Abstracts
This article, divided into three parts, had the aims of reviewing the most common upper-limb malformations and describing their treatments. In this first part, failure of formation is discussed. The bibliography follows after the first part.
Congenital Abnormalities; Upper Extremity; Upper Extremity Deformities, Congenital
Este artigo, dividido em três partes, tem por objetivo rever as deformidades congênitas mais comuns que afetam os membros superiores e descrever seus tratamentos. Nesta primeira parte, discute-se as falhas de formação. A bibliografia segue contínua a partir da primeira parte.
Anormalidades Congênitas; Extremidade Superior; Deformidades Congênitas das Extremidades Superiores
UPDATING ARTICLE
Congenital deformities of the upper limbs. Part I: failure of formation
Edgard Novaes França Bisneto
Attending Physician in the Hand Group, Institute of Orthopedics and Traumatology, Hospital das Clínicas, Medical School, University of São Paulo, São Paulo, Brazil
Correspondence
ABSTRACT
This article, divided into three parts, had the aims of reviewing the most common upper-limb malformations and describing their treatments. In this first part, failure of formation is discussed. The bibliography follows after the first part.
Keywords: Congenital Abnormalities; Upper Extremity; Upper Extremity Deformities, Congenital/history
INTRODUCTION
Congenital abnormalities affect between 1 and 2% of live births. Of these, around 10% have upper-limb deformities(1-3). Some of these deformities occur in isolation, but there are associations with systemic syndromes(4) that may involve blood dyscrasia, cardiopathies, central nervous system (CNS) malformations, digestive tract malformations or delayed neuropsychomotor development. These syndromes include Holt-Oram, Fanconi anemia, TAR, Apert, VACTER-L, Poland, Cornelia de Lange, Nager, etc(1). Recognizing and treating these conditions should always precede dealing with limb deformities(1). It is recommendable that all children diagnosed as presenting congenital deformities and their parents should undergo genetic assessment.
Child development is considered to be a process that starts within the uterus and involves physical growth, neurological maturation and construction of children's cognitive, social, behavioral and affective skills, thereby making them capable of responding to their needs and the needs of their environment(5). The first years of life are considered to be critical for child development, given that there is greater cerebral plasticity, which favors development of all of children's potential. Neuronal plasticity is reinforced in the developing brain, and appropriate experience during this period is fundamental for achieving adequate functioning of the neural systems(5). Because of this plasticity, adaptation to upper-limb deformity will take place, and the child's hand surgeon or therapist should advise the parents about this. The question then will be why treatment should be administered. The response also lies within the concept of cerebral plasticity: what motor capacity potential might the child attain in adulthood if the deformity is corrected, compared with non-treatment of the deformity? Obviously, the response will differ according to the situation. The present author takes the view that, if the correction of the deformities is taken together with the development of the body layout and movement coordination, the functional results in adulthood will be better than if no correction is provided, or it is done late. However, some authors have taken the view that this hypothesis does not have any scientific basis and have advocated a surgical approach applied later on, since the anatomical structures will be larger, which facilitates the surgical approach(6).
The emotional factors relating to congenital malformations of the upper limbs also have to be taken into consideration. Parents generally carry a feeling of blame and responsibility for their children's deformities. Such conditions often lead to marital and financial problems for the parents, and their appearance needs to be considered to be an event that permanently alters family life(1). Adolescents with congenital deformities are also the target of jokes at school and they tend to avoid social contact. The present author believes that all patients with congenital deformities should be referred for psychological or psychiatric assessment.
EMBRYOLOGY
Development of the limbs starts early on, at the time of embryogenesis. The buds of the upper limbs can be identified 26 days after fertilization and reach a length of 20 to 22 mm around the 53rd day of pregnancy(7). The stimulus for bud formation is provided through secretion of a protein named sonic hedgehog or Shh, by the notochord(8). The great majority of congenital deformities arise between the fourth and eighth weeks of pregnancy. After this period, the structured that have already formed mature and grow(7) (Figure 1).
The buds form through invagination of the mesoderm under the ectoderm. The cells of the somatic mesoderm will form the muscles, nerves and vessels. The cells of the so-called lateral plate mesoderm will form the bones, cartilage and tendons(7). Three axes of formation become established:
a. Proximodistal: regulated by the apical ectodermal ridge (AER). This is the ectodermal tissue that covers the mesodermal bud and promotes its differentiation. Experimental removal of this tissue in rates was found to generate transverse deformities(7).
b. Anteroposterior: regulated by the zone of polarizing activity (ZPA). This regulates growth in the pre and post-axial radioulnar direction. Failure in this regulation may give rise to mirror hand or polydactyly(8).
c. Dorsoventral: regulated by Wnt (wingless type MMTV), which differentiates between the dorsum and palm of the hand. Abnormalities of this regulation are responsible for palm duplication in humans(8).
