Abstracts
OBJECTIVE: To study the Doppler velocimetry of the fetal middle cerebral artery in pregnancies complicated by placental insufficiency, and to verify its role in the prognosis of neonatal survival. METHODS: This was a prospective study of 93 pregnant women with diagnosis of placental insufficiency detected before the 34th week of pregnancy. Placental insufficiency was characterized by abnormal umbilical artery (UA) Doppler (> 95th percentile). The following parameterswere analyzed: umbilical artery (UA) pulsatility index (PI); middle cerebral artery (MCA) PI; brain-placenta ratio - BPR (MCA-PI/UA-PI); MCA peak systolic velocity (MCA-PSV); and PI for veins (PIV) of ductus venosus (DV). The parameters were analyzed in terms of absolute values, z-scores (standard deviations from the mean), or multiples of the median (MoM). The outcome investigatedwas neonatal death during the hospitalization period after birth. RESULTS: Of the 93 pregnancies analyzed, there were 25 (26.9%) neonatal deaths. The group that died, when compared to the survival group, presented a significant association with the diagnosis of absent or reversed end-diastolic flow (88% vs. 23.6%, p < 0.001), with a higher median of UA PI (2.9 vs. 1.7, p < 0.001) and UA PI z-score (10.4 vs. 4.9, p < 0.001); higher MCAPSV MoM (1.4 vs. 1.1, p = 0.012); lower BPR (0.4 vs. 0.7, p < 0.001); higher PIV-DV (1.2 vs. 0.8, p < 0.001) and DV z-score (3.6 vs. 0.6, p < 0.001). In the logistic regression, the independent variables predictive of neonatal death were: gestational age at birth (OR = 0.45; 95% CI: 0.3 to 0.7; p < 0.001) and UA PI z-score (OR = 1.14, 95% CI: 1.0 to 1.3, p = 0.046). CONCLUSION: Despite the association verified by the univariate analysis between neonatal death and the parameters of fetal cerebral Doppler velocimetry, the multivariate analysis identified prematurity and degree of insufficiency of placental circulation as independent factors related to neonatal death in pregnancies complicated by placental insufficiency.
Placental insufficiency; Ultrasonography; Doppler; Fetal hypoxia; Umbilical cord; Middle cerebral artery; Umbilical arteries
OBJETIVO: Estudar a dopplervelocimetria da artéria cerebral média fetal em gestações complicadas pela insuficiência placentária e verificar o seu papel no prognóstico de sobrevida neonatal. MÉTODOS: Trata-se de estudo prospectivo de 93 gestantes com diagnóstico de insuficiência placentária estabelecida antes da 34ª semana. A insuficiência placentária foi caracterizada pelo Doppler de artéria umbilical (AU) alterado (> p95). Foram analisados os seguintes parâmetros: índice de pulsatilidade (IP) da artéria umbilical (AU), IP da artéria cerebral média (ACM), relação cerebroplacentária -RCP(IP-ACM/IP-AU), pico de velocidade sistólicada ACM (PVS-ACM) e IP para veias (IPV) do ducto venoso (DV). Os parâmetros foram analisados pelos valores absolutos, em escores zeta (desvios padrão a partir da média) ou múltiplos da mediana (MoM). O desfecho investigado foi o óbito neonatal no período de internação após o nascimento. RESULTADOS: Nas 93 gestações analisadas, ocorreram 25 (26,9%) óbitos neonatais. No grupo que evoluiu com óbito neonatal, quando comparado com o grupo com sobrevida, houve associação significativa com o diagnóstico de diástole zero ou reversa (88% vs. 23,6%, p < 0,001), com maior mediana do IP da AU (2,9 vs. 1,7, p < 0,001) e seu escore zeta (10,4 vs. 4,9, p < 0,001); maior valor do PVS-ACM MoM (1,4 vs. 1,1, p = 0,012); menor valor da RCP (0,4 vs. 0,7, p < 0,001); maior valor do IPV-DV (1,2 vs. 0,8, p < 0,001) e no escore zeta do DV (3,6 vs.0,6, p<0,001). Na regressão logística, as variáveis independentes para a prediçãodoóbito neonatal foram a idade gestacional no parto (OR = 0,45; IC95% 0,3 a 0,7, p < 0,001) e o escore zeta do IP-AU (OR 1,14, IC95% 1,0 a 1,3, p = 0,046). CONCLUSÃO: Apesar da associação verificada pela análise univariada entre a morte neonatal e os parâmetros da dopplervelocimetria cerebral fetal, a análise multivariada identificou a prematuridadeeograude insuficiência da circulação placentária como fatores independentes relacionados com o óbito neonatal em gestações complicadas por insuficiência placentária.
