Abstracts
OBJECTIVE: To analyze concepts of gender and sexuality present in the field of sex therapeutic interventions. METHODOLOGICAL PROCEDURES: An ethnographic observation was conducted, and it was completed with the analysis of printed material originated from the X Congresso Brasileiro de Sexualidade Humana (10th Brazilian Congress on Human Sexuality), promoted by the Sociedade Brasileira de Estudos em Sexualidade Humana (Brazilian Society of Human Sexuality Studies), and the VIII Congresso Brasileiro sobre Inadequações Sexuais (8th Brazilian Congress on Sexual Inadequacies), promoted by the Associação Brasileira para o Estudo das Inadequações Sexuais (Brazilian Association of Sexual Inadequacy Studies), both held in 2005. The analysis emphasized the interaction between the quantitative perspective in the processing of the variables (participants' gender and profession and lecture topics) and the qualitative perspective in the analysis and interpretation of the more general set of data. RESULTS: The topics of sessions and focus of presentations suggest that the field is divided by the contrast between two medical specialties: gynecology and urology, the former is aimed at female and couple dysfunctions, while the latter is aimed at male dysfunctions. CONCLUSIONS: Male sexuality is approached from the predominantly biomedical perspective, centered on the physiology of erection and drug prescription, whereas female sexuality is considered to be conditioned by relationship problems, when psychological intervention is more adequate.
Gender and Health; Sexology; Health Personnel; Health Knowledge, Attitudes, Practice
OBJETIVO: Analisar concepções de gênero e sexualidade presentes no campo de intervenções terapêuticas em torno do sexo. PROCEDIMENTOS METODOLÓGICOS: Observação etnográfica, complementada por análise documental de material impresso referente ao X Congresso Brasileiro de Sexualidade Humana, promovido pela Sociedade Brasileira de Estudos em Sexualidade Humana, e ao VIII Congresso Brasileiro sobre Inadequações Sexuais, promovido pela Associação Brasileira para o Estudo das Inadequações Sexuais, realizados em 2005. A análise privilegiou a interação entre a perspectiva quantitativa no processamento das variáveis profissão e gênero dos participantes e temas das palestras, e perspectiva qualitativa na análise e interpretação do conjunto mais geral de dados. RESULTADOS: Os temas das sessões e o enfoque das apresentações sugerem que o campo é definido pelo contraste entre duas especialidades médicas: a ginecologia e a urologia, a primeira voltada para disfunções femininas e do casal e a segunda para as disfunções masculinas. CONCLUSÕES: A sexualidade masculina é abordada por perspectiva predominantemente biomédica, centrada na fisiologia da ereção e na prescrição de medicamentos, enquanto a sexualidade feminina é apresentada como condicionada por problemas relacionais, mais adequados à intervenção psicológica.
Gênero e Saúde; Sexologia; Pessoal de Saúde; Conhecimentos, Atitudes e Prática em Saúde
OBJETIVO: Analizar concepciones de género y sexualidad presentes en el campo de intervenciones terapéuticas en torno al sexo. PROCEDIMIENTOS METODOLÓGICOS: Observación etnográfica, complementada por análisis documental de material impreso referentes al X Congreso Brasileño de Sexualidad Humana, promovido por la Sociedad Brasileña de Estudios en Sexualidad Humana y el VIII Congreso Brasileño sobre Inadecuaciones Sexuales, promovido por la Asociación Brasileña para el Estudio de las Inadecuaciones Sexuales, realizados en 2005. El análisis privilegió la interacción entre la perspectiva cuantitativa en el procesamiento de las variables profesión y género de los participantes y temas de las palestras y cualitativa en el análisis e interpretación del conjunto más general de datos. RESULTADOS: Los temas de las sesiones y el enfoque de las presentaciones sugieren que el campo es definido por el contraste entre dos especialidades médicas: la ginecología y la urología, la primera dirigida a disfunciones femeninas y de la pareja y la segunda a las disfunciones masculinas. CONCLUSIONES: La sexualidad masculina es abordada por perspectiva predominantemente biomédica, centrada en la fisiología de la erección y en la prescripción de medicamentos, mientras que la sexualidad femenina es presentada como condicionada por problemas de relación, más adecuados a la intervención psicológica.
