Abstracts
BACKGROUND: Acute kidney injury is one of the most common complications of orthotopic liver transplantation. The absence of universal criteria for definition of these conditions make comparisons difficult between studies. The conventional technique for transplantation is the total excision of the inferior vena cava during liver retro-native hepatectomy. Controversies about the effect of the conventional technique without venovenous bypass on renal function remain. AIM: To estimate the incidence and risk of acute kidney injury factors among recipients of orthotopic liver transplantation without conventional venovenous bypass. METHODS: Was studied 375 patients undergoing orthotopic liver transplantation. Variables were analyzed in preoperative, intraoperative and postoperative complications in 153 patients undergoing orthotopic liver transplantation without conventional venovenous bypass. The criterion for acute kidney injury was serum creatinine > 1.5 mg/dl or urinary debit <500 ml/24h within the first three days post-transplant. Univariate analysis and multivariate logistic regression were done. RESULTS: All transplants were performed with grafts from deceased donors. Sixty patients (39.2%) had acute kidney injury. Age, body mass index, Child-Turcotte-Pugh, urea, hypertension, and preoperative serum creatinine were higher in the acute kidney injury group. During the intraoperative period, the group acute kidney injury had more reperfusion syndrome, transfusion of red blood cells, fresh frozen plasma and platelets. Postoperatively, the duration of mechanical ventilation and postoperative creatinine levels were also variable, with significant differences for the group of acute kidney injury. After logistic regression, the reperfusion syndrome, the class C of the Child-Turcotte-Pugh and postoperative serum creatinine showed differences. CONCLUSION: Acute kidney injury after orthotopic liver transplantation without conventional venovenous bypass is a common disorder, but with good prognosis. Reperfusion syndrome, serum creatinine postoperatively and Child C are factors associated with acute kidney injury after orthotopic liver transplantation without conventional venovenous bypass.
Kidney failure; Acute renal; Failure, liver transplantation; Venovenous deviation
RADICAL: Injúria renal aguda é uma das complicações mais comuns do transplante ortotópico de fígado. A ausência de critério universal para sua definição nestas condições dificulta as comparações entre os estudos. A técnica convencional para o transplante consiste na excisão total da veia cava inferior retro-hepática durante a hepatectomia nativa. Controvérsias sobre o efeito da técnica convencional sem desvio venovenoso na função renal continuam. OBJETIVO: Estimar a incidência e os fatores de risco de injúria renal aguda entre os receptores de transplante ortotópico de fígado convencional sem desvio venovenoso. MÉTODOS: Foram avaliados 375 pacientes submetidos a transplante ortotópico de fígado. Foram analisadas as variáveis pré, intra e pós-operatórias em 153 pacientes submetidos a transplante ortotópico de fígado convencional sem desvio venovenoso. O critério para a injúria renal aguda foi valor da creatinina sérica > 1,5 mg/dl ou débito urinário < 500 ml/24h dentro dos primeiros três dias pós-transplante. Foi realizada análise univariada e multivariada por regressão logística. RESULTADOS: Todos os transplantes foram realizados com enxerto de doador falecido. Sessenta pacientes (39,2%) apresentaram injúria renal aguda. Idade, índice de massa corpórea, escore de Child-Turcotte-Pugh, ureia, hipertensão arterial sistêmica e creatinina sérica pré-operatória apresentaram maiores valores no grupo injúria renal aguda. Durante o período intraoperatório, o grupo injúria renal aguda apresentou mais síndrome de reperfusão, transfusão de concentrado de hemácias, plasma fresco e plaquetas. No pós-operatório, o tempo de permanência em ventilação mecânica e creatinina pós-operatória também foram variáveis, com diferenças significativas para o grupo injúria renal aguda. Após regressão logística, a síndrome de reperfusão, a classe C do Child-Turcotte-Pugh e a creatinina sérica pós-operatória apresentaram diferenças. CONCLUSÃO: Injúria renal aguda após transplante ortotópico de fígado convencional sem desvio venovenoso é uma desordem comum, mas apresenta bom prognóstico. Síndrome de reperfusão, creatinina sérica no pós-operatório e Child C são fatores associados a injúria renal aguda pós-transplante ortotópico de fígado convencional sem desvio venovenoso.
