ABSTRACT
Background:
The increased prevalence of obesity has led to a significant increase in the occurrence of metabolic syndrome, a recognized risk factor for increased morbidity and mortality from cardiovascular diseases. Hyperglycemia or type 2 diabetes mellitus, dyslipidemia and arterial hypertension are its main components. Since 2015, international guidelines have recognized the benefits of bariatric surgery in each isolated factor of this syndrome.
Aim:
To evaluate the impact of Roux-en-Y gastric bypass in this syndrome comparing pre- and postoperative periods with laboratory analysis and to compare waist/height ratio and BMI in relation to the determination of the cardiometabolic risk profile.
Methods:
A retrospective study was carried out, selecting 80 patients undergoing Roux-en-Y gastric bypass. Total cholesterol, HDL, LDL, triglycerides, fasting glucose, glycated hemoglobin, insulin, body mass index (BMI), vitamin D, vitamin B12, waist circumference and waist/height ratio in three periods were analyzed: the preoperative period from 1 to 6 months, postoperative from 1 to 6 months and postoperative from 1 to 2 years.
Results:
There was an improvement in all parameters of the clinical analyses. The preoperative BMI had a mean value of 39.8, in the preoperative period from 1 to 6 months, the values dropped to 33.2 and in the postoperative period of 1 year, the mean was 26. The perimeter mean values of 118.5 preoperatively, 105.2 postoperatively from 1 to 6 months and 90.3 postoperatively from 1 to 2 years. Waist/height ratio was 0.73, 0.65 and 0.56 in pre, post 1 to 6 months and 1 to 2 years respectively.
Conclusion:
Roux-en-Y gastric bypass improves metabolic syndrome and waist-to-height ratio is superior to BMI in the assessment of the cardiometabolic risk profile.
HEADINGS:
Obesity; Metabolic Syndrome; Diabetes Mellitus, type 2; Anastomosis, Roux-en-Y
RESUMO
Racional:
O aumento da prevalência da obesidade levou ao aumento significativo da ocorrência de síndrome metabólica, fator de risco reconhecido para aumento da morbimortalidade por doenças cardiovasculares. A hiperglicemia ou diabetes mellitus do tipo 2, dislipidemia e hipertensão arterial são seus principais componentes. Desde 2015, diretrizes internacionais reconheceram os benefícios da cirurgia bariátrica em cada fator isolado desta síndrome.
Objetivos:
Avaliar o impacto do bypass gástrico em Y-de-Roux nesta síndrome comparando períodos pré e pós-operatório com análise laboratorial, e comparar a razão cintura/estatura e o IMC em relação a determinação do perfil de risco cardiometabólico.
Métodos:
Realizou-se um estudo retrospectivo com base prospectiva selecionando 80 pacientes submetidos à bypass gástrico em Y-de-Roux. Foram analisados o colesterol total, HDL, LDL, triglicerídeos, glicemia de jejum, hemoglobina glicada, insulina, índice de massa corpórea (IMC), vitamina D, vitamina B12, perímetro abdominal e relação cintura/estatura em três períodos: o pré-operatório de 1 a 6 meses, pós-operatório de 1 a 6 meses e pós-operatório de 1 a 2 anos.
Resultados:
Houve melhora em todos os parâmetros das análises clínicas. O IMC, no pré-operatório, teve a média dos valores de 39,8, no pré-operatório de 1 a 6 meses, os valores caíram para 33,2 e no pós-operatório de 1 ano média foi de 26. O perímetro abdominal teve média dos valores de 118,5, no pré-operatório, 105,2 no pós-operatório de 1 a 6 meses e 90,3 no pós-operatório de 1 a 2 anos. A relação cintura/estatura teve 0,73, 0,65 e 0,56 no pré, pós 1 a 6 meses e 1 a 2 anos respectivamente.
Conclusão:
O bypass gástrico em Y-de-Roux melhora a síndrome metabólica e a relação cintura/estatura é superior ao IMC na avaliação do perfil do risco cardiometabólico.
DESCRITORES:
Obesidade; Síndrome Metabólica; Diabete Melito tipo 2; Anastomose em Y-de-Roux
INTRODUCTION
The increase in the obese population in the world is exponential, it is estimated that 30% of people are overweight or obese, significantly increasing morbidity and mortality from cardiovascular, oncological, endocrine and liver diseases, among others1111 De-Cleva R, et al. Lactate can be a marker of metabolic syndrome in severe obesity? Arq Bras Cir Dig. 2021 Jun 11;34(1):e1579. doi: 10.1590/0102-672020210001e1579. PMID: 34133526; PMCID: PMC8195466.
https://doi.org/10.1590/0102-67202021000...
,3838 Ruzzon A, Nassif PAN, Prigol L, Buzo L, Wendler G, Wendler E, Wendler IBT, Ruzzon I, Goveia CHM, Gonçalves LAP. Roux-in-Y gastrojejunal bypass: which anesthetic technique has best results? Arq Bras Cir Dig. 2021 May 14;34(1):e1530. doi: 10.1590/0102-672020200002e1530. PMID: 34008703; PMCID: PMC8121063.
https://doi.org/10.1590/0102-67202020000...
,4141 Schlottmann F, Galvarini MM, Dreifuss NH, Laxague F, Buxhoeveden R, Gorodner V. Metabolic Effects of Bariatric Surgery. J Laparoendosc Adv Surg Tech A. 2018 Aug;28(8):944-948. doi: 10.1089/lap.2018.0394. Epub 2018 Jul 13. PMID: 30004821.
https://doi.org/10.1089/lap.2018.0394...
.
Obesity, particularly abdominal obesity, is associated with resistance to the effects of insulin on the peripheral use of glucose and fatty acids, one of the components of the physiopathogenesis of type 2 diabetes mellitus, hyperinsulinemia and the increase in adipocyte cytokines. All these factors significantly increase cardiovascular risk, either alone or in combination. In addition to type 2 diabetes mellitus, other obesity-associated comorbidities, such as hypertension and dyslipidemia, are also direct risk factors for the development of cardiovascular disease. In this context, in 2014, Samson et al.4040 Samson SL, Garber AJ. Metabolic syndrome. Endocrinol Metab Clin North Am. 2014 Mar;43(1):1-23. doi: 10.1016/j.ecl.2013.09.009. PMID: 24582089.
https://doi.org/10.1016/j.ecl.2013.09.00...
called the concomitance of these comorbidities as syndrome X, currently known as metabolic syndrome (MS)99 Corcelles R, et al. Efectos del bypass gástrico sobre el riesgo cardiovascular estimado. Cirugia Espanola, [s. l.], 92(1)16-22, 2014. Disponível em: https://doi.org/10.1016/j.ciresp.2013.05.014,4040 Samson SL, Garber AJ. Metabolic syndrome. Endocrinol Metab Clin North Am. 2014 Mar;43(1):1-23. doi: 10.1016/j.ecl.2013.09.009. PMID: 24582089.
https://doi.org/10.1016/j.ecl.2013.09.00...
.
MS is characterized by abdominal perimeter greater than or equal to 102 cm in men and 88 cm in women; fasting glucose greater than 100 mg/dl; triglycerides above 150 mg/dl; HDL cholesterol less than 40 mg/dl in men and less than 50 mg/dl in women; and arterial hypertension (>130 mmHg, > 85mmHg). It is believed that obesity and insulin resistance are the main factors for the development of this syndrome1717 Guilbert L, Ortiz CJ, Espinosa O, Sepúlveda EM, Piña T, Joo P, Zerrweck C. Metabolic syndrome 2 years after laparoscopic gastric bypass. Int J Surg. 2018 Apr;52:264-268. doi: 10.1016/j.ijsu.2018.02.056. Epub 2018 Mar 1. PMID: 29501798.
https://doi.org/10.1016/j.ijsu.2018.02.0...
.
