Abstracts
We report the case of a 48-year-old male with a 2-month history of migratory polyarthralgia, and myalgia associated with fever and weight loss; one episode of bilateral testicular pain; and unilateral pulsatile headache with thickening of the left temporal artery suggestive of temporal arteritis. The patient evolved with spontaneous left perirenal hematoma, splenic infarcts, and oliguric acute renal failure. Treatment included prednisone and cyclophosphamide. The left temporal artery and the quadriceps muscle were biopsied. Clinical, laboratorial, and radiological findings, as well as the intercurrences, led to the diagnosis of polyarteritis nodosa.
polyarteritis nodosa; systemic necrotizing vasculitis; temporal arteritis; perirenal hemorrhage
Descrevemos o caso de um paciente masculino, 48 anos, com poliartralgias e mialgias migratórias, associadas a febre e emagrecimento com dois meses de evolução; um episódio de dor testicular bilateral; e cefaleia unilateral pulsátil com espessamento de artéria temporal esquerda sugerindo arterite temporal. Na evolução, o paciente apresentou hematoma perirrenal esquerdo espontâneo, infartos esplênicos e insuficiência renal aguda oligúrica. Foi tratado com prednisona e ciclofosfamida. Foram realizadas biópsias de artéria temporal esquerda e músculo quadríceps. Os achados clínicos, laboratoriais, radiológicos e intercorrências levaram ao diagnóstico de poliarterite nodosa (PAN).
poliarterite nodosa; vasculites necrotizantes sistêmicas; arterite temporal; hemorragia perirrenal
CASE REPORT
IInternal Medicine Resident (HC-UFPR)
IIMedical Student (HC-UFPR)
IIIRheumatology Resident (HC-UFPR)
IVAttending physician (HC-UFPR)
VInternal Medicine Professor (HC-UFPR)
Correspondence to
ABSTRACT
We report the case of a 48-year-old male with a 2-month history of migratory polyarthralgia, and myalgia associated with fever and weight loss; one episode of bilateral testicular pain; and unilateral pulsatile headache with thickening of the left temporal artery suggestive of temporal arteritis. The patient evolved with spontaneous left perirenal hematoma, splenic infarcts, and oliguric acute renal failure. Treatment included prednisone and cyclophosphamide. The left temporal artery and the quadriceps muscle were biopsied. Clinical, laboratorial, and radiological findings, as well as the intercurrences, led to the diagnosis of polyarteritis nodosa.
Keywords: polyarteritis nodosa, systemic necrotizing vasculitis, temporal arteritis, perirenal hemorrhage.
INTRODUCTION
Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis that affects mainly medium-size arteries, including renal, splenic, and temporal arteries, with the potential to affect any organ. Clinical manifestations can result from the occlusion or aneuriysmatic lesion of the affected blood vessels.1,2,3 We describe the case of a patient with polyarteritis nodosa with multisystem involvement, worsen by the rupture of renal microaneurysms, and clinical manifestation that mimicked giant cell arteritis, another systemic vasculitis.
CASE REPORT
A 48-year-old male was admitted with a 2-month history of migratory polyarthralgia and myalgia. He referred fever, nocturnal diaphoresis, anorexia and an 8 kg weight loss during this period. He also referred one episode of bilateral testicular pain which subsided within two days, and severe pulsatile left temporal headache. He denied any visual symptoms. On physical examination, he presented thickening of the left temporal artery and mild hypertension, but no joint changes; neurological examination was normal.
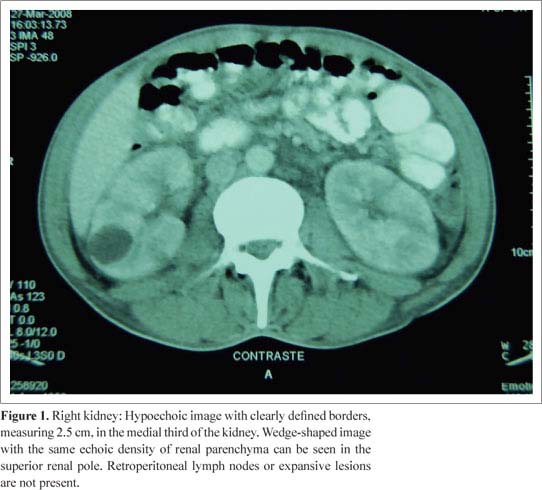
On hospital admission, the blood cell counting showed no significant abnormalities, and he had a creatinine of 1.3 mg/dL. Other tests revealed erythrosedimentation rate of 85 mm, C-reactive protein 11.3 mg/dL (reference value: up to 0.5 mg/dL), rheumatoid factor 671 IU/mL, and antineutrophil antibodies (ANCA) and ANA (antinuclear antibodies) were absent. The tuberculosis skin test (PPD skin test) was also non-reactive. Serologies for hepatitis B, C, and human immunodeficiency virus (HIV) were negative, as well as the Venereal Disease Research Laboratories (VDRL) and blood cultures. Chest X-ray, chest CT, and echocardiogram did not show any abnormalities. Abdominal CT scan showed a cortical cyst in the left kidney (Figure 1). Echo-Doppler of the temporal arteries showed old occlusion in the right artery and a hypoechoic halo in the left temporal artery.
