SUMMARY
A previously healthy, 52-year-old woman presented with a nine months history of low fever and weight loss (> 30 kg). Physical examination disclosed generalized lymphadenopathy, skin lesions, abdominal distension, mild tachypnea and a left breast mass. Laboratory tests showed anemia; (prerenal) kidney injury, low serum albumin level; and negative serology for HIV and viral hepatitis. Computed tomography (neck/chest/abdomen) showed generalized lymph node enlargement, splenomegaly, pleural effusion and ascites. We performed thoracocentesis and paracentesis, and the findings were consistent with chylothorax and chylous ascites (with no neoplastic cells). Biopsies of the breast mass, skin and lymph nodes were performed and all of them showed large round yeast cells with multiple narrow-based budding daughter cells, characteristic of Paracoccidioides brasiliensis. Consequently, paracoccidioidomycosis was diagnosed, and liposomal amphotericin B was prescribed, as well as a high protein and low fat diet (supplemented with medium chain triglycerides). Even so, her clinical status worsened, requiring renal replacement therapy. She evolved with pneumonia, septic shock and respiratory failure and subsequently died. To our knowledge, this is the first description of a case with chylothorax and breast mass due to paracoccidioidomycosis. Additionally, we discuss: 1- the importance of the inclusion of this mycosis in the differential diagnosis of chylothorax and breast mass (breast cancer), especially in endemic areas; and 2- the possible mechanism involved in the development of chylous effusions.
KEYWORDS:
Paracoccidioidomycosis; Breast neoplasms; Breast; Chylothorax; Chylous ascites
INTRODUCTION
Paracoccidioidomycosis is a systemic and frequent fungal infection in suburban and rural areas of Latin America11. Martinez R. Paracoccidioidomycosis: the dimension of the problem of a neglected disease. Rev Soc Bras Med Trop. 2010;43:480.
2. de Souza SP, Jorge VM, Xavier MO. Paracoccidioidomycosis in southern Rio Grande do Sul: a retrospective study of histopathologically diagnosed cases. Braz J Microbiol. 2014;45:243-7.
3. Góes HF, Durães SM, Lima CS, Souza MB, Vilar EA, Dalston MO. Paracoccidioidomycosis in a renal transplant recipient. Rev Inst Med Trop Sao Paulo. 2016;58:12.
4. Martinez R. Epidemiology of paracoccidioidomycosis. Rev Inst Med Trop Sao Paulo. 2015;57(Suppl 19):11-20.-55. Shikanai-Yasuda MA. Paracoccidioidomycosis treatment. Rev Inst Med Trop Sao Paulo. 2015;57(Suppl 19):31-7.. It has the highest mortality rate among mycosis infection in Brazil and a great potential to lead to disability66. Shikanai-Yasuda MA, Telles Filho FQ, Mendes RP, Colombo AL, Moretti ML. Consenso em paracoccidioidomicose. Rev Soc Bras Med Trop. 2006;39:297-310.,77. Vieira GD, Alves TC, Lima SM, Camargo LM, Sousa CM. Paracoccidioidomycosis in a western Brazilian Amazon State: clinical-epidemiologic profile and spatial distribution of the disease. Rev Soc Bras Med Trop. 2014;47:63-8.. Several clinical manifestations have been previously described in paracoccidioidomycosis, including brain abscess, as recently discussed by us88. Carvalho RM, Nunes SM, Santana AN. Brain abscess. N Engl J Med. 2014;371:1757-8.. However, our literature search performed until January the first 2016, using as a source MEDLINE (PUBMED), found no reports related to "paracoccidioidomycosis AND chylothorax" or "paracoccidioidomycosis AND breast".
This report aims to describe, to the best of our knowledge, the first case of chylothorax and breast mass in a patient with paracoccidioidomycosis. Additionally, we discuss: 1- the importance of the inclusion of this fungal infection in the differential diagnosis of chylothorax and breast mass (breast cancer), a very prevalent neoplasia in women; 2- the possible mechanisms involved in the development of chylous effusions in our patient.
CASE REPORT
A 52-year-old woman presented with a nine month history of generalized lymphadenopathy, skin lesions (multiple crusts all over her body), low fever, weight loss of more than 30 kg, vomiting, abdominal distension, mild dyspnea and a left breast mass (measuring 50 x 10 mm). She denied having any allergies or previous relevant diseases.
