Abstract
Optical coherence tomography (OCT) has generally been used as a nondestructive technique to evaluate integrities of composite restorations. We investigated marginal and internal adaptations of ceramic inlay restorations with OCT and compared them to results with the silicone replica technique. Round-shaped class I cavities were prepared on 16 human maxillary first premolar teeth. Ceramic inlays were fabricated. Silicone replicas from inlays were obtained and sectioned to measure marginal and internal adaptations with a stereomicroscope (Leica Dfc 295, Bensheim, Germany). Inlays were cemented on respective teeth. Marginal and internal adaptations were then measured with the OCT system (Thorlabs, New Jersey, USA) in 200- μm intervals. Replica and OCT measurements were compared with independent samples t-tests. A paired t-test was used to evaluate the marginal and internal adaptations of each group (p < 0.05). Marginal and internal adaptations were 100.97 ± 31.36 and 113.94 ± 39.75 μm, respectively, using the replica technique and 28.97 ± 17.86 and 97.87 ± 21.83 μm, respectively, using OCT. The differences between the techniques were significant (p = 0.00 and p = 0.01, respectively). On evaluation within the groups, internal adaptation values were found to be significantly higher than the marginal adaptation values for the replica technique (p = 0.00) and OCT (p = 0.00). Therefore, the replica and OCT techniques showed different results, with higher values of marginal and internal adaptation found with the replica technique. Marginal and internal adaptation values of ceramic inlays, whether measured by replica or OCT techniques, were within clinically acceptable limits.
Inlays; Replica Techniques; Tomography, Optical Coherence
Introduction
All-ceramic materials have been used to restore teeth with highly esthetic demands and to achieve wear-resistant restorations, especially in posterior regions.11. Santos MJ, Freitas MC, Azevedo LM, Santos GC Jr, Navarro MF, Francischone CE et al. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: 12-year follow-up. Clin Oral Investig. 2016 Sep;20(7):1683-90. https://doi.org/10.1007/s00784-015-1669-z
https://doi.org/10.1007/s00784-015-1669-...
They have been approved for the treatment of inlay cavities, achieving a high survival rate and good esthetic result.22. Holberg C, Winterhalder P, Wichelhaus A, Hickel R, Huth K. Fracture risk of lithium-disilicate ceramic inlays: a finite element analysis. Dent Mater. 2013 Dec;29(12):1244-50. https://doi.org/10.1016/j.dental.2013.09.012
https://doi.org/10.1016/j.dental.2013.09...
,33. Krämer N, Taschner M, Lohbauer U, Petschelt A, Frankenberger R. Totally bonded ceramic inlays and onlays after eight years. J Adhes Dent. 2008 Aug;10(4):307-14.,44. Frankenberger R, Taschner M, Garcia-Godoy F, Petschelt A, Krämer N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent. 2008 Oct;10(5):393-8. Ceramic inlays are advantageous, allowing for improved marginal adaptation. This is achieved due to the similarity of thermal expansion between the ceramic material and the tooth substance and the small amount of shrinkage occurring through the polymerization of the composite luting cement.55. Uludag B, Yucedag E, Sahin V. Microleakage of inlay ceramic systems luted with self-adhesive resin cements. J Adhes Dent. 2014 Dec;16(6):523-9.,66. Bott B, Hannig M. Effect of different luting materials on the marginal adaptation of Class I ceramic inlay restorations in vitro. Dent Mater. 2003 Jun;19(4):264-9. https://doi.org/10.1016/S0109-5641(02)00038-6
https://doi.org/10.1016/S0109-5641(02)00...
,77. Uludag B, Ozturk O, Ozturk AN. Microleakage of ceramic inlays luted with different resin cements and dentin adhesives. J Prosthet Dent. 2009 Oct;102(4):235-41. https://doi.org/10.1016/S0022-3913(09)60161-X
https://doi.org/10.1016/S0022-3913(09)60...
Besides these advantages, marginal discoloration, postoperative sensitivity, and recurrent caries remain problems associated with adaptation properties of ceramic inlay restorations.55. Uludag B, Yucedag E, Sahin V. Microleakage of inlay ceramic systems luted with self-adhesive resin cements. J Adhes Dent. 2014 Dec;16(6):523-9. Currently, lithium disilicate glass ceramics have been used for inlay restorations, either processed with heat-pressed or computer-aided design–computer-aided manufacturing techniques.88. Trindade FZ, Valandro LF, Jager N, Bottino MA, Kleverlaan CJ. Elastic properties of lithium disilicate versus feldspathic inlays: effect on the bonding by 3D finite element analysis. J Prosthodont. 2016 Oct. https://doi.org/10.1111/jopr.12550
https://doi.org/10.1111/jopr.12550...
Regardless of the fabrication technique, marginal and internal adaptations are important factors that determine the longevity of restorations. Marginal adaptation has a substantial impact on longevity, since it prevents secondary caries and microleakage99. Uzgur R, Ercan E, Uzgur Z, Çolak H, Yalçın M, Özcan M. Cement thickness of inlay restorations made of lithium disilicate, polymer-infiltrated ceramic and nano-ceramic CAD/CAM materials evaluated using 3D X-ray micro-computed tomography. J Prosthodont. 2016 Aug. https://doi.org/10.1111/jopr.12521
https://doi.org/10.1111/jopr.12521...
On the other hand, internal adaptation, filled with a uniform luting cement layer, plays a crucial role in the durability of the restorations. Poorly adapted restorations cause a greater problem for posterior teeth, since the primary support is the weaker cement rather than the stronger tooth structure.1010. Alajaji NK, Bardwell D, Finkelman M, Ali A. Micro-CT evaluation of ceramic inlays: comparison of the marginal and internal fit of five and three axis CAM systems with a heat press technique. J Esthet Restor Dent. 2017 Feb;29(1):49-58. https://doi.org/10.1111/jerd.12271
https://doi.org/10.1111/jerd.12271...
Marginal and internal adaptations of ceramic inlay restorations have been evaluated by many studies using destructive techniques, such as sectioning samples into slices and then measuring with a stereomicroscope,1111. Keshvad A, Hooshmand T, Asefzadeh F, Khalilinejad F, Alihemmati M, Van Noort R. Marginal gap, internal fit, and fracture load of leucite-reinforced ceramic inlays fabricated by CEREC inLab and hot-pressed techniques. J Prosthodont. 2011 Oct;20(7):535-40. https://doi.org/10.1111/j.1532-849X.2011.00745.x PMID:21806704
https://doi.org/10.1111/j.1532-849X.2011...
,1212. Thordrup M, Isidor F, Hörsted-Bindslev P. Comparison of marginal fit and microleakage of ceramic and composite inlays: an in vitro study. J Dent. 1994 Jun;22(3):147-53. https://doi.org/10.1016/0300-5712(94)90198-8PMID:8027457
https://doi.org/10.1016/0300-5712(94)901...
,1313. Audenino G, Bresciano ME, Bassi F, Carossa S. In vitro evaluation of fit of adhesively luted ceramic inlays. Int J Prosthodont. 1999 Jul-Aug;12(4):342-7. PMID:10635204 and nondestructive techniques, such as silicone replica with stereomicroscopy,1414. Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005 Jun;32(6):448-53. https://doi.org/10.1111/j.1365-2842.2005.01443.x
https://doi.org/10.1111/j.1365-2842.2005...
,1515. Molin M, Karlsson S. The fit of gold inlays and three ceramic inlay systems. A clinical and in vitro study. Acta Odontol Scand. 1993 Aug;51(4):201-6. https://doi.org/10.3109/00016359309040568
https://doi.org/10.3109/0001635930904056...
resin replica with scanning electron microscopy (SEM),1616. Ender A, Bienz S, Mörmann W, Mehl A, Attin T, Stawarczyk B. Marginal adaptation, fracture load and macroscopic failure mode of adhesively luted PMMA-based CAD/CAM inlays. Dent Mater. 2016 Feb;32(2):e22-9. https://doi.org/10.1016/j.dental.2015.11.009
https://doi.org/10.1016/j.dental.2015.11...
and micro-computed tomography (CT).99. Uzgur R, Ercan E, Uzgur Z, Çolak H, Yalçın M, Özcan M. Cement thickness of inlay restorations made of lithium disilicate, polymer-infiltrated ceramic and nano-ceramic CAD/CAM materials evaluated using 3D X-ray micro-computed tomography. J Prosthodont. 2016 Aug. https://doi.org/10.1111/jopr.12521
https://doi.org/10.1111/jopr.12521...
,1010. Alajaji NK, Bardwell D, Finkelman M, Ali A. Micro-CT evaluation of ceramic inlays: comparison of the marginal and internal fit of five and three axis CAM systems with a heat press technique. J Esthet Restor Dent. 2017 Feb;29(1):49-58. https://doi.org/10.1111/jerd.12271
https://doi.org/10.1111/jerd.12271...