Due to the need for a more effective treatment, the term “metabolic surgery” emerged from the recognition of the metabolic effects of bariatric surgery, in addition to weight loss. Currently, the most performed procedures are Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy. Most patients with MS obtain significant improvements with bariatric surgery55 Bertsias G, Mammas I, Linardakis M, Kafatos A. Overweight and obesity in relation to cardiovascular disease risk factors among medical students in Crete, Greece. BMC Public Health. 2003 Jan 8;3:3. doi: 10.1186/1471-2458-3-3. Epub 2003 Jan 8. PMID: 12517305; PMCID: PMC140012.
https://doi.org/10.1186/1471-2458-3-3...
.
A recent review by Hwuang1717 Guilbert L, Ortiz CJ, Espinosa O, Sepúlveda EM, Piña T, Joo P, Zerrweck C. Metabolic syndrome 2 years after laparoscopic gastric bypass. Int J Surg. 2018 Apr;52:264-268. doi: 10.1016/j.ijsu.2018.02.056. Epub 2018 Mar 1. PMID: 29501798.
https://doi.org/10.1016/j.ijsu.2018.02.0...
exploring ideal waist-to-height ratios and subsequent comments66 Buchwald, H. The Evolution of Metabolic/Bariatric Surgery. OBES SURG 24, 1126-1135 (2014). https://doi.org/10.1007/s11695-014-1354-3
https://doi.org/10.1007/s11695-014-1354-...
,3232 Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, Shai I, Seidell J, Magni P, Santos RD, Arsenault B, Cuevas A, Hu FB, Griffin B, Zambon A, Barter P, Fruchart JC, Eckel RH; International Atherosclerosis Society; International Chair on Cardiometabolic Risk Working Group on Visceral Obesity. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019 Sep;7(9):715-725. doi: 10.1016/S2213-8587(19)30084-1. Epub 2019 Jul 10. PMID: 31301983.
https://doi.org/10.1016/S2213-8587(19)30...
concluded that height-adjusted waist circumference (known as waist circumference index) is superior to BMI in its association with body fat. This conclusion contrasts with the recent IAC and ICCR (International Atherosclerosis Society and International Chair On Cardiometabolic Risk) Consensus report on visceral obesity, which argued that waist circumference thresholds alone are adequate for the assessment of abdominal obesity in clinical practice33 Ashwell M, Gibson S. Comments on the article 'Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review': Consideration of relationship to cardiovascular risk factors and to the public health message. Obes Rev. 2020 Sep;21(9):e13074. doi: 10.1111/obr.13074. Epub 2020 Jun 23. PMID: 32578318.
https://doi.org/10.1111/obr.13074...
,3636 Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001 Aug;2(3):141-7. doi: 10.1046/j.1467-789x.2001.00031.x. PMID: 12120099.
https://doi.org/10.1046/j.1467-789x.2001...
.
There is an unmet need to promote consistent and universal public health message that visceral/central/abdominal obesity is associated with adverse health outcomes3232 Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, Shai I, Seidell J, Magni P, Santos RD, Arsenault B, Cuevas A, Hu FB, Griffin B, Zambon A, Barter P, Fruchart JC, Eckel RH; International Atherosclerosis Society; International Chair on Cardiometabolic Risk Working Group on Visceral Obesity. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019 Sep;7(9):715-725. doi: 10.1016/S2213-8587(19)30084-1. Epub 2019 Jul 10. PMID: 31301983.
https://doi.org/10.1016/S2213-8587(19)30...
. The authors of this research have used the waist-to-height ratio (WHtR) for almost 25 years as an adjunct indicator to BMI. It is a better predictor for central obesity, and superior for cardiovascular risk factors22 Ashwell M, Cole TJ, Dixon AK. Ratio of waist circumference to height is strong predictor of intra-abdominal fat. BMJ. 1996 Aug 31;313(7056):559-60. doi: 10.1136/bmj.313.7056.559d. PMID: 8790002; PMCID: PMC2351911.
https://doi.org/10.1136/bmj.313.7056.559...
. But the waist circumference index is superior to the WHtR in this respect.
The National Institute of Excellence in Health and Care - NICE - recognized the value of WHtR as an indicator of initial risk to health. We use recent data from the UK to explore whether the WHtR-based classification identifies more cardiometabolic risk than the ‘matrix’ based on BMI and waist circumference currently used for screening. Data from the Health Survey for England of 4112 obese people were used to identify cardiometabolic risk, as indicated by elevated glycated Hb, dyslipidemia, and hypertension. HbA1c, total/HDL cholesterol and systolic blood pressure were more strongly associated with WHtR than ‘matrix’. The WHtR 0.5 cut in the initial screening translates to a simple message: the waist should be less than half the height. This allows individuals to be aware of their health risks33 Ashwell M, Gibson S. Comments on the article 'Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review': Consideration of relationship to cardiovascular risk factors and to the public health message. Obes Rev. 2020 Sep;21(9):e13074. doi: 10.1111/obr.13074. Epub 2020 Jun 23. PMID: 32578318.
https://doi.org/10.1111/obr.13074...
.
WHtR is a simple anthropometric predictor for central body fat and is easy to use from a health education perspective. WHtR >0.5 was proposed as the first level of health risk. BMI is the most used to define weight status in relation to height, and its units are in kg/m2 3636 Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001 Aug;2(3):141-7. doi: 10.1046/j.1467-789x.2001.00031.x. PMID: 12120099.
https://doi.org/10.1046/j.1467-789x.2001...
. Despite the strong correlation between body fat and BMI, it cannot distinguish between lean mass and fat mass1515 Fox A, Slater C, Ahmed B, Ammori BJ, Senapati S, Akhtar K, Ellison J, Summers LKM, Robinson A, New JP, Soran H, Adam S, Syed AA. Vitamin D Status After Gastric Bypass or Sleeve Gastrectomy over 4 Years of Follow-up. Obes Surg. 2020 Apr;30(4):1473-1481. doi: 10.1007/s11695-019-04318-0. PMID: 31820405.
https://doi.org/10.1007/s11695-019-04318...
,3535 Pitanga FJG, Lessa I. Razão cintura-estatura como discriminador do risco coronariano de adultos, Rev. Assoc. Med. Bras, 52(3):157-61. 2006.. Thus, it is important to analyze each factor that makes up MS individually, in order to verify the real impact of bariatric surgery on each comorbidity.
Thus, this study aimed to evaluate the impact of Roux-en-Y gastric bypass comparing the pre- and postoperative period of 1 to 6 months, and the postoperative period of 1 to 2 years in MS and compare waist ratio/height and BMI in relation to the determination of the cardiometabolic risk profile.
METHOD
Data were collected from the prospective file of electronic medical records of Instituto Paulo Nassif, in Curitiba, PR, from January 2017 to December 2019. This work was approved by the Research Ethics Committee of Mackenzie Evangelical Faculty of Paraná, Curitiba, PR, Brazil, under number 4,324 .990.
Sample
Eighty patients who participated in a one-year multidisciplinary bariatric surgery preparation program were evaluated.
The inclusion criteria were: 1) patients who underwent bariatric surgery by RYGB and who had laboratory measurements from three different periods; 2) standard collection 1 to 6 months before the operation; 3) standard collection from 1 to 6 months postoperatively; 4) standard collection from 1 to 2 years postoperatively.
The only exclusion criterion was being under 18 years old and over 65 years old.
Variables analyzed
The following were researched: 1) clinical analyzes were on fasting glucose, serum insulin, glycated hemoglobin, total cholesterol, total triglycerides, HDL and LDL; 2) BMI of each patient before and after the operation in the same periods; 3) abdominal perimeter measured with an inextensible measuring tape in the smallest curvature located between the ribs and the iliac crest, at the normal expiratory moment; 4) waist/height ratio determined by dividing the smallest curvature located between the ribs and the iliac crest, at the normal expiratory moment, by height, measured in centimeters.
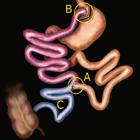
Operative technique
The RYGB consisted of building a small gastric reservoir (stomach with about 20 ml) performing two anastomoses, the gastrojejunal and the jejunojejunal (Figure 1). The rest of the stomach and the diverted intestine were not removed from the body, just excluded from the path taken by food and digestive enzymes. This deviated part anastomoses 120 cm from the duodenojejunal flexure with the jejunum, characterizing the biliopancreatic loop (Figure 1A). From the jejunojejunal anastomosis to the small gastric reservoir, also 120 cm long, characterizes the alimentary loop (Figure 1B). From the jejunojejunal anastomosis to the ileocecal valve, we have the common loop (Figure 1C).