She was hospitalized for further investigation. Laboratory testing findings showed negative serology for HIV and viral hepatitis, anemia (hemoglobin 11.0 g/dL), and low serum albumin (2.3 g/dL), mild (prerenal) acute kidney injury, and elevated C-reactive protein (over 8 times the maximum reference value).
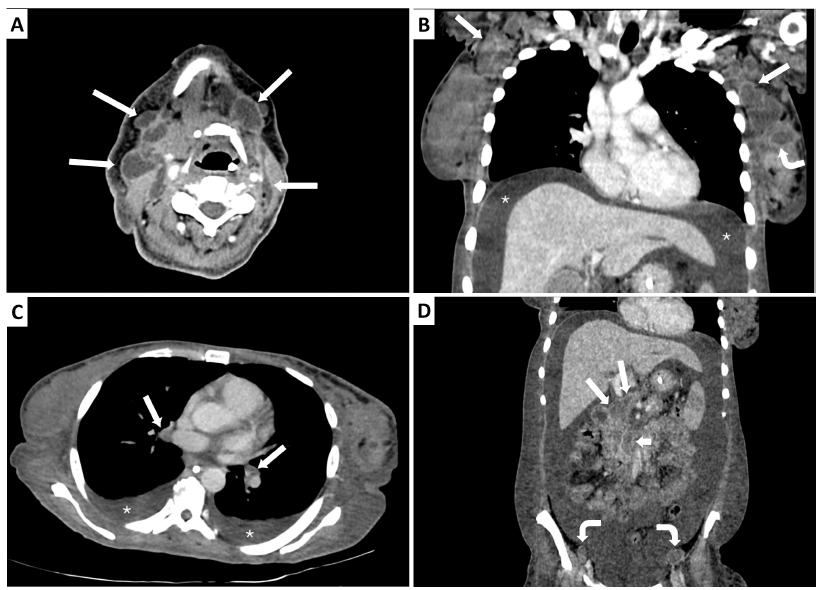
Chest radiography was performed and showed mild/moderate bilateral pleural effusions. In addition, the patient underwent a computed tomography (CT) of the neck, chest and abdomen. CT revealed the presence of a breast mass, generalized necrotic lymph node enlargement (cervical, axillary, mediastinal, abdominal and inguinal), mild splenomegaly, pleural effusion and ascites (Fig. 1).
Contrast-enhanced computed tomography scan of the neck, chest and abdomen. A) Transverse image of the neck shows multiple bilateral cervical necrotic lymphadenopathy (arrows), some coalescent. B) Oblique coronal reformatted image of the chest shows left breast mass (curved arrow), bilateral coalescent necrotic axillary lymphadenopathy (straight arrows), and ascites (stars). C) Transverse image of the chest shows bilateral necrotic hilar lymph nodes (arrows), and bilateral pleural effusion (stars). D) Coronal reformatted image of the abdomen shows periportal (long arrows), periaortic (short arrow), and bilateral external iliac (curved arrows) necrotic lymphadenopathy; and ascites.
She underwent a thoracocentesis that disclosed the presence of a milky fluid whose analysis showed a triglyceride concentration > 600 mg/dL, with no neoplastic cells. Additionally, paracentesis was performed, and the finding was consistent with chylous ascites, and neoplastic cells were not found.
Biopsies of the breast mass (core biopsy), skin lesions and enlarged inguinal lymph nodes were performed and stained using the Grocott-Gomori methenamine-silver (GGMS) technique, the gold standard to diagnose paracoccidioidomycosis according to guidelines66. Shikanai-Yasuda MA, Telles Filho FQ, Mendes RP, Colombo AL, Moretti ML. Consenso em paracoccidioidomicose. Rev Soc Bras Med Trop. 2006;39:297-310.. All of the biopsies revealed the presence of large round yeast cells with multiple narrow-based budding daughter cells, characteristic of Paracoccidioides brasiliensis.
Thereafter, liposomal amphotericin B was prescribed, as well as a high protein and low fat diet (supplemented with medium chain triglycerides). Despite the treatment, her clinical status worsened, with development of severe acute kidney injury that required renal replacement therapy, pneumonia, septic shock, and she subsequently died.