Currently, nondestructive measurement techniques for evaluating adaptations of restorations are becoming increasingly common.99. Uzgur R, Ercan E, Uzgur Z, Çolak H, Yalçın M, Özcan M. Cement thickness of inlay restorations made of lithium disilicate, polymer-infiltrated ceramic and nano-ceramic CAD/CAM materials evaluated using 3D X-ray micro-computed tomography. J Prosthodont. 2016 Aug. https://doi.org/10.1111/jopr.12521
https://doi.org/10.1111/jopr.12521...
,1010. Alajaji NK, Bardwell D, Finkelman M, Ali A. Micro-CT evaluation of ceramic inlays: comparison of the marginal and internal fit of five and three axis CAM systems with a heat press technique. J Esthet Restor Dent. 2017 Feb;29(1):49-58. https://doi.org/10.1111/jerd.12271
https://doi.org/10.1111/jerd.12271...
,1616. Ender A, Bienz S, Mörmann W, Mehl A, Attin T, Stawarczyk B. Marginal adaptation, fracture load and macroscopic failure mode of adhesively luted PMMA-based CAD/CAM inlays. Dent Mater. 2016 Feb;32(2):e22-9. https://doi.org/10.1016/j.dental.2015.11.009
https://doi.org/10.1016/j.dental.2015.11...
,1717. Han SH, Sadr A, Tagami J, Park SH. Non-destructive evaluation of an internal adaptation of resin composite restoration with swept-source optical coherence tomography and micro-CT. Dent Mater. 2016 Jan;32(1):e1-7. https://doi.org/10.1016/j.dental.2015.10.009
https://doi.org/10.1016/j.dental.2015.10...
,1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
Among nondestructive techniques, the replica technique has been used as a reliable and valid noninvasive method to determine the adaptation of crowns or veneers to the tooth structure in in vivo and in vitro studies.1414. Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005 Jun;32(6):448-53. https://doi.org/10.1111/j.1365-2842.2005.01443.x
https://doi.org/10.1111/j.1365-2842.2005...
,1515. Molin M, Karlsson S. The fit of gold inlays and three ceramic inlay systems. A clinical and in vitro study. Acta Odontol Scand. 1993 Aug;51(4):201-6. https://doi.org/10.3109/00016359309040568
https://doi.org/10.3109/0001635930904056...
,1919. McLean JW, Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971 Aug;131(3):107-11. https://doi.org/10.1038/sj.bdj.4802708
https://doi.org/10.1038/sj.bdj.4802708...
,2020. Falk A, Steyern PV, Fransson H, Thorén MM. Reliability of the impression replica technique. Int J Prosthodont. 2015 Mar-Apr;28(2):179-80. https://doi.org/10.11607/ijp.4132
https://doi.org/10.11607/ijp.4132...
,2121. Gemalmaz D, Kükrer D. In vivo and in vitro evaluation of marginal fit of class II ceromer inlays. J Oral Rehabil. 2006 Jun;33(6):436-42. https://doi.org/10.1111/j.1365-2842.2005.01562.x
https://doi.org/10.1111/j.1365-2842.2005...
,2222. Quante K, Ludwig K, Kern M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent Mater. 2008 Oct;24(10):1311-5. https://doi.org/10.1016/j.dental.2008.02.011PMID:18384869
https://doi.org/10.1016/j.dental.2008.02...
,2323. Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns—validation of the silicone replica method. J Oral Rehabil. 2008 Feb;35(2):116-22. https://doi.org/10.1111/j.1365-2842.2003.01203.x
https://doi.org/10.1111/j.1365-2842.2003...
,2424. Kim KB, Kim JH, Kim WC, Kim HY, Kim JH. Evaluation of the marginal and internal gap of metal-ceramic crown fabricated with a selective laser sintering technology: two- and three-dimensional replica techniques. J Adv Prosthodont. 2013 May;5(2):179-86. https://doi.org/10.4047/jap.2013.5.2.179
https://doi.org/10.4047/jap.2013.5.2.179...
,2525. Park JY, Bae SY, Lee JJ, Kim JH, Kim HY, Kim WC. Evaluation of the marginal and internal gaps of three different dental prostheses: comparison of the silicone replica technique and three-dimensional superimposition analysis. J Adv Prosthodont. 2017 Jun;9(3):159-69. https://doi.org/10.4047/jap.2017.9.3.159
https://doi.org/10.4047/jap.2017.9.3.159...
,2626. Guess PC, Vagkopoulou T, Zhang Y, Wolkewitz M, Strub JR. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014 Feb;42(2):199-209. https://doi.org/10.1016/j.jdent.2013.10.002
https://doi.org/10.1016/j.jdent.2013.10....
Another nondestructive technique, optical coherence tomography (OCT), has been used to evaluate marginal or internal fit of restorations.1717. Han SH, Sadr A, Tagami J, Park SH. Non-destructive evaluation of an internal adaptation of resin composite restoration with swept-source optical coherence tomography and micro-CT. Dent Mater. 2016 Jan;32(1):e1-7. https://doi.org/10.1016/j.dental.2015.10.009
https://doi.org/10.1016/j.dental.2015.10...
,1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
OCT provides high-resolution cross-sectional images based on the principle of the optical interferometer, which uses a near infrared reflected light that passes well through biological structures and materials.2727. Turkistani A, Sadr A, Shimada Y, Nikaido T, Sumi Y, Tagami J. Sealing performance of resin cements before and after thermal cycling: evaluation by optical coherence tomography. Dent Mater. 2014 Sep;30(9):993-1004. https://doi.org/10.1016/j.dental.2014.05.010
https://doi.org/10.1016/j.dental.2014.05...
,2828. Lenton P, Rudney J, Chen R, Fok A, Aparicio C, Jones RS. Imaging in vivo secondary caries and ex vivo dental biofilms using cross-polarization optical coherence tomography. Dent Mater. 2012 Jul;28(7):792-800. https://doi.org/10.1016/j.dental.2012.04.004
https://doi.org/10.1016/j.dental.2012.04...
,2929. Minamino T, Mine A, Omiya K, Matsumoto M, Nakatani H, Iwashita T et al. Nondestructive observation of teeth post core space using optical coherence tomography: a pilot study. J Biomed Opt. 2014 Apr;19(4):046004. https://doi.org/10.1117/1.JBO.19.4.046004
https://doi.org/10.1117/1.JBO.19.4.04600...
,3030. Kim SH, Kang SR, Park HJ, Kim JM, Yi WJ, Kim TI. Improved accuracy in periodontal pocket depth measurement using optical coherence tomography. J Periodontal Implant Sci. 2017 Feb;47(1):13-9. https://doi.org/10.5051/jpis.2017.47.1.13
https://doi.org/10.5051/jpis.2017.47.1.1...
,3131. Matheus TC, Kauffman CM, Braz AK, Mota CC, Gomes AS. Fracture process characterization of fiber-reinforced dental composites evaluated by optical coherence tomography, SEM and optical microscopy. Braz Dent J. 2010;21(5):420-7. https://doi.org/10.1590/S0103-64402010000500008
https://doi.org/10.1590/S0103-6440201000...
,3232. Lin CL, Kuo WC, Chang YH, Yu JJ, Lin YC. Examination of ceramic/enamel interfacial debonding using acoustic emission and optical coherence tomography. Dent Mater. 2014 Aug;30(8):910-6. https://doi.org/10.1016/j.dental.2014.05.023
https://doi.org/10.1016/j.dental.2014.05...
OCT can provide structure details and has been confirmed as a proven technique in a clinical setting.3030. Kim SH, Kang SR, Park HJ, Kim JM, Yi WJ, Kim TI. Improved accuracy in periodontal pocket depth measurement using optical coherence tomography. J Periodontal Implant Sci. 2017 Feb;47(1):13-9. https://doi.org/10.5051/jpis.2017.47.1.13
https://doi.org/10.5051/jpis.2017.47.1.1...
In dentistry, OCT has been mostly used to evaluate sealing performances of composite, amalgam restorations or adhesives.1717. Han SH, Sadr A, Tagami J, Park SH. Non-destructive evaluation of an internal adaptation of resin composite restoration with swept-source optical coherence tomography and micro-CT. Dent Mater. 2016 Jan;32(1):e1-7. https://doi.org/10.1016/j.dental.2015.10.009
https://doi.org/10.1016/j.dental.2015.10...
,1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
,2727. Turkistani A, Sadr A, Shimada Y, Nikaido T, Sumi Y, Tagami J. Sealing performance of resin cements before and after thermal cycling: evaluation by optical coherence tomography. Dent Mater. 2014 Sep;30(9):993-1004. https://doi.org/10.1016/j.dental.2014.05.010
https://doi.org/10.1016/j.dental.2014.05...
28. Lenton P, Rudney J, Chen R, Fok A, Aparicio C, Jones RS. Imaging in vivo secondary caries and ex vivo dental biofilms using cross-polarization optical coherence tomography. Dent Mater. 2012 Jul;28(7):792-800. https://doi.org/10.1016/j.dental.2012.04.004
https://doi.org/10.1016/j.dental.2012.04...
