ABSTRACT
Objective:
to analyze the national and international scientific research regarding the impact of the bundles in the prevention of central venous catheter-related bloodstream infection in an adult intensive care unit.
Method:
integrative review of articles published in Portal Capes, Virtual Health Library, PubMed, Science Direct, Cochrane, CINAHL and SCOPUS, between 2011 and 2016.
Results:
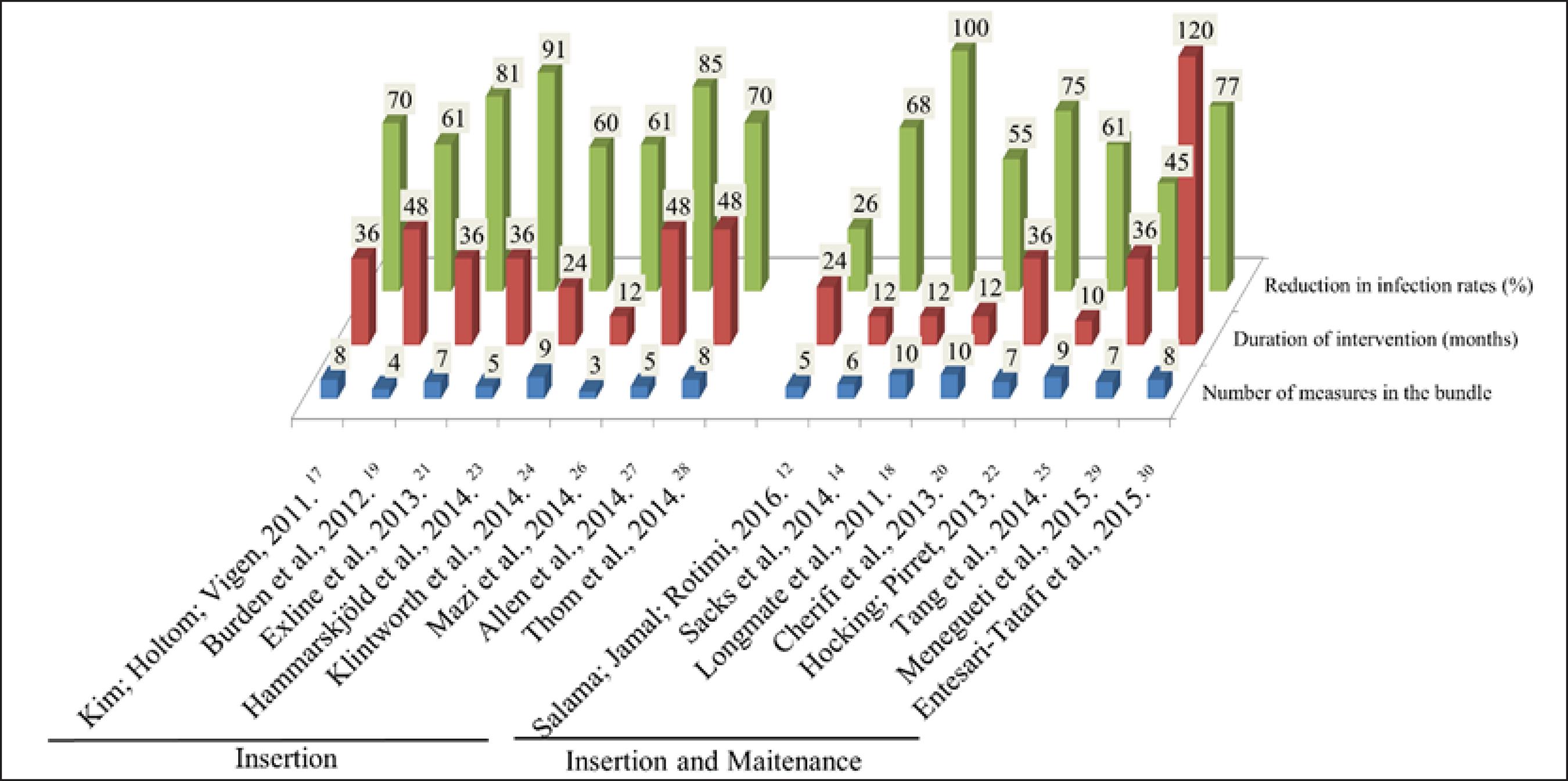
16 articles were found, 100% related to the implementation of the bundles for the insertion of the central venous catheter and 50% to related to the maintenance of this device. The intervention time was varied, as were the number of measurements and the analyzation period analyzed (catheter insertion / maintenance). However, all studies showed that there was a reduction of between 26% e 100% of bloodstream infections related to the use of the device.
Conclusion:
the adoption of the bundle showed a positive impact on the reduction of infections. However, there was no direct relationship between the number of measures described in the studies or length of implementation time or higher rates of infection reduction.
DESCRIPTORS:
Catheter-related infections; Catheters; Intensive care unit; Hospital infection; Patient safety
RESUMO
Objetivo:
analisar as produções científicas nacionais e internacionais sobre o impacto dos bundles na prevenção de infecção da corrente sanguínea relacionada ao cateter venoso central em unidade de terapia intensiva adulta.
Método:
revisão integrativa de artigos publicados no Portal Capes, Biblioteca Virtual em Saúde, PubMed, Science Direct, Cochrane, CINAHL e SCOPUS, entre 2011 e 2016.
Resultados:
encontraram-se 16 artigos, 100% relacionados à implementação dos bundles para a inserção do cateter venoso central e 50% à manutenção deste dispositivo. O tempo de intervenção foi variado, bem como o número de medidas e o período analisado (inserção/manutenção do cateter). No entanto, a redução da infecção da corrente sanguínea relacionada ao dispositivo foi apontada em todos os estudos entre 26% e 100%.
Conclusão:
a adoção de bundle evidenciou um impacto positivo na redução da infecção. Todavia, não se observou uma relação direta entre o número de medidas descritas nos estudos ou o maior tempo de implementação e taxas mais altas de redução da infecção.
DESCRITORES:
Infecções relacionadas a cateter; Cateteres; Unidade de terapia intensiva; Infecção hospitalar; Segurança do paciente
RESUMEN
Objetivo:
analizar las producciones científicas nacionales e internacionales sobre el impacto del bundles en la prevención de infección del flujo sanguíneo relacionado al catéter venoso central en unidad de terapia intensiva adulta.
Método:
revisión integrativa de artículos publicados en el Portal Capes, Biblioteca Virtual en Salud, PubMed, Science Direct, Cochrane, CINAHL y SCOPUS, entre 2011 y 2016.
Resultados:
se encontraron 16 artículos, 100% relacionados a la implementación de los lotes para la inserción del catéter venoso central y 50% al mantenimiento de este dispositivo. El tiempo de intervención fue variado, así como el número de medidas y el período analizado (inserción / mantenimiento del catéter). Sin embargo, la reducción de la infección del flujo sanguíneo relacionado con el dispositivo fue señalada en todos los estudios entre el 26% y el 100%.
Conclusión:
la adopción del lote evidenció un impacto positivo en la reducción de la infección. Sin embargo, no se observó una relación directa entre el número de medidas descritas en los estudios o el mayor tiempo de implementación y tasas más altas de reducción de la infección.