Género y Salud; Sexología; Personal de Salud; Conocimientos, Actitudes y Práctica en Salud
ORIGINAL ARTICLE
Gender differences in the field of sexology: new contexts and old definitions
Diferencias de género en el campo de la sexología: nuevos contextos y viejas definiciones
Fabiola RohdenI; Jane RussoII
IDepartamento de Antropologia. Instituto de Filosofia e Ciências Humanas. Universidade Federal do Rio Grande do Sul. Porto Alegre, RS, Brasil
IIDepartamento de Políticas e Instituições de Saúde. Instituto de Medicina Social. Universidade do Estado do Rio de Janeiro. Rio de Janeiro, RJ, Brasil
Correspondence Correspondence: Fabiola Rohden Depto. de Antropologia Instituto de Filosofia e Ciências Humanas Universidade Federal do Rio Grande do Sul Av. Bento Gonçalves, 9500 - Campus do Vale 91509-900 Porto Alegre, RS, Brasil E-mail: fabiola.rohden@gmail.com
ABSTRACT
OBJECTIVE: To analyze concepts of gender and sexuality present in the field of sex therapeutic interventions.
METHODOLOGICAL PROCEDURES: An ethnographic observation was conducted, and it was completed with the analysis of printed material originated from the X Congresso Brasileiro de Sexualidade Humana (10th Brazilian Congress on Human Sexuality), promoted by the Sociedade Brasileira de Estudos em Sexualidade Humana (Brazilian Society of Human Sexuality Studies), and the VIII Congresso Brasileiro sobre Inadequações Sexuais (8th Brazilian Congress on Sexual Inadequacies), promoted by the Associação Brasileira para o Estudo das Inadequações Sexuais (Brazilian Association of Sexual Inadequacy Studies), both held in 2005. The analysis emphasized the interaction between the quantitative perspective in the processing of the variables (participants' gender and profession and lecture topics) and the qualitative perspective in the analysis and interpretation of the more general set of data.
RESULTS: The topics of sessions and focus of presentations suggest that the field is divided by the contrast between two medical specialties: gynecology and urology, the former is aimed at female and couple dysfunctions, while the latter is aimed at male dysfunctions.
CONCLUSIONS: Male sexuality is approached from the predominantly biomedical perspective, centered on the physiology of erection and drug prescription, whereas female sexuality is considered to be conditioned by relationship problems, when psychological intervention is more adequate.
Descriptors: Gender and Health. Sexology. Health Personnel. Health Knowledge, Attitudes, Practice.
RESUMEN
OBJETIVO: Analizar concepciones de género y sexualidad presentes en el campo de intervenciones terapéuticas en torno al sexo.
PROCEDIMIENTOS METODOLÓGICOS: Observación etnográfica, complementada por análisis documental de material impreso referentes al X Congreso Brasileño de Sexualidad Humana, promovido por la Sociedad Brasileña de Estudios en Sexualidad Humana y el VIII Congreso Brasileño sobre Inadecuaciones Sexuales, promovido por la Asociación Brasileña para el Estudio de las Inadecuaciones Sexuales, realizados en 2005. El análisis privilegió la interacción entre la perspectiva cuantitativa en el procesamiento de las variables profesión y género de los participantes y temas de las palestras y cualitativa en el análisis e interpretación del conjunto más general de datos.
RESULTADOS: Los temas de las sesiones y el enfoque de las presentaciones sugieren que el campo es definido por el contraste entre dos especialidades médicas: la ginecología y la urología, la primera dirigida a disfunciones femeninas y de la pareja y la segunda a las disfunciones masculinas.
CONCLUSIONES: La sexualidad masculina es abordada por perspectiva predominantemente biomédica, centrada en la fisiología de la erección y en la prescripción de medicamentos, mientras que la sexualidad femenina es presentada como condicionada por problemas de relación, más adecuados a la intervención psicológica.
Descriptores: Género y Salud. Sexología. Personal de Salud. Conocimientos, Actitudes y Práctica en Salud.
