| Argentina/2013 (Herscovici et al. 31) |
cRCT 6 months |
6 405 (171/234) 9-11 years |
- Offering healthier foods |
- Workshops about healthy eating habits and physical activity with students - Health-focused workshops with parents at school |
Compared to CG: - boys and girls: ↓ consumption of hamburgers and hot dogs - girls: ↑ consumption of skim milk and orange juice |
| Australia/2014 (Chellappah et al. 32) |
cRCT 8 weeks |
4 271 (137/134) 9-10 years |
- Offering fruits every day during break - Encouraging students to eat fruits in class before break |
- Did not include this component |
Compared to baseline: - ↓ WC Compared to CG: - ↑ vegetable and fruit intake |
| Australia/2021 (Ooi et al. 33) |
cRCT 6 months |
6 862 (389/473) 12-15 years |
- Decreasing accessibility and appeal of SSB - Changing the regular curriculum - Installing water fountains - Peer-led school challenge designed and led by a student committee |
- Lessons about SSB consumption with students - Sending health messages (push notifications) to students and parents - Sending newsletter snippets to parents |
No significant differences |
| Belgium/2006 (Haerens et al. 34) |
cRCT 2 years |
15 2,991 (759/2,232 ***) 11-15 years |
Group 1 + Group 2: - Offering fruit at very low prices or free of charge at least once a week - Offering water at a lower price than soft drinks or for free - Offering fruit as a dessert during lunch break - Hanging health-related folders and posters - Providing free water cans - Increasing the amount of time students spend in moderate-to-vigorous physical activity - Promoting physical activity during the school day and after school - Receiving box with sports materials (ropes, Frisbees, etc.) |
Group 1 + Group 2: - Encouraging teachers to organize extra support activities (healthy food) - Getting personalized feedback regarding physical activity and healthy eating for students Only Group 1: - Sending communications and activities and involving parents in interactive meetings |
At 2 years follow-up, compared Group 1 to CG: - girls: lower increase in BMI and BMI (z-score) At 2 years follow-up, compared Group 1 to Group 2: - girls: lower increase in BMI (z-score) |
| Chile/2004 (Kain et al. 35) |
cRCT 6 months |
5 3,086 (945/2,141) 6-10 years |
- Changing the regular curriculum - Training school canteen staff (including owners) - Providing extra physical activity time for students - Providing sports equipment |
- Lessons about healthy eating and physical activity - Healthy snacks contest (stickers and prize) - Training sessions with teachers - Involving parents in meetings |
Compared to baseline: - boys: ↓ BMI (z-score), WC |
| China/2014 and 2015 (Xu et al. 36,37) |
cRCT 8 months |
8 1,182 (544/638) 10 years |
- Changing the regular curriculum - Hanging health-related messages and posters (school canteen, classroom, gymnasium, and playground) - Promoting fun events |
- Lessons about healthy eating habits and physical activity with students - Training sessions with teachers - Involving parents in health classes at school |
Compared to CG: - ↓ consumption frequency of red meat, fried snacks and soft drinks - ↑ consumption frequency of vegetables - IG was more likely to achieve a 0.5kg BMI reduction |
| China/2015 (Cao et al. 38) |
cRCT 2 years + 9 months |
14 1,854 (889/965) 6-7 years |
- Offering more fruits and vegetables in the school canteen - Reducing the fat content of food - Disseminating obesity-related health information (blackboard newspaper, morning meeting, and class meeting) - Increasing the amount of time students spend in physical activity - Providing a strip of skipping rope to students (physical activity at home) |
- Lessons about health education (theme class meetings or seminars, brochures) to students and parents - Training sessions with teachers - Sending communications and activities to parents |
At 3 years follow-up, compared to CG: - ↓ odds of developing obesity or overweight - ↓ BMI (z-score) (especially for overweight and obese students) |
| China/2019 (Liu et al. 39) |
cRCT 1 year |
12 1,889 (959/930) 7-11 years |
- Changing rules regarding selling unhealthy foods - Not allowing SSB, unhealthy snacks, and electronic products (smartphones and tablets) in school - Providing practical suggestions to improve children’s dietary intake - Changing the regular curriculum - Hanging posters about health education knowledge - Increasing the amount of time students spend in moderate-to-vigorous physical activity - Providing sports equipment (rope jumping and shuttlecock kicking) |
- Lessons about behavioral knowledge, skills, healthy eating habits, childhood obesity prevention, and physical activity with students - Training sessions with teachers - Encouraging extracurricular activities at home - Involving parents in extracurricular physical activity and discussions about intervention approaches |