Falência renal; Insuficiência renal aguda; Transplante de fígado; Desvio venovenoso
ORIGINAL ARTICLE
Correspondence
ABSTRACT
BACKGROUND: Acute kidney injury is one of the most common complications of orthotopic liver transplantation. The absence of universal criteria for definition of these conditions make comparisons difficult between studies. The conventional technique for transplantation is the total excision of the inferior vena cava during liver retro-native hepatectomy. Controversies about the effect of the conventional technique without venovenous bypass on renal function remain.
AIM: To estimate the incidence and risk of acute kidney injury factors among recipients of orthotopic liver transplantation without conventional venovenous bypass.
METHODS: Was studied 375 patients undergoing orthotopic liver transplantation. Variables were analyzed in preoperative, intraoperative and postoperative complications in 153 patients undergoing orthotopic liver transplantation without conventional venovenous bypass. The criterion for acute kidney injury was serum creatinine > 1.5 mg/dl or urinary debit <500 ml/24h within the first three days post-transplant. Univariate analysis and multivariate logistic regression were done.
RESULTS: All transplants were performed with grafts from deceased donors. Sixty patients (39.2%) had acute kidney injury. Age, body mass index, Child-Turcotte-Pugh, urea, hypertension, and preoperative serum creatinine were higher in the acute kidney injury group. During the intraoperative period, the group acute kidney injury had more reperfusion syndrome, transfusion of red blood cells, fresh frozen plasma and platelets. Postoperatively, the duration of mechanical ventilation and postoperative creatinine levels were also variable, with significant differences for the group of acute kidney injury. After logistic regression, the reperfusion syndrome, the class C of the Child-Turcotte-Pugh and postoperative serum creatinine showed differences.
CONCLUSION: Acute kidney injury after orthotopic liver transplantation without conventional venovenous bypass is a common disorder, but with good prognosis. Reperfusion syndrome, serum creatinine postoperatively and Child C are factors associated with acute kidney injury after orthotopic liver transplantation without conventional venovenous bypass.
Headings: Kidney failure. Acute renal. Failure, liver transplantation. Venovenous deviation.
INTRODUCTION
The venovenous bypass (DVV) was introduced as the standard technique of liver transplantation in the mid-1980s as a solution to the venous system and inferior vena cava stasis caused by the door clamping during the anhepatic phase of the operation28. The surgeons believed that relief of stasis in porta and cava will improve intraoperative hemodynamic stability by reducing the impact on venous return to right atrium during the clamping of these veins. In addition, the DVV bring other benefits such as protection of renal function and decrease intraoperative bleeding. This technical solution was quickly accepted among surgeons and it was done compulsorily until the description of liver transplantation technique piggyback let this procedure be performed with preservation of retro-hepatic cava vein and, therefore, no need of DVV, since the clamping of the inferior cava is only partial18,32.
Lately, its benefits have been questioned by several authors15,27. First, the placement of the DVV is capable of life-threatening complications, such as air embolism or venous thrombi and hypothermia8. Moreover, thanks to effective compensatory mechanisms, the benefits to reduced cardiac output do not appear to be as advantageous, given to the fact that this reduction, when it is not used, is not associated with increased morbidity and postoperative mortality5.
Specifically, with respect to the development of acute kidney injury (AKI) after surgery, the data are still conflicting. As use of the DVV is defended by reducing the harmful effects of clamping the vena cava on the renal perfusion pressure, some authors have shown that there is a higher incidence of acute renal failure (ARF) when the DVV ceases to be used in cases operated by standard technique4. The results of these observations are fragile, firstly because the number of patients operated in this way is relatively small when considering the results published by major liver transplant centers. Secondly, the research methodology was different in the published work.