Insuficiência placentária; Ultrassonografia; Doppler; Hipóxia fetal; Cordão umbilical; Artéria cerebral média; Artérias umbilicais
ORIGINAL ARTICLE
Doppler velocimetry of the fetal middle cerebral artery and other parameters of fetal well-being in neonatal survival during pregnancies with placental insufficiency*
Roseli Mieko Yamamoto Nomura**; Juliana Ikeda Niigaki; Flávia Thiemi Horigome; Rossana Pulcineli Vieira Francisco; Marcelo Zugaib
Medical School, Universidade de São Paulo, Universidade de São Paulo, São Paulo, SP, Brazil
ABSTRACT
OBJECTIVE: To study the Doppler velocimetry of the fetal middle cerebral artery in pregnancies complicated by placental insufficiency, and to verify its role in the prognosis of neonatal survival.
METHODS: This was a prospective study of 93 pregnant women with diagnosis of placental insufficiency detected before the 34th week of pregnancy. Placental insufficiency was characterized by abnormal umbilical artery (UA) Doppler (> 95th percentile). The following parameters were analyzed: umbilical artery (UA) pulsatility index (PI); middle cerebral artery (MCA) PI; brain-placenta ratio BPR (MCA-PI/UA-PI); MCA peak systolic velocity (MCA-PSV); and PI for veins (PIV) of ductus venosus (DV). The parameters were analyzed in terms of absolute values, z-scores (standard deviations from the mean), or multiples of the median (MoM). The outcome investigated was neonatal death during the hospitalization period after birth.
RESULTS: Of the 93 pregnancies analyzed, there were 25 (26.9%) neonatal deaths. The group that died, when compared to the survival group, presented a significant association with the diagnosis of absent or reversed end-diastolic flow (88% vs. 23.6%, p < 0.001), with a higher median of UA PI (2.9 vs. 1.7, p < 0.001) and UA PI z-score (10.4 vs. 4.9, p < 0.001); higher MCA-PSV MoM (1.4 vs. 1.1, p = 0.012); lower BPR (0.4 vs. 0.7, p < 0.001); higher PIV-DV (1.2 vs. 0.8, p < 0.001) and DV z-score (3.6 vs. 0.6, p < 0.001). In the logistic regression, the independent variables predictive of neonatal death were: gestational age at birth (OR = 0.45; 95% CI: 0.3 to 0.7; p < 0.001) and UA PI z-score (OR = 1.14, 95% CI: 1.0 to 1.3, p = 0.046).
CONCLUSION: Despite the association verified by the univariate analysis between neonatal death and the parameters of fetal cerebral Doppler velocimetry, the multivariate analysis identified prematurity and degree of insufficiency of placental circulation as independent factors related to neonatal death in pregnancies complicated by placental insufficiency.
