Abstract
This article discusses the safeguarding of the right to health, within the scope of a set of constitutional rights, materialized by public policies that organize the National Health Service in Portugal. Before the degradation of supply terms, frequently based on an association that observes the demographic aging as enough condition to justify the increase in health costs, legitimizing consequent restrictions on the supply. We conduct a literature review to search for factors that validate this association, examining arguments to understand this process; debating the validity of prospecting health costs using age-based models versus predictive models that consider the time to death. Additionally, we analyze the evolution of the main causes of mortality in Portugal between 1990 and 2017 for the groups 50-59 years and ≥70 years, causes of disability, as well as the prospects for public health financing in the percentage of GDP in countries of the Organization for Economic Co-operation and Development by 2030, while urgent and necessary solutions for Health Systems are considered, so they can gain efficiency without degrading performance, contributing and investing in a necessary co-responsibility in health on the demand side.
Keyword:
Aging; Social Rights; Health Costs; Innovation; National Health Service
Resumo
Neste artigo discute-se a salvaguarda do direito à saúde, no âmbito de um conjunto de direitos constitucionais, materializados por políticas públicas que organizam o Serviço Nacional de Saúde em Portugal. Diante da degradação dos termos da oferta, frequentes vezes ancorados em uma associação que, de per se, observa o envelhecimento demográfico como condição suficiente para justificar o aumento dos custos em saúde, legitimando assim restrições na oferta. Procedemos a uma revisão da literatura na busca de fatores capazes de validar essa associação, examinando argumentos necessários à compreensão desse processo, debatendo a validade de se perspectivarem custos em saúde utilizando modelos baseados na idade versus modelos preditivos que consideram o tempo até à morte - time-to-death. Adicionalmente, analisa-se a evolução das principais causas de mortalidade em Portugal entre 1990 e 2017 para os grupos 50-59 anos e ≥70 anos, causas de incapacidade, bem como as perspectivas de financiamento público em saúde em percentagem do PIB nos países da Organização para a Cooperação e Desenvolvimento Econômico até 2030, enquanto se equacionam soluções de adaptação urgente e necessária dos Sistemas de Saúde, de modo a que possam ganhar eficiência sem degradar a performance, contribuindo e investindo em uma também necessária corresponsabilização em saúde do lado da procura.
Palavras-chave:
Direitos Sociais; Envelhecimento; Custo em Saúde; Inovação; Serviço Nacional de Saúde
Introduction
To discuss the right to health protection requires a prior framework on the evolution of a set of social rights and public policies embodied by States as provisional instruments for these rights. This text aims to question the argument and the legitimacy of a discourse that claims the inevitability of increased health costs, through an association that intrinsically justifies demographic aging and intergenerational equity as a sufficient condition to explain the increase in direct payments made by health care users, while legitimizing cuts in health expenditure by States. Therefore, the path of the guarantees legally assumed by the Portuguese State with regard to the right to health will be examined, continuing a discussion on the adequacy of the registration and allocation of health expenditure for the elderly and the way this discourse has been used by different States to communicate budget cuts in the field of public health services.
In the Portuguese case, the organization of the Health System (SS) is based on a mixed system, whose structuring bases are located in the 1970s, when an important reform of the health services took place, in which, for the first time, a national health system is conceived, ordered from governmental, central and local levels. In this new context, the State assumed itself as responsible for and guarantor of the national health standard, recognizing the enjoyment of the right to health by individuals and communities, a fact that was greatly improved by the creation of a National Health Service (SNS), which emerged in 1979 .
The existence of the Portuguese SNS is, to date, anchored in art. 64 of the Constitution (from 1976 and the following years), which (1) establishes the right to health protection, through a universal and general SNS which, taking into account the economic and social conditions of citizens, tends to be free; (2) recognizes that the right to health protection is a State’s priority task, and (3) sets forth that the SNS should continue to perform decentralized and participatory management.
According to Canotilho and Moreira (2007, p. 56 in Monge, 2019MONGE, C. O direito fundamental à proteção da saúde. e-Púbica - Revista Eletrónica de Direito Público, Lisboa, v. 6, n. 1, p. 75-100, 2019. Disponível em: <Disponível em: https://bit.ly/2Ay6ORh
>. Acesso em: 20 dez. 2019.
https://bit.ly/2Ay6ORh...
, p. 84), the right to health protection, declared as a fundamental right, constitutes evidence: “for citizens, it is not only a defense barrier against State interference; it is also, first of all, a catalog of rights to action or services provided by the State.”
Thus, the majority of health expenditure, in which the State is, simultaneously, the main provider and payer, through the SNS, is mostly financed by the State budget, with the user having a significantly smaller and variable percentage of the costs spent in the use of services, through the application of moderating fees, with two levels of co-participation, one of which dictating the total exemption from any payment for: economic failure, minors, pregnant women, cancer patients, and some chronic diseases. The current distribution of health costs, therefore, has shown a consistent trend of change, in the sense of a decrease in state co-participation in and/or coverage of health expenditure, with the consequent increase in direct payments by users, a fact that will be demonstrated below, defending a more liberal trend with the establishment of rates or (co) payments indexed to the level of income earned by citizens, thereby reducing the costs borne by the State.
At the same time, the State has allowed the expansion and strengthening of several private providers, placing itself increasingly as “user” of these services by establishing agreements or contracts. As can be seen, it is not the totality of health services that attracts private capital, but only those, capital intensive, whose return is previously assured, oriented towards the occupation of areas where the SNS is inefficient, or has divested in capital and human resources, generating longer average waiting times, a fact particularly observed after the Memorandum of Understanding that dictated external financial support for Portugal in 2011. Despite the gradual growth of private health insurance in Portugal, which reached in 2018 the highest value since the creation of the SNS, 2.6 million policies, growth of 3% compared to the same period of 2017 (ASF, 2019ASF - AUTORIDADE DE SUPERVISÃO DE SEGUROS E FUNDOS DE PENSÕES. Relatório de evolução da atividade seguradora: 3º trimestre. Lisboa, 2019. Disponível em: <Disponível em: https://bit.ly/3dodCjc
>. Acesso em: 11 dez. 2019.
https://bit.ly/3dodCjc...
), it is difficult to foresee the acceptance of alternative, global and lifetime insurance, without any exclusion of disease groups, age group or health status of the insured, based on a public logic, which is not very attractive to private entities.
The Basic Law on Health recently reformulated (Portugal, 2019PORTUGAL. Lei nº 95/2019, de 4 de setembro de 2019. Aprova a Lei de Bases da Saúde e revoga a Lei nº 48/90, de 24 de agosto, e o Decreto-Lei nº 185/2002, de 20 de agosto. Diário da República, Poder Executivo, Lisboa, 4 set. 2019. Série I, n. 169, p. 55-66. Disponível em: <Disponível em: https://bit.ly/3coBB0n
>. Acesso: 11 dez. 2019.
https://bit.ly/3coBB0n...
