 patients, familial dyslipidemia was suspected by the attending physician in only 29 (14.5%), although most of them (97%) were aware of their high blood cholesterol levels. Only 18% had the perception they were at high risk for CVD, only 30% were aware of their LDLc goals, and 37% were not on lipid-lowering medication.
Dyslipidemia and Subclinical Atherosclerosis
• Subclinical atherosclerosis, including markers like coronary artery calcium score and carotid intima-media thickness, has been used as surrogate for atherosclerosis and CVD. Thus, its association with abnormal lipid profiles can be of epidemiological interest.
• In a study of more than 3600 individuals, Generoso et al . demonstrated that HDLc was associated with coronary artery calcium even after adjustment for traditional cardiovascular risk factors in a Brazilian population. However, this association was no longer significant after adjustment for TG. 360360. Generoso G, Bensenor IM, Santos RD, Staniak HL, Sharovsky R, Santos IS, Goulart AC, Jones SR, Kulkarni KR, Blaha MJ, Toth PP, Lotufo PA, Bittencourt MS. High-density Lipoprotein-cholesterol Subfractions and Coronary Artery Calcium: The ELSA-Brasil Study. Arch Med Res. 2019;50(6):362-7. doi: 10.1016/j.arcmed.2019.10.006. In addition, that study evaluated HDLc subfractions and demonstrated they were not associated with coronary artery calcification once adjusted for total HDLc. Furthermore, the same group showed the association between HDLc and carotid intima-media thickness, and its modification by the presence of diabetes. 361361. Generoso G, Bensenor IM, Santos IS, Santos RD, Goulart AC, Jones SR, Kulkarni KR, Blaha MJ, Toth PP, Lotufo PA, Bittencourt MS. Diabetes Alters the Association Between High-Density Lipoprotein Subfractions and Carotid Intima-Media Thickness: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Diab Vasc Dis Res. 2018;15(6):541-7. doi: 10.1177/1479164118788080.
• Laurinavicius et al . studied the association between very high HDLc levels and carotid intima-media thickness. 362362. Laurinavicius AG, Santos IS, Santos RD, Bensenor IM, Conceição RD, Lotufo PA. Extremely Elevated HDL-Cholesterol Levels are not Associated With Increased Carotid Intima-Media Thickness: Data From ELSA Brasil. J Clin Lipidol. 2016;10(4):898-904.e1. doi: 10.1016/j.jacl.2016.03.007. Very high HDLc likely characterizes hyperalphalipoproteinemia, a dysfunctional HDLc condition. Despite prior evidence, their study did not demonstrate an association between such profile and carotid intima-media thickness. 362362. Laurinavicius AG, Santos IS, Santos RD, Bensenor IM, Conceição RD, Lotufo PA. Extremely Elevated HDL-Cholesterol Levels are not Associated With Increased Carotid Intima-Media Thickness: Data From ELSA Brasil. J Clin Lipidol. 2016;10(4):898-904.e1. doi: 10.1016/j.jacl.2016.03.007.
• In an analysis of TG-rich lipoproteins in the ELSA-Brasil study, Bittencourt et al . demonstrated that those particles are associated with coronary artery calcification even after adjusting for significant risk factors. 363363. Bittencourt MS, Santos RD, Staniak H, Sharovsky R, Kondapally R, Vallejo-Vaz AJ, Ray KK, Bensenor I, Lotufo P. Relation of Fasting Triglyceride-Rich Lipoprotein Cholesterol to Coronary Artery Calcium Score (From the ELSA-Brasil Study). Am J Cardiol. 2017;119(9):1352-8. doi: 10.1016/j.amjcard.2017.01.033.
• In a study of octogenarian Brazilians, the authors found that the association between LDLc and coronary artery calcification weakens with age, whereas the association of HDLc does not. 364364. Freitas WM, Quaglia LA, Santos SN, Paula RC, Santos RD, Blaha M, Rivera JJ, Cury R, Blumenthal R, Nadruz-Junior W, Agatston A, Figueiredo VN, Nasir K, Sposito AC; Brazilian Study on Healthy Aging. Low HDL Cholesterol but not High LDL Cholesterol is Independently Associated With Subclinical Coronary Atherosclerosis in Healthy Octogenarians. Aging Clin Exp Res. 2015;27(1):61-7. doi: 10.1007/s40520-014-0249-4..
• Collectively, those studies demonstrate a robust association of lipid profile with subclinical atherosclerosis, corroborating findings of the association between dyslipidemia and CVD.
Future Research
• Current data on the epidemiology of dyslipidemia in the contemporary Brazilian population is limited. Additional studies on its prevalence in the broad population as well as in specific high-risk groups, such as those with a lower socioeconomic status, are needed.
• The frequency of cholesterol screening in Brazil, according to sex and age groups, needs to be investigated.
• Local Brazilian data on dyslipidemia impact on the healthcare system, including costs, are yet to be addressed.
10. OBESITY AND OVERWEIGHT
ICD-10 E66
See Tables 10-1 through 10-14 and Charts 10-1 through 10-10
| BMI | Body Mass Index |
| BMI_i | Imputed Body Mass Index |
| CI | Confidence Interval |
| CVD | Cardiovascular Diseases |
| DALYs | Disability-Adjusted Life-Years |
| ELSA-Brasil | The Brazilian Longitudinal Study of Adult Health (in Portuguese , Estudo Longitudinal de Saúde do Adulto ) |
| ERICA | Brazilian Study of Cardiovascular Risk in Adolescents (in Portuguese, Estudo dos Riscos Cardiovasculares em Adolescentes ) |
| FU | Federative Unit |
| GBD | Global Burden of Disease |
| HR | Hazard Ratio |
| ICER | Incremental Cost-Effectiveness Ratio |
| NCD | Noncommunicable Chronic Diseases |
| OR | Odds Ratio |
| PNS | Brazilian National Health Survey (in Portuguese, Pesquisa Nacional de Saúde ) |
| PR | Prevalence Ratio |
| QALYs | Quality-Adjusted Life-Years |
| RR | Relative Risk |
| SABE | Health, Well-Being, and Aging survey (in Spanish, Salud, Bienestar y Envejecimiento ) |
| SDI | Sociodemographic Index |
| SUS | Brazilian Unified Health System (in Portuguese, Sistema Único de Saúde ) |
| UI | Uncertainty Interval |
| VIGITEL | Telephone Survey for Surveillance of Non-Communicable Chronic Diseases (in Portuguese, Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico ) |
| WHO | World Health Organization |
| YLDs | Years Lived with Disability |
| YLLs | Years of Life Lost |
– Prevalence of excess weight and obesity in the total population aged 18 years and over, by sex and age groups, in Brazil, in 2019.*
– Percentage of overweight adults, according to an imputation method (BMI_i ≥ 25 kg/m2), by sex, in the capitals of the Brazilian states and the Distrito Federal.*
– Percentage of obese adults, according to an imputation method (BMI_i ≥ 30 kg/m2), by sex, in the capitals of the Brazilian states and the Distrito Federal.*
– Number of deaths, age-standardized mortality rates due to all causes attributable to high BMI, per 100 000 inhabitants, in 1990 and 2019, and percent change of rates in the period, in Brazil and Federative Units.
– Age-standardized mortality rates due to all causes attributable to high BMI, per 100 000 inhabitants, by sex, in 1990 and 2019, and percent change of rates in the period, in Brazil and Federative Units.
– Number of deaths, crude and age-standardized mortality rates due to all causes attributable to high BMI, by age group, in Brazil in 1990 and 2019, and percent change of rates in the period.
– Number of deaths, age-standardized mortality rates due to cardiovascular diseases attributed to high BMI (per 100 000 inhabitants), in 1990 and 2019, and percent change of rates in the period, in Brazil and its Federative Units.
– Age-standardized mortality rates due to cardiovascular diseases attributed to high BMI (per 100 000 inhabitants), by sex, in 1990 and 2019, and percent change of rates in the period, in Brazil and its Federative Units.
– Number of deaths, crude and age-standardized mortality rates due to cardiovascular disease attributable to high BMI, by age group, in 1990 and 2019, and percent change of rates in the period, in Brazil.
– Number of DALYs and age-standardized rates of DALYs due to all causes attributable to high BMI (per 100 000 inhabitants), in 1990 and 2019, and percent change of rates in the period, in Brazil and Federative Units.
– Number of DALYs, crude and age-standardized rates of DALYs due to all causes attributable to high BMI in Brazil, in 1990 and 2019, by age group, and percent change of rates in the period.
– Number of DALYs and age-standardized rates of DALYs due to cardiovascular diseases attributed to high BMI (per 100 000 inhabitants), in 1990 and 2019, and percent change of rates in the period, in Brazil and Federative Units.
– Age-standardized rates of DALYs due to cardiovascular diseases attributed to high BMI (per 100 000 inhabitants), by sex, in 1990 and 2019, and percent change of rates in the period, in Brazil and Federative Units.
– Number of deaths due to all causes attributed to high BMI, all ages, from 1990 to 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Crude and age-standardized mortality rate due to all causes attributed to high BMI, per 100 000, in Brazil, from 1990 to 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Proportional mortality due to all causes attributed to high BMI, by age group and sex, in Brazil, 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Age-standardized mortality rates due to diseases attributed to high BMI, stratified by all causes in Brazil, 1990 and 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Age-standardized mortality rates due to specific causes attributed to high BMI, per 100 000 inhabitants, by sex (women to the left and men to the right), in the Brazilian Federative Units, in 2019. The colored bars represent the specific causes of death according to the legend. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Correlation between the Sociodemographic Index (SDI) 2019 and the percent change of the age-standardized rates of mortality from cardiovascular disease attributed to high BMI, 1990 - 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Absolute number of YLLs (A), YLDs (B), and DALYs (C) due to high BMI, all ages, both sexes, Brazil, from 1990 to 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Rates of YLLs (A), YLDs (B), and DALYs (C) attributed to high BMI for all ages and age-standardized, per 100 000, both sexes, Brazil, from 1990 to 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Age-standardized rates of DALYs due to specific causes attributed to high BMI, per 100 000 inhabitants, by sex (women to the left and men to the right), in the Brazilian Federative Units, in 2019. The colored bars represent the specific causes of death according to the legend. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
– Age-standardized rates of DALYs due to cardiovascular diseases attributed to high BMI, in Brazil, 1990 and 2019. Data from the Global Burden of Disease (GBD) 2019 Study. 4646. Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
http://ghdx.healt...
Overview
• According to the WHO, obesity is defined as abnormal or excessive fat accumulation that presents a risk to health, being present when the BMI is equal to or greater than 30 kg/m2. Obesity is a multifactorial condition, related not only to the imbalance between calorie intake and expenditure, which results from a diet rich in high-sugar and high-fat foods, but also to genetic, metabolic, environmental, economic, and sociocultural factors, which eventually lead to the accumulation of excess body fat. In addition to being included in the NCD group, obesity is considered an important risk factor for conditions such as diabetes mellitus, hypertension, and CVD. Obesity is currently considered a pandemic, with impact on both developed and developing countries and consequences for the individual, social, familial, and financial levels. Overweight, defined as BMI over 25 kg/m2, is also associated with the complications observed in obese individuals, which increase in parallel with BMI increase. 365365. World Health Organization. Obesity [Internet]. Geneva: World Health Organization; 2020. [cited 2021 Nov 09]. Available From: https://www.who.int/health-topics/obesity.
https://www.who.int/health-topics/obesit...
Despite the limitations of the use of BMI to assess excess weight, such as its inability to define the amount of body fat that contributes to body weight, 366366. Nuttall FQ. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today. 2015;50(3):117-28. doi: 10.1097/NT.0000000000000092. the WHO currently uses that variable for its definitions.
• The deaths and disease burden attributed to obesity increased globally between 1990 and 2019: from 2.20 (95% UI, 1.21 – 3.43) to 5.02 (95% UI, 3.22 – 7.11) million deaths, and from 67.3 (95% UI, 38 - 104) to 160 (95% UI, 106 - 219) million DALYs in absolute numbers. Obesity contributed to more YLLs [119 million (79.6 - 164)] than YLDs [40.9 million (24.5 - 60.9)] worldwide in 2019. Most of that increase might have resulted from population growth and aging, evidenced after age standardization (4,9% {7,3-24,6} deaths, 18% {2,2- 42,3} DALYs, and 8,3% [-6,6–31,2] YLLs). 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010.
• Obesity contributes to compound most cardiovascular risk factors, particularly to increase blood pressure, blood glucose, and serum lipid levels, and has adverse effects due to serum inflammation and changes in heart structure and function. This association manifests in the relationship existing between obesity and the increased prevalence of hypertension, coronary artery disease, heart failure, and atrial fibrillation. Thus, although there is no clear consensus whether obesity is a disease or a risk factor, this chapter approaches obesity as a cardiovascular risk factor. 367367. Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy Weight and Obesity Prevention: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72(13):1506-31. doi: 10.1016/j.jacc.2018.08.1037.
• It is worth noting that, for the purpose of age-standardization of the rates, we considered the global population used by the GBD Study.
Prevalence
• Table 10-1 shows the prevalence of excess weight and obesity among individuals aged 18 years and over, by sex and age group, in Brazil, in 2019, according to anthropometric data from the PNS. In Brazil, the percentages of adults (age ≥18 years) with excess weight and obesity in 2019 were, respectively, 57.5% (95% CI, 54.8 – 60.2) and 21.8 % (95% CI, 19.2 – 24.7) for men, and 62.6% (95% CI, 59.1 – 66.0) and 29.5% (95% CI, 25.4 – 34.0) for women. Progressive increase of excess weight was observed with age increase, ranging from 33.7% (95% CI, 27.4 – 40.6) [male: 25.7% (95% CI, 19.1 – 33.7); female: 41.7% (95% CI, 31.1 – 53.1)] in the age group of 18-24 years to 70.3% (95% CI, 67.4 – 73.1) [male: 67.1% (95% CI, 62.1 – 71.8); female: 73.1% (95% CI, 68.8 -77.0)] in the age group of 40-59 years. For the age group of 60+ years, there was a slight reduction in the excess weight prevalence, 64.4% (95% CI, 60.5 – 68.1) [male: 63.3% (95% CI, 56.9 – 69.2); female: 65.3% (95% CI, 60.3 – 69.7)]. The same occurred with obesity, a progressive increase with age increase, ranging from 10.7% (95% CI, 7.7 – 14.7) [male: 7.9% (95% CI, 4.8 – 12.8); female: 13.5% (95% CI, 8.8 – 20.4)] in the age group of 18-24 years to 34.4% (95% CI, 29.7 – 39.4) [male: 30.2% (95% CI, 24.8 – 36.3); female: 38.0% (95% CI, 32.3 - 44.0)] in the age group of 40-59 years. For the age group of 60+ years, there was a slight reduction in obesity prevalence, 24.8% (95% CI, 20.9 – 29.1) [male: 21.2% (95% CI, 15.6 – 28.1); female: 27.5% (95% CI, 23.0 -32.5)]. It is worth noting the higher prevalence of excess weight and obesity in the female sex for all age groups.
• Table 10-2 shows the percentage of overweight adults, according to a method of imputation (BMI_i ≥ 25 kg/m2), by sex, in the Brazilian capitals and the Distrito Federal, according to Vigitel 2019 data. The capitals Campo Grande, Cuiabá, Fortaleza, Manaus, Natal, Porto Alegre, Porto Velho, Recife, Rio Branco, Rio de Janeiro, and São Paulo showed percentages higher than the national values for both sexes. For men, the capitals Boa Vista, Campo Grande, Cuiabá, Curitiba, Florianópolis, Fortaleza, Goiana, Manaus, Natal, Porto Alegre, Recife, and Rio Branco showed percentages higher than the national values. It is worth noting that, for female excess weight, the number of capitals above the national mean was smaller: Manaus, Natal, Recife, Rio Branco, Rio de Janeiro, Salvador, São Paulo, and Distrito Federal.
• Table 10-3 shows the percentages of adults with obesity, according to a method of imputation (BMI_i ≥ 30 kg/m2), by sex, in the Brazilian capitals and the Distrito Federal, according to Vigitel 2019 data. The capitals Aracajú, Boa Vista, Campo Grande, Cuiabá, Macapá, Manaus, Natal, Porto Alegre, Recife, Rio de Branco, and Rio de Janeiro showed percentages higher than the national values for both sexes. For men, the capitals Belém, Belo Horizonte, Boa Vista, Campo Grande, Cuiabá, Curitiba, Goiânia, Macapá, Manaus, Natal, Porto Alegre, Porto Velho, Recife, Rio Branco, and Rio de Janeiro showed percentages higher than the national values. Women had higher percentages of obesity compared to men, contrary to that observed for excess weight. The capitals with female obesity percentage above the national mean were Aracajú, Campo Grande, Cuiabá, João Pessoa, Macapá, Maceió, Manaus, Porto Alegre, Porto Velho, Recife, Rio Branco, Rio de Janeiro, and São Paulo.
• Felisbino-Mendes et al ., using data from the GBD study 2017, have reported that the age-standardized prevalence of obesity in Brazil was higher in the female sex (29.8%) compared to that in the male sex (24.6%) in 2017. However, men showed a higher increase of obesity (244.1%) compared to women (165.7%) from 1990 to 2017. An annual increase over 300% was observed in most states of the Northern and Northeastern regions for men, probably due to the delay in the epidemiological transition in those regions. More than half of the population had excess weight in most Brazilian states, except for Maranhão and Piauí. 368368. Felisbino-Mendes MS, Cousin E, Malta DC, Machado ÍE, Ribeiro ALP, Duncan BB, Schmidt MI, Silva DAS, Glenn S, Afshin A, Velasquez-Melendez G. The Burden of Non-Communicable Diseases Attributable to High BMI in Brazil, 1990-2017: Findings From the Global Burden of Disease Study. Popul Health Metr. 2020;18(Suppl 1):18. doi: 10.1186/s12963-020-00219-y. These findings are consistent with those indicating higher prevalence of obesity in more challenged populations that migrated from under-nutrition to over-nutrition, contributing to inadequate nutrition around the world. 369369. Peng W, Berry EM. Global Nutrition 1990-2015: A Shrinking Hungry, and Expanding Fat World. PLoS One. 2018;13(3):e0194821. doi: 10.1371/journal.pone.0194821.
• Flores-Ortiz et al ., assessing self-reported weight and height data of 572 437 adults of both sexes in the Brazilian capitals and the Distrito Federal, from 2006 to 2016, have estimated the overall prevalence of obesity, which increased from 11.7% to 18.1% in men, and from 12.1% to 18.8% in women, being more marked in the Northern, Northeastern, and West-Central regions. 370370. Flores-Ortiz R, Malta DC, Velasquez-Melendez G. Adult Body Weight Trends in 27 Urban Populations of Brazil From 2006 to 2016: A Population-Based Study. PLoS One. 2019;14(3):e0213254. doi: 10.1371/journal.pone.0213254.
• Araújo et al ., using Vigitel data from 2008 to 2015, reported an increase in overweight and obesity in Brazilian women of reproductive age, which occurred independently of age, formal education, marital status, race/skin color, and household region (except for women aged 30-39 years, black, and living in the Southern region). Those authors emphasized that, compared to the general population, there was a higher increase of obesity in women aged 18-49 years, in addition to an increase in the prevalence of overweight in women aged 18-29 years in the period, indicating the early occurrence of that risk factor for CVD and NCD. 371371. Araújo FG, Velasquez-Melendez G, Felisbino-Mendes MS. Prevalence Trends of Overweight, Obesity, Diabetes and Hypertension Among Brazilian Women of Reproductive Age Based on Sociodemographic Characteristics. Health Care Women Int. 2019;40(4):386-406. doi: 10.1080/07399332.2019.1570516. It is worth noting that the Vigitel uses self-reported diagnosis.
• A cross-sectional population-based study was conducted in 2002 and 2003 with participants from the “Household inquiry on risk behavior and self-reported morbidity from NCDs”. The study assessed 23 457 individuals aged 15 years or older, living in 16 Brazilian capitals (Aracaju, Belém, Belo Horizonte, Brasília, Campo Grande, Curitiba, Florianópolis, Fortaleza, João Pessoa, Manaus, Natal, Porto Alegre, Recife, Rio de Janeiro, São Paulo, and Vitória). There were 3142 elderly, of whom 1868 (59.4%) were women and 1274 (40.6%) were men. The mean age was 69.5±0.19 years, and 1742 (55.4%) were 60-69 years old. The prevalence of obesity was 17.7% in the age group ‘60-69 years’, 22.9% in the age group ‘70-79 years’, and 17.5% in the age group ‘80+ years’. Obesity was more frequent in women (19.3%; 95% CI, 16.6 - 22.3; χ2= 9.5; p = 0.03). 372372. Pereira JC, Barreto SM, Passos VM. The Profile of Cardiovascular Health of Elderly Brazilian People Needs to Improve: A Population-Based Study. Arq Bras Cardiol. 2008;91(1):1-10. doi: 10.1590/s0066-782x2008001300001.
• A study with 157 postmenopausal women from two public outpatient clinics in the city of São Paulo, Brazil, has reported mean BMI of 28.0 kg/m2and 34.4% of obesity, which was classified as class I in 26.1%, class II in 5.7%, and class III in 2.6%. There was a statistically significant association of the overall obesity prevalence with education level (p=0.006), physical activity (p<0.001), use of hormone-replacement therapy in menopause (p=0.007), and number of pregnancies (p=0.002). Abdominal obesity prevalence was 73.8%. The proportion of women with abdominal obesity was higher among those with up to 7 years of schooling (p=0.030). 373373. França AP; Aldrighi JM, Marucci MFN. Factors associated With body and abdominal obesity in post-menopausal women. Rev Bras Saude Mater Infant. 2008:8(1):65-73. doi: 10.1590/S1519-38292008000100008.
• A population-based cross-sectional study using data from the PNS 2013 has reported ideal BMI (<25 kg/m2) in 46.8% of the women (95% CI, 45.5 - 48.1), 40.5% of the men (95% CI, 39 - 42), and 43.7% of the total sample (95% CI, 42.7 - 44.7). When stratifying by age group, the ideal BMI prevalence was 54.2% (95% CI, 52.4 - 55.8) in the age group ‘18-35 years’, 36.8% (95% CI, 35.4 - 38.2) in the age group ‘36-59 years’, and 40.9% (95% CI, 38.6 - 43.2) in the age group ‘60+ years’. Ideal BMI was more frequent in the Northeastern region (47.5%) and less frequent in the Southern region (40.4%) of Brazil. 374374. Velasquez-Melendez G, Felisbino-Mendes MS, Matozinhos FP, ClaroI R, Gomes CS, Malta DC. Ideal cardiovascular health prevalence in the Brazilian population – National Health Survey (2013). Rev Bras Epidemiol. 2015;18(Suppl 2):97-108. doi: 10.1590/1980-5497201500060009.
• The ELSA-Brasil is a cohort of 15 105 voluntary active or retired civil servants from universities or research institutions from 6 Brazilian cities, enrolled from August 2008 to December 2010, aged between 35 and 74 years, composed mostly of women (54%) and middle-aged adults (78% aged <60 years). A sub-study including 14 545 participants aged 35-74 years, mostly (54.1%) women, has shown that 22.7% (n = 3298) of the participants were obese and 40.8% (n = 5934), overweight. In addition, a ‘metabolically healthy status’, according to multiple criteria, was identified in 12.0% (n = 396) of the obese and in 25.5% (n = 1514) of the overweight individuals, being associated with younger age, female sex, lower BMI, and weight change in all BMI categories after the age of 20 years. 375375. Diniz MFHS, Beleigoli AMR, Ribeiro ALP, Vidigal PG, Bensenor IM, Lotufo PA, Duncan BB, Schmidt MI, Barreto SM. Factors Associated With Metabolically Healthy Status in Obesity, Overweight, and Normal Weight at Baseline of ELSA-Brasil. Medicine. 2016;95(27):e4010. doi: 10.1097/MD.0000000000004010. Another sub-study, including 6453 men and 7686 women and assessing the association of BMI and waist circumference with the socio-occupational class, has shown that, for women, the effects of low and intermediate socio-occupational class were greater for those with waist circumference between 80 and 88 cm or overweight, while for men, the low and intermediate socio-occupational class associated with adequate waist circumference or normal BMI. 376376. Oliveira TL, Griep RH, Guimarães JN, Giatti L, Chor D, Fonseca MJM. Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): Socio-Occupational Class as an Effect Modifier for the Relationship Between Adiposity Measures and Self-Rated Health. BMC Public Health. 2019;19(1):734. doi: 10.1186/s12889-019-7072-y. Another sub-study assessing the entire cohort has reported a higher prevalence of overweight among men, while obesity was more common among women. Insufficient time for self-care and leisure was associated with overweight (PR = 1.29; 95% CI, 1.04 - 1.61) and obesity (PR = 1.65; 95% CI, 1.28 - 2.12) among women working more than 40 hours/week, and the authors concluded that the results were due to gender inequality involving the relation between time use and health. 377377. Pinto KA, Griep RH, Rotenberg L, Almeida MCC, Barreto RS, Aquino EML. Gender, Time Use and Overweight and Obesity in Adults: Results of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). PLoS One. 2018;13(3):e0194190. doi: 10.1371/journal.pone.0194190. Another study using multilevel logistic regression models adjusted to age, education, skin color, state of residence, individual level, and social cohesion and perceived violence scores has shown that women living in less socially cohesive areas and more violent neighborhoods were more likely to be obese as compared to their counterparts (OR 1.25, 95% CI, 1.02 - 1.53; OR 1.28, 95% CI, 1.04 - 1.56, respectively). 378378. Chaparro MP, Pina MF, Cardoso LO, Santos SM, Barreto SM, Giatti Gonçalves L, Matos SMA, Fonseca MMJ, Chor D, Griep RH. The Association Between the Neighbourhood Social Environment and Obesity in Brazil: A Cross-Sectional Analysis of the ELSA-Brasil Study. BMJ Open. 2019;9(9):e026800. doi: 10.1136/bmjopen-2018-026800.
Children and Adolescents
• The increase in obesity prevalence has also been observed among Brazilian children and adolescents. A meta-analysis of 21 studies with 18 463 Brazilian children/adolescents has estimated a 14.1% obesity prevalence, 16.1% for boys and 14.95% for girls, with no significant difference between sexes (PR = 1.06; 95% CI, 0.81 - 1.40; p> 0.05). 379379. Aiello AM, Mello LM, Nunes MS, Silva AS, Nunes A. Prevalence of Obesity in Children and Adolescents in Brazil: A Meta-analysis of Cross-sectional Studies. Curr Pediatr Rev. 2015;11(1):36-42. doi: 10.2174/1573396311666150501003250.
• The ERICA study has assessed 73 399 students, 55.4% of the female sex, with mean age of 14.7±1.6 years. The prevalence of obesity was 8.4% (95% CI, 7.9 - 8.9), lower in the Northern region and higher in the Southern region, and, regarding sex, higher among men. Obese adolescents had a higher prevalence of hypertension, 28.4% (95% CI, 25.5 - 31.2), as compared to overweight adolescents, 15.4% (95% CI, 17.0 - 13.8), and eutrophic adolescents, 6.3% (95% CI, 5.6 - 7.0). The fraction of hypertension attributable to obesity was 17.8%. 299299. Bloch KV, Klein CH, Szklo M, Kuschnir MC, Abreu Gde A, Barufaldi LA, da Veiga GV, Schaan B, da Silva TL, de Vasconcellos MT, Moraes AJ, Borges AL, de Oliveira AM, Tavares BM, de Oliveira CL, Cunha Cde F, Giannini DT, Belfort DR, Santos EL, de Leon EB, Fujimori E, Oliveira ER, Magliano Eda S, Vasconcelos Fde A, Azevedo GD, Brunken GS, Guimarães IC, Faria Neto JR, Oliveira JS, de Carvalho KM, Gonçalves LG, Monteiro MI, Santos MM, Jardim PC, Ferreira PA, Montenegro RM Jr, Gurgel RQ, Vianna RP, Vasconcelos SM, Goldberg TB. ERICA: Prevalences of Hypertension and Obesity in Brazilian Adolescents. Rev Saude Publica. 2016;50(Suppl 1):9s. doi: 10.1590/S01518-8787.2016050006685.
• A systematic review with meta-analysis published by Sbaraini et al. in 2021 compiled data from 151 studies on overweight and obesity prevalence in Brazilian adolescents aged 10-19 years. An increase in overweight prevalence was observed in recent decades: 8.2% (95% CI, 7.7 - 8.7) up to 2000, 18.9% (95% CI, 14.7 - 23.2) from 2000 to 2009, and 25.1% (95% CI, 23.4 - 26.8) from 2010 onward, a pattern similar to that of obesity prevalence. The Southeastern and Southern regions had the highest overweight and obesity prevalence, with no difference between sexes. 337337. Sbaraini M, Cureau FV, Ritter JDA, Schuh DS, Madalosso MM, Zanin G, Goulart MR, Pellanda LC, Schaan BD. Prevalence of Overweight and Obesity Among Brazilian Adolescents Over Time: A Systematic Review and Meta-Analysis. Public Health Nutr. 2021:1-12. doi: 10.1017/S1368980021001464.
• The determinants of obesity prevalence increase include diet changes, environment, greater offer of high-energy food, marketing, urbanization, and reduced time and space for physical activities. 380380. GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, Salama JS, Vos T, Abate KH, Abbafati C, Ahmed MB, Al-Aly Z, Alkerwi A, Al-Raddadi R, Amare AT, Amberbir A, Amegah AK, Amini E, Amrock SM, Anjana RM, Ärnlöv J, Asayesh H, Banerjee A, Barac A, Baye E, Bennett DA, Beyene AS, Biadgilign S, Biryukov S, Bjertness E, Boneya DJ, Campos-Nonato I, Carrero JJ, Cecilio P, Cercy K, Ciobanu LG, Cornaby L, Damtew SA, Dandona L, Dandona R, Dharmaratne SD, Duncan BB, Eshrati B, Esteghamati A, Feigin VL, Fernandes JC, Fürst T, Gebrehiwot TT, Gold A, Gona PN, Goto A, Habtewold TD, Hadush KT, Hafezi-Nejad N, Hay SI, Horino M, Islami F, Kamal R, Kasaeian A, Katikireddi SV, Kengne AP, Kesavachandran CN, Khader YS, Khang YH, Khubchandani J, Kim D, Kim YJ, Kinfu Y, Kosen S, Ku T, Defo BK, Kumar GA, Larson HJ, Leinsalu M, Liang X, Lim SS, Liu P, Lopez AD, Lozano R, Majeed A, Malekzadeh R, Malta DC, Mazidi M, McAlinden C, McGarvey ST, Mengistu DT, Mensah GA, Mensink GBM, Mezgebe HB, Mirrakhimov EM, Mueller UO, Noubiap JJ, Obermeyer CM, Ogbo FA, Owolabi MO, Patton GC, Pourmalek F, Qorbani M, Rafay A, Rai RK, Ranabhat CL, Reinig N, Safiri S, Salomon JA, Sanabria JR, Santos IS, Sartorius B, Sawhney M, Schmidhuber J, Schutte AE, Schmidt MI, Sepanlou SG, Shamsizadeh M, Sheikhbahaei S, Shin MJ, Shiri R, Shiue I, Roba HS, Silva DAS, Silverberg JI, Singh JA, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tegegne BS, Terkawi AS, Thakur JS, Tonelli M, Topor-Madry R, Tyrovolas S, Ukwaja KN, Uthman OA, Vaezghasemi M, Vasankari T, Vlassov VV, Vollset SE, Weiderpass E, Werdecker A, Wesana J, Westerman R, Yano Y, Yonemoto N, Yonga G, Zaidi Z, Zenebe ZM, Zipkin B, Murray CJL. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13-27. doi: 10.1056/NEJMoa1614362.
https://doi.org/10.1056/NEJMoa1614362...