-2929. Minamino T, Mine A, Omiya K, Matsumoto M, Nakatani H, Iwashita T et al. Nondestructive observation of teeth post core space using optical coherence tomography: a pilot study. J Biomed Opt. 2014 Apr;19(4):046004. https://doi.org/10.1117/1.JBO.19.4.046004
https://doi.org/10.1117/1.JBO.19.4.04600...
,3333. Bakhsh TA, Sadr A, Shimada Y, Mandurah MM, Hariri I, Alsayed EZ et al. Concurrent evaluation of composite internal adaptation and bond strength in a class-I cavity. J Dent. 2013 Jan;41(1):60-70. https://doi.org/10.1016/j.jdent.2012.10.003
https://doi.org/10.1016/j.jdent.2012.10....
,3434. Melo LS, Araujo RE, Freitas AZ, Zezell D, Vieira ND, Girkin J et al. Evaluation of enamel dental restoration interface by optical coherence tomography. J Biomed Opt. 2005 Nov-Dec;10(6):064027. https://doi.org/10.1117/1.2141617
https://doi.org/10.1117/1.2141617...
,3535. Makishi P, Shimada Y, Sadr A, Tagami J, Sumi Y. Non-destructive 3D imaging of composite restorations using optical coherence tomography: marginal adaptation of self-etch adhesives. J Dent. 2011 Apr;39(4):316-25. https://doi.org/10.1016/j.jdent.2011.01.011
https://doi.org/10.1016/j.jdent.2011.01....
,3636. Monteiro GQ, Montes MA, Gomes AS, Mota CC, Campello SL, Freitas AZ. Marginal analysis of resin composite restorative systems using optical coherence tomography. Dent Mater. 2011 Dec;27(12):e213-23. https://doi.org/10.1016/j.dental.2011.08.400
https://doi.org/10.1016/j.dental.2011.08...
,3737. Braz AK, Kyotoku BB, Braz R, Gomes AS. Evaluation of crack propagation in dental composites by optical coherence tomography. Dent Mater. 2009 Jan;25(1):74-9. https://doi.org/10.1016/j.dental.2008.04.011
https://doi.org/10.1016/j.dental.2008.04...
,3838. Sinescu C, Negrutiu ML, Todea C, Balabuc C, Filip L, Rominu R et al. Quality assessment of dental treatments using en-face optical coherence tomography. J Biomed Opt. 2008 Sep-Oct;13(5):054065. https://doi.org/10.1117/1.2992593
https://doi.org/10.1117/1.2992593...
However, according to our knowledge, few studies exist in the literature related to the investigation of the adaptation of ceramic restorations to tooth structures using OCT. We quantitatively evaluated the marginal and internal adaptations of ceramic inlay restorations using OCT and compared the results with those of the silicone replica technique. Thus, the objectives of the study were to compare the OCT and replica techniques to assess marginal and internal fit and to investigate the marginal and internal adaptation of ceramic inlays. The hypotheses of the study were as follows: (1) there were no significant differences between the adaptation values of the OCT and replica technique, and (2) marginal and internal adaptation of ceramic inlays had similar values.
Methodology
For the study, we selected 16 extracted human maxillary first premolar teeth free of caries, cracks, and restorations. The number of inlays for each group was determined by a power calculation as 16 to detect a difference of 20 μm with a power of 80% and an error probability of 0.05. The same 16 teeth and inlays were analyzed via the replica and OCT techniques (n = 16 per technique). Ethical approval was obtained from the Research Ethics Committee of Ege University Medical Faculty (14-12.1/12). The teeth were stored in a saline solution for 30 days. Roots were embedded in plastic cylinders 3 mm away from the cervical lines using a self-curing acrylic resin. The orientations of the teeth long axes were obtained perpendicular to the surface of the plastic cylinders using a parallelometer (Degussa F1; DeguDent, Hanau, Germany). Tubercles were removed by trimming to obtain a flat occlusal surface. Round class I occlusal cavities were prepared with a 6° axial taper and a 1.5-mm occlusal depth by one operator using the inlay cavity preparation bur (#959KR.018, Lot: 494511; Komet, Lemgo, Germany) with a high-speed air turbine under water cooling. Cavity dimensions were approximately 3 mm buccolingually and mesiodistally (Figure 1). Internal angles were rounded and enamel margins that remained at the occlusal surfaces were not beveled. Impressions were made using a polyvinyl siloxane impression material (Affinis Precious; Coltane, Whaledent, Switzerland) with customized stock trays after the cavities were rinsed and air-dried. The teeth were then kept in water at room temperature.
A representative view of cavity dimensions of round shaped Class I cavity: a = 1.5 mm occlusal dept, r = radius of the cavity.
Stone casts were prepared using Type IV dental die stone (GC Fujirock EP; GC Europe, Leuven, Belgium) according to the manufacturer’s instructions. One working cast and one master cast were acquired for each inlay. Cavity surfaces were lined with a die spacer (Rem-e-die; Ivoclar Vivadent, Schaan, Liechtenstein; approximately 10 μm) at 0.5 mm from the marginal areas. A full-contour inlay wax up was made for each stone die. Wax patterns were invested in a phosphate-bonded investment material (IPS Press Vest Speed; Ivoclar Vivadent). The pressing process was performed according to the manufacturer’s instructions using a pressable lithium disilicate glass-ceramic (IPS e.max Press; Ivoclar Vivadent) in a press furnace EP 600 (Ivoclar Vivadent) at 915°C. The inlays were devested and cleaned. The devested inlays were glazed with IPS e.max Ceram Glaze Liquid (Ivoclar Vivadent) in a Programat P200 furnace (Ivoclar Vivadent) at 770°C. All 16 inlay restorations fabricated were fitted on their respective master dies. Minimal adjustments on the internal surfaces were performed using a blunt diamond bur with low speed after marking with a silicone-disclosing medium (Fit Checker, GC Europe). Internal surfaces were sandblasted (50 μm alumina, 2 bar, 5 s). One expert dental technician fabricated the inlays.
Replica measurements
The inlays were inspected on their corresponding teeth. Each inlay cavity was filled with a light-body silicone (Elite HD Light Body Fast Setting; Zhermack, Rovigo, Italy) using the manufacturer’s dispenser. Then, the inlays were placed on the respective teeth with a constant load of 50 N using a universal testing machine (Shimadzu Corporation, Tokyo, Japan). After the light-body silicone material set, the inlays with silicone films (replicas) were removed from the teeth. The replicas were stabilized with a heavy-body silicone material (Elite HD, Zhermack) using the manufacturer’s dispenser. The inlays were removed from the silicones after the heavy-body silicone had set. The replicas with heavy-body silicone were cut into four equal segments with a razor blade buccolingually and mesiodistally. A light optical microscope (Leica Dfc 295; Leica Microsystems, Bensheim, Germany) at a 40x magnification and the software (Leica Application Suite; Leica Microsystems) were used to measure the adaptation values. Marginal adaptations were measured at six points (Figure 2). Internal adaptations were measured at three points from axial walls and three points from the pulpal floor of the replicas (Figure 3). Perpendicular distances from the inlays to the teeth were used. A total of 72 points were measured per replica. Equidistant points to each other, dividing the measurement area into approximately equal segments, were used to standardize measurements among all specimens. Each measurement was repeated three times and the mean values were used. One investigator performed the measurements.
A representative stereomicroscopic image of the replica: six points were used to measure marginal adaptation of the inlay (C, cement line).
Measurement of internal adaptation: three points were used from axial walls and three points from the pulpal floor of the replicas (C, cement line).
Cementation procedure
The teeth were cleaned with fluoride-free pumice before cementation using a polishing brush. Inlays were cemented with an adhesive luting system (Variolink N, Ivoclar Vivadent) according to the manufacturer’s instructions as follows. Adherent surfaces of the teeth were etched with 37% phosphoric acid (30 s for enamel that remained at the occlusal surfaces, 15 s for dentine), rinsed with water, and then gently air-dried to remove excess water, leaving the cavity visibly wet.11. Santos MJ, Freitas MC, Azevedo LM, Santos GC Jr, Navarro MF, Francischone CE et al. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: 12-year follow-up. Clin Oral Investig. 2016 Sep;20(7):1683-90. https://doi.org/10.1007/s00784-015-1669-z
https://doi.org/10.1007/s00784-015-1669-...
,1111. Keshvad A, Hooshmand T, Asefzadeh F, Khalilinejad F, Alihemmati M, Van Noort R. Marginal gap, internal fit, and fracture load of leucite-reinforced ceramic inlays fabricated by CEREC inLab and hot-pressed techniques. J Prosthodont. 2011 Oct;20(7):535-40. https://doi.org/10.1111/j.1532-849X.2011.00745.x PMID:21806704
https://doi.org/10.1111/j.1532-849X.2011...
