Abstracts
INTRODUCTION: Dysmorphic red blood cells (RBCs) in the urine are a strong indicator of a glomerular bleeding source. RBC casts, which while generally following RBC dysmorphism are not frequently seen on routine urinalysis, are also important indicators of glomerular hematuria. OBJECTIVE: This study tested the superiority of a urine concentration technique (CT) over the standard method (SM) for RBC cast identification in a group of patients suspected of glomerular hematuria. MATERIAL AND METHODS: Of a total of 4,227 routine urinary samples, 249 with dysmorphic hematuria were selected. The samples were processed according to two techniques: standard method (SM) and concentration technique (CT). The percentages of RBC cast identification according to each method were compared. RESULTS: The CT showed a higher rate of RBC casts (52.6%) compared to the SM (8.4%) (p < 0.001). DISCUSSION AND CONCLUSION: We suggest that the SM did not sufficiently concentrate the urine sample, the RBC casts remaining in the supernatant and being discarded. The CT increased the sensitivity of the RBC cast yield. The CT, associated with the presence of RBC dysmorphism, was useful to increase the agreement of the two parameters used for identification of glomerular-based bleeding and the diagnosis of glomerular diseases, important causes of chronic kidney disease.
Urinary sediment; Dysmorphic red blood cells; Red blood cell casts; Glomerular hematuria; Glomerulonephritis
INTRODUÇÃO: A presença de hemácias dismórficas na urina é um forte indicativo da origem glomerular do sangramento, sendo uma ferramenta importante no diagnóstico de glomerulonefrites. Os cilindros hemáticos geralmente acompanham as hemácias dismórficas, sendo também fortes indicadores de hematúria glomerular, embora não sejam encontrados com frequência no exame parcial de urina. OBJETIVO: Comparar duas técnicas de concentração de amostras em uma série de exames de urina com hematúria dismórfica. MATERIAL E MÉTODOS: Foram selecionadas 249 amostras com hematúria dismórfica a partir de 4.277 amostras de urina de rotina. As amostras foram processadas utilizando-se duas técnicas: a convencional e a de concentração. O percentual de identificação dos cilindros hemáticos foi comparado de acordo com a metodologia utilizada. RESULTADOS: A presença de cilindros hemáticos pela técnica de concentração foi estatisticamente maior (52,6%) em comparação com a positividade pela metodologia convencional (8,4%) (p < 0,001). DISCUSSÃO E CONCLUSÃO: Sugere-se que a técnica convencional não concentrou suficientemente a amostra de urina e os cilindros hemáticos ficaram no sobrenadante, sendo descartados. A utilização da técnica de concentração aumentou a sensibilidade técnica para a pesquisa dos cilindros hemáticos. Portanto, a técnica de concentração, associada à presença de hemácias dismórficas, mostrou-se útil para aumentar a concordância dos dois parâmetros laboratoriais para a detecção da hematúria de origem glomerular como auxílio diagnóstico das glomerulopatias, importante causa de doença renal crônica.
Sedimento urinário; Dismorfismo hemático; Cilindros hemáticos; Hematúria glomerular; Glomerulonefrite
ORIGINAL ARTICLES
Carmen Antonia Sanches ItoI; Roberto Pecoits-FilhoII; Larissa BailI; Mônica Arcoverde WosiackI; Danieli AfinoviczI; Aline Borsato HauserIII
IUniversidade Estadual de Ponta Grossa - UEPG
IICentro de Ciências Biológicas e da Saúde da Pontifícia Universidade Católica do Paraná - PUC/PR
IIIUniversidade Federal do Paraná - UFPR
Correspondence to
ABSTRACT
INTRODUCTION: Dysmorphic red blood cells (RBCs) in the urine are a strong indicator of a glomerular bleeding source. RBC casts, which while generally following RBC dysmorphism are not frequently seen on routine urinalysis, are also important indicators of glomerular hematuria.