DESCRIPTORES:
Infecciones relacionadas con catéter; Catéteres; Unidad de terapia intensiva; Infección hospitalaria; Seguridad del paciente
INTRODUCTION
Hospital-acquired infections (HAI) are defined as a local or systemic condition resulting from an adverse reaction to the presence of an infectious agent or its toxin and without evidence that the infection was present or incubated at the time of patient admission in hospital or outpatient setting. They are diagnosed, usually after 48 hours after hospitalization.11 World Health Organization. Report on the burden of endemic health care-associated infection worldwide. A systematic review of the literature. [Internet]. 2011[cited 2016 Jun 07]. Available from: http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf
http://apps.who.int/iris/bitstream/10665...
The main HAI are: respiratory tract infection, urinary tract infection, blood stream and surgical site infection.22 Agência Nacional de Vigilância Sanitária. Medidas de prevenção de infecção relacionada à assistência à saúde. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2013:1-87.
Data from the National Healthcare Safety Network (NHSN) show that, among HAI, central venous catheter-related bloodstream infection (CVC) are the leading cause of infection in the Intensive Care Unit (ICU).33 National Healthcare Safety Network. NHSN Central Line-associated Bloodstream Infection Surveillance in 2014. National Center for Emerging and Zoonotic Infectious Diseases. [Internet]. 2014 Mar [cited 2016 Feb 02]. Available from: http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf
http://www.cdc.gov/nhsn/PDFs/training/tr...
It is estimated that 30,000 new cases occur in ICU departments in the United States each year.44 National Healthcare Safety Network. Patient Safety Component Manual [Internet]. 2017 Jan [cited 2017 Feb 14]. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf
https://www.cdc.gov/nhsn/pdfs/pscmanual/...
In 2014, 26.5 infections per 1,000 catheters / day occurred in England. In other European countries, there was an occurrence of around 13.3 infections per 1,000 catheters/day.55 Mok Q. How I diagnose and manage catheter-associated blood stream infections. J Paediatr Child Health [Internet]. 2015 May [cited 2016 Jun 07]; 25(5):243-4. Available from: http://www.paediatricsandchildhealthjournal.co.uk/article/S1751-7222(14)00223-6/pdf
http://www.paediatricsandchildhealthjour...
-66 Martínez-Morel HR, Sánchez-Payá J, Molina-Gómez MJ, García-Shimizu P, García RV, Villanueva-Ruiz C, et al. Catheter-related bloodstream infection: burden of disease in a tertiary hospital. J Hosp Infect [Internet]. 2014 Jul [cited 2016 Feb 02]; 87(3):165-70. Available from: http://www.sciencedirect.com/science/article/pii/S0195670114001285
http://www.sciencedirect.com/science/art...
This type of infection is associated with an increase in hospitalization time ranging between an extra 10 and 20 days and with a cost of approximately US $ 30,000.00 per patient.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
The systematization of epidemiological data on CVC-related bloodstream infection in the ICU in Brazil was started in 2010, with the creation of FormSUS. The rates of infection varied between 4.1 and 5.1 infections per 1000 CVC / day by 2015.88 Agência Nacional de Vigilância Sanitária. Avaliação dos indicadores nacionais de infecção relacionada à assistência ano de 2014 e relatório de progresso. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2015. Data regarding prolonged hospitalization and its associated costs are not known in official publications.99 Souza ES, Belei RA, Carrilho CMDM, Matsuo T, Yamada-Ogatta SF, Andrade G et al. Mortalidade e riscos associados a infecção relacionada à assistência à saúde. Texto Contexto Enferm [Internet]. 2015 Jan-Mar [cited 2017 Feb 14]; 24(1): 220-8. Available from: http://www.redalyc.org/pdf/714/71438421027.pdf
http://www.redalyc.org/pdf/714/714384210...
However, the mortality rate from CVC infections in then ICU can affect up to 69% of patients.22 Agência Nacional de Vigilância Sanitária. Medidas de prevenção de infecção relacionada à assistência à saúde. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2013:1-87.
The use of an intravascular device, especially CVC, is the main risk factor for bloodstream infection, and approximately 90% of these are related to its use.33 National Healthcare Safety Network. NHSN Central Line-associated Bloodstream Infection Surveillance in 2014. National Center for Emerging and Zoonotic Infectious Diseases. [Internet]. 2014 Mar [cited 2016 Feb 02]. Available from: http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf
http://www.cdc.gov/nhsn/PDFs/training/tr...
,1010 The Joint Commission. Preventing central line-associated bloodstream infections: a global challenge, a global perspective. Oak Brook, IL: Joint Commission Resources. [Internet]. 2012 May [cited 2016 Feb 02]. Available from: https://www.jointcommission.org/assets/1/18/CLABSI_Monograph.pdf
https://www.jointcommission.org/assets/1...
CVC-related bloodstream infections are considered, in most cases, as an avoidable complication of patient safety and may be prevented by interventions during insertion and manipulation of the catheters. The Institute for Health Improvement promoted the"Save 100,000 lives" campaign in 2004, which introduced the concept of a central line bundle, which is based on the adoption of a set of measures based on integrated scientific evidence in order to reduce these infections.1111 Institute for Health Improvement. Protecting 5 million lives. Cambridge [Internet]. 2004 [cited 2016 Jun 07]. Available from: http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx
http://www.ihi.org/engage/initiatives/co...
These measures are described by the Center for Disease Control and Prevention (CDC) and have been included in clinical practice in the form of intervention packages, called bundles.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
,1111 Institute for Health Improvement. Protecting 5 million lives. Cambridge [Internet]. 2004 [cited 2016 Jun 07]. Available from: http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx
http://www.ihi.org/engage/initiatives/co...
-1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
There are several suggested measures to prevent CVC-related infection, which make up the bundles which can be performed separately or together. The needs of each institution should be considered as a priority, in addition to the patient's profile, the human and material resources, the availability of education, training and supervision with the team responsible for insertion maintenance and care of the intravenous devices.1313 Labeau SO, Vandijck DM, Rello J, Adam S, Rosa A, Wenisch C, et al. Centers for Disease Control and Prevention guidelines for preventing central venous catheter-related infection: results of a knowledge test among 3405 European intensive care nurses. Crit Care Med [Internet]. 2009 Jan [cited 2016 Jun 07]; 37(1):320-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19050628
http://www.ncbi.nlm.nih.gov/pubmed/19050...
-1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
Bundles have been widely disseminated and are being implemented in hospital institutions. Their adoption has been identified as effective in preventing and reducing CVC- related bloodstream infections and improving the quality of service. However, professional adherence to these measures remain low, which in turn causes a high incidence of this infection. Another gap in the knowledge is the absence of studies that address the results of health professional adherence to the recommendations of preventative practices related to this type of infection. Therefore, strategies that point to improvements in clinical practice and increased patient safety should be encouraged, especially those focused on insertion time and maintenance of the CVC.
The knowledge of the teams who are responsible for insertion and maintenance of the CVC and bundle and its impact on the prevention of bloodstream infection may highlight evidence related to safe practices which are needed improve patient care, especially those under critical conditions. This could be used to review CVC insertion and manipulation practices, leading to better quality of care and reducing the morbidity and mortality due to this infection.