Teeth surfaces were conditioned with Syntac Primer for 15s, air-dried, Syntac Adhesive for 10s, air-dried, and then Heliobond (Ivoclar Vivadent) was applied, air-thinned but not lightcured, respectively according to the manufacturer’s instructions (Variolink N, Ivoclar). The intaglio surfaces of the inlays were etched with 4.9% hydrofluoric acid (IPS Ceramic Etching gel; Ivoclar Vivadent) for 20 s and were rinsed with water for 60 s, then air-dried. A silane coupling agent (Monobond S; Ivoclar Vivadent) was used for 60s, air-dried and then bonding agent (Heliobond, Ivoclar Vivadent) was applied, air-thinned, but not cured. Base and catalyst (1:1) of dual polymerizing resin cement (Lot: W36476, Variolink N, Ivoclar Vivadent) were mixed and applied in the cavities. Inlays were seated into the cavities with a constant load of 50 N in a universal testing machine (Shimadzu) to standardize the cementation procedures. Excess cement was removed and glycerin gel (Liquid Strip; Ivoclar Vivadent) was applied at the margins and then light-cured (Elipar S10; 3M ESPE, St Paul, MN, USA) for 40 s. Finishing was performed with finishing diamonds and polishing disks (SofLex Pop-on; 3M ESPE).
OCT measurements
OCT measurements of marginal adaptations of ceramic inlays were performed as described in a previous study using the Thorlabs OCT system,1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
which took spectral domain OCT images with 930-nm wavelengths.3939. Yilmazlar I, Sabuncu M. Speckle noise reduction based on induced mode hopping in a semiconductor laser diode by drive current modulation. Opt Laser Technol. 2015 Oct;73:19-22. https://doi.org/10.1016/j.optlastec.2015.04.014
https://doi.org/10.1016/j.optlastec.2015...
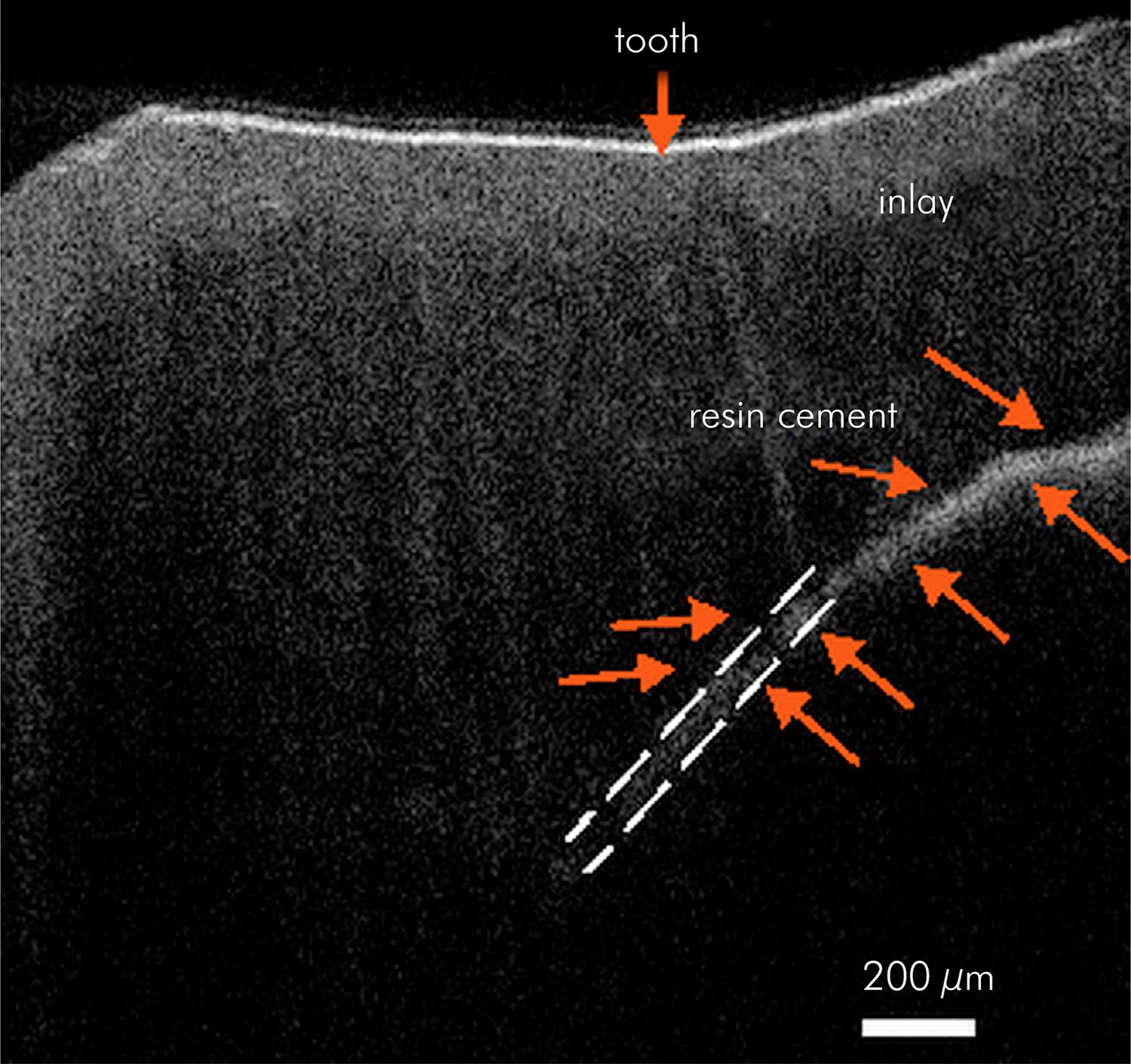
The 100-nm-broad diode allowed for low speckle noise imaging. The A-scan line rate was 1.2 kHz and the B-scan frame rate was 512 line/frame. Resolution of the OCT images in depth and lateral scan were 7 μm and 8 μm, respectively. The imaging depth was approximately 1.7 mm and the measurements had a signal-to-noise ratio (SNR) of 83 dB. OCT spectrum was optimized on the B-scan to apply fine adjustments. The tooth was placed in the reference arm so that the probe and beam oriented 90° with respect to the tooth occlusal surface. The infrared beam first hit the tooth from the occlusal surface and scanned over the entire marginal adaptation area (tooth-resin cement-inlay) in 200-μm intervals. The table on which the tooth was placed was adjustable with a micrometer screw to achieve a smooth and precise 200-μm incremental shift between successive measurements. Using the ruler tool on the image processing software, the marginal adaptation was measured and recorded during each scan (Figure 4). These data were then averaged to estimate the mean marginal adaptation values.
A representative of optical coherence tomographic scan with transversal view of a tooth after inlay cementation. The marginal adaptation was measured from cement thickness.
Internal adaptation measurements were performed by moving the teeth closer to the probe to scan a deeper internal region.3737. Braz AK, Kyotoku BB, Braz R, Gomes AS. Evaluation of crack propagation in dental composites by optical coherence tomography. Dent Mater. 2009 Jan;25(1):74-9. https://doi.org/10.1016/j.dental.2008.04.011
https://doi.org/10.1016/j.dental.2008.04...
The light beam from the OCT source was projected onto the tooth from the occlusal area as previously for marginal measurements. Backscattered light that carried information about the internal adaptation (Figure 5) was saved and then examined in the Fourier domain by applying a Fourier Transform (FT; Figure 6). Since light reflected from different sample depths produces interference patterns with the different frequency components, the FT data gave information about light scattered from the inlay, resin cement, and tooth. A strong back reflection due to an abrupt refractive index change resulted in the first peak in the depth profile when the light beam encountered ceramic inlay after air. The signal sees no peaks as it travels through a medium in which there are no large indexes of refractive changes.3434. Melo LS, Araujo RE, Freitas AZ, Zezell D, Vieira ND, Girkin J et al. Evaluation of enamel dental restoration interface by optical coherence tomography. J Biomed Opt. 2005 Nov-Dec;10(6):064027. https://doi.org/10.1117/1.2141617
https://doi.org/10.1117/1.2141617...
The signal level, therefore, will rise again when light arrives at the resin cement interface. At the end of the resin cement there will be another slight peak. The magnitude of the peak becomes smaller as the light intensity is reduced as it travels into the sample. The optical path length between these two peaks corresponded to the optical path length of the resin cement. To convert the optical path length to the actual thickness, the optical path length should be divided to the refractive index of the luting cement, which is approximately 1.5 at the measured wavelength.3535. Makishi P, Shimada Y, Sadr A, Tagami J, Sumi Y. Non-destructive 3D imaging of composite restorations using optical coherence tomography: marginal adaptation of self-etch adhesives. J Dent. 2011 Apr;39(4):316-25. https://doi.org/10.1016/j.jdent.2011.01.011
https://doi.org/10.1016/j.jdent.2011.01....
,3636. Monteiro GQ, Montes MA, Gomes AS, Mota CC, Campello SL, Freitas AZ. Marginal analysis of resin composite restorative systems using optical coherence tomography. Dent Mater. 2011 Dec;27(12):e213-23. https://doi.org/10.1016/j.dental.2011.08.400
https://doi.org/10.1016/j.dental.2011.08...
This procedure resulted in an accurate quantitative measurement of the internal adaptation. The conversion of optical path length to thickness is explained in the literature.4040. Sabuncu M, Akdoğan M. Utilizing optical coherence tomography in the nondestructive and noncontact measurement of egg shell thickness. Scient World J. 2014;2014(3):205191. https://doi.org/10.1155/2014/205191
https://doi.org/10.1155/2014/205191...