RYGB demonstration: A) Jejunojejunal anastomosis 120 cm from the duodenal flexure (biliopancreatic loop - in brown); B) Gastrojejunal anastomosis 120 cm from the jejunojejunal anastomosis (food loop - in purple); C) Common handle (in blue).
Statistical analysis
Results of quantitative variables were described as mean, standard deviation, median, minimum and maximum. Categorical variables were described by frequency and percentage. To assess the correlation between two quantitative variables, Pearson’s linear correlation coefficients were estimated. To compare the evaluations before, after 1 to 6 months and after 1 to 2 years, in relation to quantitative variables, the analysis of variance model (ANOVA) with repeated measures and the Bonferroni test were used for comparisons of the two evaluations to two. Regarding categorical variables, comparisons were made using the binomial test. For the comparison of two groups, in relation to quantitative variables, the Student t test for independent samples was used. The condition of normality of continuous variables was assessed using the Kolmogorov-Smirnov test. Data from variables that did not meet this condition were submitted to a logarithmic transformation. Values of p<0.05 indicated statistical significance. For multiple comparisons using the binomial test, p values were corrected by Bonferroni. Data were analyzed using the computer program Stata/SE v.14.1. StataCorpLP, USA.
RESULTS
Descriptive statistics
The analysis presented below was performed based on data from 80 patients undergoing RYGB.
Evaluation of surgical results on clinical variables
Categorical variables
For each of them, the null hypothesis that there was no difference between the distributions in the pre-assessment and in the assessment of 1 to 6 months, vs. the alternative hypothesis that there was. This same comparative analysis was performed for the pre, 1 to 2 years, 1 to 6 months, and 1 to 2 years of evaluation moments. Table 2 presents descriptive statistics of the variables at each time of evaluation and p values of the statistical tests.
Quantitative variables
For each of these variables that met the condition of normality, the null hypothesis was tested that the means in the three assessments (pre, post 1-6 m and post 1-2 y) were equal, vs. the alternative hypothesis that the means were not. In the case of rejection of the null hypothesis, the evaluation moments were compared two by two.
For each of the quantitative variables that did not meet the normality condition, the null hypothesis that the results in the three evaluations (pre, post 1-6 m and post 1-2 y) were equal, vs. the alternative hypothesis that they weren’t. In the case of rejection of the null hypothesis, the evaluation moments were compared two by two.
Table 3 presents descriptive statistics of the variables at each evaluation moment and p values of the statistical tests.
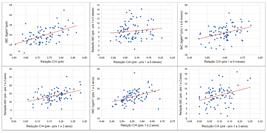
Assessment of the correlation between BMI and WHtR
For each of the evaluation moments (pre, post 1 to 6 m and after 1 to 2 y) and for the differences between the evaluations, the null hypothesis was tested that the correlation coefficient between BMI and WHtR was equal to zero (there was no correlation between the two variables) vs. the alternative hypothesis that the correlation coefficient was non-zero (there was correlation). Table 4 shows the values of Pearson’s linear correlation coefficients and the p values of the statistical tests.
Assessment of the association between BMI and cardiometabolic risk
For this analysis, two groups were defined according to cardiometabolic risk: group 1 - patients who had cardiometabolic risk in the pre and post 1 to 6 months assessments and stopped having it after 1 to 2 years (n=8); group 2 - patients who had cardiometabolic risk in all assessments (pre, post 1 to 6 m and post 1 to 2 y, n=72)
For each moment of BMI assessment and for the reductions between assessments, the null hypothesis that the BMI means were equal in both groups was tested, vs. the alternative hypothesis that the means were different.
Table 5 and Figure 2 show descriptive statistics of the evolutionary graphic BMI according to groups 1 and 2, and the p values of the statistical tests. For reductions, positive values indicate a reduction in BMI and negative values indicate an increase.
DISCUSSION
The increased prevalence of MS due to the obesity pandemic, secondary to the current sedentary lifestyle associated with poor diet, has been correlated with higher morbidity and mortality from cardiovascular diseases. MS, in addition to harming the quality of life and health of its individual patients, has become a public health problem. This is due to the costly costs applied to the treatment of chronic diseases involved in MS on an individual basis, in addition to the complications brought about by the syndrome1212 Engin, A. The definition and prevalence of obesity and metabolic syndrome. In: ADVANCES IN EXPERIMENTAL MEDICINE AND BIOLOGY. [S. l.]: Springer New York LLC, 2017. v. 960, p. 1-17. Disponível em: https://doi.org/10.1007/978-3-319-48382-5_1
https://doi.org/10.1007/978-3-319-48382-...
,1313 Fernandes G, Santo MA, Crespo AFCB, Biancardi GB, Mota FC, Antonangelo L, de Cleva R. Early glycemic control and incretin improvement after gastric bypass: the role of oral and gastrostomy route. Surg Obes Relat Dis. 2019 Apr;15(4):595-601. doi: 10.1016/j.soard.2019.01.013. Epub 2019 Jan 31. PMID: 30803884.
https://doi.org/10.1016/j.soard.2019.01....
,1414 Fleischmann R, Kremer J, Cush J, Schulze-Koops H, Connell CA, Bradley JD, Gruben D, Wallenstein GV, Zwillich SH, Kanik KS; ORAL Solo Investigators. Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med. 2012 Aug 9;367(6):495-507. doi: 10.1056/NEJMoa1109071. PMID: 22873530.
https://doi.org/10.1056/NEJMoa1109071...
.
In this context, metabolic surgery has been shown to significantly improve some of the MS components, the main ones being DM2, dyslipidemia and abdominal perimeter. According to the literature, there is a consensus that there is improvement in the laboratory parameters of patients who undergo metabolic surgery, with RYGB being the most performed procedure currently1818 Hayoz C, Hermann T, Raptis DA, Brönnimann A, Peterli R, Zuber M. Comparison of metabolic outcomes in patients undergoing laparoscopic roux-en-Y gastric bypass versus sleeve gastrectomy - a systematic review and meta-analysis of randomised controlled trials. Swiss Med Wkly. 2018 Jul 5;148:w14633. doi: 10.4414/smw.2018.14633. PMID: 30035801.
https://doi.org/10.4414/smw.2018.14633...
,3434 Oliveira SC, Neves JS, Souteiro P, Pedro J, Magalhães D, Guerreiro V, Bettencourt-Silva R, Costa MM, Varela A, Barroso I, Freitas P; AMTCO Group, Carvalho D. Impact of Bariatric Surgery on Long-term Cardiovascular Risk: Comparative Effectiveness of Different Surgical Procedures. Obes Surg. 2020 Feb;30(2):673-680. doi: 10.1007/s11695-019-04237-0. PMID: 31749108.
https://doi.org/10.1007/s11695-019-04237...
.
In addition to clinical and laboratory parameters, a remarkable factor is that the improvement in MS decreases cardiovascular risk. Corroborating other studies11 Aekplakorn W, Pakpeankitwatana V, Lee CM, Woodward M, Barzi F, Yamwong S, Unkurapinun N, Sritara P. Abdominal obesity and coronary heart disease in Thai men. Obesity (Silver Spring). 2007 Apr;15(4):1036-42. doi: 10.1038/oby.2007.604. PMID: 17426340.
https://doi.org/10.1038/oby.2007.604...
,66 Buchwald, H. The Evolution of Metabolic/Bariatric Surgery. OBES SURG 24, 1126-1135 (2014). https://doi.org/10.1007/s11695-014-1354-3
https://doi.org/10.1007/s11695-014-1354-...
,99 Corcelles R, et al. Efectos del bypass gástrico sobre el riesgo cardiovascular estimado. Cirugia Espanola, [s. l.], 92(1)16-22, 2014. Disponível em: https://doi.org/10.1016/j.ciresp.2013.05.014,1717 Guilbert L, Ortiz CJ, Espinosa O, Sepúlveda EM, Piña T, Joo P, Zerrweck C. Metabolic syndrome 2 years after laparoscopic gastric bypass. Int J Surg. 2018 Apr;52:264-268. doi: 10.1016/j.ijsu.2018.02.056. Epub 2018 Mar 1. PMID: 29501798.
https://doi.org/10.1016/j.ijsu.2018.02.0...
