Abstracts
In order to evaluate atypical aspects of hepatocellular carcinoma at computed tomography and magnetic resonance imaging, we have retrospectively evaluated 100 patients with diagnosed hepatocellular carcinoma, based on combined imaging studies, laboratory results, biopsy and surgery. We have selected those cases with atypical findings at computed tomography or magnetic resonance imaging, including cystic lesions, bleeding tumors, with calcifications, with spontaneous regression, pedunculated tumors, hypovascular lesions, giant hepatocellular carcinomas, and those with unusual local invasiveness. The hepatocellular carcinoma is the most usual primary malignant lesion of the liver and usually it has a typical aspect and is associated with hepatic cirrhosis. However, in a significant number of cases, some uncommon findings can be responsible for a delayed diagnosis.
Hepatocellular carcinoma; Liver; Atypical findings; Ultrasound; Computed tomography; Magnetic resonance imaging
O objetivo deste trabalho foi descrever e ilustrar aspectos incomuns do hepatocarcinoma na tomografia computadorizada e ressonância magnética. A partir da análise retrospectiva de 100 casos de pacientes com hepatocarcinoma diagnosticado por análise combinada de exames de imagem, dosagem de alfa-feto-proteína, biópsia percutânea ou ressecção cirúrgica, selecionamos aqueles com apresentação atípica em um ou mais métodos de imagem ou aqueles com evolução não usual, ilustrando os seus principais aspectos de imagem. Entre os casos apresentados, escolhemos pacientes com hepatocarcinomas císticos, hemorrágicos, rotos e causando hemoperitônio, calcificados, com regressão espontânea, exofíticos, hipovasculares, gigantes e com disseminação não usual. O hepatocarcinoma é o tumor maligno mais comum do fígado e freqüentemente tem apresentação típica e associada à cirrose hepática. Porém, em alguns casos, apresentações atípicas podem retardar o seu diagnóstico.
Hepatocarcinoma; Fígado; Aspectos atípicos; Ultra-sonografia; Tomografia computadorizada; Ressonância magnética
ICONOGRAPHIC ESSAY
Unusual presentations of hepatocellular carcinoma: an iconographic essay* * Study developed at Scopo Diagnóstico, Hospital São Luiz Service of US/CT/MRI, São Paulo, SP.
Giuseppe D'IppolitoI; Luiz de Abreu JuniorII; Maria Lucia BorriII; Mário de Melo Galvão FilhoII; Luiz Guilherme C. HartmannII; Angela Maria Borri WoloskerII; Marcelo RibeiroIII; Marcelo Zindel SalemIV; Adriano MisiaraV
IAdjunct Professor, Department of Imaging Diagnosis, Universidade Federal de São Paulo-Escola Paulista de Medicina, Radiologist responsible for the Service of US/CT/MRI of Hospital São Luiz
IIMD Radiologists at the Sector of Imaging Diagnosis of the Hospital São Luiz
IIIPhD in Surgical Gastroenterology by the Universidade Federal de São Paulo-Escola Paulista de Medicina
IVPhD in Surgical Gastroenterology by the Faculdade de Medicina da Universidade de São Paulo
VMaster degree in Surgical Gastroenterlogy by the Universidade Federal de São Paulo-Escola Paulista de Medicina
Mailing address Mailing address: Prof. Dr. Giuseppe D'Ippolito Rua Professor Filadelfo Azevedo, 617, ap. 61, Vila Nova Conceição São Paulo, SP, Brasil 04508-011 E-mail: giuseppe_dr@uol.com.br
ABSTRACT
In order to evaluate atypical aspects of hepatocellular carcinoma at computed tomography and magnetic resonance imaging, we have retrospectively evaluated 100 patients with diagnosed hepatocellular carcinoma, based on combined imaging studies, laboratory results, biopsy and surgery. We have selected those cases with atypical findings at computed tomography or magnetic resonance imaging, including cystic lesions, bleeding tumors, with calcifications, with spontaneous regression, pedunculated tumors, hypovascular lesions, giant hepatocellular carcinomas, and those with unusual local invasiveness. The hepatocellular carcinoma is the most usual primary malignant lesion of the liver and usually it has a typical aspect and is associated with hepatic cirrhosis. However, in a significant number of cases, some uncommon findings can be responsible for a delayed diagnosis.