A representative transversal view of internal adaptation of ceramic inlay was measured through optical scan of internal resin cement.
Fourier transform data of backscattered light from the inlay, resin cement, and tooth. A strong back reflection due to an abrupt refractive index change results in the first peak in the depth profile when the light beam encounters ceramic inlay after air. The signal sees no peaks as it travels through a medium in which there are no large indexes of refractive changes. Therefore, the signal level will rise again when light arrives at the resin cement interface. At the end of the resin cement, there will be another slight peak. The optical path length between these two peaks corresponds to the optical path length of the resin cement.
Statistical analysis
Replica and OCT measurements of marginal and internal adaptation values of inlays were statistically evaluated with SPSS 13.0 (SPSS, Chicago, IL, USA). The Levene test was used to check the normality of the variances, and the independent samples t-test was used to compare the adaptation values between the replica and OCT groups. The paired t-test was used to evaluate marginal and internal adaptations of each group.
Results
Mean marginal and internal adaptation values of the ceramic inlays that were measured using the replica and OCT techniques are presented in the Table 1. There were significant differences between the measurement techniques. Marginal (t = 41.32, F = 3.102, p = 0.00) and internal (t = 2.57, F = 6.57, p = 0.01) adaptation values were higher for replica than for OCT measurements. When marginal and internal adaptation values were evaluated within the groups, there were significant differences for replica (t = 3.34, p = 0.00) and OCT (t = 25.88, p = 0.00) groups. Internal adaptation values were higher than the marginal adaptation values.
Discussion
According to our results, marginal and internal adaptation values with OCT were lower than those with the replica technique. Thus, the first hypothesis was rejected. Marginal and internal adaptations of ceramic inlays were 28.97 and 97.87 μm, respectively, with OCT and 100.97 and 113.94 μm, respectively, with the replica technique. When marginal and internal adaptation values were evaluated within the groups, significant differences were found between both techniques. Internal adaptation values were higher than the marginal adaptation values. Thus, the second hypothesis was also rejected. Marginal adaptation value found by OCT technique showed better results than replica technique in this study. OCT systems have the advantage of real time and direct evaluation of the structures.3636. Monteiro GQ, Montes MA, Gomes AS, Mota CC, Campello SL, Freitas AZ. Marginal analysis of resin composite restorative systems using optical coherence tomography. Dent Mater. 2011 Dec;27(12):e213-23. https://doi.org/10.1016/j.dental.2011.08.400
https://doi.org/10.1016/j.dental.2011.08...
However, the replica technique indirectly represents the cement film thickness1414. Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005 Jun;32(6):448-53. https://doi.org/10.1111/j.1365-2842.2005.01443.x
https://doi.org/10.1111/j.1365-2842.2005...
and had some limitations and inherent errors, such as identification of restoration margins and finishing lines.2020. Falk A, Steyern PV, Fransson H, Thorén MM. Reliability of the impression replica technique. Int J Prosthodont. 2015 Mar-Apr;28(2):179-80. https://doi.org/10.11607/ijp.4132
https://doi.org/10.11607/ijp.4132...
,2121. Gemalmaz D, Kükrer D. In vivo and in vitro evaluation of marginal fit of class II ceromer inlays. J Oral Rehabil. 2006 Jun;33(6):436-42. https://doi.org/10.1111/j.1365-2842.2005.01562.x
https://doi.org/10.1111/j.1365-2842.2005...
In addition, the defects on the replica or in the cutting process could affect evaluation of the film thickness.2222. Quante K, Ludwig K, Kern M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent Mater. 2008 Oct;24(10):1311-5. https://doi.org/10.1016/j.dental.2008.02.011PMID:18384869
https://doi.org/10.1016/j.dental.2008.02...
,2323. Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns—validation of the silicone replica method. J Oral Rehabil. 2008 Feb;35(2):116-22. https://doi.org/10.1111/j.1365-2842.2003.01203.x
https://doi.org/10.1111/j.1365-2842.2003...
Higher adaptation values of ceramic inlays measured using the replica technique in our study could have arisen due to the aforementioned factors related to the indirect evaluation. The OCT technique seemed to give more reliable information about the adaptation of inlays because of direct evaluation. It is important to assess restorations non-invasively especially in clinical conditions. The replica technique and OCT are reliable, reproducible, and noninvasive techniques used to determine in vivo and in vitro adaptation of restorations to tooth surface without causing damage.1414. Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005 Jun;32(6):448-53. https://doi.org/10.1111/j.1365-2842.2005.01443.x
https://doi.org/10.1111/j.1365-2842.2005...
,1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
,2020. Falk A, Steyern PV, Fransson H, Thorén MM. Reliability of the impression replica technique. Int J Prosthodont. 2015 Mar-Apr;28(2):179-80. https://doi.org/10.11607/ijp.4132
https://doi.org/10.11607/ijp.4132...
,2323. Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns—validation of the silicone replica method. J Oral Rehabil. 2008 Feb;35(2):116-22. https://doi.org/10.1111/j.1365-2842.2003.01203.x
https://doi.org/10.1111/j.1365-2842.2003...
,3333. Bakhsh TA, Sadr A, Shimada Y, Mandurah MM, Hariri I, Alsayed EZ et al. Concurrent evaluation of composite internal adaptation and bond strength in a class-I cavity. J Dent. 2013 Jan;41(1):60-70. https://doi.org/10.1016/j.jdent.2012.10.003
https://doi.org/10.1016/j.jdent.2012.10....
,3535. Makishi P, Shimada Y, Sadr A, Tagami J, Sumi Y. Non-destructive 3D imaging of composite restorations using optical coherence tomography: marginal adaptation of self-etch adhesives. J Dent. 2011 Apr;39(4):316-25. https://doi.org/10.1016/j.jdent.2011.01.011
https://doi.org/10.1016/j.jdent.2011.01....
Thus in this study replica and OCT techniques were used. Previous studies had proved the facility of OCT to investigate adaptation of restorations without cutting the specimens.2727. Turkistani A, Sadr A, Shimada Y, Nikaido T, Sumi Y, Tagami J. Sealing performance of resin cements before and after thermal cycling: evaluation by optical coherence tomography. Dent Mater. 2014 Sep;30(9):993-1004. https://doi.org/10.1016/j.dental.2014.05.010
https://doi.org/10.1016/j.dental.2014.05...
,3333. Bakhsh TA, Sadr A, Shimada Y, Mandurah MM, Hariri I, Alsayed EZ et al. Concurrent evaluation of composite internal adaptation and bond strength in a class-I cavity. J Dent. 2013 Jan;41(1):60-70. https://doi.org/10.1016/j.jdent.2012.10.003
https://doi.org/10.1016/j.jdent.2012.10....
OCT is a device that is capable of obtaining precise tomographic images of the tissue without any invasion and can give fast data of the complete cavity and the restoration.2929. Minamino T, Mine A, Omiya K, Matsumoto M, Nakatani H, Iwashita T et al. Nondestructive observation of teeth post core space using optical coherence tomography: a pilot study. J Biomed Opt. 2014 Apr;19(4):046004. https://doi.org/10.1117/1.JBO.19.4.046004
https://doi.org/10.1117/1.JBO.19.4.04600...
In addition, with development of intraoral probe, the OCT has been used for chair side evaluation.2828. Lenton P, Rudney J, Chen R, Fok A, Aparicio C, Jones RS. Imaging in vivo secondary caries and ex vivo dental biofilms using cross-polarization optical coherence tomography. Dent Mater. 2012 Jul;28(7):792-800. https://doi.org/10.1016/j.dental.2012.04.004
https://doi.org/10.1016/j.dental.2012.04...
This approach allows the clinician to evaluate a single image with the purpose of diagnosis secondary caries adjacent to restorations and the restoration-tooth structure interface due to the optical differences.2828. Lenton P, Rudney J, Chen R, Fok A, Aparicio C, Jones RS. Imaging in vivo secondary caries and ex vivo dental biofilms using cross-polarization optical coherence tomography. Dent Mater. 2012 Jul;28(7):792-800. https://doi.org/10.1016/j.dental.2012.04.004
https://doi.org/10.1016/j.dental.2012.04...
Various studies have reported marginal adaptation values of ceramic inlays ranging from 43 to 199 μm.1212. Thordrup M, Isidor F, Hörsted-Bindslev P. Comparison of marginal fit and microleakage of ceramic and composite inlays: an in vitro study. J Dent. 1994 Jun;22(3):147-53. https://doi.org/10.1016/0300-5712(94)90198-8PMID:8027457
https://doi.org/10.1016/0300-5712(94)901...
,1313. Audenino G, Bresciano ME, Bassi F, Carossa S. In vitro evaluation of fit of adhesively luted ceramic inlays. Int J Prosthodont. 1999 Jul-Aug;12(4):342-7. PMID:10635204,1414. Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005 Jun;32(6):448-53. https://doi.org/10.1111/j.1365-2842.2005.01443.x
https://doi.org/10.1111/j.1365-2842.2005...
