ABSTRACT
Tooth autotransplantation is an option for treating patients presenting early tooth loss. The teeth most commonly removed are the first molars, and their absence could lead to several oral health problems in patients. This transplant technique consists of the transposition and repositioning of a tooth from one area to another, in the same patient. Dental implants have high success rates, but tooth autotransplantation is less complex and less expensive, because the patient’s own tooth is used. In the context of dental rehabilitation, tooth transplantation is focused on re-establishing masticatory function and esthetics. Success rates are variable, but in the majority of cases they exceed 80%. This article aims to report the case of a patient who underwent autotransplantation of the maxillary left third molar into the maxillary right first molar position. The surgical procedure was performed on two stages. After a 3-year clinical and radiographic follow-up period, a satisfactory result was achieved with the transplanted tooth presenting a healthy pulp and periodontal tissues, reestablishing the patient’s function and esthetics.
Indexing terms:
Oral surgery; Organ transplantion; Third molar; Tooth
RESUMO
O transplante dentário autógeno (autotransplante dentário) é uma opção de tratamento para pacientes que perdem dentes precocemente. Os elementos mais comumente extraídos são os primeiros molares permanentes e a falta dos mesmos pode acarretar em diversos agravos para a saúde bucal do paciente. O autotransplante dentário consiste na transposição cirúrgica e reposicionamento de um elemento dentário, de um local da boca para outro, no mesmo indivíduo. O tratamento com implantes possui elevado índice de sucesso, mas o transplante apresenta maior praticidade e menor custo, uma vez que utiliza um órgão do próprio paciente. Assim, como a reabilitação protética, tem como função o restabelecimento da mastigação e estética. As taxas de sucesso são variáveis, mas em sua maioria ultrapassam os 80%. O presente trabalho relata o caso clínico de uma paciente submetida ao transplante do germe dental do elemento 28 para o alvéolo do elemento 16. O ato cirúrgico foi realizado com a técnica de dois estágios e após o acompanhamento clínico e radiográfico de três anos, obteve-se um resultado satisfatório e o elemento transplantado apresentou saúde pulpar e periodontal, restabelecendo a função e a estética à paciente.
Termos de indexação:
Cirurgia bucal; Transplante de órgãos; Terceiro molar; Dente
INTRODUCTION
The first permanent molars are the teeth in the oral cavity that are most frequently lost, because they are the first permanent teeth to erupt [1,2] and are often the teeth most frequently extracted in patients at an early age. The absence of this tooth may lead to migration of adjacent teeth, making it difficult to perform later rehabilitations [3]. A treatment option for patients presenting absence of the first molars, or an unfavorable prognosis for their maintenance, is tooth transplantation. This technique consists of the transfer of a tooth from one site to another, in the same person (autogenous tooth transplantation or dental autotransplantation) [4-6]. This autotransplantation procedure enables a compromised or absent tooth to be replaced by a transplanted tooth. For this purpose, impacted third molars are generally used, and they would be transferred to a prepared or existent alveolus. This treatment is also indicated for patients with congenitally absent teeth, in cases of traumatisms, iatrogenic events or when it is unfeasible to perform prosthetic restoration [3].
Dental autotransplantation consists of a treatment option with return esthetic and functional capacity, allowing the normal development of the arches, and preventing compromise of the temporomandibular joint. Moreover, it will avoid the insertion of dental prostheses or metal implants in young individuals [7]. The success rates of dental autotransplantations reported have ranged from 0 to 100%88 Kristerson L. Autotransplantation of human premolars:A clinical and radiographic study of 100 teeth. Int J Oral Surg. 1985;14(2):200-13., however, studies have pointed out a success rate of close to 80% [9-11].
The aim of this report was to present a case of dental autotransplantation with a 3-year follow-up period, performed at the School of Dentistry of the Federal University of Minas Gerais.
