Abstracts
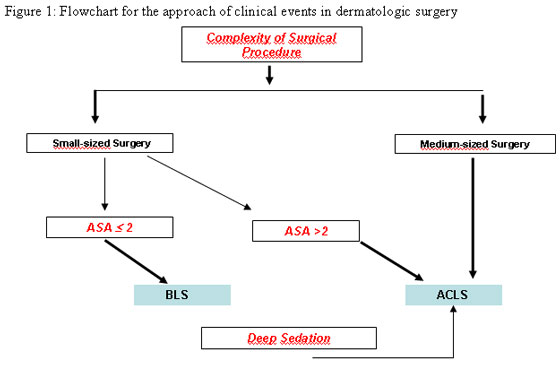
Since complexity of surgical procedures has increased, and patients' co-morbidities have become more frequent, the risk of clinical complications in dermatologic surgery has also increased in the past decades. In order to better assess these risks, a flowchart based on a ruling triad consisting of the patient's health status, sedation level, and procedure complexity was developed to establish the type of cardiovascular support adequate to each procedure. Patients undergoing small surgeries with ASA < 2 should be assigned to basic life support; patients undergoing small surgeries with ASA > 2, and those undergoing medium-sized surgeries or deep sedation should be assigned to advanced cardiac life support (ACLS).
Advanced cardiac life support; Cardiopulmonary resuscitation; Dermatology; Emergencies; Intraoperative complications; Surgical procedures, minimally invasive surgical procedures
Com o aumento da complexidade cirúrgica e comorbidades da população, o risco de intercorrências clínicas em cirurgia dermatológica aumentou nas últimas décadas. Para sua abordagem foi criado um fluxograma baseado na tríade decisória formada pelo estado físico do paciente, grau de sedação e porte do procedimento, indicando o tipo de suporte cardiovascular em cada procedimento. Pacientes submetidos a cirurgias de "porte pequeno" e ASA < 2 devem receber suporte básico de vida; os submetidos a cirurgias de "porte pequeno" e ASA > 2, a cirurgias de "porte médio" ou a sedação profunda devem receber suporte avançado de vida em cardiologia.
Complicações intraoperatórias; Dermatologia; Emergências; Procedimentos cirúrgicos minimamente invasivos; Ressuscitação cardiopulmonar; Suporte vital cardíaco avançado
COMMUNICATION
Basic life support and advanced cardiac life support: proposal of a new strategy to approach and prevent clinical events in dermatologic surgery
Fábio Roismann TimonerI; Nelson Marcos FerrariII; Manoel Carlos Sampaio de Almeida RibeiroIII; Frida Liane PlavnikIV; Carlos d'Aparecida Santos Machado FilhoV
IAssistant Physician in the Dermatologic Surgery Sector - Discipline of Dermatology - Faculdade de Medicina do ABC - Sao Paulo (SP), Brazil
IIHead of the Dermatologic Surgery Sector - Faculdade de Ciencias Medicas da Santa Casa de Sao Paulo - Sao Paulo (SP), Brasil
IIIAssistant in the Discipline of Social Medicine - Faculdade de Ciencias Medicas da Santa Casa de Sao Paulo - Sao Paulo (SP), Brazil
IVAffiliated Professor - Discipline of Nephrology- Universidade Federal de Sao Paulo - Sao Paulo (SP), Brazil
VProfessor and Head of the Discipline of Dermatology - Faculdade de Medicina do ABC - Sao Paulo (SP), Brazil
Mailing Address Mailing Address Fábio R. Timoner Av. Índico, 499 - Jardim do Mar 09750 601 São Bernardo do Campo, SP Tel./fax: 11 7872-2004 11 4123-5805 E-mail: drfabiotimoner@hotmail.com
ABSTRACT
Since complexity of surgical procedures has increased, and patients' co-morbidities have become more frequent, the risk of clinical complications in dermatologic surgery has also increased in the past decades. In order to better assess these risks, a flowchart based on a ruling triad consisting of the patient's health status, sedation level, and procedure complexity was developed to establish the type of cardiovascular support adequate to each procedure. Patients undergoing small surgeries with ASA < 2 should be assigned to basic life support; patients undergoing small surgeries with ASA > 2, and those undergoing medium-sized surgeries or deep sedation should be assigned to advanced cardiac life support (ACLS).