,1515. Molin M, Karlsson S. The fit of gold inlays and three ceramic inlay systems. A clinical and in vitro study. Acta Odontol Scand. 1993 Aug;51(4):201-6. https://doi.org/10.3109/00016359309040568
https://doi.org/10.3109/0001635930904056...
Higher marginal adaptation values are related to increased exposure of the luting cement to the oral environment, leading to an increased risk of plaque retention, caries, pulp pathology, and microcracks at the marginal edges of the restorative material or of the tooth structure.2626. Guess PC, Vagkopoulou T, Zhang Y, Wolkewitz M, Strub JR. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014 Feb;42(2):199-209. https://doi.org/10.1016/j.jdent.2013.10.002
https://doi.org/10.1016/j.jdent.2013.10....
An acceptable marginal adaptation value in clinical conditions for ceramic restorations was reported to be < 120 μm to avoid wear of the luting cement.1919. McLean JW, Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971 Aug;131(3):107-11. https://doi.org/10.1038/sj.bdj.4802708
https://doi.org/10.1038/sj.bdj.4802708...
Thus, the marginal adaptation values of our study were within clinically acceptable limits. The internal adaptation, revealed by the thickness of the cement layer, is another key factor for long-term stability of all-ceramic restorations. Although an adequate internal adaptation of a restoration is considered a significant factor for longevity, optimum values for internal adaptations have not been determined.2626. Guess PC, Vagkopoulou T, Zhang Y, Wolkewitz M, Strub JR. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014 Feb;42(2):199-209. https://doi.org/10.1016/j.jdent.2013.10.002
https://doi.org/10.1016/j.jdent.2013.10....
Like marginal adaptation measurement techniques, internal adaptations of restorations have been measured using destructive and nondestructive techniques. Among nondestructive techniques, OCT has been used previously to evaluate the internal adaptations of composite restorations.1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
,3333. Bakhsh TA, Sadr A, Shimada Y, Mandurah MM, Hariri I, Alsayed EZ et al. Concurrent evaluation of composite internal adaptation and bond strength in a class-I cavity. J Dent. 2013 Jan;41(1):60-70. https://doi.org/10.1016/j.jdent.2012.10.003
https://doi.org/10.1016/j.jdent.2012.10....
,3535. Makishi P, Shimada Y, Sadr A, Tagami J, Sumi Y. Non-destructive 3D imaging of composite restorations using optical coherence tomography: marginal adaptation of self-etch adhesives. J Dent. 2011 Apr;39(4):316-25. https://doi.org/10.1016/j.jdent.2011.01.011
https://doi.org/10.1016/j.jdent.2011.01....
Internal adaptations of metal-ceramic and all-ceramic veneers were evaluated in a previous study,3838. Sinescu C, Negrutiu ML, Todea C, Balabuc C, Filip L, Rominu R et al. Quality assessment of dental treatments using en-face optical coherence tomography. J Biomed Opt. 2008 Sep-Oct;13(5):054065. https://doi.org/10.1117/1.2992593
https://doi.org/10.1117/1.2992593...
but to our knowledge, internal adaptation of ceramic inlays has not been evaluated in the literature. In our study, OCT was used to measure the internal adaptation values of ceramic inlays. Since the imaging depth of the OCT system used in our study was 1.7 mm, class I cavities that were 1.5 mm deep were prepared to evaluate internal adaptations. In several studies, internal adaptation values for ceramic inlays were reported to be 67–227 μm and internal adaptation values were higher than those of the marginal adaptations.1414. Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005 Jun;32(6):448-53. https://doi.org/10.1111/j.1365-2842.2005.01443.x
https://doi.org/10.1111/j.1365-2842.2005...
,2626. Guess PC, Vagkopoulou T, Zhang Y, Wolkewitz M, Strub JR. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014 Feb;42(2):199-209. https://doi.org/10.1016/j.jdent.2013.10.002
https://doi.org/10.1016/j.jdent.2013.10....
Similar to these results, internal adaptation values were higher than the marginal adaptation values with the replica and OCT techniques in our study. This could be related to die spacer thickness or finishing techniques, such as damage from the glass particles used to remove investment material from the inlays and using burs for adaptation procedures of inlays to teeth.
Measurement techniques of adaptations of restorations should be reliable, reproducible, and standardized. Most techniques for assessing marginal integrity of restorations, such as sectioning the samples and penetrating liquids, were destructive techniques that should be performed in vitro only.3838. Sinescu C, Negrutiu ML, Todea C, Balabuc C, Filip L, Rominu R et al. Quality assessment of dental treatments using en-face optical coherence tomography. J Biomed Opt. 2008 Sep-Oct;13(5):054065. https://doi.org/10.1117/1.2992593
https://doi.org/10.1117/1.2992593...
Nondestructive techniques, such as radiographs, CT, nuclear magnetic resonance, the replica technique, and OCT, have been used in vivo. Radiography and CT are invasive techniques for patients and have limited detection capacities.3838. Sinescu C, Negrutiu ML, Todea C, Balabuc C, Filip L, Rominu R et al. Quality assessment of dental treatments using en-face optical coherence tomography. J Biomed Opt. 2008 Sep-Oct;13(5):054065. https://doi.org/10.1117/1.2992593
https://doi.org/10.1117/1.2992593...
In our study, silicone replicas were evaluated with the optical microscopes that are often used in studies.2020. Falk A, Steyern PV, Fransson H, Thorén MM. Reliability of the impression replica technique. Int J Prosthodont. 2015 Mar-Apr;28(2):179-80. https://doi.org/10.11607/ijp.4132
https://doi.org/10.11607/ijp.4132...
,2323. Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns—validation of the silicone replica method. J Oral Rehabil. 2008 Feb;35(2):116-22. https://doi.org/10.1111/j.1365-2842.2003.01203.x
https://doi.org/10.1111/j.1365-2842.2003...
Measuring three-dimensional (3D) replicas with computerized techniques2424. Kim KB, Kim JH, Kim WC, Kim HY, Kim JH. Evaluation of the marginal and internal gap of metal-ceramic crown fabricated with a selective laser sintering technology: two- and three-dimensional replica techniques. J Adv Prosthodont. 2013 May;5(2):179-86. https://doi.org/10.4047/jap.2013.5.2.179
https://doi.org/10.4047/jap.2013.5.2.179...
,2525. Park JY, Bae SY, Lee JJ, Kim JH, Kim HY, Kim WC. Evaluation of the marginal and internal gaps of three different dental prostheses: comparison of the silicone replica technique and three-dimensional superimposition analysis. J Adv Prosthodont. 2017 Jun;9(3):159-69. https://doi.org/10.4047/jap.2017.9.3.159
https://doi.org/10.4047/jap.2017.9.3.159...
and micro-CT99. Uzgur R, Ercan E, Uzgur Z, Çolak H, Yalçın M, Özcan M. Cement thickness of inlay restorations made of lithium disilicate, polymer-infiltrated ceramic and nano-ceramic CAD/CAM materials evaluated using 3D X-ray micro-computed tomography. J Prosthodont. 2016 Aug. https://doi.org/10.1111/jopr.12521
https://doi.org/10.1111/jopr.12521...
,1010. Alajaji NK, Bardwell D, Finkelman M, Ali A. Micro-CT evaluation of ceramic inlays: comparison of the marginal and internal fit of five and three axis CAM systems with a heat press technique. J Esthet Restor Dent. 2017 Feb;29(1):49-58. https://doi.org/10.1111/jerd.12271
https://doi.org/10.1111/jerd.12271...
that allows high-resolution measurement could provide more reliable results. However, 3D computerized and silicone replica techniques are reported as applicable methods for the marginal and internal adaptation evaluation.2525. Park JY, Bae SY, Lee JJ, Kim JH, Kim HY, Kim WC. Evaluation of the marginal and internal gaps of three different dental prostheses: comparison of the silicone replica technique and three-dimensional superimposition analysis. J Adv Prosthodont. 2017 Jun;9(3):159-69. https://doi.org/10.4047/jap.2017.9.3.159
https://doi.org/10.4047/jap.2017.9.3.159...
In addition, one study reported that marginal adaptation could not be measured by 3D since margins represent a line.2424. Kim KB, Kim JH, Kim WC, Kim HY, Kim JH. Evaluation of the marginal and internal gap of metal-ceramic crown fabricated with a selective laser sintering technology: two- and three-dimensional replica techniques. J Adv Prosthodont. 2013 May;5(2):179-86. https://doi.org/10.4047/jap.2013.5.2.179
https://doi.org/10.4047/jap.2013.5.2.179...
Thus, two-dimensional analysis of replicas with an optical microscope seemed to be a proper technique.
The OCT system has been previously compared with other techniques, such as optical microscopy, SEM, confocal laser scanning microscopy, and acoustic emission techniques.3131. Matheus TC, Kauffman CM, Braz AK, Mota CC, Gomes AS. Fracture process characterization of fiber-reinforced dental composites evaluated by optical coherence tomography, SEM and optical microscopy. Braz Dent J. 2010;21(5):420-7. https://doi.org/10.1590/S0103-64402010000500008
https://doi.org/10.1590/S0103-6440201000...
