Abstracts
Muckle-Wells syndrome is a rare autosomal dominant disease that belongs to a group of hereditary febrile syndromes. It is characterized by recurrent and self-limited episodes of fever, urticaria, arthralgia, myalgia and conjunctivitis since childhood, which are related to exposure to cold temperatures. Lately, progressive sensorineural hearing loss occurs. Amyloidosis is the main complication and can be found in about 25% of the cases. It has been demonstrated that there is an association with mutations in the NLRP3 gene, which codifies cryopyrin, a protein responsible for regulating the production of proinflammatory cytokines, such as interleukin-1Beta. The authors report four cases of the disease within a family.
Arthralgia; Conjunctivitis; Fever; Genetic diseases, inborn; Hearing loss, sensorineural; Interleukin-1Beta; Urticaria
A síndrome de Muckle-Wells é doença autossômica dominante rara, incluída no grupo das síndromes febris hereditárias. Caracteriza-se por episódios recorrentes e autolimitados de febre, urticária, artralgia, mialgia e conjuntivite, desde a infância, relacionados com a exposição ao frio. Mais tardiamente, há perda auditiva neurossensorial progressiva. Amiloidose, a principal complicação, desenvolve-se em cerca de 25% dos casos. Associa-se a mutações no gene NLRP3 (antes CIAS1) que codifica a criopirina, proteína reguladora da produção de citocinas pró-inflamatórias, como a interleucina-1beta. Relata-se a ocorrência dessa doença incomum em quatro membros de uma única família.
Artralgia; Conjuntivite; Doenças genéticas inatas; Febre; Interleucina-1beta; Perda auditiva neurossensorial; Urticária
CLINICAL CASE
Four cases of Muckle-Wells Syndrome within the same family*
Ana Francisca Junqueira Ribeiro PereiraI; Luciana Baptista PereiraII; Everton Carlos Siviero do ValeIII; Leandro Augusto TanureIV
IResident of the Dermatological Service of the University Hospital of the Federal University of Minas Gerais (UFMG) - Belo Horizonte (MG), Brazil
IIAssistant Professor of the Dermatological Service of the Faculty of Medicine of the Federal University of Minas Gerais (UFMG) - Belo Horizonte (MG), Brazil
IIIAssistant Professor of the Dermatological Service of the University Hospital of the Federal University of Minas Gerais (UFMG) - Belo Horizonte (MG), Brazil
IVMD, ongoing master course in the Rheumatology Service of the University Hospital of the Federal University of Minas Gerais (UFMG) - Belo Horizonte (MG), Brazil
Mailing address
ABSTRACT
Muckle-Wells syndrome is a rare autosomal dominant disease that belongs to a group of hereditary febrile syndromes. It is characterized by recurrent and self-limited episodes of fever, urticaria, arthralgia, myalgia and conjunctivitis since childhood, which are related to exposure to cold temperatures. Lately, progressive sensorineural hearing loss occurs. Amyloidosis is the main complication and can be found in about 25% of the cases. It has been demonstrated that there is an association with mutations in the NLRP3 gene, which codifies cryopyrin, a protein responsible for regulating the production of proinflammatory cytokines, such as interleukin-1Beta. The authors report four cases of the disease within a family.
Keywords: Arthralgia; Conjunctivitis; Fever; Genetic diseases, inborn; Interleukin-1Beta; Hearing loss, sensorineural; Urticaria
INTRODUCTION
Muckle-Wells syndrome (MWS, Muckle-Wells syndrome is a rare autosomal dominant disease that belongs to a group of hereditary febrile syndromes. It is associated with mutations in the NLRP3 gene (before known as CIAS1) which codifies cryopyrin. This protein is responsible for regulating the production of proinflammatory cytokines, such as interleukin-1Beta. There have been already described more than 50 mutations in this gene, some related with different phenotypes. The rareness of this syndrome is the reason for presenting these four cases.
