Abstract
The objective of this study was to investigate the relationship between the management capacity of Pharmaceutical Services and socioeconomic indices in Brazilian municipalities, analyzing which contextual factors are involved in its development. Data from a cross-sectional exploratory study at national scale and indicators were used to define the capacity of Pharmaceutical Services management. Pearson’s chi-square test and multivariate analysis were performed to associate Pharmaceutical Services management capacity with socioeconomic indices of each municipality. The results prove the existence of significant relationships between management capacity and socioeconomic indicators, suggesting that management capacity is influenced by the environment in which it operates. Municipalities that presented superior results were those with better socioeconomic indices and better conditions and structure of their healthcare system, reflecting a greater number of professionals, greater participation of popular social control and use of public resources. Municipalities with a smaller population size and lower socio-economic indices have less ability to manage pharmaceutical services, revealing worsening inequalities for its citizens. The existence of an adequate minimum structure, a qualified workforce, service organization, and opportunities for political articulation are essential for such municipalities to develop and improve their management capacity and obtain proper financing based on socioeconomic indicators to facilitate effective access to and adequate use of medicines for the population.
Keywords:
Pharmaceutical service management; Primary health care; Socioeconomic indicators; Socioeconomic inequalities
INTRODUCTION
Ensuring access to essential medicines is one of the most complex challenges for all healthcare systems, including the medicines supply chain. Dedicated policies need to be put in place to achieve this aim (WHO, 2019). In primary health care, access to essential medicines means resolving the care process for most health conditions (WHO, 2003).
Beyond problems related to the pharmaceutical market and the high prices, the healthcare system stipulations in terms of patients’rights, financial support, and the organization of the pharmaceutical services are crucial to ensure access to essential medicines in an efficient manner to address the population’s healthcare needs (Rocha et al., 2021).
Access to well-known and newer essential medicines for priority health problems depends on a certain minimal level of medical and pharmaceutical services. This includes inexpensive diagnostic tests to confirm diagnosis, and a well-informed trained workforce. Strengthening the overall capacity of the healthcare and supply systems is a prerequisite to respond adequately to the population’s increased medical and pharmaceutical needs (Wirtz et al., 2017).
However, ensuring equitable access to such medicines is still one of the important problems to be surpassed. In Brazil, pharmacists play a fundamental role in access to essential medicines and in the organization of the healthcare system because, unlike most countries, medicines provided by the public system are mostly funded, purchased, distributed, and provided by public health establishments, particularly at the municipal level (Carvalho, 2016). The number of registered pharmacists surpasses 30,000 in Primary Health Care (PHC) in the Unified Healthcare system (SUS, in Portuguese). This number grew by 75% from 2008 to 2013 (Carvalho et al., 2016; Carvalho et al., 2017).
Pharmaceutical Services (PS) in the municipal healthcare system comprises an open subsystem characterized by complexities related to the organizational culture and the structure of services, procedures and workforce, as well as the political and economic context in which it operates (Bernardo, Soares, Leite, 2021). Thus, its management reflects the equity in access to medicines and population health.
Notably, healthcare equity is realized when all people can attain their full potential for health and wellbeing. Health inequity and social exclusion have been usually associated with an individual’s age, gender, social class, race, skin color, ethnicity, religious beliefs, educational status, living standards, political views, appearance, physical or mental ability, sexuality, or sexual orientation (European Commission, 2017). However, the postcode can be an additional factor related to health inequality: the postcode lotteries in healthcare systems refer to variations in health care between different geographical areas that appear arbitrary and unlinked to healthcare needs (Graley, May, McCoy, 2011). In Brazil, in contrast, the postcode may gain a more predictable meaning, due to great economic and social inequalities between the different regions of the country and between neighboring municipalities.
As PS is part of this complex arrangement of municipal health management, it is understood that it is necessary to analyze which contextual factors are involved in its development capacity and which can collaborate so that investments in PS can meet local needs, (Rocha et al., 2021; Wirtz et al., 2017; Carvalho et al., 2017; Vogler, Österle, Mayer, 2015; Gerlack et al., 2017; Pereira et al., 2021; Leite et al., 2015) considering PS within the socioeconomic environment in which it is inserted.
Public policies aimed at strengthening municipal PS management capacity have been implemented over the years, such as the QUALIFAR-SUS program, training courses for SUS pharmacists, and the inclusion of the MHDI as a criterion for the transfer of funds for the acquisition of medicines. However, despite advances, weaknesses in the development of pharmaceutical services persist in the country (Manzini et al., 2020; Mendes, Leite, Carnut, 2020) strongly related to management capacity (Gerlack et al., 2017; Rover et al., 2016; Pereira et al., 2021). Researchers must collaborate to inform decision-making related to policies, providing evidence and new hypotheses that can provoke revisiting existing policies and the creation of new ones.
In this context, this study investigated the relationship between the management capacity of municipal PS departments and the local socioeconomic system.
