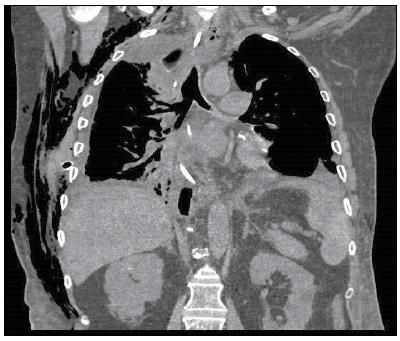
A 68-year-old man, during the postoperative period after video-assisted thoracoscopic esophagectomy for esophageal adenocarcinoma, experienced an air leak via the chest drainage system (Thopaz+; Medela, Baar, Switzerland), at an approximate flow rate of 3.0-3.5 L/min, as a complication of the surgical procedure. Physical examination showed normal breath sounds bilaterally and usual fluid drainage through the chest tube (150-200 mL/day). In addition, a sagittal CT image of the chest did not reveal clear changes in the bronchial anatomy (Figure 1). Bronchoscopic examination of the bronchial tree was ordered for suspected air leak in the upper bronchial tree.11 Argento AC, Wolfe CR, Wahidi MM, Shofer SL, Mahmood K. Bronchomediastinal fistula caused by endobronchial aspergilloma. Ann Am Thorac Soc. 2015 Jan;12(1):91-5. https://doi.org/10.1513/AnnalsATS.201406-247BC
https://doi.org/10.1513/AnnalsATS.201406...
A blackened, villous vegetative lesion, located in the right main bronchus (Figure 2), was submitted to an incisional biopsy. Direct microbiological assay and cultures revealed Aspergillus niger (Figure 2), with no vascular involvement. A diagnosis of endobronchial aspergilloma (EA) was made.
Sagittal slice from a CT scan of the chest. It was not possible to clearly identify the vegetative lesion in the right main bronchus and lobar bronchi (including the right upper lobar bronchus) with this imaging modality.
In A, image demonstrating a macroscopic lesion, caused by Aspergillus niger, in the right upper lobar bronchus. In B, photomicrograph of a direct microbiological assay (H&E; magnification, ×150).
EA is a rare entity, characterized by Aspergillus sp. growth within the bronchial lumen. It is a noninvasive form of aspergillosis, and most cases are diagnosed incidentally during bronchoscopy for reasons other than the initial diagnostic suspicion.22 Araújo D, Figueiredo M, Monteiro P. Endobronchial aspergilloma: An unusual presentation of pulmonary aspergillosis. Rev Port Pneumol (2006). 2016;22(1):61-2. https://doi.org/10.1016/j.rppnen.2015.07.003
https://doi.org/10.1016/j.rppnen.2015.07...
The patient was treated for two weeks with voriconazole and micafungin.33 Sales Mda P. Chapter 5--Aspergillosis: from diagnosis to treatment. J Bras Pneumol. 2009;35(12):1238-44. https://doi.org/10.1590/S1806-37132009001200012
https://doi.org/10.1590/S1806-3713200900...
One month later, there were no clinical signs of invasive aspergillosis or treatment complications.
REFERENCES
-
1Argento AC, Wolfe CR, Wahidi MM, Shofer SL, Mahmood K. Bronchomediastinal fistula caused by endobronchial aspergilloma. Ann Am Thorac Soc. 2015 Jan;12(1):91-5. https://doi.org/10.1513/AnnalsATS.201406-247BC
» https://doi.org/10.1513/AnnalsATS.201406-247BC -
2Araújo D, Figueiredo M, Monteiro P. Endobronchial aspergilloma: An unusual presentation of pulmonary aspergillosis. Rev Port Pneumol (2006). 2016;22(1):61-2. https://doi.org/10.1016/j.rppnen.2015.07.003
» https://doi.org/10.1016/j.rppnen.2015.07.003 -
3Sales Mda P. Chapter 5--Aspergillosis: from diagnosis to treatment. J Bras Pneumol. 2009;35(12):1238-44. https://doi.org/10.1590/S1806-37132009001200012
» https://doi.org/10.1590/S1806-37132009001200012
Publication Dates
-
Publication in this collection
2 Mar 2020 -
Date of issue
2020