Incidence
• A study derived from the ELSA-Brasil cohort with a 3.8-year follow-up of 13 625 men and women aged 35-74 years, included from 2008 to 2010, showed 7.7% and 10.6% global incidence of overweight and obesity, respectively. The highest percentages were observed among low education level (35.0%) and black (28.5%) women and young men (21.1%). The authors reported overweight increase with age, low per capita income, and fewer years of schooling. 381381. Matos SMA, Duncan BB, Bensenor IM, Mill JG, Giatti L, Molina MDCB, Fonseca MJM, Schmidt MI, Lotufo PA, Griep RH, Barreto SM, Almeida MDCC. Incidence of Excess Body Weight and Annual Weight Gain in Women and Men: Results From the ELSA-Brasil Cohort. Am J Hum Biol. 2021:e23606. doi: 10.1002/ajhb.23606.
• Using data from the Vigitel, obesity incidence and persistence were estimated among Brazilian adults from 2006 to 2009. The authors observed that the overweight incidence at the age of 20 years is estimated at 40% for men and 30% for women. The persistence of obesity, however, is estimated at 65% for the male sex and 47% for the female sex. The authors highlight the need to elaborate public policies, particularly for the youth, to reduce dietary risks and promote physical activity. 382382. Conde WL, Borges C. The Risk of Incidence and Persistence of Obesity Among Brazilian Adults According to Their Nutritional Status at the end of Adolescence. Rev Bras Epidemiol. 2011;14(Suppl 1):71-9. doi: 10.1590/s1415-790x2011000500008.
Mortality
• A meta-analysis of 239 prospective studies has shown a consistent relationship of overweight and obesity (all grades) with all-cause mortality in different populations around the world. The authors hypothesized the possibility of metabolically healthy obese individuals. 383383. Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, Cairns BJ, Huxley R, Jackson ChL, Joshy G, Lewington S, Manson JE, Murphy N, Patel AV, Samet JM, Woodward M, Zheng W, Zhou M, Bansal N, Barricarte A, Carter B, Cerhan JR, Smith GD, Fang X, Franco OH, Green J, Halsey J, Hildebrand JS, Jung KJ, Korda RJ, McLerran DF, Moore SC, O’Keeffe LM, Paige E, Ramond A, Reeves GK, Rolland B, Sacerdote C, Sattar N, Sofianopoulou E, Stevens J, Thun M, Ueshima H, Yang L, Yun YD, Willeit P, Banks E, Beral V, Chen Zh, Gapstur SM, Gunter MJ, Hartge P, Jee SH, Lam TH, Peto R, Potter JD, Willett WC, Thompson SG, Danesh J, Hu FB. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-86. doi: 10.1016/S0140-6736(16)30175-1.
• A study assessing 1450 individuals aged 60 years or more from the Bambuí Cohort Study of Aging has reported the inverse relationship of continuous BMI (HR 0.85; 95% CI, 0.80 - 0.90) with mortality, even after adjusting to confounding variables. Obesity occurred in 12.5% of the elderly and was positively associated with the female sex, higher family income, and the presence of hypertension and diabetes, and inversely associated with physical activity. Overweight was inversely (HR 0.76; 95% CI, 0.61 - 0.93) associated with mortality. Individuals with BMI between 25 kg/m2and 35 kg/m2had the lowest absolute rates of death at 10-year follow-up. The authors concluded that the usual BMI cut-off points should not be used to guide public policies for the elderly in Brazil. 384384. Beleigoli AM, Boersma E, Diniz MF, Lima-Costa MF, Ribeiro ALP. Overweight and Class I Obesity are Associated With Lower 10-Year Risk of Mortality in Brazilian Older Adults: The Bambuí Cohort Study of Ageing. PLoS One. 2012;7(12):e52111. doi: 10.1371/journal.pone.0052111.
All-cause Mortality Attributable to High BMI
• Table 10-4 shows the age-standardized rates of mortality due to all causes attributable to high BMI, per 100 000 inhabitants, and percent change of the rates, in Brazil and FUs in 1990 and 2019 (GBD 2019). The greatest decreases in the mortality percentages occurred in the Brazilian states with the highest incomes. Distrito Federal showed the greatest reduction -33.8 (-45.2;-14.6), followed by São Paulo -29.6 (-41;-9.3), Rio de Janeiro -27.7 (-39.7;-6.8), Santa Catarina -22.7 (-35.5;-1.7), Minas Gerais -21.1 (-36.5;13.9), Paraná -18.2 (-31.9;9.1, Bahia -9.7 (-23.1;16.2), Rondônia -8.7 (-29.9;33.9), Mato Grosso do Sul -7.6 (-26;24.5), and Goiás -3.8 (-29.4;49.2). Regarding obesity in men, according to Table 10-5, most FUs had a positive percent change in the death rates due to high BMI, which ranged from 7.6 (-17.9;72.3) in the state of Roraima to 63.1(4.4;230.1) in the state of Maranhão.
• Regarding obesity in women, according to Table 10-5, most FUs had a positive percent change in the death rates due to high BMI, ranging from 1.2 (-23.9;46.9) in the state of Sergipe to 109 (39.4;294.2) in the state of Maranhão, except for Distrito Federal, which showed the greatest reduction -38.2 (-49.9;-20.6), followed by São Paulo -34.4 (-46.3;-14.3), Rio de Janeiro -31.5 (-43.8;-10), Santa Catarina -28.5 (-41.7;-6.6), Minas Gerais -27.6 (-42.6;1.4), Paraná -24.5 (-38.5;2.3), Rio Grande do Sul -24.6 (-37.2;-2.6), Mato Grosso do Sul -14.5 (-32;16.7), Amazonas -13 (-30.5;17.1), Goiás -10.4 (-35.9;42.1), and Espírito Santo -1.3 (-24.9;43.5). The greatest decreases in the mortality percentages in Brazil occurred for women -16.3 (-28.8;6) as compared to men, -2.1 (-19;35.5) (Table 10-5).
• Table 10-6 shows the number of deaths and the crude and age-standardized mortality rates due to all causes attributable to high BMI in Brazil, by age group, in 1990 and 2019, in addition to the percent change of the rates in the period, according to GBD 2019 data. Considering age-standardized rates in the period, there was a percent reduction of -9.7 (-23.1;16.2).
• Chart 10-1 shows the increase in the number of deaths due to all causes attributable to high BMI, in Brazil. Chart 10-2 shows the crude and age-standardized mortality rates due to all causes attributable to high BMI from 1990 to 2019. While the crude rates increased, the age-standardized rates showed stability in the period, suggesting that population aging is the determinant of the increase. According to Brant et al ., regarding the ranking of the age-standardized mortality rates due to CVD attributable to risk factors, by sex, in 1990 and 2019, there was an increase in the incidence of high BMI, and that ranking passed from 6th to 3rd in women and from 7th to 4th in men. 269269. Brant LCC, Nascimento BR, Veloso GA, Gomes CS, Polanczyk CA, Oliveira GMM, Ribeiro ALP, malta DC. Burden of Cardiovascular Diseases Attributable to Risk Factors in Brazil: Data From the Global Burden of Disease 2019. Rev Soc Bras Med Trop. 2021;2021(54). Epub ahead of print.
• Chart 10-3 shows the distribution of proportional mortality due to all causes attributed to high BMI, by age group and sex. Proportional mortality attributed to high BMI is higher in the age group ‘50-69 years’ in men and women, with a predominance of women. Age-standardized proportional mortality was 84.4 (48.1;127.9) in 1990 and 76.2 (52.9;102.1) in 2019, with a percent change of -9.7 (-23.1;16.2).
• Chart 10-4 shows the age-standardized mortality rates due to diseases attributed to high BMI, stratified by all causes in Brazil, 1990 and 2019, according to GBD 2019. High BMI contributed mainly to mortality from: ischemic heart disease [number of deaths: 21 732.5 (11 703.8;34 207.7) in 1990 and 45 210.1 (29 102.5;63 084.1) in 2019; proportional mortality: 25.1% (13.2%;40.2%) in 1990 and 19.1 (12.2%;27.0%) in 2019]; stroke [number of deaths: 24 398.5 (14 209.8;35 441.2) in 1990 and 35 124.7 (24 073.7;46 859.7) in 2019; proportional mortality: 25% (14.2%;37.1%) in 1990 and 14.6% (9.9%;19.6%) in 2019]; and diabetes [number of deaths: 10 862.5 (6 997.5;15 055.0) in 1990 and 33 811.0 (24 964.7;43 247.8) in 2019; proportional mortality: 12.2% (7.7%;17.3%) in 1990 and 14.5% (10.5%;18.6%) in 2019]. The contribution to all causes of death was 74 266.2 (43 491.7;110 056.9) and 177 939.7 (124 637.7;237 783.0) in numbers of deaths in 1990 and 2019, respectively.
• Chart 10-5 shows the age-standardized mortality rates due to specific causes attributed to high BMI, per 100 000 inhabitants, in the FU, for all ages, by sex, according to the GBD 2019. Mortality varied in the FUs differently by sex. The highest age-standardized mortality rates (per 100 000 inhabitants) due to CVD and diabetes attributed to high BMI in women were observed in Alagoas (52.1), Pernambuco (45.0), Tocantins (42.1), Espírito Santo (40.7), Maranhão (40.5), Rondônia (40.2), and Rio de Janeiro (40.1). For men, those rates were higher in Pernambuco, Maranhão, Rio de Janeiro, Tocantins, and Alagoas. Felisbino-Mendes et al . have reported that, in 2017, obesity accounted for 12.3% of all deaths, making up a total of 165 954 deaths. Proportional mortality attributed to high BMI was more expressive in women (14.6%, 95% UI, 10.7 - 18.9) than in men (10.5%, 95% UI, 7.2 - 14.1). 368368. Felisbino-Mendes MS, Cousin E, Malta DC, Machado ÍE, Ribeiro ALP, Duncan BB, Schmidt MI, Silva DAS, Glenn S, Afshin A, Velasquez-Melendez G. The Burden of Non-Communicable Diseases Attributable to High BMI in Brazil, 1990-2017: Findings From the Global Burden of Disease Study. Popul Health Metr. 2020;18(Suppl 1):18. doi: 10.1186/s12963-020-00219-y.
• Chart 10-6 shows the correlation between the SDI 2019 and the percent change of the age-standardized mortality rates from CVD attributed to high BMI between 1990 and 2019, for all ages and both sexes. The reduction in mortality from CVD attributed to high BMI correlated with the socioeconomic improvement in the FUs and might have resulted from the late epidemiological transition and competing causes of death in the regions with the lowest income.
Mortality from Cardiovascular Diseases Attributable to High BMI
• Tables 10-7 and 10-8 show the number of deaths and age-standardized mortality rates from CVD attributed to high BMI, per 100 000 inhabitants, in 1990 and 2019, and the percent change of rates in the period, in Brazil and its FUs (GBD 2019). Most FUs showed a negative percent change of the rates of death due to high BMI in men, which ranged from -1 (-29.5;65.5) in Mato Grosso to -44.6 (-57.4;-21.5) in the Distrito Federal. The highest decreases in the percent of mortality occurred in the FUs with higher income in Brazil. The highest positive percent changes occurred in the FUs of the Northern [Tocantins 50.5 (1.6;202.0)] and Northeastern [Ceará 50.2 (-0.7;188.2)] regions. In Brazil, there was a negative change in the mortality rates from CVD attributable to high BMI for men [-22.8 (-35.9;6.2)].
• Regarding women, most states had a negative percent change of mortality rates from CVD attributable to high BMI, which ranged from -2.8 (-22.6;32.1) in Amapá to -50.4 (-60.4;-35.8) in the Distrito Federal. The highest decreases in the percent of mortality occurred in the FUs with higher income in Brazil. The highest positive percent changes occurred in the FUs of the Northern [Maranhão 89.9 (27.4;262.4)]. In Brazil, there was a negative change in the mortality rates from CVD attributable to high BMI for women [-33.9 (-43.7;-16.7)], which was higher than that for men [-22.8 (-35.9;6.2)] (Table 10-8).
• Table 10-9 shows the number of deaths, the crude and age-standardized mortality rates from CVD attributed to high BMI in Brazil, in 1990 and 2019, by age group, and the percent change of rates in the period, according to the GBD 2019. Considering the age-standardized rates in the period, the percent change was -28.5 (-38.8;-8.6).
Burden of disease
Burden of Disease from All Causes Attributable to High BMI
• Table 10-10 shows DALY in absolute numbers, age-standardized DALY rates (per 100 000 inhabitants) due to all causes of death attributed to high BMI, and the percent change of rates in Brazil and FUs in 1990 and 2019 (GBD 2019). Regarding the burden of disease in 2019, high BMI accounted for 177 939.7 (124 637.7;237 783) DALYs [76.2 (52.9;102.1) per 100 000 inhabitants]. The percent change was -9.7 (-23.1;16.2) in relation to 1990, for when 74 266.2 (43 491.7;110 056.9) DALYs [84.4 (48.1;127.9) per 100 000 inhabitants] were estimated. The FUs of the Northern [Maranhão 84.8 (25.5;250.7)] and Northeastern [Ceará 65.4 (19.9;172.1)] regions had the highest positive percent changes.
• Table 10-11 shows the number of DALYs, the crude and age-standardized DALY rates due to all causes attributed to high BMI in Brazil, in 1990 and 2019, by age group, and the percent change of the rates in the period, according to GBD 2019 data. The highest positive percent change occurred in children and adolescents, from 5 to 14 years [99.5 (53.1;158.3)].
• Charts 10-7 and 10-8 show the graphic representation of the absolute numbers and the age-standardized and all age rates of YLLs, YLDs, and DALYs due to high BMI, from 1990 to 2019, in Brazil, respectively. It is worth noting the growth trend of all absolute numbers and crude rates per 100 000 inhabitants. However, the age-standardized rates of DALYs and YLLs showed a trend towards decrease in the period, while those of YLDs increased, suggesting a growing impact on morbidity due to obesity even regardless of population aging. Felisbino-Mendes et al . have estimated that the DALYs, for both sexes, increased by 96% and 42% due to population aging and growth, respectively, and by 130% due to change in exposure to risk. 368368. Felisbino-Mendes MS, Cousin E, Malta DC, Machado ÍE, Ribeiro ALP, Duncan BB, Schmidt MI, Silva DAS, Glenn S, Afshin A, Velasquez-Melendez G. The Burden of Non-Communicable Diseases Attributable to High BMI in Brazil, 1990-2017: Findings From the Global Burden of Disease Study. Popul Health Metr. 2020;18(Suppl 1):18. doi: 10.1186/s12963-020-00219-y.
• Chart 10-9 shows the age-standardized DALYs rates due to specific causes attributed to high BMI, per 100 000 inhabitants, in the FUs, for all ages, by sex, according to GBD 2019. The DALYs varied in the FUs differently by sex. Diabetes and kidney diseases were the second major causes of DALYs attributed to high BMI, being preceded by CVD. The highest age-standardized rates of DALYs due to diabetes and kidney diseases attributed to high BMI in women (per 100 000 inhabitants) were observed in Alagoas (1320.1), Roraima (1250.8), Sergipe (1253.6), Pernambuco and Maranhão (1013.5), Paraíba (990.4), Rondônia (989.3), and Tocantins (981.7). Regarding men, those rates (per 100 000 inhabitants) were higher in Alagoas (1263.9), Sergipe (1168.1), Maranhão (1130.8), Pernambuco (1104.7), Bahia (1086.2), Roraima (1071.7), Paraíba (1047.4), Rio de Janeiro (1042.5), and Rio Grande do Norte (1024.5).
Burden of Cardiovascular Disease Attributable to High BMI
• Regarding burden of disease in 2019, high BMI accounted for 177 939.7 (95% UI, 124 637 – 237 783) DALYs due to CVD [76.2 (95% UI, 52.9 – 102.1) per 100 000 inhabitants], with higher relevance to ischemic heart disease [45 210.1 (95% UI, 29 102.5 – 63 084.1)] and stroke [35 124.7 (95% UI, 24 073.7 – 46 859.7)]. In Brazil, this risk factor contributed, in 2019, to 5 817 938.7 (95% UI, 4 197 826.2 – 7 541 630) DALYs [2404.5 (95% UI, 1733.3 – 3121.6) per 100 000 inhabitants]. The percent reduction was -6.4 (95% UI, -19.6 to 19.1) in relation to 1990, for when 2 579 849.9 (95% UI, 1 556 675.2 – 3 720 770.6) DALYs [35 124.7 (95% UI, 24 073.7 – 46 859.7)] were estimated (Chart 10-10).
• Tables 10-12 and 10-13 show the age-standardized rates of DALYs due to CVD attributed to high BMI, per 100 000 inhabitants, in 1990 and 2019, and the percent change of rates in the period, by sex, in Brazil and FUs (GBD 2019). Most FUs had a decrease in the DALYs for women in the period, which was more marked in the Distrito Federal [-34.8 (-44.7;-20)], Rio de Janeiro [-28.6 (-39.4;-10.7)], São Paulo -27.6 (-38.7;-9.2)], Santa Catarina [-22.8 (-34.8;-3.5)], Minas Gerais [-21.3 (-35.7;5.1)], and Rio Grande do Sul [-20.3 (-31.6;-0.6)]. The state of Maranhão had the highest increase between 1990 and 2019 [95.8 (33.9;254.2].
• Similar behavior was observed for men, with a percent decrease of obesity from 1990 to 2019. The highest percent decreases were observed in the Distrito Federal [-25.8 (-39.8;-0.9)], Rio de Janeiro [-22.3 (-36.9;5.4)], São Paulo [-20.2 (-35;8.7)], Rio Grande do Sul [-19.5 (-32.3;4.3)], Santa Catarina [-11.5 (-28.3;22.1)], and Minas Gerais [-8.1 (-30.2;52.3)], smaller than those observed for women. Ceará had the highest increase between 1990 and 2019 [81.8 (25.1;231.1)]. In addition, the highest percent increases were observed for women in the period (Table 10-13). It is worth noting that the same pattern was observed for Brazil as a whole, with higher percent decrease for women [-12 (-23.8;8.9)] as compared to men [-0.1 (-16.5;36.8)].
• Table 10-14 shows the number of DALYs, the crude and age-standardized rates of DALYs due to CVD attributed to high BMI in Brazil, in 1990 and 2019, by age group, and the percent change of the rates in the period, according to data from GBD 2019. The highest negative percent change occurred in the age group ‘50-69 years’ [-33.6 (-42.5;-16.5)]. There was a percent reduction of -31.2 (-40.5;-12.4) regarding the age-standardized rates in the period (Table 10-12).
Impact on Cardiovascular Health
• High BMI causes chronic systemic inflammation and high sympathetic activity, which can contribute to insulin resistance and hypertension, leading to endothelial dysfunction and atherosclerosis, contributing to diabetes mellitus. Its effect is mainly mediated by other intermediate risk factors, such as hypertension, hypercholesterolemia, and hyperglycemia. 385385. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects), Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Metabolic Mediators of the Effects of Body-Mass Index, Overweight, and Obesity on Coronary Heart Disease and Stroke: A Pooled Analysis of 97 Prospective Cohorts With 1·8 Million Participants. Lancet. 2014;383(9921):970-83. doi: 10.1016/S0140-6736(13)61836-X. Obesity has a multifactorial nature and is one of the major factors to explain the increase in NCD because of its frequent association with CVD, such as arterial hypertension, stroke, heart failure, dyslipidemia, diabetes, atrial fibrillation, and sudden death. The interventions that reduce hypertension, and cholesterol and glucose levels could solve half of the risk for coronary artery disease and three-quarters of the risk for stroke associated with high BMI. 386386. Agrawal S, Agrawal PK. Association Between Body Mass index and Prevalence of Multimorbidity in Low-and Middle-income Countries: A Cross-Sectional Study. Int J Med Public Health. 2016;6(2):73-83. doi: 10.5530/ijmedph.2016.2.5.
• Rimes-Dias and Canella have hypothesized that the NCDs associated with obesity usually require drug treatment and carried out a study with data from the PNS 2013, with 59 402 individuals aged 18 years or older. They assessed the number of medications used to treat nine NCDs related to obesity (arterial hypertension, CVD, stroke, diabetes, arthritis and rheumatism, chronic kidney disease, lung disease, chronic low back pain, and depression). The use of medications increased progressively with BMI increase. The risk of having to use medications to treat two or more NCDs was 70% greater among overweight individuals (adjusted RR = 1.66; 95% CI, 1.46 – 1.89), 170% greater among those with class I obesity (adjusted RR = 2.68; 95% CI, 2.29 – 3.12), 340% greater among those with class II obesity (adjusted RR = 4.44; 95% CI, 3.54 – 5.56), and 450% greater among those with class III obesity (adjusted RR = 5.53; 95% CI, 3.81 – 8.02) as compared to normal-weight individuals. 387387. Rimes-Dias KA, Canella DS. Medication Use and Obesity in Brazil: Results From the National Health Survey. Sci Rep. 2020;10(1):18856. doi: 10.1038/s41598-020-76058-6.
• A cross-sectional study, assessing the presence of cardiovascular risk factors according to the pattern of body fat distribution, was conducted with 113 Brazilians aged 80 years or more (mean age, 83.4 years), of both sexes, recruited from 2009 to 2010 in the city of Presidente Prudente, São Paulo state, as part of the SABE survey. The authors reported the association of abdominal and total obesity with risk factors for CVD, such as higher levels of total cholesterol and triglycerides. There was a significant association of arterial hypertension and total obesity. 388388. Gomes IC, Santos VR, Christofaro DGD, Fernandes RA, Bueno DR, Freitas Júnior IF. Cardiovascular risk factors and body fat distribution in the oldest elderly. Medicina; 2016;49(1):17-25.
• A cohort of 12-month duration, assessing 89 adolescents aged 11-14 years in the city of Presidente Prudente, has shown, after adjusting to gender, age, biological maturation, and physical activity, that the changes in femoral intima-media thickness associate with changes in body fat: for each percent increase in body fat, the femoral intima-media thickness increased by 0.007 mm. 389389. Cayres SU, Kemper HCG, Vanderlei LCM, Casonatto J, Machado-Rodrigues AM, Barbosa MF, Fernandes RA. Changes in Body Fatness Affect Cardiovascular Outcomes More Than Changes in Physical Activity. Cardiol Young. 2017;27(6):1060-7. doi: 10.1017/S1047951116001992.
Risk Factors and Prevention
• Rabacow et al . have estimated the proportion of deaths from NCDs that could be reduced in Brazil by reducing population-wide BMI by using data from the PNS 2013. The population-wide BMI reduction to a theoretical minimum risk exposure level (22.0 kg/m2) could prevent approximately 168 431 deaths per year in Brazil, of which 106 307 from CVD. The reduction to a BMI level of 24.6 kg/m2could prevent 65 721 deaths, representing 10% of the deaths from NCDs and 5.8% of all deaths. A reduction by 1.0 kg/m2in BMI at population level could prevent 30 715 deaths, representing 4.6% of the deaths from NCDs and 2.7% of all deaths. This data set emphasizes the need for adopting anti-obesity measures at national level. 390390. Rabacow FM, Azeredo CM, Rezende LFM. Deaths Attributable to High Body Mass in Brazil. Prev Chronic Dis. 2019;16:E141. doi: 10.5888/pcd16.190143.
• A study, analyzing data from the Household Budget Survey 2002/2003 and 2008/2009 and from the PNS 2013, with 234 791 adults aged 20-59 years, has shown that the highest education levels were associated with obesity and excess weight for men, and the middle school level was associated with an increase in obesity for women. The authors concluded that the findings reveal the need for nutritional education, in addition to campaigns and policies to hold the obesity epidemic. 391391. Gomes DCK, Sichieri R, Verly E Jr, Boccolini CS, de Moura Souza A, Cunha DB. Trends in Obesity Prevalence Among Brazilian Adults From 2002 to 2013 by Educational Level. BMC Public Health. 2019;19(1):965. doi: 10.1186/s12889-019-7289-9.
Health Care Utilization and Cost
• A study assessed the 1-year total direct costs associated with the outpatient and inpatient care to overweight- and obesity-related diseases, from the perspective of the SUS, in Brazil, between 2008 and 2010. The values were estimated at US$ 2.1 billion, of which US$ 1.4 billion (68.4% of the total costs) due to hospitalizations and US$ 679 million due to outpatient procedures. Using the population attributable risk, the authors reported that approximately 10% of those costs were attributable to overweight and obesity. The costs for women were higher than those for men, because of higher outpatient clinic expenses (73.3% vs. 26.7%). 392392. Bahia L, Coutinho ES, Barufaldi LA, Abreu G A, Malhão TA, Souza CP, Araujo DV. The Costs of Overweight and Obesity-Related Diseases in the Brazilian Public Health System: Cross-Sectional Study. BMC Public Health. 2012;12:440. doi: 10.1186/1471-2458-12-440. Another study has estimated the total direct cost of overweight/obesity at 3.02% of the total costs with hospitalization for men and 5.83% for women, corresponding to 6.8% and 9.3% of all hospitalizations (excluding pregnant women), respectively. 393393. Sichieri R, do Nascimento S, Coutinho W. The Burden of Hospitalization Due to Overweight and Obesity in Brazil. Cad Saude Publica. 2007;23(7):1721-7. doi: 10.1590/s0102-311x2007000700025.
• A study has assessed the cost-utility of gastric bypass surgery as compared to clinical treatment for severe obesity with and without diabetes from the SUS perspective. A 10-year time horizon and a 5% discount rate were considered in the Markov model. Over 10 years, gastric bypass surgery increased the QALYs and costs as compared to clinical treatment, resulting in an ICER of Int$ 1820.17/QALY and Int$ 1937.73/QALY for individuals with and without diabetes, respectively. The sensitivity analysis showed that the utility values and direct costs of the treatments were the parameters that affected most the ICER. The authors concluded that gastric bypass surgery has a good cost-benefit ratio for severely obese individuals from the SUS perspective, with better results for obese individuals with diabetes. 394394. Assumpção RP, Bahia LR, Rosa MQM, Correia MG, Silva EN, Zubiaurre PR, Mottin CC, Vianna DA. Cost-Utility of Gastric Bypass Surgery Compared to Clinical Treatment for Severely Obese With and Without Diabetes in the Perspective of the Brazilian Public Health System. Obes Surg. 2019;29(10):3202-11. doi: 10.1007/s11695-019-03957-7.
• A study concluded that the total costs of hypertension, diabetes, and obesity in the SUS reached R$ 3.45 billion (95% CI, 3.15 – 3.75) in 2018 (US$ 890 million). Regarding obesity as a risk factor for hypertension and diabetes, the attributable costs reached R$ 1.42 billion (95% CI, 0.98 – 1.87), representing 41% of the total costs. 395395. Nilson EAF, Andrade RCS, Brito DA, Oliveira ML. Costs Attributable to Obesity, Hypertension, and Diabetes in the Unified Health System, Brazil, 2018. Rev Panam Salud Publica. 2020;44:e32. doi: 10.26633/RPSP.2020.32.
https://doi.org/10.26633/RPSP.2020.32...
• A micro-simulation model was used to project the extent of obesity and obesity-related diseases and associated healthcare costs in Brazil by 2050. The model considered 13 diseases (coronary artery disease, stroke, hypertension, diabetes, osteoarthritis, and 8 types of cancer), simulating 3 hypothetical intervention scenarios: no intervention, and 1% and 5% reduction in BMI. The authors estimated that the healthcare costs will double by 2050 (US$ 10.1 billion), reaching US$ 330 billion in the 2010-2050 period. However, effective interventions, such as 1% and 5% reductions in mean BMI across the population, can reduce costs to US$ 302 billion and US$ 273 billion, respectively. 396396. Rtveladze K, Marsh T, Webber L, Kilpi F, Levy D, Conde W, McPherson K, Brown M. Health and Economic Burden of Obesity in Brazil. PLoS One. 2013;8(7):e68785. doi: 10.1371/journal.pone.0068785.
Future Research
• Gaps in primary data on mortality attributable to high BMI in Brazil and its FUs have been observed. Nationwide registries with measured data should be built to enable the development of more effective public policies to control obesity, which has been increasing in Brazil in both sexes and several age groups.
• Most public policies have failed to reduce obesity in adults and children, probably because obesity is multifactorial and involves many socioeconomic interests. It is worth emphasizing the role played by the food industry, which includes the offer of ultra-processed foods at lower costs, the absence of communication about the risks associated with overweight and obesity in social medias, in addition to the lifestyle in the big cities, where children are increasingly sedentary and eat high-calorie diets. Future studies with multifactorial interventions involving the whole family need to be conducted, to benefit mainly children and adolescents. 397397. World Health Organization. Obesity [Internet]. Geneva: World Health Organization; 2019. [cited 2021 Nov 09]. Available From: http://www.euro.who.int/en/healthtopics/noncommunicablediseases/obesity/obesity .
http://www.euro.who.int/en/healthtopics/...
• The patient-centered care for obesity requires future research and is an essential component of high-quality healthcare that can improve clinical outcomes and patient satisfaction, reducing healthcare costs. A study has suggested the following topics for obesity research: development of research agendas that emphasize the study of tools and techniques of patient-centered healthcare; prioritization of the analysis of patient’s barriers that prevent weight loss and assessment of tools to overcome such barriers; assessment of cultural and environmental factors that can affect one’s ability to lose weight; and implementation of evidence-based metrics for obese patients. 398398. Fastenau J, Kolotkin RL, Fujioka K, Alba M, Canovatchel W, Traina S. A Call to Action to Inform Patient-Centred Approaches to Obesity Management: Development of a Disease-Illness Model. Clin Obes. 2019;9(3):e12309. doi: 10.1111/cob.12309.
• More recent data have highlighted abdominal obesity, assessed by waist circumference, as a CVD risk marker that is independent of BMI. Studies quantifying fat depots, including ectopic fat, with imaging methods have shown that excess visceral adiposity is an independent indicator of poor cardiovascular outcomes. Studies assessing abdominal obesity in the Brazilian population need to be performed to investigate its incremental role in cardiovascular risk stratification in both sexes and several age groups. 399399. Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, Lear SA, Ndumele CE, Neeland IJ, Sanders P, St-Onge MP; American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021;143(21):e984-e1010. doi: 10.1161/CIR.0000000000000973.
11. SMOKING AND TOBACCO USE
Smoking and the consequences for cardiovascular diseases in Brazil and Federative Units, 1990 to 2019
ICD-10: Z.72.0
See Tables 11-1 through 11-13 and Charts 11-1 through 11-12
Abbreviations Used in Chapter 11
| ANVISA | Brazilian National Health Surveillance Agency (in Portuguese, Agência Nacional de Vigilância Sanitária ) |
| DALYs | Disability-Adjusted Life Years |
| NCDs | Noncommunicable Chronic Diseases |
| CVD | Cardiovascular Diseases |
| ELSA-Brasil | The Brazilian Longitudinal Study of Adult Health (in Portuguese , Estudo Longitudinal de Saúde do Adulto ) |
| ERICA | Brazilian Study of Cardiovascular Risk in Adolescents (in Portuguese, Estudo dos Riscos Cardiovasculares em Adolescentes ) |
| FU | Federative Unit |
| GBD | Global Burden of Disease |
| PeNSE | National Survey of Schoolchildren Health (in Portuguese: Pesquisa Nacional de Saúde do Escolar ) |
| PNS | Brazilian National Health Survey (in Portuguese, Pesquisa Nacional de Saúde ) |
| SDI | Sociodemographic Index |
| Vigitel | Telephone Survey for Surveillance of Non-Communicable Chronic Diseases (in Portuguese, Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico ) |
| YLDs | Years Lived with Disability |
| YLLs | Years of Life Lost |
– Percentage of 9th grade students who experimented with cigarettes, by sex and type of school, in Brazil, its regions and Federative Units.
– Percentage of 9th grade students who smoked in the 30 days prior to the survey, by sex and type of school, in Brazil, its regions and Federative Units.
– Percentage of 9th grade students who used other tobacco products in the 30 days prior to the survey, by sex and type of school, in Brazil, its regions and Federative Units.