, p. 56), assumes in Base I, Principle 2, the importance of co-responsibility in health, in its multiple dimensions:
(2) The right to health protection is a joint responsibility of people, society and the State and includes access, throughout life, to health promotion, prevention, treatment and rehabilitation, to long-term care and palliative care.
Additionally, in Base II - People’s rights and duties; due to the growing aging of Portuguese demography, the legislator emphasized the need for respecting the principles of equality and non-discrimination, specifically safeguarding the elderly’s right to health, well-being and autonomy:
(l) [the right] To the promotion of well-being and quality of life during aging, in an inclusive and active perspective that favors the ability to decide and control their lives, through the creation of adaptive mechanisms of acceptance, autonomy and independence, with determining socio-economic, environmental, social response and health care factors.
The importance of the norms that establish the right to health is emphasized, both in its general guarantees and in the specificity of its target audience, because, below, we will discuss a set of challenges that the management of the elderly’s health and well-being poses to the SNS, recognizing, simultaneously, the right of access to the disease control and health promotion, free and informed consent and the right to participate, as an individual or community, in the monitoring and evaluation of health policies in Portugal.
Demographic aging and the health profile: observation of indicators
The structural increase in aging poses specific challenges, particularly in the health field, calling for an integrative approach in terms of public policies.
In the countries of the European Union (EU), the decline in the Fertility Rate (FR) has been consistent since the 1980s, remaining below the rate of renewal of generations (Table 1), culminating in aged demographic structures, with specific needs to be met, combining access, autonomy, sustainability, responsibility, and participation.
Having developed countries as a reference, since the end of the 1980s the transition in health conditions has been confirmed, guided by changes in the frequency, magnitude and distribution of morbidity, expressed through deaths due to specific causes and disabilities, materialized by consolidation of the epidemiological transition in its most evolved phase (phase IV), marked by the growing importance of managing the disease chronicity, associated with the postponement of the progression of degenerative pathologies, together with an increase in social pathologies - accidents, suicides, homicides (Omran, 1998Omran, A. R. The epidemiologic transition theory revisited thirty years later. World Health Statistics Quarterly, Genebra, v. 53, n. 2-4, p. 99-119, 1998.).
In Portugal, the population ≥65 years represents 21.9% of the total population (INE, 2018INE - INSTITUTO NACIONAL DE ESTATÍSTICA DE PORTUGAL. Destaque: Projeções da População Residente, 2015-2080. Lisboa, 2018. Disponível em: <Disponível em: https://bit.ly/2Xe4eYH
>. Acesso em: 2 abr. 2018.
https://bit.ly/2Xe4eYH...
), reaching 30% in 2035, showing an important growth of the elderly over 75 years old (Graph 1), thanks to a constant increase of life expectancy, which, in 2035, should reach the value of 86.7 years for women and 80.9 years for men (INE projections (2017INE - INSTITUTO NACIONAL DE ESTATÍSTICA DE PORTUGAL. Evolução da população portuguesa por grupos de idade; cenário central. Lisboa, 2017. Disponível em: <Disponível em: https://bit.ly/2zLOeET
>. Acesso em:12 dez. 2019.
https://bit.ly/2zLOeET...
); central scenario).5
5
Main hypothesis: predicts a moderate recovery in fertility, with FT of 1.55 children per woman in 2080 and an increase in the average age of the mother at the birth of a child, between 1.3 and 1.8 years between 2015 and 2080 (INE, 2017).
As shown below, the main causes of death for the Portuguese population aged 50-69 years (Chart 1) are in line with those observed in countries with a high sociodemographic index, with a predominance of mortality associated with chronic and degenerative pathologies, with respiratory infections, followed by unintentional injuries, in which falls prevail, and also intentional injuries, which can be associated with mental illness and contexts of violence and social deterioration. In an interval of 27 years (1990-2017), regarding the 10 main causes of death in the elderly, not only was there an absolute reduction in premature mortality (<70 years), but also the change in their relative position was observed, the combined result of implantation of priority intervention programs, with a component of prevention of the main pathologies, associated with an improvement in access conditions through the so-called Vias Verdes (VV) with information systems integrated between the pre-hospital and hospital aspects, contributing to the achievement of mortality reduction goals.
Above 70 years of age (Chart 2), the 10 main causes of death observed in Portugal are also in line with those recorded in developed countries, except for respiratory infections and tuberculosis, which, in Western Europe, is ranked 6th, representing 4.1% of the total of deaths, against 7.4% observed in Portugal, which ranks 4th in the same age range.
Evolution of the Portuguese population by age group, 2011-2035 (projection, central scenario)
Evolution of the 10 main causes of death from 50 to 69 years old in Portugal, (% of total deaths)
Evolution of the 10 main causes of death in people aged ≥≥ 70 years in Portugal, (% of total deaths)
The higher prevalence of respiratory infection in the elderly Portuguese population has different reasons, which include the association of multimorbidity, mostly due to chronic disease, and even unique socioenvironmental factors that may be associated with energy poverty in Portugal. According to Ferreira (2018FERREIRA, P. J. Perfil das comorbilidades associadas à infeção gripal, estudo retrospetivo de 5 anos. 2018. 44 f. Dissertação (Mestrado Integrado em Medicina) - Faculdade de Medicina, Universidade de Coimbra, Coimbra, 2018.), the prevalence of Chronic Obstructive Pulmonary Disease (COPD) in older patients with a history of smoking, may justify a higher risk of respiratory infection. Elderly people with COPD, and who choose not to be vaccinated for the flu, generate hospitalization rates twice as high during the flu season when compared to the rest of the year. Souza et al. (2014SOUZA, A. et al. Hospitalização por infeção respiratória associada a fatores ambientais. Revista Brasileira em Promoção da Saúde, Fortaleza, v. 27, n. 3, p. 312-318, 2014. Disponível em: <Disponível em: https://bit.ly/3gKFakC
>. Acesso em:19 dez. 2019.
https://bit.ly/3gKFakC...
) signal a potential increase in severe seasonal morbidity for diseases of the respiratory system due to climatic variables, mainly with the appearance of cold air masses that, in addition to lowering the temperature, favor the precipitation of particulate matter from the atmosphere by decreasing the intensity of the wind current. In the Portuguese case, this issue has been gaining relevance in the scope of the discussion on the concept of energy poverty6
6
Boardman (1991 in Henriques, 2018, p. 16) proposed an economic ratio that is used in several countries, including England, where a household is considered to be energy poor if it needs to spend more than 10% of its income on energy (heating, water heating, kitchen, lighting). In Portugal, a significant part of the buildings, built before the energy efficiency regulation for buildings entered into force in 2012, shows a low thermal and energy performance.