Considering the importance of using the bundle in clinical practice for the reduction of bloodstream infections, the objective was to analyze the national and international scientific research regarding the impact of the bundles in the prevention of CVC-related bloodstream infections in adult ICU settings.
METHOD
An integrative literature review whose purpose was to gather and synthesize the available evidence in original articles regarding the theme. The scope of scientific evidence was used as a foundation, which composed the research focus: implementation and impact of bundle use in clinical practice by identifying a question of great practical relevance. In the concrete plan, the PICO strategy was adopted, structured as follows: P=Patient, I=Intervention, C=Comparison and O=Outcomes.1515 Santos CMC, Pimenta CAM, Nobre MRC. A estratégia PICO para a construção da pergunta de pesquisa e busca de evidências. Rev Latino-Am. Enfermagem [Internet]. 2007 Jun [cited 2016 Aug 01]; 15(3):508-11. Available from: http://www.scielo.br/scielo.php?pid=S0104-11692007000300023&script=sci_arttext&tlng=pt
http://www.scielo.br/scielo.php?pid=S010...
A research question was defined based on this strategy: what national and international scientific research highlight the impact of the bundle in the prevention of CVC-related bloodstream infection in the adult ICU setting?
The search for articles was carried out by the Portal Capes and Biblioteca Virtual em Saúde; and the electronic databases of U.S. National Library of Medicine (PubMed), Science Direct, Cochrane, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and SCOPUS.
Inclusion criteria included: original articles that addressed the impact of bundles in the reduction of CVC-related bloodstream infection in adult ICUs regardless of research method, as well as being published as of 2011, being the year in which the CDC published the last guideline on the prevention of infections related to intravascular devices. All other articles which did not meet these criteria were excluded.
The following controlled descriptors were used: catheter related infections, catheters, intensive care unit and hospital infection. As uncontrolled descriptors: bundle, reduction of infection rates, central venous catheter, prevention and infection of the bloodstream. All these descriptors were used alone and together with the help of boolean operators.
From the association between all the controlled and uncontrolled descriptors, 36 articles were identified, which, after reading them in full, were reduced to 16 due to the inclusion criterion approach; the implementation of bundles and their potential impact in clinical practice.
The levels of evidence were characterized by hierarchy, depending on the adopted methodological approach based on categorization which was classified into six levels:1616 Stetler CB, Morsi D, Rucki S, Broughton S, Corrigan B, Fitzgerald J, et al. Utilization-focused integrative reviews in a nursing service. Appl Nurs Res [Internet]. 1998 Nov [cited 2016 Mar 01]; 11(4):1-11. Available from: http://www.appliednursingresearch.org/article/S0897-1897(98)80329-7/pdf
http://www.appliednursingresearch.org/ar...
-
level 1: evidence resulting from the meta-analysis (controlled and randomized clinical studies);
-
level 2: evidence obtained from studies with experimental design;
-
level 3: evidence from almost experimental studies;
-
level 4: evidence from descriptive (non-experimental) studies or qualitative approach;
-
level 5: evidence from case or experience reports;
-
level 6: evidence based on expert opinions or consensus.
RESULTS
Based on the inclusion criteria, the final sample consisted of 16 articles, distributed as follows: Science Direct (5/16), Pubmed (9/16) and Cinahl (2/16). As for the research design, there were cohort studies (16/16), level of evidence 2, performed in Saudi Arabia (1/16), Australia (1/16), Belgium (1/16), Brazil (1 / 16), United States (7/16), England (1/16), Kuwait (1/16), New Zealand (1/16), Sweden (1/16) and Taiwan (1/16) Years of 2011 (2/16), 2012 (1/16), 2013 (3/16), 2014 (7/16), 2015 (2/16) and 2016 (1/16).
In 100% of the researched articles, bundles were implemented in the period of CVC insertion and 50% during their maintenance, whose measurements and results are described in table 1, taking into account the intervention, comparison and outcome assumptions, especially the fact that all studies were aimed at patients admitted to an adult ICU.
Summary of measures implemented to prevent infection related to the central venous catheter, according to the moment of its indication (insertion, maintenance and others), duration of intervention and rate of reduction. Belo Horizonte, MG, Brazil, 2016. (n=16)
The measures implemented in the CVC insertion bundle were: maximal sterile barrier precautions; (use of sterile gloves, cap, mask, apron and sterile field - 94% of studies);1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
18 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
19 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
20 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
21 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
22 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
23 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
24 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
-2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2727 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
28 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
29 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
skin asepsis (94%),1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
18 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
19 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
20 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
21 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
22 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
23 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
24 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
-2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2727 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
28 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
29 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
hand hygiene before insertion (62%),1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
24 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
25 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
26 Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
http://www.sciencedirect.com/science/art...
27 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
-2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
preference for the subclavian vein (44%),1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2727 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
avoiding femoral vein (37%),1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
immediate removal of CVC without clinical indication for its use (37%),1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
,2626 Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
http://www.sciencedirect.com/science/art...
,2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
ultrasound to guide the insertion of the catheter (19%);1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
allow the antiseptic to dry before inserting the catheter (12%);2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
CVC impregnated with antibiotic (12%); The CVC was inserted without aseptic techniques within 48 hours (12%),1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
and only designated qualified professionals to insert the CVC (12%).
The maintenance bundle comprised: daily verification of the need for CVC permanence (87%),1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2929 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
disinfection of the hub before administering medications (62%),1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
monitor the insertion site (50%),1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2929 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
dressing replacement with sterile gauze every two days and transparent dressing every 7 days or whenever they are dirty, loose or moist (50%);1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
hygiene of the hands before handling (37%),1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
and asepsis of the skin when changing the dressing (25%). Other measures that also made up the bundle were mentioned in the articles, being: training and continuing education to professionals who insert and manipulate the CVC in 56%1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
26 Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
http://www.sciencedirect.com/science/art...