INTRODUCTION
The present article aimed to analyze how doctors' and psychologists' modern interventions in sexuality update or redefine more traditional concepts of gender and sexuality.
The analysis used studies on gender and science as its framework, showing how gender conditioning factors are involved in the relationship between knowledge production and social context. Considering the fact that there is no production out of context, this analysis points to the complex integration among social demands, scientific production and reincorporation of such production in the socio-cultural environment.3,6,10,11,12,16,20,22 The most important aspect of this process is the application of the knowledge produced - in this case, the therapeutic practices.
The focus was on the interaction among different participants and on the interplay of interests and world views involved in the discourses and practices produced in this new phase of medicalization of sexuality. This phase is marked by the great presence of the pharmaceutical industry and it implies the re-updating of sexual norms, now aimed at obtaining maximum performance with the help of drugs.7,13-15,17
Medicalization has been discussed in the field of sociology of knowledge, which problematizes the reductionist use of the term. Medlicalization is a broad and complex phenomenon, which includes everything from the definition of a certain type of behavior as deviant in medical terms to scientific discoveries that make this legitimate, proposed treatments and the wide network of social, political and economic interests.5,19 It also includes specific correlated questions, such as the de-medicalization process, which involved the doctors' loss of power to the pharmaceutical industry or the diversification of professionals in sexuality treatment.8,23,24
Sexology, the main theory and practice in this process, had a double birth.1,2 The first one occurred in the second half of the 19th century, with a focus on nosography, in contrast to therapeutics, and favoring sexually transmitted diseases, the psychopathology of sexuality and eugenics. The second one was born in the 1920s, with important landmarks such as Reich's works on the function of orgasm and those of Kinsey, who helped to establish orgasm as the main problem of studies on sexuality.1,4
Proto-sexology was concentrated on the difficulties in the functioning of reproductive sexuality, such as sexually transmitted diseases, "sexual aberrations" and contraceptive techniques and it was not concerned about distinguishing itself from other areas of medicine, such as psychiatry, legal medicine or urology. On the other hand, the second sexology established its autonomy from medical specialties, especially through the affirmation of a particular object - orgasm - and an essential norm - the "ideal orgasm". Deviations from "normal" sexuality, about which 20th century sexologists were concerned, are different from traditional "aberrations": the focus is on couple and genital sexuality and it involves a broad continuum of sexual dysfunctions.1,4
METHODOLOGICAL PROCEDURES
The partial results of the research project entitled "Sexualidade, Ciência e Profissão na América Latina" (Sexuality, Science and Profession in Latin America), which had a socio-anthropological approach and was conducted by the Centro Latino-Americano em Sexualidade e Direitos Humanos (Latin American Center of Sexuality and Human Rights) in partnership with the Institut National de la Santsé et de la Recherche Medicale, were used as basis for this study. Extensive mapping of interventions in sexuality was conducted, such as the identification of main institutions, professionals, research groups, publications and qualification courses and events in six Latin American countries.18,21
The two most important Brazilian congresses in the area were analyzed: the X Congresso Brasileiro de Sexualidade Humana (10th Brazilian Congress on Human Sexuality), promoted by the Sociedade Brasileira de Estudos em Sexualidade Humana (SBRASH - Brazilian Society of Human Sexuality Studies) and the VIII Congresso Brasileiro sobre Inadequações Sexuais (8th Brazilian Congress on Sexual Inadequacies), promoted by the Associação Brasileira para o Estudo das Inadequações Sexuais (ABEIS - Brazilian Association of Sexual Inadequacy Studies), both held in 2005.
The 10th Brazilian Congress on Human Sexuality occurred between September 15th and 17th 2005, at the Centro de Convenções da Associação Médica do Rio Grande do Sul, in Porto Alegre (Southern Brazil), the city that hosted the SBRASH at that moment. The 8th Brazilian Congress on Sexual Inadequacies, promoted by the ABEIS, was held between July 28th and 30th 2005, in the city of Belo Horizonte (Southeastern Brazil).