METHOD
Evaluative research was applied to the management capacity of PS departments in the Brazilian public healthcare system and the local socioeconomic system, for which the methodological procedure adopted was divided into two stages:
I) Calculation of the Pharmaceutical Services Management Capacity Indicator (PSMind) in Brazilian municipalities’ PHC (Faraco, Rover, Leite, 2023), in a sample of 507 municipalities selected by the National Survey on Access, Use and Promotion of Rational Use of Medicines in Brazil (PNAUM). PNAUM is a cross-sectional exploratory study, consisting of the primary data survey on a representative sample of PHC services in 600 municipalities in Brazilian regions (Álvares et al., 2017; Ministério da Saúde, 2012). Due to the country size and the complexity to obtain a national sample, most studies regarding pharmaceutical services in the public healthcare system are of a local nature. The data were collected between 2014 and 2015 and represent a milestone for understanding the national panorama of access and use of medicines in the Brazilian population (Pereira et al., 2021). The variables that comprised the indicator (PSMind) were selected as described by Faraco, Rover, Leite (2023);
II) Association of PSMind with the density of pharmacists per 10,000 inhabitants, as described by Faraco et al., (2020a), and with each municipality’s socioeconomic indexes, which were collected on public databases (2014 and 2015).
Scenario characterization
The structuring of the Brazil’s public healthcare system began in 1990, with the creation of SUS, defining access to comprehensive health care as a citizens’ right, and equity as a principal. The National Pharmaceutical Policy (2004) also determined actions to strengthen the pharmaceutical services capacity at local and national healthcare system levels.
SUS is organized in levels of complexity of care, and all the 5,560 municipalities are responsible for the organization and delivery of primary health care services, including essential medicines. Public healthcare is financed primarily through taxes and is shared among a tripartite alliance for public health care provision (i.e., the national, state, and municipal governments). Estimates indicate that SUS exclusively serves 114.6 million people. The expansion of SUS has allowed Brazil to respond quickly to the population’s changing health needs, with a dramatic increase in health service coverage over just three decades. Nevertheless, despite its successful operation, the analysis of future scenarios suggests an urgent need to address persistent geographic inequalities, insufficient funding, and improvement of its management capacity (Massuda et al., 2018).
SUS is the largest public healthcare system in the world and has over 44,000 public primary care centers, where the patients have access to health care and medicines (Álvares et al., 2017). According to Brazilian studies, there was a high prevalence of full access to medicines in the country in 2014: more than 47% of all medicines prescribed for chronic diseases were accessed through primary care centers.
Study Variables
The following variables were used in this study: “PS indicators” – PSMind and the Rate of Pharmacists per 10,000 inhabitants (RPI); and “socioeconomic indexes” – population size, gross domestic product (GDP), GDPper capita, Municipal Human Development Index (HDI-M) and the Unified Healthcare System Performance Index (IDSUS).
PS indicators
PSMind is a summary indicator of PS management capacity in PHC; i.e., it measures the municipality’s capacity to manage its PS policy for the access and rational use of medicines, guided by the National Pharmaceutical Policy (PNAF) premises. In the PSMind’s definition, “management” is understood as a technical, political and social process capable of producing results; and “management capacity” is defined by Guimarães et al. (2004) as “the ability of an organization to decide with autonomy, flexibility and transparency, mobilizing resources and building the sustainability of management results”. It comprises 30 indicators organized into three dimensions: operational, organizational, and sustainability. Each dimension is made up of indicators, which have a different nature (existence of knowledge, participation, autonomy, and satisfaction), since they measure different phenomena and, for this reason, also have a different definition weight over management capacity.
Table I presents a summary of the indicators that compose the PSMind.
The complete description of the method used to calculate the PSMind, as well as the measures and parameters that compose it, are presented in the manuscripts by Faraco et al., (2020b) and Faraco, Rover, Leite (2023).
RPI represents the density of the pharmaceutical workforce in PHC in Brazil, adopting as a parameter the measure described in the International Pharmaceutical Federation (FIP) global pharmaceutical workforce reports (FIP, 2012), where density is expressed as the number of pharmacists per 10,000 population (Faraco et al., 2020a). RPI is dichotomized in municipalities that have less than one pharmacist per 10,000 inhabitants and municipalities with one or more pharmacists per 10,000 inhabitants.
Socioeconomic indexes
Population size is often used to stratify Brazilian municipalities in studies on the healthcare field (Willemann et al., 2019). Municipalities were considered small when they presented populations smaller than 20,000 inhabitants (70.4% of Brazilian municipalities); medium size when between 20,000 and 50,000 inhabitants (24.5%); and, large, with a population larger than 100,000 inhabitants (5.1%), (IBGE, 2011). GDP is the sum of all final goods and services produced by a country, state or city, usually in one year.
GDP per capita is an indicator that helps determine the degree of development of a country, state or municipality, and consists of dividing the national income coefficient (gross national product minus capital depreciation expenses and indirect taxes) by its population (Rocha, 1998).
The Municipal human development index (HDI-M) is a compound indicator that takes into consideration the three human development pillars, namely: education (measured through indicators such as adult population schooling and young population school flow), longevity (life expectancy at birth), and municipal income per capita. The lower the HDI-M, the more degraded the areas (order of counties).