Keywords: Hepatocellular carcinoma; Liver; Atypical findings; Ultrasound; Computed tomography; Magnetic resonance imaging.
INTRODUCTION
The hepatocellular carcinoma is the most usual primary malignant tumor of the liver and is frequently associated with hepatic cirrhosis. About 10% of the patients with hepatic cirrhosis develop hepatocellular carcinoma and more than 90% of the patients with this tumor carry some form of chronic hepatopathy(1,2). The higher prevalence of viral hepatitis has caused an increase in the frequency of hepatocellular carcinoma incidence in our population. Screening Programs in patients with chronic hepatitis virus infection and chronic non-viral hepatitis, have increased the early detection of hepatocellular carcinoma, with the periodical application of alpha-fetoprotein tests and abdominal ultrasound (US) every six months(3,4).
The hepatocellular carcinoma aspect in imaging studies is well known and is highly specific, allowing a safe diagnosis when this entity is associated with signs of chronic hepatitis. On the other hand, despite some authors consider that any hepatic lesion in a cirrhotic liver not fulfilling the criteria for a cyst or hemangioma should be considered as hepatocellular carcinoma unless contrary proven(2), a number of evidences have recently appeared in the literature indicating that certain hypervascular lesions occurring in cirrhotic livers may be reversible perfusion defects, with no pathological meaning(5,6). Additionally, the previous concept that hemangiomas were unusual in cirrhotic livers has been changed by reports on frequent hemangiomas in patients with chronic hepatopathy(7).
Therefore, it is important to recognize both the typical and atypical findings aspects of the hepatocellular carcinoma in the different methods of imaging diagnosis, mainly computed tomography (CT) and magnetic resonance imaging (MRI), aiming at improving these tools efficacy and allowing a possibly non-invasive and safe diagnosis while reducing the duration of treatment.
Our objective was to demonstrate the main atypical and less frequent findings of the hepatocellular carcinoma, by means of studies selected from 100 cases. The diagnosis of hapatocellular carcinoma was defined by a combination of results of imaging studies, alpha-fetoprotein blood test, percutaneous biopsies and surgical resections.
TYPICAL ASPECTS
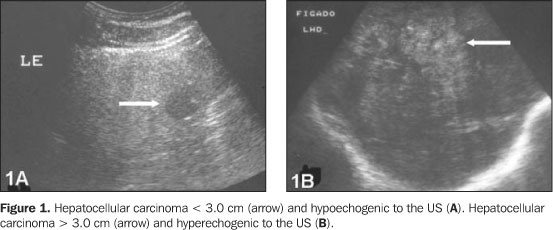
At US, the small hepatocellular carcinoma, < 3.0 cm, is shown as a hypoechogenic, homogeneous and well defined lesion (Figure 1A) The lesions > 3.0 cm in diameter usually present hyperechogenic and heterogeneous due the combined presence of necrosis, hemorrhage, fat, fibrosis and sinusoidal dilatation (Figure 1B)(8). In some cases, it is possible to identify a hypoechogenic halo representing the fibrotic capsule (Figure 2A)(2). It is important to remember that only half of hepatocellular carcinomas are identified at US when the cirrhosis process is advanced(9).
The hepatocellular carcinoma may be classified according to its macroscopic aspect as follows: a) expansile, single nodular type, well defined, encapsulated and with better prognosis(10), representing about 50% of hepatocellular carcinomas (Figure 2); b) infiltrating, consisting of a lesion with irregular although well defined borders, without capsule and frequently presenting vascular invasion (Figure 3); c) multifocal, represented by multiple nodules scattered in many hepatic segments (Figure 4)(11). The CT scan and MRI studies allow to characterize each of these findings.
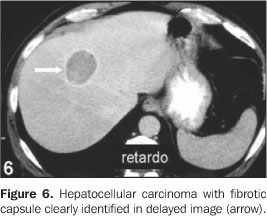
At CT, the expansile hepatocellular carcinoma is a hypodense, isodense or hyperdense lesion, depending on its constitution. The iron or copper accumulation inside the lesion as well as areas of bleeding, give the lesion a hyperdense aspect. The presence of areas of necrosis, fat and glycogen is responsible for the low values of lesion attenuation(12). After the contrast injection, typically an intense enhancement predominating in the arterial phase is observed, decreasing gradually afterwards. (Figure 5). When the fibrotic capsule is present, an enhancement is observed in the more delayed phases. (Figure 6). In large lesions, it is possible to identify a mosaic enhancement pattern resulting from the presence of areas of fibrosis, hemorrhage, arteriovenous anastomosis and intratumoral necrosis (Figure 7)(2). A predominantly arterial enhancement is observed in about 80% of the lesions, representing its irrigation by the hepatic artery and its differentiation degree(13).