Keywords: Placental insufficiency; Ultrasonography; Doppler; Fetal hypoxia; Umbilical cord; Middle cerebral artery; Umbilical arteries
Introduction
The main complication of the placental insufficiency is the restricted fetal development, which is associated with higher perinatal morbidity and mortality.1,2 The inappropriate interaction between the trophoblast and maternal tissues is involved in its physiopathology,3 promoting an increased resistance of the capillaries of terminal villi, with consequent reduction in maternal-fetal exchanges and fetal hypoxemia. As a result of hypoxemia, the fetus starts to present hemodynamic adaptations, a phenomenon known as centralization of fetal circulation.4 This centralization is characterized by the redistribution of blood flow to vital organs such as the brain, heart, and adrenal glands, to the detriment of others such as the spleen, kidneys, and peripheral circulation. The duration and efficacy of this mechanism depend on the adaptability of the fetus and on preservation of the hemodynamic balance.5,6
Doppler velocimetry is the most frequently used method in clinical practice to identify fetal centralization, as it allows for a non-invasive evaluation of fetal and fetal-placental circulations.7 This method may be used in the early detection of pathologies associated with defective placentation, and it is useful to prognosticate restricted fetal development.8 In normal pregnancies, the vascular resistance in the umbilical arteries (UA) is low; conversely, the resistance in the cerebral territory of the fetus is high. In cases of placental insufficiency, progressive fetal hypoxemia stimulates the chemoreceptors, triggering a response that leads to vasodilation of vital organs and vasoconstriction of the remaining organs.9
The combination of fetal and fetal-placental parameters appears to be an interesting investigation method both for placental function and hemodynamic adaptations of the fetus. Studies in animal models demonstrate that the centralization of fetal circulation has significant correlation with hypoxemia and hypoxia.10 The brain-placenta ratio (BPR),11,12 calculated by the ratio between the Doppler velocimetric indices of the middle cerebral artery (MCA) and the UA, has been described as predictive of the neonatal prognosis.13-15 For a better understanding of the adaptations in fetal cerebral circulation regarding hypoxia and hypoxemia, this study aimed to evaluate fetal MCA Doppler velocimetry in pregnancies with placental insufficiency, and to verify its role in the prognosis of neonatal survival.
Methods
This cross-sectional study was conducted in a university hospital, during the period from May of 2009 to July of 2012, and included high-risk pregnant women hospitalized in the Obstetrics ward with diagnosis of placental insufficiency. To calculate the size of the sample, considering the proportion of neonatal deaths of 30% in fetuses with restricted development described by Mari et al.,16 in order to obtain a case group of at least 25 neonatal deaths, a minimum of 83 pregnancies were necessary. After a difference in the proportion of neonatal deaths was verified in this study, 93 cases were included in order to contemplate 25 cases of deaths. All participants consented to participate in the research. The research project and the informed consent were approved by the ethics committee of the institution, under No. 1359/09.
The following inclusion criteria were used: singleton pregnancy; live fetus; diagnosis of placental insufficiency characterized by abnormal UA Doppler (pulsatility index > percentile 95) performed between 26 and 34 weeks of gestational age; intact choroamniotic membranes; three-dimensional fetal ultrasonography with no signs of abnormalities; no signs of chromosomal abnormalities; absence of chorioamnionitis or other perinatal infections; and birth at the institution. Cases in which a congenital anomaly was detected in the newborn, cases of fetal anemia, and cases in which the fetal Doppler examination was not possible up to three days before birth were excluded.
Fetal well-being was assessed through antenatal cardiotocography, fetal biophysical profile (BPP), and obstetric Doppler velocimetry. The examinations were performed in the patients during the hospitalization period, in intervals that ranged from one to three days. The BPP parameters were evaluated through ultrasonography (tone, fetal body movements, fetal breathing movements, and amniotic fluid volume). The ultrasound equipment used included a Philips® model Envisor; GE model Voluson 730 Expert, equipped with convex transducer; and a Hewllet Packard® traditional cardiotocography machine. The fetal heart rate (FHR) was evaluated through the cardiotocography. The trace was classified as regular when it presented at least two transient accelerations with 15 bpm of range within a 30-minute window, baseline FHR between 110 and 160 bpm, variability greater than 5 bpm, and absence of decelerations; and was classified as suspicious in the absence of transient accelerations with normal baseline FHR and reduced and abnormal variability in the presence of decelerations or absent variability. In the BPP, a score of zero (abnormal) or two (regular) was attributed to each parameter. The final classification corresponded to the sum of the points. The amniotic fluid volume was assessed through the amniotic fluid index (AFI). Its values were classified as regular when higher than 5.0 cm, and values lower than 5.0 cm were characterized as oligohydramnios.
