Abstracts
INTRODUCTION: The main risk factors for hypertensive and ischemic cardiovascular disease of the metabolic syndrome (MS) can be favorably change by the life style (LS). OBJECTIVE: Evaluate the effect of a lifestyle modification program (LMP) on cardiovascular risk factors of the Metabolic Syndrome (MS). MATERIALS AND METHODS: In this clinical trial, 08 volunteers (05 women) with MS underwent a biweekly nutritional intervention and a physical exercise program, using a treadmill, at 65-75 % of maximum heart rate, during 30 minutes, three times a week. After tree mouths on LPM the data were compared using Student's t-test. RESULTS: There was a dramatic reduction in systolic blood pressure (-7.5%), triglycerides (-6.7%) and high density lipoprotein (-8%). Moreover, there was a reduction in resting double product (-11%) and an increase in physical conditioning expressed by the workload in watts (29%), as well as in the oxygen consumption (24%). CONCLUSION: Until this moment, these results indicate that food habits change, associated to frequently physical exercise can reduce the triglycerides concentration as well as SBD and DP. Besides, since the relevance of the results obtained at the end of the program, we believe that the continuity of the activities proposed by this study can benefit other individuals with MS.
Risk factors; Lifestyle; Food habits; Physical exercise; Metabolic syndrome
INTRODUÇÃO: Os principais fatores de risco para as doenças cardiovasculares hipertensivas e isquêmicas da síndrome metabólica (SM) podem ser favoravelmente modificados pelo estilo de vida (EV). OBJETIVO: Avaliar o efeito de um programa de modificação do estilo de vida sobre os fatores de risco cardiovascular de voluntários com síndrome metabólica (SM). MATERIAIS E MÉTODOS: Ensaio clínico em que oito voluntários (cinco mulheres) com diagnóstico de SM foram submetidos, ao longo de três meses, à intervenção nutricional quinzenal e a um programa de exercício físico, realizado em esteira rolante com intensidade de 65% a 75% da frequência cardíaca máxima, com duração de 30 minutos, três vezes por semana. Após o programa os dados foram comparados pelo teste t de Student. RESULTADOS: Houve redução significativa da pressão arterial sistólica (-7,5%), triglicerídeos (-6,7%) e lipoproteínas de alta densidade (-8%). Além disso, o índice de trabalho cardíaco avaliado em repouso reduziu significativamente (-11%), ao passo que o condicionamento físico expresso pelo trabalho muscular e consumo de oxigênio aumentaram significativamente (29% e 24%, respectivamente). CONCLUSÃO: Até o momento, esses resultados indicam que a mudança nos hábitos alimentares associados à prática regular de exercício físico pode reduzir beneficamente as concentrações de triglicerídeos, bem como a PAS e o DP. Além disso, devido à relevância dos resultados obtidos ao final do programa, acredita-se que a continuidade das atividades propostas neste estudo possa beneficiar outros indivíduos com SM.
Fatores de risco; Estilo de vida; Hábitos alimentares; Exercício físico; Síndrome metabólica
ORIGINAL ARTICLES
Benefits of lifestyle modification on the metabolic syndrome
Luiza Armani ValmorbidaI; Alice Carvalho BorsattoII; Ana Maria FeoliIII; Maria Terezinha AntunesIV; Márcia Koja BreigeironV; Fabrício Edler MacagnanVI
IPhysiotherapist, graduated from the Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS -Brazil, e-mail: luizavalmorbida@gmail.com
IIPhysiotherapist, graduated from the Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS -Brazil, e-mail: aliceborsatto@gmail.com
IIINutritionist, PhD in Biological Sciences (Biochemistry) from the Universidade Federal do Rio Grande do Sul (UFRGS) and lecturer at the PUCRS, Porto Alegre, RS -Brazil, e-mail: anamariafeoli@hotmail.com
IVNutritionist, PhD in Biomedical Gerontology from the PUCRS and lecturer at the Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, RS -Brazil, e-mail: mtantunes@ufcspa.edu.br
VNurse, PhD in Biological Sciences (Physiology) from the UFRGS and lecturer at the UFRGRS, Porto Alegre, RS – Brazil, e-mail: mbreigeiron@gmail.com
VIPhysiotherapist, PhD in Health Sciences from the PUCRS and lecturer at the Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, RS -Brazil, e-mail: fabriciom@ufcspa.edu.br
ABSTRACT
INTRODUCTION: The main risk factors for hypertensive and ischemic cardiovascular disease of the metabolic syndrome (MS) can be favorably change by the life style (LS).