Although they measure the same phenomena, the indicators taken into account in the HDI-M are more adequate to assess the development of Brazilian municipalities and metropolitan regions. By synthesizing a complex reality into a single number, HDI-M and its three components make it possible to compare Brazilian municipalities over time.
IDSUS is a set of indicators proposed to monitor and assess the SUS performance in a contextualized manner to direct investments and contribute to increasing the quality and effectiveness of health services provided by the state (Forte, Nobre, 2014).
The index also seeks to assess the performance of SUS in relation to its principles and guidelines: regionalization, hierarchization, decentralization with a single command, and tripartite responsibility (Reis, Oliveira, Sellera, 2012).
IDSUS is a summary indicator composed of a set of 24 indicators that measure access to health services and the healthcare system's effectiveness. The data sources for the IDSUS indicators are from national information systems, with the participation of states and municipalities, and include several datasets on health indicators, although fragmented and without interaction (Reis, Oliveira, Sellera, 2012).
Considering that Brazilian socioeconomic characteristics affect the municipality assessment, the index considers homogeneous groups of municipalities grouped according to the demographic profile, population health condition, and healthcare system structure (Reis, Oliveira, Sellera, 2012), since Brazilian municipalities have different socioeconomic and structural conditions (Forte, Nobre, 2014; Reis, Oliveira, Sellera, 2012; Oliveira, Passador, 2016).
Data Analysis
Pearson’s chi-square test was applied to measure the relationship between the variables: PSMind, RPI, population size, GDP, GDP per capita, IDSUS, and HDI-M.
Total proportions were calculated by comparing the PSMind categories (critical situation, unsatisfactory situation, need for improvement and adequate situation) with the other indicators. SPSS software (IBM) version 25 was used, with the Complex Samples Plan (CSPLAN) command set. Sample commands and weights were applied to adjust the sampling design by clusters (described by Álvares et al., 2017).
To verify the existence of a linear association between the variables, Poisson regressions were performed using STATA software version 12 (StataCorp LP, College Station, Texas, USA), using the svy command set, suitable for analysis of complex samples, with a 5% significance level.
The research was approved by the National Commission of Ethics in Research (CONEP), through Opinion No. 398.131, dated Sep 16, 2013.
RESULTS
Table II characterizes the sample according to the results obtained for each of the analyzed indicators.
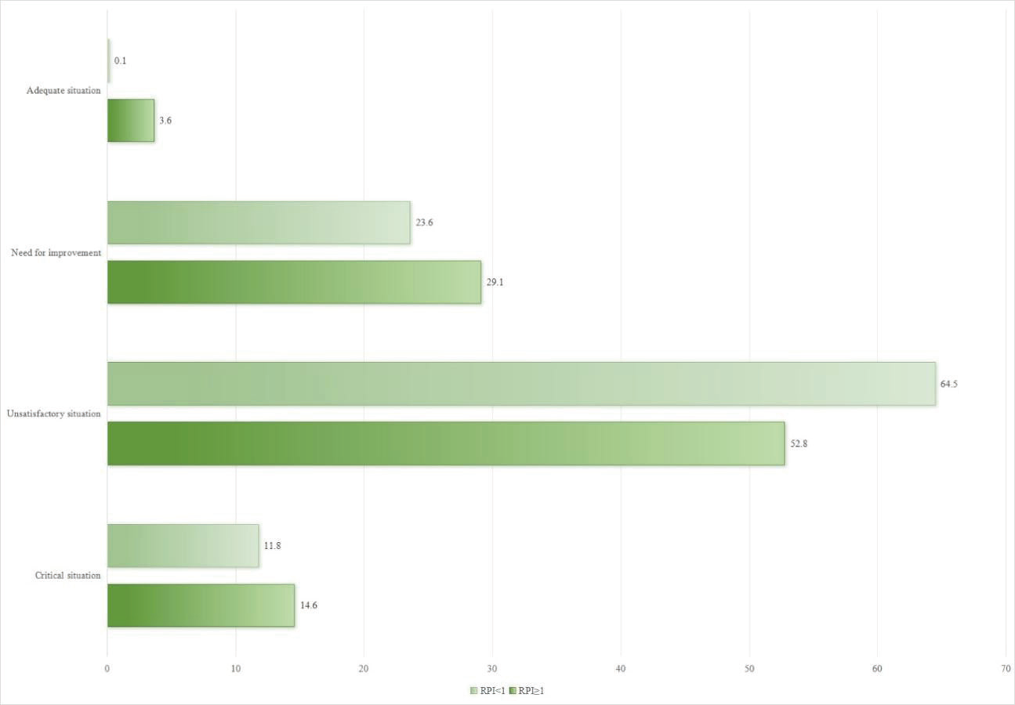
It is possible to observe that there is a statistically significant association between the manage capacity of PS (PSMind) and RPI (Figure 1).
Association between PSMind and RPI, Brazil (2015). Legend: p-value = 0.018; Chi-square test.