Ultrasonography equipment was used for the study of fetal cerebral circulation. Doppler velocimetry was performed through machines equipped with pulsed Doppler device (duplex Doppler) and color flow mapping, 3.5-MHz sector transducer, and low-pass filter (25 Hz). The sample volume was adjusted to the diameter of each vessel evaluated, and the angle of insonation was always kept below 30º. In the insonation of the middle cerebral artery, the angle of insonation was close to zero. All examinations were performed with the patient in the supine position with the head elevated, in the absence of fetal body or breathing movements and with fetal heart rate between 110 and 160 bpm. Doppler velocimetry of the umbilical arteries (UA), middle cerebral artery (MCA), and ductus venosus (DV) were then performed. UA Doppler velocimetry was performed based on insonation of the vessel close to its insertion in the placenta. The MCA was used to evaluate the cerebral vessels because it is an easily reproducible technique. The insonation of the vessel was performed in its proximal third from the Circle of Willis. The DV was evaluated in a cross and oblique section of the fetal abdomen. For each vessel examined, three to five uniform sonograms were obtained, and the average value of each result was used for the calculation of the pulsatility indices (PI) for arteries and the pulsatility index for veins (PIV) of the ductus venosus. All pulsatility index values were also analyzed in z-scores (number of standard deviations from the mean), calculated for each gestational age.14 The values of MCA peak systolic velocity (MCA-PSV) were analyzed pursuant to their absolute value and also based on the multiples of the median (MoM) for gestational age.17
Since 2005, the clinical protocol for follow-up of the cases of placental insufficiency is based on the follow-up of fetal well-being through serial biophysical profile and arterial and venous Doppler velocimetry. The decision to perform the delivery is taken after individual analysis of the cases, based on clinical data of the mother and the fetal condition. The occurrence of any of the following abnormalities characterized the decrease in fetal well-being: low variability of fetal heart rate (< 5 bpm) or late decelerations in the cardiotocography, abnormal fetal biophysical profile (< 6), or pulsatility indices for veins (PIV) of the ductus venosus greater than 1.0. Data from the last evaluation of fetal well-being performed before birth or before the beginning of corticosteroid therapy prior to the resolution were analyzed. Additional delivery and newborn clinical data were obtained through inquiry to the medical records and registers of births, filed in the Medical Files Department of the institution, as well as information obtained from inquiry to the department's computerized database.
The following perinatal outcomes were also investigated: gestational age at birth; weight of the newborn; adequacy of the weight of the newborn; pH at birth in blood of the umbilical cord artery; gender; Apgar scores at minutes 1, 5 and 10; need for orotracheal intubation (OTI) and admission in the Intensive Care Unit (ICU); as well as maternal demographic variables: mother's age, parity, ethnicity, and complications of the current pregnancy. The gestational age was calculated from the last menstrual period (LMP), when compatible with the gestational age estimated by the ultrasonography performed no later than the 20th week of pregnancy. In cases in which such correlation was not observed, the gestational age was calculated through data from the first ultrasonography. The weight of the newborn, in grams, was measured in the delivery room, and the adequacy was evaluated through comparison with normative data from Alexander et al.18 thus, newborns with weight below the 10th percentile of the corresponding range were classified as small for the gestational age.
Data related to the population characteristics that result in neonatal death is presented in Table 1. All cases in which the newborn died during hospitalization were characterized as neonatal death, regardless of the postnatal moment (early, late, or child) at which the death took place.
Results were analyzed through the Medcalc software, version 11.5.1.0. (Medcalc Software - Belgium). Categorical variables were analyzed descriptively, by calculating absolute and relative frequencies. In order to analyze the continuous variables, the results were expressed as mean, median, standard deviation, minimum, and maximum. The Chi-squared test was used to compare proportions, and Fisher's exact test was used when applicable (position in the sentence mostly). Student's t-test was used to compare the averages among the groups for variables with normal distribution, and the Mann-Whitney U-test was used for abnormal distribution variables. The logistic regression model was used to identify the independent variables associated with the neonatal death outcome. The value of 0.05 (alpha = 5%) was adopted as the significance level. Thus, descriptive levels (p) below this value were deemed significant (p < 0.05).