In the last two decades, preceding the advent of the spiral CT and dynamic MRI, the Lipiodol® arteriography followed by abdominal CT was considered the most sensible pre-surgical method for detection of hepatocellular carcinoma(14,15). The abdominal CT scan performed between two and four weeks, after intra-arterial injection of liposoluble contrast, demonstrates the contrastation of tumoral nodules (Figure 5B)(16). More recent studies have proved that the spiral and multislice CT, as well as the contrast-enhanced MRI present sensitivity similar or superior to Lipiodol® CT(17,18); this method is reserved only for therapeutic indications, combining the use of liposoluble contrast media with the intra-arterial injection of chemotherapic substances(19). It is interesting to observe that, in some cases, the hepatocellular carcinoma can be identified only by Lipiodol® CT and, in others, only by the spiral CT (Figure 8); in these cases, the arterial CT presents false-negative results due to the preferentially portal irrigation in well differentiated lesions(18).
In the MRI, the expansile hepatocellular carcinoma is usually hyperintense in T1 (61%) and in T2 (75%) (Figures 9 and 10). The T1 signal hyperintensity is due to the presence of Cooper, fat or blood inside the lesion, combined with the presence of zinc in the hepatic parenchyma(20,21)The hypersignal in the T2 weighted images is due to peliosis and hypervascularization(22).The fibrotic capsule tends to be hypointense in the T1 and T2 weighted images and with delayed enhancement (Figures 2C and 2D). After the injection of paramagnetic contrast media, the hepatocellular carcinoma presents an enhancement pattern similar to that observed in tomographic studies (Figure 9)(2).
UNUSUAL ASPECTS
In our experience, about 20% of the hepatocellular carcinomas do not present the above mentioned aspects and have unusual presentations.
Giant hepatocellular carcinoma Making systematic use of screening methods, most of hepatocellular carcinomas are diagnosed with diameter of < 5.0 cm(23). However, it is still possible to find large lesions in its initial presentation. (Figure 10). Even when the tumor is large, the patient may benefit from the surgical resection, provided there is no sign of distant dissemination. In these cases, the prognosis is apparently similar to those of patients carrying small, non-disseminated lesions(24). But, it is important to remember that large tumors, mainly those occupying four or more hepatic segments, present higher risk of spontaneous disruption(25).
Hepatocellular carcinoma with spontaneous regression There are many papers in the literature, demonstrating about 30 cases of hepatocellular carcinoma with spontaneous regression and disappearance (Figure 11)(2628), even in the presence of distant metastases(29,30). In spite of various hypotheses formulated, for example, tumoral irrigation deficiency(27,28), none of them seems to be completely satisfactory(26).
Cystic hepatocellular carcinoma The cystic presentation of the hepatocellular carcinoma is extremely rare(31), only four cases were described in the literature up to 2000(32). In such cases, the lesion had a multilocular aspect in a non-cirrhotic liver(3134). The cystic hepatocellular carcinoma should be differentiated from that large and with central necrosis, as apparently they are distinct forms of presentation (Figure 12).
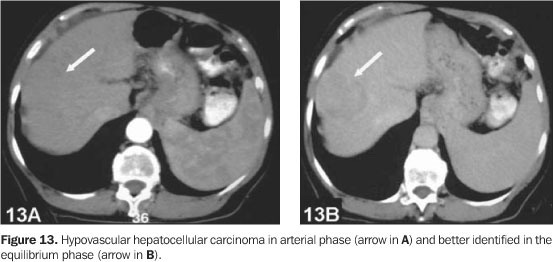
Hypovascular hepatocellular carcinoma The tumoral lesion is predominantly irrigated by the arterial system; but well differentiated tumors may present preferably portal irrigation, which also is related to the degree of hepatic cirrhosis (Figure 13)(13).