– Proportion of current users of tobacco products aged 18 years and over, by sex, in Brazil, its regions, Federative Units, and urban and rural areas.
– Proportion of current tobacco users aged 18 years and over, by sex, in Brazil, its regions, Federative Units, and urban and rural areas.
– Proportion of current tobacco users aged 18 years and over, by age group, in Brazil, its regions, Federative Units, and urban and rural areas.
– Proportion of current tobacco users aged 18 years and over, by education level, in Brazil, its regions, Federative Units, and urban and rural areas.
– Proportion of current tobacco users aged 18 years and over, by skin color or race, in Brazil, its regions, Federative Units, and urban and rural areas.
– Prevalence of smokers over 18 years of age in the main Brazilian capitals, by sex, according to the Vigitel household survey.
– Age-standardized rate (per 100 000) of deaths attributed to tobacco, and percent change of rates, by sex, in Brazil and Federative Units, 1990 and 2019.
– Number and age-standardized rates (per 100 000) of deaths attributed to tobacco, and percent change of rates, in Brazil and Federative Units, 1990 and 2019.
– Proportion of non-smokers aged 18 years and over exposed to secondhand smoke in the closed workplace, by sex, in Brazil, its regions, Federative Units, and urban and rural areas.
– Distribution of persons aged 15 and over, using electronic devices with liquid nicotine or chopped tobacco leaf, according to major regions and federation units.
– Current smoking prevalence trends according to the GBD 2017 estimates and Brazilian surveys (crude values) of individuals aged 20 years and more, Brazil, 1989 to 2017.
– Trend of smoking prevalence, by sex, according to the Vigitel data, in Brazilian capitals, between 2006 and 2019.
– Mortality rate and age-standardized mortality rate, by sex, absolute number of deaths associated with tobacco use, and mortality rates (all ages and age-standardized), from 1990 to 2019.
– Absolute number of deaths attributed to tobacco and secondhand smoke, by all causes of deaths, for both sexes, 2019.
– Age-standardized mortality rates due to smoking and secondhand smoke for both sexes, by all causes of death, Brazil, 1990 and 2019.
– Total number of deaths due to cardiovascular diseases attributed to tobacco and secondhand smoke, for both sexes. Each color represents a specific cause of cardiovascular death, 1990.
– Total number of deaths due to cardiovascular diseases attributed to tobacco and secondhand smoke, for both sexes. Each color represents a specific cause of cardiovascular death, 2019.
– Correlation between the 2019 Sociodemographic Index (SDI) and percent change of mortality rates attributable to smoking between 1990 and 2019, in Brazil.
Overview
Definitions
• Current smoker: An adult who has smoked cigarettes in his or her lifetime and who currently smokes cigarettes. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
, 400400. Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2. Adolescents who smoked at least one day in past 30 days were considered current cigarette smokers. 401401. Benziger CP, Roth GA, Moran AE. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob Heart. 2016;11(4):393-7. doi: 10.1016/j.gheart.2016.10.024.
• Secondhand smoke: Also called passive smoking. Usually refers to cigarette smoke in the environment of a nonsmoker. 400400. Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2.
• Former (past) smoker: An adult who has smoked in his or her lifetime but who had quit smoking at the time of interview. 400400. Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2.
• Experimenting with tobacco use: Defined as having tried cigarettes at least once in life. 401401. Benziger CP, Roth GA, Moran AE. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob Heart. 2016;11(4):393-7. doi: 10.1016/j.gheart.2016.10.024.
• Electronic smoking devices, more commonly called electronic cigarettes or e-cigarettes, are battery-operated devices that provide nicotine, flavors, and other chemicals to the user in an aerosol. 33. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):254-743. doi: 10.1161/CIR.0000000000000950. , 402402. Silva ALOD, Moreira JC. The Ban of Eletronic Cigarettes in Brazil: Success or Failure? Cien Saude Colet. 2019;24(8):3013-24. doi: 10.1590/1413-81232018248.24282017. The liquids used in these devices can be quite different in terms of chemical composition, nicotine concentration, and additives used, and more than 8000 flavors of electronic cigarettes have been described. Discrepancy between the composition declared on the packaging and the actual composition of the product has been shown.
• The SDI is a composite index that measures per capita income, fertility, and education. It mirrors sociodemographic development. The SDI allows you to compare states and countries according to their development. 403403. GBD 2015 Mortality and Causes of Death Collaborators. Global, Regional, and National Life Expectancy, All-Cause Mortality, and Cause-Specific Mortality for 249 Causes of Death, 1980-2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459-44. doi: 10.1016/S0140-6736(16)31012-1.
https://doi.org/10.1016/S0140-6736(16)31...
Tobacco and total CVD
• Tobacco use is one of the main preventable causes of death in Brazil and worldwide. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
, 400400. Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2. Tobacco is one of the main risk factors for NCDs, such as CVD, cancer, chronic respiratory diseases, intrauterine growth restriction, and predisposition to premature birth. 33. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):254-743. doi: 10.1161/CIR.0000000000000950. The negative impact of tobacco on health results from both the direct consumption of various forms of tobacco products (smoked, inhaled or chewed) and the exposure to secondhand smoke. 400400. Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2. , 404404. Oberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide Burden of Disease From Exposure to Second-Hand Smoke: A Retrospective Analysis of Data From 192 Countries. Lancet. 2011;377(9760):139-46.
• Tobacco is an independent risk factor for CVD and multiplies the risk when associated with other risk factors, such as hypertension, dyslipidemia, and diabetes mellitus. 405405. Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2010. There is a marked increase in the risk of CVD even at low levels of tobacco exposure, including secondhand smoke and cigar smoking. In addition, the risk grows, but to a lesser extent, with the increase in the number of cigarettes per day. 3434. Baptista E, Queiroz B, Rigotti J. Decomposition of Mortality Rates From Cardiovascular Disease in the Adult Population: A Study for Brazilian Micro-Regions Between 1996 and 2015. Rev. Bras. Estud. Popul. 2018;35(2):e00050. doi: 10.20947/S102-3098a0050.
• Current or past smoking is associated with an increased risk of heart failure with reduced and preserved ejection fraction. 406406. Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of heart failure: A systematic review and meta-analysis of prospective studies. Eur J Prev Cardiol. 2019;26(3):279-288. doi: 10.1177/2047487318806658. , 407407. Watson M, Dardari Z, Kianoush S, Hall ME, DeFilippis AP, Keith RJ, Benjamin EJ, Rodriguez CJ, Bhatnagar A, Lima JA, Butler J, Blaha MJ, Rifai MA. Relation Between Cigarette Smoking and Heart Failure (From the Multiethnic Study of Atherosclerosis). Am J Cardiol. 2019;123(12):1972-7. doi: 10.1016/j.amjcard.2019.03.015.
• Tobacco consumption through different forms of smoking is associated with an increased risk for cardiovascular events, with an OR of 1.67 (95% CI, 1.25 - 2.24) for the association of ischemic heart disease and heart failure with waterpipe smoking. 408408. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabé E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castañeda-Orjuela C, Catalá-López F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Søreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3(4):524-48. doi: 10.1001/jamaoncol.2016.5688.
• Non-smokers exposed to secondhand smoke at home or at work have their risk of developing CVD increased by 25% to 30%. 44. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010. , 88. Ribeiro ALP, Duncan BB, Brant LCC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular Health in Brazil: Trends and Perspectives. Circulation. 2016;133(4): 422-33. doi: https://doi.org/10.1161/CIRCULATIONAHA.114.008727 .
https://doi.org/10.1161/CIRCULATIONAHA.1...
Exposure to secondhand smoke increases the risk of stroke by 20% to 30% and is associated with increased mortality after the event. 33. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):254-743. doi: 10.1161/CIR.0000000000000950. , 405405. Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2010.
Measurements
• The prevalence of smoking will be addressed according to the most recent population surveys in Brazil: the ELSA-Brasil Study; the PNS 2019 (containing estimates for the population aged 18 years and over); the PeNSE 2015 Survey, containing estimates for teenagers aged 13 to 15 years; the ERICA Study, which included 74 589 adolescents aged 12 to 17 years, from municipalities with over 100 000 inhabitants; and trend estimates for adults in the Brazilian capitals between 2006 and 2019. 401401. Benziger CP, Roth GA, Moran AE. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob Heart. 2016;11(4):393-7. doi: 10.1016/j.gheart.2016.10.024. , 409409. GBD 2015 Tobacco Collaborators. Smoking Prevalence and Attributable Disease Burden in 195 Countries and Territories, 1990-2015: A Systematic Analysis From the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885-906. doi: 10.1016/S0140-6736(17)30819-X.
https://doi.org/10.1016/S0140-6736(17)30...
, 410410. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde do Escolar: 2015. Rio de Janeiro: IBGE; 2016.
• Mortality rates and adjusted hazard ratios of the association between smoking and death are shown in Brazilian cohorts. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
, 404404. Oberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide Burden of Disease From Exposure to Second-Hand Smoke: A Retrospective Analysis of Data From 192 Countries. Lancet. 2011;377(9760):139-46.
• Mortality rates and absolute numbers of deaths attributable to tobacco will be presented for Brazil and its 27 FUs in 1990 and 2019. Estimates are from the GBD Study 2019. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
Prevalence
Prevalence of tobacco use among adolescents
• Tables 11-1 to 11-3 show the prevalence of smoking indicators among adolescents of the ninth grade, aged 13 to 15 years, according to data from the PeNSE 2015 survey. 410410. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde do Escolar: 2015. Rio de Janeiro: IBGE; 2016.
• In addition, according to data from the PeNSE 2015 survey, 18.4% (95% CI, 17.8 - 19) of the adolescents aged 13 to 15 years have already tried cigarettes in their lifetime. The prevalence was higher among males (19.4%; 95% CI, 16.6 - 18.2) than among females (17.4%; 95% CI, 18.7 - 20.0). The share of adolescents who tried smoking ranged from 27.0% in Mato Grosso do Sul to 9.3% in Sergipe, being highest in the Southern (24.9%) and lowest in the Northeastern region. 410410. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde do Escolar: 2015. Rio de Janeiro: IBGE; 2016.
• The prevalence of current smoking or having smoked in the 30 days prior to the survey was 5.6% (95% CI, 5.3 - 5.9), with no difference according to sex (male 5.8%; 95% CI, 5.4 - 6.3; female 5.4%; 95% CI, 4.9 - 5.8). The use of other tobacco products was 6.1% (95% CI, 5.7 - 6.4) among male adolescents and 5.6% (95% CI, 5.1 - 6.0) among females. 410410. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde do Escolar: 2015. Rio de Janeiro: IBGE; 2016.
• The ERICA study, a cross-sectional, nationwide, school-based study of cardiovascular risks, included 74 589 adolescents aged 12 to 17 years, from municipalities with over 100 000 inhabitants. The results showed that 18.5% (95% CI, 17.7-19.4) of the adolescents had smoked at least once in life, 5.7% (95% CI, 5.3 - 6.2) smoked at the time of the research, and 2.5% (95% CI, 2.2 - 2.8) smoked often, without significant difference between sexes. 401401. Benziger CP, Roth GA, Moran AE. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob Heart. 2016;11(4):393-7. doi: 10.1016/j.gheart.2016.10.024.
• In the Southern region, there was a higher prevalence of experimenting with tobacco use (23.3%; 95% CI, 21.5 - 25.3), current tobacco use (7.3%; 95% CI, 6.2 - 8.7), and tobacco use for 7 consecutive days (3.8%; 95% CI, 2.8 - 5.1) as compared to the Northern (19.2%, 5.9%, and 2.2%, respectively) and Northeastern regions (15.2%, 4.7%, and 1.5%, respectively).
• There was no statistically significant difference in the prevalence of tobacco use according to socioeconomic indicators (reported ethnicity, education level, mother’s education level, and father’s education level) for both sexes.
• The prevalence was higher among adolescents who had paid jobs in the year prior to the study, for both sexes [9.3% (95% CI, 8.1 - 10.5) vs 5.0% (95% CI, 4.3-5.6) for males; 8.8% (95% CI, 7.5 - 10.1) vs 4.6% (95% CI, 4.0-5.1) for females]. In addition, there was a higher prevalence among those who did not live with both parents as compared to those who did [8.0% (95% CI, 6.8 - 9.2) vs 4.8% (95% CI, 4.0-5.5) for males; 6.4% (95% CI, 5.7 – 7.1) vs 4.4% (95% CI, 3.8 - 5.1) for females].
• Females attending public schools reported smoking more often [5.7% (95% CI, 5.1 - 6.2)] than those from private schools [3.7% (95% CI, 2.3 - 5.1)]. In the male sex, the difference was not significant, 6.1% (95% CI, 5.6 - 6.9) and 5.2% (95% CI, 3.5 - 7.0), respectively.
• Adolescents having the presence of smokers at home had a higher prevalence of smoking, 8.1% (95% CI, 6.7 - 9.6) vs no presence, 5.4% (95% CI, 4.7 - 6.1), for males, and 7.1% (95% CI, 6.2 - 8.0) vs no presence, 4.5% (95% CI, 4.0 - 5.1), for females. Furthermore, a higher prevalence was seen in those in contact with smokers outside home: males, 9.9% (95% CI, 8.6 - 11.1) vs 3.6% (95% CI, 3.0 - 4.3); and females, 7.6% (95% CI, 6.8 - 8.4) vs 2.7% (95% CI, 2.2 - 3.3).
Prevalence of tobacco use among adults
• PNS 2019 data, identified in Table 11-4, indicate that 12.8% (95% CI, 12.4 - 13.2) of adults use some tobacco product, being the use higher among males (16.2%; 95% CI, 15.6 - 16.9), than among females (9.9%; 95% CI, 9.3 - 10.3). 306306. Brasil. Ministério da Saúde. Pesquisa Nacional de Saúde: 2019: Percepção do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal - Brasil e Grandes Regiões. Brasília: IBGE; 2020.
• The prevalence of some tobacco product use is higher in the rural area (14.3%) than in the urban area (12.6%), as well as higher in the Southern (14.7%) than in the Northern (10.7%) region.
• The proportion of tobacco smokers over 18 years of age in 2019 was 12.6% (95% CI, 12.2 - 13.0), and, according to sex, 15.9% (95% CI, 15.3 - 16.6) of males and 9.6% (95% CI, 9.2 - 10.1) of females (Table 11-1). 306306. Brasil. Ministério da Saúde. Pesquisa Nacional de Saúde: 2019: Percepção do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal - Brasil e Grandes Regiões. Brasília: IBGE; 2020. Regarding age groups, the prevalence was as follows, from the highest to the lowest: 14.9% (95% CI, 14.2 - 15.5) in the 40-59 years group; 10.8% (95% CI, 9.6 - 12.0) in the 18-24 years group; 12.0% (95% CI, 11.2 - 12.7) in the 25-39 years group; and 11.9% (95% CI, 11.2 - 12.6) in the 60 years or older group (Table 11-5). 306306. Brasil. Ministério da Saúde. Pesquisa Nacional de Saúde: 2019: Percepção do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal - Brasil e Grandes Regiões. Brasília: IBGE; 2020.
• The prevalence is lower in populations with higher education and income, being 17.6% (95% CI, 16.8 - 18.4) among those without education or with incomplete primary education, 15.5% (95% CI, 14.3 - 16.6) among those with complete primary education and incomplete secondary education, 9.6% (95% CI, 8.9 - 10.2) among individuals with complete secondary education and incomplete college education, and 7.1% (95% CI, 6.3 - 7.8) among those with complete college education (Table 11-7). 306306. Brasil. Ministério da Saúde. Pesquisa Nacional de Saúde: 2019: Percepção do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal - Brasil e Grandes Regiões. Brasília: IBGE; 2020.
• The prevalence of smoking was higher among black individuals (13.7%; 95% CI, 12.5 - 15) as compared to “pardos” or mixed race involving African ancestry (13.5%; 95% CI, 12.9 - 14.2) and white individuals (11.8%; 95% CI, 11.2 - 12.4) (Table 11-8). 306306. Brasil. Ministério da Saúde. Pesquisa Nacional de Saúde: 2019: Percepção do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal - Brasil e Grandes Regiões. Brasília: IBGE; 2020.
• The Vigitel 2019 showed a frequency of adult smokers of 9.8%, higher in males (12.3%) than in females (7.7%). In the total population, the frequency of smokers tended to be lower among young adults (less than 25 years of age) and among those aged 65 years and over. The frequency of smoking decreased with increasing schooling, and was particularly high among men with up to 8 years of schooling (16.8%). 410410. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde do Escolar: 2015. Rio de Janeiro: IBGE; 2016.
• According to the GBD Study 2019, in Brazil, the prevalence of secondhand smoke at home is 9.2% (95% UI, 8.8 - 9.8%), higher among females (10.2%; 95% CI, 8.7 - 10.8%) than among males (7.9%; 95% UI, 7.3 - 8.5%). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• The prevalence of secondhand smoke at work is 8.4% (95% CI, 8.8 - 9.8), higher among males (10.4%; 95% CI, 9.4 - 11.3) than among females (8.7%; 95% CI, 6.1 - 7.4) (Table 11-12). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• The use of electronic cigarettes was measured for the first time in the PNS 2019, revealing a prevalence of 0.6%, with greater electronic cigarette use in the Distrito Federal (2.2%) and in the states of Mato Grosso do Sul (2.1%) and Paraná (2.1%) (Table 11-13). 405405. Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2010.
Prevalence trend
• The prevalence obtained in the main national household surveys, in the Vigitel telephone survey for participants aged 18 years or older, and in the PNS points to a significant decrease in the prevalence of smoking in the adult population, with a 37.6% reduction from 2006 to 2019. This trend is similar to that found in other national studies (Table 11-9, Chart 11-1). 306306. Brasil. Ministério da Saúde. Pesquisa Nacional de Saúde: 2019: Percepção do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal - Brasil e Grandes Regiões. Brasília: IBGE; 2020. , 400400. Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2. , 410410. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde do Escolar: 2015. Rio de Janeiro: IBGE; 2016. , 411411. Brasil. Ministério da Saúde. Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília: Ministério da Saúde; 2018. However, the index is 0.5% higher than that calculated in 2018.
• According to Vigitel data, in the Brazilian capitals, between 2006 and 2019, there was a decline in smoking for both sexes. After 2015, the decline was smaller, even with stability for males (Table 11-9 and Chart 11-2). 400400. Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2. , 411411. Brasil. Ministério da Saúde. Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília: Ministério da Saúde; 2018.
• Among adolescents, in comparison with the PeNSE 2012 survey, the prevalence of current smoking remained unchanged at 5.0% (2012) and 5.6% (2015). However, the use of other tobacco products increased from 4.8% (95% CI, 4.6 - 5.0) in 2012 to 6.1% (95% CI, 5.7 - 6.4) in 2015, with a higher proportion among males. Cigarette smoking together with the use of other tobacco products increased by 18%, from 7.6% (2012) to 9.0% (2015). The hookah was the most used product in 2015 (71.6%; 95% CI, 68.8 - 74.2), being more frequent among females (4% among male adolescents and 5.6% among female adolescents). 405405. Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2010. , 412412. Malta DC, Hallal ALC, Machado ÍE, Prado RRD, Oliveira PPV, Campos MO, Souza MFM. Factors Associated With the use of Waterpipe and other Tobacco Products Among Students, Brazil, 2015. Rev Bras Epidemiol. 2018;21(Suppl 1):e180006. doi: 10.1590/1980-549720180006.supl.1.
• According to the GBD Study 2019, passive smoking deaths decreased between 1990 and 2019. The main causes of passive smoking death from CVD were ischemic heart disease and stroke. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
In 1990, there were 7489 (5.03 per 100 000 inhabitants) deaths from ischemic heart disease due to secondhand smoke and, in 2019, there were 6934 deaths (3.2 per 100 000 inhabitants). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
In 1990, there were 4400 (2.96 per 100 000 inhabitants) deaths from stroke due to secondhand smoke and, in 2019, it decreased to 3219 (1.3 per 100 000 inhabitants). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
Mortality
Tobacco and total mortality
•Table 11-10 shows the age-standardized rate of deaths (per 100 000 inhabitants) attributed to tobacco, and the percent change of rates by sex between 1990 and 2019, in Brazil and each FU. Table 11-11 shows the number and age-standardized rate of deaths attributed to tobacco and percent change of rates. These data were estimated by the GBD considering the existing literature and the population attributable fraction due to smoking, that is, the proportion of cases attributed to tobacco use (Chart 11-3). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• According to GBD data in 1990, the absolute number of deaths attributed to tobacco was 168 443 (95% UI, 159 638 – 176 773) and in 2019 it increased to 191 127 (95% UI, 180 887 – 202 595) deaths (Table 11-11). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• The absolute number of deaths attributed to tobacco increased, mainly due to population aging and growth; however, there was a reduction by 58.8% (95% UI, 56.3 - 61.1) in mortality rates attributable to smoking, from 199.9 per 100 000 inhabitants (95% UI, 189.1 - 210.6) in 1990 to 82.4 per 100 000 inhabitants (95% UI, 77.9 - 87.5) in 2019 (Table 11-11). This reduction occurred due to the reduction in risk or the prevalence of smokers. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• Mortality rates due to tobacco decreased in all Brazilian FUs and, in 2019, the highest mortality rate attributable to smoking was found in the states of Rio Grande do Sul (104.6; 95% UI, 94.4 -115.9), Acre (99.8; 95% UI, 89.7 - 109.8), and Pernambuco (97.7; 95% UI, 87 - 108.7). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• Chart 11-4 shows the Proportional mortality attributable to tobacco by age group. The proportion is highest among men, aged 60 to 74 years, male.
• Chart 11-5 shows the absolute numbers of deaths attributed to tobacco and secondhand smoke. The use of smoked tobacco has contributed to more than 190 000 deaths from NCDs and others, including CVD (65 693), cancer (53 000: lungs, oral cavity, breast), chronic respiratory diseases, infectious respiratory diseases and tuberculosis, diabetes, digestive diseases, kidney diseases (Charts 11-5 and 11-6). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
Tobacco and CVD mortality
• Analysis of the specific causes of deaths attributable to smoking indicates that CVD mortality decreased from 88.0 per 100 000 inhabitants (95% UI, 81.3 - 94.3) in 1990 to 26.3 per 100 000 inhabitants (95% CI, 23.8 - 28.9) in 2019. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• In 2019, smoking was responsible for 65 696 deaths from CVD. In addition, there was a decrease in the mortality rates of some CVDs attributable to smoking, such as ischemic heart disease and stroke, in the studied period (Charts 11-7 and 11-8). 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
Among CVDs, the greatest reduction in mortality attributed to smoking was observed for ischemic heart disease. There was a reduction from 41 564 deaths [47.2 (95% UI, 43.8 - 50.4) per 100 000 inhabitants] in 1990 to 35 218 deaths [14.7 (95% UI, 16.0 - 13.5) per 100 000 inhabitants] in 2019. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• Stroke deaths decreased from 28 468 [31.8 (95% UI, 29.0 - 34.8) per 100 000 inhabitants] in 1990 to 17 577 [7.4 (95% UI, 6.6 - 8.3) per 100 000 inhabitants] in 2019. The deaths from aortic aneurysm increased from 1678 [7.4 (95% UI, 1.7 - 2.0) per 100 000 inhabitants] in 1990 to 3999 [1.7 (95% UI, 1.5 - 1.9) per 100 000 inhabitants] in 2019, and the deaths from peripheral arterial diseases increased from 343 [0.4 (95% UI, 0.2 - 0.8) per 100 000 inhabitants] in 1990 to 674 [0.3 (95% UI, 0.1 - 0.6) per 100 000 inhabitants] in 2019. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• Overall, larger reductions in smoking-attributable mortality rates were observed in the FUs with higher SDI, with the highest declines observed in those with high SDI (Distrito Federal, Rio de Janeiro, São Paulo, Santa Catarina, Paraná, Minas Gerais) and the smallest reductions in the UFs of the Northern and Northeastern regions of Brazil, with lower SDIs (Rio Grande do Norte, Ceará, Bahia, Pará, Paraíba) (Pearson correlation: 0.637; p < 0.001) (Chart 11-9). 3434. Baptista E, Queiroz B, Rigotti J. Decomposition of Mortality Rates From Cardiovascular Disease in the Adult Population: A Study for Brazilian Micro-Regions Between 1996 and 2015. Rev. Bras. Estud. Popul. 2018;35(2):e00050. doi: 10.20947/S102-3098a0050.
Burden of Disease
Tobacco total burden of disease
• Charts 11-10, 11-11 and 11-12 show the trends from 1990 to 2019 for the metrics YLLs, YLDs and DALYs. In all situations, crude and age-standardized rates declined. 1919. GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
https://doi.org/10.1016/S0140-6736(20)30...
• GBD 2019 data estimated a reduction in the age-standardized DALY rate attributable to tobacco per 100 000 inhabitants in Brazil by 59% (95% UI, 56% - 61%) between 1990 [4614.5 (95% UI, 4372.3 - 4888.0)] and 2019 [1893.7 (95% UI, 1768.6 - 2028.0)]. The differences in the curves in Chart 11-12 reflect DALYs adjusted for differences in the age distribution of the population, with the ‘all ages’ curve driven mainly by a combination of population growth and aging.
• The reduction in DALY rates is a consequence of the decrease in YLLs by 61% (95% UI, 58 - 63%) between 1990 and 2019. In both instances, a combination of reduced smoking exposure and reduced risk-deleted DALY rates contributed to overall reductions.
• There was a heterogeneous reduction in age-standardized DALYs attributed to tobacco in the different FUs and regions of Brazil, more pronounced in the Southeastern, Southern and West-Central FUs, with a modest reduction in the Northern FUs and an even more discreet reduction in most Northeastern FUs.
Tobacco cardiovascular burden of disease
• GBD 2019 data estimated age-standardized DALY rates attributable to tobacco per 100 000 inhabitants in Brazil of 650 (95% UI, 604 - 701), a reduction of 69% (95% UI, 67 - 71) as compared to the 1990 age-standardized DALY rate, 2124 (95% UI, 1993 - 2254).
• The age-standardized YLL rates per 100 000 inhabitants were 2040 (95% UI, 1919 - 2164) in 1990 and 611 (95% UI, 568 - 657) in 2019, a reduction of 70% (95% UI, 68% - 72%) in the period.
• The age-standardized YLD rates per 100 000 inhabitants were 84 (95% UI, 60 - 108) in 1990 and 39 (95% UI, 28 - 51) in 2019, a reduction of 54% (95% UI, 50-57%).
Economic Impact of Tobacco
In Brazil, the economic impact of tobacco, including the direct cost (costs of diagnosis, treatment, and follow-up), was recently estimated using a developed probabilistic microsimulation economic model of the natural history, medical costs, and quality-of-life losses associated with the most common tobacco-related diseases. Data inputs were obtained through literature review, vital statistics, and hospital databases. Chronic obstructive pulmonary diseases, CVD, lung cancer, and stroke accounted for 78% of that cost. In 2015, the total direct cost of tobacco was estimated at US$ 11.8 billion per year, 70% corresponding to the direct cost associated with health care and the remainder associated with the indirect cost due to the loss of productivity due to premature death and inability. Tobacco represented 22% of the direct costs of CVD in Brazil and 17% of the direct costs of stroke. The cost attributed to secondhand smoke was US$ 1.36 billion. 413413. Pichon-Riviere A, Alcaraz A, Palacios A, Rodríguez B, Reynales-Shigematsu LM, Pinto M, Castillo-Riquelme M, Peña Torres E, Osorio DI, Huayanay L, Loza Munarriz C, de Miera-Juárez BS, Gallegos-Rivero V, De La Puente C, Del Pilar Navia-Bueno M, Caporale J, Roberti J, Virgilio SA, Augustovski F, Bardach A. The Health and Economic Burden of Smoking in 12 Latin American Countries and the Potential Effect of Increasing Tobacco Taxes: An Economic Modelling Study. Lancet Glob Health. 2020;8(10):1282-94. doi: 10.1016/S2214-109X(20)30311-9. , 414414. Pinto M, Bardach A, Palacios A, Biz A, Alcaraz A, Rodriguez B, Augustovski F, Pichon-Riviere A. Burden of Smoking in Brazil and Potential Benefit of Increasing Taxes on Cigarettes for the Economy and for Reducing Morbidity and Mortality. Cad Saude Publica. 2019;35(8):e00129118. doi: 10.1590/0102-311X00129118.
The health costs attributed to the use of tobacco represent an estimate of 5.7% of all government spending on health and 0.7% of the gross domestic product. It is estimated that, in Brazil, 25.6% of the resources spent are recovered through taxes on tobacco. 413413. Pichon-Riviere A, Alcaraz A, Palacios A, Rodríguez B, Reynales-Shigematsu LM, Pinto M, Castillo-Riquelme M, Peña Torres E, Osorio DI, Huayanay L, Loza Munarriz C, de Miera-Juárez BS, Gallegos-Rivero V, De La Puente C, Del Pilar Navia-Bueno M, Caporale J, Roberti J, Virgilio SA, Augustovski F, Bardach A. The Health and Economic Burden of Smoking in 12 Latin American Countries and the Potential Effect of Increasing Tobacco Taxes: An Economic Modelling Study. Lancet Glob Health. 2020;8(10):1282-94. doi: 10.1016/S2214-109X(20)30311-9. , 414414. Pinto M, Bardach A, Palacios A, Biz A, Alcaraz A, Rodriguez B, Augustovski F, Pichon-Riviere A. Burden of Smoking in Brazil and Potential Benefit of Increasing Taxes on Cigarettes for the Economy and for Reducing Morbidity and Mortality. Cad Saude Publica. 2019;35(8):e00129118. doi: 10.1590/0102-311X00129118.
Future Research
Due to the lack of longitudinal data, the long-term CVD risks associated with e-cigarette use are unknown. Limited information on the health risks of electronic tobacco products is currently available. More research and extended follow-up are still necessary because e-cigarette, including electronic hookah use, have become prevalent among youth.
Finally, despite the positive results of the tobacco control program, advances in tobacco control are still necessary in the country. The following steps include regulatory measures (price/taxation increase, warning spaces on the packaging, adoption of plain packaging), social measures (support for small farmers to move forward from replacing tobacco cultivation with other crops), and legal actions (supervision of tobacco products, border control and combat of illegal trade, support policies to create tobacco control funds to compensate for smoking-related healthcare costs at federal and subnational level).
Referências
-
1Oliveira GMM, Brant LCC, Polanczyk CA, Biolo A, Nascimento BR, Malta DC, Souza MFM, Soares GP, Xavier GF Jr, Machline-Carrion MJ, Bittencourt MS, Pontes Neto OM, Silvestre OM, Teixeira RA, Sampaio RO, Gaziano TA, Roth GA, Ribeiro ALP. Cardiovascular Statistics - Brazil 2020. Arq Bras Cardiol. 2020;115(3):308-439. doi: 10.36660/abc.20200812.
-
2Malta DC, Passos VMA, Machado ÍE, Marinho Souza MF, Ribeiro ALP. The GBD Brazil Network: Better Information for Health Policy Decision-Making in Brazil. Popul Health Metr. 2020;18(Suppl 1):23. doi: 10.1186/s12963-020-00224-1.
-
3Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):254-743. doi: 10.1161/CIR.0000000000000950.
-
4Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010.
-
5Shemilt I, Thomas J, Morciano M. A Web-Based Tool for Adjusting Costs to a Specific Target Currency and Price Year. Evid. Policy. 2010;6(1):51-9. doi:10.1332/174426410X482999.
-
6Malta DC, Teixeira R, Oliveira GMM, Ribeiro ALP. Cardiovascular Disease Mortality According to the Brazilian Information System on Mortality and the Global Burden of Disease Study Estimates in Brazil, 2000-2017. Arq Bras Cardiol. 2020;115(2):152-160. doi: 10.36660/abc.20190867.