CLASSIFICATION
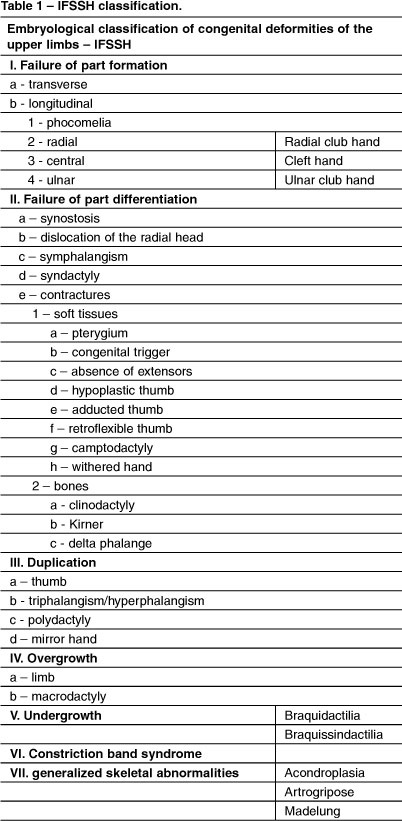
There are several classification systems for congenital deformities of the upper limbs(3,9). The best known system is the Swanson classification of 1976, with modification in 1983(2). This is based on defects during the embryonic phase and is recognized by the IFSSH (International Federation of Societies for Surgery of the Hand) (Table 1).
FAILURE OF FORMATION OF THE PARTS
1 - Transverse
Congenital amputations can occur at any level: Amelia - absence of a limb; hemimelia - absence of the forearm or hand; acheiria - absence of the hand; adactyly and aphalangia - absence of the fingers and phalanges(10).
These are differentiated from congenital constriction syndrome by the presence of hypotrophy proximally to the stump and absence of other constriction points(10).
There are few surgical options, and fitting a prosthesis should be considered, although there may be lack of adherence to treatment and a constant need for adjustment of the cartridges in children.
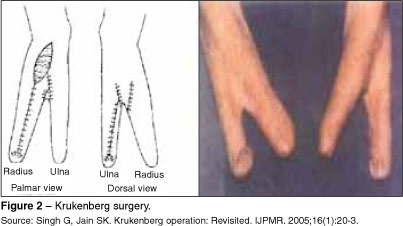
Amputations below the elbow are more common(3), and for this condition, Krukenberg surgery has been described. In this, the radius is separated from the ulna, which takes on the function of a pincer to pick up objects(11). Krukenberg surgery is little used around the world, mainly in centers in Germany and India, and generally after traumatic amputation. The main criticism of the procedure lies in its cosmetic appearance. For this reason, the present author avoids indicating this procedure, even though good functional results have been described in the literature(11) (Figure 2).
In situations of adactyly, microsurgical transplantation of the hallux and/or the second toe needs to be considered, with the aim of constructing a finger pincer(12). In our setting, there is still much resistance, both among the patients and among the multiprofessional teams who follow up these children, with regard to accepting this procedure.
2 - Longitudinal
a - Phocomelia
Phocomelia is defined as the absence of an intercalary segment. It may be complete - hand inserted in the trunk, with absence of the upper arm and forearm; proximal - absence or hypoplasia of the upper arm, with forearm and hand inserted in the trunk; or distal - hand inserted in the arm(10). Phocomelia is very rare and its prevalence increased by 60% with the use of thalidomide during the first trimester of pregnancy(3). The preferred treatment consists of fitting a prosthesis, and surgery is reserved for facilitating the use of prostheses(3,10).
b - Radial club hand: dysplasia of the radius
Radial club hand or congenital absence of the radius is a complex pre-axial deformity that affects not only the skeleton but also all of the pre-axial structures of the upper limb(13). Other abnormalities have also been reported, such as in the glenoid, humeral head, coronoid fossa, capitellum and distal humerus. The range of motion (ROM) of the elbow may be diminished(13).
The forearm is short because the ulna is also shorter: on average, 60% of the normal size(13). The diaphysis of the ulna may be curved towards the radius. The radius may be totally or partially absent. The radiocarpal joint does not exist, the ulnar head is subluxated and the triangular fibrocartilage complex does not exist(13). The trapezium, scaphoid and first metacarpal may be absent or partially present. Alterations to the capitate, trapezoid, semilunar, pyramidal and pisiform are rare(13).