Since 2000, there is a Liver Transplantation Program in the state of Pernambuco, northeastern Brazil. This program, which was the first in this vast region of the country, is today one of the most productive in Brazil, with an average of 80 transplants per year since 2006. During this period, both for technical reasons as to believe that liver transplantation could be achieved by the conventional technique without DVV, was accumulated experience with this way of performing the transplant, both in adults and children.
This paper presents the results using the conventional technique without DVV for liver transplantation in adults and the risk factors associated with development of postoperative ARF in these patients.
METHODS
Patients
Was reviewed medical records of 375 patients undergoing orthotopic liver transplantation (TOC), conducted by the Liver Transplant Program HUOC-UPE, from August 1999 to December 2009. Patients were allocated to the surgical technique based on decision of the surgical team at the time of operation. In general, patients from the severe group were operated by conventional technique, because surgeons felt more comfortable to operate them with this technique.
They adopted the following exclusion criteria: liver transplantation piggyback technique, the age of 16 years, acute liver failure, death during surgery, transplants between live persons, transplant with hemitransposicion with cavo-portal transplantation; "split liver"; domino transplant; double transplant liver/kidney; retransplantation; incomplete data.
Technical procedures
Patients were separated into two groups according to the onset of ARF in the postoperative period and the presence of serum creatinine ≥ 1.5 mg/dl or urine output <500 ml/24hs in the first three postoperative days. Hourly diuresis was measured during this period and laboratory tests repeated at least every 12 hours.
Were analyzed the following variables: 1) identification - hospital records, age, gender, weight, height, blood type, body mass index (BMI); 2) preoperative - Model for end-stage liver disease (MELD), class functional Child-Turcotte-Pugh score, presence of previous operation and the following laboratory tests: BUN, creatinine, glucose, sodium, potassium, albumin, platelet count, international normalized ratio (INR) and creatinine clearance; 3) operative - operative time, warm ischemia, cold and total intraoperative urine output (ml/kg/hour), presence of reperfusion syndrome; 4) postoperative - INR, platelets, urea, creatinine, sodium and potassium (on intensive care unit - ICU admission, 1st to 3rd day after surgery), albumin, glucose, transaminases (at baseline); diuresis the first 24 hours, duration of stay in ICU, hospital renal replacement therapy (dialysis), duration of mechanical ventilation (extubated in room in less than 6 h postoperatively between 6 h and 12 h, between 12 h and 24 h postoperatively and after 24 h); 5) evolution - the presence of reoperation, graft function (dysfunction or primary non-functioning), use of antibiotics, sepsis, biliary and vascular complications, retransplantation (during the first 30 days); 6) donor - the cause of death, age, ICU stay, length of intubation, presence of heart failure, inotropic support, macrosteatosis, transaminases, bilirubin, sodium, graft weight, graft extended criterion.
Morbidity was assessed by analysis of the incidence of biliary complications, vascular and septic, within the first six months after orthotopic liver transplantation without conventional venovenous bypass (TOF-C). Biliary complications were defined as stenosis (narrowing of the bile duct confirmed by cholangiography, cholangioresonance or cholestasis in the presence of clinical or laboratory data) or fistula, content-free bile in the peritoneum diagnosed by reoperation, ultrasound or computed tomography. Thrombosis of the hepatic artery and portal vein was diagnosed by using abdominal ultrasound or angiography, respectively, during a routine or under suspicion.
All recipients of TOF-C underwent the same immunosuppression regimen: tacrolimus, mycophenolate mofetil and corticosteroids. The management followed the clinical course on postoperative period.
Surgical technique
Procedure in the donor
The stages of operation were: incision, exploration and inspection, mobilization of the organ, in situ perfusion, removal of the graft liver perfusion ex situ, closure of the incision. Packaging and transportation to the receiving center were the final steps.
Organ perfusion was performed with some preservation solution (the solution of the University of Wisconsin - UW was first used in liver transplantation program at HUOC-UPE, but today is used Celsior solution®).
Procedure at the recipient
After anesthetic preparation, the patient's chest and abdomen were prepared with a povidone-iodine and covered with surgical drapes. The most commonly used incision was bilateral subcostal extension with or without median superior access to the xiphoid process.