» https://doi.org/10.36660/abc.20190867 -
7Castro MC, Massuda A, Almeida G, Menezes-Filho NA, Andrade MV, Noronha KVMS, Rocha R, Macinko J, Hone T, Tasca R, Giovanella L, Malik AM, Werneck H, Fachini LA, Atun R. Brazil’s Unified Health System: The First 30 Years and Prospects for the Future. Lancet. 2019;394(10195):345-56. doi: 10.1016/S0140-6736(19)31243-7.
-
8Ribeiro ALP, Duncan BB, Brant LCC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular Health in Brazil: Trends and Perspectives. Circulation. 2016;133(4): 422-33. doi: https://doi.org/10.1161/CIRCULATIONAHA.114.008727 .
» https://doi.org/10.1161/CIRCULATIONAHA.114.008727 -
9Ribeiro ALP, Oliveira GMM. Toward a Patient-Centered, Data-Driven Cardiology. Arq Bras Cardiol. 2019;112(4):371-3. doi: 10.5935/abc.20190069.
-
10Brasil. Ministério da Saúde. Manual de Instruções para o Preenchimento da Declaração de Óbito. Brasília: Ministério da Saúde; 2011.
-
11Jorge MH, Laurenti R, Gotlieb SL. Análise da Qualidade das Estatísticas Vitais Brasileiras: A Experiência de Implantação do SIM e do SINASC. Cien Saude Colet. 2007;12(3):643-54. doi: 10.1590/s1413-81232007000300014.
-
12França E, Abreu DX, Rao C, Lopez AD. Evaluation of Cause-of-Death Statistics for Brazil, 2002-2004. Int J Epidemiol. 2008;37(4):891-901. doi: 10.1093/ije/dyn121.
-
13Escosteguy CC, Portela MC, Medronho RA, Vasconcellos MT. O Sistema de Informações Hospitalares e a Assistência ao Infarto Agudo do Miocárdio. Rev Saude Publica. 2002;36(4):491-9. doi: 10.1590/s0034-89102002000400016.
-
14Rocha TAH, Silva NCD, Amaral PVM, Barbosa ACQ, Vissoci JRN, Thomaz EBAF, Queiroz RCS, Harris M, Facchini LA. Geolocation of Hospitalizations Registered on the Brazilian National Health System’s Hospital Information System: A Solution Based on the R Statistical Software. Epidemiol Serv Saude. 2018;27(4):e2017444. doi: 10.5123/S1679-49742018000400016.
-
15Malta DC, Stopa SR, Szwarcwald CL, Gomes NL, Silva JB Jr, Reis AA. Surveillance and Monitoring of Major Chronic Diseases in Brazil - National Health Survey, 2013. Rev Bras Epidemiol. 2015;18(Suppl 2):3-16. doi: 10.1590/1980-5497201500060002.
-
16GBD 2019 Viewpoint Collaborators. Five Insights From the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1135-59. doi: 10.1016/S0140-6736(20)31404-5.
» https://doi.org/10.1016/S0140-6736(20)31404-5 -
17GBD 2019 Demographics Collaborators. Global Age-Sex-Specific Fertility, Mortality, Healthy Life Expectancy (HALE), and Population Estimates in 204 Countries and Territories, 1950-2019: A Comprehensive Demographic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1160-203. doi: 10.1016/S0140-6736(20)30977-6.
» https://doi.org/10.1016/S0140-6736(20)30977-6 -
18GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-22. doi: 10.1016/S0140-6736(20)30925-9.
» https://doi.org/10.1016/S0140-6736(20)30925-9 -
19GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223-49. doi: 10.1016/S0140-6736(20)30752-2.
» https://doi.org/10.1016/S0140-6736(20)30752-2 -
20França EB, Passos VMA, Malta DC, Duncan BB, Ribeiro ALP, Guimarães MDC, Abreu DMX, Vasconcelos AMN, Carneiro M, Teixeira R, Camargos P, Melo APS, Queiroz BL, Schmidt MI, Ishitani L, Ladeira RM, Morais-Neto OL, Bustamante-Teixeira MT, Guerra MR, Bensenor I, Lotufo P, Mooney M, Naghavi M. Cause-Specific Mortality for 249 Causes in Brazil and States During 1990-2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Popul Health Metr. 2017;15(1):39. doi: 10.1186/s12963-017-0156-y.
-
21GBD 2016 Brazil Collaborators. Burden of Disease in Brazil, 1990-2016: A Systematic Subnational Analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10149):760-75. doi: 10.1016/S0140-6736(18)31221-2.
» https://doi.org/10.1016/S0140-6736(18)31221-2 -
22Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for Enhancing Public Health Utility of National Causes-of-Death Data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9.
-
23World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013-2020. Geneva: WHO Library Cataloguing-In-Publication Data; 2013.
-
24Alves CG, Morais Neto OL. Trends in Premature Mortality Due to Chronic Non-Communicable Diseases in Brazilian Federal Units. Cien Saude Colet. 2015;20(3):641-54. doi: 10.1590/1413-81232015203.15342014.
-
25Duncan BB, Chor D, Aquino EM, Bensenor IM, Mill JG, Schmidt MI, Lotufo PA, Vigo A, Barreto SM. Doenças Crônicas Não Transmissíveis no Brasil: Prioridade para Enfrentamento e Investigação. Rev Saude Publica. 2012;46(Suppl 1):126-34. doi: 10.1590/s0034-89102012000700017.
-
26Malta DC, França E, Abreu DMX, Perillo RD, Salmen MC, Teixeira RA, Passos V, Souza MFM, Mooney M, Naghavi M. Mortality Due to Noncommunicable Diseases in Brazil, 1990 to 2015, According to Estimates From the Global Burden of Disease study. Sao Paulo Med J. 2017;135(3):213-21. doi: 10.1590/1516-3180.2016.0330050117.
-
27Nascimento BR, Brant LCC, Oliveira GMM, Malachias MVB, Reis GMA, Teixeira RA, Malta DC, França E, Souza MFM, Roth GA, Ribeiro ALP. Cardiovascular Disease Epidemiology in Portuguese-Speaking Countries: data From the Global Burden of Disease, 1990 to 2016. Arq Bras Cardiol. 2018;110(6):500-11. doi: 10.5935/abc.20180098.
-
28Malta DC, Bernal RT, Souza MF, Szwarcwald CL, Lima MG, Barros MB. Social Inequalities in the Prevalence of Self-Reported Chronic Non-Communicable Diseases in Brazil: National Health Survey 2013. Int J Equity Health. 2016;15(1):153. doi: 10.1186/s12939-016-0427-4.
-
29Brant LCC, Nascimento BR, Passos VMA, Duncan BB, Bensenõr IJM, Malta DC, Souza MFM, Ishitani LH, França E, Oliveira MS, Mooney M, Naghavi M, Roth G, Ribeiro ALP. Variations and Particularities in Cardiovascular Disease Mortality in Brazil and Brazilian States in 1990 and 2015: Estimates From the Global Burden of Disease. Rev Bras Epidemiol. 2017;20(Suppl 01):116-28. doi: 10.1590/1980-5497201700050010.
-
30Gonçalves RPF, Haikal DS, Freitas MIF, Machado ÍE, Malta DC. Self-Reported Medical Diagnosis of Heart Disease and Associated Risk Factors: National Health Survey. Rev Bras Epidemiol. 2019;22(Suppl 2):E190016.SUPL.2. doi:10.1590/1980-549720190016.supl.2.
-
31Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM, Aquino EM, Passos VM, Matos SM, Molina Mdel C, Carvalho MS, Bensenor IM. Cohort Profile: Longitudinal Study of Adult Health (ELSA-Brasil). Int J Epidemiol. 2015;44(1):68-75. doi: 10.1093/ije/dyu027.
-
32Massa KHC, Duarte YAO, Chiavegatto Filho ADP. Análise da Prevalência de Doenças Cardiovasculares e Fatores Associados em Idosos, 2000-2010. Cien Saude Colet. 2019;24(1):105-14. doi: 10.1590/1413-81232018241.02072017.
-
33Mansur AP, Favarato D. Mortality Due to Cardiovascular Diseases in Women and Men in the Five Brazilian Regions, 1980-2012. Arq Bras Cardiol. 2016;107(2):137-46. doi: 10.5935/abc.20160102.
-
34Baptista E, Queiroz B, Rigotti J. Decomposition of Mortality Rates From Cardiovascular Disease in the Adult Population: A Study for Brazilian Micro-Regions Between 1996 and 2015. Rev. Bras. Estud. Popul. 2018;35(2):e00050. doi: 10.20947/S102-3098a0050.
-
35Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of Primary Health Care on Mortality From Heart and Cerebrovascular Diseases in Brazil: A Nationwide Analysis of Longitudinal Data. BMJ. 2014;349:g4014. doi: 10.1136/bmj.g4014.
-
36Lotufo PA. Trends in Cardiovascular Diseases and Heart Disease Death Rates Among Adults Aged 45-64: Brazil, 2000-2017. Sao Paulo Med J. 2019;137(3):213-5. doi: 10.1590/1516-3180.2019.1373.220719.
-
37Villela PB, Klein CH, de Oliveira GMM. Socioeconomic factors and mortality due to cerebrovascular and hypertensive disease in Brazil. Rev Port Cardiol. 2019;38(3):205-12. doi: 10.1016/j.repc.2018.07.007.
-
38Soares GP, Klein CH, Silva NA, Oliveira GM. Progression of Mortality due to Diseases of the Circulatory System and Human Development Index in Rio de Janeiro Municipalities. Arq Bras Cardiol. 2016;107(4):314-22. doi: 10.5935/abc.20160141.
-
39Soares GP, Brum JD, Oliveira GM, Klein CH, Silva NAS. Evolution of Socioeconomic Indicators and Cardiovascular Mortality in Three Brazilian States. Arq Bras Cardiol. 2013;100(2):147-56. doi: 10.5935/abc.20130028.
-
40Lotufo PA, Fernandes TG, Bando DH, Alencar AP, Benseñor IM. Income and Heart Disease Mortality Trends in Sao Paulo, Brazil, 1996 to 2010. Int J Cardiol. 2013;167(6):2820-3. doi: 10.1016/j.ijcard.2012.07.006.
-
41Baptista E, Queiroz B. The Relation Between Cardiovascular Mortality and Development: Study for Small Areas in Brazil, 2001–2015. Demographic Res. 2019;41(51):1437-52. doi: 10.4054/DemRes.2019.41.51.
-
42Silveira IH, Oliveira BFA, Cortes TR, Junger WL. The Effect of Ambient Temperature on Cardiovascular Mortality in 27 Brazilian Cities. Sci Total Environ. 2019;691:996-1004. doi: 10.1016/j.scitotenv.2019.06.493.
-
43Brasil. Ministério da Saúde. DATASUS. Informações de Saúde, Morbidade e Informações Epidemiológicas [Internet]. Brasília: Ministério da Saúde; 2016 [cited 2021 Nov 09]. Available From: http://datasus.saude.gov.br/informacoes-de-saude/tabnet/epidemiologica .
» http://datasus.saude.gov.br/informacoes-de-saude/tabnet/epidemiologica -
44Frias PG, Szwarcwald CL, Morais Neto OL, Leal MD, Cortez-Escalante JJ, Souza PR Jr, Almeida WD, Silva JB Jr. Utilização das Informações Vitais para a Estimação de Indicadores de Mortalidade no Brasil: Da Busca Ativa de Eventos ao Desenvolvimento de Métodos. Cad Saude Publica. 2017;33(3):e00206015. doi: 10.1590/0102-311X00206015.
-
45Almeida WDS, Szwarcwald CL. Adequacy of Mortality Data and Correction of Reported Deaths From the Proactive Search of Deaths. Cien Saude Colet. 2017;22(10):3193-203. doi: 10.1590/1413-812320172210.12002016.
-
46Global Burden of Disease Study 2019 (GBD 2019) Results. Global Health Data Exchange website [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME) [cited 2021 Nov 09]. Available From: http://ghdx.healt .
» http://ghdx.healt -
47Abe IM, Lotufo PA, Goulart AC, Benseñor IM. Stroke Prevalence in a Poor Neighbourhood of São Paulo, Brazil: Applying a Stroke Symptom Questionnaire. Int J Stroke. 2011;6(1):33-9. doi: 10.1111/j.1747-4949.2010.00538.x.
-
48Fernandes TG, Benseñor IM, Goulart AC, Tavares BM, Alencar AP, Santos IS, Lotufo PA. Stroke in the Rain Forest: Prevalence in a Ribeirinha Community and an Urban Population in the Brazilian Amazon. Neuroepidemiology. 2014;42(4):235-42. doi: 10.1159/000362210.
-
49Goulart AC, Bustos IR, Abe IM, Pereira AC, Fedeli LM, Benseñor IM, Lotufo PA. A Stepwise Approach to Stroke Surveillance in Brazil: The EMMA (Estudo de Mortalidade e Morbidade do Acidente Vascular Cerebral) Study. Int J Stroke. 2010;5(4):284-9. doi: 10.1111/j.1747-4949.2010.00441.x.
-
50Bensenor IM, Goulart AC, Szwarcwald CL, Vieira ML, Malta DC, Lotufo PA. Prevalence of Stroke and Associated Disability in Brazil: National Health Survey--2013. Arq Neuropsiquiatr. 2015;73(9):746-50. doi: 10.1590/0004-282X20150115.
-
51Cabral NL, Cougo-Pinto PT, Magalhaes PS, Longo AL, Moro CH, Amaral CH, Costa G, Reis FI, Gonçalves AR, Nagel V, Pontes-Neto OM. Trends of Stroke Incidence From 1995 to 2013 in Joinville, Brazil. Neuroepidemiology. 2016;46(4):273-81. doi: 10.1159/000445060.
-
52Cabral NL, Gonçalves AR, Longo AL, Moro CH, Costa G, Amaral CH, Souza MV, Eluf-Neto J, Fonseca LA. Trends in Stroke Incidence, Mortality and Case Fatality Rates in Joinville, Brazil: 1995-2006. J Neurol Neurosurg Psychiatry. 2009;80(7):749-54. doi: 10.1136/jnnp.2008.164475.
-
53Minelli C, Cabral NL, Ujikawa LT, Borsetti Neto FA, Chiozzini EML, Reis GC, Borin LA, Carvalho CC. Trends in the Incidence and Mortality of Stroke in Matão, Brazil: The Matão Preventing Stroke (MAPS) Study. Neuroepidemiology. 2020;54(1):75-82. doi: 10.1159/000503005.
-
54Minelli C, Fen LF, Minelli DP. Stroke Incidence, Prognosis, 30-Day, and 1-Year Case Fatality Rates in Matão, Brazil: A Population-Based Prospective Study. Stroke. 2007;38(11):2906-11. doi: 10.1161/STROKEAHA.107.484139.
-
55Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, Ribeiro ALP, Bensenõr IJM. Cerebrovascular Disease in Brazil From 1990 to 2015: Global Burden of Disease 2015. Rev Bras Epidemiol. 2017;20(Suppl 1):129-141. doi: 10.1590/1980-5497201700050011.
-
56Passos VM, Ishitani LH, Franco GC, Lana GC, Abreu DM, Marinho MF, França EB. Consistent Declining Trends in Stroke Mortality in Brazil: Mission Accomplished? Arq Neuropsiquiatr. 2016;74(5):376-81. doi: 10.1590/0004-282X20160055.
-
57Guimarães RM, Andrade SS, Machado EL, Bahia CA, Oliveira MM, Jacques FV. Diferenças regionais na transição da mortalidade por doenças cardiovasculares no Brasil, 1980 a 2012. Rev Panam Salud Publica. 2015;37(2):83-9.
-
58Fernandes TG, Bando DH, Alencar AP, Benseñor IM, Lotufo PA. Income Inequalities and Stroke Mortality Trends in Sao Paulo, Brazil, 1996-2011. Int J Stroke. 2015;10(100):34-7. doi: 10.1111/ijs.12526.
-
59Katz M, Bosworth HB, Lopes RD, Dupre ME, Morita F, Pereira C, Franco FG, Prado RR, Pesaro AE, Wajngarten M. A Time-Series Analysis of the Relation Between Unemployment Rate and Hospital Admission for Acute Myocardial Infarction and Stroke in Brazil Over More Than a Decade. Int J Cardiol. 2016;224:33-6. doi: 10.1016/j.ijcard.2016.08.309.
-
60Adami F, Figueiredo FW, Paiva LS, Sá TH, Santos EF, Martins BL, Valenti VE, Abreu LC. Mortality and Incidence of Hospital Admissions for Stroke among Brazilians Aged 15 to 49 Years between 2008 and 2012. PLoS One. 2016;11(6):e0152739. doi: 10.1371/journal.pone.0152739.
-
61Dantas LF, Marchesi JF, Peres IT, Hamacher S, Bozza FA, Neira RAQ. Public Hospitalizations for Stroke in Brazil From 2009 to 2016. PLoS One. 2019;14(3):e0213837. doi: 10.1371/journal.pone.0213837.
-
62Rossetto C, Soares JV, Brandão ML, Rosa NGD, Rosset I. Causes of Hospital Admissions and Deaths Among Brazilian Elders Between 2005 and 2015. Rev Gaucha Enferm. 2019;40:e20190201. doi: 10.1590/1983-1447.2019.20190201.
-
63Pimenta L, Dutra VGP, Castro ALB, Guimarães RM. Analysis of Conditions Sensitive to Primary Care in a Successful Experience of Primary Healthcare Expansion in Brazil, 1998-2015. Public Health. 2018;162:32-40. doi: 10.1016/j.puhe.2018.05.011.
-
64Santos EFS, Antunes JLF. Fatores Associados à Falta de Assistência Hospitalar nos Óbitos por Doença Cerebrovascular, São Paulo, Brasil: Análise Comparativa entre 1996-1998 e 2013-2015. Cad Saude Publica. 2020;36(4):e00227718. doi: 10.1590/0102-311X00227718.
-
65Carvalho JJ, Alves MB, Viana GÁ, Machado CB, Santos BF, Kanamura AH, Lottenberg CL, Neto MC, Silva GS. Stroke Epidemiology, Patterns of Management, and Outcomes in Fortaleza, Brazil: A Hospital-Based Multicenter Prospective Study. Stroke. 2011;42(12):3341-6. doi: 10.1161/STROKEAHA.111.626523.
-
66Alves MB, Silva GS, Miranda RCA, Massaud RM, Vaccari AMH, Cendoroglo-Neto M, Diccini S. Patterns of Care and Temporal Trends in Ischemic Stroke Management: A Brazilian Perspective. J Stroke Cerebrovasc Dis. 2017;26(10):2256-63. doi: 10.1016/j.jstrokecerebrovasdis.2017.05.008.
-
67Lange MC, Braga GP, Nóvak EM, Harger R, Felippe MJDB, Canever M, Dall’Asta I, Rauen J, Bazan R, Zetola V. Key Performance Indicators for Stroke From the Ministry of Health of Brazil: Benchmarking and Indicator Parameters. Arq Neuropsiquiatr. 2017;75(6):354-8. doi: 10.1590/0004-282X20170051.
-
68Nasi LA, Ferreira-Da-Silva AL, Martins SC, Furtado MV, Almeida AG, Brondani R, Wirth L, Kluck M, Polanczyk CA. Implementation of a Dedicated Cardiovascular and Stroke Unit in a Crowded Emergency Department of a Tertiary Public Hospital in Brazil: Effect on Mortality Rates. Acad Emerg Med. 2014;21(1):40-6. doi: 10.1111/acem.12291.
-
69Machline-Carrion MJ, Santucci EV, Damiani LP, Bahit MC, Málaga G, Pontes-Neto OM, Martins SCO, Zétola VF, Normilio-Silva K, Freitas GR, Gorgulho A, Salles A, Silva BGP, Santos JY, Jesuíno IA, Bueno PRT, Cavalcanti AB, Guimarães HP, Xian Y, Bettger JP, Lopes RD, Peterson ED, Berwanger O; BRIDGE-Stroke Investigators. Effect of a Quality Improvement Intervention on Adherence to Therapies for Patients With Acute Ischemic Stroke and Transient Ischemic Attack: A Cluster Randomized Clinical Trial. JAMA Neurol. 2019;76(8):932-41. doi: 10.1001/jamaneurol.2019.1012.
-
70Schmidt MH, Selau CM, Soares PS, Franchi EF, Piber VD, Quatrin LB. Acidente Vascular Cerebral e Diferentes Limitações: Uma Análise Interdisciplinar. Arq Ciênc Saúde UNIPAR. 2019;23(2):139-44. doi: 10.25110/arqsaude.v23i2.2019.6404.
-
71Carvalho-Pinto BP, Faria CD. Health, Function and Disability in Stroke Patients in the Community. Braz J Phys Ther. 2016;20(4):355-66. doi: 10.1590/bjpt-rbf.2014.0171.
-
72Araújo DV, Teich V, Passos RB, Martins SC. Analysis of the Cost-Effectiveness of Thrombolysis With Alteplase in Stroke. Arq Bras Cardiol. 2010;95(1):12-20. doi: 10.1590/s0066-782x2010005000067.
-
73Conforto AB, Yamamoto FI, Oba-Shinjo SM, Pinto JG, Hoshino M, Scaff M, Marie SK. Screening for MELAS Mutations in Young Patients With Stroke of Undetermined Origin. Arq Neuropsiquiatr. 2007;65(2B):371-6. doi: 10.1590/s0004-282x2007000300001.
-
74Avezum A, Oliveira GBF, Lanas F, Lopez-Jaramillo P, Diaz R, Miranda JJ, Seron P, Camacho-Lopez PA, Orlandini A, Bernabe-Ortiz A, Mattos AC, Islam S, Rangarajan S, Teo K, Yusuf S. Secondary CV Prevention in South America in a Community Setting: The PURE Study. Glob Heart. 2017;12(4):305-13. doi: 10.1016/j.gheart.2016.06.001.
-
75Vinereanu D, Al-Khalidi HR, Rao MP, He W, Lopes RD, Bahit CM, Ciobanu AO, Fox KA, Pokorney SD, Xian Y, Jiang J, Kamath DY, Berwanger O, Tajer C, Huo Y, Xavier D, Granger CB. Regional Differences in Presentation and Antithrombotic Treatment of Patients With Atrial Fibrillation: Baseline Characteristics From a Clustered Randomized Trial to IMProve Treatment With AntiCoagulanTs in Patients With Atrial Fibrillation (IMPACT-AF). Am Heart J. 2017;192:38-47. doi: 10.1016/j.ahj.2017.07.004.
-
76Pontes-Neto OM, Silva GS, Feitosa MR, Figueiredo NL, Fiorot JA Jr, Rocha TN, Massaro AR, Leite JP. Stroke Awareness in Brazil: Alarming Results in a Community-Based Study. Stroke. 2008;39(2):292-6. doi: 10.1161/STROKEAHA.107.493908.
-
77Falavigna A, Teles AR, Vedana VM, Kleber FD, Mosena G, Velho MC, Mazzocchin T, Silva RC, Lucena LF, Santin JT, Roth F. Awareness of Stroke Risk Factors and Warning Signs in Southern Brazil. Arq Neuropsiquiatr. 2009;67(4):1076-81. doi: 10.1590/s0004-282x2009000600022.
-
78Rissardo JP, Caprara ALF, Prado ALC. Stroke Literacy in a South Brazilian City: A Community Based Survey. J Stroke Cerebrovasc Dis. 2018;27(9):2513-8. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.006.
-
79Martins SCO, Sacks C, Hacke W, Brainin M, Figueiredo FA, Marques Pontes-Neto O, Germain PML, Marinho MF, Wiegering AH, McGhie DV, Cruz-Flores S, Ameriso SF, Villareal WMC, Durán JC, Passos JEF, Nogueira RG, Carvalho JJF, Silva GS, Moro CHC, Oliveira-Filho J, Gagliardi R, Sousa EDG, Soares FF, Campos KP, Teixeira PFP, Gonçalves IP, Carquin IRS, Collazos MM, Romero GEP, Figueredo JIM, Barboza MA, López MÁC, Góngora-Rivera F, Cantú-Brito C, Novarro-Escudero N, Velázquez Blanco MÁ, Morvil CAAR, Bareiro ABO, Rojas GM, Flores A, Hancco-Saavedra JA, Pérez Jimenez V, Argomedo CA, Kadota LR, Crosa R, Cuervo DLM, Souza AC, Carbonera LA, Guzmán TFÁ, Maldonado N, Cabral NL, Anderson C, Lindsay P, Hennis A, Feigin VL. Priorities to Reduce the Burden of Stroke in Latin American Countries. Lancet Neurol. 2019;18(7):674-83. doi: 10.1016/S1474-4422(19)30068-7.
-
80Birck MG, Goulart AC, Lotufo PA, Benseñor IM. Secondary Prevention of Coronary Heart Disease: A Cross-Sectional Analysis on the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Sao Paulo Med J. 2019;137(3):223-33. doi: 10.1590/1516-3180.2018.0531140319.
-
81Barbosa E, Eibel B, Brandão AA, Feitosa ADM, Miranda RD, Kobeissi E, Beaney T, Poulter NR, Mota-Gomes MA, Barroso WKS. May Measurement Month 2017: Brazilian Results-Americas. Eur Heart J Suppl. 2019;21(Suppl D):25-7. doi: 10.1093/eurheartj/suz079.
-
82Silva PGMBE, Berwanger O, Santos ESD, Sousa ACS, Cavalcante MA, Andrade PB, Neuenschwander FC, Vargas Filho H, Guimarães JI, Andrade J, Paola AAV, Malachias MVB, Mattos LAPE, Precoma DB, Bacal F, Dutra OP. One Year Follow-up Assessment of Patients Included in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2020;114(6):995-1003. doi: 10.36660/abc.20190879.
-
83Franken M, Giugliano RP, Goodman SG, Baracioli LM, Godoy LC, Furtado RHM, Lima FG, Nicolau JC. Performance of Acute Coronary Syndrome Approaches in Brazil: A Report From the BRACE (Brazilian Registry in Acute Coronary SyndromEs). Eur Heart J Qual Care Clin Outcomes. 2020;6(4):284-92. doi: 10.1093/ehjqcco/qcz045.
-
84Nicolau JC, Franken M, Lotufo PA, Carvalho AC, Marin Neto JA, Lima FG, Dutra O, Knobel E, de Oliveira CC, Timerman S, Stefanini E. Use of Demonstrably Effective Therapies in the Treatment of Acute Coronary Syndromes: Comparison Between Different Brazilian Regions. Analysis of the Brazilian Registry on Acute Coronary Syndromes (BRACE). Arq Bras Cardiol. 2012 Apr;98(4):282-9. doi: 10.1590/s0066-782x2012000400001.
-
85Santos IS, Goulart AC, Brandão RM, Santos RC, Bittencourt MS, Sitnik D, Pereira AC, Pastore CA, Samesima N, Lotufo PA, Bensenor IM. One-year Mortality after an Acute Coronary Event and its Clinical Predictors: The ERICO Study. Arq Bras Cardiol. 2015;105(1):53-64. doi: 10.5935/abc.20150044.
-
86Berwanger O, Guimarães HP, Laranjeira LN, Cavalcanti AB, Kodama AA, Zazula AD, Santucci EV, Victor E, Tenuta M, Carvalho V, Mira VL, Pieper KS, Weber B, Mota LH, Peterson ED, Lopes RD; Bridge-Acs Investigators. Effect of a Multifaceted Intervention on Use of Evidence-Based Therapies in Patients With Acute Coronary Syndromes in Brazil: The BRIDGE-ACS Randomized Trial. JAMA. 2012;307(19):2041-9. doi: 10.1001/jama.2012.413.
-
87Moraes SA, Freitas IC. Doença Isquêmica do Coração e Fatores Associados em Adultos de Ribeirão Preto, SP. Rev Saude Publica. 2012;46(4):591-601. doi: 10.1590/s0034-89102012005000056.
» https://doi.org/10.1590/s0034-89102012005000056 -
88Alves L, Cesar JA, Horta BL. Prevalence of Angina Pectoris in Pelotas, South of Brazil. Arq Bras Cardiol. 2010;95(2):179-85. doi: 10.1590/s0066-782x2010005000075.
-
89Lotufo PA, Malta DC, Szwarcwald CL, Stopa SR, Vieira ML, Bensenor IM. Prevalence of Angina Pectoris in the Brazilian Population From the Rose Questionnaire: Analysis of the National Health Survey, 2013. Rev Bras Epidemiol. 2015;18(Suppl 2):123-31. doi: 10.1590/1980-5497201500060011.
-
90Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Socio-Demographic Index (SDI) 1950–2019. Seattle: Institute for Health Metrics and Evaluation; 2020.
-
91Souza MF, Alencar AP, Malta DC, Moura L, Mansur AP. Serial Temporal Analysis of Ischemic Heart Disease and Stroke Death Risk in Five Regions of Brazil From 1981 to 2001. Arq Bras Cardiol. 2006;87(6):735-40. doi: 10.1590/s0066-782x2006001900009.
-
92Mansur AP, Favarato D. Mortality Due to Cardiovascular Diseases in Brazil and in the Metropolitan Region of São Paulo: A 2011 Update. Arq Bras Cardiol. 2012;99(2):755-61. doi: 10.1590/s0066-782x2012005000061.
-
93Bassanesi SL, Azambuja MI, Achutti A. Premature Mortality Due to Cardiovascular Disease and Social Inequalities in Porto Alegre: From Evidence to Action. Arq Bras Cardiol. 2008;90(6):370-9. doi: 10.1590/s0066-782x2008000600004.
-
94Ishitani LH, Franco GC, Perpétuo IH, França E. Desigualdade Social e Mortalidade Precoce por Doenças Cardiovasculares no Brasil. Rev Saude Publica. 2006;40(4):684-91. doi: 10.1590/s0034-89102006000500019.
-
95Brasil. Ministério da Saúde. Hospital Information System of the Unified Health System (SIH/SUS) [Internet]. Brasília: Ministry of Health of Brazil [cited 2021 Nov 09]. Available From: http://tabnet.datasus.gov.br/ .
» http://tabnet.datasus.gov.br/ -
96Oliveira JC, Almeida-Santos MA, Cunha-Oliveira J, Oliveira LCS, Barreto IDC, Lima TCRM, Arcelino LAM, Prado LFA, Silveira FS, Nascimento TAS, Ferreira EJP, Barreto RV, Moraes EV, Mendonça JT, Sousa ACS, Barreto-Filho JA; VICTIM Register Investigators. Disparities in Access and Mortality of Patients With ST-Segment-Elevation Myocardial Infarction Using the Brazilian Public Healthcare System: VICTIM Register. J Am Heart Assoc. 2019;8(20):e013057. doi: 10.1161/JAHA.119.013057.
-
97Mattos LAP, Berwanger O, Santos ES, Reis HJ, Romano ER, Petriz JL, Sousa AC, Neuenschwander FC, Guimarães JI, Andrade JP. Clinical Outcomes at 30 days in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2013;100(1):6-13. doi: 10.1590/s0066-782x2013000100003.
-
98Piegas LS, Avezum A, Guimarães HP, Muniz AJ, Reis HJ, Santos ES, Knobel M, Souza Rd. Acute Coronary Syndrome Behavior: Results of a Brazilian Registry. Arq Bras Cardiol. 2013;100(6):502-10. doi: 10.5935/abc.20130101.
-
99Soeiro AM, Silva PGMBE, Roque EAC, Bossa AS, Biselli B, Leal TCAT, Soeiro MCFA, Pitta FG, Serrano CV Jr, Oliveira MT Jr. Prognostic Differences Between Men and Women With Acute Coronary Syndrome. Data From a Brazilian Registry. Arq Bras Cardiol. 2018;111(5):648-53. doi: 10.5935/abc.20180166.
-
100Lana MLL, Beaton AZ, Brant LCC, Bozzi ICRS, Magalhães O, Castro LRA, Silva FCT Jr, Silva JLP, Ribeiro ALP, Nascimento BR. Factors Associated With Compliance to AHA/ACC Performance Measures in a Myocardial Infarction System of Care in Brazil. Int J Qual Health Care. 2017;29(4):499-506. doi: 10.1093/intqhc/mzx059.