27 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
28 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
29 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
and feedback of the results, indicated in 31%.1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
.2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
.2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
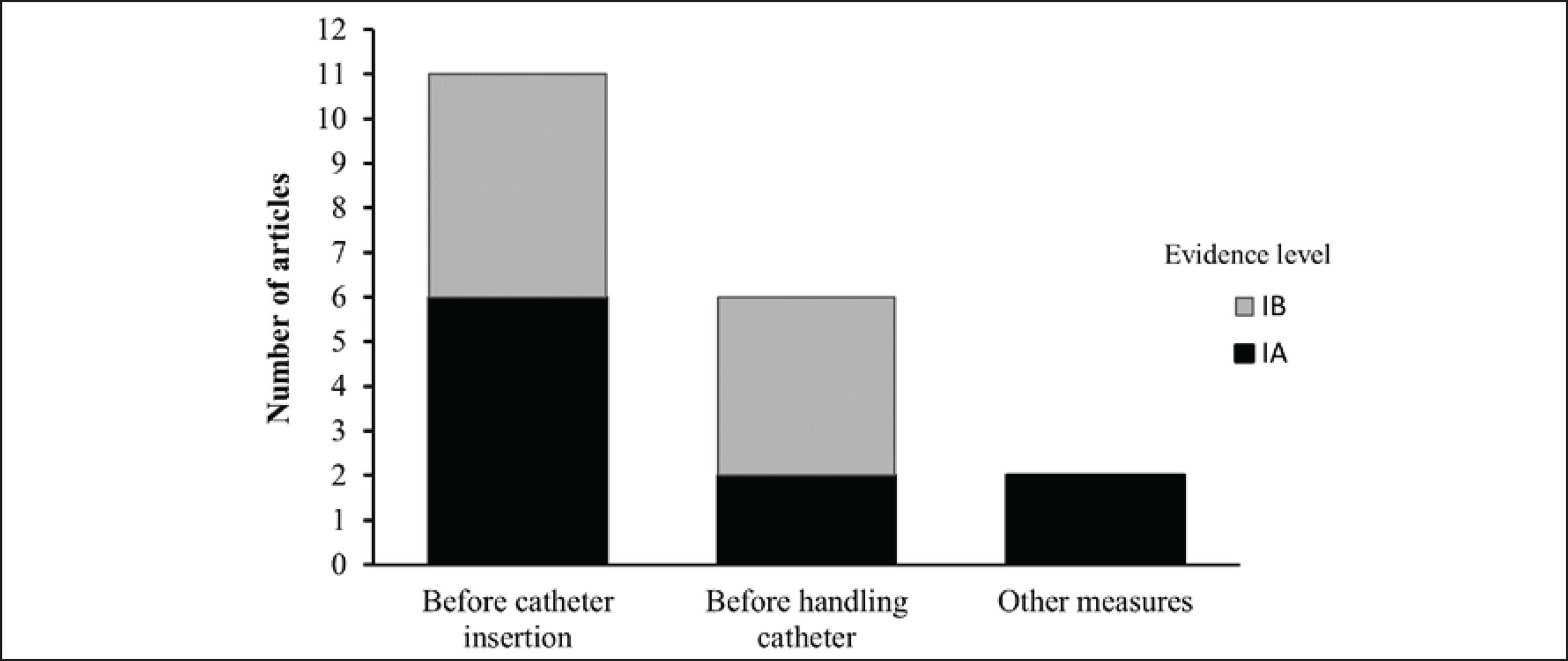
The frequency with which the measurements were described in the studies are shown in figure 1.
Frequency of measurements contained in bundles (interventions), observed in published studies. Belo Horizonte, MG, Brazil, 2016
The measurements contained in the bundle to prevent CVC-related infection were classified according to the levels of evidence and divided into categories IA, IB, IC and II, and with the subject unresolved.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
These classifications are used to demonstrate which preventive measures present the best scientific evidence for applicability in clinical practice, in isolation or when composing a bundle. Thus, the frequency of the adopted measurements in the studies analyzed at the time of their indication was based on the levels of evidence, according to figure 2.
Frequency of the adopted measurements in the studies analyzed, by level of evidence. Belo Horizonte, MG, Brazil, 2016
The number of measures that composed the bundle in each study with the duration of the intervention and the rate of reduction of CVC-related bloodstream infections after the bundle implementation were also related. The results are shown in figure 3.
Frequency of the adopted measurements in the studies analyzed, by duration of intervention and rate of reduction. Belo Horizonte, MG, Brazil, 2016
The impact of the bundle on reducing costs due to infection was measured in only two articles, with savings of US$539,902.00 and US$198,600.00 in each one after its implementation.1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
Although it is not the objective of this study, it is highlighted that agents related to the cause of CVD bloodstream infections were described in only 31% of the studies, including: Negative-Coagulase Staphylococcus, Staphylococcus aureus, Enterococcus spp, Klebsiella Pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Candida spp.1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
In the studies, 19 measures that compose bundles to prevent CVC-related bloodstream infections were found in the studies. Of these, 11 were used for catheter insertion, six during maintenance and two in continuing education and feedback of the results as a global part of the process.
Measures classified with levels of evidence AI were less used to compose the bundles. For example, for insertion of the CVC: preference for the subclavian vein (44%), avoidance of insertion in the femoral (37%), immediate removal of CVC without clinical indication (37%), CVC impregnated with antibiotic, designation of professionals qualified to use the CVC (12%). During catheter maintenance: skin asepsis when changing dressing (25%). And, like other measures: training and continuing education of professionals (62%) and feedback of results (31%).
DISCUSSION
The risk of bloodstream infection is also related to the catheter insertion site,77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
there is a greater prominence for insertion in the femoral and smaller for subclavian, whose predominant factor is the quantity and diversity of microorganisms found in each of the above mentioned regions.3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
Catheterization in the subclavian vein has been associated with a lower rate of infection compared to catheterization in the femoral. Studies in ICU in the United States, when comparing the infectious complications and the bacterial colonization of these two insertion sites, found that the incidence of infectious complications caused by insertion in the femoral site was 3.75 higher than in the subclavian and that the rate of colonization of the catheter was 20 % for the femoral site and 4% in the subclavian site.3232 Merrer J, Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically III patients a randomized controlled trial. JAMA [Internet]. 2001 Aug [cited 2016 May 07]; 286(6):700-7. Available from: http://jama.jamanetwork.com/article.aspx?articleid=194073
http://jama.jamanetwork.com/article.aspx...
-3333 Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med [Internet]. 2015 Sep [cited 2016 May 07]; 373:1220-9. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1500964#t=article
http://www.nejm.org/doi/full/10.1056/NEJ...
Another finding is the lack of emphasis on attention to the immediate removal of CVC without clinical indication. The CDC guidelines strongly recommend such a measure, since the risk of developing bloodstream infection increases with each day of use.3434 Burdeu G, Currey J, Pilcher D. Idle central venous catheter-days pose infection risk for patients after discharge from intensive care. Am J Infect Control [Internet]. 2014 Apr [cited 2016 Jun 07]; 42(4):453-55. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313013692
http://www.sciencedirect.com/science/art...
In a university hospital in the United States, CVC permanence and clinical indication was verified with the following inference: out of 1.433 catheters/day, 25% had no indication for use.3535 Tejedor SC, Tong D, Stein J, Payne C, Dressler D, Xue W et al. Temporary central venous catheter utilization patterns in a large tertiary care center: tracking the "idle central venous catheter". Infect Control Hosp Epidemiol [Internet]. 2012 Jan [cited 2016 May 13]; 33(1):50-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22173522
http://www.ncbi.nlm.nih.gov/pubmed/22173...
Similarly, in another North American study, the percentage of patients with an unnecessary CVC was 48.9%.3636 Tiwari MM, Hermsen ED, Charlton ME, Anderson JR, Rupp ME. Inappropriate intravascular device use: a prospective study. J Hosp Infect [Internet]. 2011 Jun [cited 2016 Jun 07]; 78(2):128-32. Available from: http://www.sciencedirect.com/science/article/pii/S0195670111001149
http://www.sciencedirect.com/science/art...