An ethnographic observation was conducted and complemented with documental analysis of printed material. Researchers (two in the SBRASH Congress and one in the ABEIS Congress) participated in activities promoted by the congresses. In the lectures and seminars, a diversity of themes was observed, with a focus on the lecturers and audience (number of people, number of women and men, and others) and researchers sought to approach participants in informal conversations. Physical structuring of space (conference rooms and common space between events) was also observed. Folders and promotion materials distributed on stands or during the lectures were collected, in addition to programs and official bulletins from congresses.
RESULTS AND DISCUSSION
History of the field and its main associations
In the 1970s, in the city of Rio de Janeiro (Southeastern Brazil), the Núcleo de Sexologia da Sociedade de Ginecologia e Obstetrícia do Rio de Janeiro (SGORJ - Sexology Center of the Rio de Janeiro Society of Gynecology and Obstetrics) was founded by gynecologists and psychologists. In the beginning of the 1980s, participants of this center founded the Comissão Nacional Especializada em Sexologia (Brazilian Committee Specialized in Sexology), included in the Federação Brasileira das Associações de Ginecologia e Obstetrícia (FEBRASGO - Brazilian Federation of Gynecology and Obstetrics Associations), in partnership with professionals from other Brazilian regions.
Between 1983 and 1989, seven Encontros Nacionais de Sexologia (National Meetings on Sexology) were held. The assembly for the foundation of the Sociedade Brasileira de Estudos em Sexualidade Humana (SBRASH) occurred in the city of Gramado, RS, in 1987, while the first congress occurred in Rio de Janeiro, in 1989.
The SBRASH was created to promote scientific exchange among professionals specialized in different dimensions of human sexuality and it was comprised of 227 members in 2005. According to the social statute approved in 2003, it stopped being only a multidisciplinary group of discussion about sexuality issues, thus broadening its reach. This society aimed to guarantee the preservation of ethical values when field activities are performed, to issue professional qualification certificates, to certify professional qualification courses in this area, and to provide specialized technical support to affiliated professionals and institutions.ª a Sociedade Brasileira de Estudos em Sexualidade Humana. Estatuto. Rio de Janeiro; 2008 [cited 2008 Jan 13]. Available from: http://www.sbrash.org.br/portal/index.php?option=com_content&task=view&id=170&Itemid=104 It is responsible for the publication of the Revista Brasileira de Sexualidade Humana (Brazilian Journal of Human Sexuality) and it organizes the main event in this area every two years, the Brazilian Congress on Human Sexuality.
The SBRASH is the result of oppositions faced by the Brazilian Committee Specialized in Sexology in the FEBRASGO itself, which included psychologists and educators, among other professionals. The foundation of a multidisciplinary society was the way found to deal with the emerging tension between subordination to medicine and the process of autonomy of their specialty, a landmark in this field.
In São Paulo, the "second sexology" seems to have begun in the same period, between the late 1970s and early 1980s. In 1984, the Instituto H. Ellis (H. Ellis Institute) was founded, a "specialized center of sexuality disorders",b b Instituto H. Ellis. São Paulo; 2002 [cited 2008 Apr 28]. Available from: http://www.instituto-h-ellis.com.br/unidade_freicaneca/sobre.asp whose group of professionals were responsible for the creation of the Associação Brasileira para o Estudo da Impotência (ABEI - Brazilian Association of Studies on Impotence) in 1987, founded with the objective of holding the 4th World Meeting on Impotence in Brazil, in 1990, an event organized by the International Society for Impotence Research. The ABEI became the main promoter of "sexual medicine" in this country and it was mostly comprised of urologists. Following the worldwide movement towards replacing the term "impotence" by "erectile dysfunction", the ABEI became the Associação Brasileira para o Estudo das Inadequações Sexuais (ABEIS) in 2003.
The ABEIS holds regional scientific events including more than 300 health professionals, especially doctors (urologists and gynecologists) and psychologists. Themes on sexuality, sexual anatomy and physiology, sexual dysfunction, diagnosis and treatment techniques (medical, drug-based, surgical, and psychotherapeutic) of sexual problems are the issues of the Ciclo de Educação Continuada (Continuing Education Cycle). In 2004, this Cycle was comprised of 143 lecturers and 956 participants in eight Brazilian cities, with the support of the Departamento de Andrologia da Sociedade Brasileira de Urologia (Brazilian Society of Urology Department of Andrology); the Sociedade Latino-americana para o Estudo da Impotência Sexual (Latin American Society of Studies on Sexual Impotence), now known as the Sociedade Latino-americana de Medicina Sexual (Latin American Society of Sexual Medicine); and SBRASH.