After inspection of the liver abnormalities searching unexpected situations (non suspected hepatoma or vascular anomalies) falciform, triangular and coronary ligaments were cut. Next, attention was given to the portal triad. Its dissection was performed and the elements (bile duct, hepatic artery and portal vein) were ligated according to the need to accelerate or not the operative time.
As the technique of liver transplantation was the conventional one, the vena cava was mobilized in the retroperitoneum to be included in the receiver diseased liver resection. The receiver hepatectomy was completed sectioning the inferior vena cava above and below-hepatic (between vascular clamps). The liver graft was packed into the abdominal cavity of the receptor and vascular repair occurred in the following sequence: inferior vena cava to the hepatic veins, vena cava inferior infra-hepatic, and portal vein anastomosis following coronary artery bypass, hepatic artery anastomosis; anastomosis of the biliary tract.
The abdominal closure was performed after careful observation of hemostasis and, possibly, drain placement.
Concepts
ARF was considered with the presence of serum creatinine ≥ 1.5 mg/dL or diuresis <500 ml/24 h (within the first three days after surgery)31.
MELD - Model for end-stage liver disease - prognostic model to evaluate the survival of patients with terminal liver disease 11 was calculated as follows:
Ischemia time cold, was the period between the start of perfusion of the organ, still in the deceased donor with a preservation solution and placing the graft on the recipient's body; hot, was the period between the onset of vascular reconstruction to restore the flow blood for the "new" organ; total, the sum of two times of ischemia. The measurement were performed in minutes.
Reperfusion syndrome were cardiovascular changes after revascularization of the body characterized by over 30% decrease in mean arterial pressure compared to baseline that lasted over a minute and occurred within the first five minutes after reperfusion. The presence of arrhythmia, bradycardia and hypovolemia could also be associated with the syndrome.
Sepsis - systemic inflammatory response to infection (SIRS) - was characterized by the presence of at least two of the following parameters: hypothermia (body temperature <36°C) or fever (> 38°C), tachycardia (heart rate> 90 bpm ), tachypnea (respiratory rate> 20 bpm or pCO 2 <32 mmHg), leukocytosis (>12 x 109 cells/L), leukopenia (<4 x 109 cells/l) or more than 10% of immature cells.
Antibiotic therapy was used with antibiotics for more than five days postoperatively.
Graft extended criterion was seen as bodies that did not have all the necessary qualities to be called ideal or Brisceño score of ≥ 33.
BMI - body mass index - were calculated by the formula: BMI = weight (kg)/height (m)2.
RESULTS
One hundred and fifty-three patients among 375 who underwent orthotopic liver transplantation during the period August 1999 to December 2009 were eligible for this study. The causes of exclusion were a piggyback transplant (n = 89), recipients under 16 years (n = 75), acute liver failure (n = 10), intraoperative death (n = 5), with a live donor transplant (n = 2), split liver (n = 2), domino transplants (n = 5), double transplant (liver-kidney) (n = 1), hemitransposition cavoportal (n = 2), retransplantation (n = 10) and incomplete data (n = 21). The demographic characteristics of patients are presented in Table 1.
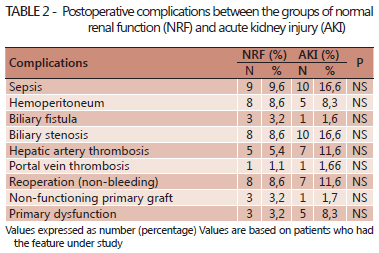
There were no differences in postoperative complications between the groups (Table 2).
Among the 153 patients, 60 (39.2%) developed ARF during the first three days after TOF-C. Hemodialysis was performed in 13 patients in the ARF group, which represents 8.5% of surgical patients and 21.6% of patients who had ARF. There were two deaths among dialysis patients by the seventh day after surgery and two in the same period among patients from group normal renal function (NRF). The indications for renal replacement therapy, hemodialysis were hypervolemic (five patients), uremia (five patients), and both in three patients.