-
101Marino BC, Marcolino MS, Reis RS Jr, França AL, Passos PF, Lemos TR, Antunes IO, Ferreira CG, Antunes AP, Ribeiro ALP. Epidemiological Profile and Quality Indicators in Patients With Acute Coronary Syndrome in Northern Minas Gerais - Minas Telecardio 2 Project. Arq Bras Cardiol. 2016;107(2):106-15. doi: 10.5935/abc.20160095.
-
102Filgueiras Filho NM, Feitosa Filho GS, Solla DJF, Argôlo FC, Guimarães PO, Paiva Filho IM, Carvalho LGM, Teixeira LS, Rios MNO, Câmara SF, Novais VO, Barbosa LS, Ballalai CS, De Lúcia CV, Granger CB, Newby LK, Lopes RD. Implementation of a Regional Network for ST-Segment-Elevation Myocardial Infarction (STEMI) Care and 30-Day Mortality in a Low- to Middle-Income City in Brazil: Findings From Salvador’s STEMI Registry (RESISST). J Am Heart Assoc. 2018;7(14):e008624. doi: 10.1161/JAHA.118.008624.
-
103Guimarães PO, Sampaio MC, Malafaia FL, Lopes RD, Fanaroff AC, Silva PGMB, Santos TM, Okada MY, Mouallem ARE, Diniz MDS, Custódio JV, Garcia JCT, Furlan V. Clinical Outcomes and Need for Intensive Care After Non-ST-Segment-Elevation Myocardial Infarction. Eur J Intern Med. 2020;76:58-63. doi: 10.1016/j.ejim.2020.02.008.
-
104Helber I, Alves CMR, Grespan SM, Veiga ECA, Moraes PIM, Souza JM, Barbosa AH, Gonçalves I Jr, Fonseca FAH, Carvalho ACC, Caixeta A. The Impact of Advanced Age on Major Cardiovascular Events and Mortality in Patients With ST-Elevation Myocardial Infarction Undergoing a Pharmaco-Invasive Strategy. Clin Interv Aging. 2020;15:715-22. doi: 10.2147/CIA.S218827.
-
105Machado GP, Pivatto F Jr, Wainstein R, Araujo GN, Carpes CK, Lech MC, Valle FH, Bergoli LCC, Gonçalves SC, Wainstein MV. An Overview of Care Change in the Last 6 year in Primary PCI in ST-Elevation Myocardial Infarction in a Tertiary University Brazilian Hospital. Int. J. Cardiovasc. Sci. 2019;32(2):125-33. doi: 10.5935/2359-4802.20180090.
-
106Ferreira LCM, Nogueira MC, Carvalho MS, Teixeira MTB. Mortality Due to Acute Myocardial Infarction in Brazil From 1996 to 2016: 21 Years of Disparities in Brazilian Regions. Arq Bras Cardiol. 2020;115(5):849-59. doi: 10.36660/abc.20190438.
» https://doi.org/10.36660/abc.20190438 -
107Lodi-Junqueira L, Silva JL, Ferreira LR, Gonçalves HL, Athayde GR, Gomes TO, Borges JC, Nascimento BR, Lemos PA, Ribeiro ALP. In-Hospital Mortality Risk Prediction After Percutaneous Coronary Interventions: Validating and Updating the Toronto Score in Brazil. Catheter Cardiovasc Interv. 2015;86(6):239-46. doi: 10.1002/ccd.25916.
-
108Paula LJC, Lemos PA, Medeiros CR, Marin-Neto JA, Figueiredo GL, Polanczyk CA, Wainstein MV, Ribeiro ALP, Lodi-Junqueira L, Oliveira FRA, Sarmento-Leite R, Mattos LA, Cantarelli MJC, Brito FS Jr, Carvalho ACC, Barbosa MR. Construção e validação de um sistema integrado de dados de intervenção coronária percutânea no Brasil (Registro ICP-BR): Perfil clínico dos primeiros 1.249 pacientes incluídos]. Rev Bras Cardiol Inv. 2010;18:256-62.
-
109Piegas LS, Haddad N. Percutaneous Coronary Intervention in Brazil: Results From the Brazilian Public Health System. Arq Bras Cardiol. 2011;96(4):317-24. doi: 10.1590/s0066-782x2011005000035.
-
110Ferreira RM, Souza E Silva NA, Salis LHA. Complications After Elective Percutaneous Coronary Interventions: A Comparison Between Public and Private Hospitals. Indian Heart J. 2018;70(1):32-6. doi: 10.1016/j.ihj.2017.06.012.
-
111Pinton F, Prado G, Bezerra C, Mariani J, Campos C, Caixeta A, Franken M, Lemos PA. TCT-795 Trends in the Prevalence and In-Hospital Outcomes of Radial Versus Femoral Access in Percutaneous Coronary Intervention: A Report With 158,363 Patients From the Brazilian Nationwide PCI Registry (CENIC). J Am Coll Cardiol. 2019;74(13):779. doi:10.1016/j.jacc.2019.08.942.
-
112Pinton F, Prado G, Bezerra C, Mariani J, Campos C, Caixeta A, Franken M, Lemos PA. TCT-422 Clinical Outcomes and Predictors of Mortality Among 847 Nonagenarians Undergoing Percutaneous Coronary Intervention: Insights From a Brazilian Nationwide PCI Registry (CENIC Registry). J Am Coll Cardiol. 2019;74(13):418. doi:10.1016/j.jacc.2019.08.513.
-
113Silva CGSE, Klein CH, Godoy PH, Salis LHA, Silva NASE. Up to 15-Year Survival of Men and Women after Percutaneous Coronary Intervention Paid by the Brazilian Public Healthcare System in the State of Rio de Janeiro, 1999-2010. Arq Bras Cardiol. 2018;111(4):553-61. doi: 10.5935/abc.20180184.
-
114Gomes WJ, Moreira RS, Zilli AC, Bettiati LC Jr, Figueira FAMDS, D’ Azevedo SSP, Soares MJF, Fernandes MP, Ardito RV, Bogdan RAB, Campagnucci VP, Nakasako D, Kalil RAK, Rodrigues CG, Rodrigues AB Jr, Cascudo MM, Atik FA, Lima EB, Nina VJDS, Heluy RA, Azeredo LG, Henrique OS Jr, Mendonça JT, Silva KKOG, Pandolfo M, Lima JD Jr, Faria RM, Santos JG, Paez RP, Coelho GHB, Pereira SN, Senger R, Buffolo E, Caputi GM, Santo JADE, Oliveira JAB, Berwanger O, Cavalcanti AB, Jatene FB. The Brazilian Registry of Adult Patient Undergoing Cardiovascular Surgery, the BYPASS Project: Results of the First 1,722 Patients. Braz J Cardiovasc Surg. 2017;32(2):71-6. doi: 10.21470/1678-9741-2017-0053.
-
115Paez RP, Hossne NA Jr, Santo JADE, Berwanger O, Santos RHN, Kalil RAK, Jatene FB, Cavalcanti AB, Zilli AC, Bettiati LC Jr, Figueira FAMDS, D’Azevedo SSP, Soares MJF, Fernandes MP, Ardito RV, Bogdan RAB, Campagnucci VP, Nakasako D, Rodrigues CG, Rodrigues AB Jr, Cascudo MM, Atik FA, Lima EB, Nina VJDS, Heluy RA, Azeredo LG, Henrique OS Jr, Mendonça JT, Silva KKOG, Pandolfo M, Lima Júnior JD, Faria RM, Santos JGD, Coelho GHB, Pereira SN, Senger R, Buffolo E, Caputi GM, Oliveira JAB, Gomes WJ; BYPASS Registry Study Group. Coronary Artery Bypass Surgery in Brazil: Analysis of the National Reality Through the BYPASS Registry. Braz J Cardiovasc Surg. 2019;34(2):142-8. doi: 10.21470/1678-9741-2018-0313.
-
116Hueb W, Lopes NH, Gersh BJ, Soares P, Machado LA, Jatene FB, Oliveira SA, Ramires JA. Five-Year Follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): A Randomized Controlled Clinical Trial of 3 Therapeutic Strategies for Multivessel Coronary Artery Disease. Circulation. 2007;115(9):1082-9. doi: 10.1161/CIRCULATIONAHA.106.625475.
-
117Hueb W, Lopes N, Gersh BJ, Soares PR, Ribeiro EE, Pereira AC, Favarato D, Rocha AS, Hueb AC, Ramires JA. Ten-Year Follow-up Survival of the Medicine, Angioplasty, or Surgery Study (MASS II): A Randomized Controlled Clinical Trial of 3 Therapeutic Strategies for Multivessel Coronary Artery Disease. Circulation. 2010;122(10):949-57. doi: 10.1161/CIRCULATIONAHA.109.911669.
-
118Hueb W, Rezende PC, Gersh BJ, Soares PR, Favarato D, Lima EG, Garzillo CL, Jatene FB, Ramires JAF, Filho RK. Ten-Year Follow-Up of Off-Pump and On-Pump Multivessel Coronary Artery Bypass Grafting: MASS III. Angiology. 2019;70(4):337-44. doi: 10.1177/0003319718804402.
-
119Gonzales-Tamayo L, Campos CM, Lisboa LAF, Dallan LAO, Jatene FB, Mejia OAV. Choosing the Best Mortality Predictor for Isolated Cabg in Complex Coronary Artery Disease Patients: Performance Comparison of STS, Euroscore II, and Syntax Score II. J Am Coll Cardiol. 2019;73(9):2129. doi:10.1016/S0735-1097(19)32735-4.
-
120Buffolo E, Branco JN, Gerola LR, Aguiar LF, Teles CA, Palma JH, Catani R. Off-Pump Myocardial Revascularization: Critical Analysis of 23 Years’ Experience in 3,866 Patients. Ann Thorac Surg. 2006;81(1):85-9. doi: 10.1016/j.athoracsur.2005.07.032.
-
121Lisboa LA, Moreira LF, Mejia OV, Dallan LA, Pomerantzeff PM, Costa R, Puig LB, Jatene FB, Marcial MB, Stolf NA. Evolution of Cardiovascular Surgery at the Instituto do Coração: Analysis of 71,305 surgeries. Arq Bras Cardiol. 2010;94(2):162-8, 174-81, 164-71. doi: 10.1590/s0066-782x2010000200006.
-
122Santos CA, Oliveira MA, Brandi AC, Botelho PH, Brandi JC, Santos MA, Godoy MF, Braile DM. Risk Factors for Mortality of Patients Undergoing Coronary Artery Bypass Graft Surgery. Rev Bras Cir Cardiovasc. 2014;29(4):513-20. doi: 10.5935/1678-9741.20140073.
-
123Lobato PHM, Vieira FM Jr, Nunes MBG, Galucio VAQL, Barreto EL. Clinical Course of Patients Undergoing Myocardial Revascularization Surgery in a Public Cardiology Referral Hospital in Pará, Brazil. Int J Cardiovasc Sci. 2019;32(3):217-26. doi: 10.5935/2359-4802.20180095.
-
124Stevens B, Pezzullo L, Verdian L, Tomlinson J, George A, Bacal F. The Economic Burden of Heart Conditions in Brazil. Arq Bras Cardiol. 2018;111(1):29-36. doi: 10.5935/abc.20180104.
-
125Azambuja MI, Foppa M, Maranhão MF, Achutti AC. Economic Burden of Severe Cardiovascular Diseases in Brazil: An Estimate Based on Secondary Data. Arq Bras Cardiol. 2008;91(3):148-71. doi: 10.1590/s0066-782x2008001500005.
-
126Schlatter RP, Hirakata VN, Polanczyk CA. Estimating the Direct Costs of Ischemic Heart Disease: Evidence From a Teaching Hospital in BRAZIL, A Retrospective Cohort Study. BMC Cardiovasc Disord. 2017;17(1):180. doi: 10.1186/s12872-017-0615-1.
-
127Hertz JT, Fu T, Vissoci JR, Rocha TAH, Carvalho E, Flanagan B, Andrade L, Limkakeng AT, Staton CA. The Distribution of Cardiac Diagnostic Testing for Acute Coronary Syndrome in the Brazilian Healthcare System: A national Geospatial Evaluation of Health Access. PLoS One. 2019;14(1):e0210502. doi: 10.1371/journal.pone.0210502.
-
128Schlatter R, Etges AP, Neyeloff JL, Cruz LN, Kopittke L, Moreira L, Polanczyk CA. PCV51 a Microcosting study for Angioplasty Procedure: real world data in southern Brazil. Value in Health 2019;22:128. doi: 10.1016/j.jval.2019.04.487.
-
129Silva GSD, Colósimo FC, Sousa AG, Piotto RF, Castilho V. Coronary Artery Bypass Graft Surgery Cost Coverage by the Brazilian Unified Health System (SUS). Braz J Cardiovasc Surg. 2017;32(4):253-9. doi: 10.21470/1678-9741-2016-0069.
-
130Teich V, Piha T, Fahham L, Squiassi HB, Paloni EM, Miranda P, Araújo DV. Acute Coronary Syndrome Treatment Costs From the Perspective of the Supplementary Health System. Arq Bras Cardiol. 2015;105(4):339-44. doi: 10.5935/abc.20150129.
-
131Barbosa JL, Thiers CA, Silva AFR, Vianna MM, Gedeon POPR, Neto LM, Moreira, MBUD, Faria LF, Tura, BR. Impact of Complications of Myocardial Revascularization Surgery on Expenses During Hospital Stay. Int. J. Cardiovasc. Sci. 2019;32(1):28-34. doi: 10.5935/2359-4802.20180083.
-
132Neto AFCB, Campos FZ, Gonçalves RB, Gomes IC, Sternick EB, Almeida AM. Costs and Clinical Outcomes in Percutaneous Coronary Intervention by the Brazilian National Health System. Int J Cardiovasc Sci. 2016;29(6):431-42. doi: 10.5935/2359-4802.20170007. doi: 10.5935/2359-4802.20170007.
-
133Marino BCA, Ribeiro ALP, Alkmim MB, Antunes AP, Boersma E, Marcolino MS. Coordinated Regional Care of Myocardial Infarction in a Rural Area in Brazil: Minas Telecardio Project 2. Eur Heart J Qual Care Clin Outcomes. 2016;2(3):215-24. doi: 10.1093/ehjqcco/qcw020.
-
134Marcolino MS, Brant LCC, Araujo JG, Nascimento BR, Castro LR, Martins P, Lodi-Junqueira L, Ribeiro ALP. Implementation of the Myocardial Infarction System of Care in City of Belo Horizonte, Brazil. Arq Bras Cardiol. 2013;100(4):307-14.
-
135Bocchi EA. Heart Failure in South America. Curr Cardiol Rev. 2013;9(2):147-56. doi: 10.2174/1573403x11309020007.
-
136Arteaga E, Ianni BM, Fernandes F, Mady C. Benign Outcome in a Long-Term Follow-up of Patients With Hypertrophic Cardiomyopathy in Brazil. Am Heart J. 2005;149(6):1099-105. doi: 10.1016/j.ahj.2004.09.049.
-
137Chagas disease in Latin America: An Epidemiological Update Based on 2010 Estimates. Wkly Epidemiol Rec. 2015;90(6):33-43.
-
138Martins-Melo FR, Ramos AN Jr, Alencar CH, Heukelbach J. Prevalence of Chagas Disease in Brazil: A Systematic Review and Meta-Analysis. Acta Trop. 2014;130:167-74. doi: 10.1016/j.actatropica.2013.10.002.
-
139Sabino EC, Ribeiro ALP, Salemi VM, Oliveira CDL, Antunes AP, Menezes MM, Ianni BM, Nastari L, Fernandes F, Patavino GM, Sachdev V, Capuani L, Almeida-Neto C, Carrick DM, Wright D, Kavounis K, Goncalez TT, Carneiro-Proietti AB, Custer B, Busch MP, Murphy EL; National Heart, Lung, and Blood Institute Retrovirus Epidemiology Donor Study-II (REDS-II), International Component. Ten-year Incidence of Chagas Cardiomyopathy Among Asymptomatic Trypanosoma Cruzi-Seropositive Former Blood Donors. Circulation. 2013;127(10):1105-15. doi: 10.1161/CIRCULATIONAHA.112.123612.
-
140Nunes MCP, Buss LF, Silva JLP, Martins LNA, Oliveira CDL, Cardoso CS, Brito BOF, Ferreira AM, Oliveira LC, Bierrenbach AL, Fernandes F, Busch MP, Hotta VT, Martinelli LMB, Almeida Soeiro MCF, Brentegani A, Salemi VMC, Menezes MM, Ribeiro ALP. Incidence and Predictors of Progression to Chagas Cardiomyopathy: Long-Term Follow-Up of Trypanosoma Cruzi Seropositive Individuals. Circulation. 2021;144:1553–66. doi: 10.1161/circulationaha.121.055112.
-
141Martins-Melo FR, Alencar CH, Ramos AN Jr, Heukelbach J. Epidemiology of Mortality Related to Chagas’ Disease in Brazil, 1999-2007. PLoS Negl Trop Dis. 2012;6(2):e1508. doi: 10.1371/journal.pntd.0001508.
-
142Nóbrega AA, Araújo WN, Vasconcelos AMN. Mortality Due to Chagas Disease in Brazil According to a Specific Cause. Am J Trop Med Hyg. 2014;91(3):528-33. doi: 10.4269/ajtmh.13-0574.
-
143Simões TC, Borges LF, Assis ACP, Silva MV, Santos J, Meira KC. Chagas Disease Mortality in Brazil: A Bayesian Analysis of Age-Period-Cohort Effects and Forecasts for Two Decades. PLoS Negl Trop Dis. 2018;12(9):e0006798. doi: 10.1371/journal.pntd.0006798.
-
144Martins-Melo FR, Ramos AN Jr, Alencar CH, Lange W, Heukelbach J. Mortality of Chagas’ disease in Brazil: Spatial Patterns and Definition of High-Risk Areas. Trop Med Int Health. 2012;17(9):1066-75. doi: 10.1111/j.1365-3156.2012.03043.x.
-
145Capuani L, Bierrenbach AL, Alencar AP, Mendrone A Jr, Ferreira JE, Custer B, Ribeiro ALP, Sabino EC. Mortality Among Blood Donors Seropositive and Seronegative for Chagas Disease (1996-2000) in São Paulo, Brazil: A Death Certificate Linkage Study. PLoS Negl Trop Dis. 2017;11(5):e0005542. doi: 10.1371/journal.pntd.0005542.
-
146Ayub-Ferreira SM, Mangini S, Issa VS, Cruz FD, Bacal F, Guimarães GV, Chizzola PR, Conceição-Souza GE, Marcondes-Braga FG, Bocchi EA. Mode of Death on Chagas Heart Disease: Comparison With Other Etiologies. A Subanalysis of the REMADHE Prospective Trial. PLoS Negl Trop Dis. 2013;7(4):e2176. doi: 10.1371/journal.pntd.0002176.
-
147Lima-Costa MF, Peixoto SV, Ribeiro ALP. Chagas Disease and mortality in Old Age as an Emerging Issue: 10 Year Follow-Up of the Bambuí Population-Based Cohort Study (Brazil). Int J Cardiol. 2010;145(2):362-3. doi: 10.1016/j.ijcard.2010.02.036.
-
148Nadruz W Jr, Gioli-Pereira L, Bernardez-Pereira S, Marcondes-Braga FG, Fernandes-Silva MM, Silvestre OM, Sposito AC, Ribeiro ALP, Bacal F, Fernandes F, Krieger JE, Mansur AJ, Pereira AC. Temporal Trends in the Contribution of Chagas Cardiomyopathy to Mortality Among Patients With Heart Failure. Heart. 2018;104(18):1522-1528. doi: 10.1136/heartjnl-2017-312869.
-
149Borges-Pereira J, Coura JR, Zauza PL, Pirmez C, Xavier SS. Chagas Disease in Virgem da Lapa, Minas Gerais, Brazil: Left Ventricle aneurysm and the Risk of Death in the 24-Year Interval. Mem Inst Oswaldo Cruz. 2020;115:e200056. doi: 10.1590/0074-02760200056.
-
150Ferreira AM, Sabino ÉC, Oliveira LC, Oliveira CDL, Cardoso CS, Ribeiro ALP, Damasceno RF, Nunes MDCP, Haikal DSA. Impact of the Social Context on the Prognosis of Chagas Disease Patients: Multilevel Analysis of a Brazilian Cohort. PLoS Negl Trop Dis. 2020;14(6):e0008399. doi: 10.1371/journal.pntd.0008399.
-
151Oliveira CL, Nunes MCP, Colosimo EA, de Lima EM, Cardoso CS, Ferreira AM, de Oliveira LC, Moreira CHV, Bierrenbach AL, Haikal DSA, Peixoto SV, Lima-Costa MF, Sabino EC, Ribeiro ALP. Risk Score for Predicting 2-Year Mortality in Patients With Chagas Cardiomyopathy From Endemic Areas: SaMi-Trop Cohort Study. J Am Heart Assoc. 2020;9(6):e014176. doi: 10.1161/JAHA.119.014176.
-
152Global Burden of Disease Study 2017 (GBD 2017) results. Global Health Data Exchange website. Seattle, WA: Institute for Health Metrics and Evaluation (IHME), University of Washington; 2017. [cited 2021 Nov 09]. Available From: http://ghdx.healthdata.org/g .
» http://ghdx.healthdata.org/g -
153Ciapponi A, Alcaraz A, Calderón M, Matta MG, Chaparro M, Soto N, Bardach A. Burden of Heart Failure in Latin America: A Systematic review and Meta-Analysis. Rev Esp Cardiol. 2016;69(11):1051-60. doi: 10.1016/j.rec.2016.04.054.
-
154Moraes RS, Fuchs FD, Moreira LB, Wiehe M, Pereira GM, Fuchs SC. Risk Factors for Cardiovascular Disease in a Brazilian Population-Based Cohort Study. Int J Cardiol. 2003;90(2-3):205-11. doi: 10.1016/s0167-5273(02)00556-9.
-
155Jorge AL, Rosa ML, Martins WA, Correia DM, Fernandes LC, Costa JA, Moscavitch SD, Jorge BA, Mesquita ET. The Prevalence of Stages of Heart Failure in Primary Care: a Population-Based Study. J Card Fail. 2016;22(2):153-7. doi: 10.1016/j.cardfail.2015.10.01.
» https://doi.org/10.1016/j.cardfail.2015.10.01 -
156Nogueira IDB, Nogueira PAMS, Fonseca AMC, Santos, TZM, Souza DE, Ferreira GMH. Prevalência de Insuficiência Cardíaca e Associação com Saúde Autorreferida no Brasil: Pesquisa Nacional de Saúde – 2013. Acta Fisiátrica. 2019;26(2):95-101. doi: 10.11606/issn.2317-0190.v26i2a164952
-
157Fochat RC, Polonini HC, Barbosa SEM, Chicourel EL, Raposo NRB. Prevalence of Major Public Health Impact Diseases Among Frail Elderly Residents in the Zona da Mata region in the State of Minas Gerais. Rev APS. 2016;19(2):268-76.
-
158Balieiro HM, Osugue RK, Rangel SP, Brandão R, Balieiro TL, Bernardez S, Mesquita ET. Clinical and Demographic Profile and Quality Indicators for heart Failure in a Rural Area. Arq Bras Cardiol. 2009;93(6):637-42. doi: 10.1590/s0066-782x2009001200020.
-
159Bierrenbach AL, Alencar GP, Martinez C, Souza M de FM de, Policena GM, França EB. Redistribution of Heart Failure Deaths Using Two Methods: Linkage of Hospital Records With Death Certificate Data and Multiple Causes of death data. Cad Saude Publica. 2019;35(5):e00135617. doi:10.1590/0102-311x00135617.
-
160Gaui EN, Klein CH, Oliveira GM. Mortality due to Heart Failure: Extended Analysis and Temporal Trend in Three States of Brazil. Arq Bras Cardiol. 2010;94(1):55-61. doi: 10.1590/s0066-782x2010000100010.
-
161Freitas HF, Chizzola PR, Paes AT, Lima AC, Mansur AJ. Risk Stratification in a Brazilian Hospital-Based Cohort of 1220 Outpatients With Heart Failure: Role of Chagas’ Heart Disease. Int J Cardiol. 2005;102(2):239-47. doi: 10.1016/j.ijcard.2004.05.025.
-
162Gioli-Pereira L, Marcondes-Braga FG, Bernardez-Pereira S, Bacal F, Fernandes F, Mansur AJ, Pereira AC, Krieger JE. Predictors of One-Year Outcomes in Chronic Heart Failure: The Portrait of a Middle Income Country. BMC Cardiovasc Disord. 2019;19(1):251. doi: 10.1186/s12872-019-1226-9.
-
163Abreu CD, Xavier RM, Nascimento JS, Ribeiro ALP. Long-Term Outcome After Cardiac Resynchronization Therapy: A Nationwide Database. Int J Cardiol. 2012;155(3):492-3. doi: 10.1016/j.ijcard.2011.12.083.
-
164Albuquerque DC, Souza Neto JD, Bacal F, Rohde LE, Bernardez-Pereira S, Berwanger O, Almeida DR; Investigadores Estudo BREATHE. I Brazilian Registry of Heart Failure - Clinical Aspects, Care Quality and Hospitalization Outcomes. Arq Bras Cardiol. 2015;104(6):433-42. doi: 10.5935/abc.20150031.
-
165Tavares LR, Victer H, Linhares JM, de Barros CM, Oliveira MV, Pacheco LC, Viana CH, Pereira SB, Silva GP, Mesquita ET. Epidemiology of Decompensated Heart Failure in the City of Niterói: EPICA - Niterói Project. Arq Bras Cardiol. 2004;82(2):125-8. doi: 10.1590/s0066-782x2004000200003.
-
166Wajner A, Zuchinali P, Olsen V, Polanczyk CA, Rohde LE. Causes and Predictors of in-Hospital Mortality in Patients Admitted With or for Heart Failure at a Tertiary Hospital in Brazil. Arq Bras Cardiol. 2017;109(4):321-30. doi: 10.5935/abc.20170136.
-
167Rohde LE, Clausell N, Ribeiro JP, Goldraich L, Netto R, William Dec G, DiSalvo TG, Polanczyk CA. Health Outcomes in Decompensated Heart Failure: A Comparison of Tertiary Hospitals in Brazil and United States. Int J Cardiol. 2005;102:71-7. doi: 10.1016/j.i.
-
168Godoy HL, Silveira JA, Segalla E, Almeida DR. Hospitalization and Mortality Rates for Heart Failure in Public Hospitals in São Paulo. Arq Bras Cardiol. 2011;97(5):402-7. doi: 10.1590/s0066-782x2011005000096.
-
169Nicolao CZ, Ferreira JB, Paz AA, Linch GFC, Rover M, Souza EN. Heart Failure: An Overview of Morbidity and Mortality in Rio Grande do Sul. Int J Cardiovac Sci. 2019;32(6):596-604. doi: 10.5935/2359-4802.20190032.
-
170Fernandes ADF, Fernandes GC, Mazza MR, Knijnik LM, Fernandes GS, Vilela AT, Badiye A, Chaparro SV. A 10-Year Trend Analysis of Heart Failure in the Less Developed Brazil. Arq Bras Cardiol. 2020;114(2):222-31. doi: 10.36660/abc.20180321.
-
171Registro Brasileiro de Transplantes. Dimensionamento dos transplantes no Brasil e em cada estado (2009-2016). São Paulo: Associação Brasileira de Transplante de Órgãos; 2016.
-
172Goldraich LA, Neyeloff JL, Etges APBS, Zeilmann LG, Hastenteufel LT, Ghisleni EC, Clausell N. Heart Transplantation Cost Composition in Brazil: A Patient-Level Microcosting Analysis and Comparison With International Data. J Card Fail. 2018;24(12):860-3. doi: 10.1016/j.cardfail.2018.10.011.
-
173Cestari V, Pessoa VL, Souza Neto JD, Moreira T, Florêncio R, Vasconcelos GG, Souza L, Braga A, Sobral MG. Clinical Evolution of Patients Using Ventricular Assist Devices as a Bridge for Transplantation. Transplant Proc. 2018;50(3):796-803. doi: 10.1016/j.transproceed.2018.02.014.
-
174Thomas H, Diamond J, Vieco A, Chaudhuri S, Shinnar E, Cromer S, Perel P, Mensah GA, Narula J, Johnson CO, Roth GA, Moran AE. Global Atlas of Cardiovascular Disease 2000-2016: The Path to Prevention and Control. Glob Heart. 2018;13(3):143-63. doi: 10.1016/j.gheart.2018.09.511.
-
175Iung B, Vahanian A. Epidemiology of Acquired Valvular Heart Disease. Can J Cardiol. 2014;30(9):962-70. doi: 10.1016/j.cjca.2014.03.022.
-
176Nascimento BR, Beaton AZ, Nunes MC, Diamantino AC, Carmo GA, Oliveira KK, Oliveira CM, Meira ZM, Castilho SR, Lopes EL, Castro IM, Rezende VM, Chequer G, Landay T, Tompsett A, Ribeiro ALP, Sable C; PROVAR (Programa de RastreamentO da VAlvopatia Reumática) Investigators. Echocardiographic Prevalence of Rheumatic Heart Disease in Brazilian Schoolchildren: Data From the PROVAR study. Int J Cardiol. 2016;219:439-45. doi: 10.1016/j.ijcard.2016.06.088.
-
177Santos JPAD, Carmo GALD, Beaton AZ, Lourenço TV, Diamantino AC, Nunes MDCP, Sable C, Nascimento BR. Challenges for the Implementation of the First Large-Scale Rheumatic Heart Disease Screening Program in Brazil: The PROVAR Study Experience. Arq Bras Cardiol. 2017;108(4):370-374. doi: 10.5935/abc.20170047.
-
178Ribeiro GS, Tartof SY, Oliveira DW, Guedes AC, Reis MG, Riley LW, Ko AI. Surgery for Valvular Heart Disease: A Population-Based Study in a Brazilian Urban Center. PLoS One. 2012;7(5):e37855. doi: 10.1371/journal.pone.0037855.
-
179Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, Forouzanfar MH, Longenecker CT, Mayosi BM, Mensah GA, Nascimento BR, Ribeiro ALP, Sable CA, Steer AC, Naghavi M, Mokdad AH, Murray CJL, Vos T, Carapetis JR, Roth GA. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990-2015. N Engl J Med. 2017;377(8):713-722. doi: 10.1056/NEJMoa1603693.
-
180Alves Meira ZM, de Castilho SR, Lins Barros MV, Maria Vitarelli A, Diniz Capanema F, Moreira NS, Moreira Camargos PA, Coelho Mota CC. Prevalence of rheumatic fever in children From a public high school in Belo Horizonte. Arq Bras Cardiol. 1995;65(4):331-4.
-
181Tarasoutchi F, Montera MW, Grinberg M, Piñeiro DJ, Sánchez CR, Bacelar AC, Lopes AS, Fernandes JR, Pires LJ, Moraes RC, Accorsi TA, Colafranceschi AS, Kiyose AT, Fiorelli AI, Bacelar AC, Lopes AS, Ramos AI, Boer BN, Abdulmassih Neto C, Sánchez CR, Esteves CA, Weksler C, Piñeiro DJ, Kruczan DD, Rossi EG, Mesquita ET, Brito FS Jr, Bacal F, Bosh F, Urzua FF, Moraes F, Tarasoutchi F, Costa FD, Barbosa GV, Spina GS, Murad H, Hernández HM, Fernandes JR, Mangione JA, Brito JC, Murillo JR, Plana JC, Paganini JJ, Krauss J, Moura LA, Pires LJ, Carvalho LA, Cardoso LF, Katz M, Vieira ML, Montera MW, Barbosa Mde M, Barbosa Mde R, Grinberg M, Villagrán OA, Pomerantzeff PM, Lavitola Pde L, Moraes RC, Leite RE, Sampaio RO, Franco S, Martins SM, Bordignon S, Accorsi TA, David TE, Duré VR, Rossei V, Ávila WS. Brazilian Guidelines for Valve Disease - SBC 2011 / I Guideline Inter-American Valve Disease - 2011 SIAC. Arq Bras Cardiol. 2011;97(Suppl 1):1-67. doi: 10.1590/s0066-782x2011002000001.