Among the municipalities that present RPI ≥ 1, it is observed that 14% (95%CI [10.5; 19.8]) are in a critical situation. On the other hand, municipalities with better management capacity conditions have RPI ≥ 1, indicating an association between PS management capacity and a higher density of pharmacists working in PHC in municipal healthcare services.
A significant association is also identified between the studied socioeconomic indexes (population size, GDP, GDP per capita, HDI-M and IDSUS) and PS management capacity, as shown in Table III.
Among the differences found in the comparison between population sizes, the highest proportion of municipalities in adequate situation was found in the size category above 100 thousand inhabitants (7.6% 95% CI [1.3; 33.6]). In critical situation, there is a higher prevalence of municipalities with a population of up to 25,000 inhabitants (15.7% CI95% [11.8; 20.5]).
In the association between PSMind and HDI-M, it was observed that the higher the HDI-M, the greater the proportion of municipalities with better management capacity (need for improvement and adequate situation) and the smaller the proportion of municipalities with PSMind in critical or unsatisfactory situation.
It is also observed that a greater proportion of municipalities and satisfactory health indicators (IDSUS) tend to have adequate PS management capacity. Group 4 stands out, which is composed of municipalities that have medium/high complexity of care (MAC) structure level and unsatisfactory economic and health indicators, with 12% of municipalities (95%CI [4.5; 28.4]) in critical situation in PSMind, and no municipality with capacity to manage PS in adequate situation.
Group 5, despite having low MAC structure level and medium socioeconomic and health conditions, presents 4% municipalities (95%CI [1.8; 9.1]) with the capacity to manage PS in adequate situation. Group 6, composed of municipalities with low health and socioeconomic condition levels, presents a higher proportion of municipalities in critical situation (18.7%, 95%CI [12.7; 26.6]).
As for the comparison between PSMind and income indicators (GDP and GDP per capita), a linear decrease in the proportion of municipalities in critical situation is observed as the range of the two indicators increases.
In the univariate Poisson regression analysis, no statistically significant differences were observed between PSMind and RPI. Nevertheless, in the practical scenario and considering the limitations of this study, this is a significant difference that deserves further analysis. Figure 2 illustrates the results of the univariate analyses of the Poisson regression model.
than that of the DEC group. In addition, the CCl4+DEC group also showed a reduction in GR levels (P>0.01).
The “High HDI-M” category had a higher prevalence (66.5%) of municipalities with PSMind in adequate situation or in need of improvement than the “Low HDI-M” category. The category high in relation to medium HDI-M has a higher prevalence (37.5%) in municipalities with an indicator of PS in adequate situation.
As for the comparison between PSMind and IDSUS, it is observed that Groups 5 and 6, formed by poorer municipalities and with less technologically dense health services (David, Shimizu, Silva, 2015), present a lower prevalence (56.6% and 71.5%, respectively) of PSMind in adequate situation when in comparison with the municipalities in Group 1. The municipalities in Groups 3 and 4 also demonstrate a lower prevalence (52.3% and 85.7%, respectively) of adequate PS management capacity when compared with the municipalities in Group 5.
It is also evident that municipalities with a higher GDP per capita had a lower prevalence of PSMind in good conditions when compared to lower income (up to $9100) municipalities. As for GDP, no differences were found in the association with PSMind.
The association of PSMind with the indicator referring to population size demonstrates that municipalities with 25,000 to 100,000 inhabitants have a 50% higher prevalence of having better conditions of PS management capacity when compared to larger municipalities (above 100,000 inhabitants).
Figure 3 presents the results of the multivariable Poisson Regression analyses, which reinforce the association of PSMind with HDI-M and IDSUS.
When the IDSUS regression is adjusted, it is observed that low HDI-M municipalities had a lower prevalence (69.4%) of PSMind in adequate conditions when in comparison with high HDI-M municipalities. Nevertheless, medium HDI-M municipalities reduce this prevalence to 38.7%. When adjusted by HDI-M, there is a lower prevalence (50.2%) of PS management capacity in good conditions in municipalities in Group 3 compared to Group 1. Likewise, municipalities in Groups respectively) of presenting PSMind in good condition 4 and 5 have a lower prevalence (72.4% and 49.4%, when compared with municipalities in Group 1.
DISCUSSION
The results regarding the capacity to manage services that guarantee access to medicines at the municipal level show the influence of the economic and social environment on the organization, operation, and sustainability of these services.
In the sample of municipalities studied here, there is at least one pharmacist hired by the municipalities to work in PHC in each municipality (Carvalho et al., 2017). However, the density of professionals in relation to the municipality’s population is linked to greater management capacity (in the univariate analyses). Studies have shown that the pharmacist’s role has statistically significant results in reducing the lack of medication, improving the quality of prescriptions, and reducing the number of medicines prescribed among patients undergoing pharmacotherapy follow-up in PHC health centers, in which they assume a relevant role in reducing health-related problems and improving the quality of services provided (Pereira et al., 2021). The higher density of pharmacists in municipal health services is also related to the higher proportion of patients who claim to receive information about their medicines and treatments (Faraco et al., 2020).