Risk factors for preoperative
Traumatic brain injury and stroke were the most common causes of brain death in ARF groups (84.5%) vs NRF (85.4%), respectively. No significant difference in the use of liver grafts with extended criteria among the groups (ARF = 45.0% and NRF = 32.3%, P = 0.1555).
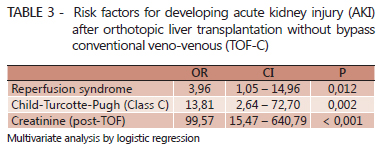
Recipient features
The univariate analysis, considering the parameters of the ARF group vs NRF, showed significant differences for age (53 ± 10 vs 47 ± 15, P = 0.005), the score Child-Turcotte-Pugh (P <0.001), the index body mass [24.69 (16.85 to 35.26) vs 25.9 (20.82 to 43.60), P = 0.0074], urea [23,50 (9-68) vs 29 ( 12-112), P = 0.0008], serum [0.80 (0.2 to 1.6) vs 1.04 (0.40 to 2.90), P <0.001] and creatinine clearance [105.3 (51.15 to 240.6) vs 81.39 (19.27 to 209.5), P = 0.0009] (Table 1). No difference was found for gender, MELD score, cause of cirrhosis, diabetes mellitus, serum albumin, sodium and potassium. The multivariate analysis by logistic regression analysis showed that patients with a score Child-Turcotte-Pugh class C was equal to 14 times more likely to develop ARF than those with Child-A, OR = 13.8%, 95.0% CI = 2.64 to 72.70, P = 0.002 (Table 3).
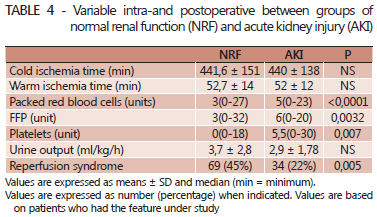
Intraoperative and postoperative risk factors
Univariate analysis showed significant differences between patients who developed ARF vs NRF for the presence of reperfusion syndrome (22.0% vs 45.0%, P = 0.005) and transfusion of packed red blood cells [3 (0-27) vs 5 (0-23), P <0.0001], fresh frozen plasma [3 (0-32) vs 6 (0-20), P = 0.0032] and platelets [0 (0-18) vs 5.5 (0-30), P = 0.007] (Table 4). Multivariate analysis by logistic regression analysis showed that patients with reperfusion syndrome were four times more likely to evolve with ARF than patients without reperfusion syndrome (OR = 3.96, 95% CI = 1.05 to 14.96; P = 0.012).
Among the parameters associated with postoperative ARF, univariate analysis showed a difference to the value of serum creatinine between the ARF and NRF groups [0.9 (0.46 to 1.4) vs 1.57 (0.3 to 3 19), P <0.0001] and for the period of mechanical ventilation [2 (1-5) vs 2 (1-5), P = 0.0039] (Table 4).
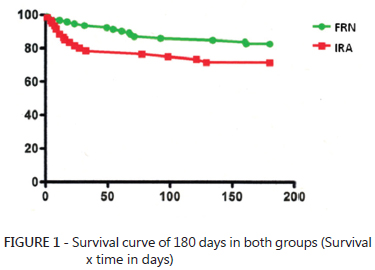
ARF group patients showed no differences in the analysis of survival at 180 days compared with patients of group NRF (71.6% vs 82.2%, P = 0.07) (Figure 1).
There was considerable overlap of values for postoperative serum creatinine among groups of patients NRF and AKI. According to the calculations of C-statistics, the area under the curve for serum creatinine postoperative was 0.89 (0.8335 to 0.9518, 95% CI). Data analysis showed that the value of postoperative serum creatinine = 1.10 mg/dl, the sensitivity and specificity of the test to predict postoperative AKI/TOF-C are, respectively, 80.2 and 80.5, considered the best cutt-off for predicting AKI. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were higher for post-operative serum creatinine compared to values calculated for the value of CTP class C and reperfusion syndrome (Table 5).