OBJECTIVE: Evaluate the effect of a lifestyle modification program (LMP) on cardiovascular risk factors of the Metabolic Syndrome (MS).
MATERIALS AND METHODS: In this clinical trial, 08 volunteers (05 women) with MS underwent a biweekly nutritional intervention and a physical exercise program, using a treadmill, at 65-75 % of maximum heart rate, during 30 minutes, three times a week. After tree mouths on LPM the data were compared using Student's t-test.
RESULTS: There was a dramatic reduction in systolic blood pressure (-7.5%), triglycerides (-6.7%) and high density lipoprotein (-8%). Moreover, there was a reduction in resting double product (-11%) and an increase in physical conditioning expressed by the workload in watts (29%), as well as in the oxygen consumption (24%).
CONCLUSION: Until this moment, these results indicate that food habits change, associated to frequently physical exercise can reduce the triglycerides concentration as well as SBD and DP. Besides, since the relevance of the results obtained at the end of the program, we believe that the continuity of the activities proposed by this study can benefit other individuals with MS.
Keywords: Risk factors. Lifestyle. Food habits. Physical exercise. Metabolic syndrome.
Introduction
Metabolic syndrome (MS) is a clinical condition defined by the association of several cardiovascular risk factors, which, when present, increase overall mortality one and a half times and mortality from cardiovascular causes two and a half times (1.2). Two factors are closely related to the development of MS: abdominal obesity and insulin resistance (1, 2). In the United States, the prevalence of MS, when adjusted for age, is 27% (3). In Brazil, the prevalence of MS has not been precisely determined, nevertheless it is estimated that approximately 30% of Brazilians are obese (4).
Thus, there is a clear association between excess weight and the development of MS (5), to the degree that waist circumference is part of the criteria established by both the World Health Organization (WHO), and the National Cholesterol Evaluation Program for Adult Treatment Panel III (ATP III) for MS diagnosis (6). The treatment of the SM consists primarily of modifying cardiovascular risk factors, such as reducing body weight and waist circumference, normalizing dyslipidemia, reducing blood pressure (BP) and improving glycemic control. Hence, the practice of regular exercise and the modification of food habits, along with pharmacological strategies, play a central role in the treatment and prevention of MS (6).
In addition, diets that include fish oils, which are rich in fatty acids and omega-3, are useful in reducing plasma levels of triglycerides and very low density lipoproteins (VLDL), especially in the postprandial state. Epidemiological studies show that the intake of fatty acids and omega-3 are associated with reduced cardiovascular risk mainly by reducing the inflammatory status and platelet aggregation. The use of omega-3 also acts in the control of blood pressure by increasing the bioavailability of nitric oxide and improving endothelial function. However, its effect on insulin resistance remains unclear (7, 8).
In addition, maintenance of good physical fitness acts favorably on the cardiovascular risk factors that comprise the diagnosis of MS by improving insulin sensitivity and thus reducing the risk of developing type II diabetes mellitus and coronary artery disease (CAD) (9). It has recently been demonstrated that obese individuals with high functional capability, as shown by peak oxygen consumption (VO ), have lower plasma concentrations of low density lipoproteins (LDL), higher concentrations of high density lipoprotein (HDL) and lower BP values (10). Besides the improvement in dyslipidemia and the reduction in BP, obese individuals can benefit from the practice of regular exercise due to the reduction of inflammatory markers related to central obesity (11).
Previous data have also shown that regular aerobic exercise can reduce blood pressure by 06 to 10 mmHg, in both previously sedentary men and women. Thus, regular exercise can also help to control BP in the case of the risk of hypertension and reduce the mortality rate of physically fit hypertensive individuals, when compared to their normotensive counterparts (12). With the reduction in BP, there is also a reduction in cardiac work index represented by the double product (DP) (13), which is extremely beneficial in cases of overweight and insulin resistance, which are commonly seen in MS (14,15).