Nevertheless, hiring pharmacists, as an isolated factor, does not guarantee better PS management. Other aspects influence the management capacity of PS in PHC. The results obtained in the comparison between the PSMind and the socioeconomic indexes indicate that the municipalities with the worst socioeconomic indexes are also those with PSMind in a deficient situation.
The association between PSMind and IDSUS reinforces this indicator (PSMind), demonstrating that municipalities with better management capacity results are those with superior HDI-M, and also better healthcare system conditions and structures. Likewise, the comparison between PSMind and HDI-M demonstrates that the higher the HDI-M, the greater the proportion of municipalities with good PS management capacity, considering that these municipalities have the best socioeconomic indicators, reflecting a greater number of professionals, greater participation of popular social control, better health center structure and, thus, a better capacity to manage and use public resources.
Municipalities with higher GDP and GDP per capita have more resources needed for structuring services, which can positively impact the PS management capacity. The literature suggests, however, that there is no direct relationship between a country’s greater wealth and its population’s higher health level (Mendonça, Diercks, Kopittke, 2016). Above a certain threshold, increases in wealth do not translate into better health for the population (Barata, 2009), highlighting the strategic role of system and service management components (Mendonça, Diercks, Kopittke, 2016).
In Brazil, a study conducted with public and private sector managers emphasizes the weaknesses in management related to professional inexperience and delays in including new technologies that contribute to the processes of health work management and organization (Lorenzetti et al., 2014). In addition, working conditions are also associated with differences in the infrastructure of healthcare facilities that influence pharmacists’ ability to implement innovations and a broader scope of practice (Carvalho et al., 2017; Manzini et al., 2020; Leite et al., 2018).
Despite the various strategies to improve PHC financing and investment in training during the period in which the data for this study was collected (Manzini et al., 2020), it is known that Brazilian municipalities face an array of difficulties, especially minor ones, as they do not have enough own resources to finance expenses not covered by the federal government (Mendes, Leite, Carnut, 2020; David, Shimizu, Silva, 2015). Overall, the public healthcare service network is insufficient and there is difficulty in maintaining human resources in small municipalities (David, Shimizu, Silva, 2015). The extraordinary growth of healthcare training schools, particularly pharmacy schools, over the last decade has been unable to change this situation.
The findings of this study indicate that municipalities with a smaller population size and a lower HDI-M have less ability to manage PS, revealing worsening inequalities for citizens of municipalities with such characteristics, as well as difficulties in accessing healthcare and achieving expected living conditions due to economic issues and social weaknesses, as measured by the HDI-M (longevity, education and income), in addition to financial restraints that hinder access to essential medicines. Pharmaceutical policies are important tools to deal with socioeconomic inequalities, considering that issues related to the use of medicines generate health impacts, as well as social and economic ones, not only for the patient but also for society as a whole (Minaei et al., 2019). Considering that PS is part of the management of the municipal healthcare system (Costa et al., 2017) it could be used more effectively as a valuable tool to improve access to medicines and reduce inequities in opportunities for people to realize their full potential for development and well-being (Vogler, Österle, Mayer, 2015).
Vogler, Österle, Mayer (2015) defined that equitable access to and use of medicines should be determined by health care needs and no other potential factor. The authors argue that the policies and the literature related to this issue involve three major topics: measuring the extent of the inequalities, identifying the factors that determine inequalities, and addressing measures that help reduce existing inequalities.
In view of this, the implementation and management of services that guarantee access to medicines in municipalities require joint and articulated strategies between the healthcare system and political planning, pointing to the imperative need to direct efforts to better understand municipal strengths and weaknesses. Understanding and heeding to components that are more or less developed in the PS management of each municipality is fundamental for national public policies to be able to face persistent inequities, since the same health policy can be successful in certain contexts and not in others. As pointed out by Maceira, Brumana, Aleman (2022), the difference depends on how well some of the core components of the policies are implemented.
In view of the context and the strong association between socioeconomic indicators and the management capacity of PS, the recommendation is that national regulations should be reviewed regarding the distribution of federal resources to municipalities in order for the pharmaceutical workforce to remain and receive training, in addition to stimulating the development of socio-technical systems of municipal PS (including organizational culture, intersectoral collaboration, infrastructure, and social participation). In the search for better equity in access to medicines in primary care, these national initiatives should consider each municipality’s unique needs to guide and define public policies (Mendes, Peixoto, Leite, 2024).