The brachial biceps muscle is frequently abnormal and is inserted in the lacertus fibrosus. Other abnormalities are observed in the deltoid, pectoralis major and brachialis(13). In the forearm, the abnormalities are proportional to the absence of the radius and affect the radial flexion-pronation musculature. The brachioradialis, supinator and small finger extensor are absent or hypotrophic. The short and long radial extensors of the carpus may be present. The extrinsic and intrinsic musculature of the thumb is absent or hypotrophic, even in the presence of the thumb(13).
The brachial plexus is normal. There are abnormalities of the musculocutaneous nerve and the radial nerve generally ends at the elbow. The median nerve makes up for the absence of the radial nerve(13). The radial artery is absent or hypoplastic. Distal perfusion is supplied by the ulnar artery or, in some cases, by persistence of the median artery(13).
Radial club hand may arise as an isolated alteration, generally unilaterally; however, it is frequently associated with other syndromes: Fanconi anemia, TAR, Lewis, Nager, Roberts, VACTER-l, Holt-Oram and trisomy 18, among others(13,14). Although rare, affecting between 1:30,000 and 1:100,000 live births, it is considered to be the commonest deformity of longitudinal formation(13,14).
The classification most used for radial club hand is the system described by Bayne and Klug(13,14) (Table 2):
Type I - Radius apparently normal, but shorter, since the distal epiphysis takes longer to appear and has lower potential for growth.
Type II - Hypoplastic radius. Abnormalities in the proximal and distal epiphyses, resulting in a miniature radius.
Type III - Absence of the proximal or distal third. Absence of the distal third is more common. The ulna is hypertrophied and angled radially.
Type IV - Complete absence of the radius. This is the commonest and severest form.
James and Bednar(14) modified this classification, so as to include cases of absence of the thumb with a normal radius(3).
Conservative treatment with placement of a series of orthoses and stretching are recommended from the time of birth, independent of the type of deformity. For type I and II patients, this may be the only type of treatment. In cases in which there is angling greater than 20° or significant shortening of the radius, the radial extensors of the carpus can be transferred to the ulnar extensor of the carpus and, in some cases, the ulna can be stretched or epiphyseal distraction of the radius can be performed(15).
There is unanimity in the recent literature that surgery is indicated for types III and IV, and the only discussion is in relation to the technique to be used and the time at which surgery should be performed(6,10,13-19).
Centralization and radialization of the carpus are the surgical procedures most used for correcting radial club hand(13-15,17,18). In the centralization procedure, the carpus is centered on the ulna, while in the radialization procedure described by Buck-Gramcko(20) for increasing the leverage between the carpus and the ulna and impeding recurrence, the radial portion of the carpus is placed on the ulna. Recently, "ulnarization" of the carpus was described, in which the carpus is displaced medially in relation to the ulna. This procedure is still only performed by very few centers and there is no backing in the literature.
It is worth emphasizing the study by Vilkki(21), with microsurgical transposition of the second metatarsal-phalangeal joint as a radial support for the carpus. This joint hypertrophies with time and allows flexion-extension of the wrist. However, these results were not reproduced in other centers(15) (Figure 3).
The child's growth makes it difficult to perform centralization or radialization of the carpus in only a single surgical procedure. Therefore, in these cases, pre-centralization of the carpus by means of external fixators is necessary(15,16). The age from which pre-centralization is necessary is debatable, but the present author considers that it is necessary from the age of 18 months onwards.
In situations in which reduction is difficult, there is the possibility of performing total or partial proximal carpectomy and promoting transfer of the radial extensors of the carpus to the extensor carpi ulnaris (EUC), if this is present(13-15,20).
For children over the age of 18 months at our clinic, we perform the wrist correction as two procedures. In the first, we perform pre-centralization using single-plane external fixators. The parents are instructed to promote distraction at a speed of 0.5 to 1 mm/day. After an average of four weeks, we remove the external fixators and perform centralization of the carpus over the ulna. The operation is performed by means of a bilobulated dorsal incision(13) and a longitudinal incision in the retinaculum and joint capsule. Whenever there are radial extensor tendons present, we transfer them to the ulnar portion of the carpus. In all cases of difficulty in achieving the ideal positioning of the carpus over the ulna, we have no hesitation in performing total or partial proximal carpectomy. The hand and wrist are fixed using one or two intramedullary 1.5 or 2.0 mm Kirschner wires. We do not consider it necessary to place wires inside the metacarpals. In cases in which the angle of the ulnar diaphysis is greater than 30°, we perform osteotomy on the ulna to rectify this. Immobilization from the axilla to the palm is applied for four to six weeks, followed by a nighttime orthoses during the growth phase (Figures 4 A-C and 5).