Although the cardioprotective effect associated with the practice of regular exercise has been widely described in the literature, the mechanisms by which exercise acts on MS remain unclear (15). However, it is known that this effect can be favorably amplified by the association of interventions involving nutritional re-education (6-8). Therefore, the aim of this study was to evaluate the effect of a program involving a change in lifestyle that includes dietary intervention and regular exercise on cardiovascular risk factors in subjects with MS.
Materials and methods
This study is a non-controlled clinical trial with a single-arm, which was conducted by the MERC (modificação do estilo de vida e risco cardiovascular - lifestyle and cardiovascular risk modification) research group. This group involves the participation of the college of nutrition nursing and physiotherapy (FAENFI), the college of pharmacy (FAFARM), college of psychology (FAPSI) and the college of biosciences (FABIO), at the Pontifical Catholic University of Rio Grande do Sul (PUCRS).
The sample consisted of 8 volunteers (5 women) diagnosed with MS (Table 1), from the cardiology outpatient clinic at the Hospital São Lucas (HSL) of PUCRS.
The study volunteers, aged between 30 and 59 years, had 03 or more of the following findings (according to the Brazilian Guidelines for Diagnosis and Treatment of Metabolic Syndrome ATP III) (6): waist circumference > 88 cm for women and > 102 cm for men; systolic blood pressure (SBP) > 130 mmHg and diastolic blood pressure (DBP) > 85 mmHg; fasting glucose > 110 mg/dl; triglycerides > 150 mg/dL, HDL cholesterol <40 mg/dL for men and <50 mg/dL for women.
Subjects who had one or more of the following: absolute contraindication to physical activity due to musculoskeletal, neurological, vascular, pulmonary and/or cardiac problems; users of oral hypoglycemic agents, users of hypolipidemic agents; those practicing regular physical activity (30 minutes two or more times per week); and those unable to return and undergo monitoring were excluded.
Data collection was performed following the approval of the study protocol by the Scientific Committee of FAENFI and Ethics Committee of PUCRS (CEP) under the registration number: 0603024. All the volunteers read and signed the Free Informed Consent Form.
Assessments
After the screening, performed at the cardiology outpatient clinic, volunteers were sent to the Centre for Rehabilitation (CR) of HSL-PUCRS where the preand post-MERC research participation assessments were scheduled.
Assessment of the biochemical markers of cardiovascular risk involved the following procedures: Blood collection performed in the morning between 8:30 am and 9:30 am during a 10h to 12h of period of fasting; analysis of total cholesterol (TC) performed based on the enzymatic method proposed by Allain et al. (16). For the high density lipoprotein (HDL) cholesterol, the technique was based on a method of precipitating non-HDL-cholesterol similar to that used by Burstein et al. (17 ) followed by enzymatic detection similar to that proposed by Allain et al. (16). Triglyceride analysis was based on an enzymatic method described by Spayd et al. (18). Glucose analysis was performed based on the method previously described by Trinder (19) and Curme et al. (20). The glucose, total cholesterol, HDL and triglyceride concentrations were obtained using reflectance spectrophotometry. All analyzes were performed at the Biochemistry Laboratory of the HSL-PUCRS.
The anthropometric assessment involved measuring the weight, height, body mass index (BMI) and waist circumference (WC) of the participants. Weight was measured with a suitably calibrated electronic scale (Plena®), while a wall stadiometer (Welmy®) was used to obtain the height. The BMI was calculated using the formula: BMI=weight (kg)/height (m)2.
The BP and heart rate (HR) measurements were taken after five minutes of rest and during walking sessions, at 15 and 30 minutes. BP was measured using an aneroid sphygmomanometer (Taycos®). HR was measured on a heart monitor (Polar®). The cardiac work index, as represented by the double product (DP), was calculated using the formula: DP = SBP (mmHg) x HR (Bpm).