These data demonstrate that the factors associated with development of AKI in postoperative TOF-C and Child C in the recipient are the record of reperfusion syndrome and intraoperative values of 1.1 mg/dl for serum creatinine in the first three days postoperatively and the plateau indicating serum creatinine higher than the other identified factors.
DISCUSSION
This retrospective study includes a series of patients undergoing TOF-C, on Liver Transplant Center located in one of the poorest regions of Brazil. This program has significant experience in TOF-C because in the initial roll out of the liver transplant occurred many restrictions. Believing that it could be safer without venovenous bypass (DVV), the surgical team was encouraged to start the liver transplant program. With increasing experience and use of the technique in patients with more advanced stage of liver disease, this option became common and safe. In monitoring these patients were not identified serious complications inherent in the technique (TOF-C).
The AKI is early and severe complication after the TOF9. Some authors have suggested that the DVV not reduce the incidence of postoperative ARF. In this study, incidence of 39.2% was observed. Among the studies was found discrepancies (13% to 94%) in incidence, and this occurred due to lack of consensus on the definition of ARF after liver transplantation 35.
The preoperative AKI is considered a risk factor for the development of ARF in transplants12. The preoperative renal function, assessed by serum creatinine, is part of the MELD score is a stratification of patients on the waiting list for liver transplantation14,30. MELD is responsible for the allocation of liver grafts in the USA, Brazil and several other countries. The higher the value, the more severe the patient1,2. In this study, no difference between the values of MELD group NRF and the AKI. A recent study showed, contrary to others, that MELD> 23 is an independent risk factor for complications, especially the AKI27.
The score Child-Turcotte-Pugh - CTP is still used in the evaluation of patients with terminal liver disease6. It remains an easy, fast and secure way to rate the severity of the cirrhotic patient, especially in convalescence. There is considerable controversy about the superiority of MELD compared to CTP7.
In this study, the class C of CTP was more prevalent in the group that developed ARF, which met the opinion of several authors. This result can be interpreted as if the study population was almost exclusively in cirrhotic patients (not patients with hepatocarcinoma pure, metabolic diseases). With the increase of obesity in the population in general, the body mass index (BMI) has become a target in evaluating candidates for liver transplantation21. As in other studies, increased BMI (BMI> 27) was associated with postoperative complications of liver transplantation. There is still no reason for the origin of these complications. It is believed that increased BMI may affect the dose and volume of distribution for drugs with potential nephrotoxicity. The BMI, in patients evaluated in this study was higher in patients with ARF after TOF-C.
Ischemia of the liver graft, cold or hot, has always been a determining factor for good organ function postoperatively, ie is a direct determinant of the success of liver transplantation19. Thus, despite the development of new solutions for organ preservation programs idealize always perform the procedure with the least possible time of graft ischemia20. In this study, there was no significant difference in ischemic time between the hot and cold NRF group and the AKI.
Several factors may lead to hemodynamic instability during the FOT-C, as bleeding during the dissection of the diseased organ, coagulopathy inherent liver disease and hypotension after reperfusion of the graft11. The reflection of hemodynamic instability is the early onset of ARF after TOF25,26. This study found greater use of PRBC, FFP and platelets in the ARF group compared to the group NRF. Also, more patients in the ARF group had reperfusion syndrome.
Association in the use of blood products intraoperatively and in postoperative complications, especially the AKI, is shown in several studies17. It is believed that the adverse effects from transfusion of blood products are associated with activation of inflammatory mediators, coagulation and immune reactions. The presence of reperfusion syndrome can lead to irreversible damage to the liver graft, leading to dysfunction or non-functioning of the liver22. Other complications such as ARF are associated with patients who presented this syndrome intraoperatively. In this study, reperfusion was longer in the ARF group. In multivariate analysis, was confirmed as an independent risk factor for the onset of ARF post-TOF-C (P = 0.012).