Results
In this study, 25 (26.9%) neonatal deaths occurred. Among the population characteristics and aspects of the birth that were identified as related to neonatal death, there was a significant association with gestational age at birth (p < 0.001) and weight of the newborn (p < 0.001) (table 1). the analysis of apgar scores at minutes 1, 5, and 10 also showed a significant association with neonatal death when these scores presented a value lower than 7.
Table 2 shows the results regarding the examinations for evaluation of fetal well-being. The group that died presented a significant association (p = 0.045) with abnormal cardiotocography results and low values of BPP (p = 0.012, Chi-squared for trend). No significant association with the assessment of the amniotic fluid volume was found.
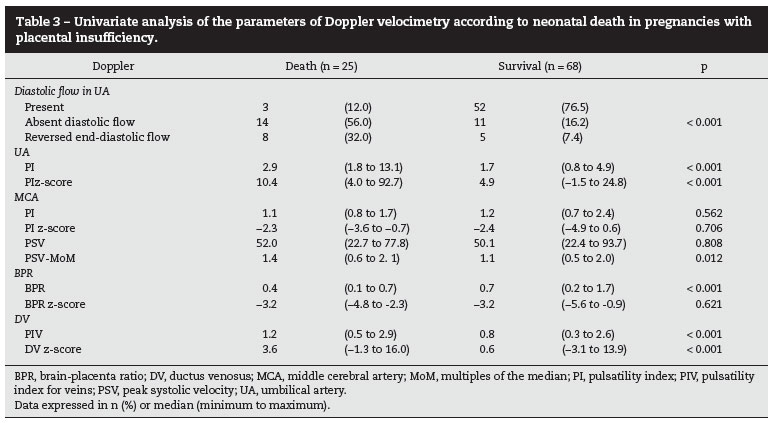
The results of the analysis of arterial and venous Doppler velocimetry are shown in Table 3. Neonatal mortality was significantly associated with the diagnosis of absent or reversed end-diastolic flow (p < 0.001), higher values of ua pi (p < 0.001), and higher z-score (p < 0.01). when the results of mca doppler velocimetry were analyzed, the group that died showed the highest median of psv-mom (p = 0.012) when compared to the survival group. the value of the bpr also presented the lowest median in the group that died (p < 0.001). The analysis of the values of DV Doppler velocimetry showed significantly higher values in the PIV median (p < 0.001) and its z-score (p < 0.001) in the group that died.
The Doppler velocimetric variables were studied on a multivariate basis in order to predict neonatal death through the logistic regression model. The following variables, with significance lower than 0.1 for the outcome, were included in the model: gestational age (GA) at birth, weight of the newborn, ethnicity, diagnosis of diabetes, UA PI z-score, PSV-MoM, and DV z-score. After performing the analysis, the independent variables remaining in the final model were: GA at birth and UA PI Z-score (Table 4). This model correctly predicted 86.0% of the cases of neonatal death.
Discussion
This study analyzed the factors associated with neonatal death in pregnancies with early diagnosed placental insufficiency, and found that the outcome of neonatal death was independently associated with the gestational age at which the birth occurs and UA PI (z-score). The Doppler velocimetric parameters of the evaluation of MCA were not shown to be an independent factor for the cases studied. In this population, the prematurity and impairment of the placental area proved to have a key role in the prognosis of survival of the newborn. Data suggest that the degree of cerebral circulation vasodilation did not exert any influence on survival, which appears to depend on the degree of impairment of the fetoplacental circulation.