Oxygen uptake (VO2) was estimated based on prediction equations originally proposed by Balk (21) and currently described in the Guidelines of the American College of Sports Medicine for Stress Testing and its Prescription (22). According to Balk, the relative oxygen uptake (expressed as ml.kg.min-1) is given by the following equation: VO2= Speed x 0.1 + 3.5 (walking on a flat surface) and VO2 = % slope x 100-1 x speed x 1.8 (walking on a sloping surface), where the speed must be given in meters per second (m/s) and the slope is given in percentage of vertical displacement relative to horizontal displacement. These estimates were made during the physical exercise at the beginning and end of the program.
The muscular workload (Watts-W) was determined by means of the equation proposed by Foss & Keteyian (23) using the international system of units (IS), where 01 liters of oxygen consumed per minute is equal to 351.91 W. Thus, the relative VO2 (ml.kg.min-1) estimated for a walk on a flat/sloped surface was transformed into absolute VO2 (liters/min) (= relative VO2 x body weight). These estimates were made during exercise sessions held at the beginning and end of the program.
The Lifestyle Modification Program Proposed in the MERC Research
After the initial assessments, the volunteers started the activities proposed in the MERC research. The lifestyle modification protocol consisted of a regular exercise program and nutritional intervention as described below.
Physical exercise
The exercise sessions were performed on an electric treadmill, for continuous 30 minutes, 03 times a week, at a speed and grade sufficient to maintain the HR within the range of 65% to 75% of the maximum HR predicted for the age (220-age), as recommended in the Brazilian Guideline for the Diagnosis and Treatment of Metabolic Syndrome (6). In cases where the HR did not reach the established range the load was increased by increasing the grade on the treadmill. Thus the workload combined speed and grade which were adjusted daily throughout the program in order to maintain the HR within the limits prescribed for physical exertion. The participants performed 10 minutes of stretching before and immediately after each exercise session.
Nutritional intervention
This consisted of nutritional counseling, which involved an individualized dietary plan and fortnightly sessions with weight evaluation and monitoring of adherence to the diet. In each of the sessions, topics such as healthy eating, food labeling, trans fats, functional food, food pyramid, sodium intake; the five-a-day program; substitute foods were addressed and any doubts were clarified. Monitoring the diet consisted of enquiring about the difficulties encountered by the patient in adhering to the arrangements agreed during the previous consultation as well as following the proposed dietary plan. The dietary plan was designed to be low calorie, normolipidemic and hyposodic. In addition, the volunteers took a daily supplement of omega-3 fatty acids (3g/per day of fish oil).
Data Analysis
The data were presented as mean and standard deviation of the mean. The effects of the lifestyle modification program on the variables were evaluated using the Student's t test for paired averages because in the Kolmogorov-Smirnov normality test the data showed a Gaussian distribution and were therefore classified as parametric. The cutoff point used to determine the statistical difference was p <0.05. The statistical analysis was conducted with the aid of SPSS, version 17.0.
Results
The lifestyle modification program proposed in this study was shown to have a positive and significant effect by reducing plasma concentrations of triglycerides (6.7%) and SBP at rest (7.5%). In addition, there was also beneficial, although slight, and non-significant reduction in weight (2.7%), BMI (4.2%) and WC (3.3%). However, the values for both serum concentration of TC and DBP remained virtually unchanged (-0.8%) and (0.2%), respectively. Moreover, contrary to expectations, there was a discreet and nonsignificant increase in fasting glucose (2%), while HDL cholesterol was significantly reduced (8%) after the program (Table 1).
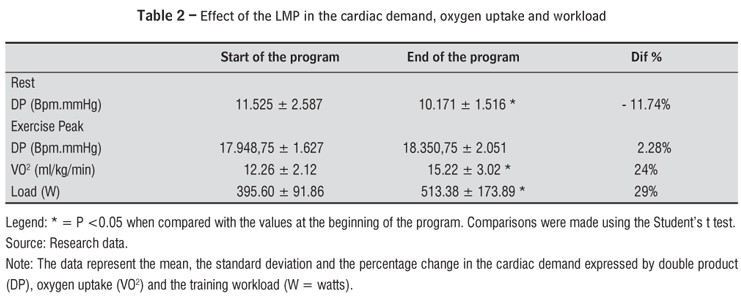
Regarding the cardiac demand, it can be seen (Table 2) to be significantly reduced at rest (-11.7%), while the estimated oxygen uptake during the training session, as well as the workload used during the training sessions increased significantly by the end of the program (24% and 29%, respectively). Interestingly, the rate of cardiac work assessed during exercise in the training session, remained virtually unchanged (2.2%).