,3131 Nassif PAN, et al. Alterações nos parâmetros pré e pós-operatórios de pacientes com síndrome metabólica, submetidos a Bypass gastrointestinal em Y de Roux. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo), [s. l.], v. 22, n. 3, p. 165-170, 2009. Disponível em: https://doi.org/10.1590/s0102-67202009000300006
https://doi.org/10.1590/s0102-6720200900...
, this research showed improvement in the variables that contribute to the development of cardiovascular diseases.
Metabolic surgery has been shown to have a great anti-diabetogenic effect, which leads to early resolution of the disease picture, even before major weight loss. As proposed by Varaschim et al. (2012)4343 Varaschim M, Nassif PA, Moreira LB, do Nascimento MM, Vieira GM, Garcia RF, Sue KM, Cruz MA. Changes in clinical and laboratory parameters in obese patients with type 2 diabetes mellitus submitted to Roux-en-y gastrojejunal bypass without ring. Rev Col Bras Cir. 2012 May-Jun;39(3):178-82. English, Portuguese. PMID: 22836564., this fact can be explained by the endocrine effect produced by this procedure. The comparison between the pre- and postoperative periods was significant, while the comparison between the two postoperative periods was not. Similar results were obtained for glycated hemoglobin values, which also decreased when compared pre- and postoperatively.
One of the main factors that contribute to the development of DM2 is insulin resistance, which causes an increase in serum insulin concentration. In this context, metabolic surgery proves to be efficient in decreasing insulin resistance, as the values drop considerably after the procedure. The present study obtained preoperative insulin values averaging 22.2 μIU/ml, in the first postoperative period it was 8.1 μIU/ml and 6.1 μIU/ml in the second - all with significance (p<0.001).
The main risk factor for coronary disease, among the components of MS, is dyslipidemia. It is known that metabolic surgery has a positive influence on improving the lipid profile. As described by Guilbert et al. (2018)1717 Guilbert L, Ortiz CJ, Espinosa O, Sepúlveda EM, Piña T, Joo P, Zerrweck C. Metabolic syndrome 2 years after laparoscopic gastric bypass. Int J Surg. 2018 Apr;52:264-268. doi: 10.1016/j.ijsu.2018.02.056. Epub 2018 Mar 1. PMID: 29501798.
https://doi.org/10.1016/j.ijsu.2018.02.0...
the reduction in triglyceride levels is mainly associated with weight loss, that is, it presents a gradual reduction, a fact that was confirmed by the results of the present study, in which the initial mean was 152.5 mg/dl, the 96 mg/dl in the first postoperative period and 82.1 mg/dl in the second (p<0.001). In the analysis of HDL, the results showed an average of 49.6 mg/dl in the pre, 45.6 mg/dl in the post 1 to 6 months and in the 1 to 2 years period with an average of 57.5 mg/dl - all with significance (p<0.001). Guilbert et al. (2018)1717 Guilbert L, Ortiz CJ, Espinosa O, Sepúlveda EM, Piña T, Joo P, Zerrweck C. Metabolic syndrome 2 years after laparoscopic gastric bypass. Int J Surg. 2018 Apr;52:264-268. doi: 10.1016/j.ijsu.2018.02.056. Epub 2018 Mar 1. PMID: 29501798.
https://doi.org/10.1016/j.ijsu.2018.02.0...
also discuss HDL and explain that, unlike triglycerides, HDL goes through two phases, a decline immediately after the operation and then an increase in the first six months, reflecting the gradual qualitative change, with maturation of the particles, accompanied by an increase in its antioxidant potential, favoring its cardiovascular protection properties. For both components, changes in lifestyle after the operation (increased physical activity and type of diet) have a direct impact 2222 Jensen MD, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014 Jun 24;129(25 Suppl 2):S102-38. doi: 10.1161/01.cir.0000437739.71477.ee. Epub 2013 Nov 12. Erratum in: Circulation. 2014 Jun 24;129(25 Suppl 2):S139-40. PMID: 24222017; PMCID: PMC5819889.
https://doi.org/10.1161/01.cir.000043773...
,3333 Nevill AM, Duncan MJ, Lahart IM, Sandercock GR. Scaling waist girth for differences in body size reveals a new improved index associated with cardiometabolic risk. Scand J Med Sci Sports. 2017 Nov;27(11):1470-1476. doi: 10.1111/sms.12780. Epub 2016 Oct 10. PMID: 27726187.
https://doi.org/10.1111/sms.12780...
.
Elevated LDL levels are an important component in the pathophysiology of atherosclerosis; thus, metabolic surgery to improve LDL levels contributes to lower cardiovascular risk. In this work, LDL values were found with a mean of 96.6 mg/dl before the operation, after which the mean dropped to 85.4 mg/dl at first and then to 76.2 mg/dl (p<0.001 in all analyses). The values found corroborate Nassif et al. (2009)3131 Nassif PAN, et al. Alterações nos parâmetros pré e pós-operatórios de pacientes com síndrome metabólica, submetidos a Bypass gastrointestinal em Y de Roux. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo), [s. l.], v. 22, n. 3, p. 165-170, 2009. Disponível em: https://doi.org/10.1590/s0102-67202009000300006
https://doi.org/10.1590/s0102-6720200900...
, who also showed a progressive drop in LDL. In the analysis of total cholesterol, the results showed a mean of 174.6 mg/dl preoperatively, 149.5 mg/dl and 150.2 mg/dl, respectively, in the first and second postoperative periods. There was significance only in the comparison between pre and postoperative periods (p<0.001).
BMI is the parameter used to indicate the surgical treatment of obesity, in addition to evaluating the efficiency of its short- and long-term results. The variables found were a mean BMI of 39.8 kg/m2 preoperatively, which decreased to 33.2 kg/m2 in 1 to 6 months after the procedure and to 26 kg/m2 in 1 to 2 years - there was significance at all values (p<0.001). Nassif et al. (2009)3131 Nassif PAN, et al. Alterações nos parâmetros pré e pós-operatórios de pacientes com síndrome metabólica, submetidos a Bypass gastrointestinal em Y de Roux. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo), [s. l.], v. 22, n. 3, p. 165-170, 2009. Disponível em: https://doi.org/10.1590/s0102-67202009000300006
https://doi.org/10.1590/s0102-6720200900...
showed similar results with a progressive drop in BMI values, which is expected according to the literature. Also, regarding weight loss, Iannelli et al. (2011)2020 Iannelli A, Anty R, Schneck AS, Tran A, Gugenheim J. Inflammation, insulin resistance, lipid disturbances, anthropometrics, and metabolic syndrome in morbidly obese patients: a case control study comparing laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Surgery. 2011 Mar;149(3):364-70. doi: 10.1016/j.surg.2010.08.013. Epub 2010 Oct 8. PMID: 20932542.
https://doi.org/10.1016/j.surg.2010.08.0...
stated that RYGB proved to be significantly efficient.
However, there are several limitations of BMI, which include: non-differentiation of lean and fat mass, making it difficult to assess muscular patients; do not differentiate visceral fat from subcutaneous fat; it has special tables for children and seniors1010 Courcoulas AP, Goodpaster BH, Eagleton JK, Belle SH, Kalarchian MA, Lang W, Toledo FG, Jakicic JM. Surgical vs medical treatments for type 2 diabetes mellitus: a randomized clinical trial. JAMA Surg. 2014 Jul;149(7):707-15. doi: 10.1001/jamasurg.2014.467. PMID: 24899268; PMCID: PMC4106661.
https://doi.org/10.1001/jamasurg.2014.46...