CASE REPORTS
CASE 1
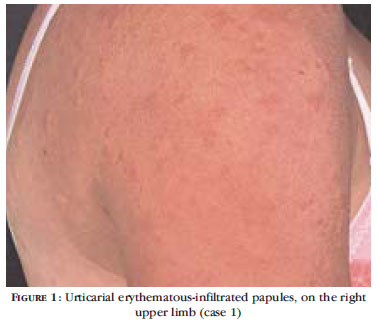
Female pacient, aged 43, presents recurrent condition of urticaria (Figures 1, 2 and 3), arthralgias and edema of the knees and ankles, apart from conjunctival hyperemia from the very early months of life, which lasts for about two or three days and is related to exposure to the cold. The cutaneous condition is usually not very pruriginous with a discrete local ardency. The patient has been complaining of hypoacusis for some years and audiometry has shown progressive sensorineural hearing loss. The antinucleus factor (ANF), cryoglobulins, anti-cardiolipins and lupic anticoagulants are persistently negative. The speed of ESR (Erythrocyte Sedimentation Rate) and activated protein C (APC) are high, dosages of the levels of C3 and C4 are normal. Laboratory review, routine urine-test and radiography of the chest and hands did not present any alterations. Histopathological exams of the urticarial lesions of the skin showed, on the dermis, discrete lymphohistiocytic perivascular inflammatory infiltrate, with some neutrophils and eosinophils, apart from edema and vascular inflammatory agression, suggesting neutrophilic vasculitis of small vessels (Figure 4). The direct immunofluorescene was negative for IgA, IgG, IgM e C3.
CASE 2
Female patient, aged 24, with episodes of pain and edema on the ankles, associated with non-pruriginous urticaria, related to the cold, since infancy. Laboratory exams show high ESR, negative ANF, normal levels of C3 and C4 and routine urine-tests without any alterations. Skin biopsy revealed discrete lymphocytic perivascular inflammatory infiltrate, with a few neutrophils, on the superior dermis, with agressions to the vessels. The direct immunofluorescene was negative. Audiometry has shown discrete sensorineural hearing loss, on the left side.
CASE 3
Male patient, aged 20, presents episodes of urticaria, conjunctival hyperemia (Figure 5) and arthralgia in the knees, since early infancy, that gets worse with exposure to the cold. The cutaneous lesions are not pruriginous, and there is a a feeling of increase of the local temperature. There is sensorineural deafness on the left side. The ESR and APC are high, ANF is negative and the levels of C3 and C4 are normal. The routine urine-test diagnosed hypocalciuria. Histopathological exams of the skin showed only chronic dermatitis. Genetic studies showed normal karyotype and the research on chromosome breakage was negative.
CASE 4
Female patient, aged 17, with recalcitrant condition of non-pruriginous urticaria (Figure 6) and pain in the ankles, from the early years of life associated with exposure to the cold. There is a discrete bilateral sensorineural hearing loss. ANF is negative and routine urine-exams, ESR, APC and levels of C3 and C4 are normal. Histopathological exams showed discrete lymphocytic exsudate with a few neutrophils around the small vessels, on the superior dermis, with vascular agression besides epidermis on the limits of normality Direct immunofluorescene was negative.
DISCUSSION
The MWS is characterized by recurrent and selflimited episodes of fever, urticaria, arthralgia, myalgia and conjunctivitis since childhood, and sometimes related to exposure to the cold.1,2 Headaches, 3abdominal pain,3,4 and growth retardation can still be observed in the clinical condition. Later, there is progressive. sensorineural hearing loss1. Amyloidosis type AA, present in about 25%of the cases, is the main complication of the disease, with predominance of renal problems.1,2
In general, cutaneous eruption is the first symptom to be noticed and it is characterized by migratory maculopapular rashes5. Pruritus is unsual but there might be a burning sensation5. The histological findings of perivascular dermal inflammatory infiltrate mainly consisting of polymorphonuclear cells contrast with the typical infiltrate of eosinophils and lymphocytes of the classical urticaria, leading to the use of the term pseudo-urticaria, by some authors, to refer to the eruption of MWS5. Although the classical urticaria lesions are the most characteristic dermatological manifestations, El-Darouti et al. Describe six cases of sclerodermoid lesions, with hyperpigmentation, sclerosis and hypertrichosis4 .