The use of the catheter without a clinical indication is considered a risk factor and rates of bloodstream infection can be dramatically reduced if CVC are evaluated daily in order to assess necessity and length of use and thus be removed immediately when they are no longer necessary.3636 Tiwari MM, Hermsen ED, Charlton ME, Anderson JR, Rupp ME. Inappropriate intravascular device use: a prospective study. J Hosp Infect [Internet]. 2011 Jun [cited 2016 Jun 07]; 78(2):128-32. Available from: http://www.sciencedirect.com/science/article/pii/S0195670111001149
http://www.sciencedirect.com/science/art...
The use of 0.5% chlorhexidine solution for CVC insertion site dressing change and asepsis has been recommended in order to prevent CVC-related infection by reducing local microbes. Chlorhexidine is widely used as an antiseptic in health care due to its excellent antimicrobial activity, its prolonged residual effect and its rapid action. Rates of bloodstream infection can be significantly reduced when asepsis is performed at each dressing change.3737 Weber DJ, Rutala WA. Central line-associated bloodstream infections: prevention and management. Infect Dis Clin North Am [Internet]. 2011 Mar [cited 2016 May 01]; 5(1):77-102. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21315995
http://www.ncbi.nlm.nih.gov/pubmed/21315...
-3838 Chen W, Li S, Li L, Wu X, Zhang W. Effects of daily bathing with chlorhexidine and acquired infection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus: a meta-analysis. J Thorac Dis. 2013 Aug [cited 2016 Jun 15]; 5(4):518-24. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3755671/
http://www.ncbi.nlm.nih.gov/pmc/articles...
With daily cleaning of the CVC insertion site with 2% chlorhexidine during one year of intervention, it was possible to obtain a 58% reduction in infection rates in an ICU of a public hospital in Chicago.3939 Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med [Internet]. 2007 Oct [cited 2016 Jun 15]; 167(19):2073-9. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=413356
http://archinte.jamanetwork.com/article....
Similarly, also in Chicago, the same intervention provided a 99% reduction in infections.4040 Munoz-Price LS, Hota B, Stemer A, Weinstein RA. Prevention of bloodstream infections by use of daily chlorhexidine baths for patients at a long-term acute care hospital. Infect Control Hosp Epidemiol [Internet]. 2009 Nov [cited 2016 Jun 15]; 30(11):1031-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19751155
http://www.ncbi.nlm.nih.gov/pubmed/19751...
Using a similar project, there was a 50% reduction of vancomycin-resistant Enterococcus sppand 32% for methicillin-resistant Staphylococcus aureus over a six-month period.4141 Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med [Internet]. 2009 Jun [cited 2016 Jun 15]; 37(6):1858-65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19384220
http://www.ncbi.nlm.nih.gov/pubmed/19384...
The use of chlorhexidine at each dressing exchange has been considered a simple practice to implement, with low cost and high impact In reducing bloodstream infections.4141 Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med [Internet]. 2009 Jun [cited 2016 Jun 15]; 37(6):1858-65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19384220
http://www.ncbi.nlm.nih.gov/pubmed/19384...
The continuing education and training programs of health professionals have been shown to be effective in preventing and reducing CVC-related infections, in addition to improving the quality of services provided. To ensure the quality of these programs, the following should be included: adequate CVC insertion and maintenance techniques, periodic assessment of knowledge, adherence to measures, infection surveillance and reporting, feedback on infection reduction and audit of the processes and results.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
,4242 Chesshyre E, Goff Z, Bowen A, Carapetis J. The prevention, diagnosis and management of central venous line infections in children. J infect [Internet]. 2015 Jun [cited 2016 Jul 07]; 71(1):59-75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25934326
http://www.ncbi.nlm.nih.gov/pubmed/25934...
-4343 Cherry RA, West CE, Hamilton MC, Rafferty CM, Hollenbeak CS, Caputo GM. Reduction of central venous catheter associated blood stream infections following implementation of a resident oversight and credentialing policy. Patient Saf Surg [Internet]. 2011 Jun [cited 2016 Jun 07]; 5:2-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123176/
http://www.ncbi.nlm.nih.gov/pmc/articles...
An educational intervention in the multidisciplinary team in the ICU of a Saint Louis hospital in the United States, which lasted for three years, addressed the recommended measures during the insertion and maintenance of the CVC, and resulted in the a 66% reduction of bloodstream infection.4444 Zack J. Zeroing in on zero tolerance for central line-associated bacteremia. Am J Infect Control [Internet]. 2008 Dec [cited 2016 Jul 07]; 36(10):176. Available from: http://www.sciencedirect.com/science/article/pii/S0196655308007992
http://www.sciencedirect.com/science/art...
It is therefore also important to only designate trained professionals who demonstrate competency for the insertion and maintenance of the CVC,77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
in addition to providing training with a global and multidisciplinary approach, including behavioral and educational interventions for the whole team involved in catheter insertion and maintenance.4545 Esposito S, Purrello SM, Bonnet E, Noveli A, Tripodi F, Pascale R. et al. Central venous catheter-related biofilm infections: an up-to-date focus on meticillin-resistant Staphylococcus aureus. J Glob Antimicrob Resist [Internet]. 2013 Apr [cited 2016 Jul 07]; 1(1):71-8. Available from: https://www.researchgate.net/publication/236889298
https://www.researchgate.net/publication...
Other measures were also composed in the bundles and presented a level of evidence IB, being strongly recommended for implementation,77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
such as: maximal sterile barrier precautions; skin asepsis, hand hygiene before insertion, use of ultrasound to guide the insertion of the catheter, allowing the antiseptic to dry before inserting the catheter and replacing the CVC without aseptic techniques within 48 hours. Measures associated with catheter maintenance were: to verify the need for CVC to remain, to monitor the insertion site, to disinfect the hub before administering medication, to replace the dressing with sterile gauze every two days, and to dress it every seven days or more when it is dirty, loose or moist and hand hygiene before handling.
The maximal sterile barrier precautions consists of sterile glove, cap, mask, apron and a sterile field, which contributes to reduce the microbial contamination of the professional and the environment for the patient at the time of insertion of the CVC and the subsequent risk of infection.4646 Matsui Y, Shimatani M, Kuzuhara K, Miyazaki Y, Horiuchi T, Tajima Y, et al. Three-year prospective, observational study of central line-associated bloodstream infections in a 600-bed Japanese acute care hospital. Am J Infect Control [Internet]. 2015 Feb [cited 2016 Jul 07]; 43(5):294-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25737305
http://www.ncbi.nlm.nih.gov/pubmed/25737...
The same occurs when the skin is cleaned before insertion of the catheter, where it is recommended to use chlorhexidine alcohol >0.5%, which should be allowed to dry before insertion of the CVC. Thus, it will promote a residual effect and reduce the spread of extra luminal microorganisms towards the catheter insertion site.4747 Garcia R. Surgical skin antisepsis. Perioperative Nursing Clinics [Internet]. 2011 Dec [cited 2016 Jul 07]; 5(4):457-77. Available from: http://www.periopnursing.theclinics.com/article/S1556-7931(10)00064-1/pdf
http://www.periopnursing.theclinics.com/...