At 12 months follow-up, compared to CG: - ↓ percentage of children consuming SSB/day |
| China/2019 (Li et al. 40) |
cRCT 1 year |
40 1,641 (809/832) 6-7 years |
- Providing vegetables every day - Reducing the fat, sugar, and salt content of school meals - Offering smaller portion sizes - Testing school lunch improvement goals (school staff and commercial suppliers) - Creating a committee (physical activity levels) - Challenge of healthy behaviors (students, parents, teachers) - Increasing the amount of physical activity |
- Lessons and workshops about healthy eating and an active lifestyle with students - Handing out program handbooks (intervention activities) to school’s principals and class teachers - Promoting fun and active family games - Involving parents in workshops (with educational leaflets) |
Compared to CG: - ↓ BMI z-score, WC - ↑ consuming at least five daily portions of fruit and vegetables - ↓ weekly consumption of SSB and unhealthy snacks |
| Ecuador/2017 (Ochoa-Avilés et al. 41) |
cRCT 2 years + 4 months |
20 1,430 (728/702) 12-14 years |
- Changing the regular curriculum - Training school staff (recipes, leaflets, workshops) |
- Lessons and workshops about healthy eating habits (booklets, games, didactic material) with students - Preparation of a healthy breakfast with students - Involving parents in workshops at school (booklets) |
Compared to baseline: - ↓ WC - ↓ unhealthy snacks, added sugar, daily fruit and vegetables intake (decreased in both groups, but lower in IG) |
| England/2001 (Sahota et al. 42) |
cRCT 1 year |
10 613 (312/301) 7-11 years |
- Offering healthier foods - Changing the regular curriculum - Additional sessions supplied by the project manager |
- Lessons about healthy eating habits and physical activity with students - Training sessions with teachers |
Compared to baseline: - ↑ vegetable intake among all children - ↓ fruit intake among obese children - ↑ consumption of high-sugar foods and drinks among overweight children |
| Fiji/2011 (Kremer et al. 43) |
QE 2 years |
18 7,237 (4,567/2,670) 13-18 years |
- Offering healthier meals - Training school canteen staff (offering breakfast, opening earlier) - Changing the regular curriculum - Changing school policies for a healthy canteen (guidelines) - Building school gardens - Hanging posters and distributing pamphlets about healthy snacks - Promoting events, assembly (healthy eating habits) with students - Promoting physical activity during the school day - Providing sports equipment (hoops, ropes) and water bottles |
- Lessons about healthy eating habits with students and parents - Training on vegetable garden, pot plant technology, healthy meal preparation - Training sessions with teachers - Sending communications (newsletter, school website) and activities to parents |
Compared to CG: - ↓ %BF - ↑ vegetable intake (at school) |
| German/2009 (Muckelbauer et al. 44,45) |
cRCT 10 months |
33 3,190 (1,469/1,721) 7-8 years |
- Providing water bottles for children - Installing water fountains provided cooled, filtered, plain, or optionally carbonated water |
- Lessons about the importance of water for the body and the water circuit in nature with students - Training sessions with teachers |
Compared to CG: - ↓ risk of overweight - ↑ water consumption |
| India/2010 (Singhal et al. 46) |
cRCT 6 months |
2 201 (102/99) 15-17 years |
- Offering healthier foods - Stopping the sale of unhealthy foods - Promoting physical activity during the school day and after school |
- Lessons about healthy eating habits with students - Conducting a health camp with teachers and parents (nutritional counseling) - Counseling by phone for parents - Individual counseling by nutritionist |
Compared to CG: - ↓ WC - ↓ proportion of children consumed aerated drinks, unhealthy foods (burger/pizza/French fries/noodles) - ↑ proportion of children brought tiffin (packed lunch) and brought a fruit in their tiffin |
| India/2011 (Singhal et al. 47) |
cRCT 6 months |
2 134 (57/77) 15-17 years |
- Offering healthier foods - Stopping the sale of unhealthy foods - Promoting physical activity during the school day and after school |
- Lessons about healthy eating habits with students - Conducting a health camp with teachers and parents (nutritional counseling) - Counseling by phone for parents - Individual counseling with children held by a nutritionist |
Compared to CG: - ↓ WC |
| Indonesia/2022 (Kurniawan et al. 48) |
QE 5 months |
2 350 (196/164) 9-11 years |
- Training canteen staff - Training students’ peer leader club |