Bleeding hepatocellular carcinoma The intratumoral bleeding is not frequent and usually is a result of local ischemia due to the rapid growth of the lesion(35). The hemoperitoneum subsequent to bleeding of the hepatocellular carcinoma occurs in 515% of the cases (Figure 14)(36). The tumors carrying higher risk of bleeding are those located in the left lobe, those of larger diameter, with minimal thickness of the peritumoral parenchyma, with high Child-Pugh score and high transaminases level, and those with high prothrombin time(37). The presence of blood inside the lesion can be characterized by hyperdense areas at CT studies and hyperintense in T1 weighted images(38).
Calcified hepatocellular carcinoma As previously mentioned, the hepatocellular carcinoma may necrose and bleed, which leads to the appearance of dystrophic calcifications(12). Calcifications may occur in 7.525% of the hepatocellular carcinomas(12,39), but, in our studies only 5% of the patients studied presented calcifications (Figure 15). It is important to remember that the presence of liver calcification without textural or local perfusional changes should be considered as being of probable residual origin(40).
Hepatocellular carcinoma with fat In spite of the hepatocellular carcinoma lipomatous transformation being frequently described(8,41)and fat being observed in the tumor cells cytoplasm(12), its identification is not frequent in imaging studies(39,42). The presence of focal deposit of fat in the hepatocellular carcinoma can be detected by means of negative density determination inside the lesion region (Figure 16)(8); on the other hand, the intracellular fat is more easily detected in MRI, using gradient-echo sequences with phase opposition technique (Figure 17)(43,44).
Exophytic hepatocellular carcinoma The pedunculated hepatocellular carcinoma is extremely rare(45)and should be considered among the differential diagnoses when a solid mass in contact with a cirrhotic liver is observed (Figure 18).
Unusual dissemination Some cases of direct gastric infiltration by the hepatocellular carcinoma(46,47)were described, with extension to the right atrium via inferior vena cava(48,49), like these presented hereon (Figures 19 and 20).
CONCLUSION
The hepatocellular carcinoma usually presents typical features in imaging studies. But, in a considerable number of cases, it may surprise the radiologist with unusual aspects deserving to be known, aiming at optimizing the efficacy of the available diagnostic tools.
REFERENCES
Received May 2, 2005.
Accepted after revision May 25, 2005.
- 1. D'Ippolito G, Faria S, Szejnfeld J. Carcinoma hepatocelular: aspectos tomográficos. Radiol Bras 2000;33:295299.
- 2. Fernandez MP, Redvanly RD. Primary hepatic malignant neoplasms. Radiol Clin North Am 1998;36: 333348.
- 3. Kubota K, Ina H, Okada Y, Irie T. Growth rate of primary single hepatocellular carcinoma: determining optimal screening interval with contrast enhanced computed tomography. Dig Dis Sci 2003; 48:581586.
- 4. Borzio M, Fargion S, Borzio F, et al. Impact of large regenerative, low grade and high grade dysplastic nodules in hepatocellular carcinoma development. J Hepatol 2003;39:208214.
- 5. Ito K, Fujita T, Shimizu A, et al. Multiarterial phase dynamic MRI of small early enhancing hepatic lesions in cirrhosis or chronic hepatitis: differentiating between hypervascular hepatocellular carcinomas and pseudolesions. AJR 2004;183: 699705.
- 6. Shimizu A, Ito K, Koike S, Fujita T, Shimizu K, Matsunaga N. Cirrhosis or chronic hepatitis: evaluation of small (< or = 2-cm) early-enhancing hepatic lesions with serial contrast-enhanced dynamic MR imaging. Radiology 2003;226:550555.
- 7. Brancatelli G, Federle MP, Blachar A, Grazioli L. Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology 2001;219:6974.
- 8. Yoshikawa J, Matsui O, Takashima T, et al. Fatty metamorphosis in hepatocellular carcinoma: radiologic features in 10 cases. AJR 1988;151:717720.
- 9. Dodd GD 3rd, Miller WJ, Baron RL, Skolnick ML, Campbell WL. Detection of malignant tumors in end-stage cirrhotic livers: efficacy of sonography as a screening technique. AJR 1992;159:727733.
- 10. Lai EC, Ng IO, Ng MM, et al. Long-term results of resection for large hepatocellular carcinoma: a multivariate analysis of clinicopathological features. Hepatology 1990;11:815818.