OBJECTIVE: This study tested the superiority of a urine concentration technique (CT) over the standard method (SM) for RBC cast identification in a group of patients suspected of glomerular hematuria.
MATERIAL AND METHODS: Of a total of 4,227 routine urinary samples, 249 with dysmorphic hematuria were selected. The samples were processed according to two techniques: standard method (SM) and concentration technique (CT). The percentages of RBC cast identification according to each method were compared.
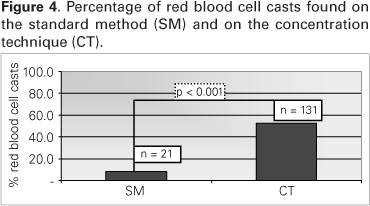
RESULTS: The CT showed a higher rate of RBC casts (52.6%) compared to the SM (8.4%) (p < 0.001).
DISCUSSION AND CONCLUSION: We suggest that the SM did not sufficiently concentrate the urine sample, the RBC casts remaining in the supernatant and being discarded. The CT increased the sensitivity of the RBC cast yield. The CT, associated with the presence of RBC dysmorphism, was useful to increase the agreement of the two parameters used for identification of glomerular-based bleeding and the diagnosis of glomerular diseases, important causes of chronic kidney disease.
Keywords: Urinary sediment. Dysmorphic red blood cells. Red blood cell casts. Glomerular hematuria. Glomerulonephritis.
RESUMO
INTRODUÇÃO: A presença de hemácias dismórficas na urina é um forte indicativo da origem glomerular do sangramento, sendo uma ferramenta importante no diagnóstico de glomerulonefrites. Os cilindros hemáticos geralmente acompanham as hemácias dismórficas, sendo também fortes indicadores de hematúria glomerular, embora não sejam encontrados com frequência no exame parcial de urina.
OBJETIVO: Comparar duas técnicas de concentração de amostras em uma série de exames de urina com hematúria dismórfica.
MATERIAL E MÉTODOS: Foram selecionadas 249 amostras com hematúria dismórfica a partir de 4.277 amostras de urina de rotina. As amostras foram processadas utilizando-se duas técnicas: a convencional e a de concentração. O percentual de identificação dos cilindros hemáticos foi comparado de acordo com a metodologia utilizada.
RESULTADOS: A presença de cilindros hemáticos pela técnica de concentração foi estatisticamente maior (52,6%) em comparação com a positividade pela metodologia convencional (8,4%) (p < 0,001).
DISCUSSÃO E CONCLUSÃO: Sugere-se que a técnica convencional não concentrou suficientemente a amostra de urina e os cilindros hemáticos ficaram no sobrenadante, sendo descartados. A utilização da técnica de concentração aumentou a sensibilidade técnica para a pesquisa dos cilindros hemáticos. Portanto, a técnica de concentração, associada à presença de hemácias dismórficas, mostrou-se útil para aumentar a concordância dos dois parâmetros laboratoriais para a detecção da hematúria de origem glomerular como auxílio diagnóstico das glomerulopatias, importante causa de doença renal crônica.
Palavras-chave: Sedimento urinário. Dismorfismo hemático. Cilindros hemáticos. Hematúria glomerular. Glomerulonefrite.
INTRODUCTION
The presence of dysmorphic red blood cells (RBCs) in the urine is a strong indicator of a glomerular source for the bleeding, being an important tool for the diagnosis of glomerulonephritides. In addition, the presence of RBC casts in the urine of patients with dysmorphic hematuria is directly associated with a glomerular source for the bleeding; therefore, the finding of a single RBC cast is enough to indicate the glomerular nature of the hematuria.1,2 Because glomerulopathies are potentially progressive renal diseases, tools to increase our diagnostic threshold are important for the prevention of chronic kidney disease (CKD).3,4
An abnormal number of RBCs on urine microscopy is a relatively common finding in laboratory practice, and definition of its origin makes it easier to identify its source in the urinary tract. Besides clinical history and physical examination, laboratory investigation of RBC morphology is the initial step towards diagnosis.