- Lessons about eating habits and physical activity with students - Promoting healthy home food weekly to be eaten together at school during recess - Training sessions with teachers - Involving parents in seminars (health promotion) - Sending communications (leaflets) to parents |
Compared to baseline: ↑ BMI (both groups, but higher in CG) Compared to CG: - ↑ eating fruits and vegetables behavior |
| Iran/2016 (Amini et al. 49) |
cRCT 18 weeks |
12 334 # (167/167) 10-12 years |
- Offering healthier foods - Stopping the sale of unhealthy foods - Increasing the amount of physical activity |
- Lessons about healthy eating habits with students - Involving parents in health classes at school |
Compared to CG: - ↓ BMI (z-score) Compared to baseline: - ↑ WC (both groups, but higher in CG) - ↑ energy, fat intake |
| Italia/2016 (Ermetici et al. 50) |
QE 2 years |
6 487 (225/262) 11-15 years |
- Replacing unhealthy foods with healthy foods and beverages in vending machines - Changing the regular curriculum - Hanging posters (healthy diet, water consumption, physical activity) - Providing a reusable water bottle - Creating more opportunities for exercise during breaks (an additional hour a week of movement) - Giving a pedometer to students |
- Lessons about healthy eating habits (textbook) with students - Sending communications (automated text messages) to parents and students - Involving parents in activities sent home (textbook) |
Compared to CG: - ↓ BMI (z-score) - ↓ SSB, high-energy snack consumption Intervention effect in subgroup analysis: - ↓ BMI (z-score) and high-energy snacks consumption in girls with overweight/obesity |
| Lebanon/2014 (Habib-Mourad et al. 51) |
cRCT 3 months |
8 374 (181/193) 9-11 years |
- Changing the regular curriculum - Training canteen staff (recommendations about healthy snacks and drinks) - Hanging posters (healthy food choices) in the school canteen |
- Lessons about healthy eating habits and physical activity (fun and interactive activities) with students - Training sessions with teachers - Involving parents in meetings, school events, and activities sent home (food samples, recipes, healthy lunch boxes) - Sending communications to parents (pamphlets) |
No significant differences |
| Malaysia/2018 (Koo et al. 52) |
QE 3 months |
2 83 # (40/43) 9-11 years |
- Changing availability of whole grain foods (delivered daily in school) |
- Lessons about whole grains recommendations and a balanced diet - Individual diet counseling for parents (booklet and recipes with whole grain foods) |
At 9 months follow-up, compared to CG: - ↓ BMI-for-age (z-score), %BF, WC At 3 months follow-up, compared to baseline: - ↓ %BF, WC |
| Malaysia/2021 (Teo et al. 53) |
QE 3 months |
6 523 (272/251) 7-11 years |
- Offering healthier foods - Training school canteen staff - Providing a skipping rope to students |
- Lessons about health awareness, nutrition, food hygiene, and physical activity with students - Training sessions with teachers - Involving parents in monitoring the program’s implementation (visit the school canteen) |
At 3 months follow-up, compared to CG: - ↓ BMI-for-age |
| Malaysia/2022 (Majid et al. 54) |
QE 4 weeks |
6 340 ## (93/247 ***) 14-15 years |
Intervention one + two: - Training school canteen staff - Giving a “Healthy Canteen Booklet” to school canteen staff Only intervention two: - Subsidy for healthy foods (fruits, vegetables, low-energy-dense kuih - traditional cake) - Students receive coupons that subsidize the price of healthy foods weekly - Allocation of funds to prepare healthy food was given to the school - Installing water fountains |
- Did not include this component |
Compared to baseline: - ↓ WC in intervention two - ↓ energy in all arms - ↑ fat intake and %BF in intervention one |
| Mexico/2009 (Colín-Ramirez et al. 55) |
cRCT 1 year |
10 619 (315/304) 8-10 years |
- Offering healthier foods - Creating more opportunities for exercise during the school day |
- Lessons about healthy eating habits and physical activity (classes and fun activities) with students - Training sessions with teachers - Involving parents in lectures and activities at home (menu and snack suggestions, recommendations for a healthy lifestyle) |
Compared to baseline: - ↓ energy and saturated fat intakes - ↑ WC in both groups (only significant in CG) |
| Mexico/2012 (Bacardí-Gascon et al. 56) |
QE 6 months |
4 532 (280 ###/252) 8-9 years |
- Offering healthier foods - Changing the regular curriculum |
- Lessons about healthy eating habits and physical activity with students and parents - Meetings with the school board and teachers (improve school meals, snacks offered in the school canteen, and physical activity installations) |