» https://doi.org/10.1590/s0066-782x2011002000001 -
182Moraes RC, Katz M, Tarasoutchi F. Clinical and Epidemiological Profile of Patients With Valvular Heart Disease Admitted to the Emergency Department. Einstein. 2014;12(2):154-8. doi: 10.1590/s1679-45082014ao3025.
-
183Carvalho LMA, Araujo FDR, Meira ZMA. Doppler Echocardiographic Follow-Up of Mitral and Aortic Regurgitation in Children and Adolescents With Subclinical and Mild Rheumatic Carditis. Int J Cardiovasc Sciences. 2017;30(5):391-400. doi: 10.5935/2359-4802.20170065.
-
184Meira ZM, Goulart EM, Mota C. Comparative Study of Clinical and Doppler Echocardiographic Evaluations of the Progression of Valve Diseases in Children and Adolescents With Rheumatic Fever. Arq Bras Cardiol. 2006;86(1):32-8. doi: 10.1590/s0066-782x2006000100006.
-
185Nunes MCP, Sable C, Nascimento BR, Lima EM, da Silva JLP, Diamantino AC, Oliveira KKB, Okello E, Aliku T, Lwabi P, Colosimo EA, Ribeiro ALP, Beaton AZ. Simplified Echocardiography Screening Criteria for Diagnosing and Predicting Progression of Latent Rheumatic Heart Disease. Circ Cardiovasc Imaging. 2019;12(2):e007928. doi: 10.1161/CIRCIMAGING.118.007928.
-
186Bechtlufft BM, Nascimento BR, Sable C, Fraga CL, Barbosa MM, Reis SD, Diamantino AC, Meira ZMA, Castilho SRT, Arantes NF, Oliveira KK, Silva JLP, Rezende BF, Costa WAA, Mata MD, Pereira AF, Ribeiro ALP, Beaton AZ, Pereira Nunes MC. Validation of a Simplified Score for Predicting Latent Rheumatic Heart Disease Progression Using a Prospective Cohort of Brazilian Schoolchildren. BMJ Open. 2020;10(5):e036827. doi: 10.1136/bmjopen-2020-036827.
-
187Nascimento BR, Nunes MCP, Lima EM, Sanyahumbi AE, Wilson N, Tilton E, Rémond MGW, Maguire GP, Ribeiro ALP, Kazembe PN, Sable C, Beaton AZ; Programa de Rastreamento da Valvopatia Reumática (PROVAR) Investigators. Outcomes of Echocardiography-Detected Rheumatic Heart Disease: Validating a Simplified Score in Cohorts From Different Countries. J Am Heart Assoc. 2021;10(18):e021622. doi: 10.1161/JAHA.121.021622.
-
188Soares ACd, Passos LSA, Sable C, Beaton A, Ribeiro VT, Gollob KJ, Dutra WO, Nunes MCP. Circulating Cytokines Predict Severity of Rheumatic Heart Disease. Int J Cardiol. 2019;289:107-9. doi: 10.1016/j.ijcard.2019.04.063.
-
189Tormin JPAS, Nascimento BR, Sable CA, da Silva JLP, Brandao-de-Resende C, Rocha LPC, Pinto CHR, Neves EGA, Macedo FVB, Fraga CL, Oliveira KKB, Diamantino AC, Ribeiro ALP, Beaton AZ, Nunes MCP, Dutra WO; PROVAR (Programa de RastreamentO da VAlvopatia Reumática) investigators. Cytokine Gene Functional Polymorphisms and Phenotypic Expression as Predictors of Evolution From Latent to Clinical Rheumatic Heart Disease. Cytokine. 2021;138:155370. doi: 10.1016/j.cyto.2020.155370.
-
190GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, Regional, and National Incidence, Prevalence, and Years Lived With Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-858. doi: 10.1016/S0140-6736(18)32279-7.
» https://doi.org/10.1016/S0140-6736(18)32279-7 -
191Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E, Ravaud P, Vahanian A. A prospective Survey of Patients With Valvular Heart Disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24(13):1231-43. doi: 10.1016/s0195-668x(03)00201-x.
-
192Nascimento BR, Sable C, Nunes MCP, Diamantino AC, Oliveira KKB, Oliveira CM, Meira ZMA, Castilho SRT, Santos JPA, Rabelo LMM, Lauriano KCA, Carmo GAL, Tompsett A, Ribeiro ALP, Beaton AZ; PROVAR (Rheumatic Valve Disease Screening Program) Investigators. Comparison Between Different Strategies of Rheumatic Heart Disease Echocardiographic Screening in Brazil: Data From the PROVAR (Rheumatic Valve Disease Screening Program) Study. J Am Heart Assoc. 2018;7(4):e008039. doi: 10.1161/JAHA.117.008039.
-
193Diamantino AC, Nascimento BR, Nunes MCP, Sable CA, Oliveira KKB, Rabelo LC, Franco J, Diamantino LC, Barbosa MM, Reese AT, Olivieri L, de Lima EM, Martins LNA, Colosimo EA, Beaton AZ, Ribeiro ALP; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática e outras Doenças Cardiovasculares) investigators. Impact of Incorporating Echocardiographic Screening Into a Clinical Prediction Model to Optimise Utilisation of Echocardiography in Primary Care. Int J Clin Pract. 2021;75(3):e13686. doi: 10.1111/ijcp.13686.
-
194Nascimento BR, Martins JFBS, Nascimento ER, Pappa GL, Sable CA, Beaton AZ, Gomes PR, Nunes MC, Oliveira KKB, Franco J, Pereira AFC, Rezende BDF, Mata MDO, AL Ribeiro, Meira W. Deep learning for automatic identification of Rheumatic Heart Disease in Echoca. J Am Coll Cardiol. 2020;75(11):3577.
-
195Freeman RV, Otto CM. Spectrum of Calcific Aortic Valve Disease: Pathogenesis, Disease Progression, and Treatment Strategies. Circulation. 2005;111(24):3316-26. doi: 10.1161/CIRCULATIONAHA.104.486738.
-
196Grinberg M, Accorsi TA. Aortic stenosis in the elderly: a Brazilian perspective. Arq Bras Cardiol. 2009 Feb;92(2):e9-12. doi: 10.1590/s0066-782x2009000200016.
-
197Xavier RMA, Azevedo VMP, Godoy PH, Migowski A, Ribeiro ALP, Chaves RBM, Correia MG, Xavier CA, Hashimoto LA, Weksler C, Silva NASE. Medium-Term Outcomes of 78,808 Patients after Heart Valve Surgery in a Middle-Income Country: A Nationwide Population-Based Study. BMC Cardiovasc Disord. 2017;17(1):302. doi: 10.1186/s12872-017-0725-9.
-
198Zilli AC, Guizilini S, Rocco IS, Santo JADE, Berwanger O, Kalil RAK, Jatene FB, Cavalcanti AB, Santos RHN, Gomes WJ. Valve Heart Surgery in Brazil - The BYPASS Registry Analysis. Braz J Cardiovasc Surg. 2020;35(1):82-90. doi: 10.21470/1678-9741-2019-0408.
-
199GBD 2019 Universal Health Coverage Collaborators. Measuring Universal Health Coverage Based on an Index of Effective Coverage of Health Services in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1250-84. doi: 10.1016/S0140-6736(20)30750-9.
» https://doi.org/10.1016/S0140-6736(20)30750-9 -
200Dougherty S, Beaton A, Nascimento BR, Zühlke LJ, Khorsandi M, Wilson N. Prevention and Control of Rheumatic Heart Disease: Overcoming Core Challenges in Resource-Poor Environments. Ann Pediatr Cardiol. 2018;11(1):68-78. doi: 10.4103/apc.APC_135_17.
-
201GBD 2017 DALYs and HALE Collaborators. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 359 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859-922. doi: 10.1016/S0140-6736(18)32335-3.
» https://doi.org/10.1016/S0140-6736(18)32335-3 -
202Global Burden of Disease Study. Disease GB. GBD Compare - Viz Hub [Internet]. Seattle: Institute for Health Metrics and Evaluation (IHME); 2019. Available From: https://vizhub.healthdata.org/gbd-compare/ .
» https://vizhub.healthdata.org/gbd-compare/ -
203Nunes MCP, Tan TC, Elmariah S, Lodi-Junqueira L, Nascimento BR, Lago R, Silva JLP, Reis RCP, Zeng X, Palacios IF, Hung J, Levine RA. Net Atrioventricular Compliance is an Independent Predictor of Cardiovascular Death in Mitral Stenosis. Heart. 2017;103(23):1891-1898. doi: 10.1136/heartjnl-2016-310955.
-
204Pivatto F jR, Teixeira Filho GF, Sant’anna JR, Py PM, Prates PR, Nesralla IA, Kalil RA. Advanced age and Incidence of Atrial Fibrillation in the Postoperative Period of Aortic Valve Replacement. Rev Bras Cir Cardiovasc. 2014;29(1):45-50. doi: 10.5935/1678-9741.20140010.
-
205Sá MP, Sá MV, Albuquerque AC, Silva BB, Siqueira JW, Brito PR, Ferraz PE, Lima Rde C. Predicting Risk of Atrial Fibrillation After Heart Valve Surgery: Evaluation of a Brazilian Risk Score. Rev Bras Cir Cardiovasc. 2012;27(1):117-22. doi: 10.5935/1678-9741.20120017.
-
206Marrone LCP, Brunelli JPf, Saute Rl, Tomasi Gh, Madeira Bc, Martins WA, Rohr RD, Heck AP, Botton LR, Castro MM, Bodanese R, Bodanese LC, Marrone ACH, Costa JC. Cardioembolic Sources in Stroke Patients in South of Brazil. Thrombosis. 2014;2014:753-780. doi: 10.1155/2014/753780.
-
207Sampaio RO, Jonke VM, Falcão JL, Falcão S, Spina GS, Tarasoutchi F, Grinberg M. Prevalence of Coronary Artery Disease and Preoperative Assessment in Patients With Valvopathy. Arq Bras Cardiol. 2008;91(3):183-6. doi: 10.1590/s0066-782x2008001500010.
-
208Kruczan DD, Silva NA, Pereira Bde B, Romão VA, Correa Filho WB, Morales FE. Coronary Artery Disease in Patients With Rheumatic and Non-Rheumatic Valvular Heart Disease Treated at a Public Hospital in Rio de Janeiro. Arq Bras Cardiol. 2008;90(3):197-203. doi: 10.1590/s0066-782x2008000300010.
-
209Cazelli JG, Camargo GC, Kruczan DD, Weksler C, Felipe AR, Gottlieb I. Prevalence and Prediction of Obstructive Coronary Artery Disease in Patients Undergoing Primary Heart Valve Surgery. Arq Bras Cardiol. 2017;109(4):348-356. doi: 10.5935/abc.20170135.
-
210Rede Interagencial de Informação para a Saúde. Indicadores e Dados Básicos de Saúde [Internet]. Brasília: Ministério da Saúde; 2020 [cited 2020 Nov 09]. Available From: https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ .
» https://datasus.saude.gov.br/acesso-a-informacao/indicadores-e-dados-basicos/ -
211Lopes MACQ, Nascimento BR, Oliveira GMM. Treatment of Aortic Stenosis in Elderly Individuals in Brazil: How Long Can We Wait? Arq Bras Cardiol. 2020;114(2):313-18. doi: 10.36660/abc.2020003.
-
212Ubels J, Sable C, Beaton AZ, Nunes MCP, Oliveira KKB, Rabelo LC, Teixeira IM, Ruiz GZL, Rabelo LMM, Tompsett AR, Ribeiro ALP, Sahlen KG, Nascimento BR; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática e Outras Doenças Cardiovasculares) investigators. Cost-Effectiveness of Rheumatic Heart Disease Echocardiographic Screening in Brazil: Data From the PROVAR+ Study: Cost-effectiveness of RHD screening in Brazil. Glob Heart. 2020;15(1):18. doi: 10.5334/gh.529.
-
213Fonseca LGA, Lima INDF, Gualdi LP. Characterization of Brazilian Hospital Admissions due to Cardiovascular Diseases: A Longitudinal Study. BMC Cardiovasc Disord. 2020;20(1):311. doi: 10.1186/s12872-020-01588-w.
-
214Cardoso LF, Ayres CV, Bento AM, Tarasoutchi F, Vieira ML, Grinberg M. Immediate and Late Results of Percutaneous Mitral Valve Repair in Patients With Mitral Stenosis. Arq Bras Cardiol. 2010;94(3):383-90, 406-13. doi: 10.1590/s0066-782x2010000300020.
-
215Peixoto A, Linhares L, Scherr P, Xavier R, Siqueira SL, Pacheco TJ, Venturinelli G. Rheumatic Fever: Systematic Review. Rev Bras Clin Med. 2011;9(3):234-8.
-
216Alcici ME, Lodi-Junqueira L, Sant’Anna Athayde GR, Soares JR, Gomes Tiago DA, Tavares PL, Saad GP, Ferreira de Sales I, Okello E, Rwebembera J, Esteves WAM, Nunes MCP. The Importance of Conscious Sedation for Life-Saving Valve Procedures in Patients With Rheumatic Heart Disease From Low- to Middle-Income Countries. Glob Heart. 2019;14(3):311-16. doi: 10.1016/j.gheart.2019.07.003.
-
217Athayde GRS, Nascimento BR, Elmariah S, Lodi-Junqueira L, Soares JR, Saad GP, Silva JLP, Tan TC, Hung J, Palacios IF, Levine RA, Nunes MCP. Impact of Left Atrial Compliance Improvement on Functional Status After Percutaneous Mitral Valvuloplasty. Catheter Cardiovasc Interv. 2019;93(1):156-63. doi: 10.1002/ccd.27831.
-
218Cruz RCC, Cordeiro BS, Santos FS, Fernandes CR, Gama JMA, Ladeia AMT. Predictors of Unfavourable Outcomes in Children and Adolescents Submitted to Surgical Mitral Valvuloplasty Secondary to Chronic Rheumatic Heart Disease. Arq Bras Cardiol. 2019;113(4):748-56. doi: 10.5935/abc.20190184.
-
219Grinberg M, Jonke VM, Sampaio RO, Spina GS, Tarasoutchi F. Validation of a New Surgical Risk Score For Heart Valve Surgery: VMCP. Arq Bras Cardiol. 2009;92(4):320-5. doi: 10.1590/s0066-782x2009000400012.
-
220Garofallo SB, Machado DP, Rodrigues CG, Bordim O Jr, Kalil RA, Portal VL. Applicability of Two International Risk Scores in Cardiac Surgery in a Reference Center in BRAZIL. Arq Bras Cardiol. 2014;102(6):539-48. doi: 10.5935/abc.20140064.
-
221Brito FS Jr, Carvalho LA, Sarmento-Leite R, Mangione JA, Lemos P, Siciliano A, Caramori P, São Thiago L, Grube E, Abizaid A; Brazilian TAVI Registry Investigators. Outcomes and Predictors of Mortality After Transcatheter Aortic Valve Implantation: Results of the Brazilian registry. Catheter Cardiovasc Interv. 2015;85(5):153-62. doi: 10.1002/ccd.25778.
-
222Nunes Filho ACB, Katz M, Campos CM, Carvalho LA, Siqueira DA, Tumelero RT, Portella ALF, Esteves V, Perin MA, Sarmento-Leite R, Lemos Neto PA, Tarasoutchi F, Bezerra HG, Brito FS Jr. Impact of Acute Kidney Injury on Short- and Long-term Outcomes After Transcatheter Aortic Valve Implantation. Rev Esp Cardiol. 2019;72(1):21-29. doi: 10.1016/j.rec.2017.11.024.
-
223Monteiro C, Ferrari ADL, Caramori PRA, Carvalho LAF, Siqueira DAA, Thiago LEKS, Perin M, Lima VC, Guérios E, Brito FS Jr. Permanent Pacing After Transcatheter Aortic Valve Implantation: Incidence, Predictors and Evolution of Left Ventricular Function. Arq Bras Cardiol. 2017;109(6):550-59. doi: 10.5935/abc.20170170.
-
224Souza AL, Salgado CG, Mourilhe-Rocha R, Mesquita ET, Lima LC, Mattos ND, Rabischoffsky A, Fagundes FE, Colafranceschi AS, Carvalho LA. Transcatheter Aortic Valve Implantation and Morbidity and Mortality-Related Factors: A 5-Year Experience in Brazil. Arq Bras Cardiol. 2016;106(6):519-27. doi: 10.5935/abc.20160072.
-
225Guilherme L, Kalil J. Rheumatic Fever and Rheumatic Heart Disease: Cellular Mechanisms Leading Autoimmune Reactivity and Disease. J Clin Immunol. 2010;30(1):17-23. doi: 10.1007/s10875-009-9332-6.
-
226Nunes MC, Tan TC, Elmariah S, Lago R, Margey R, Cruz-Gonzalez I, Zheng H, Handschumacher MD, Inglessis I, Palacios IF, Weyman AE, Hung J. The Echo Score Revisited: Impact of Incorporating Commissural Morphology and Leaflet Displacement to the Prediction of Outcome For Patients Undergoing Percutaneous Mitral Valvuloplasty. Circulation. 2014;129(8):886-95. doi: 10.1161/CIRCULATIONAHA.113.001252.
-
227Nascimento BR, Beaton AZ, Nunes MCP, Tompsett AR, Oliveira KKB, Diamantino AC, Barbosa MM, Lourenço TV, Teixeira IM, Ruiz GZL, Rios JPP, Ribeiro ALP, Sable C; PROVAR+ (Programa de RastreamentO da VAlvopatia Reumática and Other Cardiovascular Diseases) Investigators. Integration of Echocardiographic Screening by Non-Physicians With Remote Reading in Primary Care. Heart. 2019;105(4):283-290. doi: 10.1136/heartjnl-2018-313593.
-
228Diamantino AC, Nascimento BR, Beaton AZ, Nunes MCP, Oliveira KKB, Rabelo LC, Barbosa MM, Tompsett AR, Olivieri L, Mata MD, Costa WAA, Pereira AF, Diamantino LC, Ribeiro ALP, Sable C, Brant LCC. Atrial Fibrillation Detection With a Portable Device During Cardiovascular Screening in Primary Care. Heart. 2020;106(16):1261-66. doi: 10.1136/heartjnl-2019-316277.
-
229Nascimento BR, Brant LCC, Castro ACT, Froes LEV, Ribeiro ALP, Cruz LV, Araújo CB, Souza CF, Froes ET, Souza SD. Impact of a Large-Scale Telemedicine Network on Emergency Visits and Hospital Admissions During the Coronavirus Disease 2019 Pandemic in Brazil: Data From the UNIMED-BH System. J Telemed Telecare. 2020:1357633X20969529. doi: 10.1177/1357633X20969529.
-
230Pinto-Filho MM, Brant LCC, Foppa M, Garcia-Silva KB, Oliveira RAM, Fonseca MJM, Alvim S, Lotufo PA, Mill JG, Barreto SM, Macfarlane PW, Ribeiro ALP. Major Electrocardiographic Abnormalities According to the Minnesota Coding System Among Brazilian Adults (From the ELSA-Brasil Cohort Study). Am J Cardiol. 2017;119(12):2081-87. doi: 10.1016/j.amjcard.2017.03.043.
-
231Kawabata-Yoshihara LA, Benseñor IM, Kawabata VS, Menezes PR, Scazufca M, Lotufo PA. Prevalence of Electrocardiographic Findings in Elderly Individuals: the Sao Paulo Aging & Health Study. Arq Bras Cardiol. 2009;93(6):602-7, 651-6. doi: 10.1590/s0066-782x2009001200015.
» https://doi.org/10.1590/s0066-782x2009001200015 -
232Santos JPAD, Ribeiro ALP, Andrade-Junior D, Marcolino MS. Prevalence of Electrocardiographic Abnormalities in Primary Care Patients According to Sex and Age Group. A Retrospective Observational Study. Sao Paulo Med J. 2018;136(1):20-28. doi: 10.1590/1516-3180.2017.0222290817.
-
233Marcolino MS, Palhares DM, Benjamin EJ, Ribeiro ALp. Atrial Fibrillation: Prevalence in a Large Database of Primary Care Patients in Brazil. Europace. 2015;17(12):1787-90. doi: 10.1093/europace/euv185.
-
234Moraes ERFL, Cirenza C, Lopes RD, Carvalho AC, Guimaraes PO, Rodrigues AAE, Paola AAV. Prevalence of Atrial Fibrillation and Stroke Risk Assessment Based on Telemedicine Screening Tools in a Primary Healthcare Setting. Eur J Intern Med. 2019;67:36-41. doi: 10.1016/j.ejim.2019.04.024.
-
235Marcolino MS, Santos TMM, Stefanelli FC, Oliveira JAQ, Silva MVRS, Andrade DF Jr, Silva GKME, Ribeiro ALP. Cardiovascular Emergencies in Primary Care: An Observational Retrospective Study of a Large-Scale Telecardiology Service. Sao Paulo Med J. 2017;135(5):481-87. doi: 10.1590/1516-3180.2017.0090110617.
-
236Paixão GMM, Silva LGS, Gomes PR, Lima EM, Ferreira MPF, Oliveira DM, Ribeiro MH, Ribeiro AH, Nascimento JS, Canazart JA, Ribeiro LB, Benjamin EJ, Macfarlane PW, Marcolino MS, Ribeiro ALP. Evaluation of Mortality in Atrial Fibrillation: Clinical Outcomes in Digital Electrocardiography (CODE) Study. Glob Heart. 2020;15(1):48. doi: 10.5334/gh.772.
-
237Jerjes-Sanchez C, Corbalan R, Barretto ACP, Luciardi HL, Allu J, Illingworth L, Pieper KS, Kayani G; GARFIELD-AF Investigators. Stroke prevention in patients From Latin American Countries With Non-Valvular Atrial Fibrillation: Insights From the GARFIELD-AF Registry. Clin Cardiol. 2019;42(5):553-60. doi: 10.1002/clc.23176.
-
238Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of Atrial Fibrillation on the Risk of Death: the Framingham Heart Study. Circulation. 1998;98(10):946-52. doi: 10.1161/01.cir.98.10.946.
-
239Emdin CA, Wong CX, Hsiao AJ, Altman DG, Peters SA, Woodward M, Odutayo AA. Atrial Fibrillation as Risk Factor for Cardiovascular Disease and Death in Women Compared With Men: Systematic Review and Meta-Analysis of Cohort Studies. BMJ. 2016;532:h7013. doi: 10.1136/bmj.h7013.
-
240Ribeiro ALP, Marcolino MS, Prineas RJ, Lima-Costa MF. Electrocardiographic Abnormalities in Elderly Chagas Disease Patients: 10-Year Follow-Up of the Bambui Cohort Study of Aging. J Am Heart Assoc. 2014;3(1):e000632. doi: 10.1161/JAHA.113.000632.
-
241Amaral CHD, Amaral AR, Nagel V, Venancio V, Garcia AC, Magalhaes PS, Longo AL, Moro CH, Reis FI, D’Avila A, Cabral NL. Incidence and Functional Outcome of Atrial Fibrillation and Non-Atrial Fibrillation- Related Cardioembolic Stroke in Joinville, Brazil: A Population-Based Study. Arq Neuropsiquiatr. 2017;75(5):288-94. doi: 10.1590/0004-282X20170039.
-
242Lange MC, Ribas G, Scavasine V, Ducci RD, Mendes DC, Zétola VHF, Cabral N, Rundek T. Stroke Recurrence in the Different Subtypes of Ischemic Stroke. The Importance of the Intracranial Disease. Arq Neuropsiquiatr. 2018;76(10):649-53. doi: 10.1590/0004-282X20180095.
-
243Figueiredo MM, Rodrigues AC, Alves MB, Cendoroglo Neto M, Silva GS. Score for Atrial Fibrillation Detection in Acute Stroke and Transient Ischemic Attack Patients in a Brazilian Population: the Acute Stroke Atrial Fibrillation Scoring System. Clinics. 2014;69(4):241-6. doi: 10.6061/clinics/2014(04)04.
-
244Goulart AC, Olmos RD, Santos IS, Tunes G, Alencar AP, Thomas N, Lip GY, Lotufo PA, Benseñor IM. The Impact of Atrial Fibrillation and Long-Term Oral Anticoagulant Use on All-Cause and Cardiovascular Mortality: A 12-Year Evaluation of the Prospective Brazilian Study of Stroke Mortality and Morbidity. Int J Stroke. 2021:1747493021995592. doi: 10.1177/1747493021995592.
-
245Kawabata-Yoshihara LA, Scazufca M, Santos Ide S, Whitaker A, Kawabata VS, Benseñor IM, Menezes PR, Lotufo PA. Atrial Fibrillation and Dementia: Results From the Sao Paulo Ageing & Health Study. Arq Bras Cardiol. 2012;99(6):1108-14. doi: 10.1590/s0066-782x2012005000106.
» https://doi.org/10.1590/s0066-782x2012005000106 -
246Braga B, Poyares D, Cintra F, Guilleminault C, Cirenza C, Horbach S, Macedo D, Silva R, Tufik S, Paola AA. Sleep-Disordered Breathing and Chronic Atrial Fibrillation. Sleep Med. 2009;10(2):212-6. doi: 10.1016/j.sleep.2007.12.007.
-
247Lima C, Martinelli M, Peixoto GL, Siqueira SF, Wajngarten M, Silva RT, Costa R, Filho R, Ramires JA. Silent Atrial Fibrillation in Elderly Pacemaker Users: A Randomized Trial Using Home Monitoring. Ann Noninvasive Electrocardiol. 2016;21(3):246-55. doi: 10.1111/anec.12294.
-
248Kiuchi MG, Chen S, Silva GR, Paz LMR, Souto GLL. Register of Arrhythmias in Patients With Pacemakers and Mild to Moderate Chronic Kidney Disease (RYCKE): Results From an Observational Cohort Study. Relampa. 2016;29(2):49-56.
-
249Mendes FS, Atié J, Garcia MI, Gripp EA, Sousa AS, Feijó LA, Xavier SS. Atrial Fibrillation in Decompensated Heart Failure: Associated Factors and In-Hospital Outcome. Arq Bras Cardiol. 2014;103(4):315-22. doi: 10.5935/abc.20140123.
-
250Duarte PAD, Leichtweis GE, Andriolo L, Delevatti YA, Jorge AC, Fumagalli AC, Santos LC, Miura CK, Saito SK. Factors Associated With the Incidence and Severity of New-Onset Atrial Fibrillation in Adult Critically Ill Patients. Crit Care Res Pract. 2017;2017:8046240. doi: 10.1155/2017/8046240.
-
251Barbieri LR, Sobral ML, Gerônimo GM, Santos GG, Sbaraíni E, Dorfman FK, Stolf NA. Incidence of Stroke and Acute Renal Failure in Patients of Postoperative Atrial Fibrillation After Myocardial Revascularization. Rev Bras Cir Cardiovasc. 2013;28(4):442-8. doi: 10.5935/1678-9741.20130073.
-
252Bohatch MS Jr, Matkovski PD, Di Giovanni FJ, Fenili R, Varella EL, Dietrich A. Incidence of Postoperative Atrial Fibrillation in Patients Undergoing On-Pump and Off-Pump Coronary Artery Bypass Grafting. Rev Bras Cir Cardiovasc. 2015;30(3):316-24. doi: 10.5935/1678-9741.20150040.
-
253Folla CO, Melo CC, Silva RC. Predictive Factors of Atrial Fibrillation After Coronary Artery Bypass Grafting. Einstein. 2016;14(4):480-85. doi: 10.1590/S1679-45082016AO3673.
-
254Marcolino MS, Palhares DM, Ferreira LR, Ribeiro ALP. Electrocardiogram and Chagas Disease: A Large Population Database of Primary Care Patients. Glob Heart. 2015;10(3):167-72. doi: 10.1016/j.gheart.2015.07.001.
-
255Cardoso CS, Sabino EC, Oliveira CD, Oliveira LC, Ferreira AM, Cunha-Neto E, Bierrenbach AL, Ferreira JE, Haikal DS, Reingold AL, Ribeiro ALP. Longitudinal Study of Patients With Chronic Chagas Cardiomyopathy in Brazil (SaMi-Trop project): A Cohort Profile. BMJ Open. 2016 ;6(5):e011181. doi: 10.1136/bmjopen-2016-011181.
-
256Rojas LZ, Glisic M, Pletsch-Borba L, Echeverría LE, Bramer WM, Bano A, Stringa N, Zaciragic A, Kraja B, Asllanaj E, Chowdhury R, Morillo CA, Rueda-Ochoa OL, Franco OH, Muka T. Electrocardiographic Abnormalities in Chagas Disease in the General Population: A Systematic Review and Meta-Analysis. PLoS Negl Trop Dis. 2018;12(6):e0006567. doi: 10.1371/journal.pntd.0006567.
-
257Rassi A Jr, Rassi A, Little WC, Xavier SS, Rassi SG, Rassi AG, Rassi GG, Hasslocher-Moreno A, Sousa AS, Scanavacca MI. Development and Validation of a Risk Score for Predicting Death in Chagas’ Heart Disease. N Engl J Med. 2006;355(8):799-808. doi: 10.1056/NEJMoa053241.
-
258Silva PGMBE, Sznejder H, Vasconcellos R, Charles GM, Mendonca-Filho HTF, Mardekian J, Nascimento R, Dukacz S, Fusco MD. Anticoagulation Therapy in Patients With Non-valvular Atrial Fibrillation in a Private Setting in Brazil: A Real-World Study. Arq Bras Cardiol. 2020 Mar;114(3):457-466. doi: 10.36660/abc.20180076.
-
259Vinereanu D, Lopes RD, Bahit MC, Xavier D, Jiang J, Al-Khalidi HR, He W, Xian Y, Ciobanu AO, Kamath DY, Fox KA, Rao MP, Pokorney SD, Berwanger O, Tajer C, Silva PGMB, Roettig ML, Huo Y, Granger CB; IMPACT-AF Investigators. A Multifaceted Intervention to Improve Treatment With Oral Anticoagulants in Atrial Fibrillation (IMPACT-AF): An International, Cluster-Randomised Trial. Lancet. 2017;390(10104):1737-1746. doi: 10.1016/S0140-6736(17)32165-7.
» https://doi.org/10.1016/S0140-6736(17)32165-7 -
260Silva RMFLD, Silva PAE, Lima MC, Sant’Anna LT, Silva TC, Moreira PHV, Gandra RM, Cavalcanti TR, Mourão PHV. Thromboembolism and Bleeding Risk Scores and Predictors of Cardiac Death in a Population With Atrial Fibrillation. Arq Bras Cardiol. 2017;109(1):5-13. doi: 10.5935/abc.20170064.
-
261Martins MAP, Costa JM, Mambrini JVM, Ribeiro ALP, Benjamin EJ, Brant LCC, Paasche-Orlow MK, Magnani JW. Health Literacy and Warfarin Therapy at two Anticoagulation Clinics in Brazil. Heart. 2017;103(14):1089-95. doi: 10.1136/heartjnl-2016-310699.
-
262Marcatto LR, Sacilotto L, Darrieux FC, Hachul DT, Scanavacca MI, Krieger JE, Pereira AC, Santos PC. Age is Associated With Time in Therapeutic Range for Warfarin Therapy in Patients With Atrial Fibrillation. Oncotarget. 2016;7(34):54194-99. doi: 10.18632/oncotarget.10944.
-
263Silva RGl, Bertollo CM, Ferreira IG, Brant LCC, Martins MAP. Assessment of Oral Anticoagulation Control at Two Pharmacist-Managed Clinics in Brazil. Int J Clin Pharm. 2017;39(6):1157-61. doi: 10.1007/s11096-017-0511-x.