Birch & Farley,5 in the 1970s, developed a method to determine the source of hematuria, which is now used in most clinical laboratories. In the 1990s, some studies, such as those by Kohler et al. and Tomita et al.,6,7 sought standardization of the criteria used to classify dysmorphic RBCs. In spite of these advances, complementary methods for identification of RBC casts may increase our sensitivity in the diagnosis of glomerulopathies, once urine, a colloidal suspension, may have some elements in the supernatant of a spun sample which will not be seen in the sediment,8 justifying the low rate of RBC casts in urine samples from patients with hematuria.2
The hypothesis of this study is that the low rate of RBC cast identification is due to the insufficient concentration reached with conventional urinalysis methods.
OBJECTIVE
Compare the two techniques for sample analysis, conventional method (CM) and concentration technique (CT), in a series of urine exams presenting dysmorphic hematuria.
METHODS
We assessed urine samples from patients referred for several medical reasons, without a suspicion of glomerulopathy, within the routine of the Clinical Analysis Laboratory of the State University of Ponta Grossa. 4,277 urine samples were collected, according to guidelines for routine urinalysis. Hematuria was defined as greater than 5,000 RBCs/mL of urine. After microscopy of the sediment, 991 samples with hematuria were selected for investigation of RBC dysmorphism and casts.
RBC dysmorphism was investigated in the 991 selected samples according to the characteristics proposed by Birch & Farley,5 who considered RBC dysmorphism to consist of the presence of more than three different cell populations which, when greater than 80%, indicates a glomerular source for the hematuria. The study was undertaken with bright-field microscopy.9 Of the 991 samples analyzed, 249 had RBC dysmorphism, and were investigated for RBC casts according to the standard method (SM) or concentration technique (CT), as shown in Chart 1.
Routinely, the SM uses a 10 mL aliquot of urine which has undergone 5-minute low-speed centrifugation (relative centrifugal force 400g). The urine is concentrated to 1:10, with removal of 9.0 ml of supernatant, the remaining 1.0 mL of sediment being analyzed in a Neubauer chamber for investigation and count of the urinary elements, such as RBC casts. In the CT, after sample analysis with the SM, those samples with dysmorphic hematuria underwent a further step, which consisted of the addition of 10 ml urine to the initial cone-shaped tube, which was centrifuged at a relative centrifugal force of 2,000 g for 10 minutes, that is, concentrating the urine to 1:100, taking into account that 0.2 mL of the sediment was used for a final volume of 20 mL.
After the supernatant was discarded, we searched for casts, including RBC casts, analyzing the sediment between slide and coverslip, under light microscopy, with 400X magnification. The result was expressed as type and number of casts per preparation (p/p), after scanning the whole extension of the sediment. RBC casts were defined as casts with entrapped RBCs (RBC casts and mixed casts, composed of RBCs and other cells) and those with hemoglobin (hemoglobin casts), according to Figure 1. The latter were always associated with the presence of other RBC casts, once in isolation they may indicate hemoglobinuria, myoglobinuria or the presence of other similar pigments.
Statistical analysis was performed with the χ2 test.
RESULTS
Of a total of 4,277 processed samples, 991 (23.2%) had hematuria on sedimentoscopy, with greater than 5,000 RBC/mL. Women had a higher prevalence rate (25.4% versus 16.7% in men; p < 0.001). Of the samples with hematuria, 249 (25.6%) had dysmorphic hematuria according to Birch & Farley's criteria,5 there being no statistically significant difference in the prevalence of hematuria between the genders in this group (Table 1).
RBC count was divided in ranges from 5,000 to 100,000/mL. Most samples were in the 5,000 - 20,000 RBCs/mL range, only 4.4% of the samples having more than 100,000 RBCs/mL, being then classified as gross hematuria (Figure 2). The rate of samples with dysmorphic hematuria varied according to age range, with patients older than 60 years showing a statistically significant difference when compared to those younger than 40 years and those between 40 and 60 years (p = 0.04 and p = 0.02, respectively), whereas those older than 40 years and between 40 and 60 years had no statistically significant difference (p = 0.78) (Figure 3).