In the last decade, some federal initiatives have been developed in this way. By the time these data were collected for the PNAUM, the QUALIFAR-SUS program was still in the process of being implemented and few municipalities had been included. Until 2022, 3508 municipalities had been included, receiving financial incentives to structure PS and promoting important advances (Mendes, Peixoto, Leite, 2024). At the same time, the Ministry of Health was offering postgraduate education in PS management for pharmacists. The course evaluation revealed positive impacts in PS (Manzini et al., 2020). Federal public funding for access to medicines and PS increased from some R$2 billion in 2003 to approximately R$15 billion in 2015. In 2019 the Ministry of Health included the HDI-M to determine financial funding related to essential medicines for the municipalities (Ministério da Saúde, 2019). However, the scenario in recent years has been of economic crisis and the process of SUS to acquire (lack of) financing, while financial funding for the procurement of essential medicines by the municipalities has decreased (considering the economic indexes), (Silva et al., 2024). Thus, new data is necessary to monitor the impact of such policies and the current socioeconomic situation of the municipalities. When new data is collected, it will be possible to compare the evolution of PS development and redetermine the impact of socio-economic conditions on PS development.
Some study limitations must be mentioned. The historical period of data collection by PNAUM (between 2014 and 2015) can be understood as a favorable political scenario for the expansion and improvement of health policies.
CONCLUSION
This study presents the results referring to the comparison between an indicator that measures the management capacity of pharmaceutical services for access to medicines in PHC in Brazil, along with municipal socioeconomic indicators. PSMind suggests that municipalities with better socioeconomic indicators, health service infrastructure, and density of pharmacists working in PHC have a superior capacity to guarantee access to medicines through public services.
The existence of an adequate minimum structure, a qualified workforce, service organization, and opportunities for political articulation are essential, as are conditions for these municipalities to develop and improve their management capacity, including adequate means of financing based on socioeconomic indicators to ensure effective access to and adequate use of medicines for the population.
REFERENCES
-
Álvares J, Alves MCGP, Escuder MML, Almeida AM, Izidoro JB, Junior AAG, et al. National Survey on Access, Use and Promotion of Rational Use of Medicines: methods. Rev Saúde Pública. 2017;51(suppl.2). doi: 10.11606/s1518-8787.2017051007027
» 10.11606/s1518-8787.2017051007027 -
Barata RB. Como e por que as desigualdades sociais fazem mal à saúde. Editora Fiocruz; 2009. https://www.arca.fiocruz.br/bitstream/handle/icict/23564/barata9788575413913.pdf?sequence=2&isAllowed=y
» https://www.arca.fiocruz.br/bitstream/handle/icict/23564/barata9788575413913.pdf?sequence=2&isAllowed=y -
Bernardo NLM, Soares L, Leite SN. A Sociotechnical Approach to Analyze Pharmaceutical Policy and Services Management in Primary Health Care in a Brazilian Municipality. Pharmacy. 2021;9(1):39. doi: 10.3390/pharmacy9010039
» 10.3390/pharmacy9010039 -
Carvalho MN, Álvares J, Costa KS, Junior AAG, Acurcio FA, Costa EA, et al. Workforce in the pharmaceutical services of the primary health care of SUS, Brazil. Rev Saúde Pública. 2017;51(2). doi: 10.11606/S15188787.2017051007110
» 10.11606/S15188787.2017051007110 -
Carvalho MN, Costa EMOD, Sakai MH, Gil CRR, Leite SN. Expansão e diversificação da força de trabalho de nível superior nas Unidades Básicas de Saúde no Brasil, 2008 -2013. Saúde Debate. 2016;40(109):154-162. doi: 10.1590/0103-1104201610912
» 10.1590/0103-1104201610912 -
Costa EA, Araújo PS, Penaforte TR, Barreto JL, Junior AAG, Acurcio FA, et al. Conceptions on pharmaceutical services in Brazilian primary health care. Rev Saúde Pública. 2017a;51. doi: 10.11606/s1518-8787.2017051007107
» 10.11606/s1518-8787.2017051007107 -
Costa KS, Tavares NUL, Nascimento Júnior JMD, Mengue SS, Álvares J, Junior AAG, et al. Pharmaceutical services in primary health care: interfederative agreement in the development of pharmaceutical policies in the Brazilian Unified Health System (SUS). Rev Saúde Pública. 2017b;51(suppl.2). doi: 10.11606/s1518-8787.201705100supl2ap
» 10.11606/s1518-8787.201705100supl2ap -
David GC, Shimizu HE, Silva EN. Primary Health Care in Brazilian municipalities: efficiency and disparities. Saúde Debate. 2015;39(SPE):232-245. doi: 10.5935/0103-1104.2015s005512
» 10.5935/0103-1104.2015s005512 -
European Commission, Secretariat-General. European Pillar of Social Rights. Publications Office; 2017. doi: 10.2792/95934
» 10.2792/95934 - Faraco E, Rover M, Leite S. Avaliação da capacidade de gestão da assistência farmacêutica na Atenção Primária à Saúde dos municípios brasileiros. Cad Saúde Coletiva. 2023. In press.