ABEIS' approach is clearly medical, when compared to that of SBRASH, and its association with the Brazilian Society of Urology Department of Andrology appears in partnerships, such as the "Jornadas de Sexualidade" (Sexuality Seminars), held in Brazilian cities. A total of four pharmaceutical laboratories (Lilly, Pfizer, Schering and Medley), manufacturers of drugs used to treat "erectile dysfunction", sponsor this association.
The appearance of ABEIS indicates the beginning of a third phase of sexology, characterized by the "medicalization" of sexuality. The urologist becomes the professional who stands out and men replace women (and couples) as main clients.
ABEIS remains out of the debate between psychologists and doctors. Although psychologists are included in its staff and management and participate in the events held by this society, the hierarchical superiority of medicine and its practices (especially the freedom to prescribe drugs) is visible in its bulletins and events promoted. At the same time, its certification becomes less relevant, because a degree in medicine enables professionals not to need any other titles.
10th Brazilian Congress on Human Sexuality
This Congress gathered approximately 500 participants, including 198 Brazilian, three Latin American and one North American lecturers. The majority of Brazilian lecturers were from the states of Rio Grande do Sul, São Paulo and Rio de Janeiro. "Culture and Health" was the main theme of the Congress, debated in 17 conferences, 35 panels, two courses, one workshop and two drama workshops, where themes, lecturers and types of presentation were selected by the Scientific Committee.
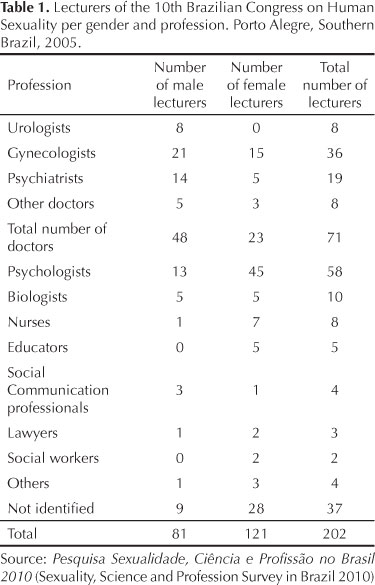
The majority of conference participants were women. Among lecturers, 58 were psychologists and 71 doctors (of which 48 were men and 23 were women) (Table 1). There were at least four times more gynecologists (21 men and 15 women) than urologists (eight men). Psychiatrists were men in their majority (14 men and five women).
On the other hand, women predominated among psychologists (45 women and 13 men), nurses (seven women and one man) and educators (five women).
There was a considerable plurality of themes discussed, although the emphasis was on sexual dysfunction (34 lectures) (Table 2). Sexual education, homosexuality and love relationships were also present. Part of the presentations had more than one author, which resulted in a higher number of lecturers than lectures. As the majority of participants were women, there were more presentations given by them.
Sexual education was a theme presented by 20 women and four men; HIV/AIDS, by 11 women and five men; adolescent pregnancy, by 14 women and four men; and adolescent sexuality, eight women and two men. These numbers indicate the strong presence of women in sexology prevention and education, which have, historically, been focused on adolescence and sexually transmitted disease prevention. In contrast, men stood out in other areas: medications (nine presentations) and reproduction, especially when associated with physiological aspects (seven men and two women).
The official program, promoted by the Scientific Committee, was comprised of 105 works, and the parallel program, 84 works, aimed to meet the demands of those enrolled. The comparison between the themes of both programs indicates that the congress organizers' interests are different from those of professionals enrolled. The scientific committee prioritized debates about clinical practice in sexual dysfunctions in the official program, with doctors alongside psychologists. The works of the parallel program mostly dealt with sexual education. The frequency of participants in presentations on sexual education, homosexuality, STDs, HIV/AIDS and contraceptives was reasonably low, compared to the audience of lectures on sexual dysfunctions.