,2626 Lima WC, et al. Análise da relação entre a estatura e o perímetro abdominal em indivíduos portadores de percentuais normais de gordura. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo) [online]. 2010, v. 23, n. 1 [Acessado 25 Outubro 2021] , pp. 24-28. Disponível em: <https://doi.org/10.1590/S0102-67202010000100007>. Epub 22 Jun 2010. ISSN 2317-6326. https://doi.org/10.1590/S0102-67202010000100007.
https://doi.org/10.1590/S0102-6720201000...
,3030 Nassif PA, Malafaia O, Ribas-Filho JM, Czeczko NG, Garcia RF, Ariede BL. Vertical gastrectomy and gastric bypass in Roux-en-Y induce postoperative gastroesophageal reflux disease? Arq Bras Cir Dig. 2014;27 Suppl 1(Suppl 1):63-8. doi: 10.1590/s0102-6720201400s100016. PMID: 25409970; PMCID: PMC4743523.
https://doi.org/10.1590/s0102-6720201400...
.
Kornerup, et al. (2019)2424 Kornerup LS, Hvas CL, Abild CB, Richelsen B, Nexo E. Early changes in vitamin B12 uptake and biomarker status following Roux-en-Y gastric bypass and sleeve gastrectomy. Clin Nutr. 2019 Apr;38(2):906-911. doi: 10.1016/j.clnu.2018.02.007. Epub 2018 Feb 15. PMID: 29506877.
https://doi.org/10.1016/j.clnu.2018.02.0...
reported a high risk of developing micronutrient deficiencies due to extensive changes in the anatomy and physiology of the gastrointestinal tract in RYGB. In 2016, the American Society of Bariatric and Metabolic Surgery updated its nutritional guidelines aimed at bariatric patients, which described great variability in vitamin deficiencies, both pre and postoperatively. The prevalence of preoperative vitamin deficiencies of 30% for vitamin B12 and 90% for vitamin D was then identified. In the present study, the mean of vitamin B12 in the analyzed periods was within the normal range, ranging from 509.8 to 639.6. These 80 patients studied were rigorously followed up and supplemented both pre- and post-operatively. Johnson et al., (2019)2323 Johnson LM, Ikramuddin S, Leslie DB, Slusarek B, Killeen AA. Analysis of vitamin levels and deficiencies in bariatric surgery patients: a single-institutional analysis. Surg Obes Relat Dis. 2019 Jul;15(7):1146-1152. doi: 10.1016/j.soard.2019.04.028. Epub 2019 May 2. PMID: 31202681.
https://doi.org/10.1016/j.soard.2019.04....
demonstrated that postoperative deficiencies had a prevalence of up to 20% for vitamin B12 and 100% for vitamin D. Our results showed preoperative vitamin D deficiency with a mean of 26.8.
RYGB compromises vitamin B12 absorption because almost no gastric acid remains in the gastric pouch, and as a result, food-bound release of B12 is substantially decreased. In addition, the production of intrinsic factor - a protein derived from the parietal cell necessary for the intestinal absorption of B12 - is reduced or absent in the bypassed stomach. Furthermore, B12 malabsorption is enhanced by the late introduction of pancreatic enzymes in the distal jejunum2424 Kornerup LS, Hvas CL, Abild CB, Richelsen B, Nexo E. Early changes in vitamin B12 uptake and biomarker status following Roux-en-Y gastric bypass and sleeve gastrectomy. Clin Nutr. 2019 Apr;38(2):906-911. doi: 10.1016/j.clnu.2018.02.007. Epub 2018 Feb 15. PMID: 29506877.
https://doi.org/10.1016/j.clnu.2018.02.0...
,4242 Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, Ahlin S, Anveden Å, Bengtsson C, Bergmark G, Bouchard C, Carlsson B, Dahlgren S, Karlsson J, Lindroos AK, Lönroth H, Narbro K, Näslund I, Olbers T, Svensson PA, Carlsson LM. Bariatric surgery and long-term cardiovascular events. JAMA. 2012 Jan 4;307(1):56-65. doi: 10.1001/jama.2011.1914. PMID: 22215166.
https://doi.org/10.1001/jama.2011.1914...
,4545 Wendler E, et al. Abreviar jejum pré-operatório e introduzir alimentação precoce auxiliam na recuperação após bypass gastrojejunal? ABCD 2021; 34(2):e1606.
As described, vitamin D deficiency is the most common preoperative deficiency, and is related to insufficient sun exposure and reduced hepatic hydroxylation77 Burton RF. Comments on the article "Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review": Relationships to previous studies. Obes Rev. 2020 Mar;21(3):e12982. doi: 10.1111/obr.12982. Epub 2019 Nov 29. PMID: 31782872.
https://doi.org/10.1111/obr.12982...
,1515 Fox A, Slater C, Ahmed B, Ammori BJ, Senapati S, Akhtar K, Ellison J, Summers LKM, Robinson A, New JP, Soran H, Adam S, Syed AA. Vitamin D Status After Gastric Bypass or Sleeve Gastrectomy over 4 Years of Follow-up. Obes Surg. 2020 Apr;30(4):1473-1481. doi: 10.1007/s11695-019-04318-0. PMID: 31820405.
https://doi.org/10.1007/s11695-019-04318...
,1616 Frayon S, Cavaloc Y, Wattelez G, Cherrier S, Lerrant Y, Ashwell M, Galy O. Potential for waist-to-height ratio to detect overfat adolescents from a Pacific Island, even those within the normal BMI range. Obes Res Clin Pract. 2018 Jul-Aug;12(4):351-357. doi: 10.1016/j.orcp.2017.12.001. Epub 2017 Dec 15. PMID: 29254830.
https://doi.org/10.1016/j.orcp.2017.12.0...
. To prevent postsurgical vitamin D deficiency, oral vitamin D supplementation of 800 IU daily is generally recommended by the American Association of Clinical Endocrinologists and The Obesity Society2525 Li Z, Zhou X, Fu W. Vitamin D supplementation for the prevention of vitamin D deficiency after bariatric surgery: a systematic review and meta-analysis. Eur J Clin Nutr. 2018 Aug;72(8):1061-1070. doi: 10.1038/s41430-017-0059-9. Epub 2017 Dec 29. PMID: 29288249.
https://doi.org/10.1038/s41430-017-0059-...
.
Recent researches with the aim of determining limit values for WHtR in different populations indicated that a cutoff point of 0.5 is the most indicated value for both genders, all ages and different populations55 Bertsias G, Mammas I, Linardakis M, Kafatos A. Overweight and obesity in relation to cardiovascular disease risk factors among medical students in Crete, Greece. BMC Public Health. 2003 Jan 8;3:3. doi: 10.1186/1471-2458-3-3. Epub 2003 Jan 8. PMID: 12517305; PMCID: PMC140012.
https://doi.org/10.1186/1471-2458-3-3...
,2727 Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, Lin RS, Shau WY, Huang KC. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord. 2002 Sep;26(9):1232-8. doi: 10.1038/sj.ijo.0802040. PMID: 12187401.
https://doi.org/10.1038/sj.ijo.0802040...
,3535 Pitanga FJG, Lessa I. Razão cintura-estatura como discriminador do risco coronariano de adultos, Rev. Assoc. Med. Bras, 52(3):157-61. 2006.. Several studies have shown that WHtR is also a better indicator for the health of children and adolescents than other anthropometric indicators. And the cutoff point of 0.5, which has been proposed, is close to those recommended for adults2121 Ikramuddin S, Korner J, Lee WJ, Connett JE, Inabnet WB, Billington CJ, Thomas AJ, Leslie DB, Chong K, Jeffery RW, Ahmed L, Vella A, Chuang LM, Bessler M, Sarr MG, Swain JM, Laqua P, Jensen MD, Bantle JP. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013 Jun 5;309(21):2240-9. doi: 10.1001/jama.2013.5835. PMID: 23736733; PMCID: PMC3954742.
https://doi.org/10.1001/jama.2013.5835...
,2929 McCarthy HD, Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message--'keep your waist circumference to less than half your height'. Int J Obes (Lond). 2006 Jun;30(6):988-92. doi: 10.1038/sj.ijo.0803226. PMID: 16432546.
https://doi.org/10.1038/sj.ijo.0803226...