, mainly through the investigation of Simões, Gregório and Seixas (2016SIMÕES, S.; Gregório, V.; Seixas, J. Mapping fuel poverty in Portugal. Energy Procedia, Amsterdã, v. 106, p. 155-165, 2016. Disponível em: <Disponível em: https://bit.ly/3eDqPER
>. Acesso em: 2 jan. 2020.
https://bit.ly/3eDqPER...
, p. 164), who recognize that Portugal, together with Greece and Italy, shows a high inability to maintain adequate housing heating, with higher impact on the poorest and most fragile elderly.
With regard to the health issues that generate disability in the elderly (Graph 2), Portugal follows the pattern present in Western Europe, among the five main pathologies that generate disability, chronic-degenerative diseases that worsen with age, requiring multiple care, such as neurological diseases as Alzheimer’s and Parkinson’s, as well as mental illness, or diabetes and chronic kidney disease, which, as we have already seen, are among the main causes of death in the elderly.
In view of the current health profile of the elderly population and the increase in the aging rate, it is not uncommon to observe an association between the growing demographic aging and the increase in health expenditure, with alerts for the risk of financial lack of sustainability of the SNS, generating arguments that justify the reduction of rights. For this reason, and also due to the accommodation of liberal policies, which had greater impact in the last decade, the role of the State as a guarantor of social rights and as a health care provider are pertinently discussed (Nossa, 2017NOSSA, P. Saúde, responsabilidade e governança: o papel do Estado e os desafios neoliberais. In: SIMPÓSIO NACIONAL DE GEOGRAFIA DA SAÚDE, 8., 2017, Dourados. Anais… Dourados: UFGD, 2017. p. 895-904. Disponível em: <Disponível em: https://bit.ly/2BmT4te
>. Acesso em: 3 jan. 2019.
https://bit.ly/2BmT4te...
). Along with this political-economic orientation, a set of circumstances that seem to give legitimacy to the defined path and that collaborate to this political debate are highlighted, bringing together diverse and no less important motivations: (1) financial crisis scenarios with a consequent weakening of resources; (2) convergence and consolidation of demographic aging; (3) increased cost of biomedical innovation; (4) growing expectations that the wealthier populations tend to have in relation to the demand for health care (Barros, 2013BARROS, P. Pela sua saúde. Lisboa: Fundação Francisco Manuel dos Santos, 2013.).
If point (1) is macro-cyclical and, in some cases, consistent with successive commitments that States have made, or have been encouraged to assume, often as debt, the remaining points derive from a social dynamic that authors like Barros (2013BARROS, P. Pela sua saúde. Lisboa: Fundação Francisco Manuel dos Santos, 2013.), Howdon and Rice (2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy
>. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy...
), and French et al. (2017FRENCH, B. et al. End-of-life medical spending in last twelve months of life is lower than previously reported. Health Affairs, Bethesda, v. 36, n. 7, p. 1211-1217, 2017. Disponível em: <Disponível em: https://bit.ly/2MjHvVP
>. Acesso em: 2 jan. 2020.
https://bit.ly/2MjHvVP...
) indicate that may be over-dimensioned.
Demographic aging and increased health expenditure: discussion of a narrative
The warning that social policies, and specifically health policies, can be captured by gerontocratic interests has been the subject of discussion by critics of the social State, addressing the risk of jeopardizing a desirable and necessary intergenerational equity, gaining this growing significance, particularly when States face financial crises and need to cut spending. Gusmano and Allin (2014GUSMANO, M.; Allin, S. Framing the issue of ageing and health care spending in Canada, the United Kingdom and the United States. Health Economics, Policy and Law, Cambridge, v. 9, n. 3, p. 313-328, 2014. Disponível em: <Disponível em: https://bit.ly/3dnsLRN
>. Acesso em: 2 dez. 2019.
https://bit.ly/3dnsLRN...
) analyzed how the issue of aging and intergenerational equity was used to communicate to citizens, through the media, the need for making cuts or adjustments in health expenditure in Canada, in the United States of America (USA) and the United Kingdom between 2005-2010, when public expenditure faced the consequences of the last global financial crisis.
Often, the arguments presented are limited to declaring that the increasing longevity generates an increase in health care costs, although the causal links discussed are vague: “The high costs of keeping our aging population healthy and out of poverty have caused the United States and other democracies to lose rich economic and political footing” (New York Times, Oct. 14 2010 in Gusmano; Allin; 2014GUSMANO, M.; Allin, S. Framing the issue of ageing and health care spending in Canada, the United Kingdom and the United States. Health Economics, Policy and Law, Cambridge, v. 9, n. 3, p. 313-328, 2014. Disponível em: <Disponível em: https://bit.ly/3dnsLRN
>. Acesso em: 2 dez. 2019.
https://bit.ly/3dnsLRN...
, p. 5). This type of statements, amplified successively, even though they identify in the speech other (co) causers factors of the increase in health expenditure, some of which can be modified by improving the organizational efficiency of the SNS, tends to erroneously privilege what Robert Evans (in Hunter, 2010HUNTER, J. Health Minister defends modest spending hikes; need to rein in annual increases in health care spending or “system will implode”. The Globe and Mail, Toronto, 4 mar. 2010.) called “demonization of aging and/or lifestyles” as factors that pressure health costs. Gusmano and Allin (2014GUSMANO, M.; Allin, S. Framing the issue of ageing and health care spending in Canada, the United Kingdom and the United States. Health Economics, Policy and Law, Cambridge, v. 9, n. 3, p. 313-328, 2014. Disponível em: <Disponível em: https://bit.ly/3dnsLRN
>. Acesso em: 2 dez. 2019.
https://bit.ly/3dnsLRN...
) adequately illustrate this discourse of over-dimensioning aging as a factor justifying the increase in health costs. In the analysis of content published by the media, in the 65 articles published in the three countries, other factors were also mentioned as potential drivers of the increase in health costs, but which were given less emphasis and debate (Table 2).
In a careless way, some arguments combine the social expenditure allocated to the payment of pensions and other social benefits with health costs. The expenditure generated by social contracts oriented to the protection of the elderly is highlighted with greater emphasis, omitting the return that this same population generates in the societies in which they operate, boosting significantly a labor market (WHO, 2015WHO - WORLD HEALTH ORGANIZATION. World report on ageing and health. Genebra, 2015. Disponível em: <Disponível em: https://bit.ly/2XOhK5n
>. Acesso em: 12 abr. 2018.
https://bit.ly/2XOhK5n...
). Cook (2011 in WHO, 2015WHO - WORLD HEALTH ORGANIZATION. World report on ageing and health. Genebra, 2015. Disponível em: <Disponível em: https://bit.ly/2XOhK5n
>. Acesso em: 12 abr. 2018.
https://bit.ly/2XOhK5n...