Besides the MWS, the Familial Cold Autoinflammatory Syndrome, (FCAS) related to the cold and the Chronic Infantile Neurological Cutaneous and Articular Syndrome (CINCA) are also hereditary febrile diseases, autosomal dominant. The three diseases are equally related to mutations in the NLRP3 gene (before known as CIAS1) located in chromosome16. Maksimovic et al. observed different phenotypes of the three syndromes within the same family 7 and Hoffman et al. found different intra familial phenotypes as a result of the same mutation in the NLRP3 gene8. Dodé et al. identified the same mutation in two families with the MWS syndrome and in two other ones with FCAS, There was no ethnic similarity among them.9
All these findings suggest that the MWS, the FCAS and the CINCA syndromes constitute different phenotypic expressions of the same disease.3,7,10,11 There are described cases of overlapping of theses syndromes. It is believed that there is a correlation between the genotype and the phenotype generating different clinical characteristics, penetrance and gravity 12. Besides that, environmental factors and modifying genes can determine different phenotypes3,6. It seems that the FCAS represents the mildest phenotype and the CINCA the most serious one. While the FCAS basically presents itself as urticaria to the cold, fever and arthralgia in the MWS there is hearing loss and amyloidosis. As for the CINCA, there are alterations in the central nervous system and arthropathy. The development of urticaria starts very early, still in the neonatal period. The neurologic manifestations, dure to chronic aseptic meningitis occur in almost all patiens with CINCA and vary from chronic headache, vomit and papilledema till spastic paralysis and epilepsy 5.
In accordance with the different studies of families with carriers of MWS, the cases reported here respect the autossomal dominant pattern of occurence. Among the four members of this family, it can be noticed variable degrees of signs and symptoms analogously to what is described in the medical literature. So, it would be possible to classify the patients studied here as carriers of one of the three syndromes (FCAS, MWS or CINCA), that is, carriers of different spectra of one only disease. However, all the four patients presented, although in different degrees, sensorineural hearing loss, a manifestation also present in MWS. Besides that, none of them has presented, up to the moment, neurological symptoms or frank arthritis, what weakens the hypothesis of being one of these patients carrier of CINCA.
The autoinflammatory syndromes are a group of systemic inflammatory diseases that are not caused by any pathogen or autoantibody. They result from the aberrant regulation of the cytokine signaling pathways, leading to persistent or uncontrolled inflammation.11 It is not known yet if these diseases could originate themselves from normal responses to an infection, although it is precisely the persistent inflammatory condition in the absence of an apparent infection the characteristic point of such class of diseases.11
Periodic fever syndromes, accompanied by urticaria like eruptions such as: the FCAS, the MWS and the CINCA, were associated with mutations in the NLRP3 (before CIAS1) and have been jointly called periodic syndromes, associated to the cryopyrin (CAPS, cryopyrin associated periodic syndromes ).10 This group is currently, considered another spectrum of the main autoinflammatory syndromes.10 Therefore, the concept of autoinflammatory syndrome has been extended to include other rare hereditary diseases with or without periodic fever such as the pyoderma gangrenosum and pyogenic sterile arthritis10. On the other hand, the presence of some of these genetic mutations in less unsual diseases such as Behçet and Crohn diseases, led to the expansion of the spectrum of the autoinflammatory diseases to the also called.collagen diseases10 . All them share the same physyopathology, with hyperactivation of neutrophils, monocytes or macrophages besides the genetic predisposition to the deregulation of the inborn immunity signaling10. Developments in the understanding of the genetic base of periodic syndromes associated to the cryopyrin, led to the discovery of cytokine signaling molecules that are essential for the regulation of certain inflammatory pathways11. Cryopyrin is responsible for the activation pathway of interleukin-1, acting as part of a macromolecular complex called inflamassomo NALP3.11 This, in turn, activates the interleukin -1beta and the interleukin-18, resulting in immunologic stimulation, inflammation and tissue injury.11 The cryopyrin also regulates the activation pathway of the nuclear factor kappa B (NFkB) and of the apoptosis3. However, the mechanism by which such pathways are aberrantly regulated in the hereditary autoinflammatory syndromes remains obscure, although the multations in the NLRP3 gene (before CIAS1), seem to cause a persistent hyper-regulation in such pathways11, leading to na intense pro-inflammatory effect6. On the other hand, the genetic heterogeneity of the cryopyrin-associated periodic syndromes has been lately emphasized 6,13. Neven et al. managed to identify mutations in the NLRP3 gene in only 60% of the patients analyzed13.