The pharmaceutical industry was present in the main area allocated for exhibits and new products launched by several laboratories, where there were stands representing the Pfizer, Eli-Lilly, Bayer, Schering do Brasil, Herbarium Fitoterápicos, Jansen, SB Jaynco and Igefarma laboratories. At the entrance to the main room, there was the following warning: "In accordance with RDG 102/2000, issued by Anvisa [National Health Surveillance Agency], pharmaceutical laboratories are only authorized to promote or provide materials and drugs to professionals who are permitted to write prescriptions by law, i.e. doctors. The remaining participants, wearing badges identifying them as not authorized to prescribe, can only receive drug samples or products which do not require a prescription." Although the participation of the pharmaceutical industry is common in health congresses, this particular case shows how recent interventions in sexuality are associated with a greater use of specific drugs. In addition, it reflects the separation of this area between doctors and non-doctors, translated into the identification badges themselves: one identified in red as 'authorized to prescribe", distributed to doctors; and another identified in blue as "not authorized to prescribe", distributed to the remaining professionals.
8th Brazilian Congress on Sexual Inadequacy
In the first congresses held by the institution, doctors and psychologists were divided in distinct rooms and discussed different themes. However, doctors could attend the sessions aimed at psychologists, whereas psychologists could not participate in the sessions aimed at doctors. In 2005, doctors and psychologists shared the same space and discussions and worked together. This does not mean that tensions between these two professional groups have disappeared. Divergences between the practices developed by doctors and psychologists still exist, although in a more subtle form.
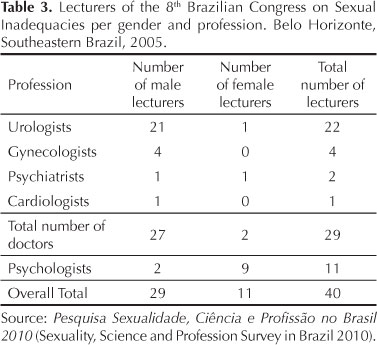
Another change observed was associated with the number of women present in the association events. In the first ABEIS congress, there was only one woman; in 2005, there were more than 30. The scientific committee was comprised of ten doctors (eight urologists) and four psychologists and it was presided by an urologist. As there was no space for the enrollment of participants, lectures resembled an intensive refresher course, with the latest developments in the area.
This congress was held by doctors, urologists in their majority, with a strong institutional presence in the pharmaceutical industry, sponsored by four pharmaceutical laboratories - three of which were manufacturers of drugs for erectile dysfunctions: Pfizer, Bayer and Eli Lilli -, specialized companies and bookstores.
Of all 40 lecturers, 29 were men (27 doctors and two psychologists) and 11 women (nine psychologists and two doctors) (Table 3). There was a predominance of urologists (21 men and one woman).
In Table 4, the distribution of lecturers per gender and theme presented contrasts with the SBRASH Congress, as the lectures or "classes" were given by one professional only. Of all 62 lectures, men gave 48 of them and thus represented the majority of lecturers, compared to women, who gave 14. The two themes that were primarily emphasized were sexual dysfunction (19 classes) and medications (18 classes). Penis implants/prostheses/ enlargement did not involve female participation.
Table 5 compares the distribution of lecturers per gender and focus of each event. The works presented that favored male or female problems in the exclusive context of sexuality were perceived as the main point of analysis, disregarding works on reproduction, violence, STDs and professional performance.
The SBRASH Congress, due to the greater presence of gynecologists, focused more on female problems (28) than male ones (18). In addition, women (42) more frequently dealt with female problems (28 lectures), compared to male problems (14 lectures). In contrast, men (36) focused on male (18) and female problems (18) equally. The ABEIS Congress showed a predominance of urologists and thus included a higher number of lectures on male problems (35 cases) than female ones (eight cases). Men (36) focused on male problems (32 cases), compared to female ones (four cases); whereas women (seven) dealt with both female (four) and male problems (three).