) demonstrated that in the United Kingdom the sum of all social support for the elderly, counted as public expenditure (social benefits and health and welfare costs), totaling £ 136 billion, achieved a return of £ 45 billion through taxation, £ 10 billion from other indirect contributions, to which was added an additional return of £ 76 trillion placed on the economy from consumption and also a return of £ 44 billion through tangible benefits in social assistance and volunteering provided by the same elderly, in a return almost invisible to society.
Moreover, it is important to understand how the forecast of increased health costs is justified. Mostly, the rising costs are based on the construction of a linear projection based on the increase in life expectancy at birth, multiplying the costs generated by individuals in the last years of life over the expected longevity gains for the future, maintaining the morbidity profile without alteration (Granados-Garcia et al., 2018GRANADOS-GARCIA, V. et al. Costos por hospitalización de adultos mayores en un hospital general regional del IMSS. Revista Médica del Instituto Mexicano del Seguro Social, Cidade do México, DF, v. 56, n. Supl. 1, p. 64-70, 2018. Disponível em: <Disponível em: https://bit.ly/3coYUqE
>. Acesso em: 12 dez. 2019.
https://bit.ly/3coYUqE...
; Howdon; Rice, 2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy
>. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy...
). Considering that the statement that, on average, older patients have higher health costs may be true, this statement may include a fallacy indexed to all individuals ≥65 years: (1) without a fine, up-to-date assessment of what age (s) the most significant health expenditures are occurring; (2) disqualifying one of the premises of the review of the epidemiological transition model of Oman (1998), which emphasizes the progressive transfer of the morbimortality burden to the older groups (> 70 years); (3) underestimating the fact that in the member countries of the Organization for Economic Cooperation and Development (OECD) life expectancy between 1985 and 2017 reached a gain of 6.6 years (1985, 73.5 years; 2017; 80 , 1 years; World Bank).7
7
World Bank - Open data. Retrieved from: <https://data.worldbank.org/>. Access on: May 14, 2020
Several authors underline the mistake of continuing to undervalue the compression of morbidity, censoring positions in which age appears as the main determinant of health needs to which local SNS budgets should be indexed (French et al., 2017FRENCH, B. et al. End-of-life medical spending in last twelve months of life is lower than previously reported. Health Affairs, Bethesda, v. 36, n. 7, p. 1211-1217, 2017. Disponível em: <Disponível em: https://bit.ly/2MjHvVP
>. Acesso em: 2 jan. 2020.
https://bit.ly/2MjHvVP...
; Howse, 2012HOWSE, K. Healthy ageing: the role of health care services. Perspectives in Public Health, Thousand Oaks, v. 132, n. 4, p. 171-177, 2012. Disponível em: <Disponível em: https://bit.ly/2yXjz7O
>. Acesso em: 12 dez. 2019
https://bit.ly/2yXjz7O...
; Lansley, 2012 in Howdon; Rice, 2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy
>. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy...
). Fries (1980FRIES, J. F. Ageing, natural death, and the compression of morbidity. The New England Journal of Medicine, Waltham, v. 303, n. 3, p. 130-135, 1980. Disponível em: <Disponível em: https://bit.ly/3gGATin
>. Acesso em: 2 jan. 2020.
https://bit.ly/3gGATin...
) was one of the first researchers who warned that the age at which symptoms of aging and chronic disease (s) first appeared could increase more rapidly than life expectancy. This prediction of postponement of morbidity for later years, anticipated a progressive displacement of health expenditure by age, especially in developed societies, correcting the dogma that aging is fatally equivalent to the expansion of morbidity with direct consequences on health costs in all years of life. As emphasized by Howdon and Rice (2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy
>. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy...
, p. 6), aging does not depend on a “biological clock,” but it is a process of increasing fragility and which is dependent on investments in health, available technology, access and quality health systems used throughout life and the environment experienced. There is evidence that, in addition to postponing the burden of morbidity, quality of life is also added to the elderly person by decreasing severe disability (which requires third-party support to perform simple daily activities), although there is less evidence regarding the reduction of less severe disabilities (WHO, 2015WHO - WORLD HEALTH ORGANIZATION. World report on ageing and health. Genebra, 2015. Disponível em: <Disponível em: https://bit.ly/2XOhK5n
>. Acesso em: 12 abr. 2018.
https://bit.ly/2XOhK5n...
).
Howdon and Rice (2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy
>. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy...
) debate and question the robustness of age-based models as predictors of health costs, stating that the results commonly achieved may not only be ambiguous, but also overestimated in terms of cost growth. According to Zweifel et al. (2004 in Howdon; Rice, 2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy
>. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy...
, p. 62), predictive models show a more accurate performance when, in addition to age, time-to-death is considered [TTD: the time measured from any observation point to death], using probit8
8
Probit - appropriate regression analysis for data sets where the dependent variable is measured in dichotomous units: Yes or no. In that case, the answer is represented by the percentage of survivors.
and OLS (Ordinary Least Squares) techniques. In this methodological context and after inclusion and control of TTD, the studies by Werblow et al. (2007 in Howdon; Rice, 2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy
>. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy...
) state that age appears only as a small determinant in the increase of health care costs in long-term care users (homes, continuing care), being statistically significant, but not revealing, however, any association with increased costs for non-institutionalized patients:
The latent assumption here is that a TTD variable proxies for this health status, which declines as individuals become more morbid as they approach death, and with ever-increasing levels of health investment to (partly) offset this decline in health status and postpone death. (Howdon; Rice, 2018HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy >. Acesso em: 2 jan. 2020.
https://bit.ly/3cnxBgy... , p. 61)
There is sufficient evidence that it is not age itself, but TTD, particularly the last year of life, which should be seen as a driver of health expenditure in the elderly. Wong et al. (2011WONG, A. et al. Exploring the influence of proximity to death on disease-specific hospital expenditures: a carpaccio of red herrings. Health Economics, Chichester, v. 20, n. 4, p. 379-400, 2011.) had already demonstrated that the period associated with the highest health expenditure occurs in the last two years of life, with variation between countries: in Australia and the Netherlands, 10% of all health expenditure is concentrated in this period of life , in the USA, 22% of health expenditure occur in the last year of life. Barros (2013BARROS, P. Pela sua saúde. Lisboa: Fundação Francisco Manuel dos Santos, 2013.) also shares this idea, specifying that end-of-life expenses are not very different, whether the last two years of life occur at 50 or 80, so when the life expectancy of a population increases, there is more people raising the point of consuming health care for older ages. In addition to this, there is the risk of interpretive bias associated with simplistic ways of registering and allocating health care expenditure in Portugal and, probably, in other countries:
Let us admit that a person spends € 10,000 on health care in the last two years of their life. If this person dies at the age of 55, the expenses for the past two years is recorded in an age group <65 years. But if the person dies at the age of 80, the expenses of the last two years of life will appear in the group ≥65 years. […] The growth in expenditure caused by aging, then, corresponds only to the expenses taken in the additional years of life, excluding the last 2 years of life from the count (on average). (Barros, 2013BARROS, P. Pela sua saúde. Lisboa: Fundação Francisco Manuel dos Santos, 2013., p. 32-33)
We should bear in mind that, maintaining the health status relatively conserved and investing in the subjects’ autonomy, we can individually reduce the costs associated with the consumption of health care, postponing them to older ages, but this may not happen at the level of a population. This dimension of uncertainty is partially discussed by Howse (2012HOWSE, K. Healthy ageing: the role of health care services. Perspectives in Public Health, Thousand Oaks, v. 132, n. 4, p. 171-177, 2012. Disponível em: <Disponível em: https://bit.ly/2yXjz7O
>. Acesso em: 12 dez. 2019
https://bit.ly/2yXjz7O...