Keywords: Advanced cardiac life support; Cardiopulmonary resuscitation; Dermatology; Emergencies; Intraoperative complications; Surgical procedures, minimally invasive surgical procedures
Dermatologic surgery is considered a safe intervention, with low incidence of complications, except in a few cases where reports show high blood pressure rates in ambulatorial procedures with local anesthesia.1-2 However, greater technical complexities of procedures such as liposuction and facial lift, removal of larger tumors, sedation, and co-morbidities affecting the aging population increase the risk of surgical complications and clinical events. Although rare, these complications may be potentially fatal .3-4
A flowchart (Figure 1) was developed to establish the type of clinical support to be adopted in each surgery: basic life support (BLS) or advanced cardiac life support (ACLS), based on the characteristics of the procedure and on the patient's co-morbidities. A list with routine medical procedures for perioperative care was also suggested. The patient's health status, according to the classification of the American Society of Anesthesiologists (ASA), complexity of dermatologic surgery, and sedation level chosen by the surgical team were considered in the development of the flowchart. These three factors combined were called the "ruling triad".
BLS and ACLS have been adopted as standardized approaches to clinical events; the former is adopted in low-risk events and the latter, in higher-risk situations. Therefore, at least one member of the medical team involved in the procedure must be qualified to give these supports, and the surgical environment must be adapted to suit this purpose.
Dermatologic procedures were classified into small-sized surgeries, that is, surgeries that typically carry very low risk based on literature reports5; for example, superficial and medium peeling, shaving, curettage, electrocoagulation, cryotherapy, laser, filling, biopsies, tumor exeresis, nail surgery, otoplasty, blepharoplasty, liposuction < 100 ml, and hair implant. medium-sized surgeries are those that involve medium risk, such as mini lift, liposuction > 100 ml, Baker's peeling and removal of extensive tumors. Sedation was defined as the level to which the reflexes of the upper respiratory tract are altered, producing hemodynamic changes.
A complementary strategy, which includes the prerequisites of the medical team and surgical environment, pre-surgical assessment and perioperative care, was developed (Chart 1). The flowchart describes the following situations: 1- Small surgery, ASA 1 or 2, indicative of BLS; 2- Small surgery, ASA > 2, indicative of ACLS, and 3- Medium-sized surgery or deep sedation, indicative of ACLS.
This is the first study in the literature to suggest a differentiated strategy for dermatologic procedures, based on the triad: patient's health status, complexity of dermatologic procedure, and sedation level.