CASE REPORT
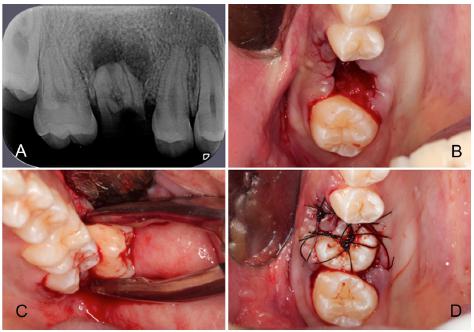
The patient G.S.V, a 17-year-old woman, melanoderma, presented to the School of Dentistry, Federal University of Minas Gerais (UFMG) in March, 2013 and was attended in the extension project of Oral Health Promotion for Adolescents. During attendance, in the clinical and radiographic exams, the presence of extensive coronal destruction of tooth 16 was verified (Figure 1A) without any possibility of performing restorative procedures, and the presence of impacted teeth 18, 28, 38 and 48.
A) Radiographic image: note the extensive coronal destruction of tooth 16, and associated periapical lesion; B) Transoperative Image: Extraction of tooth16; C) Transoperative Image: Extraction of tooth 28 (14 days after the first procedure); D) Transoperative Image: Placement of tooth 28 in the receptor bed, maintained in position by sutures (14 days after the first procedure).
After explaining the treatment possibilities to the patient (and her guardian), the patient opted to undergo dental transplantation, and was thus referred to the Residence Program in Oral and Maxillofacial Surgery and Traumatology of the “Hospital das Clinicas” of UFMG. During anamnesis, no systemic changes worthy of note were detected. In the intraoral exams, painful symptoms, edema, presence of fistula on the vestibular surface of the root remainder of tooth 16, which presented a probing depth of 2.0 mm at the vestibular surface; 2,0 mm at the palatine; 2.0 mm at the mesio-vestibular; 3.0 mm at the mesio-palatine; 5.0 mm at the disto-vestibular and 2.0 mm at the disto-palatine surfaces. Radiographic evaluation revealed the presence of periapical lesion, and by means of this analysis, measurements of the alveolus were made. Thus, the following measurements were found: 09 mm of clinical mesio-distal distance between teeth 15 and 17; and 5 mm between the alveolar bone crest and periapical lesion associated with the root remainder of tooth16. The following measurements were taken of all the third molars: the tooth equator (diameter); height of the mesial and distal cuspids; leading to tooth 28 being chosen to be transplanted, because it had dimensions compatible with those of the receptor bed.
To perform the dental transplant, the two-stage technique, under local anesthesia was used. Extraction of the root remainder of tooth 16 (Figure 1B) and later curettage of the alveolus with a view to removing the granulation tissue were performed, without intercurrences, as was planned. At the same time, the alveolus was prepared with the aid of spherical burs, by removing 04 mm in the apical direction; 01 mm in the mesial and 01 mm in the distal direction, for the purpose of suiting the receptor bed to the dimensions of the tooth to be transplanted. After two weeks, we proceeded with the transfer of tooth 28 to the alveolus of tooth 16 (Figure 1C). This tooth was extracted with great care, so that the periodontal ligament and dental pulp would not be traumatized by the surgical manipulation. The same concern was considered during insertion of tooth 28 into the previously prepared alveolus. The transplanted tooth was positioned in infra-occlusion and kept in position by means of sutures (Figure 1D).
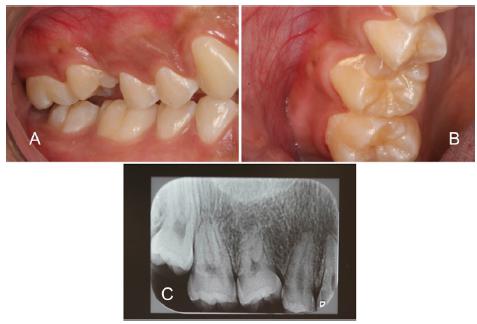
The patient was re-evaluated seven days after the surgical intervention and on clinical exam, usual healing of the surgical bed and Grade III mobility of the transplanted tooth were observed. On radiographic evaluation, the authors observed maintenance of the infra-occlusal position and aspect compatible with the post-operative period (Figure 2). Three weeks after transplantation, the tooth still presented Grade III mobility, epithelium with normal color, and no signs of gingival recession. The probing depth (PD) was evaluated and presented measurements of 2.0 mm (in the mesio-vestibular, vestibular, disto-palatine and palatine regions); and 5.0 mm (mesio-palatine and disto-vestibular regions).