,3232. Lin CL, Kuo WC, Chang YH, Yu JJ, Lin YC. Examination of ceramic/enamel interfacial debonding using acoustic emission and optical coherence tomography. Dent Mater. 2014 Aug;30(8):910-6. https://doi.org/10.1016/j.dental.2014.05.023
https://doi.org/10.1016/j.dental.2014.05...
,3535. Makishi P, Shimada Y, Sadr A, Tagami J, Sumi Y. Non-destructive 3D imaging of composite restorations using optical coherence tomography: marginal adaptation of self-etch adhesives. J Dent. 2011 Apr;39(4):316-25. https://doi.org/10.1016/j.jdent.2011.01.011
https://doi.org/10.1016/j.jdent.2011.01....
According to these reports, OCT provided similar results compared with other techniques. In addition, OCT was reported to have better visualization than SEM and optical microscopy.3131. Matheus TC, Kauffman CM, Braz AK, Mota CC, Gomes AS. Fracture process characterization of fiber-reinforced dental composites evaluated by optical coherence tomography, SEM and optical microscopy. Braz Dent J. 2010;21(5):420-7. https://doi.org/10.1590/S0103-64402010000500008
https://doi.org/10.1590/S0103-6440201000...
In our study, OCT showed lower adaptation values than the replica technique, with both values being within clinically acceptable limits. This could be related to the different flowing characteristics of the measured surfaces: light-body silicone for replica technique and luting cement for OCT.
OCT systems have the advantage of real-time evaluation of the structures. These systems have a wide range of wavelengths that produce interference images of structures.3636. Monteiro GQ, Montes MA, Gomes AS, Mota CC, Campello SL, Freitas AZ. Marginal analysis of resin composite restorative systems using optical coherence tomography. Dent Mater. 2011 Dec;27(12):e213-23. https://doi.org/10.1016/j.dental.2011.08.400
https://doi.org/10.1016/j.dental.2011.08...
The OCT systems that have ≥1260 nm wavelengths penetrate more into tissue.1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
These OCT systems were used in studies to evaluate the whole image of the fixed partial denture as well as qualitatively evaluate root canal or periodontal pocket.3030. Kim SH, Kang SR, Park HJ, Kim JM, Yi WJ, Kim TI. Improved accuracy in periodontal pocket depth measurement using optical coherence tomography. J Periodontal Implant Sci. 2017 Feb;47(1):13-9. https://doi.org/10.5051/jpis.2017.47.1.13
https://doi.org/10.5051/jpis.2017.47.1.1...
,3838. Sinescu C, Negrutiu ML, Todea C, Balabuc C, Filip L, Rominu R et al. Quality assessment of dental treatments using en-face optical coherence tomography. J Biomed Opt. 2008 Sep-Oct;13(5):054065. https://doi.org/10.1117/1.2992593
https://doi.org/10.1117/1.2992593...
Marginal and internal adaptations were evaluated in previous studies with lower wavelengths either qualitatively or quantitatively to obtain in-depth images.1818. Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
https://doi.org/10.1590/1678-77572016001...
,2727. Turkistani A, Sadr A, Shimada Y, Nikaido T, Sumi Y, Tagami J. Sealing performance of resin cements before and after thermal cycling: evaluation by optical coherence tomography. Dent Mater. 2014 Sep;30(9):993-1004. https://doi.org/10.1016/j.dental.2014.05.010
https://doi.org/10.1016/j.dental.2014.05...
,3636. Monteiro GQ, Montes MA, Gomes AS, Mota CC, Campello SL, Freitas AZ. Marginal analysis of resin composite restorative systems using optical coherence tomography. Dent Mater. 2011 Dec;27(12):e213-23. https://doi.org/10.1016/j.dental.2011.08.400
https://doi.org/10.1016/j.dental.2011.08...
Similar to previous studies, in our study, the OCT system with 930 nm wavelengths was used to quantitatively evaluate marginal and internal adaptations of ceramic inlays. Further studies should be performed to evaluate internal or marginal adaptations of restorations using OCT systems in vivo, since they could be used in clinical conditions for controlling adaptations of restorations by quantifying few micrometers gaps or diagnosing secondary caries under restorations non-invasively.
Conclusion
Within the limitations of this in vitro study, our results showed that the replica and OCT techniques had different marginal and internal adaptation values, with higher values of marginal and internal adaptation associated with the replica technique. Although OCT demonstrated lower results, all adaptation values were within clinically acceptable limits. The OCT system could be used to quantitatively evaluate adaptation of ceramic inlay restorations noninvasively.
References
-
1Santos MJ, Freitas MC, Azevedo LM, Santos GC Jr, Navarro MF, Francischone CE et al. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: 12-year follow-up. Clin Oral Investig. 2016 Sep;20(7):1683-90. https://doi.org/10.1007/s00784-015-1669-z
» https://doi.org/10.1007/s00784-015-1669-z -
2Holberg C, Winterhalder P, Wichelhaus A, Hickel R, Huth K. Fracture risk of lithium-disilicate ceramic inlays: a finite element analysis. Dent Mater. 2013 Dec;29(12):1244-50. https://doi.org/10.1016/j.dental.2013.09.012
» https://doi.org/10.1016/j.dental.2013.09.012 -
3Krämer N, Taschner M, Lohbauer U, Petschelt A, Frankenberger R. Totally bonded ceramic inlays and onlays after eight years. J Adhes Dent. 2008 Aug;10(4):307-14.
-
4Frankenberger R, Taschner M, Garcia-Godoy F, Petschelt A, Krämer N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent. 2008 Oct;10(5):393-8.
-
5Uludag B, Yucedag E, Sahin V. Microleakage of inlay ceramic systems luted with self-adhesive resin cements. J Adhes Dent. 2014 Dec;16(6):523-9.
-
6Bott B, Hannig M. Effect of different luting materials on the marginal adaptation of Class I ceramic inlay restorations in vitro. Dent Mater. 2003 Jun;19(4):264-9. https://doi.org/10.1016/S0109-5641(02)00038-6
» https://doi.org/10.1016/S0109-5641(02)00038-6 -
7Uludag B, Ozturk O, Ozturk AN. Microleakage of ceramic inlays luted with different resin cements and dentin adhesives. J Prosthet Dent. 2009 Oct;102(4):235-41. https://doi.org/10.1016/S0022-3913(09)60161-X
» https://doi.org/10.1016/S0022-3913(09)60161-X -
8Trindade FZ, Valandro LF, Jager N, Bottino MA, Kleverlaan CJ. Elastic properties of lithium disilicate versus feldspathic inlays: effect on the bonding by 3D finite element analysis. J Prosthodont. 2016 Oct. https://doi.org/10.1111/jopr.12550
» https://doi.org/10.1111/jopr.12550 -
9Uzgur R, Ercan E, Uzgur Z, Çolak H, Yalçın M, Özcan M. Cement thickness of inlay restorations made of lithium disilicate, polymer-infiltrated ceramic and nano-ceramic CAD/CAM materials evaluated using 3D X-ray micro-computed tomography. J Prosthodont. 2016 Aug. https://doi.org/10.1111/jopr.12521
» https://doi.org/10.1111/jopr.12521 -
10Alajaji NK, Bardwell D, Finkelman M, Ali A. Micro-CT evaluation of ceramic inlays: comparison of the marginal and internal fit of five and three axis CAM systems with a heat press technique. J Esthet Restor Dent. 2017 Feb;29(1):49-58. https://doi.org/10.1111/jerd.12271
» https://doi.org/10.1111/jerd.12271 -
11Keshvad A, Hooshmand T, Asefzadeh F, Khalilinejad F, Alihemmati M, Van Noort R. Marginal gap, internal fit, and fracture load of leucite-reinforced ceramic inlays fabricated by CEREC inLab and hot-pressed techniques. J Prosthodont. 2011 Oct;20(7):535-40. https://doi.org/10.1111/j.1532-849X.2011.00745.x PMID:21806704
» https://doi.org/10.1111/j.1532-849X.2011.00745.x -
12Thordrup M, Isidor F, Hörsted-Bindslev P. Comparison of marginal fit and microleakage of ceramic and composite inlays: an in vitro study. J Dent. 1994 Jun;22(3):147-53. https://doi.org/10.1016/0300-5712(94)90198-8PMID:8027457
» https://doi.org/10.1016/0300-5712(94)90198-8PMID:8027457 -
13Audenino G, Bresciano ME, Bassi F, Carossa S. In vitro evaluation of fit of adhesively luted ceramic inlays. Int J Prosthodont. 1999 Jul-Aug;12(4):342-7. PMID:10635204