A variety of complications have been described, such as infection, skin flap distress and breakage of the Kirschner wires(13). Over the long term, practically all the cases partially relapse(13-15,19). It should be borne in mind that even with this relapse, which the parents need to be made aware of, the final result is an improvement in relation to the initial deformity (Figure 6).
Controversy persists in relation to treatments for radial club hand done during adolescence and in cases of relapse. Stretching of the ulna and correction of the residual deformities can be achieved by means of osteotomy and external fixators(19). In cases of significant angling or short forearms, the present author indicates surgical treatment with external fixators, even among adolescents. As emphasized earlier, a psychological assessment on the patient is fundamental for evaluating the patient's expectations in relation to the possibilities from the treatment (Figures 7 and 8).
c - Cleft hand
The cleft deformity is characterized by absence of the central rays (the second, third and fourth rays), which become differentiated at times differing from when this occurs for the first and fifth rays. Classically, such deformities are divided into typical and atypical(3) (Table 3).
The theories involving the typical and atypical forms of cleft hand differ. While the typical form is related to possible fusion of rays, the atypical form is thought to be one of the manifestations of the teratological sequence of brachysyndactyly, occurring through necrosis of the mesenchymal tissue. Thus, neither of the two forms would be correctly classified as a failure of formation(3,23).
Manske and Halikis classified cases of cleft hand based on the contracture of the first commissure(15,24):
I. Normal web - first commissure is normal.
II. Narrow web - Moderate narrowing (IIA) or severe narrowing (IIB) of the first commissure.
III. Syndactylized web - First commissure fused; syndactyly between the thumb and second finger.
IV. Merged web - First commissure included in the cleft; second finger does not exist; thumb unstable.
V. Absent web - Absence of the commissure because of absence of the thumb and the second finger.
The treatment has two objectives: to close the cleft and to reconstruct the first commissure(15). These procedures involve skin flaps, reconstruction of the natatory ligament using digital pulleys, zetaplasty, osteotomy, resection of hypoplastic fingers or transverse bones and transposition of metacarpals in the various techniques described, including Miura and Komada, and Snow and Littler(10,15,22,24). Because of the diversity of deformations, each case requires individual surgical planning (Figures 9 A-F and 10 A-E).
Conservative treatment is reserved for very severe cases, in which there is generally great functional adaptation(24) and for patients with severe cognitive deficit, which impedes adequate rehabilitation. In considering conservative treatment for a case of cleft hand, the present author recalls a phrase written by Flatt: "functionally a triumph, but socially a disaster"(24).
d - Ulnar club hand: dysplasia of the ulna
Ulnar club hand is a set of abnormalities that affects the ulnar margin of the upper limb but also affects structures on the radial margin(15). It is four to ten times rarer than radial club hand and associations with malformations of internal organs or systemic syndromes are rare(3,14). There is an association with other skeletal malformations: congenital short femur, phocomelia, hemimelia, fibular hemimelia and congenital scoliosis(14).
The hand is hypoplastic: 90% present absence of fingers, 30% show syndactyly and 70% have abnormalities of the thumb, rotated metacarpals and hypoplastic tendons and muscles(14,15). Since the radius is always present, there is support for the carpus. The forearm is short and the elbow has diminished range of motion or radiohumeral synostosis(15).
The most accepted classification is the modified Bayne system(15):
-
Normal ulna normal; alterations restricted to the hand.
-
Hypoplastic ulna; proximal and distal epiphyses present.
-
bsence of the distal ulna.
-
Total absence of the ulna.
-
Absence of the ulna with radiohumeral synostosis.
-
Abnormalities of the glenoid and humerus.
Cole and Manske(15) classified ulnar club hand according to the abnormalities of the first commissure (Figure 11):
a. First commissure and thumb normal.
b. Moderate abnormalities of the first commissure and thumb.
c. Narrowing of the first commissure, syndactyly between the thumb and second finger, thumb in the plane of the ulnar fingers, thenar hypoplasia or absence of extrinsic tendon function.
d. Absence of the thumb.
Despite the large number of abnormalities, functioning is generally good(14,15). Surgical procedures are more indicated for correction of deformities of the hand, such as syndactyly, and for reconstruction of the first commissure. In the forearm, osteotomy of the radius is performed in cases of large angular deformity or hyperpronation. Construction of single bones, in cases of distal absence of the ulna, can also be considered. Resection of the radial head has been described, but this is not recommended because of the risk of destabilization of the elbow(15,20).