On clinical exam on the 30th post-operative day, the tooth presented a normal aspect; adjacent gingival epithelium with normal color. Grade II mobility, absence of gingival recession, absence of adhesion of the distal papilla and bacterial plaque accumulation in this region. The patient was instructed to improve cleaning in the area. The PD exam presented change only at the disto-palatine and disto-vestibular surfaces, in which a PD of 3.0 mm associated with discrete bleeding was observed.
In the post-operative exam of one year, the authors clinically observed the absence: of pathological changes in the mucosa; physiological dental mobility; and satisfactory PD, less than 3.0 mm at all the surfaces of the transplanted tooth, without signs of bleeding and/or suppuration (Figures 3A, 3B). The tooth was also submitted to pulp sensitivity tests (thermal and electrical) presenting a positive response to both tests. A periapical radiographic exam was requested (Figure 3C) which enabled the authors to observe bone neoformation adjacent to the tooth in question, with an adequate level of the interproximal bone crests. After this evaluation, the patient was maintained on an annual follow-up regime, and no alterations whatever were observed in the clinical condition. At the last return (3-year postoperative follow-up) the patient presented no complaints, and all the functional and esthetic parameters observed in the previous evaluations were shown to be stable (Figure 4).
One year of post-operative follow-up. A, B) Intraoral image: side view in habitual maximum intercuspidation (A) and occlusal (B): C) Radiographic image: note the good adaptation of the transplanted tooth, with preservation of the interproximal bone crests and periodontal ligament space.
Thee-year post-operative follow-up. A,B,C) Intraoral image: side view in habitual maximum intercuspidation (A), probing depth evaluation (B), pulp sensitivity test of the transplanted tooth (C); D) Radiographic image: note maintenance of the aspects observed in the one-year follow-up evaluation.
DISCUSSION
Dental transplantation is a feasible procedure1111 Kvint S, Lindstn R, Magnussonc A, Nilssond P, Bjerkline K. Autotransplantation of teeth in 215 patients. a follow-up study. Angle Orthod. 2010;80(3):446-51. doi: 10.2319/062509-354.1.
https://doi.org/10.2319/062509-354.1...
12 Souza JG. Transplante autógeno de germe de terceiro molar. RGO, Rev Gauch Odontol. 2002;50(3):175-6.
13 Waikakul A1, Punwutikorn J, Kasetsuwan J, Korsuwannawong S. Alveolar bone changes in autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(3):01-07.doi: 10.1016/j.tripleo.2010.11.003.
https://doi.org/10.1016/j.tripleo.2010.1...
14 Jang JH, Lee SJ, Kim E. Autotransplantation of immature third molars using a computer-aided rapid prototyping model: a report of 4 cases. J Endod. 2013;39(11):1461-6. doi: 10.1016/j.joen.2013.06.026.
https://doi.org/10.1016/j.joen.2013.06.0...
15 Choi SH, Hwang CJ. Orthognathic treatment with autotransplantation of a third molar. Am J Orthod Dentofacial Orthop. 2013 Nov;144(5):737-47. doi: 10.1016/j.ajodo.2012.12.013
https://doi.org/10.1016/j.ajodo.2012.12....
16 Koszowski R, Morawiec T, Bubitek-Bogacz A. Use of the piezosurgery technique for cutting bones in the autotransplantation of unerupted third molars. Int J Periodontics Restorative Dent. 2013;33(4):477-81.doi: 10.11607/prd.0678
https://doi.org/10.11607/prd.0678...
17 Park JM, Tatad JCI, Landayan MEA, Heo SJ, Kim SJ. Optimizing third molar autotransplantation: applications of reverse engineered surgical templates and rapid prototyping of 3D teeth. J Oral Maxillofac Surg. 2014;72:1653-59. doi: 10.1016/j.joms.2014.04.012
https://doi.org/10.1016/j.joms.2014.04.0...