) when admitting that the gains obtained in the modification of lifestyles achieved in the last decades, such as those associated with smoking reduction, may be compromised by the increasing prevalence of obesity and inactivity which affect young people and adults at present, an exponential increase in the incidence of (type 2) diabetes and related age-adjusted morbidities is expected, with a consequent impact on health expenditure. Kingston, Herrera and Jagger (2018KINGSTON, A.; Herrera, C.; Jagger, A. Forecasting the care needs of the older population in England over the next 20 years: estimates from the Population Ageing and Care Simulation (PACSim) modelling study. The Lancet Public Health, Londres, v. 3, n. 9, p. e447-e455, 2018. Disponível em: <Disponível em: https://bit.ly/36MORe3
>. Acesso em: 2 jan. 2020.
https://bit.ly/36MORe3...
) also published a prospective study on future care needs for the elderly in England (2015-2035), concluding that, in the next 20 years, the English population ≥65 years will have an increase in the number of independent individuals (4.2 years for men; 0.9 years for women) and also of those with complex care needs. We will therefore have a greater number of individuals reaching ≥85 years, but with higher levels of dependence, dementia and comorbidities, so there is urgent need of the domains of health and social support being adjusted to the complex needs of a growing public.
Financing, allocation of expenditure on health and innovation: evidence
Bearing in mind what was discussed about the responsibility of States in the provision of health costs, we find that, for Portugal and for the average of OECD countries, the percentage of GDP allocated to health expenditures grew gradually between 2000 and 2010, in Portugal decreasing by 0.7% in GDP values after the financial crisis, stabilizing at 8.8% in OECD countries. With regard to the percentage of direct payments borne by users, we observed a slight downward trend in the average of OECD countries, varying between 20.2% in 2010 and 20.6% in 2018, while in Portugal, after 2010, we see a 2.8% increase in direct costs borne by citizens to meet health needs (Graph 3).
Through these data, we cannot categorically affirm that aging is not putting pressure on health expenditure, but at least it is lawful to conclude that States have not, in recent years, been allocating a significantly increasing share of the wealth generated to cover health costs; what has been increasing, as observed in Portugal, is the weight of expenditure that citizens bear to meet their health needs, growing above the average of OECD countries, as a consequence of the need for States to reduce expenditure for reasons other than those related to aging.
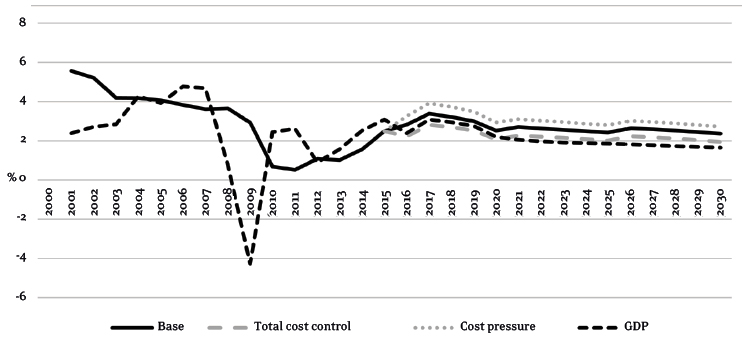
It is evident that the number of the very elderly will increase (≥85 years), in addition to the persistence of statements that associate the growth of health expenditure with aging, we find that the projection of per capita expenditure on health between 2015-2030, indexed to the GDP growth, forecasts annual growth in health expenditure of 2.7% across the OECD, for an average GDP growth of 2.1% in the same range, that is, −0.3% of the average growth in expenditure that occurred in the same period (2000-2015) (Graph 4).
Evolution of health expenditure and GDP growth trend in OECD countries (per capita %; observed and projected: 2000-2030.
Admitting the occurrence of changes in the profile of care demand, imposed by the increase in longevity, it is urgent to rethink how health services are organized at present, how morbidity profiles are managed at all ages, aiming at increasing of well-being and autonomy, bearing in mind health literacy, the digital skills of users and providers in the short and medium term.
It is necessary to act urgently if we want to privilege a system centered on people and health, in which users are partners in the promotion and management of care, expanding the capacity to make better choices, adding critical competence to drive the change in the social environment in the communities in which they operate, as well as managing a wide range of incentives/disincentives that relate health to behavior. In addition to the efficiency gains that can be induced by the digitalization of the SS, Howse (2012HOWSE, K. Healthy ageing: the role of health care services. Perspectives in Public Health, Thousand Oaks, v. 132, n. 4, p. 171-177, 2012. Disponível em: <Disponível em: https://bit.ly/2yXjz7O
>. Acesso em: 12 dez. 2019
https://bit.ly/2yXjz7O...
) emphasizes the need for change in the way providers and users relate, raising the existence of proactive citizens in the identification of health needs and in their management. This paradigm shift has long been discussed. It is known that “emancipated patients” are an important resource for improving health outcomes. In practice, user training will also require providers to have a more pedagogical and empathic attitude, not only admitting the legitimate right to reasonably disagreeing with proposed practices or strategies, but also changing their attitude as providers, feeling responsible to patients rather than responsible for patients (Anderson; Funnell 2005ANDERSON, R. M; Funnell, M. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Education and Counseling, Princeton, v. 57, n. 2, p. 153-1577, 2005. Disponível em: <Disponível em: https://bit.ly/3dmJhl7
>. Acesso em: 12 abr. 2015.
https://bit.ly/3dmJhl7...
, p. 155). According to the European Network on Patient Empowerment (Enope, 2014 in Crisp, 2014CRISP, N. (Org.) Um futuro para a saúde: todos temos um papel a desempenhar. Lisboa: Fundação Calouste Gulbenkian, 2014. Disponível em: <Disponível em: https://bit.ly/2ZTflJr
>. Acesso em : 4 abr. 2015.
https://bit.ly/2ZTflJr...