,4444 Weili Y, He B, Yao H, Dai J, Cui J, Ge D, Zheng Y, Li L, Guo Y, Xiao K, Fu X, Ma D. Waist-to-height ratio is an accurate and easier index for evaluating obesity in children and adolescents. Obesity (Silver Spring). 2007 Mar;15(3):748-52. doi: 10.1038/oby.2007.601. PMID: 17372326.
https://doi.org/10.1038/oby.2007.601...
.
Lima et al. (2010)2626 Lima WC, et al. Análise da relação entre a estatura e o perímetro abdominal em indivíduos portadores de percentuais normais de gordura. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo) [online]. 2010, v. 23, n. 1 [Acessado 25 Outubro 2021] , pp. 24-28. Disponível em: <https://doi.org/10.1590/S0102-67202010000100007>. Epub 22 Jun 2010. ISSN 2317-6326. https://doi.org/10.1590/S0102-67202010000100007.
https://doi.org/10.1590/S0102-6720201000...
verified the existence of a common waist-to-height ratio in male individuals, aged between 18 and 25 years, with normal fat percentages, to provide a personalized and non-generalized method of measuring waist circumference. The analysis of the sample of 174 individuals resulted to be in the age group of 21.2±2.1 years, with height of 174.3±6.2 cm, with a percentage of fat of 10.8%, with measurement of the abdominal circumference of 75.5±5.7 cm, and with the waist/height ratio presenting the value of 0.43±0.033. They concluded that there is a common relationship between the waist-to-height ratio among men aged between 18 and 25 years with a normal fat percentage of 43% of their height.
Study by Lucas et al. (2020)2828 Lucas RWDC, Nassif PAN, Tabushi FI, Nassif DSB, Ariede BL, Brites-Neto J, Malafaia O. Can stature, abdominal perimeter and bmi index predict possible cardiometabolic risks in future obesity? Arq Bras Cir Dig. 2020 Nov 20;33(2):e1529. doi: 10.1590/0102-672020200002e1529. PMID: 33237167; PMCID: PMC7682149.
https://doi.org/10.1590/0102-67202020000...
, using the cutoff point of 0.5 in WHtR as a reference, evaluated the development of an equation that could determine the appropriate waist measurement of the smallest abdominal perimeter, also having as premise the WHtR, but in a sample 454 individuals, 249 males and 205 females, between 18 and 65 years old, without the state of obesity. Regarding the percentage of height as a measure of the smallest waist circumference, the total female sample had an average of 44.2±1.1% and the male 45.3%±1.5. For women this percentage determined the equation of the waist-to-height ratio represented by X=(age+217)/5.875, and for men X= (age+190.89) /5.2222. The “X” in the equations represents the percentage of height measurement so that the individual fits into the category of adequate in relation to percentages of fat and BMI.
Our study found that the WHtR values after two years of postoperative RYGB were equivalent to 0.56, with a reduction equivalent to 60.7% if the objective was to reach 0.45 in the study by Lucas et al. (2020)2727 Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, Lin RS, Shau WY, Huang KC. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord. 2002 Sep;26(9):1232-8. doi: 10.1038/sj.ijo.0802040. PMID: 12187401.
https://doi.org/10.1038/sj.ijo.0802040...
.
The method of analysis of the waist/height ratio (WHtR) takes into account a perimetric measure that presents a predictive profile of the quantitative situation involving visceral fat. Therefore, the characteristics of the local subcutaneous adipose tissue may make a difference in this interpretation.
We justify the score above 0.5 due to the anatomophysiological condition common to individuals in this obesity scenario, as in addition to hypertrophy, subcutaneous adipocyte hyperplasia is present, and ends up determining a functional residue, linked to intense weight loss. These residues are called “functional and aesthetic bodily sequelae”, as mentioned by Cintra Junior et al.88 Cintra Junior W, Modolin MLA, Colferai DR, Rocha RI, Gemperli R. Post-bariatric body contouring surgery: analysis of complications in 180 consecutive patients. Rev Col Bras Cir. 2021 Jul 19;48:e20202638. English, Portuguese. doi: 10.1590/0100-6991e-20202638. PMID: 34287547.
https://doi.org/10.1590/0100-6991e-20202...
Such changes correspond to what is conventionally called dysmorphia, characterized by dermofat accumulations predominantly in the arms, breasts, abdomen and thigh, which is corroborated by the large number of patients in the RYGB postoperative period requiring submission to cosmetic surgeries, notably abdominoplasty ( dermolipectomy), as mentioned by Baroudi and Moraes44 Baroudi R, Moraes M. Philosophy, technical principles, selection, and indication in body contouring surgery. Aesthetic Plast Surg. 1991 Winter;15(1):1-18. doi: 10.1007/BF02273829. PMID: 1994645.
https://doi.org/10.1007/BF02273829...
.
The sum of the metabolic results presented indicates that this score is compatible with a low amount of body fat after 02 years of postoperative BYGR. Therefore, for this select group of patients, we believe that this anatomical and functional aspect should be taken into account, as a future criterion for reinterpreting the cutoff point, and promoting comparison with the post-surgical esthetic state. In this sense, we can infer that there was a greater reduction in the parameters of the waist/height ratio than the BMI in this period.
Although both did not manage to reach the level of normality according to their scales, when the WHtR was correlated with the BMI and the other MS markers, the superiority of the former for the identification of the cardiometabolic risk profile was evident.
CONCLUSION
The RYGB improves the metabolic syndrome and the waist/height ratio (WHtR) is superior to the BMI in the assessment of the cardiometabolic risk profile.
REFERENCES
-
1Aekplakorn W, Pakpeankitwatana V, Lee CM, Woodward M, Barzi F, Yamwong S, Unkurapinun N, Sritara P. Abdominal obesity and coronary heart disease in Thai men. Obesity (Silver Spring). 2007 Apr;15(4):1036-42. doi: 10.1038/oby.2007.604. PMID: 17426340.
» https://doi.org/10.1038/oby.2007.604 -
2Ashwell M, Cole TJ, Dixon AK. Ratio of waist circumference to height is strong predictor of intra-abdominal fat. BMJ. 1996 Aug 31;313(7056):559-60. doi: 10.1136/bmj.313.7056.559d. PMID: 8790002; PMCID: PMC2351911.
» https://doi.org/10.1136/bmj.313.7056.559d -
3Ashwell M, Gibson S. Comments on the article 'Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review': Consideration of relationship to cardiovascular risk factors and to the public health message. Obes Rev. 2020 Sep;21(9):e13074. doi: 10.1111/obr.13074. Epub 2020 Jun 23. PMID: 32578318.
» https://doi.org/10.1111/obr.13074 -
4Baroudi R, Moraes M. Philosophy, technical principles, selection, and indication in body contouring surgery. Aesthetic Plast Surg. 1991 Winter;15(1):1-18. doi: 10.1007/BF02273829. PMID: 1994645.
» https://doi.org/10.1007/BF02273829 -
5Bertsias G, Mammas I, Linardakis M, Kafatos A. Overweight and obesity in relation to cardiovascular disease risk factors among medical students in Crete, Greece. BMC Public Health. 2003 Jan 8;3:3. doi: 10.1186/1471-2458-3-3. Epub 2003 Jan 8. PMID: 12517305; PMCID: PMC140012.
» https://doi.org/10.1186/1471-2458-3-3 -
6Buchwald, H. The Evolution of Metabolic/Bariatric Surgery. OBES SURG 24, 1126-1135 (2014). https://doi.org/10.1007/s11695-014-1354-3
» https://doi.org/10.1007/s11695-014-1354-3 -
7Burton RF. Comments on the article "Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review": Relationships to previous studies. Obes Rev. 2020 Mar;21(3):e12982. doi: 10.1111/obr.12982. Epub 2019 Nov 29. PMID: 31782872.
» https://doi.org/10.1111/obr.12982 -
8Cintra Junior W, Modolin MLA, Colferai DR, Rocha RI, Gemperli R. Post-bariatric body contouring surgery: analysis of complications in 180 consecutive patients. Rev Col Bras Cir. 2021 Jul 19;48:e20202638. English, Portuguese. doi: 10.1590/0100-6991e-20202638. PMID: 34287547.