Hand hygiene is one of the main measures to prevent HAI. Therefore, it is essential to sanitize them before insertion and manipulation of the CVC, to minimize the spread of pathogenic microorganisms by the hands of health professionals and the consequent contamination of the catheter.4848 World Health Organization. Evidence for Hand Hygiene Guidelines. [Internet]. 2016 [cited 2016 Jul 07]. Available from: http://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/
http://www.who.int/gpsc/tools/faqs/evide...
-4949 Garret Jr JH. Summary of evidence-based practices for bloodstream infection prevention across the health care continuum of care for vascular access clinicians: addressing the 3 common sources of health care-associated infection transmission. J Vasc Access [Internet]. 2016 Jun [cited 2016 Jul 07]; 21(2):72-4. Available from: http://www.sciencedirect.com/science/article/pii/S1552885516300265
http://www.sciencedirect.com/science/art...
The use of ultrasound to guide CVC insertion has been used in clinical practice to minimize the occurrence of mechanical complications, such as hemorrhage, pneumothorax, arrhythmias and arterial puncture. In addition, it has been shown to be able to reduce the duration of the procedure and the number of unnecessary attempts to cannulate the vein.5050 Ozakin E, Can R, Acar N, Balogu Kaya F, Cevik AA. An evaluation of complications in ultrasound-guided central venous catheter insertion in the emergency department. Turk J Emerg Med [Internet]. 2014 Feb [cited 2016 Jul 10]; 14(2):53-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909866/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-5151 Bayci AWL, Mangla J, Jenkins CS, Ivascu FA, Robbins JM. Novel educational module for subclavian central venous catheter insertion using real-time ultrasound guidance. J Surg Educ [Internet]. 2015 Nov-Dec [cited 2016 Jul 10]; 72(6):1217-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26481424
http://www.ncbi.nlm.nih.gov/pubmed/26481...
When adherence to aseptic technique cannot be guaranteed, i.e, catheters inserted in an emergency situation, these should be replaced within 48 hours due to increased possibility of bloodstream infection.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
Checking the need for the CVC becomes important so that the duration of the patient's use of the catheter can be monitored, since the length of CVC use is a risk factor for bloodstream infections and can also result in the CVC being removed immediately when there is no longer a clinical indication for its use. The insertion site should also be monitored. If the patient presents with sensitivity at the insertion site, fever or other manifestations suggestive of infection, the CVC should be evaluated and considered as a possible source of infection.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
Disinfection of the hub prior to administration of drugs should be done by alcoholic rubbing for 15 to 30 seconds in order to avoid / reduce the spread of the microorganisms present in the hub to the internal lumen of the catheter.5252 Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, et al. Epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect [Internet]. 2014 Jan [cited 2016 Jul 10]; 86(1):1-70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24330862
http://www.ncbi.nlm.nih.gov/pubmed/24330...
Due to its relevance, this practice became a campaign by the Association for Professionals in Infection Control and Epidemiology, called "Scrub the Hub," whose purpose was to reduce infections, educate, and encourage professionals to disinfect the hub carefully before any use, consequently it has been widely disseminated and recommended.5353 Association for professionals in infection control and epidemiology. Guide to the elimination of catheter-related bloodstream infections. Washington [Internet]. 2009 [cited 2016 Jul 10]. Available from: http://www.apic.org/Resource_/EliminationGuideForm/259c0594-17b0-459d-b395-fb143321414a/File/APIC-CRBSI-Elimination-Guide.pdf
http://www.apic.org/Resource_/Eliminatio...
-5454 Sannoh S, Clones B, Munoz J, Montecalvo M, Parvez B. A multimodal approach to central venous catheter hub care can decrease catheter-related bloodstream infection. Am J Infect Control [Internet]. 2010 Aug [cited 2016 Jul 20]; 36(8):424-29. Available from: http://www.sciencedirect.com/science/article/pii/S0196655309009493
http://www.sciencedirect.com/science/art...
The occlusive dressings should be replaced as recommended, as the moisture of the skin and the presence of dirt and secretions promote an environment conducive to microbial growth. Sterile gauze dressings should be changed within 48 hours, due to the difficulty in visualizing the insertion site and the possibility of dampening while bathing patients. The transparent polyurethane semipermeable dressing allows visualization of the insertion site and, therefore, requires less frequent changes, and thus can remain intact for seven days or whenever it gets dirty, loose or moist.5555 Frasca D, Dahyot-Fizelier C, Mimoz O. Prevention of central venous catheter-related infection in the intensive care unit. Crit Care [Internet]. 2010 Mar [cited 2016 Jul 20]; 14:212. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2887105/
http://www.ncbi.nlm.nih.gov/pmc/articles...
56 Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O'Grady NP, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol [Internet]. 2014 Jul [cited 2016 Jul 20]; 35(7):753-71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24915204
http://www.ncbi.nlm.nih.gov/pubmed/24915...
-5757 Oliveira FJG, Caetano JA, Silva VM, Almeida PC, Rodrigues AB, Siqueira JF. O uso de indicadores clínicos na avaliação das práticas de prevenção e controle de infecção de corrente sanguínea. Texto Contexto Enferm [Internet]. 2015 Out-Dez [cited 2016 Set 14]; 24(4):1018-26. Available from: http://www.scielo.br/pdf/tce/v24n4/pt_0104-0707-tce-24-04-01018.pdf.
http://www.scielo.br/pdf/tce/v24n4/pt_01...
The implementation and adherence of the measures contained in bundles, in addition to reducing infection rates, have a great economic impact on the costs caused due to infections, as evidenced by some studies analyzed, which showed a reduction of US$ 539,902.00 and US$ 198,600.00 relative to CVC-related bloodstream infections. NHSN and CDC estimates have shown that the annual costs generated due to HAI were approximately US$ 9.8 billion. Among the HAI, there are bloodstream infections, with a cost of US$ 45,814.00 per treatment. When these infections are associated with a resistant microorganism, for example methicillin-resistant Staphylococcus aureus, this cost increases to US$ 58,614.00. These data demonstrate the need to promote greater progress in the prevention of these infections, as well as to investigate and improve the quality of services provided as well as political efforts.5858 Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections a meta-analysis of costs and financial impact on the us health care system. JAMA Intern Med [Internet]. 2013 Dec [cited 2016 Jul 20]; 173(22):2039-46. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=1733452
http://archinte.jamanetwork.com/article....
CONCLUSION
The implementation of bundles has been shown to reduce CVC-related bloodstream infections, regardless of intervention time and the number of measures used. However, there were variations in the studies in relation to: number of measures implemented, duration and reduction of infection rates. There was no direct relationship between the number of measures described in the studies or the longest implementation time, and the highest rates of infection reduction. It is possible that this finding cannot be explained directly, due to aspects that were not presented by the authors of the studies, such as team motivation, institutional safety culture, feedback of results to professionals and training.
REFERÊNCIAS
-
1World Health Organization. Report on the burden of endemic health care-associated infection worldwide. A systematic review of the literature. [Internet]. 2011[cited 2016 Jun 07]. Available from: http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf
» http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf -
2Agência Nacional de Vigilância Sanitária. Medidas de prevenção de infecção relacionada à assistência à saúde. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2013:1-87.