The patient evolved with severe, diffuse abdominal pain, and the physical examination showed "board-like abdomen" and a reduction in the mean corpuscular volume (MCV) and haemoglobin. A new abdominal CT (Figure 2) showed a left perirenal hematoma measuring 13.5 x 13.5 x 7.5 cm (approximate volume of 700 mL) and images suggestive of splenic infarcts. Angio-MRI of the abdominal aorta showed the same hematoma, but no aneurysm. The patient developed oliguric acute renal failure requiring hemodialysis. Due to the suspicion of polyarteritis nodosa, treatment with prednisone, 60 mg/d (1 mg/kg), and pulse cyclophosphamide, 500 mg (adjusted for the renal function), was instituted. The patient improved clinically, as well as the inflammatory activity tests. Due to the intercurrences, biopsies were only performed when the patient was clinically stable, after four weeks of treatment. Biopsy of the right quadriceps muscle showed a perivascular inflammatory infiltrate, composed by mononuclear cells, suggestive of vasculitis. Biopsy of the left temporal artery did not show signs of vasculitis. Signs and symptoms, and laboratory findings met the criteria for PAN, according to the diagnostic classification of the American College of Rheumatology.
DISCUSSION
The clinical manifestations of PAN frequently include non-specific symptoms, such as fever, fatigue, arthralgias, and weight loss. Other symptoms depend on the organs affected. The skin is frequently involved, and it may show livedo reticularis, subcutaneous nodes, ulcers, and digital ischemia.4,5 Involvement of the nervous system is more common in mononeuritis multiplex, which occurs in 60% of the cases.4,6 Muscular involvement is also common, and it includes symptoms like myalgia and muscle weakness.7 Approximately 50% of the cases of PAN are associated with gastrointestinal manifestations, and mesenteric angina is the most common of them. Mesenteric infarction and aneurysmal rupture are rare complications, but carry a high mortality rate.4 Renal involvement, due to the presence of microaneurysms of renal and interlobar arteries, and, occasionally, of the arcuate and interlobular arteries, sparing the glomeruli, is seen in approximately 40% of the cases, and it manifests as renal failure, hypertension, and perirenal hematoma due to the rupture of microaneurysms.4,8 Although rare, acute myocardial infarction may develop as a consequence of the occlusion of a coronary aneurysm.9 There are also reports of splenic infarcts secondary to vasculitis of the splenic artery or one of its main branches. The isolated involvement of organs, such as the skin, appendix, and gall bladder, has also been described.
The diagnosis is clinical and should, ideally, always be confirmed by the biopsy of an affected organ, and usually the most accessible organ is chosen. If a site for biopsy is not available, arteriography of the renal or mesenteric blood vessels showing multiple aneurysms confirms the diagnosis.10 The American College of Rheumatology criteria for diagnostic classification have a sensitivity of 87.3% and specificity of 89.3%.11 Henegar et al., in a study published in May 2008, emphasized the diagnostic importance of negative predictive parameters to reduce the rate of false-positive.12
We reported a case of PAN with muscular, testicular, renal, splenic, and temporal artery involvement. It should be emphasized that, occasionally, orchitis is one of its manifestations.13 Due to the multisystem involvement, a series of differential diagnosis, including neoplasias and paraneoplastic syndromes, rheumatoid arthritis, as well as other vasculitis, especially giant cell arteritis, due to the findings in the temporal artery, was considered. The initial diagnostic difficulty allowed the development of potentially fatal complications, such as perirenal hematoma and acute renal failure. Spontaneous perirenal hematoma is a rare complication seen more commonly as a complication of renal cell carcinoma and renal angiomyolipoma.8 Among the vasculitis, the association with PAN has been described more often.8 Due to the intercurrences, muscular and temporal artery biopsies could only be done when the patient was stable, after the institution of treatment with high doses of corticosteroids and cyclophosphamide. Muscular biopsy was suggestive of vasculitis, but not pathognomonic of PAN. Although the left temporal artery biopsy did not show signs of vasculitis, the clinical finding of this blood vessel thickening and the echo-Doppler showing a hypoechoic halo suggested this diagnosis. Several cases of PAN with involvement of the temporal artery have been described, giving the impression that it is a frequent finding, and also an easily accessible site for diagnostic biopsy.14,15 Manifestation is similar to that of giant cell arteritis, but the incidence of severe ocular complications is lower.