- 11. Okuda K, Peters RL, Simson IW. Gross anatomic features of hepatocellular carcinoma from three disparate geographic areas. Proposal of new classification. Cancer 1984;54:21652173.
- 12. Stoupis C, Taylor HM, Paley MR, et al. The Rocky liver: radiologic-pathologic correlation of calcified hepatic masses. RadioGraphics 1998;18:675685; quiz 726.
- 13. Hwang GJ, Kim MJ, Yoo HS, Lee JT. Nodular hepatocellular carcinomas: detection with arterial-, portal-, and delayed-phase images at spiral CT. Radiology 1997;202:383388.
- 14. Ohishi H, Uchida H, Ohue S, et al. Computed tomography detection of small daughter nodules in hepatocellular carcinoma after iodized oil infusion into the hepatic artery. J Comput Tomogr 1988;12: 129134.
- 15. Choi BI, Park JH, Kim BH, Kim SH, Han MC, Kim CW. Small hepatocellular carcinoma: detection with sonography, computed tomography (CT), angiography and Lipiodol-CT. Br J Radiol 1989;62: 897903.
- 16. Lencioni R, Pinto F, Armillotta N, et al. Intrahepatic metastatic nodules of hepatocellular carcinoma detected at lipiodol-CT: imaging-pathologic correlation. Abdom Imaging 1997;22:253258.
- 17. Zheng XH, Guan YS, Zhou XP, et al. Detection of hypervascular hepatocellular carcinoma: comparison of multi-detector CT with digital subtraction angiography and Lipiodol CT. World J Gastroenterol 2005;11:200203.
- 18. Nakayama A, Imamura H, Matsuyama Y, et al. Value of lipiodol computed tomography and digital subtraction angiography in the era of helical biphasic computed tomography as preoperative assessment of hepatocellular carcinoma. Ann Surg 2001;234:5662.
- 19. Colagrande S, Fargnoli R, Dal Pozzo F, Bindi A, Rega L, Villari N. Value of hepatic arterial phase CT versus lipiodol ultrafluid CT in the detection of hepatocellular carcinoma. J Comput Assist Tomogr 2000;24:878883.
- 20. Koushima Y, Ebara M, Fukuda H, et al. Small hepatocellular carcinoma: assessment with T1-weighted spin-echo magnetic resonance imaging with and without fat suppression. Eur J Radiol 2002;41:3441.
- 21. Ebara M, Fukuda H, Kojima Y, et al. Small hepatocellular carcinoma: relationship of signal intensity to histopathologic findings and metal content of the tumor and surrounding hepatic parenchyma. Radiology 1999;210:8188.
- 22. Honda H, Kaneko K, Maeda T, et al. Small hepatocellular carcinoma on magnetic resonance imaging. Relation of signal intensity to angiographic and clinicopathologic findings. Invest Radiol 1997;32: 161168.
- 23. Hanazaki K, Kajikawa S, Shimozawa N, et al. Hepatic resection for large hepatocellular carcinoma. Am J Surg 2001;181:347353.
- 24. Regimbeau JM, Farges O, Shen BY, Sauvanet A, Belghiti J. Is surgery for large hepatocellular carcinoma justified? J Hepatol 1999;31:10621068.
- 25. Kanematsu M, Imaeda T, Yamawaki Y, et al. Rupture of hepatocellular carcinoma: predictive value of CT findings. AJR 1992;158:12471250.
- 26. Feo CF, Marrosu A, Scanu AM, et al. Spontaneous regression of hepatocellular carcinoma: report of a case. Eur J Gastroenterol Hepatol 2004;16:933936.
- 27. Lin TJ, Liao LY, Lin CL, et al. Spontaneous regression of hepatocellular carcinoma: a case report and literature review. Hepatogastroenterology 2004; 51:579582.
- 28. Uenishi T, Hirohashi K, Tanaka H, Ikebe T, Kinoshita H. Spontaneous regression of a large hepatocellular carcinoma with portal vein tumor thrombi: report of a case. Surg Today 2000;30:8285.
- 29. Ikeda M, Okada S, Ueno H, Okusaka T, Kuriyama H. Spontaneous regression of hepatocellular carcinoma with multiple lung metastases: a case report. Jpn J Clin Oncol 2001;31:454458.