» https://doi.org/10.1590/0100-6991e-20202638 -
9Corcelles R, et al. Efectos del bypass gástrico sobre el riesgo cardiovascular estimado. Cirugia Espanola, [s. l.], 92(1)16-22, 2014. Disponível em: https://doi.org/10.1016/j.ciresp.2013.05.014
-
10Courcoulas AP, Goodpaster BH, Eagleton JK, Belle SH, Kalarchian MA, Lang W, Toledo FG, Jakicic JM. Surgical vs medical treatments for type 2 diabetes mellitus: a randomized clinical trial. JAMA Surg. 2014 Jul;149(7):707-15. doi: 10.1001/jamasurg.2014.467. PMID: 24899268; PMCID: PMC4106661.
» https://doi.org/10.1001/jamasurg.2014.467 -
11De-Cleva R, et al. Lactate can be a marker of metabolic syndrome in severe obesity? Arq Bras Cir Dig. 2021 Jun 11;34(1):e1579. doi: 10.1590/0102-672020210001e1579. PMID: 34133526; PMCID: PMC8195466.
» https://doi.org/10.1590/0102-672020210001e1579 -
12Engin, A. The definition and prevalence of obesity and metabolic syndrome. In: ADVANCES IN EXPERIMENTAL MEDICINE AND BIOLOGY. [S. l.]: Springer New York LLC, 2017. v. 960, p. 1-17. Disponível em: https://doi.org/10.1007/978-3-319-48382-5_1
» https://doi.org/10.1007/978-3-319-48382-5_1 -
13Fernandes G, Santo MA, Crespo AFCB, Biancardi GB, Mota FC, Antonangelo L, de Cleva R. Early glycemic control and incretin improvement after gastric bypass: the role of oral and gastrostomy route. Surg Obes Relat Dis. 2019 Apr;15(4):595-601. doi: 10.1016/j.soard.2019.01.013. Epub 2019 Jan 31. PMID: 30803884.
» https://doi.org/10.1016/j.soard.2019.01.013 -
14Fleischmann R, Kremer J, Cush J, Schulze-Koops H, Connell CA, Bradley JD, Gruben D, Wallenstein GV, Zwillich SH, Kanik KS; ORAL Solo Investigators. Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med. 2012 Aug 9;367(6):495-507. doi: 10.1056/NEJMoa1109071. PMID: 22873530.
» https://doi.org/10.1056/NEJMoa1109071 -
15Fox A, Slater C, Ahmed B, Ammori BJ, Senapati S, Akhtar K, Ellison J, Summers LKM, Robinson A, New JP, Soran H, Adam S, Syed AA. Vitamin D Status After Gastric Bypass or Sleeve Gastrectomy over 4 Years of Follow-up. Obes Surg. 2020 Apr;30(4):1473-1481. doi: 10.1007/s11695-019-04318-0. PMID: 31820405.
» https://doi.org/10.1007/s11695-019-04318-0 -
16Frayon S, Cavaloc Y, Wattelez G, Cherrier S, Lerrant Y, Ashwell M, Galy O. Potential for waist-to-height ratio to detect overfat adolescents from a Pacific Island, even those within the normal BMI range. Obes Res Clin Pract. 2018 Jul-Aug;12(4):351-357. doi: 10.1016/j.orcp.2017.12.001. Epub 2017 Dec 15. PMID: 29254830.
» https://doi.org/10.1016/j.orcp.2017.12.001 -
17Guilbert L, Ortiz CJ, Espinosa O, Sepúlveda EM, Piña T, Joo P, Zerrweck C. Metabolic syndrome 2 years after laparoscopic gastric bypass. Int J Surg. 2018 Apr;52:264-268. doi: 10.1016/j.ijsu.2018.02.056. Epub 2018 Mar 1. PMID: 29501798.
» https://doi.org/10.1016/j.ijsu.2018.02.056 -
18Hayoz C, Hermann T, Raptis DA, Brönnimann A, Peterli R, Zuber M. Comparison of metabolic outcomes in patients undergoing laparoscopic roux-en-Y gastric bypass versus sleeve gastrectomy - a systematic review and meta-analysis of randomised controlled trials. Swiss Med Wkly. 2018 Jul 5;148:w14633. doi: 10.4414/smw.2018.14633. PMID: 30035801.
» https://doi.org/10.4414/smw.2018.14633 -
19Hwaung P, Heo M, Kennedy S, Hong S, Thomas DM, Shepherd J, Heymsfield SB. Optimum waist circumference-height indices for evaluating adult adiposity: An analytic review. Obes Rev. 2020 Jan;21(1):e12947. doi: 10.1111/obr.12947. Epub 2019 Sep 10. PMID: 31507076.
» https://doi.org/10.1111/obr.12947 -
20Iannelli A, Anty R, Schneck AS, Tran A, Gugenheim J. Inflammation, insulin resistance, lipid disturbances, anthropometrics, and metabolic syndrome in morbidly obese patients: a case control study comparing laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Surgery. 2011 Mar;149(3):364-70. doi: 10.1016/j.surg.2010.08.013. Epub 2010 Oct 8. PMID: 20932542.
» https://doi.org/10.1016/j.surg.2010.08.013 -
21Ikramuddin S, Korner J, Lee WJ, Connett JE, Inabnet WB, Billington CJ, Thomas AJ, Leslie DB, Chong K, Jeffery RW, Ahmed L, Vella A, Chuang LM, Bessler M, Sarr MG, Swain JM, Laqua P, Jensen MD, Bantle JP. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013 Jun 5;309(21):2240-9. doi: 10.1001/jama.2013.5835. PMID: 23736733; PMCID: PMC3954742.
» https://doi.org/10.1001/jama.2013.5835 -
22Jensen MD, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014 Jun 24;129(25 Suppl 2):S102-38. doi: 10.1161/01.cir.0000437739.71477.ee. Epub 2013 Nov 12. Erratum in: Circulation. 2014 Jun 24;129(25 Suppl 2):S139-40. PMID: 24222017; PMCID: PMC5819889.
» https://doi.org/10.1161/01.cir.0000437739.71477.ee -
23Johnson LM, Ikramuddin S, Leslie DB, Slusarek B, Killeen AA. Analysis of vitamin levels and deficiencies in bariatric surgery patients: a single-institutional analysis. Surg Obes Relat Dis. 2019 Jul;15(7):1146-1152. doi: 10.1016/j.soard.2019.04.028. Epub 2019 May 2. PMID: 31202681.
» https://doi.org/10.1016/j.soard.2019.04.028 -
24Kornerup LS, Hvas CL, Abild CB, Richelsen B, Nexo E. Early changes in vitamin B12 uptake and biomarker status following Roux-en-Y gastric bypass and sleeve gastrectomy. Clin Nutr. 2019 Apr;38(2):906-911. doi: 10.1016/j.clnu.2018.02.007. Epub 2018 Feb 15. PMID: 29506877.
» https://doi.org/10.1016/j.clnu.2018.02.007 -
25Li Z, Zhou X, Fu W. Vitamin D supplementation for the prevention of vitamin D deficiency after bariatric surgery: a systematic review and meta-analysis. Eur J Clin Nutr. 2018 Aug;72(8):1061-1070. doi: 10.1038/s41430-017-0059-9. Epub 2017 Dec 29. PMID: 29288249.
» https://doi.org/10.1038/s41430-017-0059-9 -
26Lima WC, et al. Análise da relação entre a estatura e o perímetro abdominal em indivíduos portadores de percentuais normais de gordura. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo) [online]. 2010, v. 23, n. 1 [Acessado 25 Outubro 2021] , pp. 24-28. Disponível em: <https://doi.org/10.1590/S0102-67202010000100007>. Epub 22 Jun 2010. ISSN 2317-6326. https://doi.org/10.1590/S0102-67202010000100007.
» https://doi.org/10.1590/S0102-67202010000100007 -
27Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, Lin RS, Shau WY, Huang KC. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord. 2002 Sep;26(9):1232-8. doi: 10.1038/sj.ijo.0802040. PMID: 12187401.