The 249 samples with dysmorphic hematuria were submitted to the two techniques for RBC cast investigation: SM and CT. The SM was positive in 8.4% (n = 21), while the CT was positive in 52.6% (n = 131) of the samples analyzed (p < 0.001) (Figure 4).
DISCUSSION AND CONCLUSION
Starting in the mid 1970s, Birch & Farley5 developed a method to determine the origin of hematuria. Since then, other studies have confirmed the importance of urinary RBC morphometry. However, there has been disagreement concerning the cut-off values to be observed, once these varied among the studies. In an attempt to overcome this obstacle, Hans Kölher et al.,6 in 1991, classified urinary RBCs in nine types, observing that acanthocytes and codocytes were frequently related to glomerulopathy-associated hematuria, when present at concentrations of 5% or above. Yet, because the absence of these cells does not rule out the glomeruli as the source of hematuria, these markers have high specificity but low sensitivity.
In the following year, Tomita et al.7 proposed another classification of urinary RBCs, with the aim of standardizing the dysmorphic forms and avoiding inter-observer variability. The RBCs were divided in five non-glomerular or urologic types (N1, N2, N3, N4 and N5) and five glomerular types (G1, G2, G3, G4 and G5), with their respective ghost forms, that is, RBCs which have lost their hemoglobin. G1 cells are similar to acanthocytes, and considered very specific. Therefore, rates of only 1% of these cells already indicate glomerular hematuria. When G1 cells are not present (or their rate is lower than 1%), a total G-cell count can be made, with the cut-off point for glomerular hematuria rising to 15%.
Even when these criteria are used, analysis is at times inconclusive, the association of other parameters, such as the presence of RBC casts, being necessary. 10 In addition, assessment of urinary RBC dysmorphism, in almost all studies, is made with phase-contrast microscopy, a method which is not available in most clinical laboratories, as is the case with automated urinalysis.8,11
In general, the prevalence of hematuria depends on the study population, and may range from 1 to 22% or more, males over the age of 50 years having higher rates of hematuria associated with severe urologic diseases, such as neoplastic disorders.12-15 In our study we found a 23.2% (n = 991) prevalence rate of hematuria for the general population. When only the samples with dysmorphic hematuria (n = 249) were assessed, the rate was 5.8%.
As reported in other studies,16 women had a higher general rate of hematuria. Yet, when only dysmorphic hematuria was considered, there was no significant gender difference. This fact may be explained by the presence of several interfering factors that were not excluded in the first group, such as urinary tract infection and contamination by menstrual blood and vaginal secretions. These factors were excluded by the investigation and selection of samples with dysmorphic RBC.
As for age, our study showed that 59.8% of the samples (n = 149) belonged to patients aged 50 years or less, in disagreement with other studies which reported that microscopic hematuria was rare below the age of 50 years.16 This fact points to the early investigation of glomerular diseases in younger persons, as glomerulopathies are the second cause of CKD in Brazil.17 Moreover, Schroder16 reported the importance of investigating microscopic hematuria, present in 95.6% of his sample. Figure 3 includes the samples with hematuria (n = 991), with the statistical analysis of dysmorphic hematuria in the following age ranges: < 40 years, between 40 and 60 years, and > 60 years. There was no statistically significant difference between the 40-60 years and > 60 years groups, while the difference was statistically significant between the > 60 years group and the others. This is probably due to an increased number of hematuria-provoking conditions in persons > 60 years, such as prostatitis, neoplastic disorders and other urologic problems.
Hematuria may, therefore, be related to nephrologic or urologic problems. Once hematuria is confirmed, investigation of the bleeding source, undertaken with a search for RBC dysmorphism and RBC casts in the urine, is warranted. The additional presence of proteinuria, glycosuria and other pathological casts is helpful.