-
14Karakaya S, Sengun A, Ozer F. Evaluation of internal adaptation in ceramic and composite resin inlays by silicon replica technique. J Oral Rehabil. 2005 Jun;32(6):448-53. https://doi.org/10.1111/j.1365-2842.2005.01443.x
» https://doi.org/10.1111/j.1365-2842.2005.01443.x -
15Molin M, Karlsson S. The fit of gold inlays and three ceramic inlay systems. A clinical and in vitro study. Acta Odontol Scand. 1993 Aug;51(4):201-6. https://doi.org/10.3109/00016359309040568
» https://doi.org/10.3109/00016359309040568 -
16Ender A, Bienz S, Mörmann W, Mehl A, Attin T, Stawarczyk B. Marginal adaptation, fracture load and macroscopic failure mode of adhesively luted PMMA-based CAD/CAM inlays. Dent Mater. 2016 Feb;32(2):e22-9. https://doi.org/10.1016/j.dental.2015.11.009
» https://doi.org/10.1016/j.dental.2015.11.009 -
17Han SH, Sadr A, Tagami J, Park SH. Non-destructive evaluation of an internal adaptation of resin composite restoration with swept-source optical coherence tomography and micro-CT. Dent Mater. 2016 Jan;32(1):e1-7. https://doi.org/10.1016/j.dental.2015.10.009
» https://doi.org/10.1016/j.dental.2015.10.009 -
18Türk AG, Sabuncu M, Ünal S, Önal B, Ulusoy M. Comparison of the marginal adaptation of direct and indirect composite inlay restorations with optical coherence tomography. J Appl Oral Sci. 2016 Jul-Aug;24(4):383-90. https://doi.org/10.1590/1678-775720160012
» https://doi.org/10.1590/1678-775720160012 -
19McLean JW, Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971 Aug;131(3):107-11. https://doi.org/10.1038/sj.bdj.4802708
» https://doi.org/10.1038/sj.bdj.4802708 -
20Falk A, Steyern PV, Fransson H, Thorén MM. Reliability of the impression replica technique. Int J Prosthodont. 2015 Mar-Apr;28(2):179-80. https://doi.org/10.11607/ijp.4132
» https://doi.org/10.11607/ijp.4132 -
21Gemalmaz D, Kükrer D. In vivo and in vitro evaluation of marginal fit of class II ceromer inlays. J Oral Rehabil. 2006 Jun;33(6):436-42. https://doi.org/10.1111/j.1365-2842.2005.01562.x
» https://doi.org/10.1111/j.1365-2842.2005.01562.x -
22Quante K, Ludwig K, Kern M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent Mater. 2008 Oct;24(10):1311-5. https://doi.org/10.1016/j.dental.2008.02.011PMID:18384869
» https://doi.org/10.1016/j.dental.2008.02.011PMID:18384869 -
23Laurent M, Scheer P, Dejou J, Laborde G. Clinical evaluation of the marginal fit of cast crowns—validation of the silicone replica method. J Oral Rehabil. 2008 Feb;35(2):116-22. https://doi.org/10.1111/j.1365-2842.2003.01203.x
» https://doi.org/10.1111/j.1365-2842.2003.01203.x -
24Kim KB, Kim JH, Kim WC, Kim HY, Kim JH. Evaluation of the marginal and internal gap of metal-ceramic crown fabricated with a selective laser sintering technology: two- and three-dimensional replica techniques. J Adv Prosthodont. 2013 May;5(2):179-86. https://doi.org/10.4047/jap.2013.5.2.179
» https://doi.org/10.4047/jap.2013.5.2.179 -
25Park JY, Bae SY, Lee JJ, Kim JH, Kim HY, Kim WC. Evaluation of the marginal and internal gaps of three different dental prostheses: comparison of the silicone replica technique and three-dimensional superimposition analysis. J Adv Prosthodont. 2017 Jun;9(3):159-69. https://doi.org/10.4047/jap.2017.9.3.159
» https://doi.org/10.4047/jap.2017.9.3.159 -
26Guess PC, Vagkopoulou T, Zhang Y, Wolkewitz M, Strub JR. Marginal and internal fit of heat pressed versus CAD/CAM fabricated all-ceramic onlays after exposure to thermo-mechanical fatigue. J Dent. 2014 Feb;42(2):199-209. https://doi.org/10.1016/j.jdent.2013.10.002
» https://doi.org/10.1016/j.jdent.2013.10.002 -
27Turkistani A, Sadr A, Shimada Y, Nikaido T, Sumi Y, Tagami J. Sealing performance of resin cements before and after thermal cycling: evaluation by optical coherence tomography. Dent Mater. 2014 Sep;30(9):993-1004. https://doi.org/10.1016/j.dental.2014.05.010
» https://doi.org/10.1016/j.dental.2014.05.010 -
28Lenton P, Rudney J, Chen R, Fok A, Aparicio C, Jones RS. Imaging in vivo secondary caries and ex vivo dental biofilms using cross-polarization optical coherence tomography. Dent Mater. 2012 Jul;28(7):792-800. https://doi.org/10.1016/j.dental.2012.04.004
» https://doi.org/10.1016/j.dental.2012.04.004 -
29Minamino T, Mine A, Omiya K, Matsumoto M, Nakatani H, Iwashita T et al. Nondestructive observation of teeth post core space using optical coherence tomography: a pilot study. J Biomed Opt. 2014 Apr;19(4):046004. https://doi.org/10.1117/1.JBO.19.4.046004
» https://doi.org/10.1117/1.JBO.19.4.046004 -
30Kim SH, Kang SR, Park HJ, Kim JM, Yi WJ, Kim TI. Improved accuracy in periodontal pocket depth measurement using optical coherence tomography. J Periodontal Implant Sci. 2017 Feb;47(1):13-9. https://doi.org/10.5051/jpis.2017.47.1.13
» https://doi.org/10.5051/jpis.2017.47.1.13 -
31Matheus TC, Kauffman CM, Braz AK, Mota CC, Gomes AS. Fracture process characterization of fiber-reinforced dental composites evaluated by optical coherence tomography, SEM and optical microscopy. Braz Dent J. 2010;21(5):420-7. https://doi.org/10.1590/S0103-64402010000500008
» https://doi.org/10.1590/S0103-64402010000500008 -
32Lin CL, Kuo WC, Chang YH, Yu JJ, Lin YC. Examination of ceramic/enamel interfacial debonding using acoustic emission and optical coherence tomography. Dent Mater. 2014 Aug;30(8):910-6. https://doi.org/10.1016/j.dental.2014.05.023
» https://doi.org/10.1016/j.dental.2014.05.023 -
33Bakhsh TA, Sadr A, Shimada Y, Mandurah MM, Hariri I, Alsayed EZ et al. Concurrent evaluation of composite internal adaptation and bond strength in a class-I cavity. J Dent. 2013 Jan;41(1):60-70. https://doi.org/10.1016/j.jdent.2012.10.003
» https://doi.org/10.1016/j.jdent.2012.10.003 -
34Melo LS, Araujo RE, Freitas AZ, Zezell D, Vieira ND, Girkin J et al. Evaluation of enamel dental restoration interface by optical coherence tomography. J Biomed Opt. 2005 Nov-Dec;10(6):064027. https://doi.org/10.1117/1.2141617
» https://doi.org/10.1117/1.2141617 -
35Makishi P, Shimada Y, Sadr A, Tagami J, Sumi Y. Non-destructive 3D imaging of composite restorations using optical coherence tomography: marginal adaptation of self-etch adhesives. J Dent. 2011 Apr;39(4):316-25. https://doi.org/10.1016/j.jdent.2011.01.011
» https://doi.org/10.1016/j.jdent.2011.01.011 -
36Monteiro GQ, Montes MA, Gomes AS, Mota CC, Campello SL, Freitas AZ. Marginal analysis of resin composite restorative systems using optical coherence tomography. Dent Mater. 2011 Dec;27(12):e213-23. https://doi.org/10.1016/j.dental.2011.08.400
» https://doi.org/10.1016/j.dental.2011.08.400 -
37Braz AK, Kyotoku BB, Braz R, Gomes AS. Evaluation of crack propagation in dental composites by optical coherence tomography. Dent Mater. 2009 Jan;25(1):74-9. https://doi.org/10.1016/j.dental.2008.04.011
» https://doi.org/10.1016/j.dental.2008.04.011 -
38Sinescu C, Negrutiu ML, Todea C, Balabuc C, Filip L, Rominu R et al. Quality assessment of dental treatments using en-face optical coherence tomography. J Biomed Opt. 2008 Sep-Oct;13(5):054065. https://doi.org/10.1117/1.2992593
» https://doi.org/10.1117/1.2992593 -
39Yilmazlar I, Sabuncu M. Speckle noise reduction based on induced mode hopping in a semiconductor laser diode by drive current modulation. Opt Laser Technol. 2015 Oct;73:19-22. https://doi.org/10.1016/j.optlastec.2015.04.014
» https://doi.org/10.1016/j.optlastec.2015.04.014 -
40Sabuncu M, Akdoğan M. Utilizing optical coherence tomography in the nondestructive and noncontact measurement of egg shell thickness. Scient World J. 2014;2014(3):205191. https://doi.org/10.1155/2014/205191
» https://doi.org/10.1155/2014/205191
Publication Dates
-
Publication in this collection
2018
History
-
Received
24 Aug 2017 -
Reviewed
12 Dec 2017 -
Accepted
15 Dec 2017