-
264Oliveira LH, Mallmann FB, Botelho FN, Paul LC, Gianotto M, Abt RB, Silva NJ, Luize CM, Nogueira FL, Carvalho RS, Paola AA, Cirenza C. Cross-Sectional Study of Treatment Strategies on Atrial Fibrillation. Arq Bras Cardiol. 2012;98(3):195-202. doi: 10.1590/s0066-782x2012005000020.
-
265van der Sand CR, Leiria TL, Kalil RA. Assessment of the Adherence of Cardiologists to Guidelines for the Treatment of Atrial Fibrillation. Arq Bras Cardiol. 2013;101(2):127-33. doi: 10.5935/abc.20130148.
-
266Lopes RD, Paola AA, Lorga Filho AM, Consolim-Colombo FM, Andrade J, Mattos LAP, Bernardez-Pereira S, Berwanger O, Figueiredo MJO; RECALL Steering Committee and Investigators. Rationale and Design of the First Brazilian Cardiovascular Registry of Atrial Fibrillation: The RECALL study. Am Heart J. 2016;176:10-6. doi: 10.1016/j.ahj.2016.03.001.
-
267Barroso WKS, Rodrigues CIS, Bortolotto LA, Mota-Gomes MA, Brandão AA, Feitosa ADM, Machado CA, Poli-de-Figueiredo CE, Amodeo C, Mion D Jr, Barbosa ECD, Nobre F, Guimarães ICB, Vilela-Martin JF, Yugar-Toledo JC, Magalhães MEC, Neves MFT, Jardim PCBV, Miranda RD, Póvoa RMDS, Fuchs SC, Alessi A, Lucena AJG, Avezum A, Sousa ALL, Pio-Abreu A, Sposito AC, Pierin AMG, Paiva AMG, Spinelli ACS, Nogueira ADR, Dinamarco N, Eibel B, Forjaz CLM, Zanini CRO, Souza CB, Souza DDSM, Nilson EAF, Costa EFA, Freitas EV, Duarte EDR, Muxfeldt ES, Lima Júnior E, Campana EMG, Cesarino EJ, Marques F, Argenta F, Consolim-Colombo FM, Baptista FS, Almeida FA, Borelli FAO, Fuchs FD, Plavnik FL, Salles GF, Feitosa GS, Silva GVD, Guerra GM, Moreno Júnior H, Finimundi HC, Back IC, Oliveira Filho JB, Gemelli JR, Mill JG, Ribeiro JM, Lotaif LAD, Costa LSD, Magalhães LBNC, Drager LF, Martin LC, Scala LCN, Almeida MQ, Gowdak MMG, Klein MRST, Malachias MVB, Kuschnir MCC, Pinheiro ME, Borba MHE, Moreira Filho O, Passarelli Júnior O, Coelho OR, Vitorino PVO, Ribeiro RM Jr, Esporcatte R, Franco R, Pedrosa R, Mulinari RA, Paula RB, Okawa RTP, Rosa RF, Amaral SLD, Ferreira-Filho SR, Kaiser SE, Jardim TSV, Guimarães V, Koch VH, Oigman W, Nadruz W. Brazilian Guidelines of Hypertension - 2020. Arq Bras Cardiol. 2021;116(3):516-658. doi: 10.36660/abc.20201238.
» https://doi.org/10.36660/abc.20201238 -
268Malta DC, Gonçalves RPF, Machado ÍE, Freitas MIF, Azeredo C, Szwarcwald CL. Prevalence of Arterial Hypertension According to Different Diagnostic Criteria, National Health Survey. Rev Bras Epidemiol. 2018;21(Suppl 1):e180021. doi: 10.1590/1980-549720180021.supl.1.
-
269Brant LCC, Nascimento BR, Veloso GA, Gomes CS, Polanczyk CA, Oliveira GMM, Ribeiro ALP, malta DC. Burden of Cardiovascular Diseases Attributable to Risk Factors in Brazil: Data From the Global Burden of Disease 2019. Rev Soc Bras Med Trop. 2021;2021(54). Epub ahead of print.
-
270Lopes JAS, Giatti L, Griep RH, Lopes AADS, Matos SMA, Chor D, Fonseca MJM, Barreto SM. Life Course Socioeconomic Position, Intergenerational Social Mobility, and Hypertension Incidence in ELSA-Brasil. Am J Hypertens. 2021;34(8):801-9. doi: 10.1093/ajh/hpab029.
-
271Malta DC, Santos NB, Perillo RD, Szwarcwald CL. Prevalence of High Blood Pressure Measured in the Brazilian Population, National Health Survey, 2013. Sao Paulo Med J. 2016;134(2):163-70. doi: 10.1590/1516-3180.2015.02090911.
-
272Chor D, Ribeiro ALP, Sá Carvalho M, Duncan BB, Lotufo PA, Nobre AA, Aquino EM, Schmidt MI, Griep RH, Mdel CM, Barreto SM, Passos VM, Benseñor IJ, Matos SM, Mill JG. Prevalence, Awareness, Treatment and Influence of Socioeconomic Variables on Control of High Blood Pressure: Results of the ELSA-Brasil Study. PLoS One. 2015;10(6):e0127382. doi: 10.1371/journal.pone.0127382.
-
273Santiago ERC, Diniz ADS, Oliveira JS, Leal VS, Andrade MIS, Lira PIC. Prevalence of Systemic Arterial Hypertension and Associated Factors Among Adults From the Semi-Arid Region of Pernambuco, Brazil. Arq Bras Cardiol. 2019;113(4):687-695. doi: 10.5935/abc.20190145.
-
274Barbosa JB, Silva AA, Santos AM, Monteiro F Jr, Barbosa MM, Barbosa MM, Figueiredo Neto JA, Soares Nde J, Nina VJ, Barbosa JN. Prevalence of Arterial Hypertension and Associated Factors in Adults in São Luís, State of Maranhão. Arq Bras Cardiol. 2008;91(4):236-42. doi: 10.1590/s0066-782x2008001600009.
-
275Picon RV, Fuchs FD, Moreira LB, Riegel G, Fuchs SC. Trends in Prevalence of Hypertension in Brazil: A Systematic Review With Meta-Analysis. PLoS One. 2012;7(10):e48255. doi: 10.1371/journal.pone.0048255.
-
276Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2019: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília: Ministério da Saúde; 2019.
-
277Nascimento BR, Brant LCC, Yadgir S, Oliveira GMM, Roth G, Glenn SD, Mooney M, Naghavi M, Passos VMA, Duncan BB, Silva DAS, Malta DC, Ribeiro ALP. Trends in Prevalence, Mortality, and Morbidity Associated With High Systolic Blood Pressure in Brazil From 1990 to 2017: Estimates From the “Global Burden of Disease 2017” (GBD 2017) study. Popul Health Metr. 2020;18(Suppl 1):17. doi: 10.1186/s12963-020-00218-z.
-
278Oliveira C, Marmot MG, Demakakos P, Mambrini JVM, Peixoto SV, Lima-Costa MF. Mortality Risk Attributable to Smoking, Hypertension and Diabetes Among English and Brazilian Older Adults (The ELSA and Bambui Cohort Ageing Studies). Eur J Public Health. 2016;26(5):831-5. doi: 10.1093/eurpub/ckv225.
-
279Villela PB, Klein CH, Oliveira GM. Trends in Mortality From Cerebrovascular and Hypertensive Diseases in Brazil Between 1980 and 2012. Arq Bras Cardiol. 2016;107(1):26-32. doi: 10.5935/abc.20160092.
-
280Villela PB, Klein CH, Oliveira GMM. Cerebrovascular and Hypertensive Diseases as Multiple Causes of Death in Brazil From 2004 to 2013. Public Health. 2018;161:36-42. doi: 10.1016/j.puhe.2018.04.006.
-
281Fuchs SC, Moreira LB, Camey SA, Moreira MB, Fuchs FD. Clustering of Risk Factors for Cardiovascular Disease Among Women in Southern Brazil: A Population-Based Study. Cad Saude Publica. 2008;24(Suppl 2):S285-93. doi: 10.1590/s0102-311x2008001400013.
-
282Carvalho MV, Siqueira LB, Sousa AL, Jardim PC. The Influence of Hypertension on Quality of life. Arq Bras Cardiol. 2013;100(2):164-74. doi: 10.5935/abc.20130030.
-
283Menezes ST, Giatti L, Brant LCC, Griep RH, Schmidt MI, Duncan BB, Suemoto CK, Ribeiro ALP, Barreto SM. Hypertension, Prehypertension, and Hypertension Control: Association With Decline in Cognitive Performance in the ELSA-Brasil Cohort. Hypertension. 2021;77(2):672-81. doi: 10.1161/HYPERTENSIONAHA.120.16080.
-
284Santos JC, Moreira TM. Risk Factors and Complications in Patients With Hypertension/Diabetes in a Regional Health District of Northeast Brazil. Rev Esc Enferm USP. 2012;46(5):1125-32. doi: 10.1590/s0080-62342012000500013.
-
285Nilson EAF, Andrade RDCS, Brito DA, Oliveira ML. Costs attributable to obesity, hypertension, and diabetes in the Unified Health System, Brazil, 2018. Rev Panam Salud Publica. 2020;44:e32. doi: 10.26633/RPSP.2020.32.
» https://doi.org/10.26633/RPSP.2020.32 -
286Marinho MG, Cesse EÂ, Bezerra AF, Sousa IM, Fontbonne A, Carvalho EF. Analysis of Health Care Costs of Patients With Diabetes Mellitus and Hypertension in a Public Health Reference Unit in Recife--Brazil. Arq Bras Endocrinol Metabol. 2011;55(6):406-11. doi: 10.1590/s0004-27302011000600007.
-
287Queiroz DC, Cantarutti DC, Turi BC, Fernandes RA, Codogno J. Association between Cardiovascular Diseases and Hospitalization Among Patients Users of the Brazilian National Health System. Medicina. 2016;49(1):52-9. doi: 10.11606/issn.2176-7262.v49i1p52-59.
-
288Macinko J, Leventhal DGP, Lima-Costa MF. Primary Care and the Hypertension Care Continuum in Brazil. J Ambul Care Manage. 2018;41(1):34-46. doi: 10.1097/JAC.0000000000000222.
-
289Sousa ALL, Batista SR, Sousa AC, Pacheco JAS, Vitorino PVO, Pagotto V. Hypertension Prevalence, Treatment and Control in Older Adults in a Brazilian Capital City. Arq Bras Cardiol. 2019;112(3):271-8. doi: 10.5935/abc.20180274.
-
290Rocha TPO, Figueredo-Neto JA, Fernandes DR, Santana EEC, Abreu JER, Cardoso RLS, Melo JB. A Comparative Study among Different Treatment Adherence Methods in Hypertensive Patients. Int J Cardiovasc Sci. 2015;28(2):122-129. doi: 10.5935/2359-4802.20150015.
-
291Souza NP, Cesse EÂP, Souza WV, Fontbonne A, Barreto MNSC, Goff ML, Batista Filho M, Féart C, Lira PIC. Temporal Variation in Prevalence, Awareness and Control of Hypertension in Urban and Rural Areas in Northeast Brazil between 2006 and 2016. Cad Saude Publica. 2020;36(4):e00027819. doi: 10.1590/0102-311X00027819.
-
292Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, Mill JG, Lotufo PA, Amodeo C, Batista MC, Bodanese LC, Carvalho ACC, Castro I, Chaves H, Costa EAS, Feitosa GS, Franco RJS, Fuchs FD, Guimarães AC, Jardim PC, Machado CA, Magalhães ME, Mion D Jr, Nascimento RM, Nobre F, Nóbrega AC, Ribeiro ALP, Rodrigues-Sobrinho CR, Sanjuliani AF, Teixeira MDCB, Krieger JE; ReHOT Investigators. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90. doi: 10.1161/HYPERTENSIONAHA.117.10662.
-
293Flor LS, Wilson S, Bhatt P, Bryant M, Burnett A, Camarda JN, Chakravarthy V, Chandrashekhar C, Chaudhury N, Cimini C, Colombara DV, Narayanan HC, Cortes ML, Cowling K, Daly J, Duber H, Kavinkare VE, Endlich P, Fullman N, Gabert R, Glucksman T, Harris KP, Bouskela MAL, Maia J, Mandile C, Marcolino MS, Marshall S, McNellan CR, Medeiros DS, Mistro S, Mulakaluri V, Murphree J, Ng M, Oliveira JAQ, Oliveira MG, Phillips B, Pinto V, Ngwato TP, Radant T, Reitsma MB, Ribeiro ALP, Roth G, Rumel D, Sethi G, Soares DA, Tamene T, Thomson B, Tomar H, Ugliara Barone MT, Valsangkar S, Wollum A, Gakidou E. Community-Based Interventions for Detection and Management of Diabetes and Hypertension in Underserved Communities: A Mixed-Methods Evaluation in Brazil, India, South Africa and the USA. BMJ Glob Health. 2020;5(6):e001959. doi: 10.1136/bmjgh-2019-001959.
-
294Treff CA Jr. Physical Activity in Leisure and in Transportation Associated With Hypertension in the Longitudinal Study of Adult Health (ELSA-Brazil) [dissertation]. São Paulo: Faculdade de Medicina, Universidade de São Paulo; 2015.
-
295Pavan L, Casiglia E, Pauletto P, Batista SL, Ginocchio G, Kwankam MM, Biasin R, Mazza A, Puato M, Russo E, Pessina AC. Blood Pressure, Serum Cholesterol and Nutritional State in Tanzania and in the Amazon: Comparison With an Italian Population. J Hypertens. 1997;15(10):1083-90. doi: 10.1097/00004872-199715100-00006.
-
296Jardim PC, Gondim MR, Monego ET, Moreira HG, Vitorino PV, Souza WK, Scala LC. High Blood Pressure and Some Risk Factors in a Brazilian capital. Arq Bras Cardiol. 2007;88(4):452-7. doi: 10.1590/s0066-782x2007000400015.
-
297Moreira APL, Malta DC, Vianna RP de T, Moreira PVL, Carvalho AT de. Risk and protection factors for self-reported hypertension and diabetes in João Pessoa, Brazil. The VIGITEL survey, 2014. A cross-sectional study. Sao Paulo Med J. 2017;135(5):450-461. doi:10.1590/1516-3180.2017.0044250517.
-
298Mill JG, Baldo MP, Molina MDCB, Schmidt MI, Barreto SM, Chor D, Griep RH, Matos SM, Ribeiro ALP, Duncan BB, Aquino EM, Lotufo PA, Bensenor I. Sex-Specific Patterns in the Association Between Salt Intake and Blood Pressure: The ELSA-Brasil study. J Clin Hypertens. 2019;21(4):502-509. doi: 10.1111/jch.13509.
-
299Bloch KV, Klein CH, Szklo M, Kuschnir MC, Abreu Gde A, Barufaldi LA, da Veiga GV, Schaan B, da Silva TL, de Vasconcellos MT, Moraes AJ, Borges AL, de Oliveira AM, Tavares BM, de Oliveira CL, Cunha Cde F, Giannini DT, Belfort DR, Santos EL, de Leon EB, Fujimori E, Oliveira ER, Magliano Eda S, Vasconcelos Fde A, Azevedo GD, Brunken GS, Guimarães IC, Faria Neto JR, Oliveira JS, de Carvalho KM, Gonçalves LG, Monteiro MI, Santos MM, Jardim PC, Ferreira PA, Montenegro RM Jr, Gurgel RQ, Vianna RP, Vasconcelos SM, Goldberg TB. ERICA: Prevalences of Hypertension and Obesity in Brazilian Adolescents. Rev Saude Publica. 2016;50(Suppl 1):9s. doi: 10.1590/S01518-8787.2016050006685.
-
300Christofaro DGD, Mesas AE, Ritti Dias RM, Fernandes RA, Saraiva BTC, Palma MR, Silva DAS, Andrade SM. Association Between Hypertension in Adolescents and the Health Risk Factors of Their Parents: An Epidemiological Family Study. J Am Soc Hypertens. 2018;12(3):182-9. doi: 10.1016/j.jash.2017.12.011.
-
301Burgos MS, Reuter CP, Burgos LT, Pohl HH, Pauli LT, Horta JA, Reckziegel MB, Franke SI, Prá D, Camargo M. Comparison Analysis of Blood Pressure, Obesity, and Cardio-Respiratory Fitness in Schoolchildren. Arq Bras Cardiol. 2010;94(6):788-93. doi: 10.1590/s0066-782x2010005000046.
-
302Schommer VA, Barbiero SM, Cesa CC, Oliveira R, Silva AD, Pellanda LC. Excess Weight, Anthropometric Variables and Blood Pressure in Schoolchildren Aged 10 to 18 Years. Arq Bras Cardiol. 2014;102(4):312-8. doi: 10.5935/abc.20140038.
-
303Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD; American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction: The American Heart Association’s Strategic Impact Goal Through 2020 and Beyond. Circulation. 2010;121(4):586-613. doi: 10.1161/CIRCULATIONAHA.109.192703.
-
304Oliveira JC, Barreto-Filho JA. Public health policy based on “made-in-Brazil” Science: a challenge for the Arquivos Brasileiros de Cardiologia. Arq Bras Cardiol. 2015;105(3):211-213. doi:10.5935/abc.20150120.
-
305Krumholz HM. Outcomes research: generating evidence for best practice and policies. Circulation. 2008;118(3):309-318. doi:10.1161/CIRCULATIONAHA.107.690917.
-
306Brasil. Ministério da Saúde. Pesquisa Nacional de Saúde: 2019: Percepção do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal - Brasil e Grandes Regiões. Brasília: IBGE; 2020.
-
307Kahn CR, Ferris HA, O’NEILL BT. Pathophysiology of Type 2 Diabetes Mellitus. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A. Williams Textbook of Endocrinology. 14th ed. Philadelphia: Elsevier; 2019. Chapter 34.
-
308Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241(19):2035-2038. doi:10.1001/jama.241.19.2035.
-
309MICHAEL BROWNLEE, LLOYD P. AIELLO, JENNIFER K. SUN, MARK E. COOPER, EVA L. FELDMAN, JORGE PLUTZKY, AND ANDREW J.M. BOULTON. Complications of Diabetes Mellitus. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A. Williams Textbook of Endocrinology. 14th.
-
310Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16(2):434-444. doi:10.2337/diacare.16.2.434.
-
311Telo GH, Cureau FV, de Souza MS, Andrade TS, Copês F, Schaan BD. Prevalence of diabetes in Brazil over time: a systematic review With meta-analysis. Diabetol Metab Syndr. 2016;8(1):65. doi:10.1186/s13098-016-0181-1.
-
312International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: International Diabetes Federation; 2019.
-
313Iser BPM, Pinheiro PC, Malta DC, Duncan BB, Schmidt MI. Prediabetes and intermediate hyperglycemia prevalence in adults and associated factors, Health National Survey. Cien Saude Colet. 2021;26(2):531-540. doi:10.1590/1413-81232021262.34852020.
-
314Telo GH, Cureau F V, Szklo M, Bloch K V, Schaan BD. Prevalence of type 2 diabetes among adolescents in Brazil: Findings From Study of Cardiovascular Risk in Adolescents (ERICA). Pediatr Diabetes. 2019;20(4):389-396. doi:10.1111/pedi.12828.
-
315Schmidt MI, Bracco PA, Yudkin JS, Bensenor IM, Griep RH, Barreto SM, Castilhos CD, Duncan BB. Intermediate Hyperglycaemia to Predict Progression to Type 2 Diabetes (ELSA-Brasil): An Occupational Cohort Study in Brazil. Lancet Diabetes Endocrinol. 2019;7(4):267-77. doi: 10.1016/S2213-8587(19)30058-0.
-
316Sitnik D, Santos IS, Goulart AC, Staniak HL, Manson JE, Lotufo PA, Bensenor IM. Fasting Glucose Levels, Incident Diabetes, Subclinical Atherosclerosis and Cardiovascular Events in Apparently Healthy Adults: A 12-year Longitudinal Study. Diab Vasc Dis Res. 2016;13(6):429-37. doi: 10.1177/1479164116653356.
-
317Group DP. Incidence and trends of childhood Type 1 diabetes worldwide 1990-1999. Diabet Med. 2006;23(8):857-866. doi:10.1111/j.1464-5491.2006.01925.x.
-
318Patterson CC, Harjutsalo V, Rosenbauer J, Neu A, Cinek O, Skrivarhaug T, Rami-Merhar B, Soltesz G, Svensson J, Parslow RC, Castell C, Schoenle EJ, Bingley PJ, Dahlquist G, Jarosz-Chobot PK, Marčiulionytė D, Roche EF, Rothe U, Bratina N, Ionescu-Tirgoviste C, Weets I, Kocova M, Cherubini V, Rojnic Putarek N, deBeaufort CE, Samardzic M, Green A. Trends and Cyclical Variation in the Incidence of Childhood Type 1 Diabetes in 26 European Centres in the 25 Year Period 1989-2013: A Multicentre Prospective Registration Study. Diabetologia. 2019;62(3):408-17. doi: 10.1007/s00125-018-4763-3.
-
319Negrato CA, Lauris JRP, Saggioro IB, Corradini MCM, Borges PR, Crês MC, Leal A Jr, Guedes MFS, Gomes MB. Increasing Incidence of Type 1 Diabetes Between 1986 and 2015 in Bauru, Brazil. Diabetes Res Clin Pract. 2017;127:198-204. doi: 10.1016/j.diabres.2017.03.014.
-
320Klafke A, Duncan BB, Stevens A, Rosa Rdos S, Moura L, Malta D, Schmidt MI. The Decline in Mortality Due to Acute Complications of Diabetes Mellitus in Brazil, 1991-2010. BMC Public Health. 2015;15:772. doi: 10.1186/s12889-015-2123-5.
-
321Malhão TA, Brito ADS, Pinheiro RS, Cabral C da S, Camargo TMCR de, Coeli CM. Sex Differences in Diabetes Mellitus Mortality Trends in Brazil, 1980-2012. PLoS One. 2016;11(6):e0155996. doi:10.1371/journal.pone.0155996.
-
322Duncan BB, França EB, Passos VMA, Cousin E, Ishitani LH, Malta DC, Naghavi M, Mooney M, Schmidt MI. The Burden of Diabetes and Hyperglycemia in Brazil and its States: Findings From the Global Burden of Disease Study 2015. Rev Bras Epidemiol. 2017;20(Suppl 01):90-101. doi: 10.1590/1980-5497201700050008.
-
323Duncan BB, Cousin E, Naghavi M, Afshin A, França EB, Passos VMA, Malta D, Nascimento BR, Schmidt MI. The Burden of Diabetes and Hyperglycemia in Brazil: A Global Burden of Disease Study 2017. Popul Health Metr. 2020;18(Suppl 1):9. doi: 10.1186/s12963-020-00209-0.
-
324Cardoso CRL, Leite NC, Salles GF. Prognostic Importance of C-Reactive Protein in High Cardiovascular Risk Patients With Type 2 Diabetes Mellitus: The Rio de Janeiro Type 2 Diabetes Cohort Study. J Am Heart Assoc. 2016;5(11). doi:10.1161/JAHA.116.004554.
-
325. Diabetes and cardiovascular events in high-risk patients: Insights From a multicenter registry in a middle-income country Beatriz D Schaan 1, Jose Albuquerque de Figueiredo Neto 2, Leila Beltrami Moreira 3, Priscila Ledur 4, Luiz Alberto P Mattos 5, Danie.
-
326Rezende PC, Hlatky MA, Hueb W, Garcia RMR, Selistre LS, Lima EG, Garzillo CL, Scudeler TL, Boros GAB, Ribas FF, Serrano CV Jr, Ramires JAF, Kalil Filho R. Association of Longitudinal Values of Glycated Hemoglobin With Cardiovascular Events in Patients With Type 2 Diabetes and Multivessel Coronary Artery Disease. JAMA Netw Open. 2020;3(1):e1919666. doi: 10.1001/jamanetworkopen.2019.19666.
-
327Gomes MB, Negrato CA. Adherence to insulin therapeutic regimens in patients With type 1 diabetes. A nationwide survey in Brazil. Diabetes Res Clin Pract. 2016;120:47-55. doi:10.1016/j.diabres.2016.07.011.
-
328Cortez DN, Macedo MM, Souza DA, Santos JC, Afonso GS, Reis IA, Torres HC. Evaluating the Effectiveness of an Empowerment Program for Self-Care in Type 2 Diabetes: A Cluster Randomized Trial. BMC Public Health. 2017;17(1):41. doi: 10.1186/s12889-016-3937-5.
-
329Meiners MMMA, Tavares NUL, Guimarães LSP, Bertoldi AD, Pizzol TDSD, Luiza VL, Mengue SS, Merchan-Hamann E. Access and Adherence to Medication Among People With Diabetes in Brazil: Evidences From PNAUM. Rev Bras Epidemiol. 2017;20(3):445-59. doi: 10.1590/1980-5497201700030008.
-
330Marinho FS, Moram CBM, Rodrigues PC, Leite NC, Salles GF, Cardoso CRL. Treatment Adherence and Its Associated Factors in Patients With Type 2 Diabetes: Results From the Rio de Janeiro Type 2 Diabetes Cohort Study. J Diabetes Res. 2018;2018:8970196. doi:10.1155/2018/8970196.
-
331Silva MRRD, Diniz LM, Santos JBRD, Reis EA, Mata ARD, Araújo VE, Álvares J, Acurcio FA. Drug Utilization and faCtors Associated With Polypharmacy in Individuals With Diabetes Mellitus in Minas Gerais, Brazil. Cien Saude Colet. 2018;23(8):2565-2574. doi: 10.1590/1413-81232018238.10222016.
-
332Leitão VBG, Francisco PMSB, Malta DC, Costa KS. Tendency of use and sources for obtaining oral antidiabetic drugs for treatment of diabetes in Brazil From 2012 to 2018: analysis of the Vigitel survey. Rev Bras Epidemiol. 2021;24:e210008. doi:10.1590/1980-549720210008.
-
333Duarte FG, Moreira SS, Almeida MDCC, Souza Teles CA, Andrade CS, Reingold AL, Moreira ED Jr. Sex Differences and Correlates of Poor Glycaemic Control in Type 2 Diabetes: A Cross-Sectional Study in Brazil and Venezuela. BMJ Open. 2019;9(3):e023401. doi: 10.1136/bmjopen-2018-023401.
-
334Schneiders J, Telo GH, Bottino LG, Pasinato B, Neyeloff JL, Schaan BD. Quality indicators in type 2 diabetes patient care: analysis per care-complexity level. Diabetol Metab Syndr. 2019;11:34. doi:10.1186/s13098-019-0428-8.
-
335Alessi J, Telo GH, Oliveira GB, Schneiders J, Zanella MJB, Schaan BD. The Rational Treatment of Diabetes Mellitus in Older Adults: The adequacy of Treatment Decisions Based on Individualized Glycemic Targets in Primary and Tertiary Care. J Diabetes Complications. 2021;35(4):107835. doi: 10.1016/j.jdiacomp.2020.107835.
-
336Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, Lifestyle, and the Risk of Type 2 Diabetes Mellitus in Women. N Engl J Med. 2001;345(11):790-7. doi: 10.1056/NEJMoa010492.
-
337Sbaraini M, Cureau FV, Ritter JDA, Schuh DS, Madalosso MM, Zanin G, Goulart MR, Pellanda LC, Schaan BD. Prevalence of Overweight and Obesity Among Brazilian Adolescents Over Time: A Systematic Review and Meta-Analysis. Public Health Nutr. 2021:1-12. doi: 10.1017/S1368980021001464.
-
338Sbaraini M, Cureau FV, Sparrenberger K, Teló GH, Kuschnir MCC, Oliveira JS, Leal VS, Bloch KV, Schaan BD. Severity of Obesity is Associated With Worse Cardiometabolic Risk Profile in Adolescents: Findings From a Brazilian National Study (ERICA). Nutrition. 2020;75-6:110758. doi: 10.1016/j.nut.2020.110758.
-
339Flor LS, Campos MR, Oliveira AF, Schramm JM. Diabetes Burden in Brazil: Fraction Attributable to Overweight, Obesity, and Excess Weight. Rev Saude Publica. 2015;49:29. doi: 10.1590/s0034-8910.2015049005571.
-
340Lotufo PA, Santos RD, Figueiredo RM, Pereira AC, Mill JG, Alvim SM, Fonseca MJ, Almeida MC, Molina MC, Chor D, Schmidt MI, Ribeiro ALP, Duncan BB, Bensenor IM. Prevalence, Awareness, Treatment, and Control of High Low-Density Lipoprotein Cholesterol in Brazil: Baseline of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Clin Lipidol. 2016;10(3):568-76. doi: 10.1016/j.jacl.2015.12.029.
-
341Oliveira AP, Maia EG, Silva FM, Martins APB, Claro RM. Needed Improvements in Diabetes Prevention and Management in Brazil. Prev Chronic Dis. 2018;15:E153. doi: 10.5888/pcd15.180269.
-
342Drehmer M, Pereira MA, Schmidt MI, Molina MDCB, Alvim S, Lotufo PA, Duncan BB. Associations of Dairy Intake With Glycemia and Insulinemia, Independent of Obesity, in Brazilian Adults: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Am J Clin Nutr. 2015;101(4):775-82. doi: 10.3945/ajcn.114.102152.
-
343Lin X, Alvim SM, Simoes EJ, Bensenor IM, Barreto SM, Schmidt MI, Ribeiro ALP, Pitanga F, Almeida MC, Liu S, Lotufo PA. Leisure Time Physical Activity and Cardio-Metabolic Health: Results From the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Am Heart Assoc. 2016;5(6):e003337. doi: 10.1161/JAHA.116.003337.
-
344Werneck AO, Cyrino ES, Collings PJ, Ronque ERV, Szwarcwald CL, Sardinha LB, Silva DR. TV Viewing in 60,202 Adults From the National Brazilian Health Survey: Prevalence, Correlates, and Associations With Chronic Diseases. J Phys Act Health. 2018;15(7):510-5. doi: 10.1123/jpah.2017-0317.
-
345Malta DC, Duncan BB, Schmidt MI, Machado ÍE, Silva AGD, Bernal RTI, Pereira CA, Damacena GN, Stopa SR, Rosenfeld LG, Szwarcwald CL. Prevalence of Diabetes Mellitus as Determined by Glycated Hemoglobin in the Brazilian Adult Population, National Health Survey. Rev Bras Epidemiol. 2019;22(Suppl 02):E190006.SUPL.2. doi: 10.1590/1980-549720190006.supl.2.
-
346Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, Daemen MJ, Demer LL, Hegele RA, Nicholls SJ, Nordestgaard BG, Watts GF, Bruckert E, Fazio S, Ference BA, Graham I, Horton JD, Landmesser U, Laufs U, Masana L, Pasterkamp G, Raal FJ, Ray KK, Schunkert H, Taskinen MR, van de Sluis B, Wiklund O, Tokgozoglu L, Catapano AL, Ginsberg HN. Low-Density Lipoproteins Cause Atherosclerotic Cardiovascular Disease: Pathophysiological, Genetic, and Therapeutic Insights: A Consensus Statement From the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2020;41(24):2313-30. doi: 10.1093/eurheartj/ehz962.
-
347Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):596-646. doi: 10.1161/CIR.0000000000000678.
-
348Malta DC, Szwarcwald CL, Machado ÍE, Pereira CA, Figueiredo AW, Sá ACMGN, Velasquez-Melendez G, Santos FMD, Souza PB Jr, Stopa SR, Rosenfeld LG. Prevalence of Altered total Cholesterol and Fractions in the Brazilian Adult Population: National Health Survey. Rev Bras Epidemiol. 2019;22(Suppl 2):E190005.SUPL.2. doi: 10.1590/1980-549720190005.
» https://doi.org/10.1590/1980-549720190005 -
349Faria Neto JR, Bento VF, Baena CP, Olandoski M, Gonçalves LG, Abreu Gde A, Kuschnir MC, Bloch KV. ERICA: Prevalence of Dyslipidemia in Brazilian Adolescents. Rev Saude Publica. 2016;50(Suppl 1):10s. doi: 10.1590/S01518-8787.2016050006723.