Discussion
The analysis shows that the lifestyle modification program that combines biweekly nutritional counseling with regular exercise, which was prepared from the minimum recommendations outlined in First Brazilian Guidelines for the Diagnosis and Treatment of MS (6) is able to significantly reduce plasma levels of triglycerides, as well as the SBP. These findings indicate that lifestyle modification can produce beneficial effects in the management of MS, even in a relatively short period.
The association of regular exercise with nutritional counseling and the intake of omega-3, as recommended in this study, led to a decrease in triglycerides at a rate of 2.2 % per month. Maintenance of this rate for further six months would probably allow more volunteers to achieve the goal established by ATP III (>150 mg/dL) ( 6 ). As demonstrated by Phillipson (24), a single session of exercise can significantly decrease triglyceride levels, but this effect is brief and quickly reversed (48 hr). This reinforces the need for frequent exercise when the aim is to combat dyslipidemia. In addition to the effect of physical exercise, Phillipson (24) and Friedberg (25) showed that plasma concentrations of triglycerides may also be favorably reduced by dietary intake of omega-3. Thus, combining regular physical exercise with healthy eating habits can enhance the reduction of triglycerides, but the normalization of the values will depend on the magnitude of the initial alteration since the monthly rate of reduction is relatively small. This also implies there is a chance of failure in severe cases of hypertriglyceridemia, in which case the need for drug intervention should be evaluated.
The proposed lifestyle modification intervention employed in the present study led to a reduction in SBP of 7.55 mmHg in only 03 months. The results of this study are consistent with those reported by Cook (26) and more recently in the 5th edition of the Brazilian Guidelines on Hypertension (27), where the lifestyle modification produced a significant reduction in SBP. This underlines the assertion contained in the 5th edition of the Brazilian Guidelines on Hypertension (27) that attributes exercise and dietary planning a grade 'A' recommendation for the control and treatment of hypertension, where reductions of 9 mmHg in SBP and 4 mmHg in DBP are expected with exercise and a reduction of up to 14 mmHg in SBP is expected with improved dietary habits.
However, the benefits of lifestyle modification observed in this study do not appear to be directly related to loss of body weight because the magnitude of the weight loss was small and non-significant, being less than 1 % per month. Although weight monitoring is a relatively simple task, achieving an adequate and continuous loss of weight is a great challenge for practicing nutritionists. The weight monitoring conducted throughout this study (data not shown) showed considerable fluctuations in values. One hypothesis suggests the possible conversion of fat into muscle tissue. In any case, evaluation of weight body alone does not reflect the actual composition of the volunteers. Thus, there is no way to infer whether or not there was a gain in lean mass, and if that was the reason why overall body weight was not significantly reduced. It is important to point out that, due to the predominantly aerobic nature of the exercise program, no significant increase in lean body mass was expected but rather a reduction in fat mass. In a certain way, the rate of reduction in the circumference of the waist was apparently higher than that of the weight. This slight disparity between the reduction in WC in relation to that of body weight may be an indication that the lifestyle modification tended to reduce central adiposity, but these results do not, as yet, allow an effective conclusion to be drawn. However, as described by Rocha (28) one cannot rule out the possibility that the maintenance of body weight occurred, at least in part, due to a gain in lean mass or as a reflection of poor adherence to diet.
As expected, during the exercise sessions there was a constant adjustment in workload. Thus, both the speed and the grade of the treadmill were constantly and progressively incremented to maintain the target HR within the desired range. The importance of these findings is clinically consistent, since, according to Lacour (29), high levels of physical activity are associated with lower cardiovascular risk in both adults and in the elderly. This implies that energy consumption is of great importance in preventing cardiovascular problems and, in our study, the workload increased significantly (29%) indicating that the exercise intensity used (65-75% of the maximum HR predicted for the age) can be considered effective for the improvement of the functional capacity of volunteers with MS.