, p. 53):
Empowering patients means providing them with the opportunities and environment conducive to developing the skills, confidence and knowledge necessary to evolve from passive patients and recipients of health care to an active partner in health care.
Some of the desired goals in the management of chronic disease, which currently absorbs 80% of the investment in health (Ribeiro, 2019RIBEIRO, J. M. Saúde digital. Lisboa: Fundação Francisco Manuel dos Santos, 2019.), include patient autonomy, a reduction in the number of acute episodes, hospitalization times and readmissions, enabling a reduction in hospital occupation. More educated and trained patients can often prevent an acute episode from approaching, so some of the good practices identified involve resource reallocation, guiding them to the training and teaching of users within an integrated health system, articulating different levels of care (Crisp, 2014CRISP, N. (Org.) Um futuro para a saúde: todos temos um papel a desempenhar. Lisboa: Fundação Calouste Gulbenkian, 2014. Disponível em: <Disponível em: https://bit.ly/2ZTflJr
>. Acesso em : 4 abr. 2015.
https://bit.ly/2ZTflJr...
). The patient training program managed by Stanford Medical School (2014Stanford Medical School. Chronic Disease Management Program website patient education. 2014. Disponível em: <Disponível em: https://bit.ly/3eFCAe8
>. Acesso em: 2 jan. 2020.
https://bit.ly/3eFCAe8...
), Chronic Disease Self-Management Program, is a good practice that involves workshops developed in the community, which includes training in applied techniques to manage frustration, fatigue, pain and loneliness, physical exercise, communication with family and health professionals:
Participants demonstrated significant improvements in physical exercise, cognitive symptom management, communication with doctors, self-assessment of general health status, health disorders, fatigue and disability. They spent fewer days in the hospital and there was also a tendency for fewer outpatient visits and hospitalizations. (Crisp, 2014CRISP, N. (Org.) Um futuro para a saúde: todos temos um papel a desempenhar. Lisboa: Fundação Calouste Gulbenkian, 2014. Disponível em: <Disponível em: https://bit.ly/2ZTflJr >. Acesso em : 4 abr. 2015.
https://bit.ly/2ZTflJr... , p. 61)
This paradigm shift has to, imperatively, cover the financing model. Currently, many primary health care units are more awarded for diagnosis than for promoting treatment, autonomy and stability of the patient. Many of the priority programs for the management of chronic disease should comply with a program that would pay less for diagnosis and therapeutic adherence, but, on the contrary, favor the reduction of incidence and prevalence in the community, opposing the dominant logic of financing the production of care in detriment of quality of care. Ribeiro (2019RIBEIRO, J. M. Saúde digital. Lisboa: Fundação Francisco Manuel dos Santos, 2019.) discusses the trends that are reflected in the paradigm shift in the provision of health care, expressing the urgency of evolving into what he calls the health care center, symbolizing not only the centrality of the citizen in the SS, but also the integrated management of the information generated by the user, maximizing team work that extends to all dimensions of care provision:
What makes sense, at a time when connectivity is the great facilitator of permanent monitoring and integration of care, is to have the citizen, sick or not, connected to an institution that guarantees all means, which knows and accompanies him, guarantees him timely responses to his health problems, but, above all, helps him to stay healthy and independent. (Ribeiro: 2019RIBEIRO, J. M. Saúde digital. Lisboa: Fundação Francisco Manuel dos Santos, 2019., p. 100)
The management model that is closest to the “new hospital,” due to its integration, proximity and comprehensiveness, corresponds to the model of Local Health Units, created in Portugal since 1999 and which integrate different providers, with primary, hospital and continuing health care being responsible for the health of a population through contracts (Santana; Costa, 2008SANTANA, R.; COSTA, C. A integração vertical de cuidados de saúde: aspectos conceptuais e organizacionais. Revista Portuguesa de Saúde Pública, Lisboa, v. 7, p. 29-56, 2008.). This model of vertical integration in health advantageously replaces the previous division of competences between primary and hospital health care, whose relevance was primarily due to proximity, while replacing the former hospital centrality without questioning its role as a center of innovation of differentiation: “The hospital of the twenty-first century is the territory par excellence for the coordination of care, the driver of research, the leader of innovation and the catalyst for teamwork in the clinical professions” (Ribeiro, 2019RIBEIRO, J. M. Saúde digital. Lisboa: Fundação Francisco Manuel dos Santos, 2019., p. 99). Although these “new centers,” by assuming themselves as reference centers for therapeutic innovation and practices, may initially function as drivers of increased expenditure, it is expected that, through gains achieved in health, work in the medium term as centers of optimization of the current financing model, contributing to achieving efficiency gains.
Some countries are actively anticipating this process of differentiating and reorganizing care. Ribeiro (2019RIBEIRO, J. M. Saúde digital. Lisboa: Fundação Francisco Manuel dos Santos, 2019., p. 105) highlights the example of the Karolinska University Hospital in Stockholm, which reorganized the traditional division of clinical departments, with the emergence of a new matrix organization, grouping medical assistance, research and teaching, in specialized units, divided into six areas: women’s and children’s health; heart and circulatory system; neoplasms; neurosciences; infection and inflammation; trauma and restorative medicine. This new organization should make the response more flexible and better adapted to therapeutic innovation, integrating personalized solutions and remote care. This latter dimension is part of the so-called digital health ecosystem in which the European Union has been investing systematically since 2009. The e-health environment not only allows reducing the number and cost of users’ trips to hospitals, operating from platforms that can be integrated in a nearby health center, but also allows the automation of records with the users’ participation, through smartphones that connect personal monitoring devices. Added to this it is the important role played by the patient’s early and safe discharge, expanding the spectrum of outpatient care with quality through safety algorithms that signal the potential compromise of previously defined parameters and boost home hospitalization, freeing up beds for seriously ill patients, whose saved value can reach 25% to 30% of the daily cost (Ribeiro, 2019RIBEIRO, J. M. Saúde digital. Lisboa: Fundação Francisco Manuel dos Santos, 2019., p. 107).
Final Considerations
Despite the existence of a set of constitutional guarantees that protect social rights, including the right to health, which for now is guaranteed to all citizens through the SNS, States face neoliberal pressures that use the rationale of sustainability and intergenerational equity as a sufficient condition to, frequently, justify progressive budget cuts or restrictions, materialized in the increase in waiting times, technological obsolescence of services and by the increase in usage costs attributed to users, maintaining the proportion of public investment in terms of GDP unchanged. The issue of increased health costs, associated with demographic aging, is not always supported by an evidence-based discussion, even though some uncertainty prevails related to the increase in the number of the very elderly (≥85 years). It is necessary to continue and expand this debate by validating new models of cost allocation, as shown in the literature considered here, although this theme needs a systematic review not contemplated by this text.