Cruz-Martinez et al.,19 analyzed parameters of cerebral circulation of fetuses that are small for the gestational age and concluded that, before the beginning of labor induction, the abnormalities in cerebral Doppler identify the cases with risk of an emergency C-section and neonatal acidosis. However, the authors did not compare their results with neonatal mortality. Regarding BPR, the study shows that the reduction in the values has greater sensitivity than the analysis of vasodilation through interpretation of MCA PI in predicting emergency C-section. Additionally, the authors analyzed the tissue perfusion, and this parameter did not present an association with the final objectives, indicating that, despite the changes in the Doppler of the cerebral circulation, the perfusion is not effectively modified. This may support the fact that MCA Doppler was not identified in the present study as an independent factor in the prognosis of fetal survival. Despite the vasodilation, the protection of the fetal central nervous system would not be sufficiently effective to be an independent factor influencing the neonatal mortality. The present study did not demonstrate any association between the results of fetal MCA IP and neonatal mortality.
The identification of fetuses with placental insufficiency is usually made through UA Doppler velocimetry, which starts to show a progressive increase in the resistance of the placental area. This directly influences fetal development, as the progressive dysfunction impairs the nutrition of the fetus. Thus, the estimated fetal weight and the degree of impairment of the placental circulation are key parameters in the decision for the most opportune time to deliver. In the present study, the analysis of the degree of impairment of different circulations was performed through analysis of the z-score, i.e., based on the value of standard deviations obtained that differs from the average expected for a certain gestational age. This analysis tried to correct the influence of the gestational age on the interpretation of different Doppler results.
Neonatal mortality depends on several factors, related or not to the birth. The better the situation of the newborn, the better the neonatal outcomes. However, the maintenance of pregnancy, despite the centralization of fetal circulation, did not appear to influence postnatal survival. Different results were observed by Odibo et al.,20 who analyzed cases of intrauterine growth restriction and investigated the impact of BPR using reference values specific to the gestational age. They concluded that abnormal BPR was associated with adverse perinatal outcomes. They argued that BPR incorporates both data: placental circulation (umbilical artery) and fetal brain response (MCA). When comparing limits specific to the gestational age with cutoff values, they concluded that the efficiency of the models was similar when predicting adverse outcomes. In the analysis of perinatal mortality, specific predictive models only for this parameter were not presented, which made the comparison with the present study difficult. Other studies that also analyzed the prognostic value of BPR in fetuses with growth restriction have shown that this parameter is a predictor of changes in the FHR and of extended hospital stay for the newborn.21-23
The univariate analysis of the parameters in the fetal cerebral circulation showed that MCA vasodilation was not related to neonatal mortality, and the analysis by z-score presented the same result. The association verified through BPR appears to be influenced by the values of the umbilical artery, which was evidenced by a multivariate analysis. However, innovative data disclosed in this research refers to the significant association of MCA-PSV with neonatal survival. The patients that died presented a higher maximum velocity value, as analyzed by the number of MoM. This increase may be related to severe hemodynamic changes, in which there is a change in the aortic isthmus flow, pursuant to the hypothesis of Mari et al.,24 who, in cases of fetuses with growth restriction, highlighted this abnormality as an indicator of the deterioration in fetal circulation. These authors concluded that high values of MCA-PSV predicted the perinatal mortality and would be useful in the evaluation of fetuses with abnormal UA Doppler. Based on the longitudinal analysis of the results of the MCA Doppler velocimetry, they suggest that the MCA PI is initially abnormal in most fetuses, but they observed an increase in the MCA PI with a tendency to normalization before birth or fetal death. Based on the analysis of MCA-PSV, they verified a well-defined pattern, with progressive increase according to the advance of gestational age, and tendency to mild reduction immediately preceding birth or fetal death. In the present study, the group of fetuses who died presented a higher median of the values of MCA-PSV when compared to the survival group. However, the increase was discreet, which differed from that described by Mari et al.24. Additional studies are required to clarify this aspect.
The UA Doppler is a method that essentially evaluates the placental function.1,8 The impairment of the placental bed, which was reflected in the increased resistance to blood flow and consequent reduction in the diastolic velocity of the umbilical artery, was a factor that influenced the neonatal prognosis. When qualitatively characterized, as well as during analysis of the PI Z-score, an association with neonatal death was found. The degree of placental dysfunction, quantitatively represented by the UA PI z-score, was an independent factor that influenced the neonatal survival. It is a parameter that, together with the gestational age, should be used in clinical practice to adjust the decisions regarding the best time for delivery in pregnancies complicated by placental insufficiency.