-
Faraco EB, Guimarães L, Anderson C, Leite SN. The pharmacy workforce in public primary healthcare centers: promoting access and information on medicines. Pharm Pract (Granada). 2020a;18(4). doi: 10.18549/pharmpract.2020.4.2048
» 10.18549/pharmpract.2020.4.2048 -
Faraco EB, Rover MM, Farias MR, Leite SN. Desenvolvimento de um protocolo de indicadores para avaliação nacional da capacidade de gestão da Assistência Farmacêutica na Atenção Primária àSaúde. Rev Adm Saúde. 2020b;20(78). doi: 10.23973/ras.78.204
» 10.23973/ras.78.204 -
FIP - Fédération Internationale Pharmaceutique. 2012 FIP Global Pharmacy - Workforce Report. 2012. https://www.fip.org/file/1414
» https://www.fip.org/file/1414 -
Forte LM, Nobre FC. Avaliação do Índice de Desempenho do SUS (IDSUS) nos Municípios do RN com Vistas à Definição de Estratégias de Gestão. Rev Gest Sist Saúde 2014;03(01):82-93. doi: 10.5585/rgss.v3i1.114
» 10.5585/rgss.v3i1.114 -
Gerlack LF, Karnikowski MGO, Areda CA, Galato D, Oliveira AG, Álvares J, et al. Gestão da assistência farmacêutica na atenção primária no Brasil. Rev Saúde Pública. 2017;51(2). doi: 10.11606/S15188787.2017051007063
» 10.11606/S15188787.2017051007063 -
Graley CE, May KF, McCoy DC. Postcode Lotteries in Public Health - The NHS Health Checks Programme in North West London. BMC Public Health. 2011;11(1). doi: 10.1186/1471-2458-11-738
» 10.1186/1471-2458-11-738 -
Guimarães MC, Santos SM, Melo C, Sanches Filho A. Evaluation of management capacity in social organizations: an in-process methodological proposal. Cad Saude Publica. 2004;20(6):1642-1650. doi: 10.1590/s0102-311x2004000600023
» 10.1590/s0102-311x2004000600023 -
IBGE -Instituto Brasileiro de Geografia e Estatística. Indicadores Sociais Municipais: Uma Análise Dos Resultados Do Universo Do Censo Demográfico 2010. 2011. https://biblioteca.ibge.gov.br/bibliotecacatalogo?id=254598&view=detalhes
» https://biblioteca.ibge.gov.br/bibliotecacatalogo?id=254598&view=detalhes - Leite SN, Farias MR, Manzini F, Mendes SJ, Rover MRM, eds. Gestão Da Assistência Farmacêutica: Proposta Para Avaliação No Contexto Municipal: A Experiência Em Santa Catarina 2015. Editora da UFSC; 2015:170.
-
Leite SN, Manzini F, Adelir V, Lima MEO, Pereira MA, Araujo SQ, et al. Ciência, Tecnologia e Assistência Farmacêutica em pauta: contribuições da sociedade para a 16a Conferência Nacional de Saúde. Cien Saude Colet. 2018;23(12):4259-4268. doi: 10.1590/1413812320182312.29962018
» 10.1590/1413812320182312.29962018 -
Lorenzetti J, Lanzoni GMDM, Ferreira L, Pires DEP, Ramos FRS. Health management in Brazil: dialogue with public and private managers. Texto e Contexto – Enferm. 2014;23(2):417-442. doi: 10.1590/010407072014000290013
» 10.1590/010407072014000290013 -
Maceira D, Brumana L, Aleman JG. Reducing the equity gap in child health care and health system reforms in Latin America. Int J Equity Health. 2022;21(1). doi: 10.1186/s12939-021-01617-w
» 10.1186/s12939-021-01617-w -
Manzini F, Diehl EE, Farias MR, Santos RI, Soares L, Rech Norberto, et al. Analysis of a Blended, In-Service, Continuing Education Course in a Public Health System: Lessons for Education Providers and Healthcare Managers. Front Public Health. 2020;8. doi: 10.3389/fpubh.2020.561238
» 10.3389/fpubh.2020.561238 -
Massuda A, Hone T, Leles FAG, Castro MC, Atun R. The Brazilian health system at crossroads: progress, crisis and resilience. BMJ Global Health. 2018;3(4). doi: 10.1136/bmjgh-2018-000829
» 10.1136/bmjgh-2018-000829 -
Mendes Á, Leite MG, Carnut L. A methodology for apportioning federal SUS resources: the health needs index. Rev Saude Publica. 2020;54(77). doi: 10.11606/s1518-8787.2020054001661
» 10.11606/s1518-8787.2020054001661 - Mendes J, Peixoto R, Leite SN. Fatores sociais e técnicos relacionados ao desenvolvimento da gestão municipal da Assistência Farmacêutica: resultados do QUALIFICA_AF. Rev Saude Debate. 2024. In press.