New contexts and old gender distinctions
Based on the data observed, it is possible to organize the current field of interventions in sexuality according to three main points. The first one refers to the professions involved. There is a contrast, on the one hand, between doctors and non-doctors; on the other, inside the group of doctors, between gynecologists and urologists.
The urologist is the major representative of the third phase of sexology, known as "sexual medicine". The intense medicalization of the traditional "impotence" (currently known as "erectile dysfunction") implied a change of direction in the urological practice, as it had primarily followed a surgical approach until then. Based on the so-called male sexual dysfunctions and the association with pharmaceutical laboratories, the area of urology tends to be more and more directed towards clinical practice. The union between gynecologists and psychologists, which marked the beginning of the second phase of sexology that focused on the dysfunctional couple, stopped being the integrating center of this field. The main contrast is observed between the two medical specialties. The tension between doctors and psychologists is part of this contrast. In both cases, the double polarity - between gynecologists and urologists, on the one hand, and between doctors and psychologists, on the other - is uniquely marked by gender. The majority of professionals in the medical area are men, whereas women are mostly psychologists. Among doctors, this separation does not result from professionals' gender primarily (even among gynecologists, there is a majority of men), but rather from clientele (women and couples or men), on the one hand, and from the approach, on the other, thus leading to the second main point.
Urologists - and sexual medicine - are associated with the biomedical approach, centered on anatomical-physiological problems, whereas gynecologists and psychologists tend towards the psychological approach, characterized by the notion of sexuality as a broad and complex phenomenon, which can only be treated through a comprehensive view of an individual.8,9
The third main point, which is integrated with the second one, refers to the opposition between male sexuality (marked by the biomedical perspective, with an emphasis on the erectile dysfunction category) and female sexuality (shown to be more conditioned by the environment and by relationship or affective problems). Thus, there has been a strong process of medicalization of male impotence with the rise of urologists and of the organicist perspective in the treatment of sexuality since the 1980s. The main symptom of this process was the consolidation of erectile dysfunction as a key category to understand and treat male sexual problems.8,9,13-15
The traditional concept of a man, centered on the notion of potency, on the one hand, and on "non-relational sexuality", on the other, is emphasized. However, at the same time, there is the redefinition of this concept, once the need for medication and the resulting dependence on a specialist to guarantee the ideal potency cause man, who traditionally opposes medical control and discourse, to be disempowered.
There are frequent reports of difficulties faced by doctors and the pharmaceutical industry to establish criteria to define female sexual dysfunction. Differently from male dysfunction, whose criteria of evaluation are regulated by the functioning of the penis (frequency, duration and quality of erection), there are questions about the criteria to be used in the case of women. According to some, the main difficulty would be how to translate female complaints into specific diagnoses. It is argued that the female sexual experience depends on the social context (relationship and previous experiences, among other factors) as much as or more than genital functioning. Male sexuality exists regardless of relationships, unlike female sexuality, which is conceived as an inseparable part of relationships.17
CONCLUSIONS
We conclude that there is again an emphasis on gender differences in sexuality. Whereas male sexuality is defined by a logic of performance, assessed by erection and treated with drugs and techniques that solve the specific problem of erectile dysfunction, female sexuality is seen as a complex and intriguing phenomenon, which cannot be reduced to a particular organic function. The current medicalization of sexuality, represented by the success of drugs against erectile dysfunction, seems to concern primarily male sexuality. This would be "naturally" more objective and evidently more organic, in the sense that men are more easily separated from the conjugal pair. Male sexuality is "naturally" thought of as independent from relationships with partners, an autonomous impulse, uncontrollable, separated from relationships and affection. Women continue to be viewed as an eminently "relational" being. Their sexuality does not exist as an autonomous impulse, separated from conjugality (or from relationships). In this way, it is possible to argue that the "physical-orientation" of male sexuality corroborates the traditional gender duality, which points to women as the foundation of conjugality and vehicles of affection.
REFERENCES
Received: 6/24/25010
Approved: 2/27/2011
This research project was funded by the Ford Foundation (Process 1020.1533-3 - 2005).
The authors declare no conflicts of interest.