Among the postoperative variables, the time spent with mechanical ventilation and serum creatinine were identified as risk factors for ARF after TOF-C. The continuous mechanical ventilation may be associated with positive fluid balance, which is common in postoperative TOF-C13. For some time, the authors identified changes in pulmonary gas exchange in those who received transfusion of platelets (concentrate or apheresis)33. In this lung damage is called TRALLI29. Today, some advocates judicious indication of platelets in liver transplantation to reduce this syndrome in the postoperative period.
The serum creatinine postoperatively may reflect renal injury occurred during surgery and thus be used as a marker of renal dysfunction23. It is well established the association between increased creatinine and ARF10. However, no study has identified a predictive value for the onset of ARF in the postoperative period.
In multivariate analysis, serum creatinine after TOF-C was the most important predictor. The postoperative complications, non-IRA, no significant differences between the two groups (NRF and ARF). Survival curve of 180 days was similar on both groups (P = 0,07).
CONCLUSION
Acute kidney injury after orthotopic liver transplantation without conventional venovenous bypass is a common disorder, but with good prognosis. Reperfusion syndrome, serum creatinine above 1,10 mg/dl postoperatively and Child C are factors associated with acute kidney injury after orthotopic liver transplantation without conventional venovenous bypass.
REFERENCES
- 1. Asrani SK, Kim WR. Organ allocation for chronic liver disease: model for end-stage liver disease and beyond. Curr Opin Gastroenterol 2010; 26:209-13.
- 2. Batista TP, Sabat BD, Melo PSV et al. Impact of MELD allocation policy on survival outcomes after liver transplantation. Clinics 2011; 66:1-9.
- 3. Briceño J, Solórzano G, Pera C. A proposal for scoring marginal liver grafts. Transpl Int 2000; 13:5249-5252.
- 4. Cabezuelo JB, Ramirez P, Acosta F et al. Does the standard us piggyback surgical technique affect the development of early acute renal failure after orthotopic liver transplantation? Transpl Proc 2003; 35:1913-1914.
- 5. Chen ZS, Zeng FJ, Ming CS et al. Classic orthotopic liver transplantation without venovenous bypass: a report of 45 cases. Transpl Proc 2003; 35:364-365.
- 6. Cholongitas E, Papatheodoridis GV, Vangeli M et al. Systematic review: The model for end-stage liver disease--should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther 2005; 22:1079-1089.
- 7. Cholongitas E, Senzolo M, Triantos C et al. MELD is not enough--enough of MELD? J Hepatol 2005; 42:475-477.
- 8. Fonouni H, Mehrabi A, Sollimani M et al. The need for venovenous bypass in liver transplantation. HPB 2008; 10:196-203.
- 9. Gainza FJ. The kidney is the liver's best friend. Liver Transpl 2010;16:411.
- 10. Gurusamy KS, Pamecha V, Davidson BR. Piggyback graft for liver transplantation. Cochrane Database Syst Rev 2011; 19:1:CD00 8258.
- 11. Hilmi I, Horton CN, Planisic RM et al. The impact of post reperfusion syndrome on short-term patient and liver allograft outcome in patients undergoing orthotopic liver transplantation. Liver Transpl 2008; 14:504-508.
- 12. Iglesias JI, DePalma JA, Levine JS. Risk factors for acute kidney injury following orthotopic liver transplantation: the impact of changes in renal function while patients await transplantation. BMC Nephrol 2010; 11:30.
- 13. Jiang GQ, Peng MH, Yang DH. Effect of perioperative fluid therapy on early phase prognosis after liver transplantation. Hepatobiliary Pancreat Dis Int 2008; 7:367-372.
- 14. Kamath PS, Kim RW. The model for end-stage liver disease (MELD). Hepatology 2007; 45:797-805
- 15. Khosravi MB, Jalacian H, Lahsaee M et al. The effect of clamping of inferior vena cava and portal vein on urine output during liver transplantation. Transpl Proc 2007; 39:1197-1198.
- 16. Lacerda C, Melo P, Fonseca Neto OCL et AL. Transplante de fígado em hospital universitário do Recife: resultados iniciais. Rev Col Bras Cir 2003; 30:29-33.