Several authors have found it difficult to establish a cut-off point to characterize glomerular hematuria. In an attempt to raise specificity, Kölher & Tomita6,7 demonstrated the importance of specific morphologies, such as acanthocytes, codocytes and G1 cells, for dysmorphism determination. Unfortunately, low sensitivity means that a number of cases remain, in which the bleeding source is unknown. Besides dysmorphism, the presence of RBC casts, which although associated to non-glomerular bleeding at times are strongly associated with glomerular hematuria, may help with the diagnosis of the bleeding source.16
RBC casts are not frequently visualized in routine urinalysis.18 This is believed to be due to the insufficient sample concentration afforded by the SM. We proposed to use a CT to investigate the presence of RBC casts in samples with dysmorphic hematuria.
We employed Birch & Farley's5 criteria to classify 25.1% (n = 249) of the 991 orginal samples as dysmorphic hematuria. The presence of specific cells, such as codocytes, acanthocytes and G1 cells was investigated, but. taking into account that these structures are not always present, the main criteria used were changes in the form and size of the RBCs. The presence of RBC casts was investigated in all samples with dysmorphic hematuria, in parallel, with the SM and the CT. The SM showed an 8.4% (n = 21) positivity. The 228 negative samples on the SM were submitted to the CT, in which the sediment was re-processed under high speed rotation for a longer period, aiming to increase the concentration of the urinary elements. The CT was positive in 52.6% (n = 120), meaning a significant improvement of RBC-cast identification on the SM (r < 0.001), as can be seen in Figure 4.
The CT was effective in our study, raising the sensitivity of RBC-cast investigation. It must be highlighted that no lysis of the RBC casts happened during high speed rotation centrifugation (2,000 g), contrary to the literature, which recommends that sedimentoscopy should be performed on uncentrifuged urine, or on urine which has been submitted to a lower rotation speed (400 g).15,11 This result was observed for other casts (hyaline, granular, epithelial, leukocyte, fatty and oval fat bodies), which appeared on CT microscopy.
These data point to the possibility that a myth surrounding cast degeneration by urine centrifugation has been created. Although this concept of centrifugation-associated destruction of urinary elements has been widely accepted by the laboratory community, our data show that this is not valid as far as casts are concerned. We cannot infer about the existence of glomerulopathies in the study population, but we can certainly state that the CT increases the positivity for RBC casts.
Our population was composed of random samples not specified for glomerulopathy suspicion and without further investigation of a bleeding source. Indeed, this was a typical primary care population, for which hematuria assessment may avoid delay in the referral to a nephrologist, that is, when end-stage CKD is established and dialysis is necessary. In spite of the absence of epidemiologic studies on the occurrence of glomerular diseases in Brazil, recent studies19 have shown glomerular disorders to be the second cause of end-stage CKD in the country. These data show the importance of referral of persons with RBC casts,18 there being consensus on the primary care responsibility for diagnosing and adequately referring patients with hematuria, aiming the early detection of urologic and nephrologic conditions.20,21
Inter-laboratory methodological variation and inter-examiner variability may be obstacles to laboratory quality control. Therefore, greater attention should be paid to standardized urinalysis, while new techniques for identification of markers of renal disease are sought. While other methods are not available, we suggest the association of the CT-based RBC cast investigation and the search for RBC dysmorphism for the assessment of renal diseases in the laboratory investigation of the bleeding origin, in patients with confirmed hematuria.
This study opens new perspectives towards the study of new ways for the urinalysis-based early detection of renal diseases. The CT-based search for RBC casts must be associated with the presence of dysmorphism on routine urinalysis to prove the glomerular origin of the hematuria.
REFERENCES
- 1. Abreu PF, Requião-Moura LR, Sesso R. Avaliação diagnóstica de hematúria. J Bras Nefrol 2007;29:158-63.
- 2. Rizzoni G, Braggion F, Zacchello G. Evaluation of glomerular and nonglomerular hematuria by phase-contrast microscopy. J Pediatr 1983;103:370-4.