-1818 Kumar N, Prasad K, Lalitha RM, Ranganath K, Dexith J, Chauhan A. Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet rich fibrin: a randomized controlled clinical study. J Oral Maxillofac Surg. 2015;73(6):1042-9. doi: 10.1016/j.joms.2014.11.013
https://doi.org/10.1016/j.joms.2014.11.0...
, particularly in children and adolescents, in whom prosthetic rehabilitation and by means of implants is contra-indicated1919 Kallu R, Vinckier F, Politis C, Mwalili S, Willems G. Tooth transplantations: a descriptive retrospective study. Int J Oral Maxillofac Surg. 2005;34(7):745-55.doi: 10.1016/j.ijom.2005.03.009
https://doi.org/10.1016/j.ijom.2005.03.0...
. The teeth most commonly used for transplantation are the third molars, premolars and canines44 Ioannidou E1, Makris GP. Twelve-year follow-up of an autogenous mandibular canine Transplant.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(5):582-9.doi: 10.1016/S1079210403002609.
https://doi.org/10.1016/S107921040300260...
,55 Kim E1, Jung JY, Cha IH, Kum KY, Lee SJ. Evaluation of the prognosis and causes of failure in 182 cases of autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(1):112-9.doi: 10.1016/j.tripleo.2004.09.007.
https://doi.org/10.1016/j.tripleo.2004.0...
,88 Kristerson L. Autotransplantation of human premolars:A clinical and radiographic study of 100 teeth. Int J Oral Surg. 1985;14(2):200-13.,2020 Nethander G, Andersson JE, Hirsch JM. Autogenous free tooth transplantation in man by a 2-stage operation technique. A longitudinal intra-individual radiographic assessment. Int J Oral Maxillofac Surg. 1988;17(5):330-6., however, other teeth, including the supernumerary type may be used for this purpose2121 Andreasen JO. Atlas de reimplante e transplante de dentes. São Paulo: Medicina Panamericana; 1993..
The cost of performing transplantations must also be considered, since it is lower than that of rehabilitation with implants, or even with dental prostheses, because no high cost materials are used99 Mejàre B. A prospective study on transplantation of third molars with complete root formation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(2):231-8.doi: 10.1016/S107921040300461X
https://doi.org/10.1016/S107921040300461...
,2222 Yan Q, Li B, Long X. Immediate autotransplantation of mandibular third molar in China. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:436-440. doi: 10.1016/j.tripleo.2010.02.026
https://doi.org/10.1016/j.tripleo.2010.0...
. Another option for the treatment of tooth loss is the use of dental prostheses, however transplantation of the natural tooth has the advantage of impeding alveolar bone resorption; promoting its formation1313 Waikakul A1, Punwutikorn J, Kasetsuwan J, Korsuwannawong S. Alveolar bone changes in autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(3):01-07.doi: 10.1016/j.tripleo.2010.11.003.
https://doi.org/10.1016/j.tripleo.2010.1...
, and preserving its volume and morphology2323 Thomas S, Turner SR, Sandy JR. Autotransplantation of teeth: is there a role? Br J Orthod. 1998;25(4):275-82. doi: 10.1093/ortho/25.4.275
https://doi.org/10.1093/ortho/25.4.275...
.