-
Mendonça CS, Diercks MS, Kopittke L. Strengthening Primary Health Care in the municipalities in the Metropolitan Region of Porto Alegre, Brazil, after the introduction of the Mais Médicos (More Doctors) Program: an inter-municipal comparison. Cien Saude Colet. 2016;21(9):2871-2878. doi: https://doi.org/10.1590/141381232015219.16622016
» https://doi.org/10.1590/141381232015219.16622016 -
Minaei H, Peikanpour M, Yousefi N, Peymani P, Peiravian F, Shobeiri N, et al. Country Pharmaceutical Situation on Access, Quality, and Rational Use of Medicines: An Evidence from a middle-income country. Iran J Pharm Res. 2019;18(4):2191-2203. doi: 10.22037/ijpr.2019.111636.13273
» 10.22037/ijpr.2019.111636.13273 -
Ministério da Saúde (Brasil). Ordinance no. 2077, of September 17, 2012. Establishes the National Survey on Access, Use and Promotion of Rational Use of Medicines in Brazil (PNAUM). https://bvsms.saude. gov.br/bvs/saudelegis/gm/2012/prt2077_17_09_2012
» https://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/prt2077_17_09_2012 -
Ministério da Saúde (Brasil). Ordinance no. 3193, of December 9, 2019. Amends Consolidation Ordinance No. 6/GM/MS, of September 28, 2017, to provide for the financing of the Basic Component of Pharmaceutical Assistance within the scope of the Unified Health System (SUS). https://bvsms.saude.gov.br/bvs/saudelegis/gm/2019/prt3193_10_12_2019.html
» https://bvsms.saude.gov.br/bvs/saudelegis/gm/2019/prt3193_10_12_2019.html -
Oliveira LR, Passador CS. The Brazilian Unified National Health System: Proposal of a Cost-effectiveness Evaluation Model. BAR - Braz Admin Review. 2016;13(2). doi: 10.1590/1807-7692bar2016140120
» 10.1590/1807-7692bar2016140120 -
Pereira NC, Luiza VL, Campos MR, Chaves LA. Implementation of pharmaceutical services in Brazilian primary health care: a cross-sectional study. BMC Fam Pract. 2021;22(1). doi: 10.1186/s12875-021-01516-7
» 10.1186/s12875-021-01516-7 -
Reis AT, Oliveira PTR, SelleraPE. Sistema de Avaliação para a Qualificação do Sistema Único de Saúde (SUS). Rev Eletron Comun Inf Inov Saúde. 2012;6(2). doi: 10.3395/reciis.v6i2.543
» 10.3395/reciis.v6i2.543 -
Rocha S. Renda E Pobreza - Medidas per Capita versus Adulto-Equivalente; 1998. https://repositorio.ipea.gov.br/bitstream/11058/2487/1/td_0609.pdf
» https://repositorio.ipea.gov.br/bitstream/11058/2487/1/td_0609.pdf -
Rocha WH, Teodoro JÁ, Acurcio FA, Junior AAG, Moura ICG, Godman Brian, et al. Influence of pharmaceutical services organization on the availability of essential medicines in a public health system. J Comp Eff Res. 2021;10(6):519-532. doi: 10.2217/cer2020-0259
» 10.2217/cer2020-0259 -
Rover MR, Vargas-Pelaez CM, Farias MR, Leite SN. Acceso a medicamentos de alto precio en Brasil: la perspectiva de médicos, farmacéuticos y usuarios. Gac Sanit. 2016;30(2):110-116. doi: 10.1016/j.gaceta.2015.12.005
» 10.1016/j.gaceta.2015.12.005 -
Vogler S, Österle A, Mayer S. Inequalities in medicine use in Central Eastern Europe: an empirical investigation of socioeconomic determinants in eight countries. Int J Equity Health. 2015;14(1). doi: 10.1186/s12939-0150261-0
» 10.1186/s12939-0150261-0 -
WHO - World Health Organization Expert Committee on the Selection and Use of Essential Medicines (12th:2002:Geneva, Switzerland), World Health Organization. The Selection and Use of Essential Medicines : Report of the WHO Expert Committee, 2002 : (Including the 12th Model List of Essential Medicines). World Health Organization; 2003. https://apps.who.int/iris/handle/10665/42620
» https://apps.who.int/iris/handle/10665/42620 -
WHO - World Health Organization. Roadmap for access to medicines, vaccines and health product 20192023: comprehensive support for access to medicines, vaccines and other health products. World Health Organization. Published 2019. https://apps.who.int/iris/handle/10665/330145
» https://apps.who.int/iris/handle/10665/330145 -
Willemann MCA, Medeiros JM de, Lacerda JT, Calvo MCM. Atualização intercensitária de estratificação de municípios brasileiros para avaliação de desempenho em saúde, 2015. Epidemiol Serv Saúde. 2019;28(3). doi: 10.5123/s1679-49742019000300004
» 10.5123/s1679-49742019000300004 -
Wirtz VJ, Hogerzeil HV, Gray AL, Bigdeli M, Joncheere CP, Ewen MA, et al. Essential medicines for universal health coverage. Lancet. 2017;389(10067):403-476. doi: 10.1016/s0140-6736(16)31599-9
» 10.1016/s0140-6736(16)31599-9
Edited by
-
Associated Editor:
Inajara Rotta
Publication Dates
-
Publication in this collection
08 Dec 2025 -
Date of issue
2025
History
-
Received
15 May 2025 -
Accepted
27 Sept 2025

 Pharmaceutical services management capacity and the municipal socioeconomic scenario: persistent inequalities
Pharmaceutical services management capacity and the municipal socioeconomic scenario: persistent inequalities