Fader and Johnson investigated the complications that may occur in the routine of a dermatologic office, emphasizing the need for the training of professionals involved in basic or advanced cardiac life support. The observations and suggestions were in reference to the length of time that the medical team would take to get to the patient, but they did not refer to the complexity of the procedure or the patient's health status.4
Although most dermatologic procedures are considered low risk (less than 1%), liposuction, removal of extensive tumors, and facial lift all involve medium risk, with complication rates varying from 1 to 5%.4 Baker Phenol peel presents direct risk of cardiac toxicity, leading to arrhythmia that may be fatal. It may also present renal toxicity, with higher risk for cardiophatic or nephropatic patients.6 An important factor associated with clinical events is an increase in catecholamine levels, which may be 40 times greater than basal levels and result from different stress levels and potential for causing pain, technical complexity and duration of the procedure.7
It is relevant to stress that low-risk rates of complications in dermatologic surgery take into account intra-surgery complications, but not those that occur in the 48-hour period after surgery. It is estimated that more than half of the deaths that occur in the post-surgical period may be due to cardiac events. In patients with coronaropathy, ischemia is frequent in the post-surgical period. Sometimes activation of the sympathetic nervous system and of the adrenal medulla, due to pain or homeostatic disorders, may lead to cardiac frequency alterations and cardiac output, which may worsen the patient's clinical condition.8
Moreover, other risk factors are involved in more complex procedures, such as the amount of anesthesia, surgical topography, length of surgery, detachment area, and bleeding, which may contribute to clinical events. 9
The consideration of the patient's health status, based on the classification of ASA, is due to its practicality and wide acceptance. It also has greater predictive value for fatal cardiac complications, especially for patients with ASA > 2, surpassing the risks of the procedure itself and sedation level.10
The adoption of BLS and ACLS allows fast and coordinated action. This strategy may be used to decide which surgeries may be performed safely in a doctor's office, for having a profile closer to BLS, or in ambulatory surgery centers or hospitals, which are closer to ACLS.
In conclusion, the relevance of this proposal for evaluation and fitting of patients in dermatologic surgery will be optimized with the use of this flowchart, thus seeking the best individualized support in each case. Prospective follow-up studies may confirm the significance of this study and contribute to its improvement and redimensioning.
REFERENCES
Recebido em 27.10.2008.
Aprovado pelo Conselho Consultivo e aceito para publicação em 23.11.09.
Financial support: None.
Conflict of interest: None.
- 1. Pimentel ERA, Oliveira JP, Bloch LD, Niwa ABM. Risco de complicações durante a cirurgia dermatológica: protocolo das exéreses em fuso. An Bras Dermatol. 2005;80:493-8.
- 2. Larson MJ, Taylor RS. Monitoring vital signs during outpatient Mohs and post-Mohs reconstructive surgery performed under local anesthesia. Dermatol Surg. 2004;30:777-83.
- 3. Fader DJ, Johnson TM. Medical issues and emergencies in the dermatology office. J Am Acad Dermatol. 1997;36:1-16.
- 4. Eagle KA, Brundage BH, Chaitman BR, Ewy GA, Fleisher LA, Hertzer NR, et al. Guidelines for perioperative cardiovascular evaluation for noncardiac surgery. Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Committee on Perioperative Cardiovascular Evaluation for Noncardiac Surgery. Circulation. 1996;93:1278-317.
- 5. Dias DL, Bittencourt LAK, Cavicchio JR, Figueiredo MJ, Simões AM. Importância e fundamentos da avaliação pré-operatória para pacientes submetidos a cirurgia não cardíaca: quem deve ser avaliado e quem deve avaliar. Rev Soc Cardiol Estado de São Paulo. 2000;10:259-67.
- 6. Landau M. Cardiac complications in deep chemical peels. Dermatol Surg. 2007;33:190-3.
- 7. Malamed SF. Medical emergencies in the dental office. 4th ed. St Louis: Mosby-Year Book; 1993. p.229-53.
- 8. Baruzzi ACA, Knobel E. Quais pacientes devem receber cuidados de UTI no pós operatório e que condutas devem ser tomadas para prevenir complicações cardiovasculares? Rev Soc Cardiol Estado de São Paulo. 2000;10:282-8.
- 9. Yoho RA, Romaine JJ, O'Neil D. Review of liposuction, abdominoplasty and face-lift mortality and morbidity risk literature. Dermatol Surg. 2005;31:733-43.
- 10. Nicolai JN, Maia, LN, Costa OMC. Abordagem pré-operatória do paciente com síndrome isquêmica aguda recente. Rev Soc Cardiol Estado de São Paulo. 2000;10:324-33
Mailing Address
Publication Dates
-
Publication in this collection
06 May 2010 -
Date of issue
Feb 2010
History
-
Accepted
23 Nov 2009 -
Received
27 Oct 2008