-
350Rosini N, Machado MJ, Webster IZ, Moura SA, Cavalcante LS, Silva EL. Simultaneous Prediction of Hyperglycemia and Dyslipidemia in School Children in Santa Catarina State, Brazil Based on Waist Circumference Measurement. Clin Biochem. 2013;46(18):1837-41. doi: 10.1016/j.clinbiochem.2013.08.015.
-
351Almeida PCD, Silva JP, Pinasco GC, Hegner CC, Mattos DC, Potratz MO, Bravin LS, Silva VR, Lamounier JA. Lipid Profile in Schoolchildren in Vitória – Brazil. J Hum Growth Dev. 2016;26(1):61-6. doi: doi.org/10.7322/jhgd.110989.
-
352Alcântara Neto OD, Silva RC, Assis AM, Pinto Ede J. Factors Associated With Dyslipidemia in Children and Adolescents Enrolled in Public Schools of Salvador, Bahia. Rev Bras Epidemiol. 2012;15(2):335-45. doi: 10.1590/s1415-790x2012000200011.
-
353Silva RC, Diniz MF, Alvim S, Vidigal PG, Fedeli LM, Barreto SM. Physical Activity and Lipid Profile in the ELSA- Brasil Study. Arq Bras Cardiol. 2016;107(1):10-9. doi: 10.5935/abc.20160091.
-
354Moura FA, Dutra-Rodrigues MS, Cassol AS, Parra ES, Zago VH, Panzoldo NB, Alexandre F, Vieira IC, Vendrame F, Virginio VW, Castanho VS, Danelon MR, Nunes VS, Leança CC, Saraiva FK, Coelho OR, Nakandakare E, Quintão EC, de Faria EC, Sposito AC. Impact of Seasonality on the Prevalence of Dyslipidemia: A Large Population Study. Chronobiol Int. 2013;30(8):1011-5. doi: 10.3109/07420528.2013.793698.
-
355Santos RD, Bensenor IM, Pereira AC, Lotufo PA. Dyslipidemia According to Gender and Race: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Clin Lipidol. 2016;10(6):1362-8. doi: 10.1016/j.jacl.2016.08.008.
-
356Martinez TL, Santos RD, Armaganijan D, Torres KP, Loures-Vale A, Magalhães ME, Lima JC, Moriguchi E, Amodeo C, Ortiz J. National Alert Campaign About Increased Cholesterol: Determination of Cholesterol Levels in 81,262 Brazilians. Arq Bras Cardiol. 2003;80(6):635-8, 631-4. doi: 10.1590/s0066-782x2003000600006.
-
357Harada PH, Miname MH, Benseñor IM, Santos RD, Lotufo PA. Familial Hypercholesterolemia Prevalence in an Admixed Racial Society: Sex and Race Matter. The ELSA-Brasil. Atherosclerosis. 2018;277:273-7. doi: 10.1016/j.atherosclerosis.2018.08.021.
-
358Jannes CE, Santos RD, Silva PRS, Turolla L, Gagliardi AC, Marsiglia JD, Chacra AP, Miname MH, Rocha VZ, Salgado Filho W, Krieger JE, Pereira AC. Familial Hypercholesterolemia in Brazil: Cascade Screening Program, Clinical and Genetic Aspects. Atherosclerosis. 2015;238(1):101-7. doi: 10.1016/j.atherosclerosis.2014.11.009.
-
359Santos RD, Pereira C, Cesena F, Laurinavicius AG, Tabone V, Bittencourt MS. Cardiovascular Risk Misperception and Low Awareness of Familial Hypercholesterolemia in Individuals With Severe Hypercholesterolemia. Arq Bras Cardiol. 2021;116(4):706-12. doi: 10.36660/abc.20190516.
-
360Generoso G, Bensenor IM, Santos RD, Staniak HL, Sharovsky R, Santos IS, Goulart AC, Jones SR, Kulkarni KR, Blaha MJ, Toth PP, Lotufo PA, Bittencourt MS. High-density Lipoprotein-cholesterol Subfractions and Coronary Artery Calcium: The ELSA-Brasil Study. Arch Med Res. 2019;50(6):362-7. doi: 10.1016/j.arcmed.2019.10.006.
-
361Generoso G, Bensenor IM, Santos IS, Santos RD, Goulart AC, Jones SR, Kulkarni KR, Blaha MJ, Toth PP, Lotufo PA, Bittencourt MS. Diabetes Alters the Association Between High-Density Lipoprotein Subfractions and Carotid Intima-Media Thickness: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Diab Vasc Dis Res. 2018;15(6):541-7. doi: 10.1177/1479164118788080.
-
362Laurinavicius AG, Santos IS, Santos RD, Bensenor IM, Conceição RD, Lotufo PA. Extremely Elevated HDL-Cholesterol Levels are not Associated With Increased Carotid Intima-Media Thickness: Data From ELSA Brasil. J Clin Lipidol. 2016;10(4):898-904.e1. doi: 10.1016/j.jacl.2016.03.007.
-
363Bittencourt MS, Santos RD, Staniak H, Sharovsky R, Kondapally R, Vallejo-Vaz AJ, Ray KK, Bensenor I, Lotufo P. Relation of Fasting Triglyceride-Rich Lipoprotein Cholesterol to Coronary Artery Calcium Score (From the ELSA-Brasil Study). Am J Cardiol. 2017;119(9):1352-8. doi: 10.1016/j.amjcard.2017.01.033.
-
364Freitas WM, Quaglia LA, Santos SN, Paula RC, Santos RD, Blaha M, Rivera JJ, Cury R, Blumenthal R, Nadruz-Junior W, Agatston A, Figueiredo VN, Nasir K, Sposito AC; Brazilian Study on Healthy Aging. Low HDL Cholesterol but not High LDL Cholesterol is Independently Associated With Subclinical Coronary Atherosclerosis in Healthy Octogenarians. Aging Clin Exp Res. 2015;27(1):61-7. doi: 10.1007/s40520-014-0249-4..
-
365World Health Organization. Obesity [Internet]. Geneva: World Health Organization; 2020. [cited 2021 Nov 09]. Available From: https://www.who.int/health-topics/obesity
» https://www.who.int/health-topics/obesity -
366Nuttall FQ. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today. 2015;50(3):117-28. doi: 10.1097/NT.0000000000000092.
-
367Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy Weight and Obesity Prevention: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72(13):1506-31. doi: 10.1016/j.jacc.2018.08.1037.
-
368Felisbino-Mendes MS, Cousin E, Malta DC, Machado ÍE, Ribeiro ALP, Duncan BB, Schmidt MI, Silva DAS, Glenn S, Afshin A, Velasquez-Melendez G. The Burden of Non-Communicable Diseases Attributable to High BMI in Brazil, 1990-2017: Findings From the Global Burden of Disease Study. Popul Health Metr. 2020;18(Suppl 1):18. doi: 10.1186/s12963-020-00219-y.
-
369Peng W, Berry EM. Global Nutrition 1990-2015: A Shrinking Hungry, and Expanding Fat World. PLoS One. 2018;13(3):e0194821. doi: 10.1371/journal.pone.0194821.
-
370Flores-Ortiz R, Malta DC, Velasquez-Melendez G. Adult Body Weight Trends in 27 Urban Populations of Brazil From 2006 to 2016: A Population-Based Study. PLoS One. 2019;14(3):e0213254. doi: 10.1371/journal.pone.0213254.
-
371Araújo FG, Velasquez-Melendez G, Felisbino-Mendes MS. Prevalence Trends of Overweight, Obesity, Diabetes and Hypertension Among Brazilian Women of Reproductive Age Based on Sociodemographic Characteristics. Health Care Women Int. 2019;40(4):386-406. doi: 10.1080/07399332.2019.1570516.
-
372Pereira JC, Barreto SM, Passos VM. The Profile of Cardiovascular Health of Elderly Brazilian People Needs to Improve: A Population-Based Study. Arq Bras Cardiol. 2008;91(1):1-10. doi: 10.1590/s0066-782x2008001300001.
-
373França AP; Aldrighi JM, Marucci MFN. Factors associated With body and abdominal obesity in post-menopausal women. Rev Bras Saude Mater Infant. 2008:8(1):65-73. doi: 10.1590/S1519-38292008000100008.
-
374Velasquez-Melendez G, Felisbino-Mendes MS, Matozinhos FP, ClaroI R, Gomes CS, Malta DC. Ideal cardiovascular health prevalence in the Brazilian population – National Health Survey (2013). Rev Bras Epidemiol. 2015;18(Suppl 2):97-108. doi: 10.1590/1980-5497201500060009.
-
375Diniz MFHS, Beleigoli AMR, Ribeiro ALP, Vidigal PG, Bensenor IM, Lotufo PA, Duncan BB, Schmidt MI, Barreto SM. Factors Associated With Metabolically Healthy Status in Obesity, Overweight, and Normal Weight at Baseline of ELSA-Brasil. Medicine. 2016;95(27):e4010. doi: 10.1097/MD.0000000000004010.
-
376Oliveira TL, Griep RH, Guimarães JN, Giatti L, Chor D, Fonseca MJM. Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): Socio-Occupational Class as an Effect Modifier for the Relationship Between Adiposity Measures and Self-Rated Health. BMC Public Health. 2019;19(1):734. doi: 10.1186/s12889-019-7072-y.
-
377Pinto KA, Griep RH, Rotenberg L, Almeida MCC, Barreto RS, Aquino EML. Gender, Time Use and Overweight and Obesity in Adults: Results of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). PLoS One. 2018;13(3):e0194190. doi: 10.1371/journal.pone.0194190.
-
378Chaparro MP, Pina MF, Cardoso LO, Santos SM, Barreto SM, Giatti Gonçalves L, Matos SMA, Fonseca MMJ, Chor D, Griep RH. The Association Between the Neighbourhood Social Environment and Obesity in Brazil: A Cross-Sectional Analysis of the ELSA-Brasil Study. BMJ Open. 2019;9(9):e026800. doi: 10.1136/bmjopen-2018-026800.
-
379Aiello AM, Mello LM, Nunes MS, Silva AS, Nunes A. Prevalence of Obesity in Children and Adolescents in Brazil: A Meta-analysis of Cross-sectional Studies. Curr Pediatr Rev. 2015;11(1):36-42. doi: 10.2174/1573396311666150501003250.
-
380GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, Salama JS, Vos T, Abate KH, Abbafati C, Ahmed MB, Al-Aly Z, Alkerwi A, Al-Raddadi R, Amare AT, Amberbir A, Amegah AK, Amini E, Amrock SM, Anjana RM, Ärnlöv J, Asayesh H, Banerjee A, Barac A, Baye E, Bennett DA, Beyene AS, Biadgilign S, Biryukov S, Bjertness E, Boneya DJ, Campos-Nonato I, Carrero JJ, Cecilio P, Cercy K, Ciobanu LG, Cornaby L, Damtew SA, Dandona L, Dandona R, Dharmaratne SD, Duncan BB, Eshrati B, Esteghamati A, Feigin VL, Fernandes JC, Fürst T, Gebrehiwot TT, Gold A, Gona PN, Goto A, Habtewold TD, Hadush KT, Hafezi-Nejad N, Hay SI, Horino M, Islami F, Kamal R, Kasaeian A, Katikireddi SV, Kengne AP, Kesavachandran CN, Khader YS, Khang YH, Khubchandani J, Kim D, Kim YJ, Kinfu Y, Kosen S, Ku T, Defo BK, Kumar GA, Larson HJ, Leinsalu M, Liang X, Lim SS, Liu P, Lopez AD, Lozano R, Majeed A, Malekzadeh R, Malta DC, Mazidi M, McAlinden C, McGarvey ST, Mengistu DT, Mensah GA, Mensink GBM, Mezgebe HB, Mirrakhimov EM, Mueller UO, Noubiap JJ, Obermeyer CM, Ogbo FA, Owolabi MO, Patton GC, Pourmalek F, Qorbani M, Rafay A, Rai RK, Ranabhat CL, Reinig N, Safiri S, Salomon JA, Sanabria JR, Santos IS, Sartorius B, Sawhney M, Schmidhuber J, Schutte AE, Schmidt MI, Sepanlou SG, Shamsizadeh M, Sheikhbahaei S, Shin MJ, Shiri R, Shiue I, Roba HS, Silva DAS, Silverberg JI, Singh JA, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tegegne BS, Terkawi AS, Thakur JS, Tonelli M, Topor-Madry R, Tyrovolas S, Ukwaja KN, Uthman OA, Vaezghasemi M, Vasankari T, Vlassov VV, Vollset SE, Weiderpass E, Werdecker A, Wesana J, Westerman R, Yano Y, Yonemoto N, Yonga G, Zaidi Z, Zenebe ZM, Zipkin B, Murray CJL. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13-27. doi: 10.1056/NEJMoa1614362.
» https://doi.org/10.1056/NEJMoa1614362 -
381Matos SMA, Duncan BB, Bensenor IM, Mill JG, Giatti L, Molina MDCB, Fonseca MJM, Schmidt MI, Lotufo PA, Griep RH, Barreto SM, Almeida MDCC. Incidence of Excess Body Weight and Annual Weight Gain in Women and Men: Results From the ELSA-Brasil Cohort. Am J Hum Biol. 2021:e23606. doi: 10.1002/ajhb.23606.
-
382Conde WL, Borges C. The Risk of Incidence and Persistence of Obesity Among Brazilian Adults According to Their Nutritional Status at the end of Adolescence. Rev Bras Epidemiol. 2011;14(Suppl 1):71-9. doi: 10.1590/s1415-790x2011000500008.
-
383Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, Cairns BJ, Huxley R, Jackson ChL, Joshy G, Lewington S, Manson JE, Murphy N, Patel AV, Samet JM, Woodward M, Zheng W, Zhou M, Bansal N, Barricarte A, Carter B, Cerhan JR, Smith GD, Fang X, Franco OH, Green J, Halsey J, Hildebrand JS, Jung KJ, Korda RJ, McLerran DF, Moore SC, O’Keeffe LM, Paige E, Ramond A, Reeves GK, Rolland B, Sacerdote C, Sattar N, Sofianopoulou E, Stevens J, Thun M, Ueshima H, Yang L, Yun YD, Willeit P, Banks E, Beral V, Chen Zh, Gapstur SM, Gunter MJ, Hartge P, Jee SH, Lam TH, Peto R, Potter JD, Willett WC, Thompson SG, Danesh J, Hu FB. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-86. doi: 10.1016/S0140-6736(16)30175-1.
-
384Beleigoli AM, Boersma E, Diniz MF, Lima-Costa MF, Ribeiro ALP. Overweight and Class I Obesity are Associated With Lower 10-Year Risk of Mortality in Brazilian Older Adults: The Bambuí Cohort Study of Ageing. PLoS One. 2012;7(12):e52111. doi: 10.1371/journal.pone.0052111.
-
385Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects), Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Metabolic Mediators of the Effects of Body-Mass Index, Overweight, and Obesity on Coronary Heart Disease and Stroke: A Pooled Analysis of 97 Prospective Cohorts With 1·8 Million Participants. Lancet. 2014;383(9921):970-83. doi: 10.1016/S0140-6736(13)61836-X.
-
386Agrawal S, Agrawal PK. Association Between Body Mass index and Prevalence of Multimorbidity in Low-and Middle-income Countries: A Cross-Sectional Study. Int J Med Public Health. 2016;6(2):73-83. doi: 10.5530/ijmedph.2016.2.5.
-
387Rimes-Dias KA, Canella DS. Medication Use and Obesity in Brazil: Results From the National Health Survey. Sci Rep. 2020;10(1):18856. doi: 10.1038/s41598-020-76058-6.
-
388Gomes IC, Santos VR, Christofaro DGD, Fernandes RA, Bueno DR, Freitas Júnior IF. Cardiovascular risk factors and body fat distribution in the oldest elderly. Medicina; 2016;49(1):17-25.
-
389Cayres SU, Kemper HCG, Vanderlei LCM, Casonatto J, Machado-Rodrigues AM, Barbosa MF, Fernandes RA. Changes in Body Fatness Affect Cardiovascular Outcomes More Than Changes in Physical Activity. Cardiol Young. 2017;27(6):1060-7. doi: 10.1017/S1047951116001992.
-
390Rabacow FM, Azeredo CM, Rezende LFM. Deaths Attributable to High Body Mass in Brazil. Prev Chronic Dis. 2019;16:E141. doi: 10.5888/pcd16.190143.
-
391Gomes DCK, Sichieri R, Verly E Jr, Boccolini CS, de Moura Souza A, Cunha DB. Trends in Obesity Prevalence Among Brazilian Adults From 2002 to 2013 by Educational Level. BMC Public Health. 2019;19(1):965. doi: 10.1186/s12889-019-7289-9.
-
392Bahia L, Coutinho ES, Barufaldi LA, Abreu G A, Malhão TA, Souza CP, Araujo DV. The Costs of Overweight and Obesity-Related Diseases in the Brazilian Public Health System: Cross-Sectional Study. BMC Public Health. 2012;12:440. doi: 10.1186/1471-2458-12-440.
-
393Sichieri R, do Nascimento S, Coutinho W. The Burden of Hospitalization Due to Overweight and Obesity in Brazil. Cad Saude Publica. 2007;23(7):1721-7. doi: 10.1590/s0102-311x2007000700025.
-
394Assumpção RP, Bahia LR, Rosa MQM, Correia MG, Silva EN, Zubiaurre PR, Mottin CC, Vianna DA. Cost-Utility of Gastric Bypass Surgery Compared to Clinical Treatment for Severely Obese With and Without Diabetes in the Perspective of the Brazilian Public Health System. Obes Surg. 2019;29(10):3202-11. doi: 10.1007/s11695-019-03957-7.
-
395Nilson EAF, Andrade RCS, Brito DA, Oliveira ML. Costs Attributable to Obesity, Hypertension, and Diabetes in the Unified Health System, Brazil, 2018. Rev Panam Salud Publica. 2020;44:e32. doi: 10.26633/RPSP.2020.32.
» https://doi.org/10.26633/RPSP.2020.32 -
396Rtveladze K, Marsh T, Webber L, Kilpi F, Levy D, Conde W, McPherson K, Brown M. Health and Economic Burden of Obesity in Brazil. PLoS One. 2013;8(7):e68785. doi: 10.1371/journal.pone.0068785.
-
397World Health Organization. Obesity [Internet]. Geneva: World Health Organization; 2019. [cited 2021 Nov 09]. Available From: http://www.euro.who.int/en/healthtopics/noncommunicablediseases/obesity/obesity .
» http://www.euro.who.int/en/healthtopics/noncommunicablediseases/obesity/obesity -
398Fastenau J, Kolotkin RL, Fujioka K, Alba M, Canovatchel W, Traina S. A Call to Action to Inform Patient-Centred Approaches to Obesity Management: Development of a Disease-Illness Model. Clin Obes. 2019;9(3):e12309. doi: 10.1111/cob.12309.
-
399Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, Lear SA, Ndumele CE, Neeland IJ, Sanders P, St-Onge MP; American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021;143(21):e984-e1010. doi: 10.1161/CIR.0000000000000973.
-
400Malta DC, Flor LS, Machado ÍE, Felisbino-Mendes MS, Brant LCC, Ribeiro ALP, Teixeira RA, Macário EM, Reitsma MB, Glenn S, Naghavi M, Gakidou E. Trends in Prevalence and Mortality Burden Attributable to Smoking, Brazil and Federated Units, 1990 and 2017. Popul Health Metr. 2020;18(Suppl 1):24. doi: 10.1186/s12963-020-00215-2.
-
401Benziger CP, Roth GA, Moran AE. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob Heart. 2016;11(4):393-7. doi: 10.1016/j.gheart.2016.10.024.
-
402Silva ALOD, Moreira JC. The Ban of Eletronic Cigarettes in Brazil: Success or Failure? Cien Saude Colet. 2019;24(8):3013-24. doi: 10.1590/1413-81232018248.24282017.
-
403GBD 2015 Mortality and Causes of Death Collaborators. Global, Regional, and National Life Expectancy, All-Cause Mortality, and Cause-Specific Mortality for 249 Causes of Death, 1980-2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459-44. doi: 10.1016/S0140-6736(16)31012-1.
» https://doi.org/10.1016/S0140-6736(16)31012-1 -
404Oberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide Burden of Disease From Exposure to Second-Hand Smoke: A Retrospective Analysis of Data From 192 Countries. Lancet. 2011;377(9760):139-46.
-
405Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2010.
-
406Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of heart failure: A systematic review and meta-analysis of prospective studies. Eur J Prev Cardiol. 2019;26(3):279-288. doi: 10.1177/2047487318806658.
-
407Watson M, Dardari Z, Kianoush S, Hall ME, DeFilippis AP, Keith RJ, Benjamin EJ, Rodriguez CJ, Bhatnagar A, Lima JA, Butler J, Blaha MJ, Rifai MA. Relation Between Cigarette Smoking and Heart Failure (From the Multiethnic Study of Atherosclerosis). Am J Cardiol. 2019;123(12):1972-7. doi: 10.1016/j.amjcard.2019.03.015.
-
408Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabé E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castañeda-Orjuela C, Catalá-López F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Søreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3(4):524-48. doi: 10.1001/jamaoncol.2016.5688.
-
409GBD 2015 Tobacco Collaborators. Smoking Prevalence and Attributable Disease Burden in 195 Countries and Territories, 1990-2015: A Systematic Analysis From the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885-906. doi: 10.1016/S0140-6736(17)30819-X.
» https://doi.org/10.1016/S0140-6736(17)30819-X -
410Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde do Escolar: 2015. Rio de Janeiro: IBGE; 2016.
-
411Brasil. Ministério da Saúde. Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília: Ministério da Saúde; 2018.
-
412Malta DC, Hallal ALC, Machado ÍE, Prado RRD, Oliveira PPV, Campos MO, Souza MFM. Factors Associated With the use of Waterpipe and other Tobacco Products Among Students, Brazil, 2015. Rev Bras Epidemiol. 2018;21(Suppl 1):e180006. doi: 10.1590/1980-549720180006.supl.1.
-
413Pichon-Riviere A, Alcaraz A, Palacios A, Rodríguez B, Reynales-Shigematsu LM, Pinto M, Castillo-Riquelme M, Peña Torres E, Osorio DI, Huayanay L, Loza Munarriz C, de Miera-Juárez BS, Gallegos-Rivero V, De La Puente C, Del Pilar Navia-Bueno M, Caporale J, Roberti J, Virgilio SA, Augustovski F, Bardach A. The Health and Economic Burden of Smoking in 12 Latin American Countries and the Potential Effect of Increasing Tobacco Taxes: An Economic Modelling Study. Lancet Glob Health. 2020;8(10):1282-94. doi: 10.1016/S2214-109X(20)30311-9.
-
414Pinto M, Bardach A, Palacios A, Biz A, Alcaraz A, Rodriguez B, Augustovski F, Pichon-Riviere A. Burden of Smoking in Brazil and Potential Benefit of Increasing Taxes on Cigarettes for the Economy and for Reducing Morbidity and Mortality. Cad Saude Publica. 2019;35(8):e00129118. doi: 10.1590/0102-311X00129118.
Publication Dates
-
Publication in this collection
21 Feb 2022 -
Date of issue
Jan 2022
History
-
Received
29 July 2021 -
Accepted
10 Nov 2021







































































































 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Brazilian Mortality Information System (SIM/DATASUS) with redistribution of ill-defined causes and correction for underreporting (according to GBD 2019 estimates) and IBGE population.
Source: Brazilian Mortality Information System (SIM/DATASUS) with redistribution of ill-defined causes and correction for underreporting (according to GBD 2019 estimates) and IBGE population.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Brazilian Mortality Information System – SIM/DATASUS.
Source: Brazilian Mortality Information System – SIM/DATASUS.  Source: Brazilian Mortality Information System – SIM/DATASUS.
Source: Brazilian Mortality Information System – SIM/DATASUS. 


 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington. 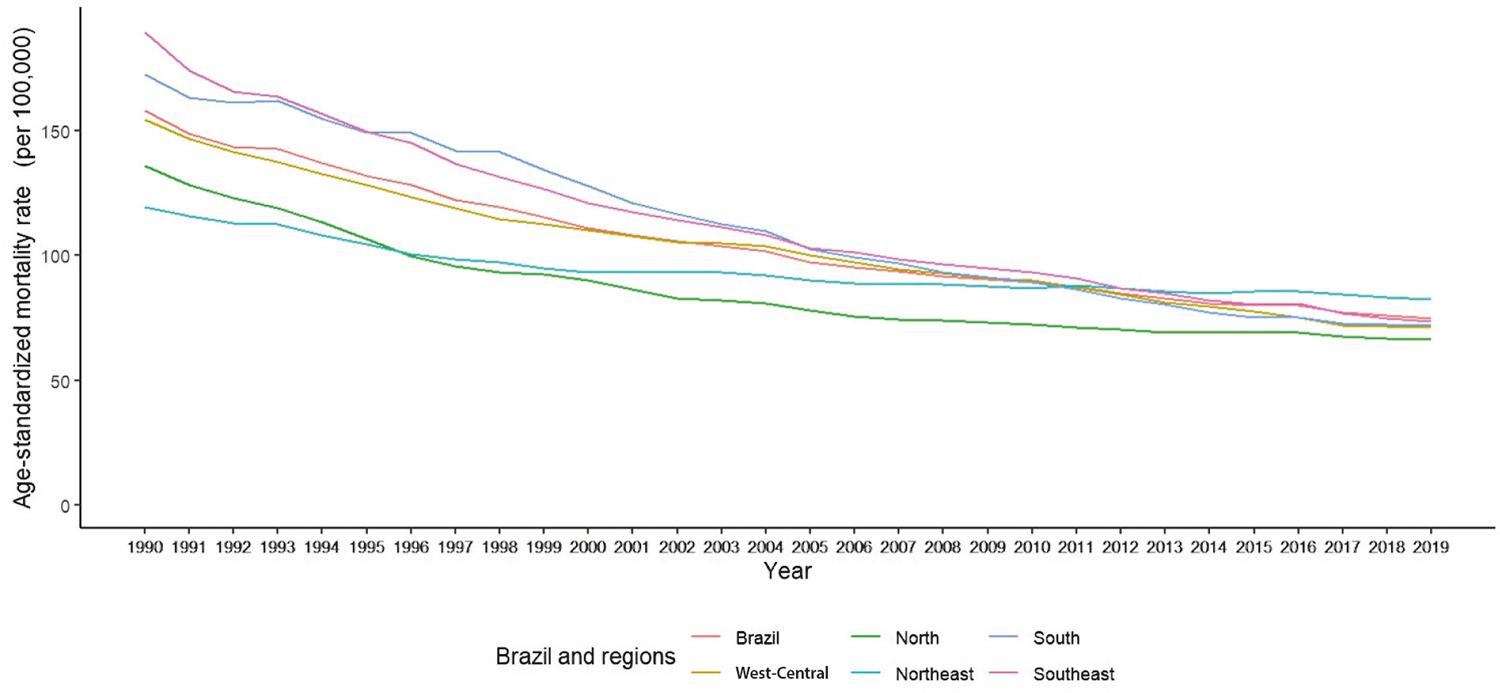 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Sources: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS)
Sources: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS)  Sources: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS)
Sources: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS)  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).
Source: Ministry of Health of Brazil – Hospital Information System of the Unified Health System (SIH/SUS).  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington. 
 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Martins-Melo et al.
Source: Martins-Melo et al.  Source: Nóbrega et al.
Source: Nóbrega et al.  Source: Nicolao et al.
Source: Nicolao et al. 
 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington. 

 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington. 
 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington. 









 Source: Malta DC et al.
Source: Malta DC et al.  Source: Vigitel – 2006 to 2019.
Source: Vigitel – 2006 to 2019.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington. 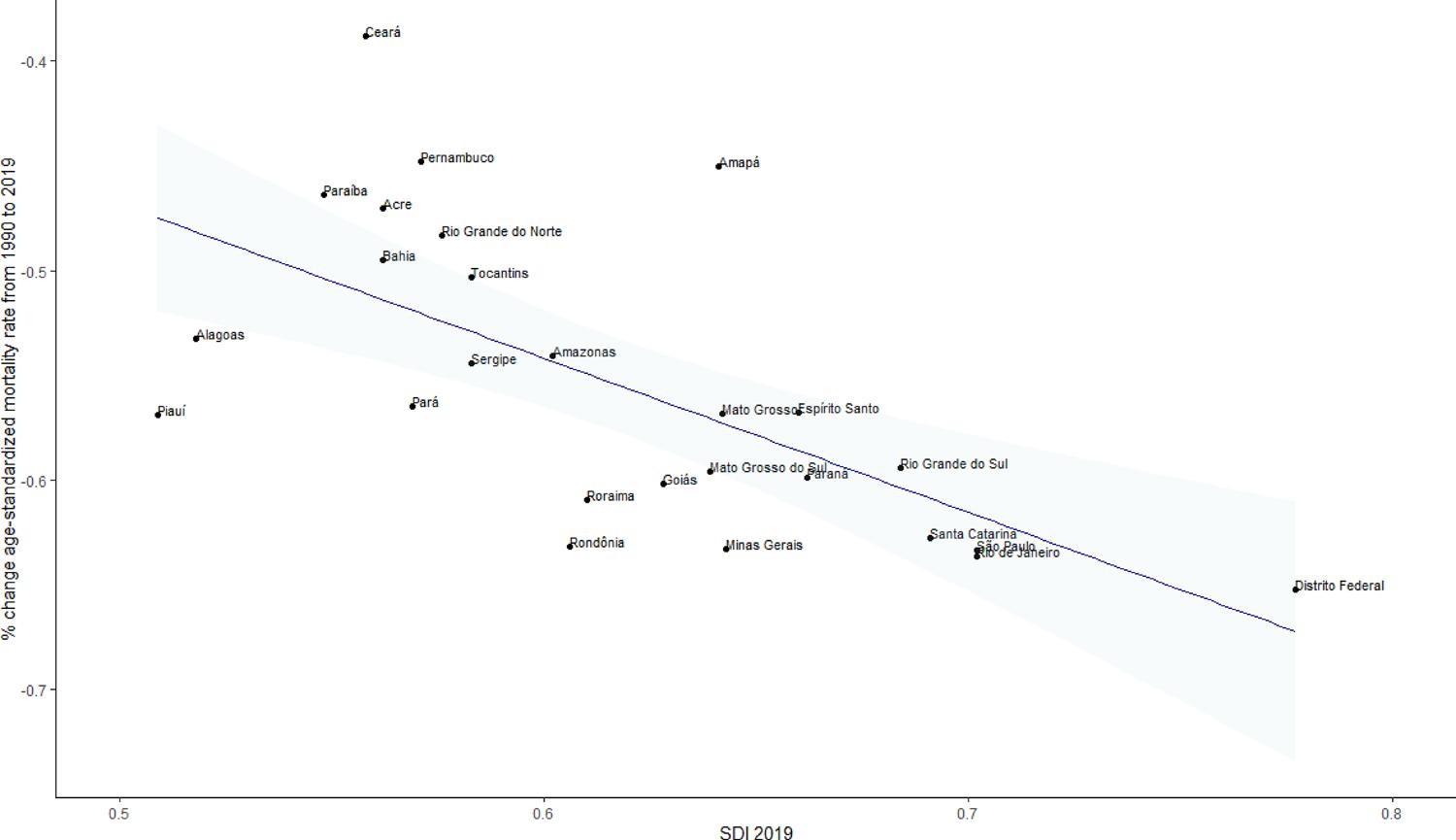 Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.  Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.
Source: Data derived from Global Burden of Disease Study 2019, Institute for Health Metrics and Evaluation, University of Washington.