The recommendation is for the donor tooth root to have 2/3 to 3/4 of the root formed, to favor revascularization and the complementary process of rhizogenesis2121 Andreasen JO. Atlas de reimplante e transplante de dentes. São Paulo: Medicina Panamericana; 1993.,2424 Lundberg T, Isaksson S. A clinical follow-up study of 278 autotransplanted teeth. Br J Oral Maxillofac Surg. 1996;34(2):181-5.. At present, two techniques - of one or two stages - have been described, which are differentiated with regard to the indication of the time when the transplanted tooth will be inserted in the receptor alveolus2121 Andreasen JO. Atlas de reimplante e transplante de dentes. São Paulo: Medicina Panamericana; 1993.. The two-stage technique has been shown to be more adequate than the former, because it enables the formation of granulation tissue (after a period of 14 days) which favors adaptation of the transplanted tooth to the receptor bed. Similarly, as a result of the improved vascularization in the receptor bed, the chances of successful treatment are greater2020 Nethander G, Andersson JE, Hirsch JM. Autogenous free tooth transplantation in man by a 2-stage operation technique. A longitudinal intra-individual radiographic assessment. Int J Oral Maxillofac Surg. 1988;17(5):330-6.. The transplanted tooth must be positioned in infra-occlusion, at a maximum of 5 mm below the occlusal level of the adjacent teeth2525 Bauss O, Sadat-Khonsari R, Engelke W, Kahl-Nieke B. Results of transplanting developing third molarsas part of orthodontic space management. J Orofac Orthop. 2003;64:40-47. and the patient must strictly follow the instructions relative to hygiene. The surgery must be performed rapidly, in a time interval of less than 18 minutes - to favor preservation of the periodontal ligament2626 Andreasen JO. Interrelation between alveolar bone and periodontal ligament repair after replantation of mature permanent incisors in monkeys. J Periodontal Res. 1981;16(2):228-35. and in an atraumatic manner, with a view to diminishing the risk of ankylosis, root resorptions and permanent infra-occlusion2727 Smith JJ, Wayman BE. Successful autotransplantation. J Endod. 1987;13(2):77-80.doi: 10.1016/S0099-2399(87)80159-0
https://doi.org/10.1016/S0099-2399(87)80...
. All of these associated precautions will enable treatment to be successful55 Kim E1, Jung JY, Cha IH, Kum KY, Lee SJ. Evaluation of the prognosis and causes of failure in 182 cases of autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(1):112-9.doi: 10.1016/j.tripleo.2004.09.007.
https://doi.org/10.1016/j.tripleo.2004.0...
,2626 Andreasen JO. Interrelation between alveolar bone and periodontal ligament repair after replantation of mature permanent incisors in monkeys. J Periodontal Res. 1981;16(2):228-35.,2828 Northway W. Autogenic dental transplants. Am J Orthod Dentofacial Orthop. 2002;121(6):592-3.,2929 Hupp JG, Mesaros SV, Aukhil I, Trope M. Periodontal ligament vitality and histologichealing of teeth stored for extended periodsbefore transplantation. Endod Dent Traumatol. 1998;14(2):79-83.. The splinting technique may be used when stabilization with sutures is not possible2121 Andreasen JO. Atlas de reimplante e transplante de dentes. São Paulo: Medicina Panamericana; 1993..
A successful transplant is achieved when the tooth in question presents no pulp and/or inflammatory changes; signs of root resorption and demonstrates sufficient root development to support the continuous function of the tooth, confirmed by clinical and radiographic evaluation88 Kristerson L. Autotransplantation of human premolars:A clinical and radiographic study of 100 teeth. Int J Oral Surg. 1985;14(2):200-13.,2020 Nethander G, Andersson JE, Hirsch JM. Autogenous free tooth transplantation in man by a 2-stage operation technique. A longitudinal intra-individual radiographic assessment. Int J Oral Maxillofac Surg. 1988;17(5):330-6.,3030 Magini RS, Schiochett C, Matteus GN, Vieira LCC. Autotransplante dental como alternativa de tratamento para perda precoce de molares permanentes. Rev Bras Odontol. 2000;57(3):170-3.. The transplanted tooth must be followed-up for a minimum period of one year, a time in which the chances of root resorption occurring are greatest. This has been shown to be the main factor in failure2020 Nethander G, Andersson JE, Hirsch JM. Autogenous free tooth transplantation in man by a 2-stage operation technique. A longitudinal intra-individual radiographic assessment. Int J Oral Maxillofac Surg. 1988;17(5):330-6.. The most common contra-indication occurs when the tooth to be transplanted presents dimensions that are incompatible with those of the receptor area considering the mesio-distal, vestibular-lingual or apical-coronal dimensions. Systemic complications such as cardiovascular, neurological, blood or infectious diseases may also contra-indicate the procedure2121 Andreasen JO. Atlas de reimplante e transplante de dentes. São Paulo: Medicina Panamericana; 1993..