It was evident that the change in the paradigm of the health care delivery model and its financing is crucial to face the concentration of morbidity and increased disability generated by longevity, in addition to the expected increase in costs associated with therapeutic innovation. The growing investment in users’ autonomy, the re-foundation of the hospital model and the use of the virtues of the digital environment in the integration and treatment of health data, generated at multiple points, are pieces of evidence already present in some societies, as has been attested here, which should continue to be investigated due to the efficiency gains they allow.
Referências
- ANDERSON, R. M; Funnell, M. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Education and Counseling, Princeton, v. 57, n. 2, p. 153-1577, 2005. Disponível em: <Disponível em: https://bit.ly/3dmJhl7 >. Acesso em: 12 abr. 2015.
» https://bit.ly/3dmJhl7 - ASF - AUTORIDADE DE SUPERVISÃO DE SEGUROS E FUNDOS DE PENSÕES. Relatório de evolução da atividade seguradora: 3º trimestre. Lisboa, 2019. Disponível em: <Disponível em: https://bit.ly/3dodCjc >. Acesso em: 11 dez. 2019.
» https://bit.ly/3dodCjc - BARROS, P. Pela sua saúde. Lisboa: Fundação Francisco Manuel dos Santos, 2013.
- CRISP, N. (Org.) Um futuro para a saúde: todos temos um papel a desempenhar. Lisboa: Fundação Calouste Gulbenkian, 2014. Disponível em: <Disponível em: https://bit.ly/2ZTflJr >. Acesso em : 4 abr. 2015.
» https://bit.ly/2ZTflJr - FERREIRA, P. J. Perfil das comorbilidades associadas à infeção gripal, estudo retrospetivo de 5 anos. 2018. 44 f. Dissertação (Mestrado Integrado em Medicina) - Faculdade de Medicina, Universidade de Coimbra, Coimbra, 2018.
- FRENCH, B. et al. End-of-life medical spending in last twelve months of life is lower than previously reported. Health Affairs, Bethesda, v. 36, n. 7, p. 1211-1217, 2017. Disponível em: <Disponível em: https://bit.ly/2MjHvVP >. Acesso em: 2 jan. 2020.
» https://bit.ly/2MjHvVP - FRIES, J. F. Ageing, natural death, and the compression of morbidity. The New England Journal of Medicine, Waltham, v. 303, n. 3, p. 130-135, 1980. Disponível em: <Disponível em: https://bit.ly/3gGATin >. Acesso em: 2 jan. 2020.
» https://bit.ly/3gGATin - GRANADOS-GARCIA, V. et al. Costos por hospitalización de adultos mayores en un hospital general regional del IMSS. Revista Médica del Instituto Mexicano del Seguro Social, Cidade do México, DF, v. 56, n. Supl. 1, p. 64-70, 2018. Disponível em: <Disponível em: https://bit.ly/3coYUqE >. Acesso em: 12 dez. 2019.
» https://bit.ly/3coYUqE - GUSMANO, M.; Allin, S. Framing the issue of ageing and health care spending in Canada, the United Kingdom and the United States. Health Economics, Policy and Law, Cambridge, v. 9, n. 3, p. 313-328, 2014. Disponível em: <Disponível em: https://bit.ly/3dnsLRN >. Acesso em: 2 dez. 2019.
» https://bit.ly/3dnsLRN - HENRIQUES, A. F. Relação entre o indicador de pobreza energética e as temperaturas do ar medidas no interior de habitações na região da Grande Lisboa na estação de inverno. 2018. 95 f. Dissertação (Mestrado Integrado Engenharia da Energia e do Ambiente) - Faculdade de Ciências, Universidade de Lisboa, Lisboa, 2018.
- HOWDON, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: implications for an ageing population. Journal of Health Economics, Amsterdã, v. 57, p. 60-74, 2018. Disponível em: <Disponível em: https://bit.ly/3cnxBgy >. Acesso em: 2 jan. 2020.
» https://bit.ly/3cnxBgy - HOWSE, K. Healthy ageing: the role of health care services. Perspectives in Public Health, Thousand Oaks, v. 132, n. 4, p. 171-177, 2012. Disponível em: <Disponível em: https://bit.ly/2yXjz7O >. Acesso em: 12 dez. 2019
» https://bit.ly/2yXjz7O - HUNTER, J. Health Minister defends modest spending hikes; need to rein in annual increases in health care spending or “system will implode”. The Globe and Mail, Toronto, 4 mar. 2010.
- IHME - INSTITUTE FOR HEALTH METRICS AND EVALUATION. GBD - Global Burden Disease. Seattle, 2017.
- INE - INSTITUTO NACIONAL DE ESTATÍSTICA DE PORTUGAL. Destaque: Projeções de População Residente - 2012-2060. Lisboa, 2014. Disponível em: <Disponível em: https://bit.ly/3eFbZ0O >. Acesso em: 12 maio 2015.
» https://bit.ly/3eFbZ0O - INE - INSTITUTO NACIONAL DE ESTATÍSTICA DE PORTUGAL. Destaque: Projeções da População Residente, 2015-2080. Lisboa, 2018. Disponível em: <Disponível em: https://bit.ly/2Xe4eYH >. Acesso em: 2 abr. 2018.
» https://bit.ly/2Xe4eYH - INE - INSTITUTO NACIONAL DE ESTATÍSTICA DE PORTUGAL. Evolução da população portuguesa por grupos de idade; cenário central. Lisboa, 2017. Disponível em: <Disponível em: https://bit.ly/2zLOeET >. Acesso em:12 dez. 2019.
» https://bit.ly/2zLOeET - KINGSTON, A.; Herrera, C.; Jagger, A. Forecasting the care needs of the older population in England over the next 20 years: estimates from the Population Ageing and Care Simulation (PACSim) modelling study. The Lancet Public Health, Londres, v. 3, n. 9, p. e447-e455, 2018. Disponível em: <Disponível em: https://bit.ly/36MORe3 >. Acesso em: 2 jan. 2020.
» https://bit.ly/36MORe3 - MONGE, C. O direito fundamental à proteção da saúde. e-Púbica - Revista Eletrónica de Direito Público, Lisboa, v. 6, n. 1, p. 75-100, 2019. Disponível em: <Disponível em: https://bit.ly/2Ay6ORh >. Acesso em: 20 dez. 2019.
» https://bit.ly/2Ay6ORh - NOSSA, P. Saúde, responsabilidade e governança: o papel do Estado e os desafios neoliberais. In: SIMPÓSIO NACIONAL DE GEOGRAFIA DA SAÚDE, 8., 2017, Dourados. Anais… Dourados: UFGD, 2017. p. 895-904. Disponível em: <Disponível em: https://bit.ly/2BmT4te >. Acesso em: 3 jan. 2019.