- 30. Nam SW, Han JY, Kim JI, et al. Spontaneous regression of a large hepatocellular carcinoma with skull metastasis. J Gastroenterol Hepatol 2005;20:488492.
- 31. Gonwa ME, Casillas J, Livingstone AS, Robinson PG. Cystic hepatocellular carcinoma: CT findings. J Comput Assist Tomogr 1991;15:10451047.
- 32. Nagano K, Fukuda Y, Nakano I, et al. An autopsy case of multilocular cystic hepatocellular carcinoma without liver cirrhosis. Hepatogastroenterology 2000;47:14191421.
- 33. Ohtomo K, Furui S, Iio M, Kodama T, Iwasaki Y, Takaku F. Multilocular cystic hepatocellular carcinoma. Radiat Med 1984;2:164166.
- 34. Pombo F, Rodriguez E, Arnal-Monreal F. Multicystic fibrolamellar hepatocellular carcinoma. CT appearance. Clin Imaging 1993;17:6769.
- 35. Nakajima T, Moriguchi M, Watanabe T, et al. Recurrence of hepatocellular carcinoma with rapid growth after spontaneous regression. World J Gastroenterol 2004;10:33853387.
- 36. Akriviadis EA. Hemoperitoneum in patients with ascites. Am J Gastroenterol 1997;92:567575.
- 37. Chen CY, Lin XZ, Shin JS, Lin CY, Leow TC, Chang TT. Spontaneous rupture of hepatocellular carcinoma. A review of 141 Taiwanese cases and comparison with nonrupture cases. J Clin Gastroenterol 1995;21:238242.
- 38. Palácio GAS, Bianco FD, Domenicis Júnior O, D'Ippolito G. Ruptura hepática espontânea e traumática: aspectos tomográficos e do tratamento minimamente invasivo. Rev Imagem 2003;25: 287292.
- 39. Stevens WR, Johnson CD, Stephens DH, Batts KP. CT findings in hepatocellular carcinoma: correlation of tumor characteristics with causative factors, tumor size, and histologic tumor grade. Radiology 1994;191:531537.
- 40. Bezerra A, D'Ippolito G, Martelli P, Pinto G, Galvão M, Szejnfeld J. Calcificações hepáticas: freqüência e significado. Radiol Bras 2003;36:199205.
- 41. Hirai K, Aoki Y, Majima Y, et al. Magnetic resonance imaging of small hepatocellular carcinoma. Am J Gastroenterol 1991;86:205209.
- 42. Freeny PC, Baron RL, Teefey SA. Hepatocellular carcinoma: reduced frequency of typical findings with dynamic contrast-enhanced CT in a non-Asian population. Radiology 1992;182:143148.
- 43. Outwater EK, Blasbalg R, Siegelman ES, Vala M. Detection of lipid in abdominal tissues with opposed-phase gradient-echo images at 1.5 T: techniques and diagnostic importance. RadioGraphics 1998;18:14651480.
- 44. Siegelman ES, Outwater EK. MR imaging techniques of the liver. Radiol Clin North Am 1998; 36:263286.
- 45. Kimura H, Inoue T, Konishi K, et al. Hepatocellular carcinoma presenting as extrahepatic mass on computed tomography. J Gastroenterol 1997;32: 260263.
- 46. Fujii K, Nagino M, Kamiya J, et al. Complete resection of hepatocellular carcinoma with direct invasion to the stomach remnant. J Hepatobiliary Pancreat Surg 2004;11:441444.
- 47. Maruyama A, Murabayashi K, Hayashi M, et al. Hepatocellular carcinoma complicated by gastrointestinal hemorrhage caused by direct tumor invasion of stomach. J Hepatobiliary Pancreat Surg 1999;6:9093.
- 48. Novotny VM, van der Hulst VP, van der Wouw PA, Blaauwgeers JL, Frissen PH. An unusual presentation and way to diagnose hepatocellular carcinoma. Neth J Med 2004;62:254256.
- 49. Lazaros G, Samara C, Nikolakopoulou Z, Tassopoulos N. Growth of hepatocellular carcinoma into the right atrium. A case of antemortem diagnosis with magnetic resonance imaging of the heart. Acta Cardiol 2003;58:563565.
Publication Dates
-
Publication in this collection
25 May 2006 -
Date of issue
Apr 2006
History
-
Received
02 May 2005 -
Accepted
25 May 2005