The venous circulation of the fetus was investigated through the DV Doppler. In this study, DV PI showed a significant association with neonatal mortality in the univariate analysis, but it did not remain as an independent factor in the logistic regression. Abnormalities in the venous circulation25 are associated with acidemia at birth26 and impairment of the cardiac function of the fetus,27,28 which indicate cases of greater severity.
Placental insufficiency is a complication of the pregnancy with high neonatal mortality, especially when there is a need to interrupt the pregnancy at an early gestational age.16 In addition to the fact that prematurity is an important factor for neonatal survival, it can be verified that the degree of impairment of the placental circulation, analyzed through the UA PI, also influenced this prognosis on an independent basis. Finally, this study demonstrated that the Doppler velocimetric parameters of assessment of the fetal cerebral circulation are associated with neonatal mortality in the univariate analysis. However, through multivariate analysis, the prematurity and degree of impairment of the placental circulation were the independent factors related to the outcome, in pregnancies with placental insufficiency.
Financial support
Research initiation scholarship from the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) was granted to the student Flávia Tiemi Horigome.
Conflicts of interest
The authors declare no conflicts of interest.
REFERENCES
- 1. Baschat AA. Fetal growth restriction - from observation to intervention. J Perinat Med. 2010;38:239-46.
- 2. Garite TJ, Clark R, Thorp JA. Intrauterine growth restriction increases morbidity and mortality among premature neonates. Am J Obstet Gynecol. 2004;191:481-7.
- 3. Brosens I, Dixon HG, Robertson WB. Fetal growth retardation and the arteries of the placental bed. Br J Obstet Gynaecol. 1977;84:656-63.
- 4. Behrman RE, Lees MH, Peterson EN, De Lannoy CW, Seeds AE. Distribution of the circulation in the normal and asphyxiated fetal primate. Am J Obstet Gynecol. 1970;108:956-69.
- 5. Wladimiroff JW, Tonge HM, Stewart PA. Doppler ultrasound assessment of cerebral blood flow in the human fetus. Br J Obstet Gynaecol. 1986;93:471-5.
- 6. Arduini D, Rizzo G, Romanini C. Changes of pulsatility index from fetal vessels preceding the onset of late decelerations in growth-retarded fetuses. Obstet Gynaecol. 1992;79:605-10.
- 7. Hecher K, Bilardo CM, Stigter RH, Ville Y, Hackelöer BJ, Kok HJ, et al. Monitoring of fetuses with intrauterine growth restriction: a longitudinal study. Ultrasound Obstet Gynecol. 2001;18:564-70.
- 8. Cruz-Martinez R, Figueiras F. The role of Doppler and placental screening. Best Pract Res Clin Obstet Gynaecol. 2009;23:845-55.
- 9. Cheema R, Dubiel M, Gudmundsson SF, et al. brain sparing is strongly related to the degree of increased placental vascular impedance. J Perinat Med. 2006;34:318-22.
- 10. Arbeille P, Maulik D, Fignon A, Stale H, Berson M, Bodard S, et al. Assessment of the fetal PO2 changes by cerebral and umbilical Doppler on lamb fetuses during acute hypoxia. Ultrasound Med Biol. 1995;21:861-70.
- 11. Gramellini D, Folli MC, Raboni S, Vadora E, Merialdi A. Cerebral-umbilical Doppler ratio as a predictor of adverse perinatal outcome. Obstet Gynecol. 1992;79:416-20.
- 12. Thiebaugeorges O, Ancel PY, Goffinet F, Bréart G, for the EPIPAGE group. A population-based study of 518 very preterm neonates from high-risk pregnancies: prognostic value of umbilical and cerebral artery Doppler velocimetry for mortality before discharge and severe neurological morbidity. Eur J Obstet Gynecol Reprod Biol. 2006;128:69-76.
- 13. Jain M, Farooq T, Shukla RC. Doppler cerebroplacental ratio for the prediction of adverse perinatal outcome. Int J Gynaecol Obstet. 2004;86:384-5.