At 6 months follow-up, compared to CG: - ↓ BMI At 24 months follow-up, compared pre- to post-intervention: - ↑ BMI, BMI (z-score), WC - ↓ abdominal obesity (WC > 90th percentile) - ↑ vegetables intake, SSB - ↓ consumption of snacks high in fat and salt, availability of SSB, cookies, chocolates, candy, and vegetables at home |
| Mexico/2012 (Levy et al. 57) |
cRCT 6 months |
60 1,019 (510/509) 10 years |
- Offering healthier foods - Training school canteen staff - Hanging posters (healthy breaks) - Broadcasting of audio spots on the schools’ physical activity systems to promote the consumption of water, fruits, vegetables, and physical activity - Hanging posters (physical activity) - Providing a school guide (to support physical activity), a CD with music for established activities, and a bottle of water for the children - Organizing games during the break |
- Lessons about healthy eating habits and physical activity (workshops, puppet theatre) with students - Training sessions with teachers - Participation of teachers in games during the break - Teachers performing activities before the start of classes (warm-ups, activation and relaxation) - Delivery of recipe calendars (healthy eating and physical activity) to parents |
Compared to baseline: - ↓ probability of shifting from the overweight to the obesity category |
| Mexico/2013 (Alvirde-García et al. 58) |
cRCT 3 years |
5 2,682 (755/1,927) 9 years |
- Offering healthier foods - Meetings with school canteen staff - Changing the regular curriculum - Increasing the amount of time students spend in moderate-to-vigorous physical activity - Promoting physical activity during and after school (guide and activity cards) |
- Lessons about healthy eating habits and physical activity (textbook and workbook) with students and parents - Training sessions with teachers - Involving parents in meetings and activities at home |
At 3 years follow-up, compared to CG: - ↓ increase of BMI variation - ↓ energy, bread, fat and sugar intake At 3 years follow-up, compared to baseline: - ↓ energy in both groups (higher in IG) At 3 years follow-up, compared to 1 year follow-up: - ↑ BMI in both groups |
| Mexico/2013 (Safdie et al. 59) |
cRCT 1.5 years |
27 860 (354/506 ***) 9-11 years |
Group 1 + Group 2: - Increasing availability of healthy foods and water at school - Reducing availability of unhealthy foods - Training school canteen staff and school authorities (booklets, workshops) - Providing sports equipment - Promoting physical activity during the school day Only Group 2: - Increasing the amount of time students spend in moderate-to-vigorous physical activity - Additional financial investment and human resources (hiring physical education teachers) |
Group 1 + Group 2: - Promoting workshops, mass communication, and marketing strategies targeted to students (healthy eating habits) - Training sessions with teachers - Distributing a booklet for parents (healthy lunch) |
At 18 months follow-up, compared to CG: - ↓ consumption of unhealthy foods at school (only group 2) At 18 months follow-up, compared to baseline: - ↑ availability of healthy foods at school (both IG) - ↓ availability of unhealthy foods at school (both IG) |
| Netherlands/2007 and 2009 (Singh et al. 60,61) |
cRCT 8 months |
18 1,053 (453/600) 12-13 years |
- Offering smaller portion sizes - Offering healthier foods - Changing the regular curriculum - Restricting access to vending machines - Providing financial encouragement to schools to offer additional physical activity options |
- Biology and physical activity lessons with students - Training sessions with teachers |
At 8 months follow-up, compared to CG: - girls: ↓ SSB consumption - boys: ↓ WC, SSB consumption At 12 months follow-up, compared to CG: - girls: ↓ SSB consumption - boys: ↓ SSB consumption |
| Peru/2017 (Aparco et al. 62) |
QE 9 months |
4 824 (347/477) 6-10 years |
- Training school canteen staff - Promoting physical activity during the school recess - Providing sports equipment (balls, cones, ropes) |
- Lessons about healthy eating habits and physical activity (educational materials, puppet theatre) with students - Training sessions with teachers - Involving parents in lessons about healthy eating habits and physical activity and activities at home |
Compared to baseline: - ↓ vegetable consumption |
| Sweden/2009 (Marcus et al. 63) |
cRCT 4 years |
10 3,135 (1,465/1,670) 6-10 years |
- Offering healthier foods - Changing the regular curriculum - Increasing the amount of physical activity - Increasing opportunities for physical activity |
- Training sessions with teachers - Communicating with parents |
Compared to baseline: - Eating habits at home were healthier (↓ sweetened cereals, high-fat dairy, and sweet products) |
| Thailand/2017 (Chawla et al. 64) |
QE 6 months |
4 453 (227/226) 8-12 years |