In the present case, the patient reported acute conditions of pain, not resolved with the use of analgesics, which frequently interfered in her quality of life. Twelve months after the surgery, the patient showed great satisfaction with the treatment, considering the esthetic and functional gains that were obtained. Moreover, she emphasized that as a result of treatment, she felt more motivated to take care of her oral hygiene, which positively influenced her interpersonal relationships.
FINAL CONSIDERATIONS
Diverse factors related to success or failure of autogenous dental transplantation must be critically evaluated. When correctly indicated and planned, transplantation presents a high level of success and low cost. Analyzing the case presented, the authors concluded that autogenous dental transplantation represents an important alternative of oral rehabilitation, allowing the return of the patient’s esthetic and functional characteristics.
REFERENCES
-
1Batista MJ, Rihs LB, Sousa MLR. Risk indicators for tooth loss in adult workers. Braz Oral Res. 2012;Sep-Oct;26(5):390-6. doi: 10.1590/S1806-83242012000500003
» https://doi.org/10.1590/S1806-83242012000500003 -
2Corraini P, Baelum V, Pannuti CM, Pustiglioni AN, Romito GA, Pustiglioni FE. Tooth loss prevalence and risk indicators in an isolated population of Brazil. Acta Odontol Scand. 2009;67:297-303.doi: 10.1080/00016350903029107. doi: 10.1080/00016350903029107
» https://doi.org/10.1080/00016350903029107 -
3Sebben G, Castilhos MDS, Silva RFC. Transplantes autógenos de terceiros molares inclusos. Rev ADP-PUCRS. 2004;5:109-11.
-
4Ioannidou E1, Makris GP. Twelve-year follow-up of an autogenous mandibular canine Transplant.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(5):582-9.doi: 10.1016/S1079210403002609.
» https://doi.org/10.1016/S1079210403002609 -
5Kim E1, Jung JY, Cha IH, Kum KY, Lee SJ. Evaluation of the prognosis and causes of failure in 182 cases of autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(1):112-9.doi: 10.1016/j.tripleo.2004.09.007.
» https://doi.org/10.1016/j.tripleo.2004.09.007 -
6Natiella, JR, Armitage JE, Greene GW. The replantation and transplantation of teeth: A review. Oral Surg Oral Med Oral Pathol. 1970;29(3):397-419.
-
7Cuffari L, Palumbo M. Transplante de germe do 3° molar. J Bras Odontol Clín. 1997;1(2):23-7.
-
8Kristerson L. Autotransplantation of human premolars:A clinical and radiographic study of 100 teeth. Int J Oral Surg. 1985;14(2):200-13.
-
9Mejàre B. A prospective study on transplantation of third molars with complete root formation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(2):231-8.doi: 10.1016/S107921040300461X
» https://doi.org/10.1016/S107921040300461X -
10Czochrowska EM, Stenvik A, Bjercke B, Zachrisson BU. Outcome of tooth transplantation: Survival and success rates 17-41 years posttreatment. Am J Orthod Dentofacial Orthop. 2002;121(2):110-9. doi: 10.1067/mod.2002.119979
» https://doi.org/10.1067/mod.2002.119979 -
11Kvint S, Lindstn R, Magnussonc A, Nilssond P, Bjerkline K. Autotransplantation of teeth in 215 patients. a follow-up study. Angle Orthod. 2010;80(3):446-51. doi: 10.2319/062509-354.1.
» https://doi.org/10.2319/062509-354.1 -
12Souza JG. Transplante autógeno de germe de terceiro molar. RGO, Rev Gauch Odontol. 2002;50(3):175-6.
-
13Waikakul A1, Punwutikorn J, Kasetsuwan J, Korsuwannawong S. Alveolar bone changes in autogenous tooth transplantation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(3):01-07.doi: 10.1016/j.tripleo.2010.11.003.
» https://doi.org/10.1016/j.tripleo.2010.11.003 -
14Jang JH, Lee SJ, Kim E. Autotransplantation of immature third molars using a computer-aided rapid prototyping model: a report of 4 cases. J Endod. 2013;39(11):1461-6. doi: 10.1016/j.joen.2013.06.026.
