Flocke9
(1997) |
Components of Primary Care Index (CPCI) |
2.899 users assisted by family doctors |
Family Doctor's Offices in Ohio (USA) |
Instrument applied in person by researchers at study sites |
Multidimensional (4): interpersonal communication, knowledge about the patient, coordination of care, preference of the patient to care with his/her family doctor |
Internal consistency |
Cassady10
(2000) |
Primary Care Assessment Tool-Child Edition (PCAT-CE) |
450 parents and caregivers of children and young people under 18 |
Primary Care Services in Washington, DC (USA) |
Instrument applied by telephone |
Multidimensional (5): Longitudinality/relationship, accessibility of first contact, coverage of available services, coverage of services provided, coordination |
Content and construct validity, internal consistency |
Cooley11
(2003) |
Medical Home Index (MHI) - Long version
|
Doctors and non-doctors members of the health team of 43 health units |
43 pediatric primary care units in various states of the USA |
Instrument applied in person by researchers at study sites |
Multidimensional (6): organizational capacity, management of chronic conditions, coordination of care, community extension, data management, improvement of quality |
Construct validity and internal consistency |
Nikbakht Van12
(2005) |
Questionnaire |
59 respondents, including managers and health professionals |
8 local palliative care networks in Rotterdam (Netherlands) |
Self-applicable instrument sent by e-mail |
Contains 200 items divided into structure (demographic characteristics, history, beginning, development stage, resources and organizations participating in the network), process (organization and administration, cooperation and external relations) and result (shared objectives and perceptions, demands for care, quality of cooperation, improvement of care services, established agreements, results associated with patients and organizations, expertise and funding) |
No psychometric validation reported |
Friedberg13
(2008) |
Questionnaire with no name specified |
308 doctors working in primary care |
Primary Care Units in Massachusetts (USA) |
Self-applicable instrument sent to participants |
Multidimensional (4): patient care and reminders, culture of striving for quality, improved access, electronic health records |
No psychometric validation reported |
| Rittenhouse14 (2008) |
Questionnaire with no name specified |
291 health service managers |
Independent medical groups and practice associations in the USA |
Instrument applied by telephone |
Multidimensional (7): personal doctor, doctor-directed medical practice with responsibility for ongoing patient care, comprehensive patient guidance, coordinated/integrated care, quality and safety with evidence-based decisions, timely access to care, and improved communication methods between patients and healthcare team, payment should be commensurated with patient care and outcomes |
No psychometric validation reported |
Birnberg15
(2011) |
Safety Net Medical Home Scale (SNMHS) |
Health service managers assisted by the health team |
65 rural and urban clinics (USA) |
Self-applicable instrument sent by e-mail |
Multidimensional (6): access and communication, patient and record follow-up, care management, referral testing and follow-up, quality improvements, external coordination |
Content validity, internal consistency and convergent validity |
Rodrigues16 (2014)
Rodrigues17 (2015) |
Assessment Tool for the Coordination of Primary Health Care Networks by PHC (Copas) |
Health professionals linked to the Family Health Strategy |
Health Units with Family Health Strategy in Minas Gerais (Brazil) |
In person self-applicable instrument |
Multidimensional (5): population, Primary Health Care, support systems, logistics systems, management system |
Internal consistency, content validity, convergent and discriminatory, ceiling and floor test |

 Evaluation instruments for primary care network structures: an integrative review
Evaluation instruments for primary care network structures: an integrative review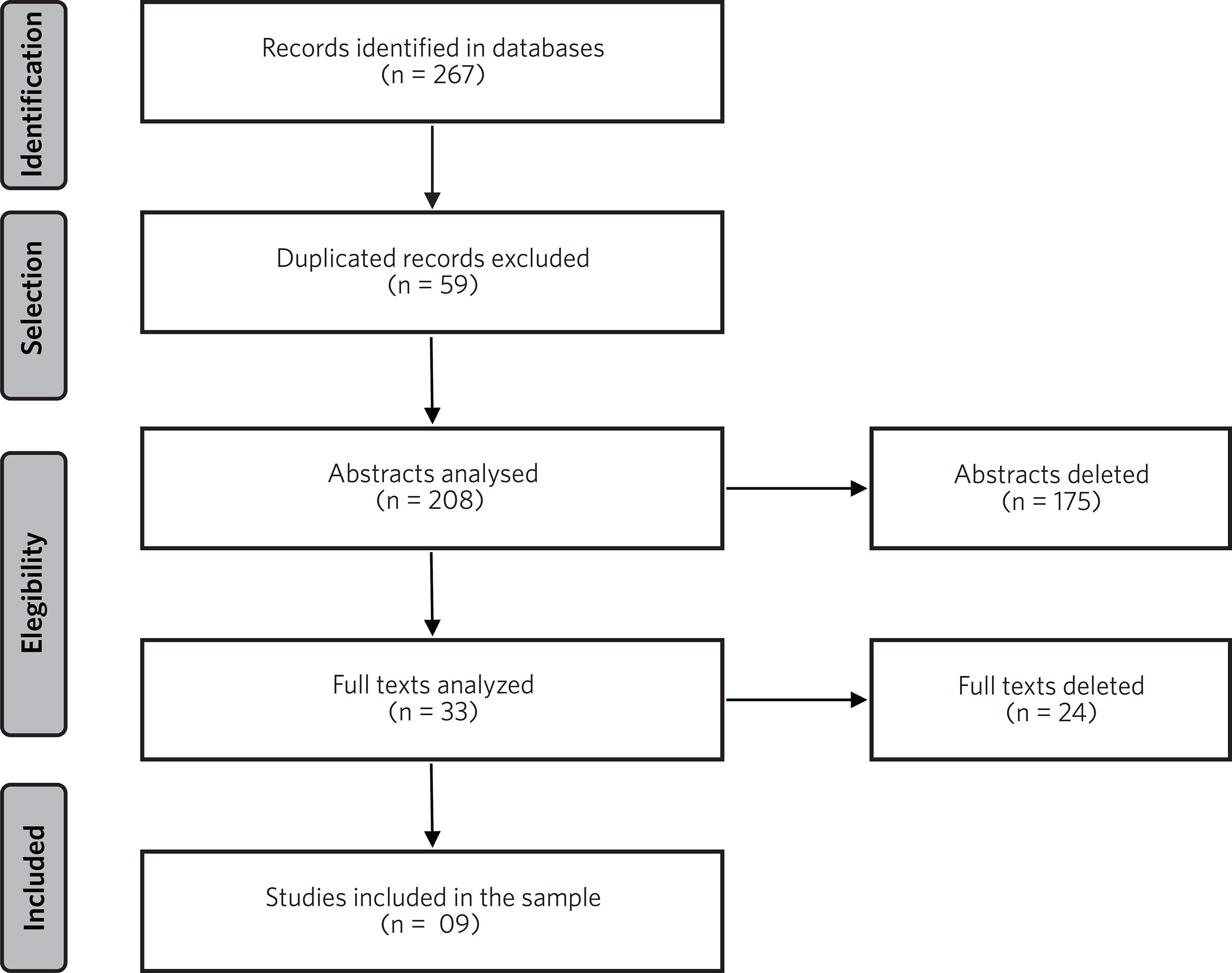 Source: Research data, 2019.
Source: Research data, 2019.