-
3National Healthcare Safety Network. NHSN Central Line-associated Bloodstream Infection Surveillance in 2014. National Center for Emerging and Zoonotic Infectious Diseases. [Internet]. 2014 Mar [cited 2016 Feb 02]. Available from: http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf
» http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf -
4National Healthcare Safety Network. Patient Safety Component Manual [Internet]. 2017 Jan [cited 2017 Feb 14]. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf
» https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf -
5Mok Q. How I diagnose and manage catheter-associated blood stream infections. J Paediatr Child Health [Internet]. 2015 May [cited 2016 Jun 07]; 25(5):243-4. Available from: http://www.paediatricsandchildhealthjournal.co.uk/article/S1751-7222(14)00223-6/pdf
» http://www.paediatricsandchildhealthjournal.co.uk/article/S1751-7222(14)00223-6/pdf -
6Martínez-Morel HR, Sánchez-Payá J, Molina-Gómez MJ, García-Shimizu P, García RV, Villanueva-Ruiz C, et al. Catheter-related bloodstream infection: burden of disease in a tertiary hospital. J Hosp Infect [Internet]. 2014 Jul [cited 2016 Feb 02]; 87(3):165-70. Available from: http://www.sciencedirect.com/science/article/pii/S0195670114001285
» http://www.sciencedirect.com/science/article/pii/S0195670114001285 -
7Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
» http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf -
8Agência Nacional de Vigilância Sanitária. Avaliação dos indicadores nacionais de infecção relacionada à assistência ano de 2014 e relatório de progresso. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2015.
-
9Souza ES, Belei RA, Carrilho CMDM, Matsuo T, Yamada-Ogatta SF, Andrade G et al. Mortalidade e riscos associados a infecção relacionada à assistência à saúde. Texto Contexto Enferm [Internet]. 2015 Jan-Mar [cited 2017 Feb 14]; 24(1): 220-8. Available from: http://www.redalyc.org/pdf/714/71438421027.pdf
» http://www.redalyc.org/pdf/714/71438421027.pdf -
10The Joint Commission. Preventing central line-associated bloodstream infections: a global challenge, a global perspective. Oak Brook, IL: Joint Commission Resources. [Internet]. 2012 May [cited 2016 Feb 02]. Available from: https://www.jointcommission.org/assets/1/18/CLABSI_Monograph.pdf
» https://www.jointcommission.org/assets/1/18/CLABSI_Monograph.pdf -
11Institute for Health Improvement. Protecting 5 million lives. Cambridge [Internet]. 2004 [cited 2016 Jun 07]. Available from: http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx
» http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx -
12Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
» http://www.ncbi.nlm.nih.gov/pubmed/26138518 -
13Labeau SO, Vandijck DM, Rello J, Adam S, Rosa A, Wenisch C, et al. Centers for Disease Control and Prevention guidelines for preventing central venous catheter-related infection: results of a knowledge test among 3405 European intensive care nurses. Crit Care Med [Internet]. 2009 Jan [cited 2016 Jun 07]; 37(1):320-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19050628
» http://www.ncbi.nlm.nih.gov/pubmed/19050628 -
14Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
» http://www.ncbi.nlm.nih.gov/pubmed/24576582 -
15Santos CMC, Pimenta CAM, Nobre MRC. A estratégia PICO para a construção da pergunta de pesquisa e busca de evidências. Rev Latino-Am. Enfermagem [Internet]. 2007 Jun [cited 2016 Aug 01]; 15(3):508-11. Available from: http://www.scielo.br/scielo.php?pid=S0104-11692007000300023&script=sci_arttext&tlng=pt
» http://www.scielo.br/scielo.php?pid=S0104-11692007000300023&script=sci_arttext&tlng=pt -
16Stetler CB, Morsi D, Rucki S, Broughton S, Corrigan B, Fitzgerald J, et al. Utilization-focused integrative reviews in a nursing service. Appl Nurs Res [Internet]. 1998 Nov [cited 2016 Mar 01]; 11(4):1-11. Available from: http://www.appliednursingresearch.org/article/S0897-1897(98)80329-7/pdf
» http://www.appliednursingresearch.org/article/S0897-1897(98)80329-7/pdf -
17Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
» http://www.sciencedirect.com/science/article/pii/S0196655311000903 -
18Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
» http://www.iqg.com.br/pbsp/img_up/01305809324.pdf -
19Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
» http://www.sciencedirect.com/science/article/pii/S0952818012002450 -
20Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/ -
21Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/ -
22Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
» http://www.sciencedirect.com/science/article/pii/S0964339712001279 -
23Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
» http://www.ncbi.nlm.nih.gov/pubmed/24485369 -
24Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
» http://www.sciencedirect.com/science/article/pii/S0196655314001710 -
25Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/ -
26Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
» http://www.sciencedirect.com/science/article/pii/S0196655314007974 -
27Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
» http://www.ncbi.nlm.nih.gov/pubmed/24837115 -
28Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
» http://www.sciencedirect.com/science/article/pii/S0196655313012029 -
29Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/ -
30Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
» http://www.ncbi.nlm.nih.gov/pubmed/25758694 -
31Polderman KH, Girbes AJ. Central venous catheter use. Part 1: mechanical complications. Intensive Care Med [Internet]. 2002 Jan [cited 2016 May 07]; 28(1):1-17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11818994
» http://www.ncbi.nlm.nih.gov/pubmed/11818994 -
32Merrer J, Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically III patients a randomized controlled trial. JAMA [Internet]. 2001 Aug [cited 2016 May 07]; 286(6):700-7. Available from: http://jama.jamanetwork.com/article.aspx?articleid=194073
» http://jama.jamanetwork.com/article.aspx?articleid=194073 -
33Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med [Internet]. 2015 Sep [cited 2016 May 07]; 373:1220-9. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1500964#t=article
» http://www.nejm.org/doi/full/10.1056/NEJMoa1500964#t=article -
34Burdeu G, Currey J, Pilcher D. Idle central venous catheter-days pose infection risk for patients after discharge from intensive care. Am J Infect Control [Internet]. 2014 Apr [cited 2016 Jun 07]; 42(4):453-55. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313013692
» http://www.sciencedirect.com/science/article/pii/S0196655313013692 -
35Tejedor SC, Tong D, Stein J, Payne C, Dressler D, Xue W et al. Temporary central venous catheter utilization patterns in a large tertiary care center: tracking the "idle central venous catheter". Infect Control Hosp Epidemiol [Internet]. 2012 Jan [cited 2016 May 13]; 33(1):50-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22173522
» http://www.ncbi.nlm.nih.gov/pubmed/22173522 -
36Tiwari MM, Hermsen ED, Charlton ME, Anderson JR, Rupp ME. Inappropriate intravascular device use: a prospective study. J Hosp Infect [Internet]. 2011 Jun [cited 2016 Jun 07]; 78(2):128-32. Available from: http://www.sciencedirect.com/science/article/pii/S0195670111001149
» http://www.sciencedirect.com/science/article/pii/S0195670111001149 -
37Weber DJ, Rutala WA. Central line-associated bloodstream infections: prevention and management. Infect Dis Clin North Am [Internet]. 2011 Mar [cited 2016 May 01]; 5(1):77-102. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21315995