DISCUSSION
The original feature of this case report is to describe the first case, to our knowledge, of a breast mass and chylothorax in a patient with paracoccidioidomycosis. Firstly, a breast mass may be the manifestation of breast cancer, a very important cancer in women. However, a breast mass may also be related to benign diseases, such as fibroadenoma, fat necrosis, tuberculosis, actinomycosis, sparganosis, sarcoidosis, granulomatosis with polyangiitis and idiopathic granulomatous mastitis99. Naraynsingh V, Hariharan S, Dan D, Harnarayan P, Teelucksingh S. Conservative management for idiopathic granulomatous mastitis mimicking carcinoma: case reports and literature review. Breast Dis. 2010;31:57-60.,1010. Tang L, Leekha S. Photo quiz. Breast mass in a 45-year-old man. Clin Infect Dis. 2015;60:438, 486-7.. Consequently, the inclusion of paracoccidioidomycosis in the differential diagnosis of breast masses is very important, because a high clinical suspicion (especially in endemic areas) may allow the correct diagnosis and treatment of this mycosis, preventing an unnecessary mastectomy.
Secondly, chylothorax classically manifests as a milky white pleural fluid. However, it may also appear as a turbid fluid. Consequently, to correctly diagnose chylothorax, it is fundamental to measure the triglyceride levels in suspected pleural effusions, such as milky or serous pleural fluids from prolonged pleural drainage after thoracic surgery or chest trauma, or when concomitant mediastinal lymphadenomegaly, granulomatous diseases, lymphangioleiomyomatosis, cirrhosis, thyroid goiter, or thoracic aortic aneurysm are present. If the triglyceride level in the pleural fluid is > 110 mg/dL, then the diagnosis of chylothorax is defined. Additionally, chylothorax is divided into traumatic and nontraumatic causes. The nontraumatic group is represented mainly by cancer (hematological malignancies and metastatic solid cancers), as well as granulomatous diseases (sarcoidosis, tuberculosis, histoplasmosis). In this report we describe the first case of chylothorax in paracoccidioidomycosis. This finding is very important, considering: 1- the significant prevalence of paracoccidioidomycosis in Latin America, 2- the fact that chylothorax is considered "idiopathic" in up to 10% of cases1111. Doerr CH, Allen MS, Nichols FC 3rd, Ryu JH. Etiology of chylothorax in 203 patients. Mayo Clin Proc. 2005;80:867-70.. Consequently, paracoccidioidomycosis-related chylous pleural effusions may be underdiagnosed, impairing the prognosis of patients.
Additionally, it is important to discuss the possible mechanisms involved in the development of a chylous pleural effusion in our patient. In other infectious granulomatous diseases, such as tuberculosis, chylothorax formation occurs through intrathoracic lymphadenitis1212. Karapolat S, Sanli A, Onen A. Chylothorax due to tuberculosis lymphadenopathy: report of a case. Surg Today. 2008;38:938-41.. In addition, intrathoracic lymphadenomegaly may obstruct the thoracic duct, leading to fluid extravasations into the pleural cavity. We believe that these physiopathological mechanisms are present in our case, based on the observed generalized, necrotic lymph node enlargement.
Finally, it is important to discuss on the gender distribution of paracoccidioidomycosis. In adults, this mycosis presents a male to female rate of 13:1 up to 100:144. Martinez R. Epidemiology of paracoccidioidomycosis. Rev Inst Med Trop Sao Paulo. 2015;57(Suppl 19):11-20.,66. Shikanai-Yasuda MA, Telles Filho FQ, Mendes RP, Colombo AL, Moretti ML. Consenso em paracoccidioidomicose. Rev Soc Bras Med Trop. 2006;39:297-310.,1313. Blotta MH, Mamoni RL, Oliveira SJ, Nouér SA, Papaiordanou PM, Goveia A, et al. Endemic regions of paracoccidioidomycosis in Brazil: a clinical and epidemiologic study of 584 cases in the southeast region. Am J Trop Med Hyg. 1999;61:390-4.. This huge difference in gender distribution may be attributed to beta-estradiol, considering that this discrepancy is not present in patients before puberty, and that the female hormone may inhibit the transformation of mycelium to yeast, and also affect the growth/reproduction of yeasts66. Shikanai-Yasuda MA, Telles Filho FQ, Mendes RP, Colombo AL, Moretti ML. Consenso em paracoccidioidomicose. Rev Soc Bras Med Trop. 2006;39:297-310.,1313. Blotta MH, Mamoni RL, Oliveira SJ, Nouér SA, Papaiordanou PM, Goveia A, et al. Endemic regions of paracoccidioidomycosis in Brazil: a clinical and epidemiologic study of 584 cases in the southeast region. Am J Trop Med Hyg. 1999;61:390-4.