REFERENCES
- 1. Kozin SH. Congenital disorders: classification and diagnosis. In: Berger RA, Weiss AP, editors. Hand surgery. Philadelphia: Lippincott Williams & Williams; 2004. p. 1405-23.
- 2. Chung MS. Congenital differences of the upper extremity: classification and treatment principles. Clin Orthop Surg. 2011;3(3):172-7.
- 3. Kozin SH. Upper-extremity congenital anomalies. J Bone Joint Surg Am. 2003;85(8):1564-76.
- 4. Smith DW. Padrões reconhecíveis de malformações congênitas. São Paulo: Manole; 1998.
- 5. Nascimento R, Piassão C. Avaliação e estimulação do desenvolvimento neuropsicomotor em lactentes institucionalizados. Rev Neurocienc. 2010;18(4):469-78.
- 6. Hung LK, Leung PC. Wong MW. Congenital hand anomalies. Principles of management. J Am Soc Surg Hand. 2002; 2(4):204-21.
- 7. Kozin SH. Embriology. In: Green DP, Pederson MD, Hotchkiss RN, Wolf SW. editors. Green´s Operative Hand Surgery. 5th ed. Philadelphia: Elsevier Churchill Livingstone; 2005. p. 1375-9.
- 8. Al-Qattan MM, Yang Y, Kozin SH. Embryology of the upper limb. J Hand Surg Am. 2009;34(7):1340-50.
- 9. Sammer DM, Chung KC. Congenital hand differences: embryology and classification. Hand Clin. 2009;25(2):151-6.
- 10. Mattar Junior R. Deformidades congênitas do membro superior. Acta Ortop Bras. 1995; 3(2):77-92.
- 11. Singh G, Jain SK. Krukenberg operation: revisited. IJPMR; 2005;16 (1):20-3.
- 12. Schenker M, Wiberg M, Kay SP, Johansson RS. Precision grip function after free toe transfer in children with hypoplastic digits. J Plast Reconstr Aesthet Surg. 2007;60(1):13-23.
- 13. D'Arcangelo M, Gupta A, Schecker LR. Radial club hand. In: Gupta A, Ray SP, Schecker LR, editors. The growing hand. Diagnosis and management of the upper extremity in children. London: Mosby; 2000. p. 147-68.
- 14. James MA, Bednar M. Deformities of the wrist and forearm. In: Green DP, Pederson MD, Hotchkiss RN, Wolf SW, editors. Green´s operative hand surgery. 5th ed. Philadelphia: Elsevier Churchill Livingstone; 2005. p. 1469-79.
- 15. Manske PR, Goldfarb CA. Congenital failure of formation of the upper limb. Hand Clin. 2009;25(2):157-70.
- 16. Sabharwal S, Finuoli AL, Ghobadi F. Pre-centralization soft tissue distraction for Bayne type IV congenital radial deficiency in children. J Pediatr Orthop.2005;25(3):377-81.
- 17. Farzan M, Mortazavi SM, Baghdadi T, Zanoosi M. Congenital radial club hand: results of centralization in 10 cases. Acta Med Iran. 2005;43(1):63-7.
- 18. Buck-Gramcko D. Radialization for radial club hand. Tech Hand Up Extrem Surg. 1999;3(1):2-12.
- 19. Kawabata H, Shibata T, Masatomi T, Yasui N. Residual deformity in congenital radial club hands after previous centralisation of the wrist. Ulnar lengthening and correction by the Ilizarov method. J Bone Joint Surg Br. 1998;80(5):762-5.
- 20. Buck-Gramcko D. Congenital disorders: radial and ulnar club hand. In: Berger RA, Weiss APC, editors. Hand Surgery. Philadelphia: Lippincott Williams & Williams; 2004. p. 1453-64.
- 21. Vilkki SK. Vascularized metatarsophalangeal joint transfer for radial hypoplasia. Semin Plast Surg. 2008;22(3):195-212.
- 22. Kay SP, McCombe D. Central hand deficiences. In: Green DP, Pederson MD, Hotchkiss RN, Wolf, SW, editors. Green´s Operative Hand Surgery. 5th ed. Philadelphia: Elsevier Churchill Livingstone; 2005.p. 1404-15.
- 23. Tonkin MA. Description of congenital hand anomalies: a personal view. J Hand Surg Br. 2006;31(5):489-97.
- 24. Kay SP, Platt A. Congenital disorders: cleft hand. In: Berger RA, Weiss APC, editors. Hand surgery. Philadelphia: Lippincott Williams & Williams; 2004. p. 1465-75.
Publication Dates
-
Publication in this collection
07 Jan 2013 -
Date of issue
Oct 2012
History
-
Received
31 Jan 2012 -
Accepted
10 Feb 2012