- 14. Baschat AA, Gembruch U. The cerebroplacental Doppler ratio revisited. Ultrasound Obstet Gynecol. 2003;21:124-7.
- 15. Maeda Mde F, Nomura RM, Niigaki JI, Miyadahira S, Zugaib M. Relação cerebroplacentária e acidemia ao nascimento em gestações com insuficiência placentária detectada antes da 34Ş semana de gestação. Rev Bras Ginecol Obstet. 2010;32:510-5.
- 16. Mari G, Hanif F, Treadwell MC, Kruger M. Gestational age at delivery and Doppler waveforms in very preterm intrauterine growth-restricted fetuses as predictors of perinatal mortality. J Ultrasound Med. 2007;26:555-9.
- 17. Mari G, Deter RL, Carpenter RL, Rahman F, Zimmerman R, Moise Jr KJ, et al. Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell alloimmunization. Collaborative Group for Doppler Assessment of the Blood Velocity in Anemic Fetuses. N Engl J Med. 2000;342:9-14.
- 18. Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163-8.
- 19. Cruz-Martínez R, Figueras F, Hernandez-Andrade E, Oros D, Gratacos E. Fetal brain Doppler to predict cesarean delivery for nonreassuring fetal status in term small-for-gestational-age fetuses. Obstet Gynecol. 2011;117:618-26.
- 20. Odibo AO, Riddick C, Pare E, Stamilio DM, Macones GA. Cerebroplacental Doppler ratio and adverse perinatal outcomes in intrauterine growth restriction: evaluating the impact of using gestational age-specific reference values. J Ultrasound Med. 2005;24:1223-8.
- 21. Bahado-Singh RO, Kovanci E, Jeffres A, Oz U, Deren O, Copel J, et al. The Doppler cerebroplacental ratio and perinatal outcome in intrauterine growth restriction. Am J Obstet Gynecol. 1999;180(3 Pt 1):750-6.
- 22. Piazze J, Padula F, Cerekja A, Cosmi EV, Anceschi MM. Prognostic value of umbilical-middle cerebral artery pulsatility index ratio in fetuses with growth restriction. Int J Gynaecol Obstet. 2005;91:233-7.
- 23. Murata S, Nakata M, Sumie M, Sugino N. The Doppler cerebroplacental ratio predicts non-reassuring fetal status in intrauterine growth restricted fetuses at term. J Obstet Gynaecol Res. 2011;37:1433-7.
- 24. Mari G, Hanif F, Kruger M, Cosmi E, Santolaya-Forgas J, Treadwell MC. Middle cerebral artery peak systolic velocity: a new Doppler parameter in the assessment of growth-restricted fetuses. Ultrasound Obstet Gynecol. 2007;29:310-6.
- 25. Ortigosa C, Nomura RM, Costa VN, Miyadahira S, Zugaib M. Fetal venous Doppler in pregnancies with placental dysfunction and correlation with pH at birth. J Matern Fetal Neonatal Med. 2012;25:2620-4.
- 26. Baschat AA, Gembruch U, Reiss I, Gortner L, Weiner CP, Harman CR. Relationship between arterial and venous Doppler and perinatal outcome in fetal growth restriction. Ultrasound Obstet Gynecol. 2000;16:407-13.
- 27. Crispi F, Hernandez-Andrade E, Pelsers MM, Plasencia W, Benavides-Serralde JA, Eixarch E, et al. Cardiac dysfunction and cell damage across clinical stages of severity in growth-restricted fetuses. Am J Obstet Gynecol. 2008;199:254. e1-8.
- 28. Nomura RM, Cabar FR, Costa VN, Miyadahira S, Zugaib M. Cardiac troponin T as a biochemical marker of cardiac dysfunction and ductus venosus Doppler velocimetry. Eur J Obstet Gynecol Reprod Biol. 2009;147:33-6.
Publication Dates
-
Publication in this collection
09 Sept 2013 -
Date of issue
Aug 2013
History
-
Received
19 Oct 2012 -
Accepted
11 Feb 2013