- Offering healthier foods - Stopping the sale of unhealthy foods - Removing vending machines - Training sessions with school staff (comic book, discussions, handbook) and teachers - Requesting vendors around the school to stop selling unhealthy food |
- Lessons about healthy eating habits, obesity consequences, growing vegetables, and physical activity (presentations, gaming, gardening/planting, comic book) with students - Involving parents in workshops, activities sent home (healthy handbook), and sending communications (report cards, meetings) |
Compared to CG: - ↓ sugary foods (chocolate and candies), fast foods consumption - ↑ vegetables consumption |
| Turkey/2011 (Sevinç et al. 65) |
cRCT 8 months |
6 6,847 (2,926/3,921 ***) 7-13 years |
Group 1 + Group 2: - Offering healthier foods in the school canteen - Distributing boxed milk during mealtime |
Group 1 + Group 2: - Lessons about healthy eating and methods of preventing obesity Only in Group 1: - Lessons about physical activity |
Group 1 and Group 2, compared to CG: - ↑ BMI (lower than CG increased) - ↓ BMI increased in boys IG compared to CG Group 1, compared to CG and group 2: - ↓ BMI increased in boys compared to girls |
| United States/1996 and 1999 (Luepker et al. 66; Webber et al. 67; Nader et al. 68) |
cRCT 3 years |
96 4,019 # (1,653/2,366 **) 8-11 years |
Group 1 + Group 2: - Training school canteen staff - Changing the regular curriculum - Increasing the amount of time students spend in moderate-to-vigorous physical activity |
Group 1 + Group 2: - Lessons about healthy eating habits, cigarette smoking, and physical activity with students - Training sessions with teachers and physical education specialists Only in Group 1: - Involving parents in activities sent home and in school events |
At 3 years follow-up, Group 1 + Group 2, compared to CG: - ↓ % energy from total fat, saturated fat - ↑ total daily energy intake (both groups, but lower in IG) At 6 years follow-up, Group 1 + Group 2, compared to CG: - ↓ % energy from total fat and saturated fat intake |
| United States/2003 (Sallis et al. 69) |
cRCT 2 years |
24 1,678 (no data) 11-13 years |
- Offering healthier foods - Providing financial encouragement to purchase kitchen and physical activity equipment - Health policy meetings - Creating a committee - Promoting physical activity before and after school, as well as after lunch |
- Training sessions with teachers - Sending communications and involving parents in school events and meetings |
Compared to CG: - ↓ BMI only in boys |
| United States/2003 (Caballero et al. 70) |
cRCT 3 years |
41 1,704 (825/879) 8-10 years |
- Reducing the fat content of school meals - Training school canteen staff - Changing the regular curriculum - Increasing the amount of time students spend in moderate-to-vigorous physical activity - Promoting physical activity in the classroom |
- Lessons about healthy eating habits and physical activity with students - Training sessions with teachers - Communicating with and involving parents in school events |
Compared to CG: - ↓ % energy from fat (24-hR, and direct observation), total energy intake (only 24-hR, not by direct observation) |
| United States/2004 (Treviño et al. 71) |
cRCT 7 months |
27 1,419 (706/713) 9 years |
- Changing the regular curriculum - Training school canteen staff |
- Lessons about healthy eating habits and physical activity with students - Training sessions with teachers - Involving parents in events, meetings, and activities at home |
No significant differences |
| United States/2007 (Williamson et al. 72) |
cRCT 1.5 year |
4 661 (313/348 §) 7-11 years |
- Offering healthier foods - Eliminating vending machines - Reducing unhealthy foods - Training school canteen staff - Creating marketing materials (menu boards, buttons, place cards) and a committee - Hanging posters (physical activity) - Promoting physical activity during and after school - Providing financial encouragement to purchase physical activity equipment |
- Training sessions with teachers - Sending communications, creating a website, and involving parents in committee |
Compared to CG: - ↓ total calories, % of calories from total dietary fat, saturated fat |
| United States/2008 (Foster et al. 73) |
cRCT 2 years |
10 1,349 (600/749) 9-11 years |
- Offering healthier foods - Creating a committee - Training all school staff |
- Lessons about healthy eating habits and physical activity with students - Involving parents in committees, meetings, and nutrition workshops |
No significant differences |
| United States/2010 (Hollar et al. 74) |
QE 2 years |
5 3,769 (737/3,032) 6-13 years |
- Offering healthier foods - Reducing unhealthy foods - Changing the regular curriculum - Hanging health-related posters - Providing a school gardening program - Increasing opportunities for physical activity |