» https://doi.org/10.1038/sj.ijo.0802040 -
28Lucas RWDC, Nassif PAN, Tabushi FI, Nassif DSB, Ariede BL, Brites-Neto J, Malafaia O. Can stature, abdominal perimeter and bmi index predict possible cardiometabolic risks in future obesity? Arq Bras Cir Dig. 2020 Nov 20;33(2):e1529. doi: 10.1590/0102-672020200002e1529. PMID: 33237167; PMCID: PMC7682149.
» https://doi.org/10.1590/0102-672020200002e1529 -
29McCarthy HD, Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message--'keep your waist circumference to less than half your height'. Int J Obes (Lond). 2006 Jun;30(6):988-92. doi: 10.1038/sj.ijo.0803226. PMID: 16432546.
» https://doi.org/10.1038/sj.ijo.0803226 -
30Nassif PA, Malafaia O, Ribas-Filho JM, Czeczko NG, Garcia RF, Ariede BL. Vertical gastrectomy and gastric bypass in Roux-en-Y induce postoperative gastroesophageal reflux disease? Arq Bras Cir Dig. 2014;27 Suppl 1(Suppl 1):63-8. doi: 10.1590/s0102-6720201400s100016. PMID: 25409970; PMCID: PMC4743523.
» https://doi.org/10.1590/s0102-6720201400s100016 -
31Nassif PAN, et al. Alterações nos parâmetros pré e pós-operatórios de pacientes com síndrome metabólica, submetidos a Bypass gastrointestinal em Y de Roux. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo), [s. l.], v. 22, n. 3, p. 165-170, 2009. Disponível em: https://doi.org/10.1590/s0102-67202009000300006
» https://doi.org/10.1590/s0102-67202009000300006 -
32Neeland IJ, Ross R, Després JP, Matsuzawa Y, Yamashita S, Shai I, Seidell J, Magni P, Santos RD, Arsenault B, Cuevas A, Hu FB, Griffin B, Zambon A, Barter P, Fruchart JC, Eckel RH; International Atherosclerosis Society; International Chair on Cardiometabolic Risk Working Group on Visceral Obesity. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019 Sep;7(9):715-725. doi: 10.1016/S2213-8587(19)30084-1. Epub 2019 Jul 10. PMID: 31301983.
» https://doi.org/10.1016/S2213-8587(19)30084-1 -
33Nevill AM, Duncan MJ, Lahart IM, Sandercock GR. Scaling waist girth for differences in body size reveals a new improved index associated with cardiometabolic risk. Scand J Med Sci Sports. 2017 Nov;27(11):1470-1476. doi: 10.1111/sms.12780. Epub 2016 Oct 10. PMID: 27726187.
» https://doi.org/10.1111/sms.12780 -
34Oliveira SC, Neves JS, Souteiro P, Pedro J, Magalhães D, Guerreiro V, Bettencourt-Silva R, Costa MM, Varela A, Barroso I, Freitas P; AMTCO Group, Carvalho D. Impact of Bariatric Surgery on Long-term Cardiovascular Risk: Comparative Effectiveness of Different Surgical Procedures. Obes Surg. 2020 Feb;30(2):673-680. doi: 10.1007/s11695-019-04237-0. PMID: 31749108.
» https://doi.org/10.1007/s11695-019-04237-0 -
35Pitanga FJG, Lessa I. Razão cintura-estatura como discriminador do risco coronariano de adultos, Rev. Assoc. Med. Bras, 52(3):157-61. 2006.
-
36Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001 Aug;2(3):141-7. doi: 10.1046/j.1467-789x.2001.00031.x. PMID: 12120099.
» https://doi.org/10.1046/j.1467-789x.2001.00031.x -
37Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, Santos RD, Arsenault B, Cuevas A, Hu FB, Griffin BA, Zambon A, Barter P, Fruchart JC, Eckel RH, Matsuzawa Y, Després JP. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020 Mar;16(3):177-189. doi: 10.1038/s41574-019-0310-7. Epub 2020 Feb 4. PMID: 32020062; PMCID: PMC7027970.
» https://doi.org/10.1038/s41574-019-0310-7 -
38Ruzzon A, Nassif PAN, Prigol L, Buzo L, Wendler G, Wendler E, Wendler IBT, Ruzzon I, Goveia CHM, Gonçalves LAP. Roux-in-Y gastrojejunal bypass: which anesthetic technique has best results? Arq Bras Cir Dig. 2021 May 14;34(1):e1530. doi: 10.1590/0102-672020200002e1530. PMID: 34008703; PMCID: PMC8121063.
» https://doi.org/10.1590/0102-672020200002e1530 -
39Said S, Mukherjee D, Whayne TF. Interrelationships with Metabolic Syndrome, Obesity and Cardiovascular Risk. Curr Vasc Pharmacol. 2016;14(5):415-425. doi: 10.2174/1570161114666160722121615. PMID: 27456105.
» https://doi.org/10.2174/1570161114666160722121615 -
40Samson SL, Garber AJ. Metabolic syndrome. Endocrinol Metab Clin North Am. 2014 Mar;43(1):1-23. doi: 10.1016/j.ecl.2013.09.009. PMID: 24582089.
» https://doi.org/10.1016/j.ecl.2013.09.009 -
41Schlottmann F, Galvarini MM, Dreifuss NH, Laxague F, Buxhoeveden R, Gorodner V. Metabolic Effects of Bariatric Surgery. J Laparoendosc Adv Surg Tech A. 2018 Aug;28(8):944-948. doi: 10.1089/lap.2018.0394. Epub 2018 Jul 13. PMID: 30004821.
» https://doi.org/10.1089/lap.2018.0394 -
42Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, Ahlin S, Anveden Å, Bengtsson C, Bergmark G, Bouchard C, Carlsson B, Dahlgren S, Karlsson J, Lindroos AK, Lönroth H, Narbro K, Näslund I, Olbers T, Svensson PA, Carlsson LM. Bariatric surgery and long-term cardiovascular events. JAMA. 2012 Jan 4;307(1):56-65. doi: 10.1001/jama.2011.1914. PMID: 22215166.
» https://doi.org/10.1001/jama.2011.1914 -
43Varaschim M, Nassif PA, Moreira LB, do Nascimento MM, Vieira GM, Garcia RF, Sue KM, Cruz MA. Changes in clinical and laboratory parameters in obese patients with type 2 diabetes mellitus submitted to Roux-en-y gastrojejunal bypass without ring. Rev Col Bras Cir. 2012 May-Jun;39(3):178-82. English, Portuguese. PMID: 22836564.
-
44Weili Y, He B, Yao H, Dai J, Cui J, Ge D, Zheng Y, Li L, Guo Y, Xiao K, Fu X, Ma D. Waist-to-height ratio is an accurate and easier index for evaluating obesity in children and adolescents. Obesity (Silver Spring). 2007 Mar;15(3):748-52. doi: 10.1038/oby.2007.601. PMID: 17372326.
» https://doi.org/10.1038/oby.2007.601 -
45Wendler E, et al. Abreviar jejum pré-operatório e introduzir alimentação precoce auxiliam na recuperação após bypass gastrojejunal? ABCD 2021; 34(2):e1606
-
Financial source:
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001 - 3
-
Central message
The increase in the global prevalence of metabolic diseases is inexplicable when considering only environmental or genetic factors. There is a need to explore the possible roles of epigenetic factors. Despite gaps in our knowledge, evidence suggests that measuring waist circumference improves patient management and should be an integral part of a preoperative protocol to improve patient care and health. -
Perspective
Much progress has been made in this interdisciplinary field in recent years, with many studies investigating various aspects of the metabolic syndrome and its associated epigenetic changes. Metabolically healthy obesity is not a stable or reliable indicator of future risk for cardiovascular disease. The waist circumference threshold for a given BMI category at different ages, by gender and by ethnicity will require further investigation. Evidence suggests that measuring waist circumference improves patient management and should be an integral part of a pre- and postoperative protocol.
Publication Dates
-
Publication in this collection
05 Jan 2022 -
Date of issue
2021
History
-
Received
09 Dec 2020 -
Accepted
23 Mar 2021