» https://bit.ly/2BmT4te - OCDE - ORGANIZAÇÃO PARA A COOPERAÇÃO E DESENVOLVIMENTO ECONÔMICO. Health at a glance 2019: OECD Indicators. Paris, 2019. Disponível em: <Disponível em: https://bit.ly/2Tbo5pZ >. Acesso em: 12 dez. 2019.
» https://bit.ly/2Tbo5pZ - Omran, A. R. The epidemiologic transition theory revisited thirty years later. World Health Statistics Quarterly, Genebra, v. 53, n. 2-4, p. 99-119, 1998.
- PORTUGAL. Lei nº 95/2019, de 4 de setembro de 2019. Aprova a Lei de Bases da Saúde e revoga a Lei nº 48/90, de 24 de agosto, e o Decreto-Lei nº 185/2002, de 20 de agosto. Diário da República, Poder Executivo, Lisboa, 4 set. 2019. Série I, n. 169, p. 55-66. Disponível em: <Disponível em: https://bit.ly/3coBB0n >. Acesso: 11 dez. 2019.
» https://bit.ly/3coBB0n - RIBEIRO, J. M. Saúde digital. Lisboa: Fundação Francisco Manuel dos Santos, 2019.
- SANTANA, R.; COSTA, C. A integração vertical de cuidados de saúde: aspectos conceptuais e organizacionais. Revista Portuguesa de Saúde Pública, Lisboa, v. 7, p. 29-56, 2008.
- SIMÕES, S.; Gregório, V.; Seixas, J. Mapping fuel poverty in Portugal. Energy Procedia, Amsterdã, v. 106, p. 155-165, 2016. Disponível em: <Disponível em: https://bit.ly/3eDqPER >. Acesso em: 2 jan. 2020.
» https://bit.ly/3eDqPER - SOUZA, A. et al. Hospitalização por infeção respiratória associada a fatores ambientais. Revista Brasileira em Promoção da Saúde, Fortaleza, v. 27, n. 3, p. 312-318, 2014. Disponível em: <Disponível em: https://bit.ly/3gKFakC >. Acesso em:19 dez. 2019.
» https://bit.ly/3gKFakC - Stanford Medical School. Chronic Disease Management Program website patient education. 2014. Disponível em: <Disponível em: https://bit.ly/3eFCAe8 >. Acesso em: 2 jan. 2020.
» https://bit.ly/3eFCAe8 - WHO - WORLD HEALTH ORGANIZATION. World report on ageing and health. Genebra, 2015. Disponível em: <Disponível em: https://bit.ly/2XOhK5n >. Acesso em: 12 abr. 2018.
» https://bit.ly/2XOhK5n - WONG, A. et al. Exploring the influence of proximity to death on disease-specific hospital expenditures: a carpaccio of red herrings. Health Economics, Chichester, v. 20, n. 4, p. 379-400, 2011.
-
5
Main hypothesis: predicts a moderate recovery in fertility, with FT of 1.55 children per woman in 2080 and an increase in the average age of the mother at the birth of a child, between 1.3 and 1.8 years between 2015 and 2080 (INE, 2017INE - INSTITUTO NACIONAL DE ESTATÍSTICA DE PORTUGAL. Evolução da população portuguesa por grupos de idade; cenário central. Lisboa, 2017. Disponível em: <Disponível em: https://bit.ly/2zLOeET >. Acesso em:12 dez. 2019.
https://bit.ly/2zLOeET... ). -
6
Boardman (1991 in Henriques, 2018HENRIQUES, A. F. Relação entre o indicador de pobreza energética e as temperaturas do ar medidas no interior de habitações na região da Grande Lisboa na estação de inverno. 2018. 95 f. Dissertação (Mestrado Integrado Engenharia da Energia e do Ambiente) - Faculdade de Ciências, Universidade de Lisboa, Lisboa, 2018., p. 16) proposed an economic ratio that is used in several countries, including England, where a household is considered to be energy poor if it needs to spend more than 10% of its income on energy (heating, water heating, kitchen, lighting). In Portugal, a significant part of the buildings, built before the energy efficiency regulation for buildings entered into force in 2012, shows a low thermal and energy performance.
-
7
World Bank - Open data. Retrieved from: <https://data.worldbank.org/>. Access on: May 14, 2020
-
8
Probit - appropriate regression analysis for data sets where the dependent variable is measured in dichotomous units: Yes or no. In that case, the answer is represented by the percentage of survivors.
Publication Dates
-
Publication in this collection
29 July 2020 -
Date of issue
2020
History
-
Received
07 Feb 2020 -
Accepted
15 Apr 2020


 Source:
Source:  Source:
Source:  NCD: noncommunicable diseasesSource:
NCD: noncommunicable diseasesSource: 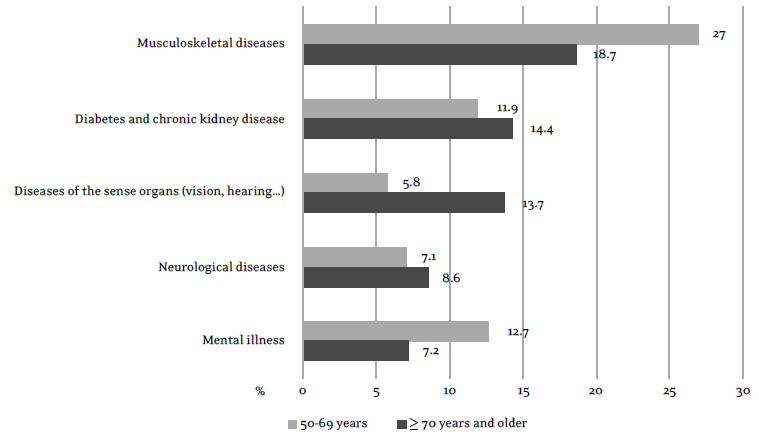 Source:
Source: 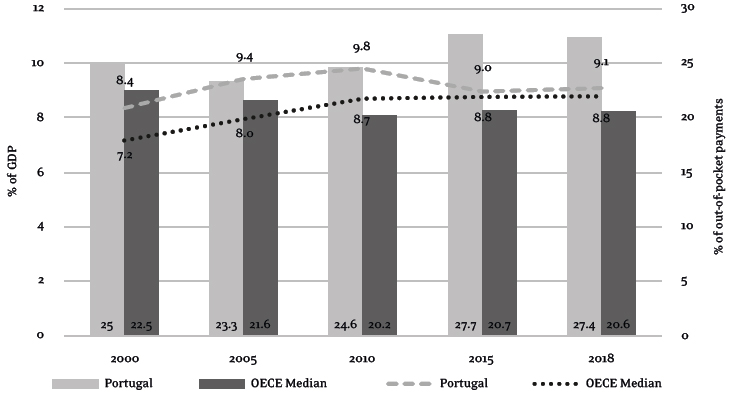 Source: OECD (2019)
Source: OECD (2019)
 Source: OECD (2019)
Source: OECD (2019)