- Lessons about healthy eating habits and physical activity with students - Training sessions with teachers - Sending communications to parents (newsletter) |
At 2 years follow-up, compared to CG: - ↓ BMI (percentile) |
| United States/2010 (Hollar et al. 75) |
QE 2 years |
5 2,494 (465/2,029) 6-13 years |
- Offering healthier foods - Reducing unhealthy foods - Changing the regular curriculum - Hanging health-related posters - Providing a school gardening program - Increasing opportunities for physical activity |
- Lessons about healthy eating habits and physical activity with students - Training sessions with teachers - Sending newsletters to parents |
At 2 years follow-up, compared to CG: - girls: ↓ BMI (z-score) |
| United States/2010 (Foster et al. 76) |
cRCT 3 years |
42 6,358 (3,169/3,189) 11 years |
- Offering healthier foods - Reducing unhealthy foods - Increasing the amount of time students spend in moderate-to-vigorous physical activity - Providing financial encouragement to purchase physical activity equipment |
- Lessons about behavioral knowledge and skills with students - Training sessions with physical education teachers - Involving parents in activities sent home and sending communications |
Compared to CG: - ↓ BMI (z-score), % of students with WC (≥ percentile 90), % of students with BMI ≥ percentile 85 (both groups) |
| United States/2012 (Coleman et al. 77) |
cRCT 2 years |
8 579 (279/300) 7-11 years |
- Offering healthier foods - Reducing unhealthy foods - Training school canteen staff - Hanging health-related posters - Performing taste tests on students - School staff modeling healthy eating - Providing free meals for staff who eat school lunches with students |
- Lessons about healthy eating habits with students - Participation of teachers and parents in the development of action plans to change school environment - Meetings with parents |
Compared to baseline: - ↑ BMI (z-score) (both groups) |
| United States/2012 (Williamson et al. 78) |
cRCT 2 years + 4 months |
17 2,060 (587/1,473 ***) 9-11 years |
Group 1 + Group 2: - Offering healthier foods (vending machine and school canteen) - Reducing unhealthy foods - Training school canteen staff - Creating marketing materials (menu boards, buttons, place cards) - Creating a committee - Hanging posters (physical activity) - Promoting physical activity during the school day and after school - Providing financial encouragement to purchase physical activity equipment |
Group 1 + Group 2: - Training sessions with teachers - Sending communications, creating a website, and involving parents in committee Only Group 2: - Lessons about healthy eating habits with students - Internet counseling for children and their parents |
At 28 months follow-up, compared Group 1 + Group 2 to CG: - ↓ %BF in boys |
| United States/2016 (Bogart et al. 79) |
cRCT 5 weeks |
10 2,439 (1,261/1,178) 12-13 years |
- Offering healthier foods - Offering a greater variety of sliced/bite-sized food and freely chilled filtered water at lunch - Training with students’ peer leader club (social marketing: intervention messages at lunchtime, taste tests, short film) - Hanging health-related and physical activity posters and nutritional postings |
- Lessons about healthy eating habits and physical activity with students - Sending parent-student activities - Communicating with parents |
Compared to CG: - ↓ BMI (percentiles) in students who were classified as obese at baseline |
| United States/2021 (Davis et al. 80) |
cRCT 9 months |
16 3,135 (1,723/1,412) 8-10 years |
- Changing the regular curriculum - Creating a committee - Building gardens |
- Lessons about nutrition, gardening, and cooking with students - Involving parents in health classes at school |
Compared to CG: - ↑ vegetable intake |
| United States/2023 (Patel et al. 81) |
cRCT 15 months |
18 1,249 (572/677) 9 years |
- Installing water fountains in which cups were also available - Kickoff assembly - Signage and modest prizes for students observed drinking water at lunch |
- Lessons about health, fiscal, and environmental benefits of drinking water with students - Sending parent-student activities |
No significant differences |

 Impact of multi-component school food environment interventions on adiposity and food consumption in children and adolescents: systematic review and meta-analysis
Impact of multi-component school food environment interventions on adiposity and food consumption in children and adolescents: systematic review and meta-analysis Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail
 Thumbnail
Thumbnail

 95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation. * Boys’ values; ** Girls’ values.