- 3. Margulis V, Sagalowsky AI. Assessment of hematuria. Med Clin North Am 2011;95:153-9.
- 4. Barros E, Manfro RC, Thomé FS, Gonçalves LF. Nefrologia: rotinas, diagnóstico e tratamento. Porto Alegre: Artmed; 2006.
- 5. Birch DF, Fairley KF. Haematuria: glomerular or non-glomerular? Lancet 1979;2:845-6.
- 6. Kohler H, Wandel E, Brunck B. Acanthocyturia: a characteristic marker for glomerular bleeding. Kidney Int 1991;40:115-20.
- 7. Tomita M, Kitamoto Y, Nakayama M, Nakayama M, Sato T. A new morphological classification of urinary erythrocytes for differential diagnosis of glomerular hematuria. Clin Nephrol 1992;37:84-9.
- 8. Hannemann-Pohl K, Kampf SC. Automation of urine sediment examination: a comparison of the Sysmex UF-100 automated flow cytometer with routine manual diagnosis (microscopy, test strips, and bacterial culture). Clin Chem Lab Med 1999;37:753-64.
- 9. Dinda AK, Saxena S, Guleria S, Tiwari SC, Dash SC, Srivastava RN, et al Diagnosis of glomerular haematuria: role of dysmorphic red cell, G1 cell and bright-field microscopy. Scand J Clin Lab Invest 1997;57:203-8.
- 10. Rizzoni G. Evaluation of glomerular and nonglomerular hematuria by phase-contrast microscopy. J Ped 1983;103:370-4.
- 11. Venkat Raman G, Pead L, Lee HA, Maskell R. A blind controlled trial of phase-contrast microscopy by two observers for evaluating the source of hematuria. Nephron 1986;44:304-8.
- 12. Bastos MG, Martins GA, de Paula RB. Diagnóstico diferencial nas hematúrias. J Bras Nefrol 1998;20:425-40.
- 13. Grossfeld GD, Wolf JS Jr, Litwan MS, Hricak H, Shuler CL, Agerter DC, et al Asymptomatic microscopic hematuria in adults: summary of the AUA best practice policy recommendations. Am Fam Physician 2001;63:1145-54.
- 14. Messing EM, Young TB, Hunt VB, Emoto SE, Wehbie JM. The significance of asymptomatic microhematuria in men 50 or more years old: findings of a home screening study using urinary dipsticks. J Urol 1987;137:919-22.
- 15. Mohr DN, Offord KP, Owen RA, Melton LJ 3rd. Asymptomatic microhematuria and urologic disease. A population-based study. JAMA 1998;256:224-5.
- 16. Schroder FH. Microscopic haematuria. BMJ 1994;309:70-2.
- 17. Kirsztajn GM. A campanha nacional de prevenção de doenças renais. J Bras Nefrol 2006;28:2-3.
- 18. McDonald MM, Swagerty D, Wetzel L. Assessment of microscopic hematuria in adults. Am Fam Physician 2006;73:1748-54.
- 19. Alves MAR. Propedêutica das Glomerulopatias. In: Barros RT, Alves MAR, Kirztajn GM, Sens YAS, M Dantas. Glomerulopatias: Patogenia, Clínica e Tratamento. 2Ş ed. São Paulo: Editora Sarvier, 2006. v. 01. 480 p.
- 20. Patel JV, Chambers CV, Gomella LG. Hematuria: etiology and evaluation for the primary care physician. Can J Urol 2008;15:54-61.
- 21. Shen X. Diagnostic algorithm for the evaluation of hematuria. J Am Acad Nurse Pract 2010;22:186-91.
Comparative analysis of two methodologies for the identification of urinary red blood cell casts
Publication Dates
-
Publication in this collection
21 Dec 2011 -
Date of issue
Dec 2011
History
-
Received
17 May 2011 -
Accepted
13 July 2011