- 1. Béjin A. Crespúsculo dos psicanalistas, manhã dos sexólogos. In: Ariès PH, Béjin A, organizadores. Sexualidades ocidentais. São Paulo: Brasiliense; 1987. p.210-35.
- 2. Béjin A. O poder dos sexólogos e a democracia sexual. In: Ariès PH, Béjin A, organizadores. Sexualidades ocidentais. São Paulo: Brasilense; 1987. p.236-54.
- 3. Bleier R. Science and gender - a critique of Biology and its theories on women. New York: Teachers College Press; 1997.
- 4. Carrara S, Russo J. A psicanálise e a sexologia no Rio de Janeiro do entreguerras: entre a ciência e a auto-ajuda. Hist Cienc Saude-Manguinhos. 2002;9(2):273-290. DOI:10.1590/S0104-59702002000200003
- 5. Conrad PH. The medicalization of society: on the transformation of human conditions into treatable disorders. Baltimore: The Johns Hopkins University Press; 2007.
- 6. Fausto-Sterling A. Sexing the body: gender, politics and the construction of sexuality. New York: Basic Books; 2000.
- 7. Fishman JR. Manufacturing desire: the commodification of female sexual dysfunction. Soc Stud Sci. 2004;34(2):187-218. DOI:10.1177/0306312704043028
- 8. Giami A. De l'impuissance à la dysfonction érectile. Destins de la médicalisation de la sexualité. In: Fassin D, Memmi D, organisateur. Le gouvernement des corps. Paris: EHESS; 2004. p.77-108.
- 9. Giami A. Changing relations between medicine, psychology and sexuality: the case of male impotence. J Soc Med. 2000;37:263-72.
- 10. Harding S. The science question in feminism. Ithaca: Cornell University Press; 1986.
- 11. Hubbard R. The politics of women's biology. New Brunswick: Rutgers University Press; 1990.
- 12. Jordanova L. Sexual visions, images of gender in science and medicine between the eighteenth and twentieth centuries. London: Harvester Wheatsheaf; 1989.
- 13. Lexchin J. Bigger and better: how Pfizer redefined erectile dysfunction. PLoS Med. 2006;3(4):1-4.
- 14. Loe M. Fixing broken masculinity: Viagra as a technology for the production of gender and sexuality. Sex Cult. 2001;5(3):97-125. DOI:10.1007/s12119-001-1032-1
- 15. Marshall B, Katz S. Forever functional: sexual fitness and the ageing male body. Body Soc. 2002;8(43):43-70. DOI:10.1177/1357034X02008004003
- 16. Moscuscci O. The science of woman: gynecology and gender in England (1800-1929). Cambridge: Cambridge University Press; 1990.
- 17. Rohden F. Diferenças de gênero e medicalização da sexualidade na criação do diagnóstico das disfunções sexuais. Rev Estud Fem. 2009;17(1):89-109. DOI: 10.1590/S0104-026X2009000100006
- 18. Rohden F, Torres I. Le champ actuel de la sexologie au Brésil: considérations initiales. Sexologies. 2006;15(1):64-71. DOI:10.1016/j.sexol.2005.11.007
- 19. Rosemberg CE. The tyranny of diagnosis: specific entities and individual experience. Milbank Q. 2002;80(2):237-60. DOI:10.1111/1468-0009.t01-1-00003
- 20. Russett CE. Sexual science. The victorian construction of womanhood. Cambridge: Harvard University Press; 1995.
- 21. Russo JA, Rohden F, Torres I, Faro L. O campo da sexologia no Brasil: constituição e institucionalização. Physis (Rio J). 2009;19(3):617-35. DOI: 10.1590/S0103-73312009000300004
- 22. Schiebinger L. O feminismo mudou a ciência? Bauru: Edusc; 2001.
- 23. Tiefer L. Sex is not a natural act and other essays. Cambridge: Westview Press; 2004.
- 24. Tiefer L. The Viagra Phenomenon. Sexualities 2006; 9(3):273-94. DOI:10.1177/1363460706065049
Publication Dates
-
Publication in this collection
10 June 2011 -
Date of issue
Aug 2011
History
-
Accepted
27 Feb 2011 -
Received
24 June 2010