» http://www.ncbi.nlm.nih.gov/pubmed/21315995 -
38Chen W, Li S, Li L, Wu X, Zhang W. Effects of daily bathing with chlorhexidine and acquired infection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus: a meta-analysis. J Thorac Dis. 2013 Aug [cited 2016 Jun 15]; 5(4):518-24. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3755671/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3755671/ -
39Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med [Internet]. 2007 Oct [cited 2016 Jun 15]; 167(19):2073-9. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=413356
» http://archinte.jamanetwork.com/article.aspx?articleid=413356 -
40Munoz-Price LS, Hota B, Stemer A, Weinstein RA. Prevention of bloodstream infections by use of daily chlorhexidine baths for patients at a long-term acute care hospital. Infect Control Hosp Epidemiol [Internet]. 2009 Nov [cited 2016 Jun 15]; 30(11):1031-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19751155
» http://www.ncbi.nlm.nih.gov/pubmed/19751155 -
41Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med [Internet]. 2009 Jun [cited 2016 Jun 15]; 37(6):1858-65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19384220
» http://www.ncbi.nlm.nih.gov/pubmed/19384220 -
42Chesshyre E, Goff Z, Bowen A, Carapetis J. The prevention, diagnosis and management of central venous line infections in children. J infect [Internet]. 2015 Jun [cited 2016 Jul 07]; 71(1):59-75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25934326
» http://www.ncbi.nlm.nih.gov/pubmed/25934326 -
43Cherry RA, West CE, Hamilton MC, Rafferty CM, Hollenbeak CS, Caputo GM. Reduction of central venous catheter associated blood stream infections following implementation of a resident oversight and credentialing policy. Patient Saf Surg [Internet]. 2011 Jun [cited 2016 Jun 07]; 5:2-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123176/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123176/ -
44Zack J. Zeroing in on zero tolerance for central line-associated bacteremia. Am J Infect Control [Internet]. 2008 Dec [cited 2016 Jul 07]; 36(10):176. Available from: http://www.sciencedirect.com/science/article/pii/S0196655308007992
» http://www.sciencedirect.com/science/article/pii/S0196655308007992 -
45Esposito S, Purrello SM, Bonnet E, Noveli A, Tripodi F, Pascale R. et al. Central venous catheter-related biofilm infections: an up-to-date focus on meticillin-resistant Staphylococcus aureus. J Glob Antimicrob Resist [Internet]. 2013 Apr [cited 2016 Jul 07]; 1(1):71-8. Available from: https://www.researchgate.net/publication/236889298
» https://www.researchgate.net/publication/236889298 -
46Matsui Y, Shimatani M, Kuzuhara K, Miyazaki Y, Horiuchi T, Tajima Y, et al. Three-year prospective, observational study of central line-associated bloodstream infections in a 600-bed Japanese acute care hospital. Am J Infect Control [Internet]. 2015 Feb [cited 2016 Jul 07]; 43(5):294-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25737305
» http://www.ncbi.nlm.nih.gov/pubmed/25737305 -
47Garcia R. Surgical skin antisepsis. Perioperative Nursing Clinics [Internet]. 2011 Dec [cited 2016 Jul 07]; 5(4):457-77. Available from: http://www.periopnursing.theclinics.com/article/S1556-7931(10)00064-1/pdf
» http://www.periopnursing.theclinics.com/article/S1556-7931(10)00064-1/pdf -
48World Health Organization. Evidence for Hand Hygiene Guidelines. [Internet]. 2016 [cited 2016 Jul 07]. Available from: http://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/
» http://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/ -
49Garret Jr JH. Summary of evidence-based practices for bloodstream infection prevention across the health care continuum of care for vascular access clinicians: addressing the 3 common sources of health care-associated infection transmission. J Vasc Access [Internet]. 2016 Jun [cited 2016 Jul 07]; 21(2):72-4. Available from: http://www.sciencedirect.com/science/article/pii/S1552885516300265
» http://www.sciencedirect.com/science/article/pii/S1552885516300265 -
50Ozakin E, Can R, Acar N, Balogu Kaya F, Cevik AA. An evaluation of complications in ultrasound-guided central venous catheter insertion in the emergency department. Turk J Emerg Med [Internet]. 2014 Feb [cited 2016 Jul 10]; 14(2):53-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909866/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909866/ -
51Bayci AWL, Mangla J, Jenkins CS, Ivascu FA, Robbins JM. Novel educational module for subclavian central venous catheter insertion using real-time ultrasound guidance. J Surg Educ [Internet]. 2015 Nov-Dec [cited 2016 Jul 10]; 72(6):1217-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26481424
» http://www.ncbi.nlm.nih.gov/pubmed/26481424 -
52Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, et al. Epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect [Internet]. 2014 Jan [cited 2016 Jul 10]; 86(1):1-70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24330862
» http://www.ncbi.nlm.nih.gov/pubmed/24330862 -
53Association for professionals in infection control and epidemiology. Guide to the elimination of catheter-related bloodstream infections. Washington [Internet]. 2009 [cited 2016 Jul 10]. Available from: http://www.apic.org/Resource_/EliminationGuideForm/259c0594-17b0-459d-b395-fb143321414a/File/APIC-CRBSI-Elimination-Guide.pdf
» http://www.apic.org/Resource_/EliminationGuideForm/259c0594-17b0-459d-b395-fb143321414a/File/APIC-CRBSI-Elimination-Guide.pdf -
54Sannoh S, Clones B, Munoz J, Montecalvo M, Parvez B. A multimodal approach to central venous catheter hub care can decrease catheter-related bloodstream infection. Am J Infect Control [Internet]. 2010 Aug [cited 2016 Jul 20]; 36(8):424-29. Available from: http://www.sciencedirect.com/science/article/pii/S0196655309009493
» http://www.sciencedirect.com/science/article/pii/S0196655309009493 -
55Frasca D, Dahyot-Fizelier C, Mimoz O. Prevention of central venous catheter-related infection in the intensive care unit. Crit Care [Internet]. 2010 Mar [cited 2016 Jul 20]; 14:212. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2887105/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2887105/ -
56Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O'Grady NP, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol [Internet]. 2014 Jul [cited 2016 Jul 20]; 35(7):753-71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24915204
» http://www.ncbi.nlm.nih.gov/pubmed/24915204 -
57Oliveira FJG, Caetano JA, Silva VM, Almeida PC, Rodrigues AB, Siqueira JF. O uso de indicadores clínicos na avaliação das práticas de prevenção e controle de infecção de corrente sanguínea. Texto Contexto Enferm [Internet]. 2015 Out-Dez [cited 2016 Set 14]; 24(4):1018-26. Available from: http://www.scielo.br/pdf/tce/v24n4/pt_0104-0707-tce-24-04-01018.pdf
» http://www.scielo.br/pdf/tce/v24n4/pt_0104-0707-tce-24-04-01018.pdf -
58Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections a meta-analysis of costs and financial impact on the us health care system. JAMA Intern Med [Internet]. 2013 Dec [cited 2016 Jul 20]; 173(22):2039-46. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=1733452
» http://archinte.jamanetwork.com/article.aspx?articleid=1733452
Publication Dates
-
Publication in this collection
2018
History
-
Received
23 Sept 2016 -
Accepted
20 Mar 2017