95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation. * Boys’ values; ** Girls’ values.
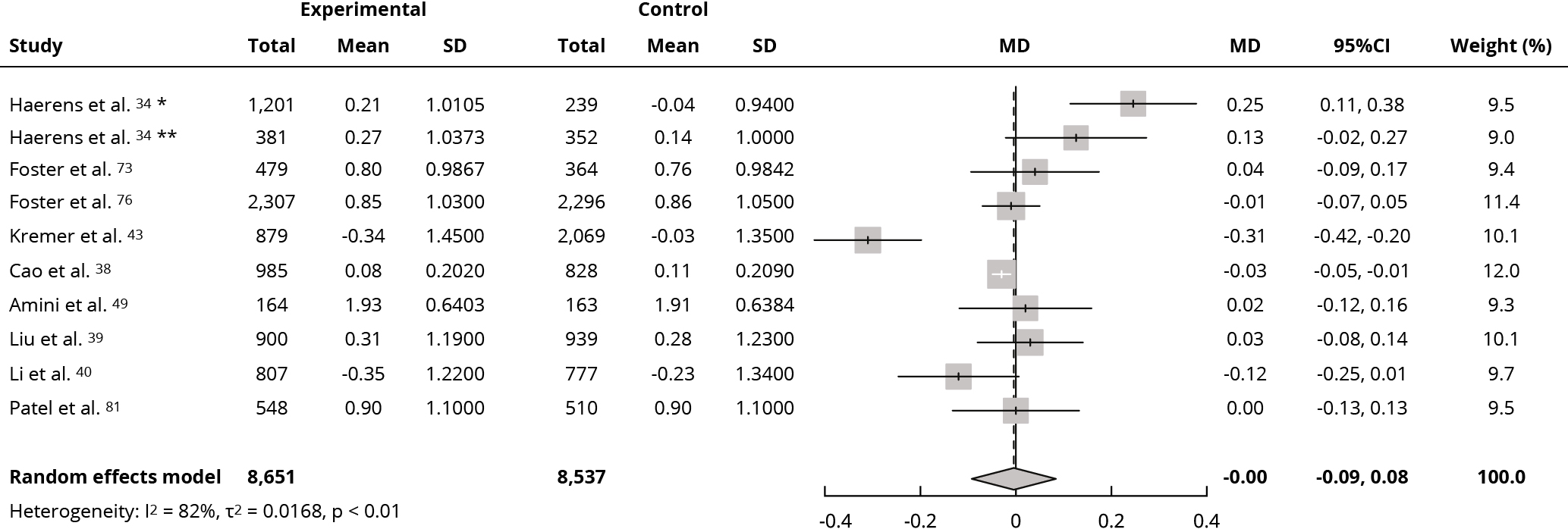 95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation. * Boys’ values; ** Girls’ values.
95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation. * Boys’ values; ** Girls’ values.
 95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation. * Boys’ values; ** Girls’ values.
95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation. * Boys’ values; ** Girls’ values.
 95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation.
95%CI: 95% confidence interval; MD: mean difference; SD: standard deviation.