- 17. Lee JP, Heo NJ, Joo KW et al. Risk factors for consequent kidney impairment and differential impact of liver transplantation on renal function. Nephrol Dial Transpl 2010; 25:2772-2785.
- 18. Lerut J, Gertsch P, Blungart LH. Piggyback adult orthotopic liver transplantation. Helv Chir Acta 1989; 56:537.
- 19. Macedo FI, Miranda LE, Fernandes JL et al. Donor age as a predictor of risk for short-term outcomes after liver transplant. Exp Clin Transpl 2010; 8:202-209.
- 20. Macedo FIB, Miranda L, Padua TC et al. Effects of donor age on patient survival in liver transplantation: short-and long-term analysis. Hepato Gastroenterol 2009; 56:1133-1136.
- 21. Nair S, Verma S, Thuluvath PJ. Obesity and its effect on survival in patients undergoing orthotopic liver transplantation in the United States. Hepatology 2002; 35:105-9.
- 22. Nikeghbalian S, Dehghani M, Salahi H et al. Effects of surgical technique on postoperative renal function after orthotopic liver transplant. Exp Clin Transpl 2009; 7:25-27.
- 23. O'Riordan A, Donaldson N, Cairns H et al. Risk score predicting decline in renal function postliver transplant: role in patient selection for combined liver kidney transplantation. Transplantation 2010; 89:1378-1384.
- 24. Oberkofler CE, Dutkowski P, Stocker R et al. Model of end stage liver disease (MELD) score greater than 23 predicts lenger of stay in the ICV but not mortality in liver transplant recipients. Crit Care 2010; 14:R117.
- 25. Ramsay M. The reperfusion syndrome: Have we made any progress? Liver Transpl 2008; 14:412-414.
- 26. Sakai T, Matsusaki T, Marsh JW et al. Comparison of surgical methods in liver transplantation: retrohepatic caval resection with venovenous bypass (VVB) versus piggyback (PB) with VVB versus PB without VVB. Transpl Int 2010; 23:1247-1258.
- 27. Schwarz B, Pomaroli A, Hoerman C et al. Liver transplantation without venovenous bypass: morbidity and mortality in patients with greater than 50% reduction in cardiac output after vena cava clamping. J Cardiothoracic Vasc Anesth 2001; 15:460-462.
- 28. Shaw Bw Jr. Some further notes on venous bypass for orthotopic transplantation of the liver. Transpl Proc 1987; 19:13-16.
- 29. Sokolovic M, Pastores SM. Transfusion therapy and acute lung injury. Expert Rev Respir Med 2010; 4:387-393.
- 30. Tenorio AL, Macedo FIB, Miranda LEC et al. Survival on waiting list for liver transplantation before and after introduction of the model for end-stage liver disease score. Transpl Proc 2010; 42:407-411.
- 31. Tinti F, Umbro I, Meçule A et al. RIFLE criteria and hepatic function in the assessment of acute renal failure in liver transplantation. Transplant Proc 2010; 42:1233-1236.
- 32. Tzakis A, Todo S, Starzl TE. Orthotopic liver transplantation with preservation of the inferior vena cava. Ann Surg 1989; 210:649-652.
- 33. Watkins TR, Nathens AB. TRALI: a new case definition, a new epidemic? Am J Respir Crit Care Med 2007; 176:839-840.
- 34. Xu X, Ling Q, Wei Q, Zheng SS et al. An effective model for predicting acute kidney injury after liver transplantation. Hepatobiliary Pancreat Dis Int 2010; 9:259-263.
- 35. Zhu M, Li Y, Xia Q et al. Strong impact of acute injury on survival after liver transplantation. Transpl Proc 2010; 42:3634-3638.
Predictors of acute kidney injury in patients undergoing a conventional orthotopic liver transplant without veno-venous bypass
Publication Dates
-
Publication in this collection
01 July 2011 -
Date of issue
June 2011
History
-
Received
20 Oct 2011 -
Accepted
25 Jan 2011