Another important finding in this study concerns the significant reduction (11%) in cardiac demand at rest. This reinforces the findings published by Cook in 1995 (26), which, at that time, demonstrated the importance of reducing cardiac work in the primary prevention of cardiovascular complications.
On the other hand, the exercise-peak DP did not alter by the end of the program. This is also important because the workload at peak exercise was 29% higher. Thus, it can be assumed that these benefits have been extended also to the activities of daily living, where lower demands on the heart during daily routine activities can also be expected. In part, the reduction of DP can be explained by the Fick equation, since according to Whelton and colleagues (14), enhanced aerobic capacity increases muscle oxygen extraction and extends the arteriovenous oxygen difference thereby reducing the cardiac demand during constant effort. However, in this study, the DP was assessed during a physical activity with a variable load, the only variable that was maintained being the HR, while the speed and slope of the treadmill were constantly adjusted. Therefore, the DP was unaltered at the end of the program, because the HR and SBP remained practically constant, even with the progressive increase of muscle workload during the sessions.
Regarding fasting glucose, there was no significant change at the end of this study. Grundy et al. (30) describe that proper lifestyle modification programs are effective in significantly reducing fasting glucose levels and improving insulin resistance. However, the mean blood glucose values found in this study were within the normal range and, probably for this reason, were not significantly altered. On the other hand, the plasma concentrations of HDL-cholesterol decreased instead of increasing. This contrasts with the findings reported by Perseghin (31), but this reduction may well have occurred because of the decrease in total intake of lipids. However, without specific control of the cholesterol intake that discussion is limited. Nonetheless, this information should serve as an alert to other studies that aim to evaluate the effect of exercise and nutritional intervention on plasma HDL-cholesterol.
Together these results indicate that dietary changes associated with regular exercise can beneficially reduce the concentrations of triglycerides and the cardiac demand in rest and during the physical activity. Moreover, due to the relevance of the results obtained at the end of the program, it is believed that the continuity of the activities proposed in this study may benefit other individuals with MS.
References
- 1. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto JT, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288(21):2709-16.
- 2. Ford ES, Giles WH. A comparison of the prevalence of the metabolic syndrome using two proposed definitions. Diabetes Care. 2003;26(3):575-81.
- 3. Haffner S, Taegtmeyer H. Epidemic obesity and the metabolic syndrome. Circulation. 2003;108(13):1541-5.
- 4. Guimarães HP, Avezum A, Piegas LS. Obesidade abdominal e síndrome metabólica Rev Soc Cardiol Estado de São Paulo. 2006;16(1):41-7.
- 5. Girman CJ, Rhodes T, Mercuri M, Pyörälä K, Kjeshus J, Pedersen TR, et al. The metabolic syndrome and risk of major coronary events in the Scandinavian Simvastatin Survival Study (4S) and the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/ TexCAPS). Am J Cardiol. 2004;93(2):136-41.
- 6. Brandão AP, coordenador. I Diretriz Brasileira para diagnóstico e tratamento da síndrome metabólica. Arq Bras Cardiol. 2005;84(Supl. 1):1-28.
- 7. Pitsavos C, Panagiotakos DB, Chrysohoou C, Papaioannou I, Papadimitriou L, Tousoulis D, et al. The adoption of Mediterranean diet attenuates the development of acute coronary syndromes in people with the metabolic syndrome. Nutr J. 2003;2:1.
- 8. Kris-Etherton PM, Harris WS, Appel LJ; American Heart Association. Nutrition Committee. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002; 19;106(21):2747-57.
- 9. Franks PW, Ekelund U, Brage S, Wong MY, Wareham NJ. Does the association of habitual physical activity with the metabolic syndrome differ by level of cardiorespiratory fitness? Diabetes Care. 2004;27(5):1187-93.
- 10. Lee S, Kuk JL, Katzmarzyk PT, Blair SN, Church TS, Ross R. Cardiorespiratory fitness attenuates metabolic risk independent of abdominal subcutaneous and visceral fat in men. Diabetes Care. 2005;28(4):895-901.