The theraupetic options are: the anti-inflammatory, the anti-histaminic1, colchicine and corticoteroids, all with satisfactory responses. Lately, it has been used a recombinant homologous of the interleukin -1beta (anakinra), with good results, observing even an improvement in the hearing loss and amyloidosis when introduced at an early stage
The dramatic response of the hereditary febrile syndromes to blockers of the activation pathways of citokines such as the anakinra, corroborates the crucial role of the inflammatory citokines, e.g, the interleukin -1beta in the pathogenesis of such syndromes3,11,12. For this reason, these citokines became the potencial therapeutic targets for this group of diseases. Better elucidation of such mechanisms can, in the future, facilitate the developement of biological strategies of treatment, ensuring a highly efficient and selective immunosuppressive intervention. 
REFERENCES
- 1. Haas N, Küster W, Zuberbier T, Henz BM. Muckle-Wells syndrome: clinical and histological skin findings compatible with cold air urticaria in a large kindred. Br J Dermatol. 2004;151:99-104.
- 2. Kagami S, Saeki H, Kuwano Y, Imakado S, Tamaki K. A probable case of Muckle-Wells syndrome. J Dermatol. 2006;2:118-21.
- 3. Farasat S, Aksentijevich I, Toro JR. Autoinflammatory diseases: clinical and genetic advances. Arch Dermatol. 2008;144:392-402.
- 4. El-Darouti MA, Marzouk SA, Abdel-Halim MR. Muckle-Wells syndrome: report of six cases with hyperpigmented sclerodermoid skin lesions. Int J Dermatol. 2006;45:239-44.
- 5. Neven B, Prieur AM, Quartier dit Maire P; Medscape. Cryopyrinopathies: update on pathogenesis and treatment. Nat Clin Pract Rheumatol. 2008;4:481-9.
- 6. Aksentijevich I, Nowak M, Mallah M, Chae JJ, Watford WT, Hofmann SR, et al. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID). Arthritis Rheum. 2002;46:3340-8.
- 7. Maksimovic L, Stirnemann J, Caux F, Ravet N, Rouaghe S, Cuisset L, et al. New CIAS1 mutation and anakinra efficacy in overlapping of Muckle-Wells and familial cold autoinflammatory syndromes. Rheumatology. 2008;47:309-10.
- 8. Hoffman HM, Mueller JL, Broide DH, Wanderer AA, Kolodner RD. Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet. 2001;29:301-5.
- 9. Dodé C, Le Dû N, Cuisset L, Letourneur F, Berthelot JM, Vaudour G, et al. New mutations of CIAS1 that are responsible for Muckle-Wells syndrome and familial cold urticaria: a novel mutation underlies both syndromes. Am J Hum Genet. 2002;70:1498-506.
- 10. Kanasawa N, Furukawa F. Autoinflammatory syndromes with a dermatological perspective. J Dermatol. 2007;34:601-18.
- 11. Shinkai K, McCalmont TH, Leslie KS. Cryopyrinassociated periodic syndromes and autoinflammation. Clin Exp Dermatol. 2007;33:1-9.
- 12. Hawkins PN, Lachmann HJ, Aganna E, McDermott MF. Spectrum of clinical features in Muckle-Wells syndrome and response to anakinra. Arthritis Rheum. 2004;50:607-12.
- 13. Neven B, Callebaut I, Prieur AM, Feldmann J, Bodemer C, Lepore L, et al. Molecular basis of the espectral expression of CIAS1 mutations associated with phagocytic cell-mediated autoinflammatory disorders CINCA/NOMID, MWS and FCU. Blood. 2004;103:2809-15.
Publication Dates
-
Publication in this collection
27 Jan 2011 -
Date of issue
Dec 2010
History
-
Received
18 Aug 2008 -
Accepted
15 Oct 2008