14. Travassos LR, Taborda CP, Colombo AL. Treatment options for paracoccidioidomycosis and new strategies investigated. Expert Rev Anti Infect Ther. 2008;6:251-62.-1515. Restrepo A, Salazar ME, Cano LE, Stover EP, Feldman D, Stevens DA. Estrogens inhibit mycelium-to-yeast transformation in the fungus: implications for resistance of females to paracoccidioidomycosis. Infect Immun. 1984;46:346-53.. These facts emphasize the rarity and importance of our case, which describes a woman with a unique clinical presentation related to paracoccidioidomycosis.
In conclusion, it is necessary to bear in mind that paracoccidioidomycosis could be a cause of breast mass and chylothorax, especially in endemic areas. In addition, a high clinical suspicion allows a rapid diagnosis and an adequate treatment, reducing negative outcomes.
ACKNOWLEDGMENTS
We would like to thank Dr. Fernanda and Dr. Walkiria of the Pathology Unit of the Hospital Regional da Asa Norte.
REFERENCES
-
1Martinez R. Paracoccidioidomycosis: the dimension of the problem of a neglected disease. Rev Soc Bras Med Trop. 2010;43:480.
-
2de Souza SP, Jorge VM, Xavier MO. Paracoccidioidomycosis in southern Rio Grande do Sul: a retrospective study of histopathologically diagnosed cases. Braz J Microbiol. 2014;45:243-7.
-
3Góes HF, Durães SM, Lima CS, Souza MB, Vilar EA, Dalston MO. Paracoccidioidomycosis in a renal transplant recipient. Rev Inst Med Trop Sao Paulo. 2016;58:12.
-
4Martinez R. Epidemiology of paracoccidioidomycosis. Rev Inst Med Trop Sao Paulo. 2015;57(Suppl 19):11-20.
-
5Shikanai-Yasuda MA. Paracoccidioidomycosis treatment. Rev Inst Med Trop Sao Paulo. 2015;57(Suppl 19):31-7.
-
6Shikanai-Yasuda MA, Telles Filho FQ, Mendes RP, Colombo AL, Moretti ML. Consenso em paracoccidioidomicose. Rev Soc Bras Med Trop. 2006;39:297-310.
-
7Vieira GD, Alves TC, Lima SM, Camargo LM, Sousa CM. Paracoccidioidomycosis in a western Brazilian Amazon State: clinical-epidemiologic profile and spatial distribution of the disease. Rev Soc Bras Med Trop. 2014;47:63-8.
-
8Carvalho RM, Nunes SM, Santana AN. Brain abscess. N Engl J Med. 2014;371:1757-8.
-
9Naraynsingh V, Hariharan S, Dan D, Harnarayan P, Teelucksingh S. Conservative management for idiopathic granulomatous mastitis mimicking carcinoma: case reports and literature review. Breast Dis. 2010;31:57-60.
-
10Tang L, Leekha S. Photo quiz. Breast mass in a 45-year-old man. Clin Infect Dis. 2015;60:438, 486-7.
-
11Doerr CH, Allen MS, Nichols FC 3rd, Ryu JH. Etiology of chylothorax in 203 patients. Mayo Clin Proc. 2005;80:867-70.
-
12Karapolat S, Sanli A, Onen A. Chylothorax due to tuberculosis lymphadenopathy: report of a case. Surg Today. 2008;38:938-41.
-
13Blotta MH, Mamoni RL, Oliveira SJ, Nouér SA, Papaiordanou PM, Goveia A, et al. Endemic regions of paracoccidioidomycosis in Brazil: a clinical and epidemiologic study of 584 cases in the southeast region. Am J Trop Med Hyg. 1999;61:390-4.
-
14Travassos LR, Taborda CP, Colombo AL. Treatment options for paracoccidioidomycosis and new strategies investigated. Expert Rev Anti Infect Ther. 2008;6:251-62.
-
15Restrepo A, Salazar ME, Cano LE, Stover EP, Feldman D, Stevens DA. Estrogens inhibit mycelium-to-yeast transformation in the fungus: implications for resistance of females to paracoccidioidomycosis. Infect Immun. 1984;46:346-53.
-
FINANCIAL SUPPORT None
Publication Dates
-
Publication in this collection
2016
History
-
Received
14 Jan 2016 -
Accepted
10 Mar 2016