» https://doi.org/10.1016/j.joen.2013.06.026 -
15Choi SH, Hwang CJ. Orthognathic treatment with autotransplantation of a third molar. Am J Orthod Dentofacial Orthop. 2013 Nov;144(5):737-47. doi: 10.1016/j.ajodo.2012.12.013
» https://doi.org/10.1016/j.ajodo.2012.12.013 -
16Koszowski R, Morawiec T, Bubitek-Bogacz A. Use of the piezosurgery technique for cutting bones in the autotransplantation of unerupted third molars. Int J Periodontics Restorative Dent. 2013;33(4):477-81.doi: 10.11607/prd.0678
» https://doi.org/10.11607/prd.0678 -
17Park JM, Tatad JCI, Landayan MEA, Heo SJ, Kim SJ. Optimizing third molar autotransplantation: applications of reverse engineered surgical templates and rapid prototyping of 3D teeth. J Oral Maxillofac Surg. 2014;72:1653-59. doi: 10.1016/j.joms.2014.04.012
» https://doi.org/10.1016/j.joms.2014.04.012 -
18Kumar N, Prasad K, Lalitha RM, Ranganath K, Dexith J, Chauhan A. Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet rich fibrin: a randomized controlled clinical study. J Oral Maxillofac Surg. 2015;73(6):1042-9. doi: 10.1016/j.joms.2014.11.013
» https://doi.org/10.1016/j.joms.2014.11.013 -
19Kallu R, Vinckier F, Politis C, Mwalili S, Willems G. Tooth transplantations: a descriptive retrospective study. Int J Oral Maxillofac Surg. 2005;34(7):745-55.doi: 10.1016/j.ijom.2005.03.009
» https://doi.org/10.1016/j.ijom.2005.03.009 -
20Nethander G, Andersson JE, Hirsch JM. Autogenous free tooth transplantation in man by a 2-stage operation technique. A longitudinal intra-individual radiographic assessment. Int J Oral Maxillofac Surg. 1988;17(5):330-6.
-
21Andreasen JO. Atlas de reimplante e transplante de dentes. São Paulo: Medicina Panamericana; 1993.
-
22Yan Q, Li B, Long X. Immediate autotransplantation of mandibular third molar in China. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:436-440. doi: 10.1016/j.tripleo.2010.02.026
» https://doi.org/10.1016/j.tripleo.2010.02.026 -
23Thomas S, Turner SR, Sandy JR. Autotransplantation of teeth: is there a role? Br J Orthod. 1998;25(4):275-82. doi: 10.1093/ortho/25.4.275
» https://doi.org/10.1093/ortho/25.4.275 -
24Lundberg T, Isaksson S. A clinical follow-up study of 278 autotransplanted teeth. Br J Oral Maxillofac Surg. 1996;34(2):181-5.
-
25Bauss O, Sadat-Khonsari R, Engelke W, Kahl-Nieke B. Results of transplanting developing third molarsas part of orthodontic space management. J Orofac Orthop. 2003;64:40-47.
-
26Andreasen JO. Interrelation between alveolar bone and periodontal ligament repair after replantation of mature permanent incisors in monkeys. J Periodontal Res. 1981;16(2):228-35.
-
27Smith JJ, Wayman BE. Successful autotransplantation. J Endod. 1987;13(2):77-80.doi: 10.1016/S0099-2399(87)80159-0
» https://doi.org/10.1016/S0099-2399(87)80159-0 -
28Northway W. Autogenic dental transplants. Am J Orthod Dentofacial Orthop. 2002;121(6):592-3.
-
29Hupp JG, Mesaros SV, Aukhil I, Trope M. Periodontal ligament vitality and histologichealing of teeth stored for extended periodsbefore transplantation. Endod Dent Traumatol. 1998;14(2):79-83.
-
30Magini RS, Schiochett C, Matteus GN, Vieira LCC. Autotransplante dental como alternativa de tratamento para perda precoce de molares permanentes. Rev Bras Odontol. 2000;57(3):170-3.
Publication Dates
-
Publication in this collection
Jan 2018
History
-
Received
10 Apr 2017 -
Reviewed
20 July 2017 -
Accepted
31 Aug 2017