PAN treatment consists of high doses of corticosteroids, which has a significant impact on survival. Oral doses of 1 mg/kg/d, or pulse therapy with 15 mg/kg IV, can be used. In severe and refractory cases, it should be associated with an immunosuppressive agent, and cyclophosphamide is the agent more commonly used. The route chosen depends on the severity of the case. Azathioprine can substitute cyclophosphamide after remission has been achieved with this drug.1,3 Clinical support for the complications of this disease is also extremely important, as well as the prevention of treatment-associated toxicity.
REFERENCES
-
1Langford CA. Treatment of polyarteritis nodosa, microscopic polyangiitis, and Churg-Strauss syndrome: Where do we stand? Arthritis & Rheumatism 2001;44(3):508-12.
-
2Gayraud M, Guillevin L, Toumelin P, Cohen P, Casassus FLP, Jarrousse B. Long-term followup of polyarteritis nodosa, microscopic polyangiitis, and Churg-Strauss syndrome. Arthritis & Rheumatism 2001;44(3):666-75.
-
3Guillevin L, Lhote F. Treatment of polyarteritis nodosa and microscopic polyangiitis. Arthritis & Rheumatism 1998;41(12):2100-5.
-
4Stone JH. Polyarteritis nodosa. Jama 2002; 288: 1632-39.
-
5Gibson LE; Su WP. Cutaneous vasculitis. Rheum Dis Clin North Am 1995;21(4):1097-113.
-
6Tervaert JW, Kallenberg C. Neurologic manifestations of systemic vasculitides. Rheum Dis Clin North Am 1993;19(4):913-40.
-
7PlumLey SG, Rubio R, Alasfar S, Jasin HE. Polyarteritis nodosa presenting as polymyositis. Semin Arthritis Rheum 2002;31(6):377-83.
-
8Daskalopoulos G, Karyotis I, Heretis I, Anezinis P, Mavromanolakis E, Delakas D. Spontaneous perirenal hemorrhage: a 10-year experience at our institution. International Urology and Nephrology 2004;36:15-9.
-
9Kastner D, Gaffney M, Tak T. Polyarteritis nodosa and myocardial infarction. Can J Cardiol 2000;16(4):515-8.
-
10Komatireddy GR, Yangco DT, Loy TS, Beale GD. Ruptured intrahepatic aneurysm as the initial manifestation of polyarteritis nodosa. J Clin Rheumatol 1998;4:333-37.
-
11Lightfoot RW Jr, Michel BA, Bloch DA, Hunder GG, Zvaifler NJ, McShane DJ, et al. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum 1990;33 (8):1088-93.
-
12Henegar C, Pagnoux C, Puéchal X, Zucker JD, Bar-Hen A, Le Guern V et al A paradigm of diagnostic criteria for polyarteritis nodosa. Arthritis & Rheumatism 2008;58(5): 1528-38.
-
13Teichman JM, Mattrey RF, Demby AM, Schmidt JD. Polyarteritis nodosa presenting as acute orchitis: a case report and review of the literature. J Urol 1993;149(5):1139-40.
-
14Hamidou MA, Moreau A, Toquet C, El Kouri D, de Faucal P, Grolleau JY. Temporal arteritis associated with systemic necrotizing vasculitis. J Rheumatol 2003;30(10):2165-9.
Perirenal hematoma and involvement of the temporal artery in a patient with polyarteritis nodosa (PAN)
Publication Dates
-
Publication in this collection
03 Aug 2009 -
Date of issue
Aug 2009
History
-
Received
21 Oct 2008 -
Accepted
12 Jan 2009