- 11. Pischon T, Hankinson SE, Hotamisligil GS, Rifai N, Rimm EB. Leisure-time physical activity and reduced plasma levels of obesity-related inflammatory markers. Obes Res. 2003;11(9):1055-64.
- 12. McArdle WD. Fisiologia do exercício: nutrição, energia e desempenho humano. 4. ed. Rio de Janeiro: Guanabara Koogan; 1998.
- 13. Wilmore JH, Costil DL. Physiology of sport and exercise. 2nd ed. Champaign: Human Kinetics; 1999.
- 14. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a metaanalysis controlled trials. Ann Intern Med. 2002;136(7):493-503.
- 15. Tompson PD, Crouse SF, Goodpaster B, Kelley D, Moyna N, Pescatello L. The acute versus the chronic response to exercise. Med Sci Sports Exerc. 2001;33(Suppl. 6):S438-45.
- 16. Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total cholesterol in serum. Clin Chem. 1974;20(4):470-5.
- 17. Burstein M, Scholnick HR, Morfin R. Rapid method for the isolation of lipoproteins from human serum by precipitation with polyanions. J. Lipid Reserch. 1970;11(6):583-95.
- 18. Spayd RW, Bruschi B, Burdick BA, Dappen GM, Eikenberry JN, Esders TW, et al. Multilayer film elements for clinical analysis: applications to representative chemical determinations. Clin Chem. 1978;24(8):1343-50.
- 19. Trinder P. Determination of glucose in blood using glucose oxidase with an alternative oxygen receptor. Ann Clin Biochem. 1969;6:24-27.
- 20. Curme HG, Columbus RL, Dappen GM, Eder TW, Fellows WD, Figueras J, et al. Multilayer film elements for clinical analysis. Clin Chem. 1978;24(8):1335-1342.
- 21. Tebexreni AS, Lima EV, Tambeiro VL, Cemafe TLBN. Protocolos tradicionais em ergometria, suas aplicações práticas versus protocolo de rampa. Rev Soc Cardiol. 2001; 11(3):519-28.
- 22. American College of Sports Medicine. Manual de pesquisa do ACSM para os testes de esforço e sua prescrição. 4. ed. Rio de Janeiro: Guanabara Koogan; 2003.
- 23. Foss ML, Keteyian SJ. Bases fisiológicas do exercício e do esporte. 6. ed. Rio de Janeiro: Guanabara Koogan, 2000.
- 24. Phillipson BE, Rothrock DW, Connor WE, Harris WS, Illingworth DR. Reduction of plasma lipids, proteins, and apoproteins by dietary fish oils in patients with hypertriglyceridemia. N Engl J Med. 1985;312(19):1210-6.
- 25. Friedberg CE, Janssen MJEM, Heine RJ, Grobbee DE. Fish oil and glycemic control in diabetes: a meta-analysis. Diabetes care. 1998;21(4):494-500.
- 26. Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701-9.
- 27. Mion D Junior, coordenador. V Diretriz Brasileira de Hipertensão. Arq Bras Cardiol. 2007;89(3):e24-e79.
- 28. Rocha NP, Catania AS, Barros CR, Pires MM, Folchetti LD, Ferreira SRG. Análise de diferentes medidas antropométricas na identificação de síndrome metabólica, com ou sem alteração do metabolismo glicídico. Arq. Bras Endocrinol Metab. 2010;54(7):636-43.
- 29. Lacour JR. Lipid metabolism and exercice. Rev Prat. 2001;51(Suppl. 12):36-41.
- 30. Grundy SM, Cleeman JI, Merz NB, Brewer HB, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227-39.
- 31. Perseghin G, Price TB, Petersen KF, Roden M, Cline GW, Gerow K, et al. Increased glucose transport-phosphorylation and muscle glycogen synthesis after exercise training in insulin-resistant subjects. N Engl J Med. 1996;335(18):1357-62.
Publication Dates
-
Publication in this collection
03 Feb 2014 -
Date of issue
Dec 2013
History
-
Received
29 Sept 2011 -
Accepted
26 Sept 2013